Abstract
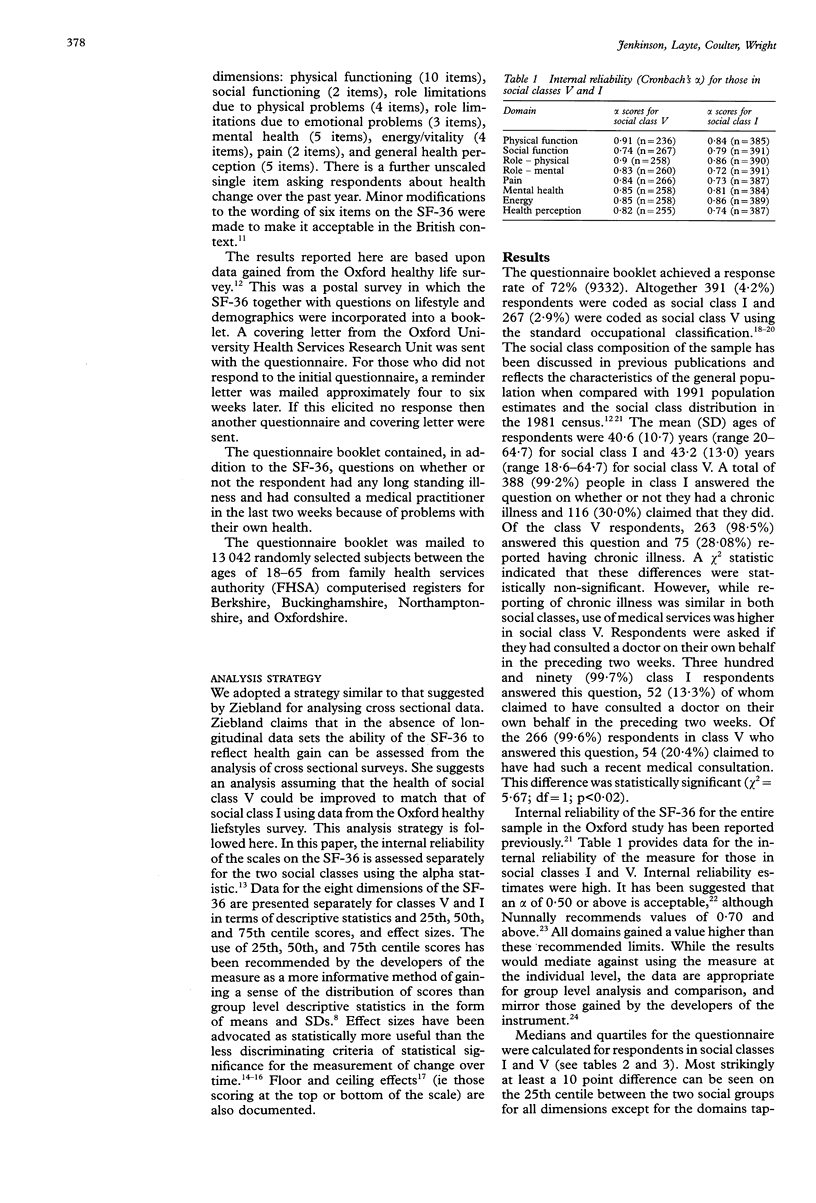
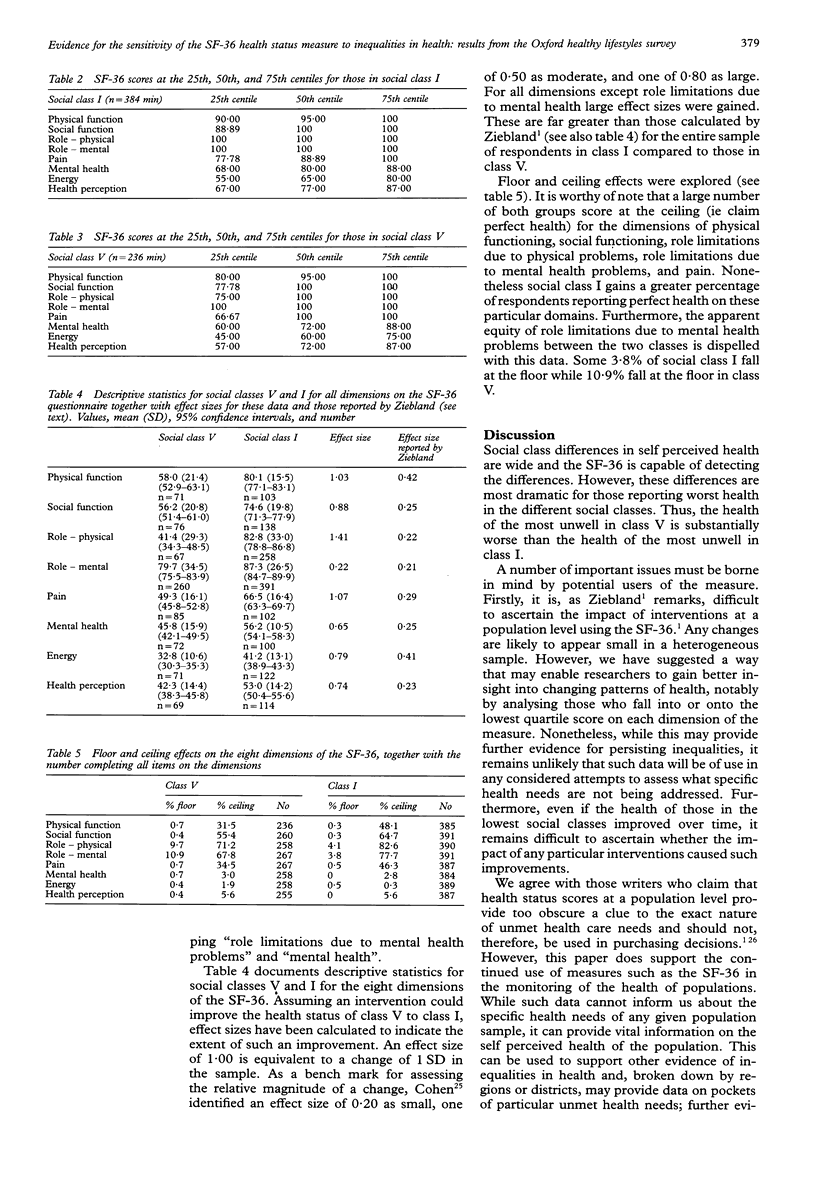
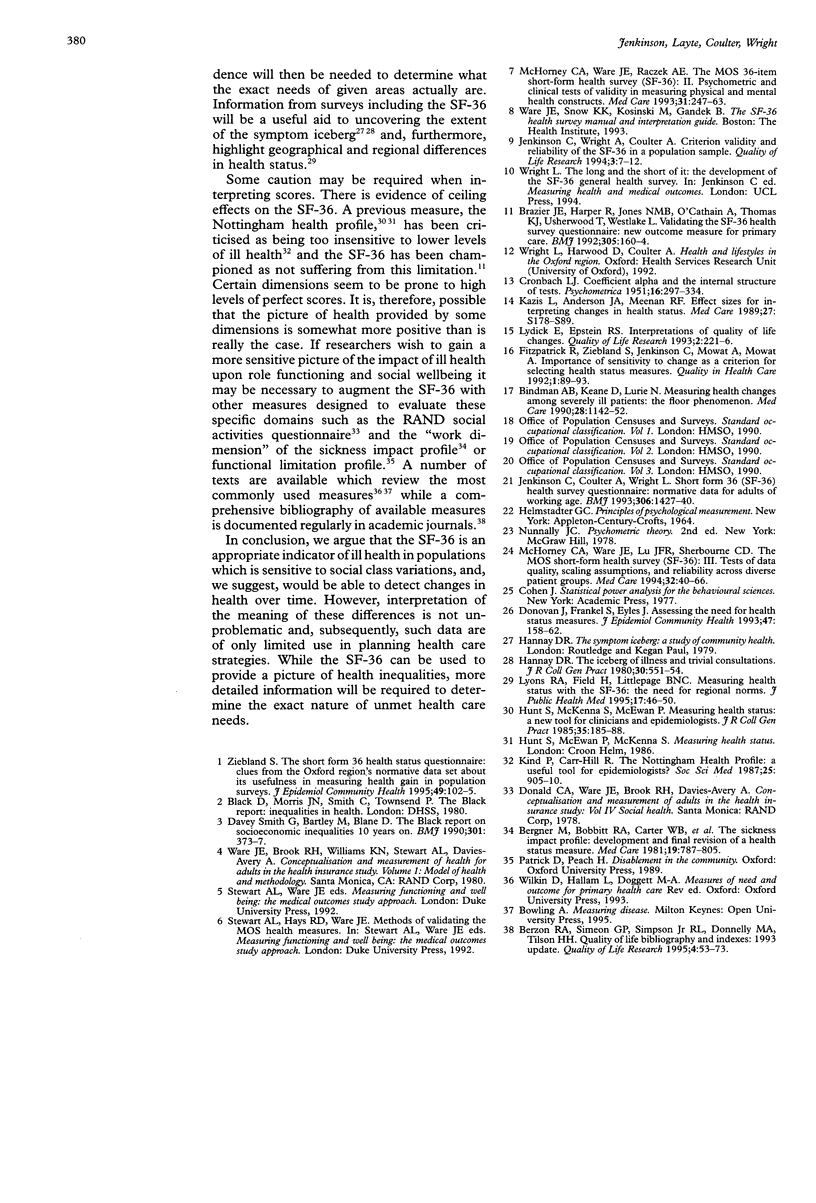
OBJECTIVES: The short form 36 (SF-36) health questionnaire may not be appropriate for population surveys assessing health gain because of the low responsiveness (sensitivity to change) of domains on the measure. An hypothesised health gain of respondents in social class V to that of those in social class I indicated only marginal improvement in self reported health. Subgroup analysis, however, showed that the SF-36 would indicate dramatic changes if the health of social class V could be improved to that of social class I. DESIGN: Postal survey using a questionnaire booklet containing the SF-36 and a number of other items concerned with lifestyles and illness. A letter outlining the purpose of the study was included. SETTING: The sample was drawn from family health services authority (FHSA) computerised registers for Berkshire, Buckinghamshire, Northamptonshire, and Oxfordshire. SAMPLE: The questionnaire was sent to 13,042 randomly selected subjects between the ages of 17-65. Altogether 9332 (72%) responded. OUTCOME MEASURES: Scores for the eight dimensions of the SF-36. STATISTICS: The sensitivity of the SF-36 was tested by hypothesising that the scores of those in the bottom quartile of the SF-36 scores in class V could be improved to the level of the scores from the bottom quartile of SF-36 scores in class I using the effect size statistic. RESULTS: SF-36 