Abstract
Background:
Foreign-born Latino children in the United States (US) have poor asthma outcomes, but the role of routine care utilization in these outcomes is unclear. Our objective was to compare select ambulatory care utilization measures for asthma between foreign-born Latino, US-born Latino, and non-Hispanic white children.
Methods:
Using a multistate network of clinics with a linked electronic health record, we compared the International Classification of Disease (ICD)-coded asthma diagnosis among those with respiratory symptoms, electronic health records documentation of diagnosis, prescriptions, and influenza vaccination of foreign-born and US-born Latino children, and non-Hispanic white children over a 10+ year study period. We also examined outcomes by country of birth in children from Mexico, Cuba, and Guatemala.
Results:
Among our study population (n = 155,902), 134,570 were non-Hispanic white, 19,143 were US-born Latino, and 2189 were foreign-born Latino. Among those with suspicious respiratory symptoms, there was no difference between these groups in the predicted probability of an ICD-coded asthma diagnosis. US-born Latino children with asthma were less likely to have asthma documented on their problem list, more likely to have an albuterol prescription, and less likely to have an inhaled steroid prescribed. All Latino children had higher rates of influenza vaccination than non-Hispanic white children.
Conclusions:
In a national network, there were few disparities between Latino (US- and foreign-born) children and non-Hispanic white comparators in many common asthma care services, except some measures in US-born Latino children. Providers should understand that their US-born Latino children may be at elevated risk for not receiving adequate asthma care.
Keywords: asthma, children, foreign-born, latino
The influence of birth country on asthma in Latino children in the United States (US) has been the subject of numerous studies but with limited resultant guidance for the direct provision of asthma care. Generally, in survey-based research, foreign-born Latino children have a varied prevalence of asthma compared to US-born non-Hispanic white children, often depending on specific country of origin.1-4 When diagnosed, the course of asthma appears worse than non-Hispanic whites—more exacerbations, worse control, and worse disease outcomes overall.5 This literature is limited by cross-sectional designs, which fail to capture clinical presentations over time, and is subject to recall bias, preventing full understanding of these worse outcomes or how clinicians may mitigate them.
Asthma is a chronic illness with predisposing factors, circumstances of initial presentation and diagnosis, and subsequent care. There is a paucity of research on asthma course and routine care in foreign-born Latinos along multiple points of this continuum. For instance, studies have found differences in asthma prevalence by self-report between nativity groups,1,2,6 but assessing differences in International Classification of Disease (ICD)-coded asthma diagnosis among those with possible clinical symptoms of asthma over time by nativity has not been documented. Few studies have examined appropriate electronic health records (EHR) documentation of asthma and its severity as a key outcome, despite numerous guidelines on this fundamental facet of asthma management.7-9 Appropriate medication prescription for asthma is also fundamental to quality care,7,8 and studies have shown ethnic differences in inhaled steroid prescribing,10,11 or in medication adherence,5 but none have evaluated the prescription of multiple medication classes by nativity. Finally, yearly influenza vaccination is a basic health care measure for children,12 yet some cross-sectional studies have shown lower influenza vaccine rates in Latino children compared with whites,13 while others have shown higher.14 To our knowledge no work has looked at these relationships by nativity utilizing multiple years of electronic health record data. For clinicians aiming to improve care, studies directly examining this health care provided to Latino (US- and foreign-born) patients are needed to guide the care of children with asthma.
To fill this gap, we conducted an observational study of the asthma care of Latino children with a documented country of birth in a large, multistate network of community health centers (CHCs) in the United States, in order to better understand the asthma care measures utilized by this population. CHCs care for thousands of vulnerable Latino children,15 and a proper examination of the care provided to this group is needed to understand the care provided in this setting. We compared non-Hispanic white children to US-born and foreign-born Latino children for asthma diagnosis and care outcomes, and we compare specific nations of origin when the population was an appropriate size for comparison. Because of some existing evidence from small sample studies that foreign-born Latino children have a generally worse asthma course,5 and that these children could have numerous, significant barriers to obtaining health care (immigration-related barriers, possible insurance, and language barriers which may limit provider-patient interactions), our overall hypothesis is that foreign-born Latino children would have received less asthma-related care compared to US-born Latino children.
Methods
Data Sources
We used EHRs from the Accelerating Data Value Across a National Community Health Center Network (ADVANCE network). These data were representative of 635 clinics in 11 states across the United States: California, Indiana, Massachusetts, Minnesota, North Carolina, New Mexico, Ohio, Oregon, Texas, Washington, and Wisconsin.
Population
Our study population consisted of children (age 3–17) seen for an ambulatory visit at least once between January 1, 2012 and January 31, 2017, within an ADVANCE clinic. Once included in the study population, we had access to EHR data as far back as 2005. Among all Latino patients in the ADVANCE network, the subpopulation of Latinos whose health record contained available birth-country data (collected by clinic staff in the course of routine clinical care) was included in this study. Additionally, we included all non-Hispanic white children, regardless of having country-of-origin information (in our network, a low proportion of white children are foreign-born).
Exclusion Criteria
Children with cystic fibrosis were excluded from our study because of possible confounding medications (n = 39). For the subset of children with asthma, 1 Latino born in Brazil and 1 from Nicaragua were also excluded due to the low country-of-origin sample size.
Dependent Variables
We examined 4 outcomes, over the entire study period, to capture the broad spectrum of asthma care in these patients. First, we examined the prevalence of EHR diagnosis (at any point in the study period) based on ICD9/10 codes in all children and the prevalence of ICD-coded asthma diagnosis among those with suspicious respiratory symptoms. These symptoms included diagnosis of wheeze, recurrent cough (≥4 visits), bronchitis, or a prescription for albuterol.16 Our intention was not to establish the diagnosis of asthma against a gold standard, but to compare the prevalence of diagnosis in similar, EHR-verified clinical scenarios across our population, which is a significant advancement over previous diagnosis literature which has relied on self-report. Second, we analyzed appropriate EHR documentation of asthma and its severity, specifically, 1) whether children who have ever had an ICD9/10 code for asthma ever had their asthma diagnosis recorded on the EHR problem list (Table 1 for citations and rationale) and 2) whether children who ever had an ICD9/10 code for asthma ever had their asthma severity recorded on the problem list. Third, we compared the prevalence and rates of common asthma medication prescription among those with ICD-coded asthma; corticosteroid medications were evaluated among children with persistent asthma, as well as all children with asthma. Fourth, we examined yearly influenza vaccination rates across the entire study sample and among those with ICD-coded asthma. Specific dependent variables and their rationale, nature, and denominator are in Table 1.
