Abstract
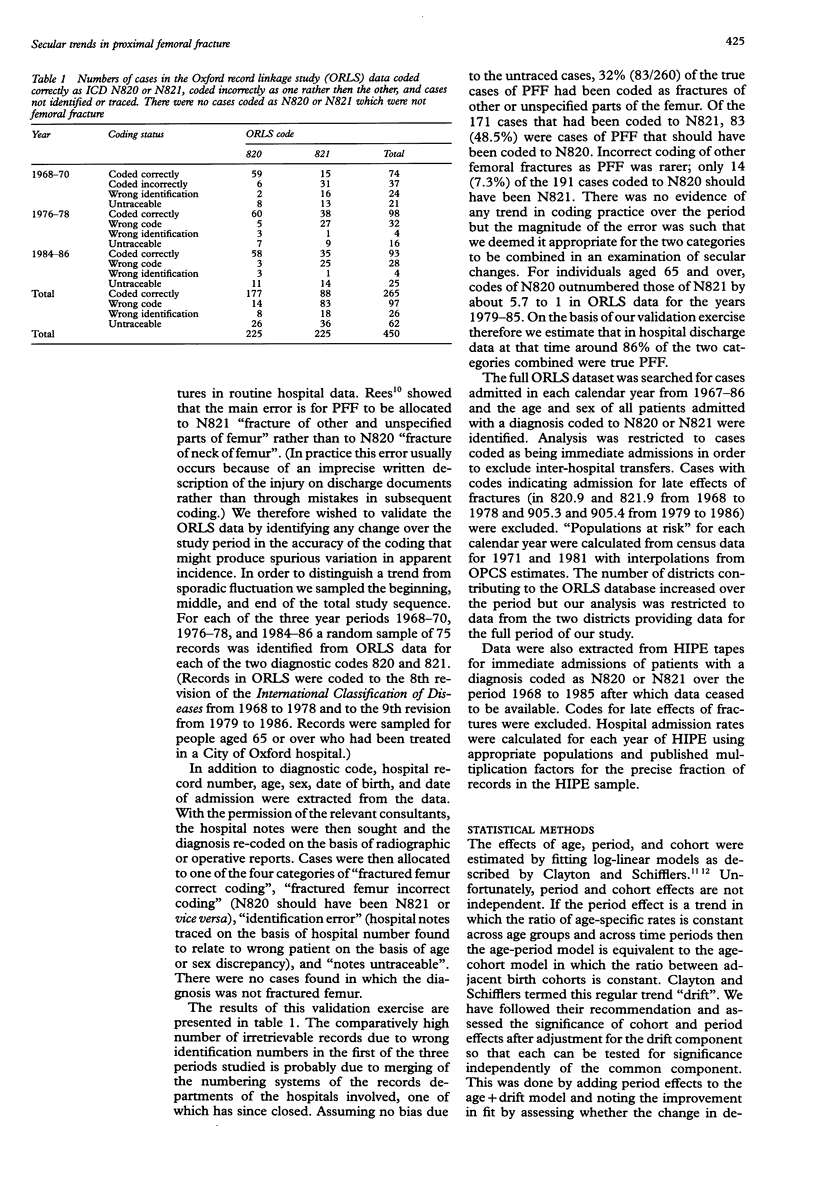
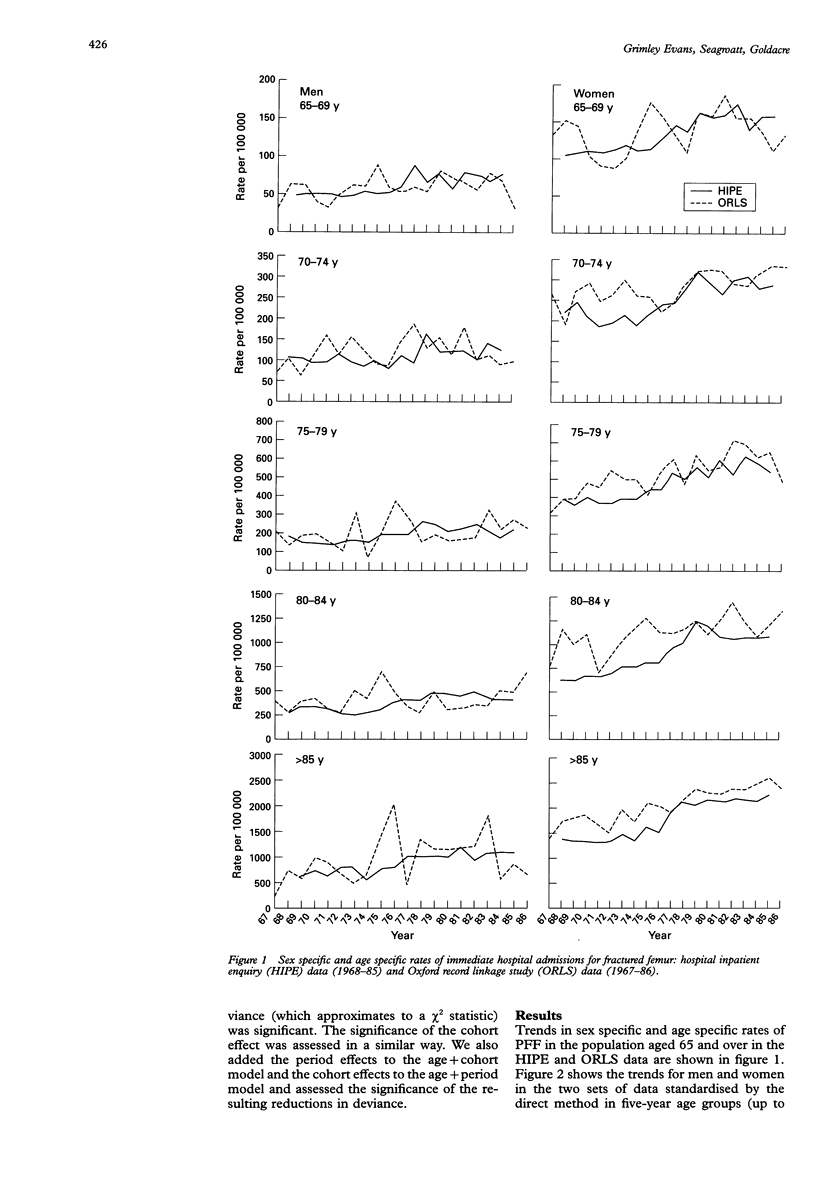
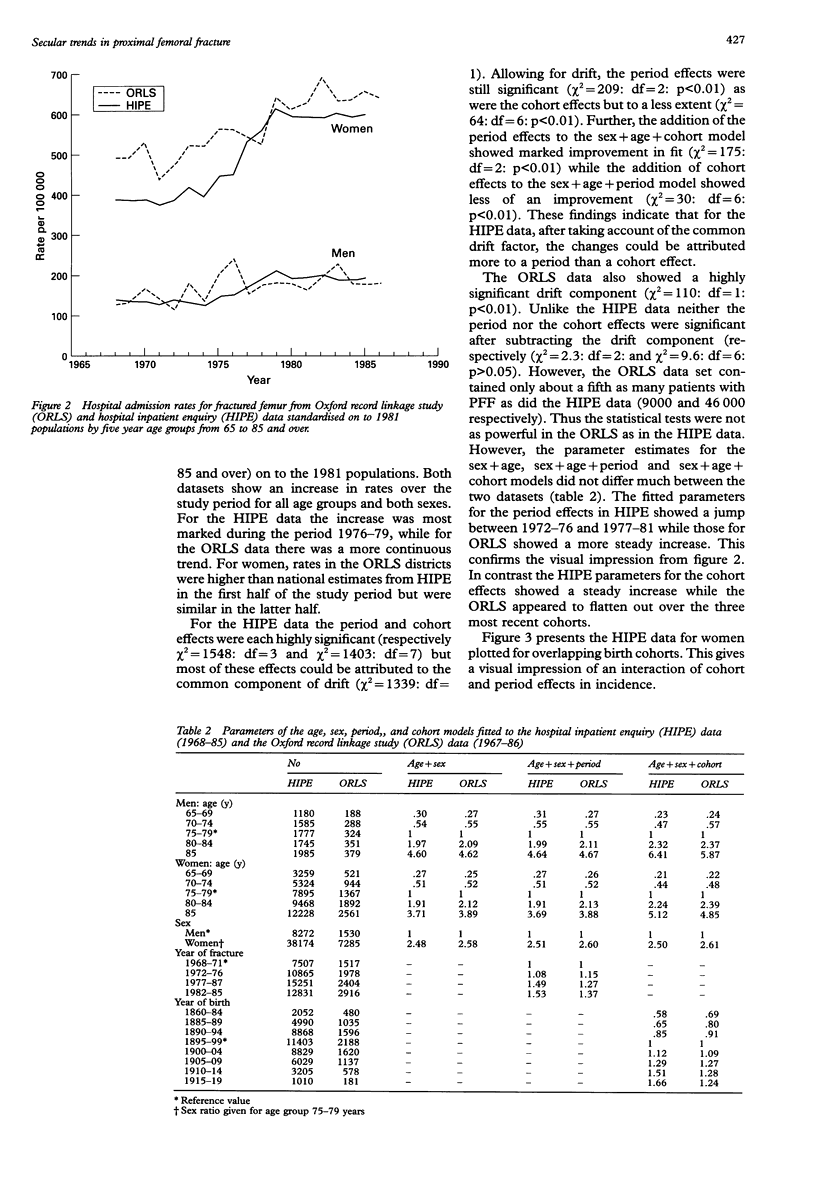
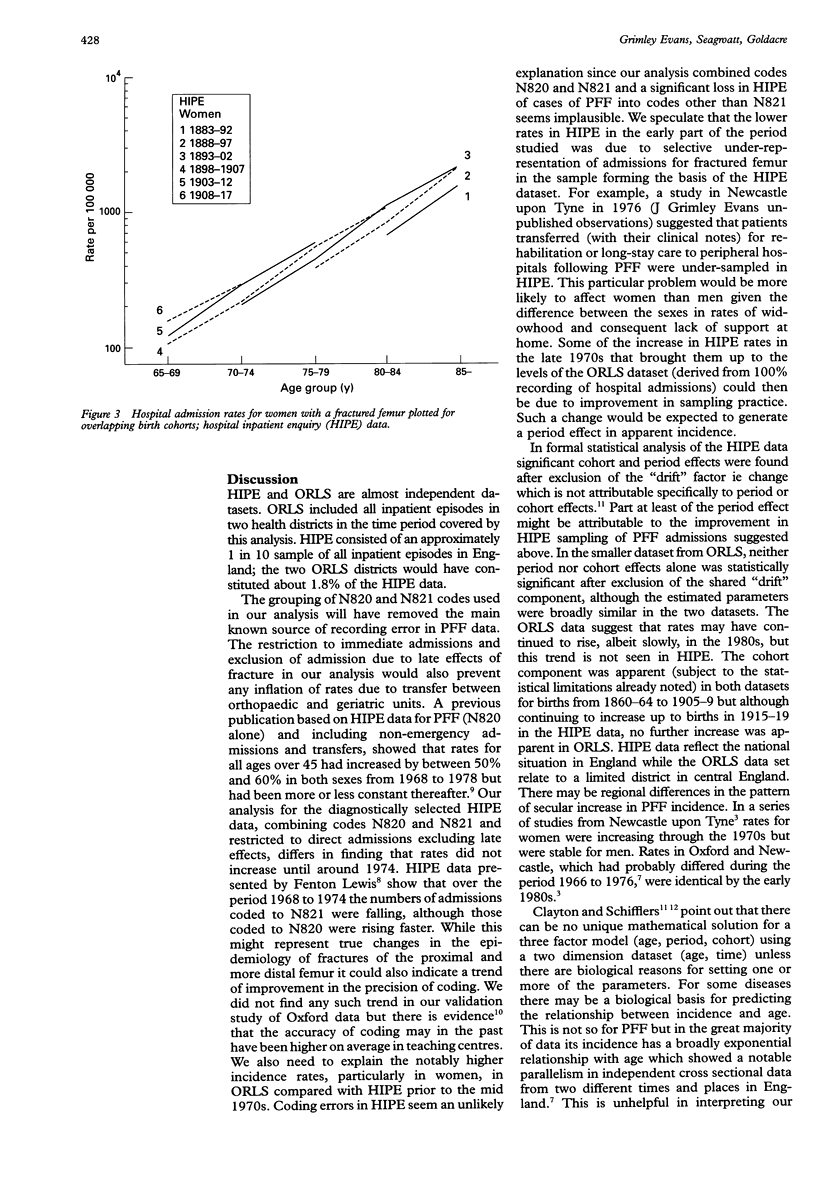
OBJECTIVE: To study hospital admission rates for fractures of the proximal femur over a period when incidence is reported to have increased, compensating for known lack of precision in coding, excluding nonemergency admissions and transfers, and modelling for age, period, and cohort effects. DESIGN: Validation of coding of a sample of hospital admissions followed by study of two sets of routinely collected statistical abstracts of hospital records; graphical analysis and statistical modelling were used to search for period and cohort effects. SETTING: Oxfordshire and west Berkshire in 1968-86, covered by the Oxford record linkage study (ORLS), and ENGLAND in 1968-85, covered by the hospital inpatient enquiry (HIPE). The ORLS and HIPE datasets are almost independent (ORLS contributed about 1.8% of the HIPE data). SUBJECTS: Records of patients aged 65 and over. OUTCOME MEASURES: Admission rates for fractured neck of femur and fracture of other and unspecified parts of femur (N820 and N821), and evidence of period and cohort effects. RESULTS: The validation study indicated that it was important to combine the codes 820 and 821 in this age group. Admission rates increased over the period studied in both HIPE and ORLS datasets. In HIPE the pattern was of two plateaux separated by a period of rapid rise in the late 1970s. In the ORLS data there was a more steady rise. Statistical analysis showed significant period and cohort effects but much of this was attributable to the component of the model common to both period and cohort effects (termed "drift"). CONCLUSIONS: The finding that admission rates increased in both datasets, combining relevant codings and restricting analysis to emergency admissions, strongly suggests that the rise was real. At least part of the period effect in the HIPE data, however, might be attributable to a sampling artefact. The cohort effect in incidence rates of femoral fracture has not been previously shown and would be compatible with a number of aetiological hypotheses.
