Abstract
Gait speed is a simple, effective indicator of age-related disease and disability. We sought to examine the prevalence and trends of slow gait speed in older Americans. Our unweighted analytic sample included 12,427 adults aged ≥ 65 years from the 2006–2016 waves of the Health and Retirement Study. Gait speed was measured in participant residences. Persons with gait speed < 0.8 or <0.6 m/s were slow. Sample weights were used to generate nationally representative estimates. The overall estimated prevalence of slow gait speed with the <0.8 m/s cut-point was 48.6% (95% confidence interval (CI): 47.4–49.8) in the 2006–2008 waves yet was 45.7% (CI: 44.3–47.1) in the 2014–2016 waves, but this downward trend was not statistically significant (p = 0.06). The estimated prevalence of slowness with the <0.6 m/s cut-point was 21.3% (CI: 20.4–22.3) for the 2006–2008 waves, 18.5% (CI: 17.5–19.4) for the 2010–2012 waves, and 19.2% (CI: 18.2–20.2) for the 2014–2016 waves, but there were again no significant trends (p = 0.61). Our findings showed that the estimated prevalence of slow gait speed in older Americans is pronounced, and different cut-points largely inform how slowness is categorized. Continued surveillance of slowness over time will help guide screening for disablement and identify sub-populations at greatest risk for targeted interventions.
Keywords: geriatrics, physical functional performance, population surveillance, walking
1. Introduction
By the year 2030, nearly 20% of the global population will be aged 60 years or older, and by the year 2050, the number of persons aged at least 80 years will triple to about 426 million [1]. In the United States, the older American population is likewise projected to increase by approximately 113% by 2030 [2]. With nearly a quarter of disease burden attributed to the older adult population, there will be a similar elevation in healthcare costs associated with age-related morbidity and disability [3,4]. Moreover, older adults experience physical dysfunction, which contributes to a loss of mobility and a decrease in quality of life [5]. Declining mobility may increase fall risk and limit basic self-care [6,7]. These characteristics contribute to the medical-related economic implications of aging due to the increased need for physician care, treatments, and hospital stays [8]. For example, it is estimated the average cost for fall-related injuries, which are related to mobility, is $30,000 with subsequent increases in costs as age elevates [9]. Accordingly, examining mobility tasks in clinical and translational research settings may help to serve as an indicator of future age-related disease and disability. Such ongoing surveillance of mobility may better inform healthcare providers by presenting insights for earlier referral to interventions that are germane to restoring mobility.
Gait speed is a wide-spread mobility assessment that evaluates the time to comfortably walk across a pre-specified distance. Gait speed is also feasible and relatively inclusive, such that little to no expenses are necessary to complete gait speed assessments, and persons are effectively asked to walk a short distance. Examinations of gait speed are an important clinical marker that is widely used to assess physical function and mobility during aging [10]. Gait speed outcomes compared to other functional measurements can be used as both a reliable and valid indicator of overall health implications that may need healthcare intervention [11]. Criterion-referenced standards categorize gait speed measures, and persons identified as categorically slow have an increased risk for several health conditions such as cognitive impairment, functional disability, and early all-cause mortality [12]. Likewise, the presence of cardiometabolic disease, neurocognitive impairment, and difficulty performing activities of daily living limitations may be present prior to the administration of gait speed assessments, thereby suggesting a bidirectional association. Given that slow gait speed represents poor physical performance and a more advanced stage of the disablement process, monitoring gait speed may provide unique health insights during aging.
Previous investigations have shown that the proportions of persons that have slow gait speed may differ based on their characteristics. For example, Manjavong et al. [13] suggest that approximately 76% of older adults in an outpatient tertiary hospital setting were considered slow, while others revealed that about 56% of older adults residing in urban areas might be slow [14]. Despite the importance of monitoring gait speed, and how gait speed changes over time, the prevalence of older adults in the United States who might be considered slow is not well understood. Surveillance of gait speed may serve as a valuable screening tool for age-related disease and disability [15]. Additionally, the assessment of gait speed compared to other physical performance assessments is time-efficient and cost-effective [16]. Examining the prevalence of slow gait speed at a population level may provide insights into the presence of mobility impairments in Americans, inform interventions for restoring mobility, and guide healthcare policy for the quickly growing older demographic. We sought to evaluate the prevalence and trends of slow gait speed in older Americans from 2006–2016.
2. Materials and Methods
2.1. Participants
We performed a secondary analysis of data from the 2006–2016 waves of the Health and Retirement Study (HRS) [17]. The HRS utilizes a longitudinal panel design to examine health and economic factors in Americans as they age [18]. New cohorts of participants enter the HRS and are followed until death. Utilizing the HRS as a data source for this study provides multidisciplinary data for a national sample of Americans, including a multistage probability design, geographical stratification, and oversampling for certain demographic groups [19]. Sampling weights are provided by the HRS for generating nationally representative data.
Core interviews in the HRS occur in waves every 2 years and response rates have regularly been >80% [20]. Starting in the 2006 wave, the nationally representative face-to-face interviews included physical measures such as gait speed. These detailed interviews were performed at alternating waves with a random half-sample of HRS participants, while the other half-sample completed core interviews [21]. Accordingly, we merged these waves of the HRS to ensure that the random half-samples completing gait speed testing were evaluated uniformly. More details about the HRS are available elsewhere [22].