Table 1.
Dependent Variables, Denominator, and Rationale
| Variable/Asthma Care Measure |
Variable Type | Denominator | Note |
|---|---|---|---|
| ICD-coded asthma diagnosis among those with suspicious respiratory symptoms | |||
| Prevalence of asthma diagnosis ever | Binary (yes/no) | Entire study sample | Based on ICD9 and ICD10 codes in an encounter or on the problem list |
| Diagnosis of asthma in the presence of symptoms suggestive of asthma | Binary (yes/no) | Those who presented with at least one symptom consistent with asthma, including wheeze, 4 or more visits for cough, bronchitis,30 and documented albuterol prescription | We chose to include albuterol prescription given the common practice of prescribing albuterol for symptom treatment even prior to an official diagnosis of asthma28 |
| Appropriate EHR documentation of asthma and its severity | |||
| Asthma on problem list | Binary (yes/no) | Children with an asthma diagnosis in the study period | Placement of chronic conditions on a “problem list” is a standard of care for chronic conditions and for the use of electronic health records9,31-33 |
| Asthma severity on problem list | Binary (yes/no) | Children with an asthma diagnosis in the study period | Documented asthma severity guides medication choices7,8 |
| Medication prescription | |||
| Albuterol prescription | Binary (yes/no), annual rate | Children with an asthma diagnosis in the study period | Albuterol is a first line prescription choice for most children with asthma7,8 |
| Inhaled corticosteroid prescription | Binary (yes/no) | Children with an asthma diagnosis in the study period and separately, children with a “persistent” (mild, moderate, or severe) asthma diagnosis in the study period | Inhaled corticosteroids are indicated in children with “persistent” asthma diagnoses7,8 |
| Oral corticosteroid prescription | Binary (yes/no) | Children with an asthma diagnosis in the study period and separately, children with a “persistent” (mild, moderate, or severe) asthma diagnosis in the study period | Oral corticosteroids are indicated for asthma exacerbations, and are prescribed during and prior to exacerbations7,8 |
| Yearly influenza vaccination rates | |||
| Influenza vaccination | Immunized in at least 50% of study years yes/no. Immunized in at least 80% of study years (yes/no) | Entire study sample | Given the indications for influenza vaccine in all children, we analyzed differences in our entire population12 |
EHR indicates electronic health record; ICD, International Classification of Disease.
Independent Variables
Our primary independent variable was a 3-category grouping of the combination of ethnicity and nativity: non-Hispanic white children, Latino children born in the United States, and Latino children born outside the United States, as indicated by place of birth denoted in the EHR. While we use Latino in the majority of our discussion because it is often preferred in our study population, the actual ethnicity information collected by clinics is Hispanic and non-Hispanic. For some analyses, we further divided Latino foreign-born children by specific country of origin. Available countries of origin included Mexico, Cuba, and Guatemala.
Covariates
To describe our study population and control for potential differences between study groups, we considered the following EHR-derived variables in our analyses: patient age at first study visit, sex, body mass index, income as percent of the US federal poverty level, health insurance status throughout the study period (never insured, some public insurance, some private insurance), and number of face-to-face clinic visits per year. We did not include preferred language because it is heavily co-linear with nativity in our sample.
Inverse Probability of Treatment Weighting
We adjusted for differences in confounders between the 3 ethnicity-nativity groups through the use of inverse-probability of treatment weighting (IPTW) using propensity scores. The application of IPTW was accomplished using the R package twang (toolkit for weighting and analysis of nonequivalent groups), version 1.5. Given that certain outcomes have different eligible populations (all children, children with ICD-coded asthma and children with persistent asthma), we utilized the aforementioned covariates in generalized boosted models to estimate average treatment effect propensity weights for the following subpopulations:
all study children for the asthma prevalence outcomes, by primary ethnicity-nativity group
all children with asthma for care-quality outcomes, by primary ethnicity-nativity group and country of origin
all children with persistent asthma for certain care-quality outcomes, by primary ethnicity-nativity group and country of origin
Absolute standardized mean differences (ASMD) calculated both before and after weighting were then used to assess weighting performance, comparing non-Hispanic whites, US-born Latinos, and foreign-born Latinos (or country of origin) for balance across confounders. An ASMD of less than 0.20 was indicative of good balance in covariates across groups.17 We also estimated the effective sample size, which is the approximate number of observations under simple random sampling that would produce variation equivalent to that of the IPTW sample.
Statistical Analysis
We described patient characteristics for both the weighted and unweighted samples including effective sample size and standardized mean differences. The binary indicator for ICD-coded asthma diagnosis was evaluated using IPTW logistic regression and a robust sandwich variance estimator with compound symmetry correlation structure to account for clustering of patients within their primary clinic, especially because asthma diagnosis may vary greatly by clinic.18 Additionally, in analyses that studied those with suspicious respiratory symptoms, we included a binary indicator for the presence of any suspicious respiratory symptom (patient ever having a diagnosis of wheeze, bronchitis, cough [4 or more instances], or documentation of an albuterol prescription) along with an interaction term with ethnicity-nativity groups. We reported predicted probabilities and contrasts together with their corresponding 95% confidence intervals (CIs) comparing non-Hispanic whites to US-born and foreign-born Latino groups. A similar approach was used for all asthma care-quality outcomes where a binary dependent variable was used. Specifically, for both the problem list outcomes (asthma ever on problem list and asthma severity ever on problem list) and prescription outcomes (documented albuterol ever, corticosteroid inhaler ever, oral steroid [OS] prescription ever) we compared by primary ethnicity-nativity group and by country of origin.
We also estimated yearly prescription rates for albuterol, inhaled corticosteroid (ICS), and OS medications among all children with ICD-coded asthma and among children with persistent asthma (for the ICS and OS steroid medications only). These estimates were derived using IPTW negative binomial regression and robust sandwich variance estimation for clustering of patients within clinics. For the analysis for children with persistent asthma, we considered a similar interaction approach with the binary indicator for the presence of any suspicious respiratory symptom as above. Rate ratios, and 95% CIs comparing groups were reported for these care-quality analyses accordingly.
