Abstract
Context:
The risk factors for anterior cruciate ligament (ACL) tear for athletes participating in pivoting sports includes young age and female sex. A previous meta-analysis has reported a reinjury rate of 15% after ACL reconstruction (ACLR) for athletes across all sports. To the best of the authors’ knowledge, this is the first systematic review and meta-analysis of available literature reporting outcomes after ACLR in soccer players.
Objective:
To review and aggregate soccer-specific outcomes data after ACLR found in current literature to help guide a more tailored discussion regarding expectations and prognosis for soccer players seeking operative management of ACL injuries.
Data Sources:
A comprehensive search of publications was performed using PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and SPORTDiscus databases.
Study Selection:
Inclusion criteria consisted of original studies, level of evidence 1 to 4, studies reporting clinical and patient-reported outcomes (PROs) after primary ACLR in soccer players at all follow-up length.
Study Design:
The primary outcomes of interest were graft failure/reoperation rates, ACL injury in contralateral knee, return to soccer time, and PROs.
Level of Evidence:
Level 4.
Data Extraction:
Search of literature yielded 32 studies for inclusion that involved 3112 soccer players after ACLR.
Results:
The overall graft failure/reoperation rate ranged between 3.0% and 24.8% (mean follow-up range, 2.3-10 years) and the combined ACL graft failure and contralateral ACL injury rate after initial ACLR was 1.0% to 16.7% (mean follow-up range, 3-10 years); a subgroup analysis for female and male players revealed a secondary ACL injury incidence rate of 27%, 95% CI (22%, 32%) and 10%, 95% CI (6%, 15%), respectively. Soccer players were able to return to play between 6.1 and 11.1 months and the majority of PROs showed favorable scores at medium-term follow-up.
Conclusion:
Soccer players experience high ACL injury rates after primary ACLR and demonstrated similar reinjury rates as found in previous literature of athletes who participate in high-demand pivoting sports.
Keywords: anterior cruciate ligament reconstruction, football, futbol, outcomes, return to sport, soccer
The anterior cruciate ligament (ACL) is a critical knee stabilizer that resists anterior and rotation forces of the tibia relative to the femur. As a result, it is the knee ligament that is commonly injured during sporting activities.13,37,56 Left untreated, athletes will experience recurrent instability, and the literature supports evidence of increased risk of chondral and meniscal injuries and early development of knee osteoarthritis.41,51,79 The current gold standard treatment for high-level athletes is ACL reconstruction (ACLR), with the goal of restoring function and achieving preinjury level of activity.27,57
Soccer (football, futbol) is undoubtedly the most popular and widely played sport in the world, with an estimated 260 million active players. 75 Due to the dynamic range of movement exhibited by a soccer player on the pitch, such as cutting, pivoting, jumping, and landing, an ACL injury can be a devastating setback that results in a premature end to the soccer player’s season. 15 In a prospective study of professional soccer players who underwent ACLR, only 85.8% were actively playing soccer and only 65% were playing at their preinjury level 3 years after surgery. 75 Another study found that, at a follow-up of 4 years after ACLR, only 71% of professional soccer players were playing soccer at a competitive level. 80
There exists a wealth of information regarding the risk factors, clinical outcomes, return-to-sport rate, and failure/revision rates for athletes who have undergone ACLR across all sports.7,17,29,40,42,47,78 Studies have shown that younger age and female sex are common risk factors for ACL injuries, especially athletes participating in pivoting sports.24,78 A systematic review by Ardern et al 7 found that 63% of all athletes returned to preinjury level of sport; in comparison, only 44% of competitive athletes managed to return to preinjury level of participation. Regarding failure/revision rates, a meta-analysis found that the overall second ACL reinjury rate in athletes was estimated to be 15%. 78 Along with vastly different demands put on an athlete’s knee for different sports, the authors highlight the importance of reporting sport-specific outcomes for the purposes of conveying expectations for athletes and coaches and optimizing rehabilitation regimen according to that sport.
There exists a number of studies pertaining to ACLR for soccer players.31,48,73,75 However, all review articles to date have focused on topics regarding epidemiology, risk factors, and prevention strategy for ACL injuries in soccer players. To the best of the authors’ knowledge, comparative review studies evaluating outcomes after ACLR solely in soccer players are lacking. Furthermore, the systematic review conducted by Warner et al 76 concluded that there is a relatively small amount of data in the literature on “sport-specific outcomes” in athletes after ACLR. The purpose of this study was to report soccer-specific outcomes with regard to soccer by performing a systematic review and meta-analysis of available literature on clinical outcomes and patient-reported outcomes (PROs) after ACLR exclusively in soccer players.
Methods
Search Strategy
A comprehensive search of publications that reported on the outcomes after ACLR in soccer players was performed by the first author in May 2020 using PubMed, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL), and SPORTDiscus databases. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRIMSA) guidelines were followed. 46 The following search terms were used for each database previously outlined: (“ACL” OR “anterior cruciate ligament”) AND “Reconstruction” AND (“soccer” OR “football” OR “futbol”). Inclusion criteria consisted of original studies, level of evidence of 1 to 4, studies focusing on clinical outcomes after ACLR in soccer (football) players, studies reporting length of time from ACLR to return to play, studies reporting time from injury to surgery, PROs, graft failure, or second ACL injury after ACLR. The exclusion criteria consisted of studies focusing on American Football players, review articles, technique papers, conference/presentation abstracts, case reports, editorials, expert opinion, non-English language studies, data pertaining exclusively to soccer players not reported, studies reporting on ACLR combined with other ligamentous procedures, or studies that did not present outcomes data.
Evaluation of Study Quality
To evaluate the methodological quality of the studies included in this review, the methodological index for nonrandomized studies (MINORS) was utilized. 65 MINORS criteria is an assessment tool to evaluate methodology and risks of bias for nonrandomized studies involving 8 criteria for noncomparative studies and an additional 4 criteria for comparative studies. Each criteria is given a score of 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate) for a maximum global score of 16 and 24 for noncomparative and comparative studies, respectively. Two independent blinded reviewers assessed each study, and discrepancies in scores were discussed by the 2 reviewers until a consensus was reached. Analyses of the means and standard deviations (range) of global scores of noncomparative and comparative studies were performed. Higher scores indicate a high-quality study and methodology with a low risk of bias (Online Appendix Table A1).
For Level 1 evidence: 1 randomized controlled trial, 44 the risk of bias assessment was conducted using Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) by 2 independent blinded reviewers. 67
Data Extraction
For all eligible studies that were included for review and meta-analysis, data were extracted from the full text and entered into a database. Data collected consisted of the article title, authors, country, publication year, journal, level of evidence, sample size, patient demographical information (sex, mean/median age, height, body mass index [BMI]), type of graft used for ACLR, concomitant knee injuries, length of time from injury to surgery, time to return to play, and outcomes of clinical follow-up (graft failure/reoperation rates, secondary ACL injury to contralateral knee, and PRO with associated follow-up time intervals). The primary PRO measures that were reported in the studies included the Knee Injury and Osteoarthritis Outcome Score (KOOS), the International Knee Documentation Committee (IKDC) score, the Lysholm score, and the Tegner Activity Scale.