scores for the population at the 25th, 50th, and 75th centiles were provided. Those who reported worse health on each dimension of the SF-36 (ie in the lowest 25% of scores) differ dramatically between social class I and V. Large effect sizes were gained on all but one dimension of the SF-36 when the health of those in the bottom quartile of the SF-36 scores in class V were hypothesised to have improved to the level of the scores from the bottom quartile of SF-36 scores in class I. CONCLUSIONS: Analysis of SF-36 data at a population level is inappropriate; subgroup analysis is more appropriate. The data suggest that if it were possible to improve the functioning and wellbeing of those in worst health in class V to those reporting the worst health in class I the improvement would be dramatic. Furthermore, differences between the classes detected by the SF-36 are substantial and more dramatic than might previously have been imagined.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bergner M., Bobbitt R. A., Carter W. B., Gilson B. S. The Sickness Impact Profile: development and final revision of a health status measure. Med Care. 1981 Aug;19(8):787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- Berzon R. A., Simeon G. P., Simpson R. L., Jr, Donnelly M. A., Tilson H. H. Quality of life bibliography and indexes: 1993 update. Qual Life Res. 1995 Feb;4(1):53–74. doi: 10.1007/BF00434384. [DOI] [PubMed] [Google Scholar]
- Bindman A. B., Keane D., Lurie N. Measuring health changes among severely ill patients. The floor phenomenon. Med Care. 1990 Dec;28(12):1142–1152. doi: 10.1097/00005650-199012000-00003. [DOI] [PubMed] [Google Scholar]
- Brazier J. E., Harper R., Jones N. M., O'Cathain A., Thomas K. J., Usherwood T., Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992 Jul 18;305(6846):160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan J. L., Frankel S. J., Eyles J. D. Assessing the need for health status measures. J Epidemiol Community Health. 1993 Apr;47(2):158–162. doi: 10.1136/jech.47.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick R., Ziebland S., Jenkinson C., Mowat A., Mowat A. Importance of sensitivity to change as a criterion for selecting health status measures. Qual Health Care. 1992 Jun;1(2):89–93. doi: 10.1136/qshc.1.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannay D. R. The 'iceberg' of illness and 'trivial' consultations. J R Coll Gen Pract. 1980 Sep;30(218):551–554. [PMC free article] [PubMed] [Google Scholar]
- Hunt S. M., McEwen J., McKenna S. P. Measuring health status: a new tool for clinicians and epidemiologists. J R Coll Gen Pract. 1985 Apr;35(273):185–188. [PMC free article] [PubMed] [Google Scholar]
- Jenkinson C., Wright L., Coulter A. Criterion validity and reliability of the SF-36 in a population sample. Qual Life Res. 1994 Feb;3(1):7–12. doi: 10.1007/BF00647843. [DOI] [PubMed] [Google Scholar]
- Kazis L. E., Anderson J. J., Meenan R. F. Effect sizes for interpreting changes in health status. Med Care. 1989 Mar;27(3 Suppl):S178–S189. doi: 10.1097/00005650-198903001-00015. [DOI] [PubMed] [Google Scholar]