Lastly, using the aforementioned approach, we estimated adjusted rates of influenza immunization for the entire study population. Overall, when a covariate in the IPTW model was found to be imbalanced between groups (ASMD ≥ 0.20), we included those confounders in our regression models. Statistical models were performed in Stata 15. All statistical testing was two-sided with a type I error set to 5%. The study was formally approved by the Oregon Health & Science University Institutional Review Board.
Results
There were 155,902 children who met inclusion criteria with an average of 3.5 years of study observation. A subset of 11,493 (7.4%) had at least one record of an ICD-coded asthma diagnosis; 2147 of these had ICD-coded persistent asthma. Patient characteristics both before and after weighting are shown in Table 2 (all children) and Appendix Table 1 (children with asthma), by ethnicity-nativity group. We observed differences between our ethnicity-nativity groups: foreign-born Latinos were more likely to be always overweight, always below 138% of the federal poverty level, and never insured.
Table 2.
Characteristics of Children in the Study Comparing US- and Foreign-Born Latinos to Non-Hispanic Whites Seen Within the ADVANCE Clinical Research Network of Community Health Centers Across 11 US States Before and After Weighting
| Characteristic | Unweighted Groups, % | Max ASMD* | Weighted Groups, % | Max ASMD | ||||
|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White | US-Born Latino | Foreign-Born Latino | Non-Hispanic White | US-Born Latino | Foreign-Born Latino | |||
| Total N/ESS | 134,570 | 19,143 | 2189 | 156,503.3 | 151,441.7 | 141,493.4 | ||
| Female | 49.5 | 50.2 | 48.8 | 0.018 | 49.6 | 50.2 | 49.8 | 0.008 |
| Age at first encounter | 0.461 | 0.049 | ||||||
| 0–3 | 30.3 | 26.1 | 9.5 | 29.5 | 29.8 | 27.0 | ||
| 3–6 | 16.4 | 16.9 | 13.9 | 16.5 | 16.6 | 18.3 | ||
| 6–11 | 24.7 | 28.3 | 24.1 | 25.2 | 24.8 | 25.2 | ||
| 11–14 | 15.2 | 15.7 | 20.1 | 15.3 | 15.4 | 15.5 | ||
| 14–17 | 13.3 | 13.0 | 32.4 | 13.5 | 13.4 | 14.0 | ||
| Body mass index† | 0.243 | 0.024 | ||||||
| Never overweight | 67.0 | 50.3 | 50.0 | 64.7 | 64.4 | 63.2 | ||
| Sometimes overweight | 12.8 | 22.0 | 21.1 | 14.1 | 14.1 | 14.2 | ||
| Always overweight | 20.2 | 27.7 | 28.9 | 21.2 | 21.5 | 22.7 | ||
| Federal poverty level | 0.610 | 0.053 | ||||||
| Above and below 138 | 9.6 | 2.9 | 5.5 | 8.7 | 8.8 | 7.3 | ||
| Always over 138 | 12.8 | 2.6 | 2.4 | 11.4 | 10.5 | 10.4 | ||
| Always under 138 | 48.9 | 52.7 | 77.6 | 49.8 | 51.0 | 52.4 | ||
| Never documented | 28.8 | 41.8 | 14.5 | 30.1 | 29.7 | 29.8 | ||
| Insurance | 0.592 | 0.077 | ||||||
| Never insured | 9.7 | 1.5 | 11.3 | 8.7 | 8.3 | 9.3 | ||
| Some private | 20.7 | 2.4 | 17.0 | 18.5 | 16.9 | 15.3 | ||
| Some private and public | 7.5 | 3.4 | 10.6 | 7.0 | 7.0 | 5.6 | ||
| Some public | 62.1 | 92.7 | 61.1 | 65.8 | 67.8 | 69.8 | ||
| Yearly visits | 0.396 | 0.049 | ||||||
| 0–1 | 38.0 | 14.7 | 18.0 | 34.9 | 34.1 | 37.2 | ||
| 1–3 | 43.1 | 50.6 | 52.0 | 44.2 | 44.7 | 42.8 | ||
| 3–5 | 11.6 | 19.7 | 17.3 | 12.7 | 13.2 | 12.3 | ||
| 5–10 | 5.7 | 10.8 | 8.6 | 6.3 | 6.2 | 6.2 | ||
| >10 | 1.6 | 4.3 | 4.1 | 2.0 | 1.9 | 1.5 | ||
ESS indicates effective sample size. Weights were obtained using inverse-probability of treatment weighting (IPTW) using propensity scores. The application of IPTW was accomplished using the R package twang (toolkit for weighting and analysis of nonequivalent groups), v. 1.5.
Maximum absolute standardized mean difference (ASMD) across all pairwise comparisons for each level of pretreatment covariate.
Body mass index (BMI) calculated using the “childsds” package in R based on age, sex, weight, and height. Overweight if BMI over the 85th percentile, obese if over the 95th percentile. Biologically implausible values were flagged as over 8 standard deviations over or 4 under the mean BMI.
Appendix Table 2 describes the unweighted sample of foreign-born Latinos by country of origin, the majority born in either Guatemala (n = 1050) or Mexico (n = 977), with a smaller sample from Cuba (n = 162). Children born in Guatemala were more frequently never overweight, had a higher proportion of private insurance, and to always be under 138% of the federal poverty level compared to non-Hispanic whites. Mexican children were more likely to not have income information documented and to never be insured.
