1. Introduction
Worldwide, up to 22% of youth have experienced physical abuse, and up to 18% have experienced sexual abuse (Stoltenborgh et al., 2015). Research on risk factors for childhood abuse (physical/sexual abuse before age 18) has mostly been conducted in community studies, identifying multiple sociodemographic risk factors including: female sex, older age, non-White race, low Socio-Economic Status (SES), parental education and social support, high family conflict, and presence of parental abuse history (Black et al., 2001a; Black et al., 2001b; Stith et al., 2009; White et al., 2015).
Abuse early in development is associated with severe adverse outcomes across the lifespan in multiple domains, including physical health (e.g., diabetes, pain conditions), psychosocial functioning (e.g., cognitive dysfunction, relationship problems), and mental health (e.g., substance use, disruptive behaviors) (Carr et al., 2018b; Felitti et al., 2019). Regarding mental health outcomes specifically, 45% of adults with psychopathology retrospectively report some type of childhood maltreatment, with 19% reporting multiple forms of abuse (Nelson et al., 2017).
Extensive research has specifically focused on the association of childhood abuse and Bipolar Disorder (BD). Two large meta-analyses indicate up to 57% of adults with BD report history of childhood abuse (9%−33% physical abuse, and 9%−40% sexual abuse) (Agnew-Blais and Danese, 2016; Daruy-Filho et al., 2011); among youth with BD, 3–20 % report physical abuse history, and 7–29% report sexual abuse history (Benarous et al., 2017; Conus et al., 2010; Daglas et al., 2014; Du rocher Schudlich, 2015; Maniglio, 2013b; Romero et al., 2009; Rucklidge, 2006). In our prior cross-sectional analysis from the Course and Outcome of Bipolar Youth (COBY) study, a multi-site longitudinal naturalistic study of youth with childhood-onset BD followed into adulthood, we documented rates of abuse using retrospective data gathered at study intake. Twenty-one percent of participants reported physical and/or sexual abuse history (9%physical, 7% sexual and 5% both), demographic and clinical correlates of abuse included living with non-intact families, history of psychosis, comorbid Post Traumatic Stress Disorder (PTSD) and Conduct Disorder (CD), and family history of mood disorders (Romero et al., 2009).
Thus far, the BD literature mainly documents detrimental associations of abuse and BD course (e.g., increased suicidality, mood recurrences, more comorbidity) (Cazala et al., 2019; Daruy-Filho et al., 2011; Marchand et al., 2005; Palmier-Claus et al., 2016; Rucklidge, 2006). Yet, to the best of our knowledge, no study to date has examined the specific risk factors (which by definition must be present prior to the outcome) that temporally precede new onset childhood abuse among youth with BD. The study of such risk factors requires prospective data to enable the identification of youth at risk for abuse, and in turn inform strategies that may mitigate long-term effects.
In the few longitudinal studies with this population, youth with BD with abuse history had worse family environment, more comorbid anxiety, mood recurrences, general distress, hopelessness, and severe mood episodes, as well as a decreased response to treatment (Conus et al., 2010; Daglas et al., 2014; Du rocher Schudlich, 2015; Neria et al., 2005). A recent COBY prospective analysis investigated the effects of severe lifetime traumatic events, including abuse, on the longitudinal course of BD among youth (Andreu Pascual et al., 2020). This study prospectively followed youth with BD and examined the associations of different types of lifetime traumatic events (e.g., accidents, death, abuse) with mood and functioning over time, demonstrating that those with more traumatic experiences had poorer psychosocial functioning, worse mood symptoms, increased mood recurrences and comorbidities. Critically, the prospective data allowed investigation of time-varying mood changes before and after the abuse. Specifically, abused participants showed greater suicidality, Substance Use Disorder (SUD), and worsening mood symptoms, specifically hypo/mania after abuse occurrence. However, this study did not evaluate specific prospective risk factors for abuse among COBY youth. Although informative, the above noted studies have one or more of the following limitations: 1) most are retrospective; 2) many lack repeated assessments that would enable temporal clarity; 3) mainly limited to community (vs clinical) samples, and largely involved children in Child Protective Services (CPS, presumably most severe cases); 4) confounding variables such as age, race or SES are not always accounted for; and 5) the research designs prohibit the analysis of temporal associations between past and prospectively ascertained factors that precede new onset abuse. Thus, prospective studies that identify risk factors that precede new onset physical and/or sexual abuse among youth with BD are warranted. Such data, while critical to inform providers and policy makers of future abuse in this high-risk group does not provide evidence of causality.
The prospective design of COBY allows us to provide new insights in the BD youth literature and to extend prior COBY findings by: 1) identifying past and intake risk factors for new onset physical and/or sexual abuse among COBY youth with BD (n=279) followed for an average of 12 years; 2) conducting, to the best of our knowledge, the first examination of predictors that temporally precede new onset physical and/or sexual abuse among youth with BD over follow-up. Given the above literature, we hypothesized that: 1) past and intake predictors for new onset abuse during follow-up would include sociodemographic and clinical factors previously identified in the literature, including low SES, lack of social support, more severe mood symptoms, increased comorbid disorders and female sex; 2) Although there are no prior studies that evaluate near-term predictors for new onset abuse, based on clinical experience and distal literature, we hypothesized that predictors ascertained during follow-up preceding new onset abuse would similarly involve variables associated with abuse in prior studies, including age, female sex, low SES, living with one parent, presence of comorbid disorders and family psychopathology.
2. Methods
2.1. Participants
Details of the COBY sample are described elsewhere (Axelson et al., 2006; Birmaher et al., 2014). Briefly, from October 2000 through July 2006, COBY enrolled 446 participants through three academic medical centers: Brown University (n=144), University of California at Los Angeles (UCLA) (n=90), and University of Pittsburgh (n=204). Participants were ages 7 to 17 years 11 months at intake (mean=12.7 ± 3.2 years, 53% males, 82% White), who met Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) (Association, 2004) criteria for BD-I (n = 260), BD-II (n = 32), or BD-Not Otherwise Specified (NOS) based on the COBY operationalized definition (n = 154) (see(Axelson et al., 2006)). BD onset age was defined by any DSM-IV mood episode onset or an episode fulfilling COBY BD-NOS criteria. Participants were enrolled regardless of current mood state, and recruited from outpatient clinics (84.4%), inpatient units (4.4%), advertisements (6.7%), and other provider referral (4.4%) at the three sites. Youth with schizophrenia, intellectual disability, autism, and mood disorders secondary to medical conditions or substance use were excluded from the study.