- Kind P., Carr-Hill R. The Nottingham health profile: a useful tool for epidemiologists? Soc Sci Med. 1987;25(8):905–910. doi: 10.1016/0277-9536(87)90260-7. [DOI] [PubMed] [Google Scholar]
- Lydick E., Epstein R. S. Interpretation of quality of life changes. Qual Life Res. 1993 Jun;2(3):221–226. doi: 10.1007/BF00435226. [DOI] [PubMed] [Google Scholar]
- Lyons R. A., Fielder H., Littlepage B. N. Measuring health status with the SF-36: the need for regional norms. J Public Health Med. 1995 Mar;17(1):46–50. [PubMed] [Google Scholar]
- McHorney C. A., Ware J. E., Jr, Lu J. F., Sherbourne C. D. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994 Jan;32(1):40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- McHorney C. A., Ware J. E., Jr, Raczek A. E. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993 Mar;31(3):247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- Smith G. D., Bartley M., Blane D. The Black report on socioeconomic inequalities in health 10 years on. BMJ. 1990 Aug 18;301(6748):373–377. doi: 10.1136/bmj.301.6748.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziebland S. The short form 36 health status questionnaire: clues from the Oxford region's normative data about its usefulness in measuring health gain in population surveys. J Epidemiol Community Health. 1995 Feb;49(1):102–105. doi: 10.1136/jech.49.1.102. [DOI] [PMC free article] [PubMed] [Google Scholar]