Full text
PDF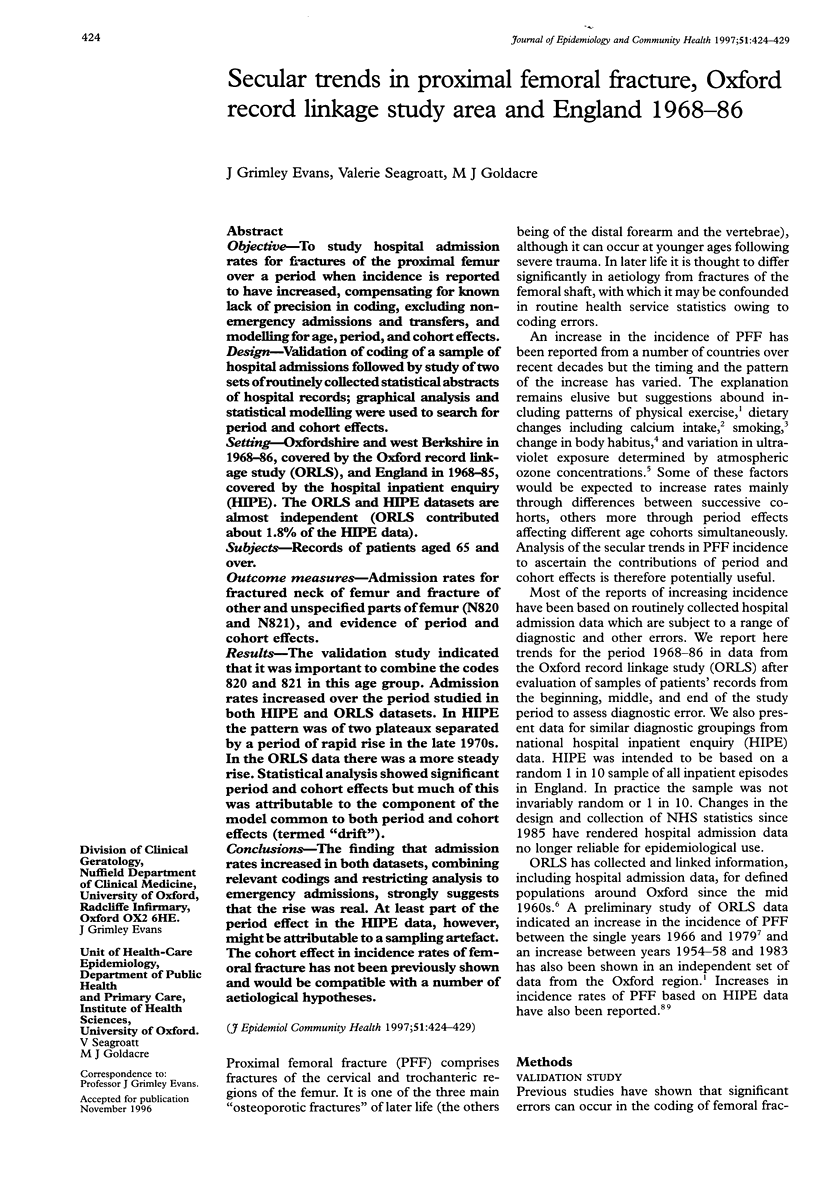
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ACHESON E. D. THE OXFORD RECORD LINKAGE STUDY: A REVIEW OF THE METHOD WITH SOME PRELIMINARY RESULTS. Proc R Soc Med. 1964 Apr;57:269–274. [PMC free article] [PubMed] [Google Scholar]
- Benn R. T. Some mathematical properties of weight-for-height indices used as measures of adiposity. Br J Prev Soc Med. 1971 Feb;25(1):42–50. doi: 10.1136/jech.25.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce W. J., Vessey M. P. Habitual physical inertia and other factors in relation to risk of fracture of the proximal femur. Age Ageing. 1988 Sep;17(5):319–327. doi: 10.1093/ageing/17.5.319. [DOI] [PubMed] [Google Scholar]
- Boyce W. J., Vessey M. P. Rising incidence of fracture of the proximal femur. Lancet. 1985 Jan 19;1(8421):150–151. doi: 10.1016/s0140-6736(85)91915-4. [DOI] [PubMed] [Google Scholar]
- Clayton D., Schifflers E. Models for temporal variation in cancer rates. I: Age-period and age-cohort models. Stat Med. 1987 Jun;6(4):449–467. doi: 10.1002/sim.4780060405. [DOI] [PubMed] [Google Scholar]
- Clayton D., Schifflers E. Models for temporal variation in cancer rates. II: Age-period-cohort models. Stat Med. 1987 Jun;6(4):469–481. doi: 10.1002/sim.4780060406. [DOI] [PubMed] [Google Scholar]
- Compston J. E., Vedi S., Croucher P. I. Low prevalence of osteomalacia in elderly patients with hip fracture. Age Ageing. 1991 Mar;20(2):132–134. doi: 10.1093/ageing/20.2.132. [DOI] [PubMed] [Google Scholar]
- Evans J. G. Incidence of proximal femoral fracture. Lancet. 1985 Apr 20;1(8434):925–926. doi: 10.1016/s0140-6736(85)91695-2. [DOI] [PubMed] [Google Scholar]
- Heaney R. P. Effect of calcium on skeletal development, bone loss, and risk of fractures. Am J Med. 1991 Nov 25;91(5B):23S–28S. doi: 10.1016/0002-9343(91)90243-q. [DOI] [PubMed] [Google Scholar]