2.2. Measures
Interviewers created a walking course in an open and preferably non-carpeted area in participant residences. A strip of tape was secured on the floor to signify the beginning and end points of the walking course after interviewers measured the distance. Using a standardized protocol, participants were advised to walk at their normal pace across the 2.5 m course. Participants then aligned their toes at the start line, and when interviewers prompted participants to start, they walked across the course. Interviewers stopped timing when the participant’s foot was touching the floor past the finish line. After the first trial was completed, the same procedures were executed for the second trial [23,24]. Those with a recent surgery, injury, or other health condition that may have influenced walking may not have engaged in gait speed testing. Persons with gait speed < 0.8 or <0.6 m/s were considered slow [25,26]. These cut-points effectively dichotomize persons with mobility limitations and those without such limitations [26]. More details about the walking speed assessment in the HRS are available elsewhere [27]. Participants also told interviewers their age, gender, race, and ethnicity.
2.3. Statistical Analysis
All analyses were performed with SAS 9.4 software (SAS Institute; Cary, NC, USA). HRS analytic guidelines informed our analyses, such that we used the survey weights which accounted for the complex sampling design to generate nationally representative estimates in the PROC SURVEYFREQ procedure [19]. The descriptive characteristics were presented as unweighted mean ± standard deviation for continuous variables and frequency (percentage) for categorical variables to improve interpretability.
Prevalence estimates for slow gait speed using both the <0.8 and <0.6 m/s cut-points were shown as a weighted percentage and 95% confidence interval (CI). These prevalence estimates for both cut-points were displayed as overall, and then stratified by age group (young-old: 65–74 years, middle-old: 75–84 years, old-old: ≥85 years), gender (male, female), race and ethnicity (Hispanic, non-Hispanic Black, non-Hispanic Other, non-Hispanic White) for each combined HRS wave (2006–2008, 2010–2012, 2014–2016). Additionally, we calculated a percent difference in the prevalence estimates for the stratified findings using the 2006–2008 waves as the reference.
Individual multilevel logistic regression models analyzed trends in slow gait speed separately using the <0.8 m/s and <0.6 m/s cut-points with the survey weights included for overall slowness, age group, sex, race and ethnicity. Repeated measures of individual persons in multiple waves were modeled using a random intercept for each participant to account for the longitudinal design in the HRS. For each model, the binary response variable was slow gait speed. In the overall model, there was only a single explanatory variable for time (i.e., wave). An additional model adjusted for time, age group (reference: young-old), and the interaction between time and age group for evaluating trends by age group. Furthermore, a model adjusted for time, sex (reference: female), and a time-by-sex interaction quantified trends by sex. Another model included explanatory variables for time, race and ethnicity (reference: non-Hispanic White), and the interaction. An alpha level of 0.05 was utilized for all analyses.
3. Results
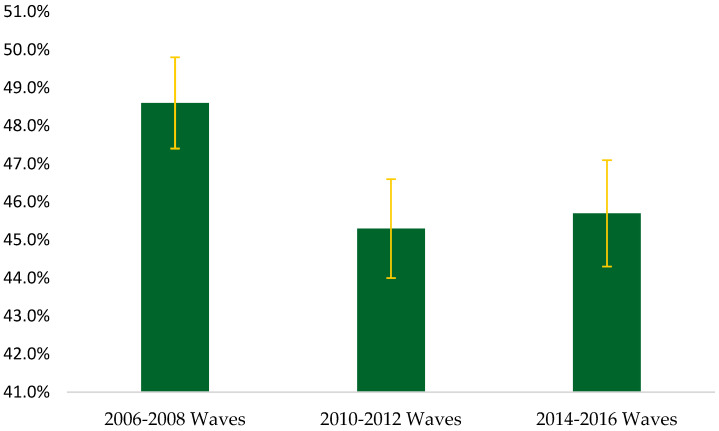
Table 1 shows the unweighted baseline descriptive characteristics of the 12,427 participants. Overall, persons were aged 72.7 ± 6.9 years and were mostly female (57.3%). Walking speed was 3.3 ± 1.7 s for young-old, 4.0 ± 2.7 s for middle-old, 5.0 s for old-old, 4.1 ± 3.3 s for Hispanic, 4.3 ± 2.5 s for non-Hispanic Black, 3.6 ± 2.6 s for non-Hispanic Other, 3.4 ± 1.8 s for non-Hispanic White, 3.8 ± 2.4 s for females, 3.3 ± 1.8 s for males. Figure 1 presents the overall prevalence of slow gait speed using a <0.8 m/s cut-point. The estimated prevalence of slow gait speed was 48.6% (CI: 47.4, 49.8), 45.3% (CI: 44.0, 46.6), and 45.7% (CI: 44.3, 47.1) in the 2006–2008, 2010–2012, and 2014–2016 waves, respectively. However, no significant trends in gait speed were observed over time (p = 0.06).
Table 1.
Unweighted descriptive characteristics of the participants.
| Overall (n = 12,427) | |
|---|---|
| Age (years) | 72.7 ± 6.9 |
| Age Category (n (%)) | |
| Young-Old (n (%)) | 8214 (66.1) |
| Middle-Old (n (%)) | 3258 (26.2) |
| Old-Old (n (%)) | 955 (7.7) |
| Sex (n (%)) | |
| Male (n (%)) | 5301 (42.7) |
| Female (n (%)) | 7126 (57.3) |
| Race and Ethnicity (n (%)) | |
| Hispanic | 1120 (9.0) |
| Non-Hispanic Black | 1648 (13.3) |
| Non-Hispanic Other | 270 (2.1) |
| Non-Hispanic White | 9389 (75.6) |
| Health Conditions | 2.3 ± 1.4 |
| Walk Speed (seconds) | 3.6 ± 2.1 |
Note: Health conditions included a count of self-reported healthcare-provider-diagnosed hypertension, diabetes, cancer, lung disease, heart disease, stroke, psychiatric problems, and arthritis (n = 12,426).
