Abstract
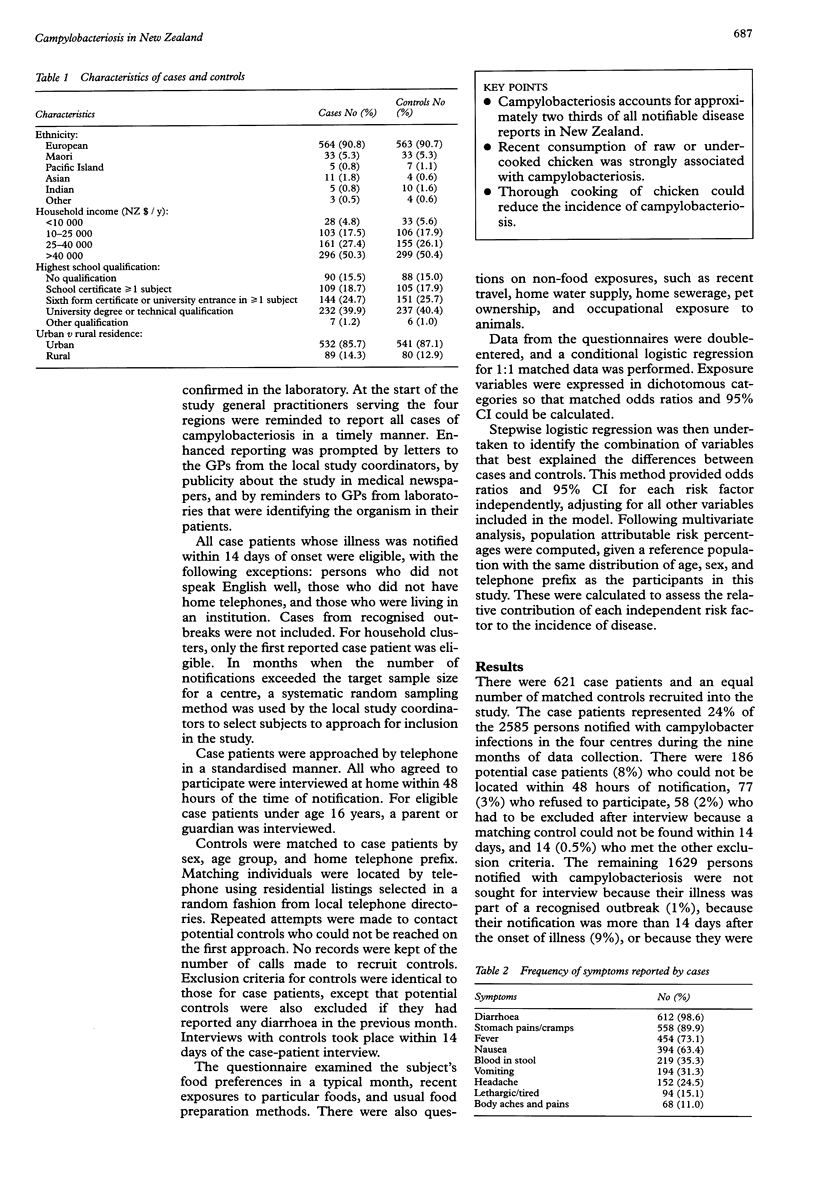
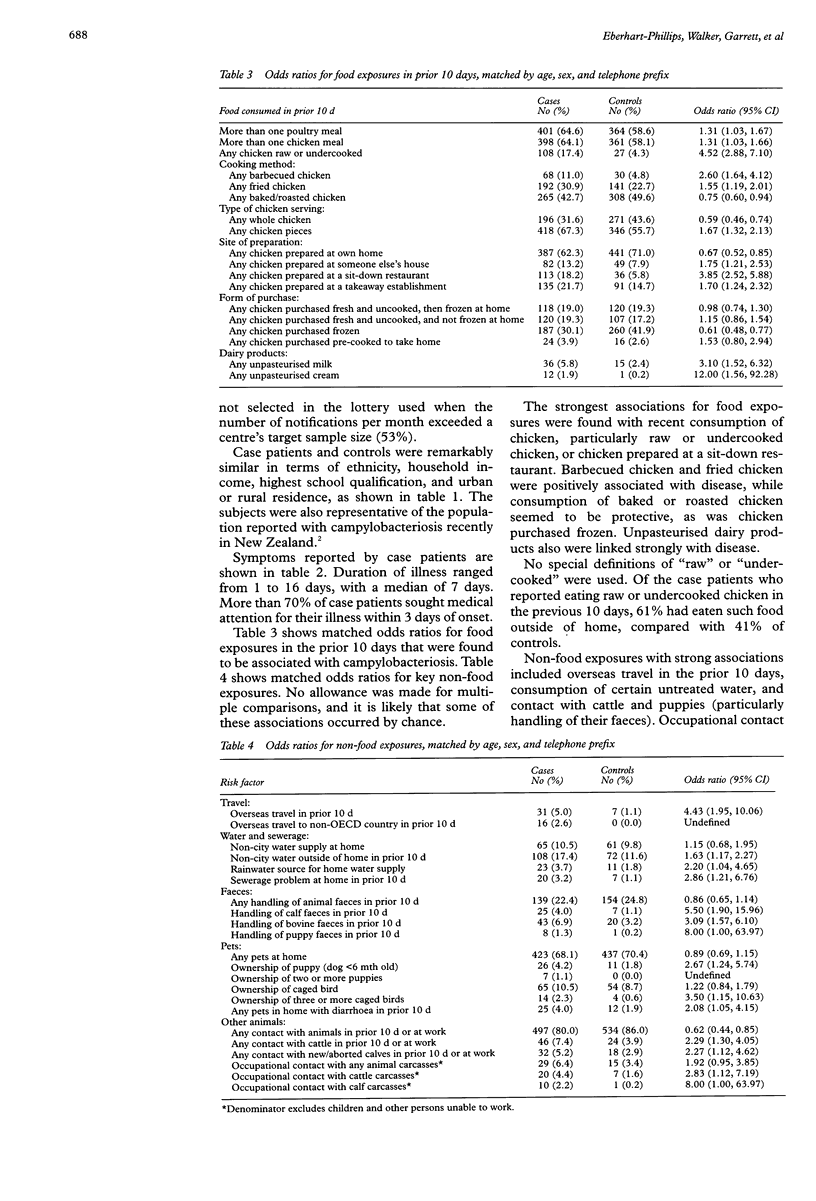
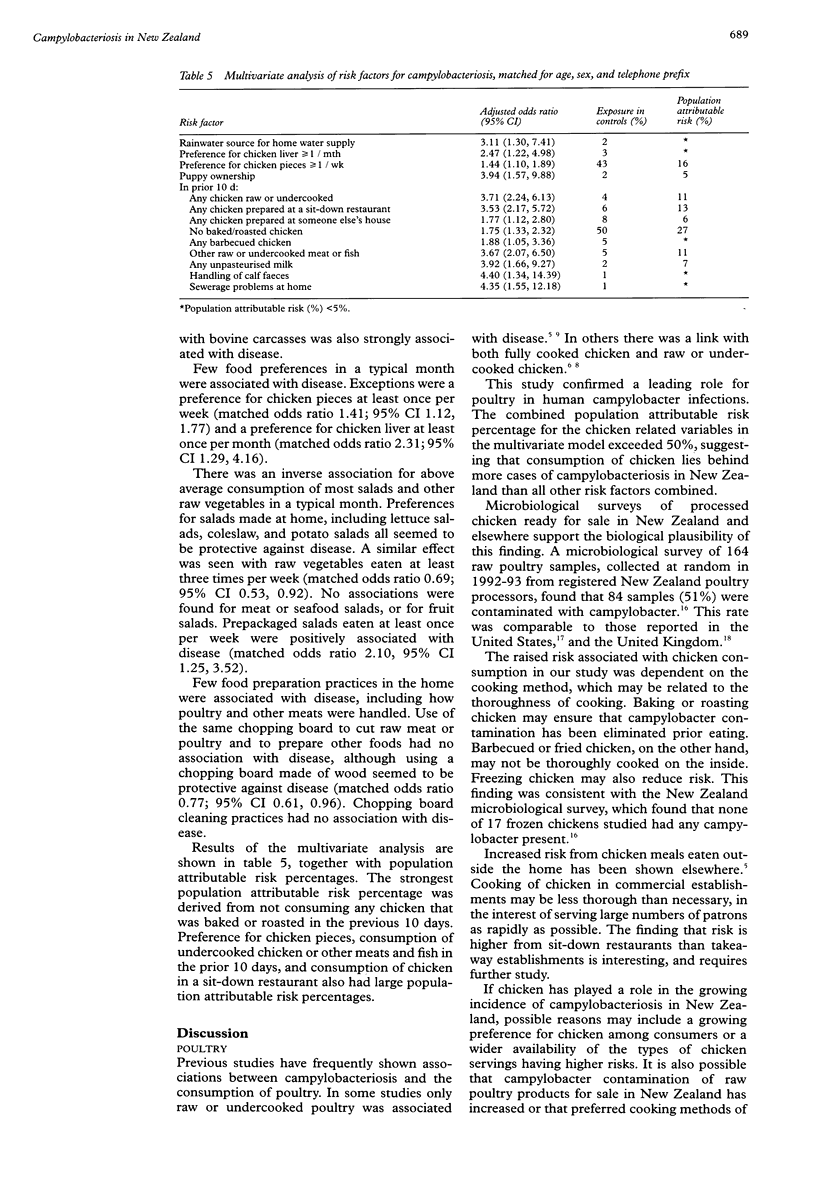
STUDY OBJECTIVE: To identify and assess the contributions of major risk factors for campylobacteriosis in New Zealand. DESIGN: Case-control study. Home interviews were conducted over nine months using a standardised questionnaire to assess recent food consumption and other exposures. SETTING: Four centres in New Zealand with high notification rates of campylobacter infections--Auckland, Hamilton, Wellington, and Christchurch. PARTICIPANTS: Case patients were 621 people notified between 1 June 1994 and 28 February 1995 as having campylobacter infection. Control subjects were selected randomly from telephone directories, and were matched 1:1 with case patients in relation to sex, age group, and home telephone prefix. RESULTS: Risk of campylobacteriosis was strongly associated with recent consumption of raw or undercooked chicken (matched odds ratio 4.52, 95% confidence interval 2.88, 7.10). There was also an increased risk with chicken eaten in restaurants (matched odds ratio 3.85; 2.52, 5.88). Recent consumption of baked or roasted chicken seemed to be protective. Campylobacteriosis was also associated with recent overseas travel, rainwater