Statistical Analysis
Ranges for mean/median age, height, BMI, concomitant articular cartilage or medial/lateral meniscal injury, time from injury to surgery, rates of graft failure/reoperation, rate of contralateral knee ACL injury, and the combined ACL reinjury, return-to-sport time, and return to competition time were reported from all studies reporting each respective variable. Graft choice, and numbers of male and female subjects were reported as counts. A random-effects meta-analysis of proportions was used to calculate pooled estimates for single proportions including proportion of hamstring grafts, allografts, and reinjury rates. All analyses were weighted for individual study size. Subgroup pooled estimates of reinjury proportions are presented with forest plots for the total study population, for studies including only male or only female athletes. Subgroup analysis for the effect of sex and type of graft on reinjury risk was not possible as individual studies did not report the necessary stratified data. All analyses were performed in R Version 4.0.0 (R is a programming language and free software environment for statistical computing and graphics supported by the R Foundation) using the metafor package. 72
Results
Study Selection
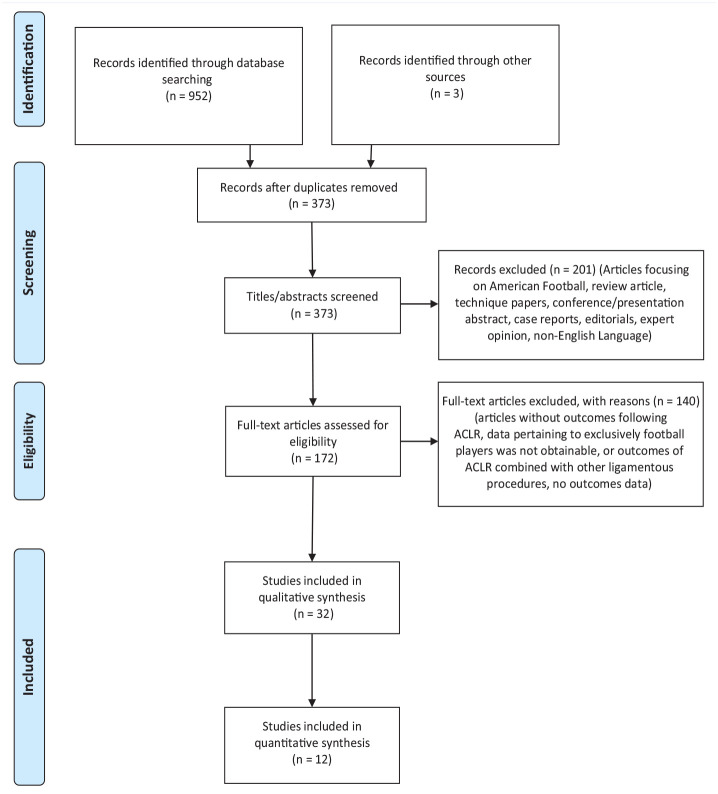
Using PRISMA guidelines, a search of literature as outlined in Methods yielded a total of 952 articles; 3 additional articles were identified using the reference lists of studies included in the final qualitative synthesis. A total of 582 articles were identified as duplicates and were excluded. Titles and abstracts of the remaining 373 articles were screened using the inclusion and exclusion criteria set out, and resulted in further exclusion of 201 articles. The full texts of 172 articles were screened and 140 studies were excluded. A total of 32 studies were used for qualitative synthesis and systematic review; 12 of the 32 studies reporting on graft failure/reoperation rate, contralateral ACL injury, or second ACL injury were included in the meta-analysis (Figure 1).
Figure 1.
PRISMA search strategy flow diagram. ACLR, anterior cruciate ligament reconstruction; PRISMA, preferred reporting items for systematic reviews and meta-analyses.
Study Characteristics
The majority of the articles that were included in the review were of Level 3 to 4 evidence; 1 of 32 (3.1%) was Level 1 evidence, 44 11 of 32 of studies were Level 2,2,5,6,9,10,14,20,24,64,75,77 11 of 32 (34.4%) of studies were Level 3 evidence,1,3,21,22,24,25,52,54,60,61,71 and 9 of 32 (28.1%) of studies were Level 4 evidence.4,12,33,35,38,58,62,74,80 The outcomes of 3112 soccer players after ACLR were available for analysis. The reported number of male athletes who underwent ACLR was 1780, compared with 1181 female athletes (Table 1). The range of mean age of soccer players who underwent ACLR was 15.7 to 29.7 years, range of mean height was 1.68 to 1.82 m, and range of mean BMI was 22.8 to 24.9 kg/m2. Of the studies that reported the type of graft used for the reconstruction, 14 of 32 (43.8%) studies used autografts1,3-5,9,14,20,33,38,44,54,60,64,74; the 2 most commonly used grafts included 1600 hamstring tendon (HT) and 663 bone-patellar-tendon-bone (BPTB) grafts. Using the concomitant procedures data, the range of patients with articular cartilage involvement was 6.5% to 30.4% and meniscal involvement was 35.6% to 60.0% (Table 2).
Table 1.
Details of soccer players treated with ACLR
| First Author (year) | Country of Origin | Level of Evidence | Study Design | Quality Criteria a | Number of ACLR | Number of Control | Number of Males | Number of Females | Mean Age of ACLR, y | Mean Age of Control, y | Mean Height of ACLR, m | Mean Height of Control, m | Mean BMI of ACLR, kg/m2 | Mean BMI of Control, kg/m2 | Graft(s) used |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Allen (2016) 1 | US | 3 | Retrospective cohort study | 90.9% | 90 | 0 | 0 | 90 | 19.6 | NR | NR | NR | 23.1 | NR | 45 HT (Au), 42 BPTB (Au), 3 BPTB (Al) |
| Almeida (2018) 2 | Brazil | 2 | Prospective case-control | 100.0% | 20 | 20 | 40 | 0 | 21ME | 20.5ME | 1.82 | 1.79 | 23.7 | 23.4 | 20 HT |
| Alonso (2009) 3 | Brazil | 3 | Cross-sectional study | 72.7% | 24 | 20 | NR | NR | 29 | 26 | 1.75 | 1.79 | NR | NR | 24 BPTB (Au) |
| Alonso (2019) 4 | Chile | 4 | Case series | 72.7% | 61 | 0 | 61 | 0 | 29.7 | NR | NR | NR | NR | NR | 50 HT (Au), 11 BPTB (Au) |
| Alvarez-Diaz (2015) 5 | Spain | 2 | Prospective pre-post, within-group comparison | 90.9% | 40 | 0 | 40 | 0 | 22.3 | NR | 1.75 | NR | 23.3 | NR | 40 BPTB (Au) |
| Angelozzi (2012) 6 | Italy | 2 | Prospective longitudinal cohort study | 72.7% | 45 | 0 | 45 | 0 | 23.4 | NR | 1.78 | NR | 24.9 | NR | 45 HT |
| Arundale (2019) 9 | Sweden | 2 | Prospective cohort study | 100.0% | 117 | 0 | 0 | 117 | NR | NR | NR | NR | NR | NR | 114 HT (Au), 2 BPTB (Au), 1 Quadriceps (Au) |
| Bak (2001) 10 | Denmark, Sweden | 2 | Prospective cohort study | 72.7% | 132 | 0 | 117 | 15 | 23ME | NR | NR | NR | NR | NR | 132 Iliotibialband (Al) |
| Barth (2019) 12 | US | 4 | Case series | 72.7% | 176 | 0 | 176 | 0 | NR | NR | NR | NR | 23.7 | NR | NR |
| Brophy (2012) 14 | US | 2 | Prospective cohort study | 90.9% | 100 | 0 | 55 | 45 | NR | NR | NR | NR | NR | NR | 28 HT (Au), 69 BPTB (Au), 4 BPTB (Al) |
| Drocco (2019) 20 | Italy | 2 | Prospective case-control study | 90.9% | 36 | 0 | 36 | 0 | NR | NR | NR | NR | NR | NR | 36 HT (Au) |
| Ellera Gomes (2014) 21 | Brazil | 3 | Retrospective case-control study | 63.6% | 28 | 27 | 55 | 0 | NR | NR | NR | NR | NR | NR | NR |
| Erickson (2013) 22 | US | 3 | Retrospective case-control study | 81.8% | 74 | 0 | 74 | 0 | 25.6 | NR | NR | NR | NR | NR | NR |