Figure 1.
Overall estimated prevalence of slowness using a <0.8 m per second cut-point.
The estimated prevalence of slow gait speed by demographic characteristics using the <0.8 m/s cut-point is displayed in Table 2. The highest estimated prevalence of slow gait speed was 36.5% (CI: 35.0, 38.1) for the young-old group, 59.1% (CI: 57.1, 61.1) for the middle-old group in the 2006–2008 waves, and 79.1% (CI: 76.3, 81.9) for the old-old group in the 2014–2016 waves. Compared to those in the young-old age group, persons in the middle-old (p < 0.001) and old-old groups (p < 0.001) had a higher prevalence of slow gait speed. When examining the prevalence estimates by race and ethnicity using the <0.8 m/s cut-point, the estimated prevalence of slow gait speed in the most recent waves (2014–2016) was 64.2% (CI: 59.4, 69.0) for Hispanic, 73.1% (CI: 69.5, 76.6) for non-Hispanic Black, 46.4% (CI: 37.6, 55.1) for non-Hispanic Other, and 41.7% (CI: 40.2, 43.2) for non-Hispanic White. Compared to non-Hispanic White, Hispanic (p < 0.001) and non-Hispanic Black (p < 0.001) had a higher prevalence of slow gait speed. The highest estimated prevalence of slow gait speed using the <0.8 m/s cut-point was 54.0% (CI: 52.4, 55.6) for females in the 2006–2008 waves and 41.3% (CI: 39.5, 43.1) for males in the 2006–2008 waves. Males had a lower slow gait speed prevalence relative to females (p < 0.001). Table 3 presents the results for the slow gait speed trends analyses with the <0.8 m/s cut-point.
Table 2.
Estimated prevalence of slowness by demographic characteristics using a <0.8 m per second cut-point.
| Variable | Weighted Frequency | Weighted Prevalence (%) | 95% Confidence Interval | ∆% † |
|---|---|---|---|---|
| Age Group | ||||
| Young-Old | ||||
| 2006–2008 Waves | 5,403,022 | 36.5 | 35.0, 38.1 | - |
| 2010–2012 Waves | 5,880,135 | 34.5 | 32.7, 36.2 | −2.0 |
| 2014–2016 Waves | 7,384,681 | 35.1 | 33.2, 37.0 | −1.4 |
| Middle-Old | ||||
| 2006–2008 Waves | 5,539,249 | 59.1 | 57.1, 61.1 | - |
| 2010–2012 Waves | 5,398,282 | 53.7 | 51.7, 55.6 | −5.4 |
| 2014–2016 Waves | 5,707,398 | 54.9 | 52.9, 56.9 | −4.2 |
| Old-Old | ||||
| 2006–2008 Waves | 2,221,729 | 76.1 | 72.8, 79.4 | - |
| 2010–2012 Waves | 2,519,977 | 74.8 | 71.6, 77.9 | −1.3 |
| 2014–2016 Waves | 3,047,428 | 79.1 | 76.3, 81.9 | 3.0 |
| Race & Ethnicity | ||||
| Hispanic | ||||
| 2006–2008 Waves | 1,061,208 | 63.6 | 59.2, 68.1 | - |
| 2010–2012 Waves | 1,028,953 | 57.7 | 52.3, 63.1 | −5.9 |
| 2014–2016 Waves | 1,560,875 | 64.2 | 59.4, 69.0 | 0.6 |
| Non-Hispanic Black | ||||
| 2006–2008 Waves | 1,304,420 | 69.4 | 65.9, 72.8 | - |
| 2010–2012 Waves | 1,654,638 | 74.5 | 71.2, 77.8 | 5.1 |
| 2014–2016 Waves | 1,890,268 | 73.1 | 69.5, 76.6 | 3.7 |
| Non-Hispanic Other | ||||
| 2006–2008 Waves | 255,375 | 51.7 | 41.9, 61.5 | - |
| 2010–2012 Waves | 296,928 | 45.5 | 36.3, 54.7 | −6.2 |
| 2014–2016 Waves | 437,165 | 46.4 | 37.6, 55.1 | −5.3 |
| Non-Hispanic White | ||||
| 2006–2008 Waves | 10,542,997 | 45.8 | 44.5, 47.1 | - |
| 2010–2012 Waves | 10,817,875 | 41.9 | 40.5, 43.3 | −3.9 |
| 2014–2016 Waves | 12,251,199 | 41.7 | 40.2, 43.2 | −4.1 |
| Gender | ||||
| Females | ||||
| 2006–2008 Waves | 8,402,444 | 54.0 | 52.4, 55.6 | - |
| 2010–2012 Waves | 8,732,664 | 51.2 | 49.5, 52.9 | −2.8 |
| 2014–2016 Waves | 10,002,946 | 51.2 | 49.4, 53.0 | −2.8 |
| Males | ||||
| 2006–2008 Waves | 4,761,556 | 41.3 | 39.5, 43.1 | - |
| 2010–2012 Waves | 5,065,730 | 37.7 | 35.8, 39.7 | −3.6 |
| 2014–2016 Waves | 6,136,561 | 38.9 | 36.9, 41.0 | −2.4 |
† 2006–2008 waves were the reference.
Table 3.