- Leach J. F., Beadle P. C., Pingstone A. R. Effect of ozone variation on disease in Great Britain: II. Femoral neck fracture. Aviat Space Environ Med. 1978 Aug;49(8):1014–1018. [PubMed] [Google Scholar]
- Lees B., Molleson T., Arnett T. R., Stevenson J. C. Differences in proximal femur bone density over two centuries. Lancet. 1993 Mar 13;341(8846):673–675. doi: 10.1016/0140-6736(93)90433-h. [DOI] [PubMed] [Google Scholar]
- Lewis A. F. Fracture of neck of the femur: changing incidence. Br Med J (Clin Res Ed) 1981 Nov 7;283(6301):1217–1220. doi: 10.1136/bmj.283.6301.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer H. E., Tverdal A., Falch J. A. Risk factors for hip fracture in middle-aged Norwegian women and men. Am J Epidemiol. 1993 Jun 1;137(11):1203–1211. doi: 10.1093/oxfordjournals.aje.a116622. [DOI] [PubMed] [Google Scholar]
- Rees J. L. Accuracy of hospital activity analysis data in estimating the incidence of proximal femoral fracture. Br Med J (Clin Res Ed) 1982 Jun 19;284(6332):1856–1857. doi: 10.1136/bmj.284.6332.1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees J. L. Secular changes in the incidence of proximal femoral fracture in Oxfordshire: a preliminary report. Community Med. 1982 May;4(2):100–103. doi: 10.1007/BF02548823. [DOI] [PubMed] [Google Scholar]
- Reid I. R., Chin K., Evans M. C., Jones J. G. Relation between increase in length of hip axis in older women between 1950s and 1990s and increase in age specific rates of hip fracture. BMJ. 1994 Aug 20;309(6953):508–509. doi: 10.1136/bmj.309.6953.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spector T. D., Cooper C., Lewis A. F. Trends in admissions for hip fracture in England and Wales, 1968-85. BMJ. 1990 May 5;300(6733):1173–1174. doi: 10.1136/bmj.300.6733.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]