| Fältström (2016) 24 | Sweden | 3 | Cross-sectional study | 90.9% | 182 | 0 | 0 | 182 | NR | NR | NR | NR | NR | NR | 177 HT, 2 BPTB, 3 Unknown |
| Fältström (2017) 25 | Sweden | 3 | Cross-sectional study | 100.0% | 77 | 77 | 0 | 154 | 18.4 | 19.5 | 1.68 | 1.68 | 22.8 | 22.1 | 74 HT, 1 BPTB, 2 Unknown |
| Fältström (2019) 26 | Sweden | 2 | Prospective cohort study | 90.9% | 117 | 119 | 0 | 236 | 19.9 | 19.5 | 1.68 | 1.67 | 23 | 22.3 | 114 HT, 2 BPTB, 1 Quadriceps |
| Guzzini (2016) 33 | Italy | 4 | Case series | 72.7% | 16 | 0 | 0 | 16 | 24.9 | NR | NR | NR | NR | NR | 16 HT (Au) |
| Herrington (2018) 35 | UK, Saudi Arabia | 4 | Cross-sectional study | 72.7% | 15 | 8 | 23 | 0 | 22.3 | 20.1 | 1.75 | 1.73 | NR | NR | 10 HT, 5 BPTB |
| Howard (2016) 39 | US | 4 | Case series | 72.7% | 78 | 0 | 0 | 78 | 19.3ME | NR | NR | NR | NR | NR | 52 BPTB (Au), 1 BPTB (Al), 13 HT (Au), 1 HT (Al), 1 Quadriceps (Au),2 Tibialis anterior (Al), 3 Achilles Tendon (Al), 1 Peroneal tendon (Al), 2 mixed HT (Au/Al)2 Unknown |
| Martin-Alguacil (2018) 44 | Spain | 1 | Randomized controlled trial | 90.9% | 51 | 0 | 39 | 12 | NR | NR | NR | NR | NR | NR | 25 HT (Au), 26 Quadriceps (Au) |
| Niederer (2018) 52 | Germany | 3 | Retrospective case-control study | 81.8% | 132 (7 bilateral) | 264 | 388 | 0 | 25.3 | NR | NR | NR | NR | NR | NR |
| Patras (2012) 54 | Greece, US | 3 | Retrospective case-control study | 63.6% | 14 | 14 | 28 | 0 | 24.8 | 21.7 | 1.77 | 1.8 | NR | NR | 14 BPTB (Au) |
| Roos (1995) 58 | Sweden | 4 | Case series | 63.6% | 121 | NR | NR | NR | NR | NR | NR | NR | NR | NR | 7 HT, 79 BPTB, 15 Synthetic,9 Retinaculum + BPTB, 11 Fascia lata strip |
| Sandon (2015) 61 | Sweden | 3 | Retrospective case-control study | 81.8% | 205 | 0 | 116 | 89 | NR | NR | NR | NR | NR | NR | 183 HT, 22 BPTB, |
| Sandon (2020) 60 | Sweden | 3 | Retrospective case-control study | 81.8% | 684 | 0 | 432 | 252 | 25.9 | NR | NR | NR | NR | NR | 556 HT (Au), 118 BPTB (Au) |
| Schiffner (2018) 62 | Germany | 4 | Case series | 63.6% | 72 (6 bilateral) | NR | 66 | 0 | 24 | NR | NR | NR | NR | NR | NR |
| Shelbourne (2009) 64 | US | 2 | Prospective cohort study | 81.8% | 102 | 0 | 25 | 77 | 15.7 | NR | NR | NR | NR | NR | 102 BPTB (Au) |
| Thomson (2018) 71 | UK, Qatar | 3 | Retrospective case-control study | 54.5% | 16 | 16 | 32 | 0 | 26 | 28 | 1.78 | 1.79 | NR | NR | 9 HT, 7 BPTB |
| Waldén (2011) 75 | Sweden | 2 | Prospective 3-cohort study | 72.7% | 71 | 0 | 57 | 14 | NR | NR | NR | NR | NR | NR | 2 Iliotibial band (Al), 35 HT, 2 BPTB (Al)21 BPTB (Au), 11 unspecified |
| Waldén (2016) 74 | Sweden | 4 | Prospective cohort study | 81.8% | 157 | 0 | 157 | 0 | NR | NR | NR | NR | NR | NR | NR |
| Welling (2019) 77 | the Netherlands, Belgium, Luxembourg, Germany | 2 | Prospective case-control study | 90.9% | 38 | 38 | 76 | 0 | 24 | 23 | NR | NR | NR | NR | 24 HT, 14 BPTB |
| Zaffagnini (2014) 80 | Italy | 4 | Case series | 90.9% | 21 | 0 | 21 | 0 | 22.9 | NR | NR | NR | NR | NR | NR |
| Summary Statistics | 80.4% ± 11.8% | Total male athletes = 1780 | Total female athletes = 1181 | Range, 15.7-29.7 | Range, 1.68-1.82 | Range,22.8-24.9 | HT = 1600, BPTB = 663, Quadriceps = 30, Iliotibial=134, Tibialis anterior = 2, Achilles = 3, Peroneal = 1, Fascia lata strip = 11, Unknown = 671 |
Table 2.
Summary of studies reporting concomitant knee injuries and/or time from injury to index aclr surgery in soccer players
| First Author (Year) | Concomitant Knee Injuries | Time from Injury to Surgery | |
|---|---|---|---|
| Articular Cartilage | Medial/Lateral Meniscal Injury | ||
| Allen (2016) 1 | 6/90 (6.7%) | 54/90 (60.0%) | NR |
| Almeida (2018) 2 | NR | NR | Median, 3 mo; Range, 1-12 mo |
| Alonso (2009) 3 | NR | NR | NR |
| Alonso (2019) 4 | NR | NR | NR |
| Alvarez-Diaz (2015) 5 | NR | NR | NR |
| Angelozzi (2012) 6 | NR | NR | Mean, 4.3 ± 2.8 mo; Range, 2-9 mo |
| Arundale (2019) 9 | 11/117 (9.4%) | 49/117 (41.9%) | <3 mo, 42/117; 3-6 mo, 35/117; 6-9 mo, 25/117; >9 mo, 15/117; Median, 3 mo; Range, 0-22 mo |
| Bak (2001) 10 | NR | 47/132 (35.6%) | Median, 15 mo; Range, 3-72 mo |
| Barth (2019) 12 | NR | NR | Mean, 13.7 ± 1 days |
| Brophy (2012) 14 | NR | NR | NR |
| Drocco (2019) 20 | NR | NR | NR |
| Ellera Gomes (2014) 21 | NR | NR | NR |
| Erickson (2013) 22 | NR | NR | NR |
| Fältström (2016) 24 | 16/182 (8.8%) | 75/182 (41.2%) | <3 mo, 42/182; 3-6 mo, 112/182; >12 mo, 20/182 |
| Fältström (2017) 25 | 5/77 (6.5%) | 31/77 (40.3%) | <3 mo, 22/77, 3-12 mo, 48/77; >12 mo, 6/77; Median, 4 mo; IQR, 5 mo |
| Fältström (2019) 26 | 11/117 (9.4%) | NR | <3 mo, 42/117, 3-6 mo, 69/117; >12 mo, 6/117, Median, 3 mo; Range, 0-22 mo; IQR, 5 mo |
| Guzzini (2016) 33 | NR | NR | Mean, 4.5 ± 2.5 days; Range, 2-11 days |
| Herrington (2018) 35 | NR | NR | NR |
| Howard (2016) 38 | NR | NR | NR |
| Martin-Alguacil (2018) 44 | NR | NR | NR |
| Niederer (2018) 52 | NR | NR | NR |
| Patras (2012) 54 | NR | NR | <6 mo, 14/14 |
| Roos (1995) 58 | NR | NR | NR |
| Sandon (2015) 61 | 39/205 (19.0%) | 95/205 (46.3%) | NR |
| Sandon (2020) 61 | 208/684 (30.4%) | 255/684 (37.3%) | Mean, 23.7 ± 41.7 mo |
| Schiffner (2018) 62 | NR | NR | NR |
| Shelbourne (2009) 64 | NR | NR | NR |
| Thomson (2018) 71 | NR | NR | NR |
| Waldén (2011) 75 | NR | NR | Mean for male athletes, 44.7 ± 36 days; Mean for female athletes, 65.3 ± 90.8 days |
| Waldén (2016) 74 | NR | NR | NR |
| Welling (2019) 77 | NR | NR | NR |
| Zaffagnini (2014) 80 | NR | NR | Mean, 48 days ± 36 days; Range, 17-98 days |
| Summary Statistics | Range, 6.5%-30.4% | Range, 35.6%-60.0% | Range, 13.7 days-23.7 mo |
ACLR, anterior cruciate ligament reconstruction; NR, not reported.