ICD-Coded Asthma Diagnosis Among Those With Suspicious Respiratory Symptoms
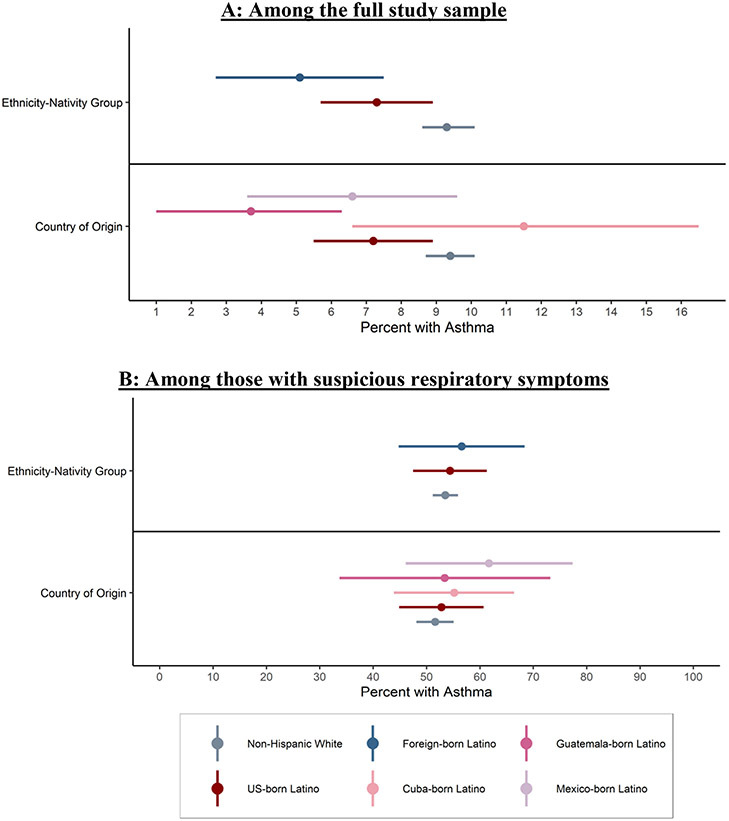
Overall, 13.2% of study participants presented with any suspicious respiratory symptoms (Appendix Table 3). Based on IPTW logistic regression modeling, both US- and foreign-born Latinos were slightly less likely than non-Hispanic whites to have an ICD-coded asthma diagnosis (Figure). Among the full study population, non-Hispanic whites saw a predicted probability (predicted prevalence of ICD-coded asthma diagnosis) of 9.3% (95% CI, 8.6%–10.1%); US-born Latinos (7.3%, 95% CI, 5.7%–8.9%) and foreign-born Latinos (5.1%, 95% CI, 2.7%–7.5%) saw lower prevalence. Among those with any suspicious respiratory symptoms, there was no difference (non-Hispanic whites: 53.5%, 95% CI, 51.2%–55.9%; US-born Latino: 54.4%, 95% CI, 47.5% −61.3%; foreign-born Latino: 56.6%, 95% CI, 44.8% −68.4%).
Figure.
Percent of ICD-coded asthma diagnosis in children, among the full study sample (panel A) and among those with suspicious respiratory symptoms (panel B). Comparisons of non-Hispanic white, US-born and foreign-born Latinos, collectively (above solid black line) and by birth country (below solid black line). (A) Among the full study sample. (B) Among those with suspicious respiratory symptoms. ICD indicates International Classification of Disease. We reported predicted probabilities (dots) and their corresponding 95% confidence intervals (lines). The binary indicator for ICD-coded asthma was evaluated using inverse probability of treatment weighted logistic regression and a robust sandwich variance estimator with compound symmetry correlation structure to account for clustering of patients within their primary clinic. For the country of origin analysis, additional adjustment was made for federal poverty level and insurance as these remained imbalanced between groups after weighting.
In IPTW adjusted analyses by country of origin (Figure), compared to non-Hispanic whites, Cuban-born children had slightly higher but nonsignificant overall predicted probabilities of ICD-coded asthma (11.5%, 95% CI, 6.6%–16.5%) as compared to non-Hispanic whites; there was no difference when any suspicious respiratory symptoms were present (55.2%, 95% CI, 43.9%–66.4%). Mexican-born children had a lower predicted probability of asthma overall (6.6%, 95% CI, 3.6%–9.6%), but a slightly higher but nonsignificant predictive probability when any suspicious respiratory symptoms were present (61.7%, 95% CI, 46.1%–77.4%). Lastly, Guatemalan-born children had a lower predicted probability of ICD-coded asthma diagnosis overall (3.7%, 95% CI, 1.0%–6.3%) but not when any suspicious respiratory symptoms were documented (53.4%, 95% CI, 33.7% −73.2%). Counts of children with specific birthplace and each specific symptom were low, limiting interpretability of these findings. However, these numbers are reported in Appendix Table 3.
EHR Problem List Documentation of Asthma, Its Severity and Medication Prescription
We examined problem list documentation and medication prescriptions of US- and foreign-born Latinos as compared to non-Hispanic whites (Table 3). In IPTW analyses, US-born Latino children with asthma were less likely to have asthma documented on their problem list ever, more likely to have ever had an albuterol prescription, have higher annual rates of albuterol prescriptions, and be less likely to have an ICS prescribed, although not when being diagnosed with persistent asthma. Foreign-born Latino children, when diagnosed with persistent asthma, had higher predicted probabilities of inhaled steroids ever being prescribed and lower predicted probabilities of OS ever being prescribed, but both of these were not statistically significant.
Table 3.
