Abstract
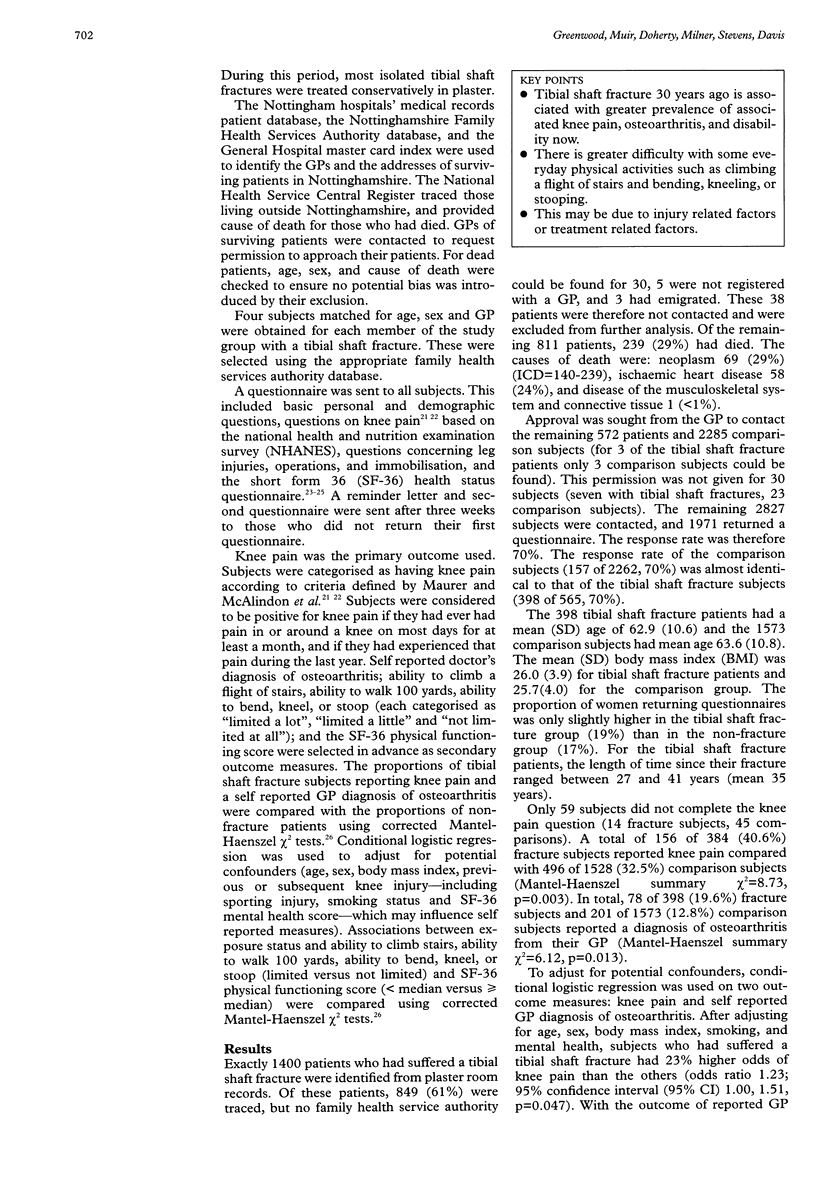
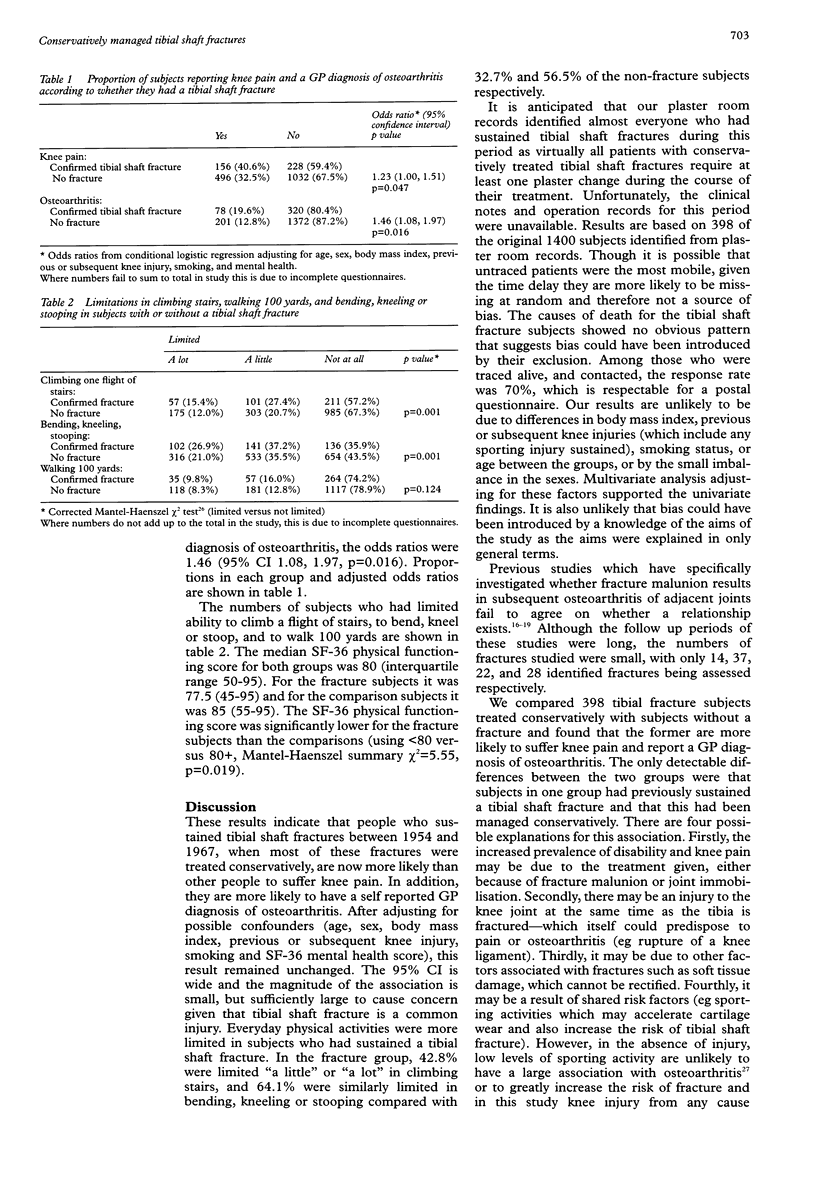
OBJECTIVES: To investigate longterm pain and disability subsequent to a tibial shaft fracture treated conservatively. DESIGN AND SETTING: Subjects who had sustained a tibial shaft fracture more than 27 years ago were compared with those who had not. SUBJECTS: 572 fracture patients (identified from the records of the plaster room) aged over 16 at the time of injury were contracted and were compared with 2285 randomly selected subjects matched for age, sex, and general practice. MAIN OUTCOME MEASURES: Self reported knee pain; self reported GP's diagnosis of osteoarthritis; ability to climb stairs, walk 100 yards, to bend, kneel, or stoop; and SF-36 physical functioning score. RESULTS: Subjects were reviewed between 27 and 41 years after tibial shaft fracture (mean 35 years). Fracture patients were more likely to suffer chronic knee pain (odds ratio 1.23; 95% confidence interval (CI) 1.00, 1.51) and report being given a diagnosis of osteoarthritis by their GP (odds ratio 1.46; 95% CI 1.08, 1.97). The ability to climb stairs, walk 100 yards, and bend, kneel, or stoop was less in the fracture group than the other subjects. The SF-36 physical function score was significantly lower in the fracture group. CONCLUSIONS: More than 27 years after a tibial shaft fracture, subjects have more knee pain than the rest of the population. They also have greater difficulty performing everyday physical activities. The excess morbidity may be due to injury factors or treatment factors, and further research is needed to investigate this important association further.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bone L. B., Johnson K. D. Treatment of tibial fractures by reaming and intramedullary nailing. J Bone Joint Surg Am. 1986 Jul;68(6):877–887. [PubMed] [Google Scholar]