Evaluation of Study Quality
MINORS criteria revealed that, for noncomparative studies, the mean global scores for 12 studies was 11.9 ± 3.0 (range, 7-18) and for 19 comparative studies the mean global scores for 19 studies was 18.1 ± 3.4 (range, 11-23). The risks of bias for 1 level of evidence 1 randomized controlled trial using RoB 2 demonstrated “low risk of bias” in the randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome, and “some concern” in the selection of the reported results and the overall bias level was determined to be “some concern.”
Outcomes After ACLR
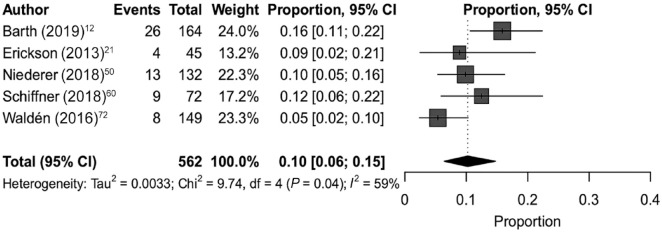
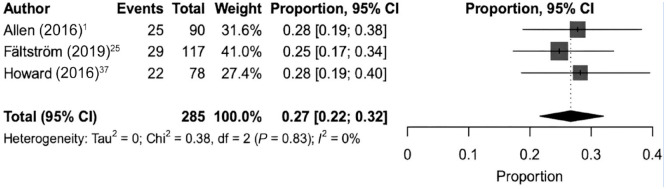
The overall graft failure/reoperation rate after ACLR in soccer players (Table 3) ranged from 3.0% to 24.8%, and the overall contralateral ACL injury rate after ACLR ranged between 1.0% and 16.7%. Three studies did not mention the laterality of a second ACL injury after ACLR.22,38,52 However, the secondary ACL injury rate regardless of laterality ranged between 5.4% and 27.8%. A stratified analysis of the secondary ACL injury rate in male soccer players was 10%, 95% CI (6%, 15%), I2 = 58.9% (Figure 2). In contrast, the secondary ACL injury rate in female soccer players was 27%, 95% CI (22%, 32%), I2 = 0.0% (Figure 3).
Table 3.
Summary of studies reporting second ACL injury after index surgery in soccer players
| First Author (Year) | Second ACL Rupture after Index ACLR | ACL Rupture in Control Group | Data Collection Method | Time from ACLR to Final Follow-up | ||
|---|---|---|---|---|---|---|
| ACL Rerupture | Contralateral Knee to First ACL Rupture | Laterality Unknown | ||||
| Allen (2016) 1 | 10/90 (11.1%) | 15/90 (16.7%) | NR | NR | Physical examination performed | Mean, 68.8 ± 46.2 mo (minimum >24 mo) |
| Almeida (2018) 2 | NR | NR | NR | NR | Physical examination performed | 6 mo |
| Alonso (2009) 3 | NR | NR | NR | NR | Physical examination performed | Mean, 36 ± 10 mo (range, 21-59 mo) |
| Alonso (2019) 4 | NR | NR | NR | NR | Physical examination performed | Mean, 22.4 ± 3.4 mo |
| Alvarez-Diaz (2015) 5 | NR | NR | NR | NR | Physical examination performed | NR |
| Angelozzi (2012) 6 | NR | NR | NR | NR | Physical examination performed | 12 mo |
| Arundale (2019) 9 | NR | NR | NR | NR | Physical examination performed | NR |
| Bak (2001) 10 | 4/132 (3.0%) | 9/132 (6.8%) | NR | NR | Physical examination performed | Median, 47 mo (range, 24-92 mo) |
| Barth (2019) 12 | 19/164 (11.6%) | 7/164 (4.2%) | NR | NR | Publicly available sources reporting injury news for professional players | NR |
| Brophy (2012) 14 | 3/100 (3.0%) | 9/100 (9.0%) | NR | NR | Questionnaire | Mean, 7.2 ± 0.9 y |
| Drocco (2019) 20 | NR | NR | NR | NR | Physical examination | ST3 cohort mean, 22.6 ± 7.7 mo; GST cohort mean, 23.0 ± 7.3 mo |
| Ellera Gomes (2014) 21 | NR | NR | NR | NR | Physical examination | NR |
| Erickson (2013) 22 | NR | NR | 4/45 | NR | Publicly available sources reporting injury news for professional players | >8 mo postoperative |
| Fältström (2016) 24 | NR | NR | NR | NR | Swedish National ACL Registry | Median, 18 mo (IQR, 13 mo) |
| Fältström (2017) 25 | NR | NR | NR | NR | Swedish National ACL Registry to identify patients and physical examination performed | Median, 18 mo (IQR, 14.5 mo) |
| Fältström (2019) 26 | 29/117 (24.8%) | NR | NR | 8/119 | Swedish National ACL Registry and questionnaire | Median, 28 mo (IQR, 14 mo; range,13-57 mo) |
| Guzzini (2016) | NR | NR | NR | NR | Physical examination | Mean, 72.6 ± 8.1 mo |
| Herrington (2018) 35 | NR | NR | NR | NR | Physical examination | Mean, 7.8 ± 1.3 mo |
| Howard (2016) 38 | NR | NR | 22/78 | NR | Questionnaire | NR |
| Martin-Alguacil (2018) 44 | NR | NR | NR | NR | Physical examination | 24 mo postoperatively |
| Niederer (2018) 52 | NR | NR | 13/132 | 2/263 | Publicly available sources reporting injury news for professional players | - |
| Patras (2012) 54 | NR | NR | NR | NR | Physical examination | Mean, 18.5 ± 4.3 mo |
| Roos (1995) 58 | NR | NR | NR | NR | Swedish National Insurance Registry | NR |
| Sandon (2015) 61 | NR | NR | NR | NR | Swedish National ACL Registry and questionnaire | 3.2 ± 1.4 y |
| Sandon (2020)60 | 46/684 (6.7%) | 109/684 (15.9%) | NR | NR | Swedish National ACL Registry and questionnaire | 10 y |
| Schiffner (2018) 62 | 4/72 (5.6%) | 5/72 (6.9%) | NR | NR | Publicly available sources reporting injury news for professional players | NR |
| Shelbourne (2009) 64 | 16/102 (15.7%) | 1/102 (1.0%) | NR | NR | Physical examination | NR |
| Thomson (2018) 71 | NR | NR | NR | NR | Physical examination | Range, 5-10 mo postoperatively |
| Waldén (2011) 75 | NR | NR | NR | NR | Questionnaire | NR |
| Waldén (2016) 74 | 6/149 (4.0%) | 2/149 (1.3%) | NR | NR | Questionnaire | 3-y follow-up |
| Welling (2019) 77 | NR | NR | NR | NR | Physical examination | 10-mo follow-up |
| Zaffagnini (2014) 80 | NR | NR | NR | NR | Physical examination | 4-y follow-up |
| Summary Statistics | Range, 3.0% - 24.8% | Range, 1.0%-16.7% | Physical examination, 19/32 (59%) Publicly available sources; 4/32 (13%) Registry, 5/32 (16%); Questionnaire, 7/32 (22%) |
Range, 5 mo-10 years; Studies with minimum 2-y follow-up, 9/32 (28%) |
||
| Total: Range, 5.4% - 27.8% | ||||||
ACL, anterior cruciate ligament; ACLR, ACL reconstruction; GST, double gracilis-semitendinosus tendon graft; NR, not reported; ST3, triple semitendinosus graft.