Asthma Care-Quality Measures in Children With ICD-Coded Asthma, Comparing US-Born and Foreign-Born Latinos to Non-Hispanic Whites
| Care-Quality Measure | Predicted Probability of Asthma Care Quality Measures, Denoted as %, or Rate of Documented Prescription | ||||
|---|---|---|---|---|---|
| Estimate | 95% CI | Difference | 95% CI | P Value | |
| Asthma on problem list (probability) | |||||
| Non-Hispanic white | 61.2 | (58.2, 64.3) | REF | ||
| US-born Latino | 50.7 | (42.6, 58.7) | −10.6 | (−19.1, −2.1) | .015 |
| Foreign-born Latino | 63.2 | (48.8, 77.7) | 2.0 | (−12.2, 16.2) | .782 |
| Asthma severity on problem list (probability) | |||||
| Non-Hispanic white | 17.5 | (15.4, 19.5) | REF | ||
| US-born Latino | 22.9 | (17.1, 28.6) | 5.4 | (−0.8, 11.6) | .089 |
| Foreign-born Latino | 17.5 | (9.0, 26.1) | 0.1 | (−8.6, 8.7) | .989 |
| Albuterol Rx ever (probability) | |||||
| Non-Hispanic white | 87.1 | (85.0, 89.2) | REF | ||
| US-born Latino | 90.9 | (88.0, 93.7) | 3.7 | (0.2, 7.2) | .036 |
| Foreign-born Latino | 92.5 | (85.0, 100.0) | 5.4 | (−2.2, 13.0) | .166 |
| Albuterol Rx yearly (rate) | |||||
| Non-Hispanic white | 3.8 | (3.2, 4.4) | REF | ||
| US-born Latino | 6.9 | (2.9, 11.0) | 3.1 | (−0.4,6.7) | .085 |
| Foreign-born Latino | 4.3 | (1.5, 7.0) | 0.4 | (−1.9,2.8) | .707 |
| Inhaled corticosteroid (ICS) Rx ever (probability) | |||||
| Non-Hispanic white | 35.0 | (32.6, 37.3) | REF | ||
| US-born Latino | 27.7 | (24.0, 31.4) | −7.3 | (−11.7, −2.8) | .001 |
| Foreign-born Latino | 42.5 | (31.6, 53.4) | 7.5 | (−3.4, 18.5) | .179 |
| ICS Rx ever, among those with persistent asthma (probability) | |||||
| Non-Hispanic white | 72.9 | (67.0, 78.7) | REF | ||
| US-born Latino | 74.2 | (67.3, 81.2) | 1.3 | (−7.4, 10.0) | .763 |
| Foreign-born Latino | 82.9 | (69.5, 96.3) | 10.0 | (−4.0, 24.1) | .163 |
| Oral steroid Rx ever (probability) | |||||
| Non-Hispanic white | 25.5 | (23.8, 27.2) | REF | ||
| US-born Latino | 23.9 | (19.2, 28.7) | −1.6 | (−6.6, 3.5) | .545 |
| Foreign-born Latino | 27.8 | (14.9, 40.7) | 2.3 | (−10.5, 15.1) | .722 |
| Oral steroid Rx ever, among those with persistent asthma (probability) | |||||
| Non-Hispanic white | 38.7 | (35.1, 42.2) | REF | ||
| US-born Latino | 38.0 | (30.2, 45.7) | −0.7 | (−8.9, 7.5) | .867 |
| Foreign-born Latino | 29.7 | (9.1, 50.3) | −9.0 | (−30.1, 12.1) | .404 |
CI indicates confidence interval; REF, reference; and Rx, prescription. Statistically significant results (ie, P value <.05) are bolded. Estimates were derived using inverse probability of treatment weighting logistic (binary outcomes) or negative binomial (rates outcomes) regression and robust sandwich variance estimation for clustering of patients within clinics. For all analyses except those pertaining to children with persistent asthma, additional regression adjustment was made for insurance type as this remained imbalanced between groups after weighting. For analyses that did subset to those with persistent asthma, additional regression adjustment was made for insurance type, federal poverty level and age as these remained imbalanced between groups after weighting.
We examined the same problem list documentation and medication prescriptions among our place of birth groups (Table 4). Cuban-born children were more likely to have asthma documented on their problem list and more likely to have ICSs prescribed. Mexican children were more likely to ever have had an albuterol prescription. Guatemalan-born children were more likely to ever have ICSs prescribed and less likely to ever have OSs prescribed when diagnosed with persistent asthma.
Table 4.
Asthma Care-Quality Measures in Children With ICD-Coded Asthma, Comparing Latino Country of Origin to Non-Hispanic Whites
| Predicted Probability of Asthma Care Quality Measures, Denoted as %, or Rate of Documented Prescription | |||||
|---|---|---|---|---|---|
| Care-Quality Measure | Estimate | 95% CI | Difference | 95% CI | P Value |
| Asthma on problem list (probability) | |||||
| Non-Hispanic white | 61.7 | (58.5, 65.0) | REF | ||
| US-born Latino | 51.1 | (43.3, 58.8) | −10.6 | (−18.6, −2.6) | .009 |
| Cuba-born Latino | 85.4 | (66.6, 104.2) | 23.6 | (4.5, 42.7) | .015 |
| Guatemala-born Latino | 47.7 | (32.6, 62.8) | −14.1 | (−29.2, 1.1) | .069 |
| Mexico-born Latino | 66.3 | (48.0, 84.7) | 4.6 | (−13.6, 22.8) | .620 |
| Asthma severity on problem list (probability) | |||||
| Non-Hispanic white | 17.2 | (15.0, 19.3) | REF | ||
| US-born Latino | 22.6 | (17.4, 27.8) | 5.4 | (−0.3, 11.1) | .062 |
| Cuba-born Latino | 13.9 | (0.0, 29.7) | −3.3 | (−19.2, 12.6) | .683 |
| Guatemala-born Latino | 27.1 | (9.8, 44.3) | 9.9 | (−7.5, 27.3) | .265 |
| Mexico-born Latino | 14.0 | (3.6, 24.3) | −3.2 | (−13.6, 7.2) | .547 |
| Albuterol Rx ever (probability) | |||||
| Non-Hispanic white | 87.6 | (85.4, 89.8) | REF | ||
| US-born Latino | 91.2 | (88.7, 93.6) | 3.6 | (0.1, 7.1) | .043 |
| Cuba-born Latino | 89.6 | (82.4, 96.7) | 2.0 | (−6.0, 10.0) | .627 |
| Guatemala-born Latino | 92.4 | (85.8, 99.1) | 4.8 | (−2.6, 12.3) | .200 |
| Mexico-born Latino | 98.3 | (95.4, 101.2) | 10.7 | (7.0, 14.4) | <.001 |
| Albuterol Rx yearly (rate) | |||||
| Non-Hispanic white | 3.4 | (2.9, 3.9) | REF | ||
| US-born Latino | 5.7 | (3.8, 7.7) | 2.3 | (0.6, 4.0) | .009 |
| Cuba-born Latino | 2.9 | (1.8, 4.0) | −0.5 | (−1.4, 0.4) | .299 |
| Guatemala-born Latino | 8.2 | (1.3, 15.1) | 4.8 | (−2.0, 11.6) | .166 |
| Mexico-born Latino | 4.5 | (0.6, 8.3) | 1.1 | (−2.5, 4.6) | .555 |
| Inhaled corticosteroid Rx ever (probability) | |||||
| Non-Hispanic white | 35.0 | (32.3, 37.7) | REF | ||
| US-born Latino | 27.6 | (23.6, 31.5) | −7.3 | (−12.0, −2.8) | .002 |
| Cuba-born Latino | 52.0 | (44.5, 59.6) | 17.1 | (8.2, 25.9) | <.001 |
| Guatemala-born Latino | 52.0 | (31.2, 72.8) | 17.0 | (−3.5, 37.6) | .104 |
| Mexico-born Latino | 32.3 | (16.2, 48.5) | −2.6 | (−18.7, 13.4) | .748 |
