Abstract
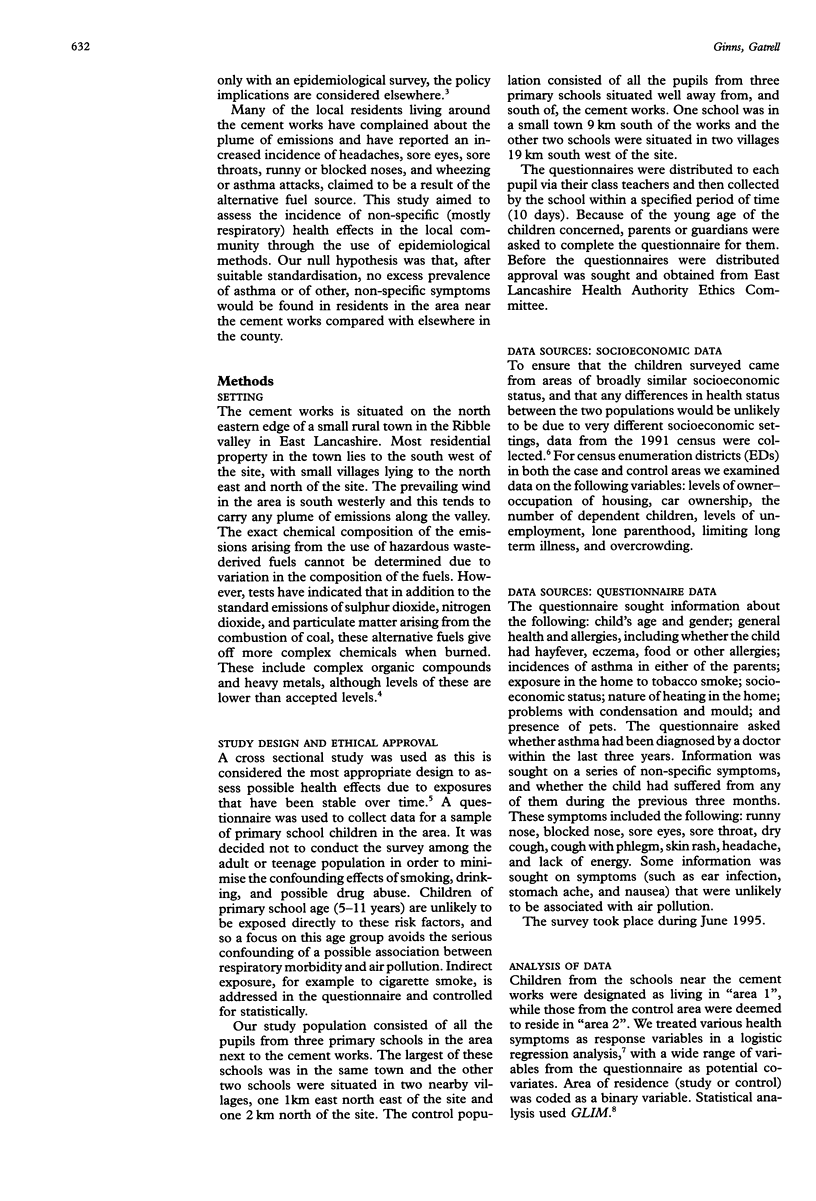
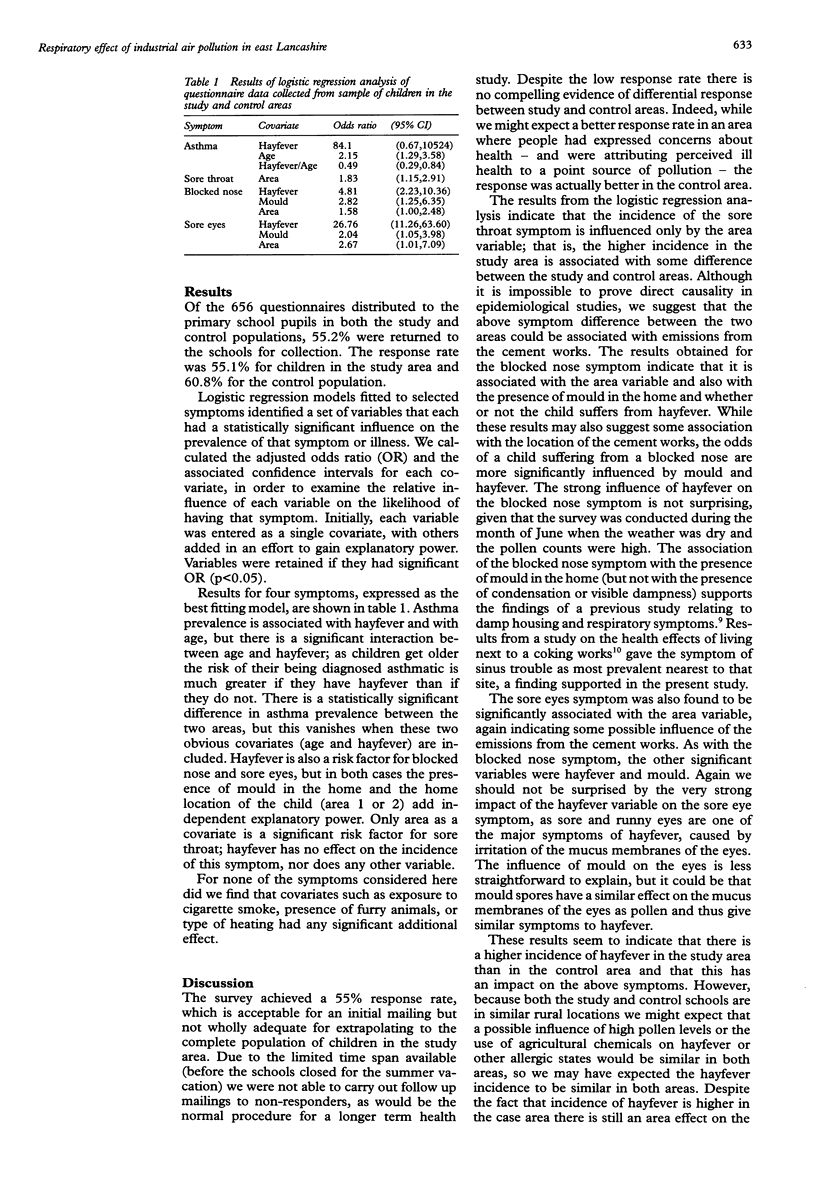
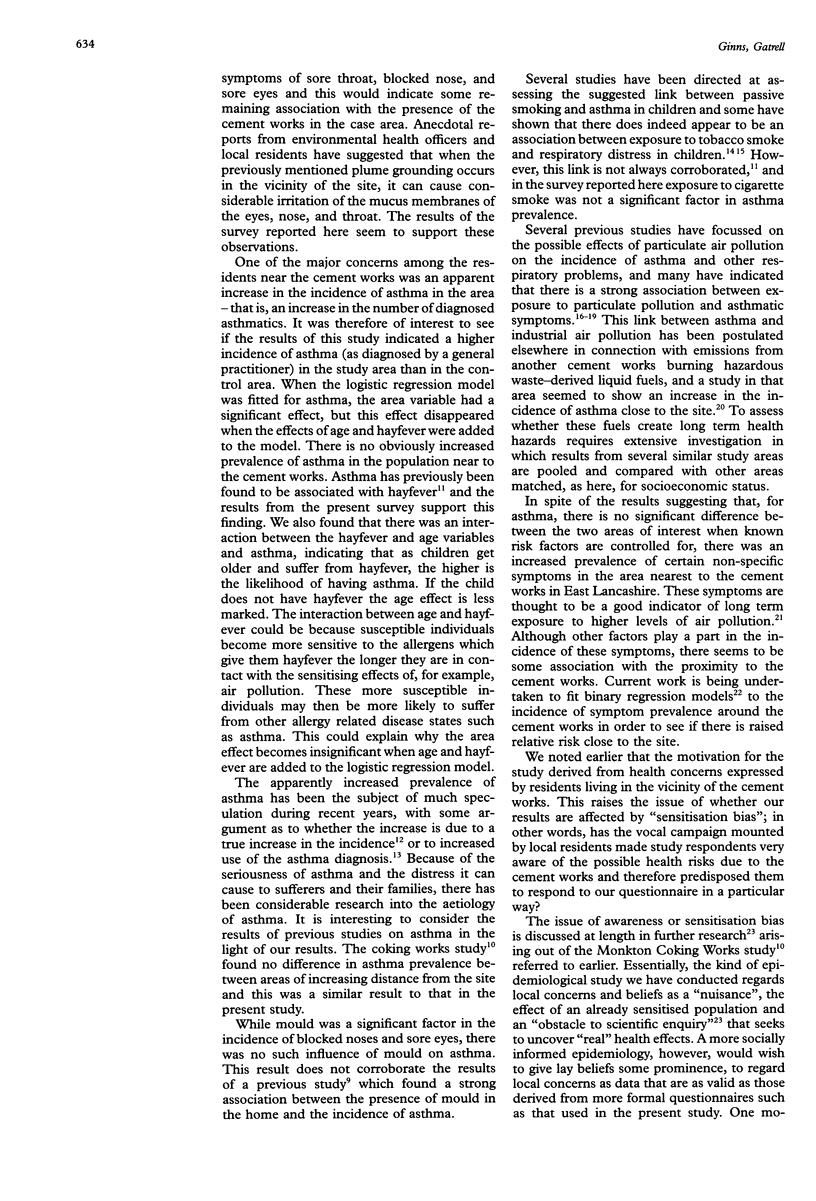
STUDY OBJECTIVE: To determine whether there was a higher incidence of respiratory ill health in children living near to a cement works than in those from a different area, and if so whether the higher incidence was due to the use of a hazardous waste-derived fuel at the works. STUDY DESIGN: A sample of the population of children living near the cement works (the study area) was compared with a sample of children living between 9 and 19 km away from the site (the control area). SETTING: The cement works is located on the north eastern edge of a small rural town in east Lancashire. METHODS: Data were collected via the use of a health questionnaire. This was distributed through selected primary schools to families who had one or more children of primary school age (5-11 years). MAIN RESULTS: The study and control populations were comparable in terms of response rates, gender, and socioeconomic indicators. There was no significant difference in the incidence of asthma (as diagnosed by a general practitioner) between the two areas when adjustment for hayfever was made. The incidence of sore throat was significantly higher in the case area, a difference not explained by other factors. For two other non-specific indicators of respiratory health (blocked nose and sore