Results for the slow gait speed trends analyses with the <0.8 m per second cut-point.
| Estimate | 95% Confidence Interval |
p-Value | |
|---|---|---|---|
| Overall Model | |||
| Intercept | −0.40 | −0.80, −0.01 | 0.04 |
| Wave | 0.18 | −0.01, 0.36 | 0.06 |
| Model 1 | |||
| Intercept | −0.45 | −0.54, −0.35 | <0.001 |
| Wave | 0.01 | −0.04, 0.06 | 0.65 |
| Middle-Old | 0.77 | 0.62, 0.92 | <0.001 |
| Old-Old | 1.66 | 1.42, 1.89 | <0.001 |
| Wave*Middle-Old | −0.03 | −0.10, 0.04 | 0.44 |
| Wave*Old-Old | −0.02 | −0.12, 0.09 | 0.71 |
| Model 2 | |||
| Intercept | 0.87 | 0.36, 1.39 | <0.001 |
| Wave | 0.13 | −0.11, 0.37 | 0.28 |
| Male | −2.90 | −3.70, −2.20 | <0.001 |
| Wave*Male | 0.08 | −0.29, 0.45 | 0.69 |
| Model 3 | |||
| Intercept | −1.20 | −1.60, −0.76 | <0.001 |
| Wave | 0.03 | −0.18, 0.24 | 0.79 |
| Hispanic | 4.23 | 2.77, 5.69 | <0.001 |
| Non-Hispanic Black | 5.36 | 4.13, 6.60 | <0.001 |
| Non-Hispanic Other | 0.78 | −2.20, 3.71 | 0.60 |
| Wave*Hispanic | −0.02 | −0.68, 0.64 | 0.94 |
| Wave*Non-Hispanic Black | 0.40 | −0.17, 0.97 | 0.16 |
| Wave*Non-Hispanic Other | 0.08 | −1.20, 1.38 | 0.90 |
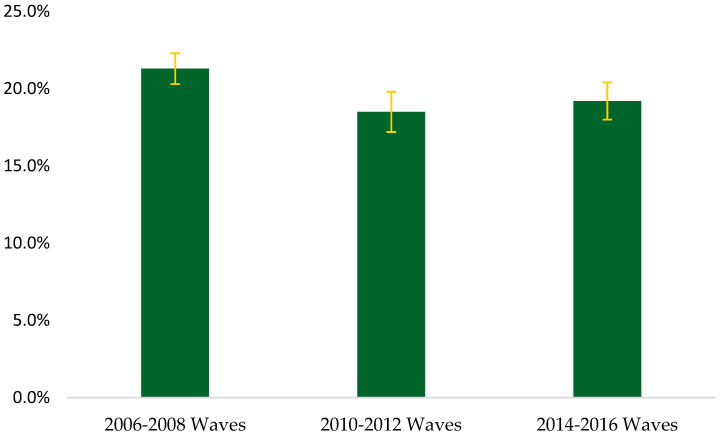
Figure 2 displays the overall estimated prevalence of slowness using a <0.6 m/s cut-point. The estimated prevalence of slow gait speed was 21.3% (CI: 20.4, 22.3) for the 2006–2008 waves, 18.5% (CI: 17.5, 19.4) for the 2010–2012 waves, and 19.2% (CI: 18.2, 20.2) for the 2014–2016 waves, but no significant trends were observed (p = 0.61). Table 4 presents the estimated prevalence of slow gait speed by demographic characteristics using a <0.6 m/s cut-point. Similar to the <0.8 m/s cut-point, the highest estimated prevalence of slowness with the <0.6 m/s was 13.5% (CI: 12.4, 14.6) for the young-old group, 26.7% (CI: 24.9, 28.5) for the middle-old group in the 2006–2008 waves, and 50.3% (CI: 46.8, 53.9) for the old-old group in the 2014–2016 waves. Compared to those in the young-old group, persons in the middle-old (p < 0.001) and old-old groups (p < 0.001) had a higher prevalence of slow gait speed. When evaluating the prevalence estimates by race and ethnicity using the <0.6 m/s cut-point, the estimated prevalence of slow gait speed in the 2014–2016 waves (most recent) was 30.4% (CI: 25.9, 34.9) for Hispanic, 37.8% (CI: 33.8, 41.7) for non-Hispanic Black, 22.2% (CI: 15.0, 29.4) for non-Hispanic Other, and 16.5% (CI: 15.5, 17.6) for non-Hispanic White. Relative to non-Hispanic White, Hispanic (p < 0.001) and non-Hispanic Black (p < 0.001) had a higher prevalence of slow gait speed. The highest estimated prevalence of slow gait speed was 25.5% (CI: 24.1, 26.9) for females and 15.7% (CI: 14.4, 17.0) for males, both in the 2006–2008 waves with the <0.6 m/s cut-point. Males had a lower gait speed prevalence compared to females (p < 0.001). The results for the slow gait speed trends analyses with the <0.6 m/s cut-point are shown in Table 5.
Figure 2.
Overall estimated prevalence of slowness using a <0.6 m per second cut-point.
Table 4.