Figure 2.
Forest plot showing pooled overall secondary ACL injury rate after ACLR in male soccer players. ACL, anterior cruciate ligament; ACLR, ACL reconstruction.
Figure 3.
Forest plot showing pooled overall secondary ACL injury rate after ACLR in female soccer players. ACL, anterior cruciate ligament; ACLR, ACL reconstruction.
Studies reported return to sport by specifying either return to soccer training and/or return to soccer match. The range of mean return to soccer training was 3 to 12.2 months and return to soccer match was 6.1 to 11.1 months (Table 4). A subset of studies reported both return to soccer training and return to soccer match.24,25,35,38,74,80 When using these subset of studies, the range of mean return to soccer training was 3 to 9 months and return to soccer match was 5.1 to 11 months.
Table 4.
Summary of studies reporting return to play after index ACLR surgery in soccer players
| First Author (Year) | Time from ACLR to Soccer Training | Time from ACLR to Soccer Match | Level of Soccer |
|---|---|---|---|
| Allen (2016) 1 | NR | NR | NR |
| Almeida (2018) 2 | NR | NR | Professional |
| Alonso (2009) 3 | Mean, 10 ± 3 mo; Range, 6-20 mo | NR | Recreational |
| Alonso (2019) 4 | - | NR | Recreational |
| Alvarez-Diaz (2015) 5 | Median, 5 mo; Range, 1-24 mo | NR | NR |
| Angelozzi (2012) 6 | NR | NR | Professional |
| Arundale (2019) 9 | NR | NR | Professional and recreational |
| Bak (2001) 10 | NR | Median, 7 mo; Range, 5-24 mo | Professional and Recreational |
| Barth (2019) 12 | NR | Mean, 310.9 ± 14.9 days | Professional |
| Brophy (2012) 14 | Mean, 12.2 ± 14.3 mo, Male athletes: Mean, 10.2 ± 7.3 mo; Female athletes: Mean, 15 ± 20.3 mo | NR | NR |
| Drocco (2019) 20 | NR | NR | NR |
| Ellera Gomes (2014) 21 | Mean, 10 ± 2.8 mo | NR | NR |
| Erickson (2013) 22 | NR | NR | Professional and recreational |
| Fältström (2016) 24 | Median, 7 mo; IQR, 13 mo | Median, 11 mo, IQR,5 mo | - |
| Fältström (2017) 25 | Median, 9 mo; Range, 3-33 mo; IQR, 5 mo | Median, 11 mo, Range, 6-34 mo, IQR=5.5 mo | Professional |
| Fältström (2019) 26 | NR | NR | NR |
| Guzzini (2016) 33 | NR | NR | Professional |
| Herrington (2018) 35 | Mean, 201.5 ± 68.7 days | Mean, 224.1 ± 75.8 days | Professional |
| Howard (2016) 38 | Median, 5.5 mo, Range, 3.8-12.7 mo | Median, 6.1 mo, Range, 3.9-33.2 mo | College |
| Martin-Alguacil (2018) 44 | NR | NR | NR |
| Niederer (2018) 52 | NR | Mean, 209 ± 93 days | Professional |
| Patras (2012) 54 | NR | NR | NR |
| Roos (1995) 58 | NR | NR | NR |
| Sandon (2015) 61 | NR | NR | NR |
| Sandon (2020) 60 | NR | NR | NR |
| Schiffner (2018) 65 | NR | NR | NR |
| Shelbourne (2009) 64 | NR | Male athletes: Mean, 5.1 ± 2 mo; Female athletes: Mean, 5.1 ± 1.9 mo | NR |
| Thomson (2018) 71 | NR | NR | Professional |
| Waldén (2011) 75 | NR | NR | Professional |
| Waldén (2016) 74 | Median, 201.5 days; IQR, 58 days | Median, 225 days; IQR, 80.3 days | Professional |
| Welling (2019) 77 | NR | NR | Recreational |
| Zaffagnini (2014) 80 | Mean, 84 ± 51 days; Range, 35-154 days | Mean, 186 ± 52 days; Range, 107-282 days | Professional |
| Summary Statistics | Range, 3 - 12.2 mo | Range, 6.1 - 11.1 mo |
ACL, anterior cruciate ligament; ACLR, ACL reconstruction; NR, not reported.
Of the 32 studies, 15 (46.9%) reported PROs. The KOOS was reported by 5 studies (Online Appendix Table A2).24,35,59,61,80 However, only 4 studies reported the 5 separate subscales (symptoms, pain, function in daily living, function in sport and recreation, and quality of life). The follow-up period for KOOS ranged from a minimum of 3 months to a maximum of 10 years. Two studies reported KOOS scores of soccer players who had returned to soccer and those who did not return.24,61 The mean function in sport and recreation subscale score for players who returned to soccer was 77.9 ± 20.9 and 51 ± 28. In contrast, the mean function in sport and recreation subscale score for players that did not return to soccer was 62.9 ± 22.2 and 72 ± 21. The IKDC score was reported in 10 studies.1,2,6,10,20,24-26,33,77 Postoperatively, the mean IKDC scores at final follow-up ranged from a minimum of 80.2 to a maximum of 95. Of note, 1 study reported 2 separate mean IKDC scores for a cohort of soccer players treated with semitendinosus in triple configuration (91.4 ± 7.9) and a cohort of soccer players treated with double semitendinosus combined with a gracilis autograft (79.6 ± 12.9). 20 Lysholm score was reported in 7 studies.1,2,10,20,33,54,61 The mean preoperative Lysholm score ranged from a minimum of 52.5 ± 5.1 to a maximum of 80.5 ± 11.9. The mean postoperative Lysholm score at final follow-up ranged from a minimum 88 ± 15 to a maximum of 96 (SD not reported). The same aforementioned study reported 2 separate mean Lysholm scores for a cohort of soccer players treated with semitendinosus in triple configuration (97.7 ± 3.8) and a cohort of soccer players treated with double semitendinosus combined with a gracilis autograft (87 ± 9.6). Finally, the Tegner activity scale was reported in 10 studies.1,5,6,10,24,26,33,54,61,77 With the exception of 2 studies,26,33 all studies that reported preoperative and postoperative follow-up Tegner activity scales after ACLR saw improvements.
Discussion
The primary findings of this systematic review and meta-analysis on clinical outcomes after ACLR on soccer players found that (1) female players experienced an incidence of secondary ACL injury of 27%, whereas the incidence in male players was 10%; (2) there is a higher rate of ipsilateral ACL injury (graft failure/reoperation) than contralateral ACL injury; (3) players were able to return to soccer matches as early as 6.1 months after ACLR; and (4) there was a general positive trend in PROs at medium-term follow-up.