eyes) there was a significantly higher incidence in the study area, although hayfever and mould were also significant influences. CONCLUSIONS: The results indicated that certain non-specific health indicators were more common in the children living near a cement works. This excess may be due to exposure to emissions from the site. However, it is not possible to draw firm conclusions because there are no epidemiological data predating the use of the hazardous waste derived fuel.
Full text
PDF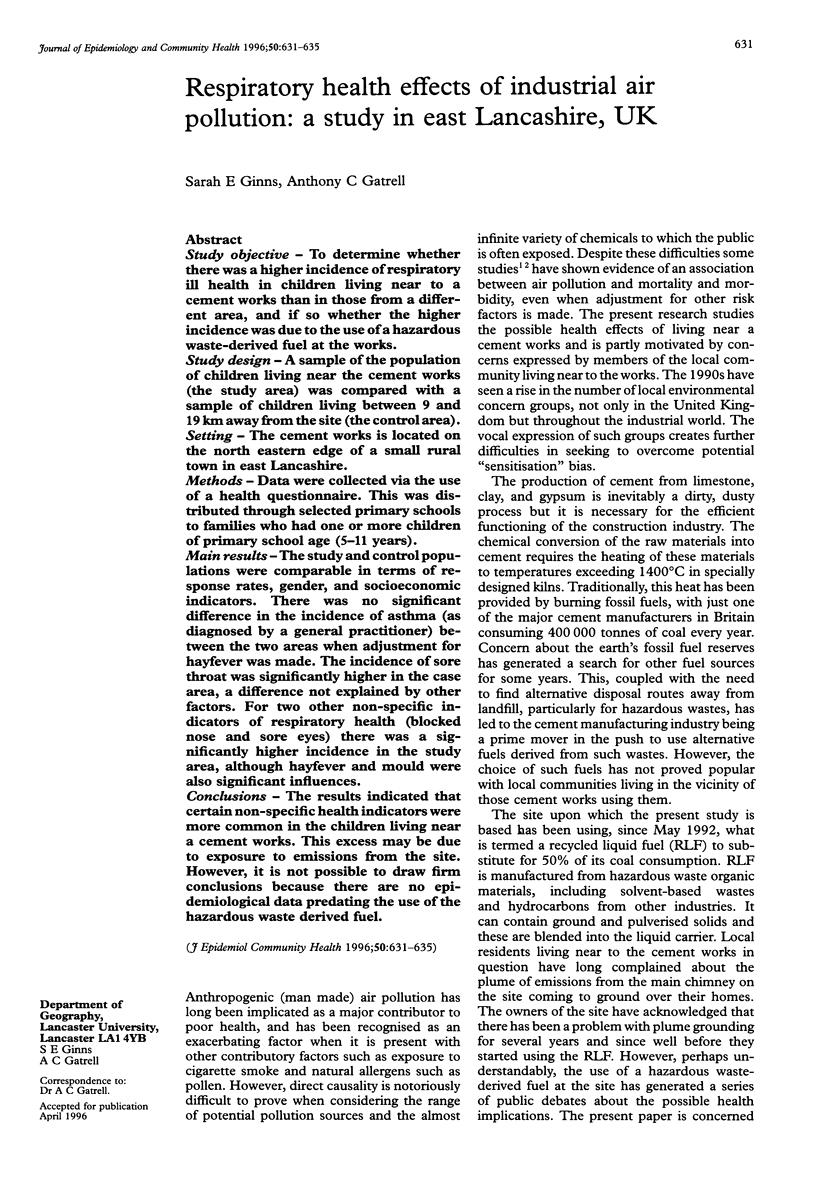
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abbey D. E., Petersen F., Mills P. K., Beeson W. L. Long-term ambient concentrations of total suspended particulates, ozone, and sulfur dioxide and respiratory symptoms in a nonsmoking population. Arch Environ Health. 1993 Jan-Feb;48(1):33–46. doi: 10.1080/00039896.1993.9938391. [DOI] [PubMed] [Google Scholar]
- Agudo A., Bardagí S., Romero P. V., González C. A. Exercise-induced airways narrowing and exposure to environmental tobacco smoke in schoolchildren. Am J Epidemiol. 1994 Sep 1;140(5):409–417. doi: 10.1093/oxfordjournals.aje.a117263. [DOI] [PubMed] [Google Scholar]
- Bates D. V. Health indices of the adverse effects of air pollution: the question of coherence. Environ Res. 1992 Dec;59(2):336–349. doi: 10.1016/s0013-9351(05)80040-4. [DOI] [PubMed] [Google Scholar]