The present analysis includes 279 participants who completed at least 4 years of follow-up assessments and had at least one follow-up assessment before age 18 (mean age throughout follow-up=18.0, range 7–32). Participants were prospectively interviewed on average every 7 months, for an average of 12 years, with a 90% retention rate. Included participants were significantly younger (Cohen’s d=0.47, p<0.0001) and had earlier BD onset (Cohen’s d=0.23, p=0.03), compared to excluded participants.
2.2. Procedure
Each University’s Institutional Review Board approved the study before enrollment, and informed consent/assent was obtained from participants and parents/primary caregivers at intake. Trained COBY staff administered semi-structured interview assessments to participants and parents. Participants aged≥18 chose whether to include parents/secondary informants in study interviews. Following assessment, research staff reviewed ratings with a study investigator that yielded final consensus ratings.
2.2.1. Measures
At intake, participants/parents were interviewed for presence of current and lifetime psychopathology using the Kiddie Schedule for Affective Disorders and Schizophrenia Present and Lifetime Version (K-SADS-PL) (Kaufman et al., 1997). Mood symptom severity was assessed through the K-SADS Mania Rating Scales (K-MRS) (Axelson et al., 2003) and depression section of the K-SADS-P (K-DRS), both derived from the K-SADS-Present Episode mood disorder section (K-SADS-P; 4th revision) (Chambers et al., 1985). Diagnostic interrater agreement was high for the K-SADS-PL (range 93%−100%). The intraclass correlation coefficients (ICC) for the K-SADS-MRS, K-SADS-DEP-P were ≥0.83. Kendall’s concordance coefficients W were 0.85 for major depressive disorder and 0.78 for mania/hypomania.
Week-by-week longitudinal changes in psychiatric symptoms were assessed using the Adolescent Longitudinal Interval Follow-Up Evaluation (A-LIFE) (Keller et al., 1987), Psychiatric Status Rating Scale (PSR). PSRs use numeric values linked to DSM-IV criteria, ranging 1–6 for mood disorders (scores indicate, respectively: ≤2euthymia, 3–4subsyndromal symptoms, ≥5syndromal symptoms). Full recovery was defined as 8 consecutive weeks with PSR score ≤2 (minimal/no mood symptoms). Recurrence was defined as PSR ≥5, with 1-week duration for mania/hypomania and 2-weeks for depression. PSR reliability for percentage of time meeting full DSM-IV criteria for a mood episode yielded ICC=0.85; without mood symptoms ICC=0.82. Reliability for PSR mood disorder ratings over COBY course=0.8 (Kendall’s W).
At intake, presence of lifetime (past/current) physical and/or sexual abuse was obtained using the PTSD section of the K-SADS-PL. Questions for evaluating physical abuse were: “When your parents got mad at you, did they hit you?”, “Have you ever been hit so that you had bruises or marks on your body, or were hurt in some way?” Inclusion criteria were bruises/injuries sustained on more than one occasion. Questions for evaluating sexual abuse were: “Did anyone ever touch you in your private parts when they shouldn’t have?”, “Has someone ever touched you in a way that made you feel bad?”, “Has anyone who shouldn’t have ever made you undress, touch you between the legs, make you get in bed with him/her, or make you play with his private parts?”, “Was Child, Youth and Family Services ever involved with your family?”. Inclusion criteria were isolated/repeated incidents of genital fondling, oral sex, vaginal or anal intercourse.
During follow-up, presence of lifetime physical and sexual abuse was assessed regularly using the Traumatic Events Screen (TES), a brief interview including the 11 items derived from the PTSD section of the K-SADS-PL (Kaufman et al., 1997), plus an additional item (victim of intimate partner violence). The TES documented severe events, including being victim of a violent crime (including physical/sexual assault) and experiencing physical/sexual abuse, among others. Abuse by a caregiver was coded as physical/sexual abuse; abuse by a significant other as intimate partner violence. The events in the TES are answered: yes/no. Events were ascertained at each follow-up separately for parents and participants, and a summary score was determined. In general, if parent/participant endorsed an event, the summary score was considered positive. If an event was reported, the interviewer recorded the total number of occurrences, dates of the first, second and most recent event. If there was discrepancy between informants, further clarification was obtained. If parent reported an event as traumatic, but participant indicated he/she did not perceive this as traumatic, the event was not given a positive score. Correlations between summary scores and parent/participant reports indicate summary scores depended more heavily on participants’ than parents’ reports (Spearman correlations=0.95 and 0.72, respectively). Spearman correlation between parents’ and participants’ reports was 0.59.
SES was ascertained using the 4-factor Hollingshead Scale at intake and during follow-up (Hollingshead, 1975). Participants’ psychosocial functioning was assessed at intake via the Children’s Global Assessment Scale (CGAS) (< age 22) (Shaffer et al., 1983), and over follow-up via the Global Assessment of Functioning (GAF) (> age 22) (Jones et al., 1995); psychosocial functioning in specific domains was assessed over follow-up using the A-LIFE Psychosocial Functioning Scale (PSF) (Keller et al., 1987). Interpersonal relationships were evaluated on the past 6 months, both for family and friends, and rated according to quality from 1 (very good: had several special friends/family members that he/she saw regularly and frequently and felt close to) to 5 (very poor: had no special friends/family members and practically no social contacts). The parent was interviewed at intake about personal psychiatric history using the Structured Clinical Interview for DSM-IV (SCID-IV) (First, 1996), and psychiatric status of first/second degree relatives was ascertained using an enhanced version of the Family History Screen (Weissman et al., 2000). Each participant and parent completed the Conflict Behavior Questionnaire (CBQ) to assess family conflict (Robin and Foster, 1989) and Family Adaptability and Cohesion Evaluation Scale-II (FACES-II) (Olsen et al., 1985) to assess family environment. The Life Events Checklist (LEC) assessed for the presence of negative and positive life events, and impact on the participant’s wellbeing, over the last 12 months at each assessment (Johnson and McCuthcheon, 1980).
2.3. Statistical Analyses
Given the differences in the nature of childhood vs. adulthood abuse and the potential differences in risk factors, COBY participants who did not have a follow-up assessment before age 18 were excluded from the analyses of childhood abuse unless they reported abuse that occurred before age 18.