| Inhaled corticosteroid Rx ever, among those with persistent asthma (probability) | |||||
| Non-Hispanic white | 70.5 | (64.4, 76.6) | REF | ||
| US-born Latino | 71.4 | (63.5, 79.2) | 0.9 | (−8.3, 10.1) | .852 |
| Cuba-born Latino* | NA | NA | |||
| Guatemala-born Latino | 87.4 | (83.5, 91.2) | 16.9 | (9.5, 24.2) | <.001 |
| Mexico-born Latino | 73.9 | (55.3, 92.5) | 3.4 | (−15.4, 22.3) | .720 |
| Oral steroid Rx ever (probability) | |||||
| Non-Hispanic white | 24.8 | (22.8, 26.6) | REF | ||
| US-born Latino | 23.0 | (18.9, 27.1) | −1.7 | (−6.2, 2.9) | .456 |
| Cuba-born Latino | 22.2 | (16.4, 28.0) | −2.6 | (−8.8, 3.7) | .422 |
| Guatemala-born Latino | 37.9 | (13.0, 62.9) | 13.2 | (−11.7, 38.1) | .300 |
| Mexico-born Latino | 21.6 | (11.4, 31.9) | −3.1 | (−13.8, 7.5) | .566 |
| Oral steroid Rx ever, among those with persistent asthma (probability) | |||||
| Non-Hispanic white | 38.7 | (34.9, 42.5) | REF | ||
| US-born Latino | 35.9 | (28.0, 43.8) | −2.8 | (−11.2, 5.6) | .515 |
| Cuba-born Latino | 54.3 | (20.3, 88.3) | 15.6 | (−19.3, 50.5) | .381 |
| Guatemala-born Latino | 5.5 | (0.0, 13.4) | −33.2 | (−42.2, −24.2) | <.001 |
| Mexico-born Latino | 41.3 | (20.8, 61.9) | 2.7 | (−18.0, 23.3) | .799 |
CI indicates confidence interval; REF, reference; Rx, prescription. Statistically significant results (ie, P value <.05) are bolded. Estimates were derived using inverse probability of treatment weighting logistic (binary outcomes) or negative binomial (rates outcomes) regression and robust sandwich variance estimation for clustering of patients within clinics. For all analyses except those pertaining to children with persistent asthma, additional regression adjustment was made for age, body mass index, federal poverty level, insurance type, and number of yearly visits as these remained imbalanced between group after weighting. For analyses subsetted to children with persistent asthma, additional regression adjustment was made for the aforementioned (age, body mass index, federal poverty level, insurance, yearly visits) and for sex.
Two observations were dropped due to insufficient sample size.
Yearly Influenza Vaccination
US-born (rate ratio = 1.67, 95% CI, 1.39–2.00) and foreign-born Latino children (rate ratio = 1.77, 95% CI, 1.32 −2.33) had higher rates of yearly influenza immunization than non-Hispanic white children. This was true in our entire study sample and among those with ICD-coded asthma (data not shown).
Discussion
We performed a novel analysis of the asthma care received by Latino children with a documented place of birth in a multistate network of CHCs in order to assess the care provided to Latino children by nativity. In this setting, many of our findings did not reveal disparities between Latino groups and non-Hispanic white comparators, including measures of EHR documentation, except for problem list in US-born Latinos, and some measures of medication prescription. This adds to a growing literature base that suggests that CHC care may help to mitigate inequity by delivering equitable care among those who can access these clinics.19,20 However, direct comparisons of CHC care to care in other settings would evaluate CHC care even further.
These findings largely disprove our hypothesis and suggest that if there are inequities in the course and outcomes of asthma among foreign-born Latino children, they may stem from other sources than these primary care measures provided in CHCs. Several other notable themes emerged from our analyses, including that there were minimal differences in diagnosis prevalence in children presenting with symptoms, US-born Latino children were less likely to have some asthma measures documented, foreign-born Latino children were not less likely to have similar measures documented, and all Latino children were more likely to have yearly influenza vaccinations.
Latino children (US- or foreign-born) were not less likely to be diagnosed with asthma than non-Hispanic whites whenever they presented with suspicious symptoms of asthma at a visit; place of birth in foreign-born children also was not associated with lower likelihood of diagnosis when presenting with a symptom. Previous research has focused on overall asthma prevalence in ethnic/native subgroups,1-4 but small differences in population prevalence may be less useful to clinicians at the point of care. Ours is one of the first large scale studies with a long study period to document similar proportions of diagnosis in children presenting with asthma symptoms. This underscores the importance of maintaining access to CHCs for vulnerable populations when experiencing symptoms.
US-born Latino children with asthma were less likely to have asthma documented on their problem list, more likely to have ever had an albuterol prescription, and less likely to have ever had an ICS prescribed (although not when being diagnosed with persistent asthma). More frequent albuterol, less frequent problem list documentation, and less ICS prescription may be indicative of more reactive/less proactive care. In several conditions, US-born Latinos have been noted to have worse outcomes/poorer disease courses than whites or foreign-born Latinos.21,22 This difference in asthma has been attributed to the healthy immigrant hypothesis23; our findings suggest that the difference between the disease course of the groups might be in the health care that they are able to utilize. However, when diagnosed with persistent asthma (the group with clear indication for inhaled steroids), US-born Latino children did not differ from other groups in ICS prescription, which reinforces that appropriate documentation of diagnosis may be a key step in care quality/equity. Overall, however, these findings underscore the need to target health disparity reduction in asthma in Latino children across the spectrum of nativity, especially in the US-born.