as a source of water at home, consumption of raw dairy products, and contact with puppies and cattle, particularly calves. CONCLUSIONS: Improperly cooked chicken seems to be associated with a large proportion of campylobacteriosis in New Zealand. Thorough cooking of chicken in homes and restaurants could reduce considerably the incidence of this disease.
Full text
PDF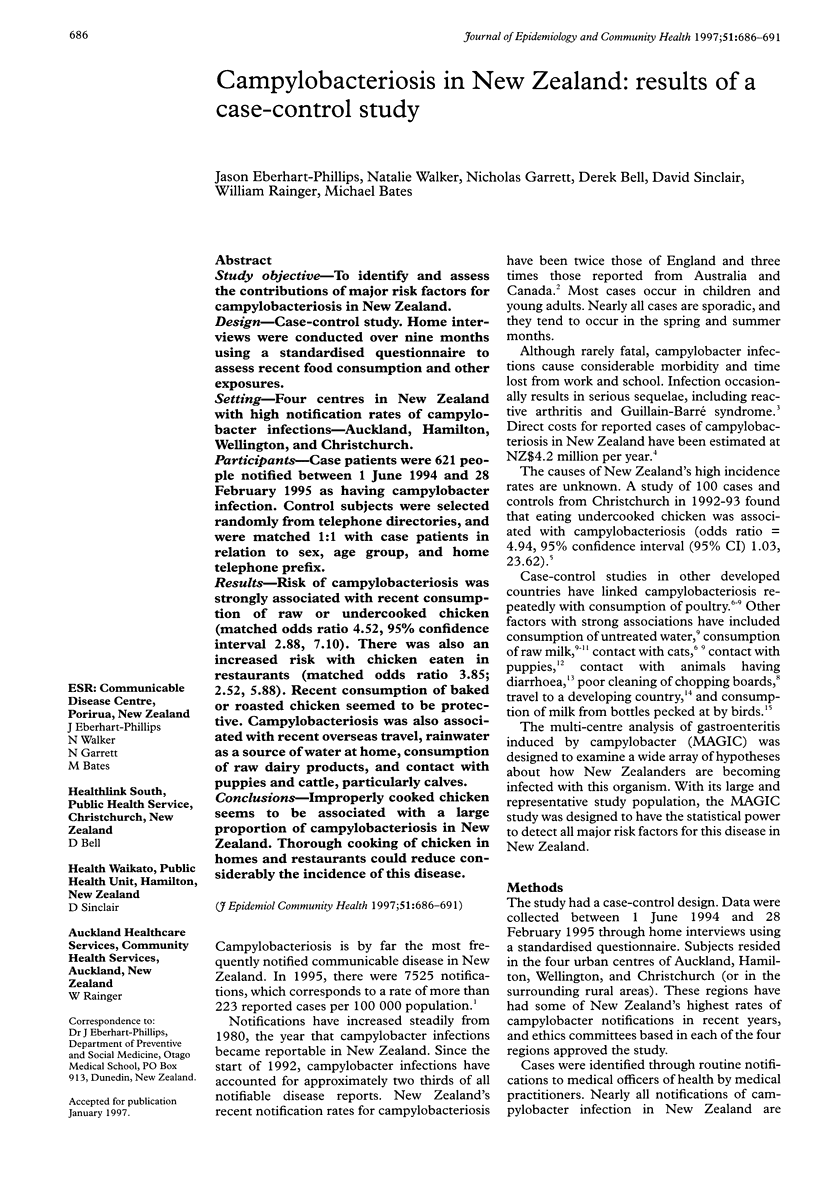

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baxter D. N. The deleterious effects of dogs on human health: 3. Miscellaneous problems and a control programme. Community Med. 1984 Aug;6(3):198–203. doi: 10.1093/oxfordjournals.pubmed.a043712. [DOI] [PubMed] [Google Scholar]
- Blaser M. J., Taylor D. N., Feldman R. A. Epidemiology of Campylobacter jejuni infections. Epidemiol Rev. 1983;5:157–176. doi: 10.1093/oxfordjournals.epirev.a036256. [DOI] [PubMed] [Google Scholar]
- Brieseman M. A. The epidemiology of campylobacter infections in Christchurch 1981-83. N Z Med J. 1985 May 22;98(779):391–393. [PubMed] [Google Scholar]
- Deming M. S., Tauxe R. V., Blake P. A., Dixon S. E., Fowler B. S., Jones T. S., Lockamy E. A., Patton C. M., Sikes R. O. Campylobacter enteritis at a university: transmission from eating chicken and from cats. Am J Epidemiol. 1987 Sep;126(3):526–534. doi: 10.1093/oxfordjournals.aje.a114685. [DOI] [PubMed] [Google Scholar]