Prevalence estimates of slow gait speed by demographic characteristics using a <0.6 m per second cut-point.
| Variable | Weighted Frequency | Weighted Prevalence (%) | 95% Confidence Interval | ∆% † |
|---|---|---|---|---|
| Age Group | ||||
| Young-Old | ||||
| 2006–2008 Waves | 2,000,914 | 13.5 | 12.4, 14.6 | |
| 2010–2012 Waves | 1,848,315 | 10.8 | 9.7, 11.9 | −2.7 |
| 2014–2016 Waves | 2,342,180 | 11.1 | 9.9, 12.3 | −2.4 |
| Middle-Old | ||||
| 2006–2008 Waves | 2,500,642 | 26.7 | 24.9, 28.5 | |
| 2010–2012 Waves | 2,312,662 | 23.0 | 21.3, 24.6 | −3.7 |
| 2014–2016 Waves | 2,500,728 | 24.0 | 22.3, 25.7 | −2.7 |
| Old-Old | ||||
| 2006–2008 Waves | 1,280,654 | 43.9 | 40.1, 47.6 | |
| 2010–2012 Waves | 1,478,506 | 43.8 | 40.1, 47.5 | −0.1 |
| 2014–2016 Waves | 1,940,661 | 50.3 | 46.8, 53.9 | 6.4 |
| Race & Ethnicity | ||||
| Hispanic | ||||
| 2006–2008 Waves | 569,762 | 34.1 | 30.0, 38.3 | |
| 2010–2012 Waves | 503,120 | 28.2 | 23.3, 33.1 | −5.9 |
| 2014–2016 Waves | 739,686 | 30.4 | 25.9, 34.9 | −3.7 |
| Non-Hispanic Black | ||||
| 2006–2008 Waves | 725,509 | 38.6 | 34.9, 42.2 | - |
| 2010–2012 Waves | 829,684 | 37.3 | 33.6, 41.0 | −1.3 |
| 2014–2016 Waves | 978,070 | 37.8 | 33.8, 41.7 | −0.8 |
| Non-Hispanic Other | ||||
| 2006–2008 Waves | 112,414 | 22.7 | 13.9, 31.5 | - |
| 2010–2012 Waves | 142,702 | 21.8 | 13.8, 29.9 | −0.9 |
| 2014–2016 Waves | 209,409 | 22.2 | 15.0, 29.4 | −0.5 |
| Non-Hispanic White | ||||
| 2006–2008 Waves | 4,374,525 | 19.0 | 17.9, 20.0 | - |
| 2010–2012 Waves | 4,163,977 | 16.1 | 15.1, 17.1 | −2.9 |
| 2014–2016 Waves | 4,856,404 | 16.5 | 15.5, 17.6 | −2.5 |
| Gender | ||||
| Females | ||||
| 2006–2008 Waves | 3,969,203 | 25.5 | 24.1, 26.9 | - |
| 2010–2012 Waves | 3,839,996 | 22.5 | 21.1, 23.9 | −3.0 |
| 2014–2016 Waves | 4,446,626 | 22.7 | 21.3, 24.2 | −2.8 |
| Males | ||||
| 2006–2008 Waves | 1,813,007 | 15.7 | 14.4, 17.0 | - |
| 2010–2012 Waves | 1,799,487 | 13.4 | 12.1, 14.7 | −2.3 |
| 2014–2016 Waves | 2,336,943 | 14.8 | 13.4, 16.2 | −0.9 |
† 2006–2008 waves were the reference.
Table 5.
Results for the slow gait speed trends analyses with the <0.6 m per second cut-point.
| Estimate | 95% Confidence Interval |
p-Value | |
|---|---|---|---|
| Overall Model | |||
| Intercept | −6.6 | −7.0, −6.3 | <0.001 |
| Wave | 0.04 | −0.12, 0.20 | 0.61 |
| Model 1 | |||
| Intercept | −1.7 | −1.9, −1.6 | <0.001 |
| Wave | −0.03 | −0.09, 0.02 | 0.25 |
| Middle-Old | 0.69 | 0.50, 0.88 | <0.001 |
| Old-Old | 1.54 | 1.24, 1.83 | <0.001 |
| Wave*Middle-Old | 0.02 | −0.07, 0.11 | 0.63 |
| Wave*Old-Old | 0.06 | −0.07, 0.20 | 0.37 |
| Model 2 | |||
| Intercept | −5.6 | −6.0, −5.1 | <0.001 |
| Wave | −0.05 | −0.25, 0.16 | 0.66 |
| Male | −2.6 | −3.3, −1.9 | <0.001 |
| Wave*Male | 0.19 | −0.14, 0.52 | 0.25 |
| Model 3 | |||
| Intercept | −7.5 | −7.8, −7.1 | <0.001 |
| Wave | −0.03 | −0.21, 0.16 | 0.77 |
| Hispanic | 4.00 | 2.75, 5.26 | <0.001 |
| Non-Hispanic Black | 5.19 | 4.14, 6.23 | <0.001 |
| Non-Hispanic Other | 0.45 | −2.10, 3.04 | 0.73 |
| Wave*Hispanic | −0.19 | −0.75, 0.38 | 0.51 |
| Wave*Non-Hispanic Black | −0.09 | −0.57, 0.39 | 0.72 |
| Wave*Non-Hispanic Other | 0.36 | −0.79, 1.51 | 0.53 |
4. Discussion
Our results indicate that the estimated prevalence of slow gait speed in American adults aged at least 65 years nearly peaked at 49% when using the <0.8 m/s cut-point and was over 20% when utilizing the <0.6 m/s threshold from the 2006–2016 HRS population waves. The estimated prevalence of older adults with slow gait speed overall had no significant trend, and the estimated prevalence of slow gait speed was greatest in old-old adults and females, regardless of cut-point used. Moreover, persons identifying as Hispanic and non-Hispanic Black had an especially high estimated prevalence of slow gait speed. Our findings provide insights into the presence of slow gait speed among older adults in the United States, and how slow gait speed might be present in specific populations. The assessment of slow gait speed presents opportunities for improvement but remains a simple and inexpensive screening method for functional disability during aging.