- Brazier J. E., Harper R., Jones N. M., O'Cathain A., Thomas K. J., Usherwood T., Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992 Jul 18;305(6846):160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridgman S. A., Baird K. Audit of closed tibial fractures: what is a satisfactory outcome? Injury. 1993 Feb;24(2):85–89. doi: 10.1016/0020-1383(93)90194-b. [DOI] [PubMed] [Google Scholar]
- Court-Brown C. M., Christie J., McQueen M. M. Closed intramedullary tibial nailing. Its use in closed and type I open fractures. J Bone Joint Surg Br. 1990 Jul;72(4):605–611. doi: 10.1302/0301-620X.72B4.2380211. [DOI] [PubMed] [Google Scholar]
- Enneking W. F., Horowitz M. The intra-articular effects of immobilization on the human knee. J Bone Joint Surg Am. 1972 Jul;54(5):973–985. [PubMed] [Google Scholar]
- Garratt A. M., Ruta D. A., Abdalla M. I., Buckingham J. K., Russell I. T. The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS? BMJ. 1993 May 29;306(6890):1440–1444. doi: 10.1136/bmj.306.6890.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadler N. M. Knee pain is the malady--not osteoarthritis. Ann Intern Med. 1992 Apr 1;116(7):598–599. doi: 10.7326/0003-4819-116-7-598. [DOI] [PubMed] [Google Scholar]
- Jenkinson C., Coulter A., Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ. 1993 May 29;306(6890):1437–1440. doi: 10.1136/bmj.306.6890.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johner R., Wruhs O. Classification of tibial shaft fractures and correlation with results after rigid internal fixation. Clin Orthop Relat Res. 1983 Sep;(178):7–25. [PubMed] [Google Scholar]