To identify the strongest predictors of childhood abuse risk, Cox proportional hazards regression modeled age of first abuse (right-censoring at age 18) implementing Least Absolute Shrinkage and Selection Operator (LASSO) for feature selection (Hastie et al., 2009). Briefly, a LASSO is a modified form of linear or generalized linear regression that penalizes overfit models via a regularization parameter that proportionally shrinks predictor magnitude coefficients toward zero, and for less important predictors, coefficients shrink to zero. Thus, predictor selection is implicitly performed, as less important variables are removed from the model without potential biases of other variable selection techniques, such as multiple comparisons and collinearity between predictor variables. Multiple imputation was used to impute missing values (five iterations); LASSO was separately implemented within each imputation iteration (lambdas selected via three-fold cross-validation within each iteration), and results were pooled across the five iterations (van Buuren S, 2011). Lastly, the stability of LASSO results was assessed by bootstrapping (Hastie et al., 2015; Schomaker and Heumann, 2018), the process described above (1000 iterations with multiple imputation and pooled LASSO uniquely implemented within each iteration) and computing the percent of iterations in which each predictor was retained (higher percentages indicate more stable, and consistently influential predictors). Predictor variables entered into the analysis were chosen based on the literature, including demographic, clinical, and family history factors, and hypothesized interactive effects between predictors including: social support as a protective factor, family history of substance abuse as a risk factor among low SES families, and more negative life events associated with abuse risk in families with worse family functioning. All baseline models controlled for age at intake.
Follow-up prediction models similarly identified factors preceding new onset physical/sexual abuse (as well as non-event censored cases). These models were useful for identifying changes that occurred in close temporal proximity (as per last follow-up interview) to first instance of abuse, including all clinical symptomatology (diagnosis, and relevant clinical variables) and any demographic changes occurring during the prior follow-up period.
3. Results
3.1. New onset abuse during follow-up
For this analysis, to ensure that past/intake predictors preceded the abuse, we excluded participants with abuse history prior to intake (n=75). This analysis includes 279 participants (44% female, 83% White) with BD-I (57%), BD-II (7%), and BD-NOS (35%). Of these, 42/279 (15%) reported new onset abuse during follow-up (62% physical, 26% sexual; 12% both), of which 20 (48%) had one instance of abuse and 22 (52%) had two or more. Sociodemographic and clinical characteristics of the included sample are noted in Table 1.
Table 1.
Sociodemographic and clinical characteristics of the included participants
| Demographics at intake | Mean (SD) or N (%) |
|---|---|
| Age | 12.14 (3.11) |
| Sex (Female) | 124 (44.44) |
| Race (White) | 231 (82.80) |
| SES | 3.43 (1.19) |
| Living Situation | |
| Both Biological Parents | 127 (45.52) |
| One Biological Parent | 130 (46.59) |
| Other (e.g., grandparents) | 22 (7.89) |
| Maternal Age at Child’s Birth | 27.05 (5.90) |
|
| |
| Lifetime (past, intake, follow-up Categorical diagnosis) | N (%) |
|
| |
| Bipolar Disorder | |
| BD-I | 193 (69.18) |
| BD-II | 41 (14.70) |
| BD-NOS | 45 (16.13) |
| Age of BD Onset | 8.99 (3.73) |
| ADHD | 193 (69.18) |
| DBD | 181 (64.87) |
| Anxiety Disorders | 204 (73.12) |
| PTSD | 46 (16.49) |
| SUD | 110 (39.43) |
| Psychosis | 95 (34.05) |
| Suicidal Ideation and/or Attempts | 213 (76.34) |
|
| |
| Family History | N (%) |
|
| |
| Depression | 246 (88.17) |
| Mania | 166 (59.5) |
| ADHD | 133 (47.67) |
| Conduct Disorder | 98 (35.13) |
| Schizophrenia | 19 (6.81) |
| Psychosis | 48 (17.2) |
| Anxiety | 214 (76.7) |
| SUD | 191 (68.46) |
| Suicidality | 146 (52.33) |
Abbreviations: ADHD= Attention Deficit Hyperactivity Disorder; BD= Bipolar Disorder; DBD= Disruptive Behavior Disorder (including Conduct Disorder [CD] and/or Oppositional Defiant Disorder [ODD]); PTSD= Post traumatic Stress Disorder; SES= Hollingshead Socioeconomic Status; SUD= Substance Use Disorder.
a). Past/intake predictors for new onset abuse during follow-up
Physical abuse.
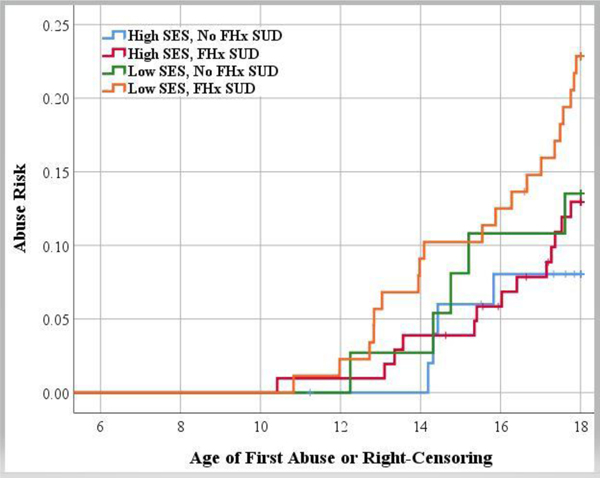
LASSO selection of the Cox proportional hazards regression predictor variables for physical abuse showed participants with more severe depressive symptoms (HR=1.29, 95% of iterations) and those with an interaction between low SES and family history of SUD were at higher risk for physical abuse over follow-up (inverted HR=1.19, 85% of iterations) than participants without presence of those factors (Figure 1). Notably, 79% of participants who suffered physical abuse had family history of SUD, and in 65% of those cases, at least one of the family members with SUD was a parent.
Figure 1: LASSO Evaluated Socioeconomical Status and Family History of Substance Use Disorders Predicting Risk for New Onset Physical/Sexual Abuse.
Abbreviations: FHx = Family History; LASSO = Least Absolute Shrinkage and Selection Operator ;SES = Socioeconomic Status, SUD = Substance Use Disorder.