The increased risks of ACL tear rates in female athletes compared with male athletes have been reported widely in the literature.8,30,34,53,59 Previous review articles have summarized the differences between male and female athletes with regard to risk of ACL injury and proposed various factors such as greater Q angle, increased posterior tibial slope, narrow femoral intercondylar notch, neuromuscular activation patterns of knee musculature, and cyclical sex hormones during menarche that may play a role in the higher rupture rates in female athletes, although no definitive consensus has been reached.69,70 A recent study by Pfeiffer et al 55 found that healthy female collegiate athletes with no previous knee injury demonstrate an increased rotatary knee laxity determined using image capture analysis during the pivot-shift test examination. The authors suggest that this higher baseline rotatory knee laxity may contribute to the poor outcomes after ACLR in female athletes. A meta-analysis of the incidence of ACL tears by Prodromos et al 56 found a female:male ratio of 2.67 for soccer players. However, there is a paucity of data regarding secondary ACL tear rates after ACLR in soccer players. Our meta-analysis found that the incidence proportion of female players who sustained secondary ACL injury was 27%, 95% CI (22%, 32%) compared with male players, who experienced 10%, 95% CI (6%, 15%) equating to a female:male ratio of 2.7. This female:male secondary ACL injury ratio subsequent to ACLR of 2.7 is comparable with the ratio of 2.67 found by Prodromos et al 56 for primary ACL injury incidence in soccer players. Although we cannot directly compare secondary ACL injury incidence with primary ACL injury, it is evident that female soccer players face a higher risk for another ACL injury compared with their male counterparts. To mitigate the higher risk of recurrent ACL tears in female athletes, previous studies evaluating the use of neuromuscular and proprioceptive training programs have found that compliance improved biomechanical deficits in ACLR knee and decreased the incidence of ACL injuries, thus highlighting the importance of a regimented rehabilitation program especially in female athletes.43,50,68
Our study found that the overall secondary ACL injury rate in soccer players after ACLR ranged between 5.4% and 27.8%. Furthermore, when subgroup analysis for ipsilateral graft failure and contralateral limb ACL injury was done, we found an incidence ranging from 3.0% to 24.8% and from 1.0% to 16.7% respectively. A systematic review by Warner et al 76 focusing on long-term outcomes after ACLR found the ipsilateral ACL graft rupture rate to be 5.8% and contralateral ACL injury to be 11.8%; although this systematic review did not focus on athletes or soccer players, the respective graft failure and contralateral ACL injury rates fall within the ranges reported in our findings. A recent systematic review and meta-analysis by Wiggins et al 78 found the overall rate of secondary ACL injury after ACLR in all athletes who had returned to sports to be 15%, ipsilateral graft failure rate to be 7%, and contralateral ACL injury rate to be 8%. The findings by Wiggins et al 78 also fall within the ranges for soccer players reported in this study. A systematic review by Barber-Westin and Noyes 11 found that age <20 years is a key determinant for risk of secondary ACL reinjury after ACLR, noting that 18% reinjured either the ACL graft and/or contralateral ACL. Previous studies have determined stringent objective criteria that must be met during the rehabilitation stage before returning to sport, which has been shown to reduce recurrent graft failure and/or contralateral ACL injury by 4-fold.32,39 Kyritsis et al 39 found associations for a 4 times greater risk of ACL graft tear in athletes who had a decreased hamstring-to-quadriceps ratio of the involved leg during isokinetic tests, and who also did not meet the 6 discharge criteria, defined as (1) isokinetic test at 60, 180, and 300 deg/s; (2) single hop; (3) triple hop; (4) triple crossover hop; (5) on-field sports-specific rehabilitation; and (6) running t test. 39 For athletes participating in pivoting sports, Grindem et al found that returning to sports no later than 9 months post-ACLR and obtaining more symmetrical quadriceps strength measured on isokinetic quadriceps strength testing were associated with a reduced reinjury rate. 32 It is currently unclear why there exists a higher rate of contralateral secondary ACL injury compared with the ipsilateral graft failure rate; however, it is likely that it can be better explained using an aggregate of the various proposed mechanisms found in the literature. One theory is that the individual athlete retains the same risk factors that resulted in the primary ACL injury, 36 and the persistence of leg strength and functional performance deficits of the reconstructed knee for up to 2 years may cause athletes to compensate with their contralateral limb, potentially increasing the stress to which the contralateral knee is subjected.23,45 This highlights the importance of rehabilitation for both the ACLR knee as well as the contralateral knee to balance and equally strengthen any deficits caused during the recovery period subsequent to the ACLR.
The choice of graft for a highly active demographic has been debated extensively in the literature. The 2 most popular are BPTB autograft and HT autograft. 18 Our review found that 1600 ACLRs were performed using HT grafts and 663 ACLR using BPTB grafts. This may reflect the geographical differences in surgeon preference for graft choice. An international survey on ACLR practices found that 72% of European surgeons favored the HT significantly as compared with 42% of North American surgeons. 16 A survey of Major League Soccer Team Physicians validated the results of the previous study by reporting that North American surgeons have a preference for using BPTB autograft in elite soccer players, citing hamstring weakness as a major concern for avoiding the use of HT. Most studies included in our review originated from European nations, which may reflect the high proportion of HT used for ACLR in soccer players. DeFazio et al 18 found in their systematic review and meta-analysis that athletes treated with BPTB autografts resulted in higher return-to-sport rates in their respective sport when compared with HT autografts. Furthermore, recent studies have found that, in young female patients, BPTB autografts lead to fewer graft failure rates.59,63 However, recent clinical trials found that, when ACLR was performed with HT grafts in athletes participating in pivoting sports in the absence of a lateral extra-articular tenodesis or anterolateral ligament reconstruction, the risk of graft failure was 2.75 and 3.1 times higher, respectively.28,66 Sonnery-Cottet et al 66 also reported that ACLR reconstructed with HT and anterolateral ligament reconstruction reduced the risk of graft failure by 2.5 times when compared with BPTB grafts.
Our review of the literature revealed that soccer players are able to return to match play as early as 3 months (range, 3-12.2 months) and soccer training at 6.1 months (range, 6.1-11.1 months). A previous study found that athletes returning to sports after ACLR within 7 months had a 15.3% risk of reinjury compared with those returning after 7 months with a risk of 5.2% (P = 0.01). Authors also found that soccer players had the highest risk of reinjury rate of 20.8% compared with rugby players with a reinjury rate of 6.4%; however, soccer players were found to have returned to activity after a mean of 8.1 months compared with 10.6 months for rugby players.
The subjective PROs that were reported were heterogenous as many studies did not report the follow-up time or follow-up times that were widely variable. Therefore, we did not perform an aggregate analysis. Most studies reported good outcome scores at medium-term follow-up and, not surprisingly, that the mean PRO scores were of a lower value for players who did not return to soccer compared with those who did return. Furthermore, the reporting of preoperative PROs was limited; however, for most studies that reported preoperative and postoperative PROs, the scores had a positive trend, therefore providing evidence for better functional outcomes after undergoing ACLR in soccer players.