- Bhopal R. S., Phillimore P., Moffatt S., Foy C. Is living near a coking works harmful to health? A study of industrial air pollution. J Epidemiol Community Health. 1994 Jun;48(3):237–247. doi: 10.1136/jech.48.3.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burney P. G., Chinn S., Rona R. J. Has the prevalence of asthma increased in children? Evidence from the national study of health and growth 1973-86. BMJ. 1990 May 19;300(6735):1306–1310. doi: 10.1136/bmj.300.6735.1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dockery D. W. Epidemiologic study design for investigating respiratory health effects of complex air pollution mixtures. Environ Health Perspect. 1993 Dec;101 (Suppl 4):187–191. doi: 10.1289/ehp.93101s4187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn C. E., Woodhouse J., Bhopal R. S., Acquilla S. D. Asthma and factory emissions in northern England: addressing public concern by combining geographical and epidemiological methods. J Epidemiol Community Health. 1995 Aug;49(4):395–400. doi: 10.1136/jech.49.4.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forastiére F., Corbo G. M., Michelozzi P., Pistelli R., Agabiti N., Brancato G., Ciappi G., Perucci C. A. Effects of environment and passive smoking on the respiratory health of children. Int J Epidemiol. 1992 Feb;21(1):66–73. doi: 10.1093/ije/21.1.66. [DOI] [PubMed] [Google Scholar]