Note: Unlike in the prediction models, SES was dichotomized in the plot above to improve interpretability. Models evaluated through LASSO.
Sexual abuse.
The strongest predictor of sexual abuse selected by LASSO was female sex (HR=2.41, 97% of iterations) (Table 2).
Table 2.
LASSO Selected Predictors of Risk for Abuse (Physical and/or Sexual)
| Physical Abuse |
Sexual Abuse |
|||
|---|---|---|---|---|
| Pooled | % of | Pooled | %of | |
| HR1 | Iterations | HR | Iterations | |
| Selected | Selected | |||
| Past and intake predictors for new onset abuse during follow-up | ||||
|
| ||||
| Sex (Female vs. Male) | --- | --- | 2.41 | 97% |
| DRS | 1.29 | 95% | --- | --- |
| SES x Family History of SUD Interaction | 0.84 | 85% | --- | --- |
|
| ||||
| Predictors ascertained during follow-up that preceded new onset abuse | ||||
|
| ||||
| Current Age 2 | 1.42 | 100% | --- | --- |
| Sex (Female vs. Male) | --- | --- | 4.33 | 100% |
| Change in Living Status | --- | --- | 2.76 | 100% |
| Interpersonal Relationship with Friends | 0.72 | 100% | 0.70 | 100% |
| Current DBD | 1.39 | 100% | --- | --- |
| SES x Family History of SUD Interaction | 0.86 | 100% | --- | --- |
: Hazard ratios were standardized for continuous predictors. Abbreviations: DBD= Disruptive Behavior Disorder (including Conduct Disorder [CD] and/or Oppositional Defiant Disorder [ODD]); DRS= Depression Rating Scale of the Kiddie Schedule for Affective Disorders and Schizophrenia in School-Aged Children; HR= Hazard Ratios; LASSO = Least Absolute Shrinkage and Selection Operator; SES=Socioeconomic Status; SUD= Substance Use Disorders.
After bootstrapping the LASSO models, the above predictors (more severe depressive symptoms, low SES, family history of SUD, female sex) were retained in 85% or more of the bootstrap iterations, indicating stable predictor selection.
b). Predictors ascertained during follow-up preceding new onset abuse
Physical abuse.
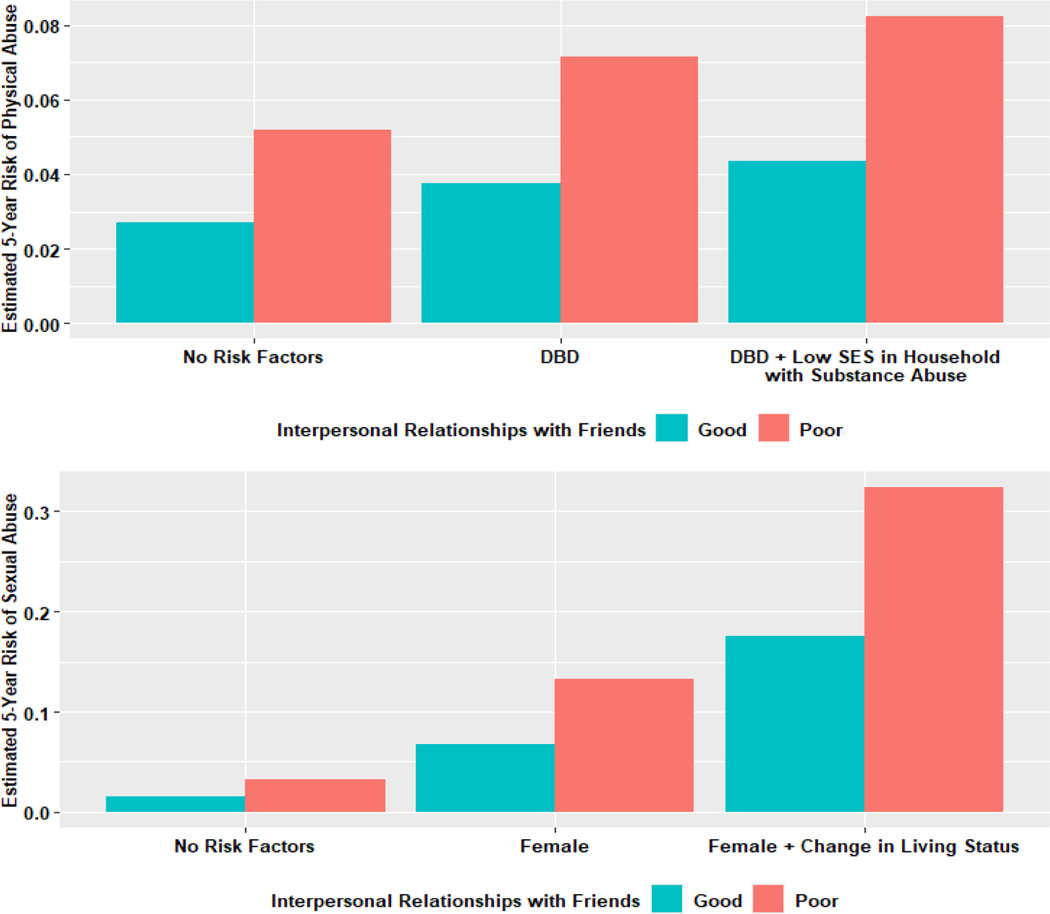
Older age (HR=1.42, 100% of iterations), comorbid Disruptive Behavior Disorder (DBD; including Conduct Disorder [CD] and/or Oppositional Defiant Disorder [ODD]) (HR=1.39, 100% of iterations), and the interaction between low SES and family history of SUD (HR=0.86, 100% of iterations) predicted new onset physical abuse. Good interpersonal relationships with friends was associated with significantly lower risk for physical abuse (HR=0.72, 100% of iterations) (Table 2).
Sexual abuse.
Models initially included a trichotomous predictor indicating whether participants lived with both, one, or no biological parents. After finding that LASSO selected living with both biological parents as a significant protective factor (HR=0.8), this was replaced with a more longitudinally-informative predictor including any changes in living status that occurred prior to the abuse. Changes in living status were associated with increased risk of sexual abuse during the next follow-up period (HR=2.76, 100% of iterations). Nearly all these instances of sexual abuse involved child living with biological mother along with a non-biologically related father (e.g., boyfriend, husband) who moved into the household. Female sex was associated with increased sexual abuse risk during the next follow-up period (HR=4.33, 100% of iterations). Good interpersonal relationships with friends were associated with decreased sexual abuse risk (HR=0.70, 100% of iterations) (Table 2).