There are several limitations to this study. One limitation is that the literature search and data extraction were performed by 1 author only. Therefore, we are unable to provide agreement assessment between >1 reviewer for the literature search and data extraction. Subgroup analysis on overall pooled secondary ACL injury rate after ACLR in male soccer players had a relatively high heterogeneity (I2 = 58.9%) and must be interpreted with caution; however, this was reported to compare with the pooled rates calculated for female soccer players, which showed low heterogeneity (I2 = 0%). There was a lack of standardization when reporting secondary ACL injury (graft failure and/or contralateral ACL tear) and our meta-analysis did not account for the variability in reporting when analyzing ACL graft failure. Some studies reported a secondary ACL injury defined by reoperation and other studies obtained these data using scheduled clinical follow-up, registry data, publicly available sources reporting injury news for professional players, and questionnaires sent to postoperative patients, which may underestimate the reinjury rate. Registry studies uses revision cases to define failure, thereby further underestimating the reinjury rate. In addition, our study was unable to report the ipsilateral versus contralateral secondary ACL injury risk for male athletes compared with female athletes due to the limited number of studies that reported the distinction. With regard to the type of graft used for ACLR, the majority of studies reported the use of HT autograft and 0% use of BPTB grafts, which may not be representative of the autografts used worldwide, and thus the data reported may not reflect the true outcome in soccer players. Studies that reported concomittent cartilage and/or meniscal injuries did not report the extent of the cartilage damage and only 3 studies provided details on whether meniscectomy or repair was performed at the time of ACLR,10,25,60 thus limiting subanalysis on the effects on return to sports and PROs. As mentioned previously, a large majority of the selected literature was Level 3 to 4; thus, the PROs may be potentially biased toward those who were satisfied with their outcomes. Furthermore, due to the variability in the PRO questionnaires that were administered, as well as the method of determining a second ACL injury, aggregate subanalysis was limited. Furthermore, the goal of reporting outcomes after ACLR in soccer players resulted in the majority of studies focusing on a younger active population and those playing in professional leagues. This may limit the ability to use our reported data as evidence to provide a meaningful discussion regarding prognosis about ACLR in soccer players who are older and/or playing at a recreational level. Finally, broadly defining secondary ACL failure to include graft failure and second ACL injury after ACLR may limit the data reporting of specific incidences of graft failure and contralateral ACL tear within this review.
Conclusion
To our knowledge, this is the first study to review the current available literature focusing on outcomes after ACLR in only soccer players. The results of this study show that the secondary reinjury rates after ACLR fall within the range of previously reported rates for all athletes in general. Furthermore, it is evident that female soccer players are at greater risk of developing a secondary ACL injury. However, literature is currently lacking on the definitive reasons for the higher risk and definitive rehabilitation programs that reduce undesirable outcomes after ACLR. We believe future studies focusing on sports-specific athletes will allow optimization of the ACLR procedure and rehabilitation protocol with the objective of maximizing a tailored-approach for treating athletes according to the sports-specific physical demands and stress placed on the athlete.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_19417381231160167 for Clinical Outcomes After ACL Reconstruction in Soccer (Football, Futbol) Players: A Systematic Review and Meta-Analysis by Ian S. Hong, Lauren A. Pierpoint, Justin E. Hellwinkel, Alexander N. Berk, Jonathan M. Salandra, Joshua D. Meade, Dana P. Piasecki, James E. Fleischli, Christopher S. Ahmad, David P. Trofa and Bryan M. Saltzman in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-2-sph-10.1177_19417381231160167 for Clinical Outcomes After ACL Reconstruction in Soccer (Football, Futbol) Players: A Systematic Review and Meta-Analysis by Ian S. Hong, Lauren A. Pierpoint, Justin E. Hellwinkel, Alexander N. Berk, Jonathan M. Salandra, Joshua D. Meade, Dana P. Piasecki, James E. Fleischli, Christopher S. Ahmad, David P. Trofa and Bryan M. Saltzman in Sports Health: A Multidisciplinary Approach
Footnotes
The following authors declared potential conflicts of interest: D.P.P. worked as a presenter for Zimmer. J.E.F. received researched support from both Arthrex and Smith & Nephew. C.S.A. received royalties from both Arthrex and Lead Player, has stock or stock options with At Peak, received research support from the MLB, and received research support from Stryker. B.M.S. received royalties from Nova Science Publishers.
Contributor Information
Ian S. Hong, OrthoCarolina Sports Medicine Center, Charlotte, North Carolina and Musculoskeletal Institute, Atrium Health, Charlotte, North Carolina.
Lauren A. Pierpoint, Steadman Philippon Research Institute, Vail, Colorado.
Justin E. Hellwinkel, Department of Orthopaedic Surgery, New York-Presbyterian/Columbia University Irving Medical Center, New York, New York.
Alexander N. Berk, OrthoCarolina Sports Medicine Center, Charlotte, North Carolina and Musculoskeletal Institute, Atrium Health, Charlotte, North Carolina.
Jonathan M. Salandra, Department of Orthopaedic Surgery, Jersey City Medical Center, RWJBarnabas Health, Jersey City, New Jersey.
Joshua D. Meade, OrthoCarolina Sports Medicine Center, Charlotte, North Carolina, and Musculoskeletal Institute, Atrium Health, Charlotte, North Carolina.
Dana P. Piasecki, OrthoCarolina Sports Medicine Center, Charlotte, North Carolina and Musculoskeletal Institute, Atrium Health, Charlotte, North Carolina.
James E. Fleischli, OrthoCarolina Sports Medicine Center, Charlotte, North Carolina and Musculoskeletal Institute, Atrium Health, Charlotte, North Carolina.
Christopher S. Ahmad, Department of Orthopaedic Surgery, New York-Presbyterian/Columbia University Irving Medical Center, New York, New York.
David P. Trofa, Department of Orthopaedic Surgery, New York-Presbyterian/Columbia University Irving Medical Center, New York, New York.
Bryan M. Saltzman, OrthoCarolina Sports Medicine Center, Charlotte, North Carolina and Musculoskeletal Institute, Atrium Health, Charlotte, North Carolina.