- Harris N. V., Weiss N. S., Nolan C. M. The role of poultry and meats in the etiology of Campylobacter jejuni/coli enteritis. Am J Public Health. 1986 Apr;76(4):407–411. doi: 10.2105/ajph.76.4.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood A. M., Pearson A. D., Shahamat M. The extent of surface contamination of retailed chickens with Campylobacter jejuni serogroups. Epidemiol Infect. 1988 Feb;100(1):17–25. doi: 10.1017/s0950268800065511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins R. S., Olmsted R., Istre G. R. Endemic Campylobacter jejuni infection in Colorado: identified risk factors. Am J Public Health. 1984 Mar;74(3):249–250. doi: 10.2105/ajph.74.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikram R., Chambers S., Mitchell P., Brieseman M. A., Ikam O. H. A case control study to determine risk factors for campylobacter infection in Christchurch in the summer of 1992-3. N Z Med J. 1994 Oct 26;107(988):430–432. [PubMed] [Google Scholar]
- Kapperud G., Skjerve E., Bean N. H., Ostroff S. M., Lassen J. Risk factors for sporadic Campylobacter infections: results of a case-control study in southeastern Norway. J Clin Microbiol. 1992 Dec;30(12):3117–3121. doi: 10.1128/jcm.30.12.3117-3121.