Defensins are a family of small cationic, antibiotic peptides that contain six cysteines in disulfide linkage. The mechanism of action of these peptides is based on their ability to form pores in the cytoplasmatic membrane in microorganisms. In plants and animals, the formation of a chemical shield from endogenous peptide antibiotics provides an active defense against the external microbial environment (1). This may explain the considerable resistance to infection of tissues that are constantly exposed to and colonized by microorganisms. In mammals, antimicrobial peptides are synthesized in skin, respiratory tract, and tongue epithelia (1).
The first peptide antibiotic that has been identified in humans, hBD-1, is produced constitutively in the epithelium of the urinary tract, trachea, and lungs (2, 5). In a recent study, a second human beta-defensin, hBD-2, has been isolated from skin. It has been demonstrated that hBD-2 is highly effective in killing gram-negative bacteria and Candida albicans (3). These findings prompted us to investigate whether beta-defensins are present in the conjunctiva of the human eye. The conjunctiva is prone to a variety of primary and secondary sources of inflammatory changes owing to its anatomic association with surrounding structures and the potential for exposure to extrinsic organisms and toxic agents. Bacterial infections of the conjunctiva are among the most common presenting ocular complaints of acute care.
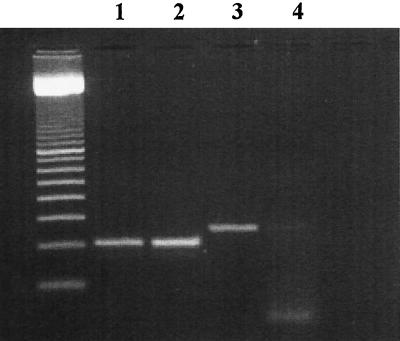
Samples of normal limbal conjunctiva were excised from two individuals who underwent intraocular surgery. Informed consent was obtained from each patient. Total cellular RNA was isolated with TRIzol (Gibco BRL, Eggenstein, Germany). The reverse transcription (RT) reaction with 1 μg of RNA of each sample was carried out in a 20-μl volume with Superscript II (Gibco BRL) according to the manufacturer’s instructions. The amplification of hBD-1 and hBD-2 was performed with 2 μl of the RT reaction mixture. Primers for hBD-1 (accession no. X92744) amplify a 206-bp fragment (hBd-1a: 5′-TCA CTT GCA GCA CTT GGC C-3′; hBD-1b: 5′-TGA GAA CTT CCT ACC TTC TG-3′). The primer design for the amplification of hBD-2 (accession no. Z71389) was that introduced by Harder et al. (3) and yielded a 255-bp fragment (hBd-2a-, 5′-CCA GCC ATC AGC CAT GAG GGT-3′; hBD-2b-, 5′-GGA GCC CTT TCT GAA TCC GCA-3′). RT-PCR derived fragments were run in 2% agarose gel electrophoresis and stained with ethidium bromide (Fig. 1).
FIG. 1.
RT-PCR products specific for human beta-defensins derived from two different conjunctiva specimens. Lanes 1 and 2, hBD-1 fragment; lanes 3 and 4, hBD-2-derived fragment. A 100-bp ladder (Pharmacia, Freiburg, Germany) is on the left.
The RT-PCR-derived signals for hBD-1 were similar in the two samples (Fig. 1, lanes 1 and 2), whereas a considerable difference was noted for hBD-2 (Fig. 1, lanes 3 and 4), indicating that hBD-2 expression may be variable. These data support the hypothesis that hBD-1 is synthesized constitutively in human conjunctival tissue, whereas the production of hBD-2 appears to be inducible by exogenous stimuli (3, 4). Since human beta-defensins have been shown to be inactivated in certain disease states (2), it seems likely that hBD-1/hBD-2-associated conjunctival immunity is compromised under various conditions, e.g., after intraocular surgery, thereby increasing the risk of bacterial infections. In view of the fact that defensins are devoid of the problems of acquired resistance, it may be speculated that the detection of conjunctival peptide antibiotics will introduce new approaches to the treatment and prophylaxis of bacterial conjunctivitis.
REFERENCES
- 1.Boman H G. Peptide antibiotics and their role in innate immunity. Annu Rev Immunol. 1995;13:61–92. doi: 10.1146/annurev.iy.13.040195.000425. [DOI] [PubMed] [Google Scholar]
- 2.Goldman M J, Anderson G M, Stolzenberg E D, Kari U P, Zasloff M, Wilson J M. Human beta-defensin-1 is a salt-sensitive antibiotic in lung that is inactivated in cystic fibrosis. Cell. 1997;88:553–560. doi: 10.1016/s0092-8674(00)81895-4. [DOI] [PubMed] [Google Scholar]
- 3.Harder J, Bartels J, Christophers E, Schröder J M. A peptide antibiotic from human skin. Nature. 1997;387:861. doi: 10.1038/43088. [DOI] [PubMed] [Google Scholar]
- 4.Stolzenberg E D, Anderson G M, Ackermann M R, Whitlock R H, Zasloff M. Epithelial antibiotic induced in states of disease. Proc Natl Acad Sci USA. 1997;94:8686–8690. doi: 10.1073/pnas.94.16.8686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao C, Wang I, Lehrer R I. Widespread expression of beta-defensin hBD-1 in human secretory glands and epithelial cells. FEBS Lett. 1996;396:319–322. doi: 10.1016/0014-5793(96)01123-4. [DOI] [PubMed] [Google Scholar]