After bootstrapping the LASSO models, the above predictors (older age, DBD, low SES and family history of SUD interaction, living status changes, female sex) were retained in 100% of the bootstrap iterations, indicating extremely stable predictor selection.
After observing that depression at intake, but not during follow-up, was predictive of physical abuse risk, a sensitivity analysis reimplemented the follow-up LASSO using only factors that were also available at intake to assess whether depression is a retained risk factor. Depression was retained by LASSO (26% of bootstrap iterations). Rerunning this model after reintroducing interpersonal relationships during follow-up as a predictor resulted in the retention of this variable instead of depression in 100% of bootstrap iterations. Thus, depression’s role as a predictor of future abuse risk may be explained by the absence of protective factors (i.e., interpersonal relationships).
Estimated 5-year-risk was evaluated to illustrate cumulative risk of physical/sexual abuse given presence/absence of LASSO-identified risk and protective factors (Figure 2).
Figure 2: Estimated additive 5-year risk of physical/sexual abuse.
Abbreviations: DBD=Disruptive Behavior Disorder (including Conduct Disorder [CD] and/or Oppositional Defiant Disorder [ODD]); SES=Socioeconomic Status. Note: For the risk estimates above, assessment age was held constant at the mean value=14.5
The above analyses were also completed with the included participants (n=279) plus the initially excluded participants who had physical/sexual abuse history prior to intake (n=75). Abuse history was a significant abuse predictor during follow-up (HR= 1.99, 100% of iterations; HR=1.66, 100% of iterations, respectively). Moreover, if past abuse was present, participant SUD increased physical abuse risk (HR=1.54, 31% of iterations) in the upcoming follow-up period. All other predictors noted in the above analyses (older age, DBD, low SES and family history of SUD interaction, living status changes, female sex, protective relationship with friends) were similar and remained significant.
4. Discussion
To our knowledge, this is the first study among youth with BD to prospectively examine lifetime (past/intake and follow-up) risk factors for new onset physical/sexual abuse, specifically those that temporally precede new onset abuse.
Fifteen per cent (42/279) of youth with BD reported new onset abuse during follow-up (62% physical, 26% sexual; 12% both). More severe depression at intake, low SES in families with history of SUD, older age and more DBD symptoms predating abuse were associated with increased risk for first physical abuse. About 79% of the participants who experienced new onset physical abuse had family history of SUD, and in 65% of those cases, at least one of the family members with SUD was a parent. Being female and not living with both biological parents (specifically living status changes) in the follow-up period preceding the abuse were associated with increased risk for first sexual abuse. Living with the biological mother and the presence of a non-biologically related father increased risk for sexual abuse three-fold. However, good interpersonal relationships with friends prospectively evaluated during follow-up was associated with decreased risk for both physical and sexual abuse.
COBY is the only study to also evaluate the abuse prevalence among youth with BD prospectively, reporting that 15% (62% physical, 26% sexual; 12% both) of participants with no prior abuse history experienced first abuse instance in their lives during the follow-up. Two epidemiological studies among children of general population that used prospective measures to evaluate abuse, reported prevalence of abuse among children of 7% and 20% respectively (Newbury et al., 2018; Shaffer et al., 2008). Importantly, our study adds to the literature by identifying abuse risk factors ascertained prospectively and temporally preceding new onset abuse. As such, our study may provide new perspectives on risk assessment and prevention that might enable identification of vulnerable youth with BD to potentially mitigate risk and decrease vulnerability to ongoing victimization.
While low SES and family history of SUD at intake and during follow-up were independent risk factors for new physical abuse onset, their interaction most potently predicted physical abuse. Other adult/youth BD studies also report that low SES and separately, family psychopathology, are associated with both types of abuse (Leverich et al., 2002; Romero et al., 2009). Community studies also find low SES and family instability (common among families with psychopathology), is associated with physical abuse risk (Sidebotham et al., 2006). These findings emphasize the need for identification and referral of parents of youth with BD for SUD treatment, as well as connection with case management and social services for low resourced families. We found older age during follow-up increased risk for first physical abuse, although other studies among youth with BD have not reported such association (Marchand et al., 2005). In community studies, younger age has been associated with maltreatment and may be partially explained by the increased vulnerability at younger ages (Zeanah and Humphreys, 2018). Other community studies indicate older age might be a risk factor for certain types of abuse (i.e., sexual) associated with increasing peer interactions during adolescence (Finkelhor et al., 2009). However, perpetrator information was not available in COBY.
We found that severe depression at intake is associated with increased risk for first physical abuse. Of note, childhood trauma has been associated with depression later in life, partly explained by the cognitive dimension of depression and resulting difficulties in emotion regulation (Huh et al., 2017). Retrospective studies have also reported an association between severe depression and physical abuse (Agnew-Blais and Danese, 2016; Daglas et al., 2014; Daruy-Filho et al., 2011), but others have found that only manic symptom severity was associated with abuse (Du rocher Schudlich, 2015). In line with this, a study among general population parents and risk for new onset abuse in their children, reported that parents with comorbid SUD and depression were found to be risk factors for new onset abuse among their children (Chaffin et al., 1996). Our findings were further explored, showing that such risk of depression was potentially related with some of the core symptoms of depression (e.g., isolation, low self-esteem…) that impact interpersonal relationships, and might place this youth in a vulnerable position, related with lack of protective factors (i.e., interpersonal relationships). In a longitudinal study among adults with BD, social support appeared to be associated with less depression at follow-up; findings were consistent with a mediational model suggesting that self-esteem may be one of the mechanisms whereby social support influences depression over time (Johnson et al., 2000). Retrospective studies have also reported an association between severe depression and risk for abuse (Agnew-Blais and Danese, 2016; Daglas et al., 2014; Daruy-Filho et al., 2011; Haussleiter et al., 2020; Saito et al., 2019). Of note, depression not only increases the risk for abuse, but abuse during childhood also increases the risk to develop depression later in life (Huh et al., 2017; Vares et al., 2015), which may be also partly explained by the cognitive dimension of depression and the resulting difficulties in emotion regulation resulting from trauma. Moreover, in a metanalytic review of the literature for child abuse, child’s social competence was moderately related to child’s physical abuse (Stith et al., 2009). Several studies have found a positive correlation between social isolation and abuse (Hazler and Denham, 2002), which can be embedded by specific aspects related with social support such as higher levels of belonging, availability of individuals who will engage in joint activities and provide physical and emotional support. Further, self-esteem might buffer an individual against downturns in self-evaluation. To our knowledge, this is the first study that uses a temporal sequence among youth with BD to analyze risk factors for abuse, so we are not able to compare this finding.