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed A. M., Harris N. V., DiGiacomo R. F. The role of exposure to animals in the etiology of Campylobacter jejuni/coli enteritis. Am J Epidemiol. 1993 Jan 1;137(1):108–114. doi: 10.1093/oxfordjournals.aje.a116592. [DOI] [PubMed] [Google Scholar]
- Schmid G. P., Schaefer R. E., Plikaytis B. D., Schaefer J. R., Bryner J. H., Wintermeyer L. A., Kaufmann A. F. A one-year study of endemic campylobacteriosis in a midwestern city: association with consumption of raw milk. J Infect Dis. 1987 Jul;156(1):218–222. doi: 10.1093/infdis/156.1.218. [DOI] [PubMed] [Google Scholar]
- Skirrow M. B. Campylobacter. Lancet. 1990 Oct 13;336(8720):921–923. doi: 10.1016/0140-6736(90)92282-m. [DOI] [PubMed] [Google Scholar]
- Southern J. P., Smith R. M., Palmer S. R. Bird attack on milk bottles: possible mode of transmission of Campylobacter jejuni to man. Lancet. 1990 Dec 8;336(8728):1425–1427. doi: 10.1016/0140-6736(90)93114-5. [DOI] [PubMed] [Google Scholar]
- Wood R. C., MacDonald K. L., Osterholm M. T. Campylobacter enteritis outbreaks associated with drinking raw milk during youth activities. A 10-year review of outbreaks in the United States. JAMA. 1992 Dec 9;268(22):3228–3230. [PubMed] [Google Scholar]