Although foreign-born Latino children showed higher estimates of albuterol rates and probability of ICS prescription, and lower probability of OS, these were not statistically significant. It is notable that foreign-born children, whom we hypothesized to be more likely to not receive the same care measures as non-Hispanic whites, did not receive less in the measures we studied. Future research will need to examine additional factors in foreign-born Latino children, such as community level social determinants of health that may affect asthma outcomes, or more detailed and secondary care measures like medication adherence, or use of care for asthma exacerbations.
Mexican children were more likely to have ever received an albuterol prescription, and Guatemalan children were more likely to receive ICSs but less likely to receive OSs. More frequent prescription of albuterol, while not signifying a lack of care overall, may indicate worse asthma control. Frequent use of albuterol can make the medication less effective24 and is an indication for other medications to be prescribed to achieve better control.7,8 Further research is needed to understand this pattern in Mexican children. Guatemalan children had the preferable pattern of more ICSs and fewer OSs, suggesting appropriate maintenance medications for their asthma.
Latino patients, regardless of birth place, had higher rates of annual influenza vaccinations than non-Hispanic whites. This is consistent with work in other Latino populations and with other immunizations.19 It underscores that while immunizations remain a priority in asthma care (and prevention in general), Latino children in CHCs do not suffer differential use of influenza vaccine as compared to non-Hispanic whites. Other work has suggested that Latino populations may be at risk for vaccine hesitancy,25 but our findings suggest that significant numbers of Latinos—especially those accessing care at CHCs—are actually high utilizers of vaccines. This may need to be considered in society-wide vaccination campaigns. White populations may need more education or intervention on this issue.
Our work has limitations. Our analysis does not utilize a gold standard for asthma diagnosis; therefore, we could not ascertain accuracy of diagnoses. Asthma severity was noted in a minority of patients; findings could differ is this documentation was more universal. Further work can examine this association by validating these chart diagnoses against spirometry. We did not have medication adherence, more specific symptom and albuterol use frequency information, or education data, all of which are crucial in asthma management. Rates of prescription fills and other markers of adherence need to be examined in settings such as CHCs, where many children receive the majority of their health care.15 Our analysis included only Latino children with a place of birth documented in the EHR, so may not represent all foreign or US-born Latinos. Collection of this country of origin is not common; further research is necessary to understand why some patients have this documented and others do not. It is also crucial to understand the degree to which providers view and utilize these data when available, and whether it impacts the care which is delivered. We also only had sufficient sample size to analyze 3 countries of origin outside the United States. In our dataset, Puerto Rican children are considered US-born. This differs from many previous analyses, although Puerto Rican children have access to a form of Medicaid26 and may not face the same potential immigration-related barriers as our foreign-born group. While it is possible that patients received care outside of the CHCs in our network, this is generally a population with fewer health care options27 and previous work has suggested that patients in our network do not leave, even when they undergo insurance change.28 Additional investigations into the influence of parental nativity on US-born children would also be a key next step and factor we were unable to consider and may factor significantly into asthma care.29 Finally, medications received in the emergency department would only be included if the primary care clinic recorded those medications in the EHR.
Conclusions
We found that in US CHCs, settings where a large volume of asthma care is delivered to low-income children, there were few disparities between Latino children and non-Hispanic white comparators in many common asthma care measures. Of note, US-born Latino children with asthma were less likely to have asthma documented on their problem list, more likely to have ever had an albuterol prescription, and less likely to have ever had an ICS prescribed, although not when being diagnosed with persistent asthma. Foreign-born children, whom we hypothesized to be more likely to not receive the same care measures as non-Hispanic whites, received equivalent care to non-Hispanic white children in the measures we studied. Latino patients, regardless of birth place, had higher rates of annual influenza vaccinations than non-Hispanic whites. The CHC model of care needs further study for its potential to mitigate health inequity, and providers should understand that their US-born Latino children may be at elevated risk for not receiving adequate asthma care. Further research can more fully investigate the asthma course of US-born Latino children.
Supplementary Material
What’s New?
This study demonstrates equitable care for foreign-born Latino children in the United States community health centers, and documents less utilization of some primary care measures for asthma in US-born Latino children.
Acknowledgments
The research reported in this manuscript was conducted with the ADVANCE (Accelerating Data Value Across a National Community Health Center Network) Clinical Research Network, a partner of PCOR-net, the National-Patient Centered Clinical Network, an initiative of the Patient Centered outcomes Research Institute (PCORI). The ADVANCE network is led by OCHIN in partnership with the Health Choice Network, Fenway Health, Oregon Health and Science University, and the Robert Graham Center/HealthLandscape. ADVANCE is funded through PCORI award number 13-060-4716.
Funding:
This work received funding from the United States National Institute for Minority Health and Health Disparities (Grant no. R01MD011404).
Footnotes
The authors have no conflicts of interest to disclose.
Financial disclosure: The other authors have indicated they have no financial relationships relevant to this article to disclose.
Supplementary Data
Supplementary data related to this article can be found online at https://doi.org/10.1016/j.acap.2021.10.003.
Contributor Information
John Heintzman, Department of Family Medicine, Oregon Health & Science University, Portland, Ore; OCHIN Inc., Portland, Ore.
Jorge Kaufmann, Department of Family Medicine, Oregon Health & Science University, Portland, Ore.
Steffani Bailey, Department of Family Medicine, Oregon Health & Science University, Portland, Ore.
Jennifer Lucas, Department of Family Medicine, Oregon Health & Science University, Portland, Ore.
Shakira F. Suglia, Department of Epidemiology, Emory University Rollins School of Public Health, Atlanta, Ga.
Jon Puro, OCHIN Inc., Portland, Ore.
Sophia Giebultowicz, OCHIN Inc., Portland, Ore.
David Ezekiel-Herrera, Department of Family Medicine, Oregon Health & Science University, Portland, Ore.
Miguel Marino, Biostatistics Group, OHSU-PSU School of Public Health, Portland, Ore.