The overall prevalence of slow gait speed in older adults has decreased from the 2006–2008 waves to the 2014–2016 waves, although these findings were not statistically significant. Not controlling for age-related morbidities and disabilities may have informed our prevalence estimates, and additional waves of HRS data may have yielded greater insights in this regard. Impairments in mobility tend to increase with age, and thus, it was not surprising that our findings indicated an elevation in gait speed prevalence with the advancing age group. For example, the older adult population aged 85 years and older generally displayed a greater prevalence of slow gait speed compared to young-old and middle-old adults. These findings can be attributed to physiological age-related declines such as frailty and cognitive impairment, and serve as a potential precursor to morbidities and mortality [28].
Gender may inform differences in gait speed, with women having a greater prevalence in slowness compared to men. This finding could be due to higher rates of osteoporosis in women than in men, wherein mobility and balance are potentially reduced, and fear of falling may be greater due to bone and joint frailty [29,30]. Furthermore, sarcopenia linked to menopausal hormonal deficiencies in estrogen presents adverse impacts related to musculoskeletal function in daily activities such as walking [31]. A higher proportion of women with obesity compared to men can further reduce mobility [32], and height differences between females and males is important to note for how stature may have influenced walking speed [33,34]. These findings pose health implications, suggesting women are a target group for the prevention and treatment of slow gait speed. Exercise and physical activity has shown promise to be an effective treatment in slowing the process of muscle loss, and pharmaceutical therapies such as the use of myostatin inhibitors can be utilized as an additional form of treatment [35].
Race and ethnicity were also factors, as there were high prevalence estimates for slow gait speed prevalence for Hispanic and non-Hispanic Black. These differences may be attributable to health disparities and the presence of other morbid conditions such as obesity, which in turn, may lead to dynapenia, joint pain, and instability during aging [36,37,38]. Furthermore, race and ethnicity factors and socioeconomic status can affect access to quality healthcare and treatment, thereby leading to an accelerated rate of aging [39]. Such implications for slow gait speed can be used as a predictive healthcare method for potential cognitive impairment, functional disability, and premature mortality, which can help inform the need for interventions [40]. Overall, interventions largely consist of resistance, aerobic, flexibility, and ambulation training in addition to task-oriented motor learning exercises. Moreover, community-based interventions could be useful for focusing on self-efficacy and care [41,42]. Due to its cost- and time-effectivity, the administration of gait speed as a preventative and diagnostic tool in healthcare settings is particularly useful.
Some limitations should be noted. Standardization in residence settings of participants was not controlled for such as carpet or hard flooring where gait speed was performed. Additionally, the footwear of participants was not similar, which has the capacity to induce biomechanical impacts on gait [43]. The HRS utilized a 2.5 m distance for ascertaining walking speed, but other distances and protocols may have influenced the findings [44]. Because these gait speed data were collected from 2006–2016, there is a possibility that select participants did not subsequently continue gait speed measurements due to morbidities, movement in care facilities, and death, which may have implications on our findings. Despite these limitations, our investigation revealed slow gait speed estimates amongst older Americans and vulnerable populations who are a target for prevention and intervention. We recommend gait speed continues to be monitored alongside other cognitive and physical (e.g., handgrip strength) indicators as the older adult population increases to help inform the need for intervention.
5. Conclusions
The overall estimated prevalence of slow gait speed in Americans aged at least 65 years peaked at approximately 49% when using the <0.8 m/s cut-point and was >20% when categorizing slowness with the <0.6 m/s cut-point for the 2006–2016 HRS populations waves. The prevalence estimates of older adults who displayed slowness generally increased from the young-old age category to the old-old age category. Females and non-Hispanic Black had higher slow gait speed prevalence estimates, which present target populations for potential healthcare intervention. Examining gait speed remains a simple screening method for age-related disease and disability, and using different cut-points will inform how persons are categorized as slow. As the older American population continues increasing, health conditions that are germane to this age demographic will likewise elevate. Therefore, gait speed assessments could be a valuable screening tool for guiding healthcare providers and relevant policies in helping older Americans live longer with independence.
Author Contributions
Conceptualization, R.M.; methodology, R.M.; formal analysis, R.M.; writing—original draft preparation, E.S. and R.M.; writing—review and editing, S.A., J.B., M.B., C.C., S.F., T.H. and J.N.; supervision, R.M.; funding acquisition, R.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data utilized in this investigation are publicly available from the Health and Retirement Study website.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R15AG072348 (to R.M.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.World Health Organization Ageing and Health Available. [(accessed on 8 August 2023)]. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
- 2.Colby S., Ortman J. Projections of the Size and Composition of the U.S. Population: 2014 to 2060; Population Estimates and Projections. [(accessed on 8 August 2023)]; Available online: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf.
- 3.Promoting Health for Older Adults. Centers for Disease Control and Prevention. [(accessed on 8 August 2023)]; Available online: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/promoting-health-for-older-adults.htm.
- 4.Prince M.J., Wu F., Guo Y., Gutierrez Robledo L.M., O’Donnell M., Sullivan R., Yusuf S. The Burden of Disease in Older People and Implications for Health Policy and Practice. Lancet. 2015;385:549–562. doi: 10.1016/S0140-6736(14)61347-7. [DOI] [PubMed] [Google Scholar]
- 5.Roberts S., Colombier P., Sowman A., Mennan C., Rölfing J.H.D., Guicheux J., Edwards J.R. Ageing in the Musculoskeletal System. Acta Orthop. 2016;87:15–25. doi: 10.1080/17453674.2016.1244750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berg R.L., Cassells J.S. The Second Fifty Years: Promoting Health and Preventing Disability. National Academies Press (US); Washington, DC, USA: 1992. [(accessed on 8 August 2023)]. Falls in Older Persons: Risk Factors and Prevention. Available online: https://www.ncbi.nlm.nih.gov/books/NBK235613/ [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention Resource Algorithm for Fall Risk Screening, Assessment, and Intervention. [(accessed on 8 August 2023)]; Available online: https://www.cdc.gov/steadi/pdf/STEADI-Algorithm-508.pdf.