- Kaplan B. A., Mascie-Taylor C. G. Biosocial factors in the epidemiology of childhood asthma in a British national sample. J Epidemiol Community Health. 1985 Jun;39(2):152–156. doi: 10.1136/jech.39.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffatt S., Phillimore P., Bhopal R., Foy C. 'If this is what it's doing to our washing, what is it doing to our lungs?' Industrial pollution and public understanding in north-east England. Soc Sci Med. 1995 Sep;41(6):883–891. doi: 10.1016/0277-9536(94)00380-c. [DOI] [PubMed] [Google Scholar]
- Pope C. A., 3rd, Dockery D. W. Acute health effects of PM10 pollution on symptomatic and asymptomatic children. Am Rev Respir Dis. 1992 May;145(5):1123–1128. doi: 10.1164/ajrccm/145.5.1123. [DOI] [PubMed] [Google Scholar]
- Schwartz J., Slater D., Larson T. V., Pierson W. E., Koenig J. Q. Particulate air pollution and hospital emergency room visits for asthma in Seattle. Am Rev Respir Dis. 1993 Apr;147(4):826–831. doi: 10.1164/ajrccm/147.4.826. [DOI] [PubMed] [Google Scholar]
- Strachan D. P., Anderson H. R. Trends in hospital admission rates for asthma in children. BMJ. 1992 Mar 28;304(6830):819–820. doi: 10.1136/bmj.304.6830.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strachan D. P., Sanders C. H. Damp housing and childhood asthma; respiratory effects of indoor air temperature and relative humidity. J Epidemiol Community Health. 1989 Mar;43(1):7–14. doi: 10.1136/jech.43.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]