Comorbid DBD also predicted physical abuse during follow-up. Other studies show comorbidity in youth with BD is associated with physical abuse (Cazala et al., 2019; Du rocher Schudlich, 2015; Marchand et al., 2005). Youth/adults with other disorders manifested by behavior problems (e.g., Attention Deficit Hyperactivity Disorder) are also at elevated risk for physical abuse (Black et al., 2001a; Fuller-Thomson et al., 2014).
Additionally, when including participants with past abuse history (n=75), we observed that participants with past abuse history and SUD diagnosis were at greater risk for physical abuse in the upcoming follow-up period. Literature among BD youth and adults have also reported that SUD has been associated with abuse (Brown et al., 2005; Du rocher Schudlich, 2015; Maniglio, 2013). The significance of such association has a complex nature and the effects of early-abuse in the brain could partially explain this relationship; abuse survivors may tend to use substances as a coping strategy in order to alleviate painful internal states (Roesler and Dafler, 1993). Further, SUD has been associated with increased risk for maltreatment in adolescent community samples (Thornberry et al., 2014), perpetuating this daunting cycle and placing these youth at increased risk for revictimization. The relationship of how individuals with past abuse and comorbid SUD are at increased risk for recurrent physical abuse among BD youth should be further studied.
For sexual abuse, we found females had more than four times the risk for sexual abuse than males both at intake and follow-up. Other studies in BD youth/adults (Conus et al., 2010; Maniglio, 2013b; Marchand et al., 2005), as well as community studies, have similarly reported higher rates of sexual abuse among females than males (Black et al., 2001b). Not living with both biological parents over follow-up was also associated with subsequent risk of first sexual abuse. In fact, prospectively evaluated changes in living status, specifically, living with a biological mother and a stepfather/mother’s boyfriend moving into the house, nearly tripled the risk of subsequent new onset sexual abuse among females. In the BD literature, having single or divorced parent(s) has been associated with abuse, but has not previously been demonstrated as a temporally precedent risk factor (Conus et al., 2010; Marchand et al., 2005; Rucklidge, 2006). Prospective studies including community samples also found that living in single-parent families and having a biologically unrelated father posed increased risk for any type of abuse (Sidebotham et al., 2006; White et al., 2015). Similar to our findings, community studies have reported that female sex and not living with both biological parents, parents with low educational level and unemployment, or single parent households were associated with lifetime abuse (Schick et al., 2016).
Good relationships with friends during follow-up was associated with lower risk for physical/sexual abuse. This holds special importance since sequelae of abuse include psychosocial impairment, suicidality, and comorbid psychopathology (Carr et al., 2018). To the best of our knowledge, there are no other BD studies reporting protective factors for abuse, although in community studies, social support and having good friends is associated with decreased risk for both types of abuse (Finkelhor, 2007; Flemming et al., 1997; Sidebotham et al., 2006). In a longitudinal study among adults with BD, positive relationships with friends was inversely associated with severity of depression over time, and predicted a better illness course (Johnson et al., 2000). The above findings highlight the importance of fostering supportive relationships among youth with BD in order to not only mitigate risk of first onset physical and/or sexual abuse, but also potentially contribute to improvement in their mood episodes and, thus, decrease their ongoing risk for victimization.
4.1. Limitations
The results presented above need to consider the following limitations. First, participants were mostly White, and recruited from clinical settings, limiting the generalizability of the results. Nonetheless, similar clinical course and morbidity of youth with BD has been observed in non-clinical populations (Lewinsohn et al., 2000). Second, COBY did not recruit a control group, so conclusions cannot be drawn on abuse predictors among youth with BD relative to controls. Third, although prospective data on abuse and follow-up variables were gathered longitudinally, these data were assessed retrospectively at each follow-up period encompassing an average of 7-months. While all reports of abuse are retrospective, we limited the time interval between assessments to minimize retrospective recall. Fourth, severity/frequency of abuse, perpetrator information, parents’ abuse history, other forms of abuse (e.g., emotional abuse, neglect), or interventions/services for abuse were not systematically assessed. Finally, abuse was not further corroborated with other sources of information (e.g., CPS) due to confidentiality.
4.2. Conclusions
To summarize, this is the first study to prospectively evaluate risk factors both at intake and over follow-up temporally preceding new onset physical and/or sexual abuse among youth with BD. Our study broadens prior research scope on this population by establishing temporal precedence of risk factors for new onset abuse through longitudinal analyses, instead of using cross-sectional associations. These results have several clinical implications, including the importance of providers identifying high risk individuals and circumstances (i.e., those with above noted predictors of female sex, severe depression, DBD, not living with both biological parents, low SES in families with SUD) that may inform strategies to diminish abuse risk.