- Kettelkamp D. B., Hillberry B. M., Murrish D. E., Heck D. A. Degenerative arthritis of the knee secondary to fracture malunion. Clin Orthop Relat Res. 1988 Sep;(234):159–169. [PubMed] [Google Scholar]
- Kristensen K. D., Kiaer T., Blicher J. No arthrosis of the ankle 20 years after malaligned tibial-shaft fracture. Acta Orthop Scand. 1989 Apr;60(2):208–209. doi: 10.3109/17453678909149256. [DOI] [PubMed] [Google Scholar]
- McAlindon T. E., Cooper C., Kirwan J. R., Dieppe P. A. Knee pain and disability in the community. Br J Rheumatol. 1992 Mar;31(3):189–192. doi: 10.1093/rheumatology/31.3.189. [DOI] [PubMed] [Google Scholar]
- McKellop H. A., Sigholm G., Redfern F. C., Doyle B., Sarmiento A., Luck J. V., Sr The effect of simulated fracture-angulations of the tibia on cartilage pressures in the knee joint. J Bone Joint Surg Am. 1991 Oct;73(9):1382–1391. [PubMed] [Google Scholar]
- Merchant T. C., Dietz F. R. Long-term follow-up after fractures of the tibial and fibular shafts. J Bone Joint Surg Am. 1989 Apr;71(4):599–606. [PubMed] [Google Scholar]
- Oni O. O., Hui A., Gregg P. J. The healing of closed tibial shaft fractures. The natural history of union with closed treatment. J Bone Joint Surg Br. 1988 Nov;70(5):787–790. doi: 10.1302/0301-620X.70B5.3192581. [DOI] [PubMed] [Google Scholar]
- Puno R. M., Vaughan J. J., Stetten M. L., Johnson J. R. Long-term effects of tibial angular malunion on the knee and ankle joints. J Orthop Trauma. 1991;5(3):247–254. doi: 10.1097/00005131-199109000-00001. [DOI] [PubMed] [Google Scholar]
- Rüedi T., Webb J. K., Allgöwer M. Experience with the dynamic compression plate (DCP) in 418 recent fractures of the tibial shaft. Injury. 1976 May;7(4):252–257. doi: 10.1016/s0020-1383(75)80002-7. [DOI] [PubMed] [Google Scholar]