- 8.Newman P., Juliette C., Damico A. Medicare per Capita Spending by Age and Service: New Data Highlights Oldest Beneficiaries. Health Aff. 2015;34:335–339. doi: 10.1377/hlthaff.2014.1371. [DOI] [PubMed] [Google Scholar]
- 9.Florence C.S., Bergen G., Atherly A., Burns E., Stevens J., Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J. Am. Geriatr. Soc. 2018;66:693–698. doi: 10.1111/jgs.15304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehmet H., Robinson S.R., Yang A.W.H. Assessment of Gait Speed in Older Adults. J. Geriatr. Phys. Ther. 2020;43:42. doi: 10.1519/JPT.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 11.Studenski S., Perera S., Patel K., Rosano C., Faulkner K., Inzitari M., Brach J., Chandler J., Cawthon P., Connor E.B., et al. Gait Speed and Survival in Older Adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park H., Aul C., DeGutis J., Lo O.-Y., Poole V.N., McGlinchey R., Bean J.F., Leritz E., Esterman M. Evidence for a Specific Association between Sustained Attention and Gait Speed in Middle-to-Older-Aged Adults. Front. Aging Neurosci. 2021;13:326. doi: 10.3389/fnagi.2021.703434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manjavong M., So-Ngern A., Limpawattana P., Kamsuanjig T., Manomaiwong N., Chokkhatiwat P., Srisuwannakit K., Khammak C. Prevalence and Factors Influencing Slow Gait Speed among Geriatric Patients at Outpatient Clinic of a Tertiary Care Hospital. Ir. J. Med. Sci. 2023:1–7. doi: 10.1007/s11845-023-03364-z. [DOI] [PubMed] [Google Scholar]
- 14.Castell M.-V., Sánchez M., Julián R., Queipo R., Martín S., Otero Á. Frailty Prevalence and Slow Walking Speed in Persons Age 65 and Older: Implications for Primary Care. BMC Fam. Pract. 2013;14:86. doi: 10.1186/1471-2296-14-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pinter D., Ritchie S.J., Gattringer T., Bastin M.E., Hernández M.D.C.V., Corley J., Maniega S.M., Pattie A., Dickie D.A., Gow A.J., et al. Predictors of Gait Speed and Its Change over Three Years in Community-Dwelling Older People. Aging. 2018;10:144–153. doi: 10.18632/aging.101365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beaudart C., Rolland Y., Cruz-Jentoft A.J., Bauer J.M., Sieber C., Cooper C., Al-Daghri N., Carvalho I., Bautmans I., Bernabei R., et al. Assessment of Muscle Function and Physical Performance in Daily Clinical Practice: A Position Paper Endorsed by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) Calcif. Tissue Int. 2019;105:1–14. doi: 10.1007/s00223-019-00545-w. [DOI] [PubMed] [Google Scholar]
- 17.Health and Retirement Study. HRS Data Products. [(accessed on 8 August 2023)]. Available online: https://hrs.isr.umich.edu/data-products.
- 18.Sonnega A., Faul J.D., Ofstedal M.B., Langa K.M., Phillips J.W.R., Weir D.R. Cohort Profile: The Health and Retirement Study (HRS) Int. J. Epidemiol. 2014;43:576–585. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Health and Retirement Study. HRS Survey Design and Methodology. [(accessed on 8 August 2023)]. Available online: https://hrs.isr.umich.edu/documentation/survey-design.
- 20.Health and Retirement Study. Sample Sizes and Response Rates. [(accessed on 3 August 2023)]. Available online: https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf.
- 21.Fisher G.G., Ryan L.H. Overview of the Health and Retirement Study and Introduction to the Special Issue. Work Aging Retire. 2018;4:1–9. doi: 10.1093/workar/wax032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Health and Retirement Study. HRS Data Book. [(accessed on 8 August 2023)]. Available online: https://hrs.isr.umich.edu/about/data-book.
- 23.McGrath R., Lang J.J., Ortega F.B., Chaput J.-P., Zhang K., Smith J., Vincent B., Piñero J.C., Garcia M.C., Tomkinson G.R. Handgrip Strength Asymmetry Is Associated with Slow Gait Speed and Poorer Standing Balance in Older Americans. Arch. Gerontol. Geriatr. 2022;102:104716. doi: 10.1016/j.archger.2022.104716. [DOI] [PubMed] [Google Scholar]
- 24.McGrath B.M., Johnson P.J., McGrath R., Cawthon P.M., Klawitter L., Choi B.-J. A Matched Cohort Analysis for Examining the Association between Slow Gait Speed and Shortened Longevity in Older Americans. J. Appl. Gerontol. 2022;41:1905–1913. doi: 10.1177/07334648221092399. [DOI] [PubMed] [Google Scholar]
- 25.Cawthon P.M., Manini T., Patel S.M., Newman A., Travison T., Kiel D.P., Santanasto A.J., Ensrud K.E., Xue Q.-L., Shardell M., et al. Putative Cut-Points in Sarcopenia Components and Incident Adverse Health Outcomes: An SDOC Analysis. J. Am. Geriatr. Soc. 2020;68:1429–1437. doi: 10.1111/jgs.16517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cawthon P.M., Patel S.M., Kritchevsky S.B., Newman A.B., Santanasto A., Kiel D.P., Travison T.G., Lane N., Cummings S.R., Orwoll E.S., et al. What Cut-Point in Gait Speed Best Discriminates Community-Dwelling Older Adults with Mobility Complaints from Those without? A Pooled Analysis from the Sarcopenia Definitions and Outcomes Consortium. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:e321–e327. doi: 10.1093/gerona/glab183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crimmins E., Guyer H., Langa K., Ofstedal M.B., Wallace R. Documentation of Physical Measures, Anthropometrics and Blood Pressure in the Health and Retirement Study. [(accessed on 8 August 2023)]. Available online: https://hrs.isr.umich.edu/sites/default/files/biblio/dr-011.pdf.