References:
- Agnew-Blais J, Danese A, 2016. Childhood maltreatment and unfavourable clinical outcomes in bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry 3, 342–349. [DOI] [PubMed] [Google Scholar]
- Andreu Pascual M, Levenson JC, Merranko J, Gill MK, Hower H, Yen S, Strober M, Goldstein TR, Goldstein BI, Ryan ND, Weinstock LM, Keller MB, Axelson D, Birmaher B, 2020. The Effect of Traumatic Events on the Longitudinal Course and Outcomes of Youth with Bipolar Disorder. Journal of affective disorders 274, 126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association AP, 2004. The Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV). American Psychiatric Association, Arlington, VA. [Google Scholar]
- Axelson D, Birmaher B, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Bridge J, Keller M, 2006. Phenomenology of children and adolescents with bipolar spectrum disorders. Archives of general psychiatry 63, 1139–1148. [DOI] [PubMed] [Google Scholar]
- Axelson D, Birmaher BJ, Brent D, Wassick S, Hoover C, Bridge J, Ryan N, 2003. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. J Child Adolesc Psychopharmacol 13, 463–470. [DOI] [PubMed] [Google Scholar]
- Benarous X, Raffin M, Bodeau N, Dhossche D, Cohen D, Consoli A, 2017. Adverse Childhood Experiences Among Inpatient Youths with Severe and Early-Onset Psychiatric Disorders: Prevalence and Clinical Correlates. Child Psychiatry Hum Dev 48, 248–259. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Gill MK, Axelson DA, Goldstein BI, Goldstein TR, Yu H, Liao F, Iyengar S, Diler RS, Strober M, Hower H, Yen S, Hunt J, Merranko JA, Ryan ND, Keller MB, 2014. Longitudinal trajectories and associated baseline predictors in youths with bipolar spectrum disorders. The American journal of psychiatry 171, 990–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black D, Heyman R, Smith Slep AM, 2001a. Risk factors for child physical abuse. Aggression and Violent Behavior 6, 121–188. [Google Scholar]
- Black DA, Heyman RE, Smith Slep AM, 2001b. Risk factors for child sexual abuse. Aggression and Violent Behavior 6 203–229. [Google Scholar]
- Brown GR, McBride L, Bauer MS, Williford WO, Cooperative Studies Program 430 Study, T., 2005. Impact of childhood abuse on the course of bipolar disorder: a replication study in U.S. veterans. Journal of affective disorders 89, 57–67. [DOI] [PubMed] [Google Scholar]
- Carr A, Duff H, Craddock F, 2018a. A Systematic Review of Reviews of the Outcome of Noninstitutional Child Maltreatment. Trauma Violence Abuse, 1524838018801334. [DOI] [PubMed] [Google Scholar]
- Carr A, Duff H, Craddock F, 2018b. A Systematic Review of the Outcome of Child Abuse in Long-Term Care. Trauma Violence Abuse, 1524838018789154. [DOI] [PubMed] [Google Scholar]
- Cazala F, Bauer IE, Meyer TD, Spiker DE, Kazimi IF, Zeni CP, Zunta-Soares GB, Soares JC, 2019. Correlates of childhood trauma in children and adolescents with bipolar disorder spectrum: A preliminary study. Journal of affective disorders 247, 114–119. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Kelleher K, Hollenberg J, 1996. Onset of physical abuse and neglect: psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse Negl 20, 191–203. [DOI] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M, 1985. The assessment of affective disorders in children and adolescents by semistructured interview. Test-retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version. Archives of general psychiatry 42, 696–702. [DOI] [PubMed] [Google Scholar]
- Conus P, Cotton S, Schimmelmann BG, Berk M, Daglas R, McGorry PD, Lambert M, 2010. Pretreatment and outcome correlates of past sexual and physical trauma in 118 bipolar I disorder patients with a first episode of psychotic mania. Bipolar Disord 12, 244–252. [DOI] [PubMed] [Google Scholar]
- Daglas R, Conus P, Cotton SM, Macneil CA, Hasty MK, Kader L, Berk M, Hallam KT, 2014. The impact of past direct-personal traumatic events on 12-month outcome in first episode psychotic mania: trauma and early psychotic mania. Aust N Z J Psychiatry 48, 1017–1024. [DOI] [PubMed] [Google Scholar]
- Daruy-Filho L, Brietzke E, Lafer B, Grassi-Oliveira R, 2011. Childhood maltreatment and clinical outcomes of bipolar disorder. Acta psychiatrica Scandinavica 124, 427–434. [DOI] [PubMed] [Google Scholar]
- Du rocher Schudlich T, 2015. Physical and Sexual abuse in Early-onset bipolar disorder in youths receiving outpatient services: Frequent, but not specific. Journal of Abnormal child psychology 43, 453–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS, 2019. REPRINT OF: Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 56, 774–786. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, 2007. Prevention of sexual abuse through educational programs directed toward children. Pediatrics 120, 640–645. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner H, Ormrod R, Hamby SL, 2009. Violence, abuse, and crime exposure in a national sample of children and youth. Pediatrics 124, 1411–1423. [DOI] [PubMed] [Google Scholar]
- First MBS, R L; Gibbon M; Williams JBW, 1996. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). American Psychiatry Publishing, Inc. [Google Scholar]
- Flemming J, Mullen P, Bammer G, 1997. A STUDY OF POTENTIAL RISK FACTORS FOR SEXUAL ABUSE IN CHILDHOOD. Child Abuse & Neglect 21, 49–58. [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson E, Mehta R, Valeo A, 2014. Establishing a Link Between Attention Deficit Disorder/Attention Deficit Hyperactivity Disorder and Childhood Physical Abuse. Journal of Aggression, Maltreatment & Trauma 23, 188–198. [Google Scholar]
- Hastie T, Tibshirani R, Friedman J, 2009. The elements of statistical learning: prediction, inference and data mining. Springer-Verlag, New York. [Google Scholar]
- Hastie T, Tibshirani R, Wainwright M, 2015. Statistical Learning with Sparsity. Chapman and Hall/CRC, New York. [Google Scholar]
- Haussleiter IS, Neumann E, Lorek S, Ueberberg B, Juckel G, 2020. Role of child maltreatment and gender for bipolar symptoms in young adults. Int J Bipolar Disord 8, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB, 1975. Four Factor Index of Social Status. New Haven, CT: Yale University. [Google Scholar]
- Huh HJ, Kim KH, Lee HK, Chae JH, 2017. The relationship between childhood trauma and the severity of adulthood depression and anxiety symptoms in a clinical sample: The mediating role of cognitive emotion regulation strategies. Journal of affective disorders 213, 44–50. [DOI] [PubMed] [Google Scholar]
- Johnson JH, McCuthcheon SM, 1980. Assessing life stress in older children and adolescents: Preliminary findings with the Life Events Checklists., Washington, DC. [Google Scholar]