References
- 1.Camacho-Rivera M, Kawachi I, Bennett GG, et al. Revisiting the Hispanic health paradox: the relative contributions of nativity, country of origin, and race/ethnicity to childhood asthma. J Immigr Minor Health.. 2015;17:826–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eldeirawi KM, Persky VW. Associations of acculturation and country of birth with asthma and wheezing in Mexican American youths. J Asthma.. 2006;43:279–286. [DOI] [PubMed] [Google Scholar]
- 3.Holguin F, Mannino DM, Anto J, et al. Country of birth as a risk factor for asthma among Mexican Americans. Am J Respir Crit Care Med. 2005;171:103–108. [DOI] [PubMed] [Google Scholar]
- 4.Iqbal S, Oraka E, Chew GL, et al. Association between birthplace and current asthma: the role of environment and acculturation. Am J Public Health. 2014;104(suppl 1):S175–S182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arcoleo KJ, McGovern C, Kaur K, et al. Longitudinal patterns of Mexican and Puerto Rican Children's Asthma Controller Medication Adherence and Acute Healthcare use. Ann Am Thorac Soc. 2019;16:715–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holguin F, Mannino DM, Antó J, et al. Country of birth as a risk factor for asthma among Mexican Americans. Am J Respir Crit Care Med. 2005;171:103–108. [DOI] [PubMed] [Google Scholar]
- 7.British Thoracic Society. British Guideline on the Management of Asthma. Available at: https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/. Accessed March 1, 2021.
- 8.National Heart Lung, and Blood Institute. Guidelines From the National Asthma Education and Prevention Program. 2007. Available at: https://www.nhlbi.nih.gov/health-topics/guidelines-for-diagnosis-management-of-asthma. Accessed March 1, 2021.
- 9.Center for Medicare/Medicaid Services. Eligible Professional Meaningful Use Core Measures Measure 3 of 13. 2014. Available at: https://www.cms.gov/regulations-and-guidance/legislation/ehrincentiveprograms/downloads/ep_mu_tableofcontents.pdf. Accessed March 1, 2021.
- 10.Kharat AA, Borrego ME, Raisch DW, et al. Assessing disparities in the receipt of inhaled corticosteroid prescriptions for asthma by Hispanic and non-Hispanic white patients. Ann Am Thorac Soc. 2015;12:174–183. [DOI] [PubMed] [Google Scholar]
- 11.Crocker D, Brown C, Moolenaar R, et al. Racial and ethnic disparities in asthma medication usage and health-care utilization: data from the National Asthma Survey. Chest. 2009;136:1063–1071. [DOI] [PubMed] [Google Scholar]
- 12.Grohskopf LA, Alyanak E, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices - United States, 2019-20 influenza season. MMWR Recomm Rep. 2019;68:1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anandappa M, Adjei Boakye E, Li W, et al. Racial disparities in vaccination for seasonal influenza in early childhood. Public Health. 2018;158:1–8. [DOI] [PubMed] [Google Scholar]
- 14.Schuller KA, Probst JC. Factors associated with influenza vaccination among US children in 2008. J Infect Public Health. 2013;6:80–88. [DOI] [PubMed] [Google Scholar]
- 15.National Association of Community Health Centers. Community Health Center Chartbook 2020. .Available at: https://www.nachc.org/research-and-data/research-fact-sheets-and-infographics/chartbook-2020-final/. Accessed February 1, 2021.
- 16.Hueston W. BMJ Best Practice: Acute Bronchitis. .Available at: https://bestpractice.bmj.com/topics/en-us/135. Accessed February 1, 2021. [Google Scholar]
- 17.McCaffrey DF, Griffin BA, Almirall D, et al. A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat Med. 2013;32:3388–3414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kenyon CC, et al. Variability in diagnosed asthma in young children in a large pediatric primary care network. Acad Pediatr. 2021;20:958–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heintzman J, Bailey SR, Cowburn S, et al. Pneumococcal vaccination in low-income Latinos: an unexpected trend in Oregon Community Health Centers. J Health Care Poor Underserved.. 2016;27:1733–1744. [DOI] [PubMed] [Google Scholar]
- 20.Heintzman J, Hatch B, Coronado G, et al. Role of race/fthnicity, language, and insurance in use of cervical cancer prevention services among low-income Hispanic women, 2009-2013. Prev Chronic Dis. 2018;15:E25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sangaramoorthy M, Yang J, DeRouen MC, et al. Disparities in hepatocellular carcinoma incidence in California: an update. Cancer Epidemiol Biomark Prev. 2020;29:79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fryar CD, Fakhouri TH, Carroll MD. The association of nativity/length of residence and cardiovascular disease risk factors in the United States. Prev Med. 2020;130:105893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jerschow E, Strizich G, Xue X, et al. Effect of relocation to the U.S. on asthma risk among Hispanics. Am J Prev Med. 2017;52:579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nelson HS, Raine D, Doner HC, et al. Subsensitivity to the bronchodilator action of albuterol produced by chronic administration. Am Rev Respir Dis. 1977;116:871–878. [DOI] [PubMed] [Google Scholar]
- 25.Grohskopf LA, Liburd LC, Redfield RR. Addressing influenza vaccination disparities during the COVID-19 pandemic. JAMA. 2020;324:1029–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Center for Medicare/Medicaid Services. Puerto Rico. 2021. Available at: https://www.medicaid.gov/state-overviews/puerto-rico.html. Accessed February 1, 2021.
- 27.Rodríguez MA, Bustamante AV, Ang A. Perceived quality of care, receipt of preventive care, and usual source of health care among undocumented and other Latinos. J Gen Intern Med. 2009;24(suppl 3):508–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Malley JP, O’Keeffe-Rosetti M, Lowe RA, et al. Health care utilization rates after Oregon’s 2008 Medicaid expansion: within-group and between-group differences over time among new, returning, and continuously insured enrollees. Med Care. 2016;54:984–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weinstein SM, et al. Parent nativity and child asthma control in families of Mexican Heritage: the effects of parent depression and social support. Acad Pediatr. 2021;20:967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.BMJ Best Practice. Acute Bronchitis. 2018. Available at: https://bestpractice.bmj.com/topics/en-us/135. Accessed February 1, 2021. [Google Scholar]
- 31.Jolly SE, Navaneethan SD, Schold JD, et al. Chronic kidney disease in an electronic health record problem list: quality of care, ESRD, and mortality. Am J Nephrol. 2014;39:288–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wright A, McCoy AB, Hickman TT, et al. Problem list completeness in electronic health records: a multi-site study and assessment of success factors. Int J Med Inform. 2015;84:784–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coleman K, Austin BT, Brach C, et al. Evidence on the chronic care model in the new millennium. Health Aff (Millwood). 2009;28:75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.