- 28.Afilalo J., Kim S., O’Brien S., Brennan J.M., Edwards F.H., Mack M.J., McClurken J.B., Cleveland J.C., Smith P.K., Shahian D.M., et al. Gait Speed and Operative Mortality in Older Adults following Cardiac Surgery. JAMA Cardiol. 2016;1:314–321. doi: 10.1001/jamacardio.2016.0316. [DOI] [PubMed] [Google Scholar]
- 29.Salari N., Ghasemi H., Mohammadi L., Rabieenia E., Shohaimi S., Mohammadi M. The Global Prevalence of Osteoporosis in the World: A Comprehensive Systematic Review and Meta-Analysis. J. Orthop. Surg. Res. 2021;16:609. doi: 10.1186/s13018-021-02772-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rolland Y., Cesari M., Fielding R.A., Reginster J.Y., Vellas B., Cruz-Jentoft A.J. The ICFSR Task Force Osteoporosis in Frail Older Adults: Recommendations for Research from the ICFSR Task Force 2020. J. Frailty Aging. 2021;10:168–175. doi: 10.14283/jfa.2021.4. [DOI] [PubMed] [Google Scholar]
- 31.Khadilkar S.S. Musculoskeletal Disorders and Menopause. J. Obstet. Gynaecol. India. 2019;69:99–103. doi: 10.1007/s13224-019-01213-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muhammad T., Boro B., Kumar M., Srivastava S. Gender Differences in the Association of Obesity-Related Measures with Multi-Morbidity among Older Adults in India: Evidence from LASI, Wave-1. BMC Geriatr. 2022;22:171. doi: 10.1186/s12877-022-02869-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roser M., Appel C., Ritchie H. Human Height. [(accessed on 1 September 2023)]. Available online: https://ourworldindata.org/human-height.
- 34.Wolff C., Steinheimer P., Warmerdam E., Dahmen T., Slusallek P., Schlinkmann C., Chen F., Orth M., Pohlemann T., Ganse B. Effects of Age, Body Height, Body Weight, Body Mass Index and Handgrip Strength on the Trajectory of the Plantar Pressure Stance-Phase Curve of the Gait Cycle. Front. Bioeng. Biotechnol. 2023;11:1110099. doi: 10.3389/fbioe.2023.1110099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.White T.A., LeBrasseur N.K. Myostatin and Sarcopenia: Opportunities and Challenges-A Mini Review. Gerontology. 2014;60:289–293. doi: 10.1159/000356740. [DOI] [PubMed] [Google Scholar]
- 36.Gonzalez M., Gates D.H., Rosenblatt N.J. The Impact of Obesity on Gait Stability in Older Adults. J. Biomech. 2020;100:109585. doi: 10.1016/j.jbiomech.2019.109585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention Adult Obesity Facts. [(accessed on 8 August 2023)]; Available online: https://www.cdc.gov/obesity/data/adult.html.
- 38.Centers for Disease Control and Prevention Obesity, Race/Ethnicity, and COVID-19. [(accessed on 8 August 2023)]; Available online: https://www.cdc.gov/obesity/data/obesity-and-covid-19.html.
- 39.How Discrimination in Health Care Affects Older Americans, and What Health Systems and Providers Can Do? [(accessed on 29 August 2023)]. Available online: https://www.commonwealthfund.org/publications/issue-briefs/2022/apr/how-discrimination-in-health-care-affects-older-americans.
- 40.Perera S., Patel K.V., Rosano C., Rubin S.M., Satterfield S., Harris T., Ensrud K., Orwoll E., Lee C.G., Chandler J.M., et al. Gait Speed Predicts Incident Disability: A Pooled Analysis. J. Gerontol. A Biol. Sci. Med. Sci. 2016;71:63–71. doi: 10.1093/gerona/glv126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brach J.S., VanSwearingen J.M. Interventions to Improve Walking in Older Adults. Curr. Transl. Geriatr. Exp. Gerontol. Rep. 2013;2:230–238. doi: 10.1007/s13670-013-0059-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wong A.K.C., Wong F.K.Y., Wong M.C.S., Chow K.K.S., Kwan D.K.S., Lau D.Y.S. A Community-Based Health–Social Partnership Program for Community-Dwelling Older Adults: A Hybrid Effectiveness–Implementation Pilot Study. BMC Geriatr. 2022;22:789. doi: 10.1186/s12877-022-03463-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moisan G., Descarreaux M., Cantin V. The Influence of Footwear on Walking Biomechanics in Individuals with Chronic Ankle Instability. PLoS ONE. 2020;15:e0239621. doi: 10.1371/journal.pone.0239621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boulifard D.A., Ayers E., Verghese J. Home Based Gait Speed Assessment: Normative Data and Racial/Ethnic Correlates Among Older Adults. J. Am. Med. Dir. Assoc. 2019;20:1224–1229. doi: 10.1016/j.jamda.2019.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data utilized in this investigation are publicly available from the Health and Retirement Study website.