- Johnson SL, Meyer B, Winett C, Small J, 2000. Social support and self-esteem predict changes in bipolar depression but not mania. Journal of affective disorders 58, 79–86. [DOI] [PubMed] [Google Scholar]
- Jones SH, Thornicroft G, Coffey M, Dunn G, 1995. A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF). Br J Psychiatry 166, 654–659. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N, 1997. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC, 1987. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of general psychiatry 44, 540–548. [DOI] [PubMed] [Google Scholar]
- Leverich GS, McElroy SL, Suppes T, Keck PE Jr., Denicoff KD, Nolen WA, Altshuler LL, Rush AJ, Kupka R, Frye MA, Autio KA, Post RM, 2002. Early physical and sexual abuse associated with an adverse course of bipolar illness. Biological psychiatry 51, 288–297. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Klein DN, Seeley JR, 2000. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disord 2, 281–293. [DOI] [PubMed] [Google Scholar]
- Maniglio R, 2013a. The impact of child sexual abuse on the course of bipolar disorder: a systematic review. Bipolar Disord 15, 341–358. [DOI] [PubMed] [Google Scholar]
- Maniglio R, 2013b. Prevalence of child sexual abuse among adults and youths with bipolar disorder: a systematic review. Clinical psychology review 33, 561–573. [DOI] [PubMed] [Google Scholar]
- Marchand WR, Wirth L, Simon C, 2005. Adverse life events and pediatric bipolar disorder in a community mental health setting. Community Ment Health J 41, 67–75. [DOI] [PubMed] [Google Scholar]
- Nelson J, Klumparendt A, Doebler P, Ehring T, 2017. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry 210, 96–104. [DOI] [PubMed] [Google Scholar]
- Neria Y, Bromet EJ, Carlson GA, Naz B, 2005. Assaultive trauma and illness course in psychotic bipolar disorder: findings from the Suffolk county mental health project. Acta psychiatrica Scandinavica 111, 380–383. [DOI] [PubMed] [Google Scholar]
- Newbury JB, Arseneault L, Moffitt TE, Caspi A, Danese A, Baldwin JR, Fisher HL, 2018. Measuring childhood maltreatment to predict early-adult psychopathology: Comparison of prospective informant-reports and retrospective self-reports. J Psychiatr Res 96, 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen DH, Portner J, Lavee Y, 1985. Family Adaptability and Cohesion Evaluation Scales (FACES-II). University of Minessota Press, Minneapolis, MN. [Google Scholar]
- Palmier-Claus JE, Berry K, Bucci S, Mansell W, Varese F, 2016. Relationship between childhood adversity and bipolar affective disorder: systematic review and meta-analysis. Br J Psychiatry 209, 454–459. [DOI] [PubMed] [Google Scholar]
- Robin AL, Foster SL, 1989. Negotiating Parent-Adolescent Conflict: A behavioral- Family Systems Approach. Guilford Press, New York, NY. [Google Scholar]
- Roesler TA, Dafler CE, 1993. Chemical dissociation in adults sexually victimized as children: alcohol and drug use in adult survivors. J Subst Abuse Treat 10, 537–543. [DOI] [PubMed] [Google Scholar]
- Romero S, Birmaher B, Axelson D, Goldstein T, Goldstein BI, Gill MK, Iosif AM, Strober MA, Hunt J, Esposito-Smythers C, Ryan ND, Leonard H, Keller M, 2009. Prevalence and correlates of physical and sexual abuse in children and adolescents with bipolar disorder. Journal of affective disorders 112, 144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rucklidge JJ, 2006. Psychosocial functioning of adolescents with and without paediatric bipolar disorder. Journal of affective disorders 91, 181–188. [DOI] [PubMed] [Google Scholar]
- Saito T, Toda H, Inoue T, Koga M, Tanichi M, Takeshita S, Nakagawa R, Nagamine M, Masuya J, Tanabe H, Shimizu K, Kusumi I, Yoshino A, 2019. Relationship between the subtypes of child abuse and affective temperaments: Comparison of depression and bipolar disorder patients and healthy controls using the reclassified Child Abuse and Trauma Scale. Journal of affective disorders 257, 396–403. [DOI] [PubMed] [Google Scholar]
- Schick M, Schonbucher V, Landolt MA, Schnyder U, Xu W, Maier T, Mohler-Kuo M, 2016. Child Maltreatment and Migration: A Population-Based Study Among Immigrant and Native Adolescents in Switzerland. Child Maltreat 21, 3–15. [DOI] [PubMed] [Google Scholar]
- Schomaker M, Heumann C, 2018. Bootstrap Inference when Using Multiple Imputation.. Statistics in Medicine 37, 2252–2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer A, Huston L, Egeland B, 2008. Identification of child maltreatment using prospective and self-report methodologies: a comparison of maltreatment incidence and relation to later psychopathology. Child Abuse Negl 32, 682–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S, 1983. A children’s global assessment scale (CGAS). Archives of general psychiatry 40, 1228–1231. [DOI] [PubMed] [Google Scholar]
- Sidebotham P, Heron J, Team AS, 2006. Child maltreatment in the “children of the nineties”: a cohort study of risk factors. Child Abuse Negl 30, 497–522. [DOI] [PubMed] [Google Scholar]
- Stith SM, Christopher Davies TLL,, Boykin EL, Alder MC, Harris JM, Som A, McPherson M, Dees JEMEG, 2009. Risk factors in child maltreatment: A meta-analytic review of the literature. Aggression and Violent Behavior 14, 13–29. [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg M, Alink L, IJzendoorn M, 2015. The Prevalence of Child Maltreatment across the Globe: Review of a Series of Meta-Analyses. Child Abuse Review 24, 37–50. [Google Scholar]
- Thornberry TP, Matsuda M, Greenman SJ, Augustyn MB, Henry KL, Smith CA, Ireland TO, 2014. Adolescent risk factors for child maltreatment. Child Abuse Negl 38, 706–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S G-OK, 2011. mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software 45, 1–67. [Google Scholar]
- Vares EA, Salum GA, Spanemberg L, Caldieraro MA, Souza LH, Borges Rde P, Fleck MP, 2015. Childhood trauma and dimensions of depression: a specific association with the cognitive domain. Braz J Psychiatry 38, 127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M, 2000. Brief screening for family psychiatric history: the family history screen. Archives of general psychiatry 57, 675–682. [DOI] [PubMed] [Google Scholar]
- White OG, Hindley N, Jones DP, 2015. Risk factors for child maltreatment recurrence: An updated systematic review. Med Sci Law 55, 259–277. [DOI] [PubMed] [Google Scholar]
- Zeanah CH, Humphreys KL, 2018. Child Abuse and Neglect. Journal of the American Academy of Child and Adolescent Psychiatry 57, 637–644. [DOI] [PMC free article] [PubMed] [Google Scholar]