References
- 1. Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44(10):2492-2498. [DOI] [PubMed] [Google Scholar]
- 2. Almeida AM de, Santos Silva PR, Pedrinelli A, Hernandez AJ. Aerobic fitness in professional soccer players after anterior cruciate ligament reconstruction. PLoS ONE. 2018;13(3):e0194432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alonso AC, Greve JMD, Camanho GL. Evaluating the center of gravity of dislocations in soccer players with and without reconstruction of the anterior cruciate ligament using a balance platform. Clinics (Sao Paulo). 2009;64(3):163-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alonso J, Malig S, Fontboté C, Azar C, Vergara F, Yáñez R. Return to play after anterior cruciate ligament reconstruction among amateur soccer players. Rev Chil Ortop Traumatol. 2019;60(2):35-38. [Google Scholar]
- 5. Alvarez-Diaz P, Alentorn-Geli E, Ramon S, et al. Effects of anterior cruciate ligament reconstruction on neuromuscular tensiomyographic characteristics of the lower extremity in competitive male soccer players. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3407-3413. [DOI] [PubMed] [Google Scholar]
- 6. Angelozzi M, Madama M, Corsica C, et al. Rate of force development as an adjunctive outcome measure for return-to-sport decisions after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):772-780. [DOI] [PubMed] [Google Scholar]
- 7. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596-606. [DOI] [PubMed] [Google Scholar]
- 8. Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34(2):86-92. PMID: 16558564 [PMC free article] [PubMed] [Google Scholar]
- 9. Arundale AJH, Kvist J, Hägglund M, Fältström A. Jumping performance based on duration of rehabilitation in female football players after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):556-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bak K, Jørgensen U, Ekstrand J, Scavenius M. Reconstruction of anterior cruciate ligament deficient knees in soccer players with an iliotibial band autograft: a prospective study of 132 reconstructed knees followed for 4 (2-7) years. Scand J Med Sci Sports. 2001;11(1):16-22. [DOI] [PubMed] [Google Scholar]
- 11. Barber-Westin S, Noyes FR. One in 5 athletes sustain reinjury upon return to high-risk sports after ACL reconstruction: a systematic review in 1239 athletes younger than 20 years. Sports Health. 2020;12(6):587-597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barth KA, Lawton CD, Touhey DC, et al. The negative impact of anterior cruciate ligament reconstruction in professional male footballers. Knee. 2019;26(1):142-148. [DOI] [PubMed] [Google Scholar]
- 13. Beynnon BD, Vacek PM, Newell MK, et al. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med. 2014;42(8):1806-1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517-2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brumitt J, Mattocks A, Engilis A, Isaak D, Loew J. Prior history of anterior cruciate ligament (ACL) reconstruction is associated with a greater risk of subsequent ACL injury in female collegiate athletes. J Sci Med Sport. 2019;22(12):1309-1313. [DOI] [PubMed] [Google Scholar]
- 16. Chechik O, Amar E, Khashan M, Lador R, Eyal G, Gold A. An international survey on anterior cruciate ligament reconstruction practices. Int Orthop. 2013;37(2):201-206. PMID: 22782378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cronström A, Tengman E, Häger CK. Risk factors for contra-lateral secondary anterior cruciate ligament injury: a systematic review with meta-analysis. Sports Med. 2021;51(7):1419-1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. DeFazio MW, Curry EJ, Gustin MJ, et al. Return to sport after ACL reconstruction with a BTB versus hamstring tendon autograft: a systematic review and meta-analysis. Orthop J Sports Med. 2020;8(12):2325967120964919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Drocco L, Camazzola D, Ferracini R, et al. Tripled semitendinosus with single harvesting is as effective but less invasive compared to standard gracilis-semitendinosus harvesting. Muscles Ligaments Tendons J. 2019;7(4):564-572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ellera Gomes JL, Palma HM, Ruthner R. Influence of hip restriction on noncontact ACL rerupture. Knee Surg Sports Traumatol Arthrosc. 2014;22(1):188-191. [DOI] [PubMed] [Google Scholar]
- 22. Erickson BJ, Harris JD, Cvetanovich GL, et al. Performance and return to sport after anterior cruciate ligament reconstruction in male major league soccer players. Orthop J Sports Med. 2013;1(2):232596711349718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ernst GP, Saliba E, Diduch DR, Hurwitz SR, Ball DW. Lower extremity compensations following anterior cruciate ligament reconstruction. Phys Ther. 2000;80(3):251-260. [PubMed] [Google Scholar]
- 24. Fältström A, Hägglund M, Kvist J. Factors associated with playing football after anterior cruciate ligament reconstruction in female football players: factors associated with playing football. Scand J Med Sci Sports. 2016;26(11):1343-1352. [DOI] [PubMed] [Google Scholar]
- 25. Fältström A, Hägglund M, Kvist J. Functional performance among active female soccer players after unilateral primary anterior cruciate ligament reconstruction compared with knee-healthy controls. Am J Sports Med. 2017;45(2):377-385. [DOI] [PubMed] [Google Scholar]
- 26. Fältström A, Kvist J, Gauffin H, Hägglund M. Female soccer players with anterior cruciate ligament reconstruction have a higher risk of new knee injuries and quit soccer to a higher degree than knee-healthy controls. Am J Sports Med. 2019;47(1):31-40. [DOI] [PubMed] [Google Scholar]
- 27. Filbay SR, Grindem H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract Res Clin Rheumatol. 2019;33(1):33-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Getgood AMJ, Bryant DM, Litchfield R, et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY study randomized clinical trial. Am J Sports Med. 2020;48(2):285-297. [DOI] [PubMed] [Google Scholar]
- 29. Glogovac G, Schumaier AP, Grawe BM. Return to sport following revision anterior cruciate ligament reconstruction in athletes: a systematic review. Arthroscopy. 2019;35(7):2222-2230. [DOI] [PubMed] [Google Scholar]
- 30. Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med. 2016;44(10):2716-2723. [DOI] [PubMed] [Google Scholar]
- 31. Grimm PD, Mauntel TC, Potter BK. Combat and noncombat musculoskeletal injuries in the US military. Sports Med Arthrosc Rev. 2019;27(3):84-91. [DOI] [PubMed] [Google Scholar]
- 32. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Guzzini M, Mazza D, Fabbri M, et al. Extra-articular tenodesis combined with an anterior cruciate ligament reconstruction in acute anterior cruciate ligament tear in elite female football players. Int Orthop. 2016;40(10):2091-2096. [DOI] [PubMed] [Google Scholar]
- 34. Harmon KG, Ireland ML. Gender differences in noncontact anterior cruciate ligament injuries. Clin Sports Med. 2000;19(2):287-302. [DOI] [PubMed] [Google Scholar]
- 35. Herrington L, Ghulam H, Comfort P. Quadriceps strength and functional performance after anterior cruciate ligament reconstruction in professional soccer players at time of return to sport. J Strength Cond Res. 2018;35(3):769-775. [DOI] [PubMed] [Google Scholar]
- 36. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492-501. [DOI] [PubMed] [Google Scholar]
- 37. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311-319. [PMC free article] [PubMed] [Google Scholar]
- 38. Howard JS, Lembach ML, Metzler AV, Johnson DL. Rates and determinants of return to play after anterior cruciate ligament reconstruction in National Collegiate Athletic Association Division I soccer athletes: a study of the Southeastern conference. Am J Sports Med. 2016;44(2):433-439. [DOI] [PubMed] [Google Scholar]
- 39. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946-951. [DOI] [PubMed] [Google Scholar]
- 40. Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52(2):128-138. [DOI] [PubMed] [Google Scholar]
- 41. Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury: high OA prevalence in ACL-injured female soccer players. Arthritis Rheum. 2004;50(10):3145-3152. [DOI] [PubMed] [Google Scholar]
- 42. Losciale JM, Zdeb RM, Ledbetter L, Reiman MP, Sell TC. The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2019;49(2):43-54. [DOI] [PubMed] [Google Scholar]
- 43. Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003-1010. [DOI] [PubMed] [Google Scholar]
- 44. Martin-Alguacil JL, Arroyo-Morales M, Martín-Gomez JL, et al. Strength recovery after anterior cruciate ligament reconstruction with quadriceps tendon versus hamstring tendon autografts in soccer players: a randomized controlled trial. Knee. 2018;25(4):704-714. [DOI] [PubMed] [Google Scholar]
- 45. Mattacola CG, Perrin DH, Gansneder BM, Gieck JH, Saliba EN, McCue FC. Strength, functional outcome, and postural stability after anterior cruciate ligament reconstruction. J Athl Train. 2002;37(3):262-268. [PMC free article] [PubMed] [Google Scholar]
- 46. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336-341. [DOI] [PubMed] [Google Scholar]
- 47. Mohtadi NG, Chan DS. Return to sport-specific performance after primary anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2018;46(13):3307-3316. [DOI] [PubMed] [Google Scholar]
- 48. Montalvo AM, Schneider DK, Silva PL, et al. ‘What’s my risk of sustaining an ACL injury while playing football (soccer)?’ A systematic review with meta-analysis. Br J Sports Med. 2019;53(21):1333-1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2010;13:2-12. [DOI] [PubMed] [Google Scholar]
- 50. Nagelli C, Di Stasi S, Tatarski R, et al. Neuromuscular training improves self-reported function and single-leg landing hip biomechanics in athletes after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2020;8(10):232596712095934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Nebelung W, Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy. 2005;21:696-702. [DOI] [PubMed] [Google Scholar]
- 52. Niederer D, Engeroff T, Wilke J, Vogt L, Banzer W. Return to play, performance, and career duration after anterior cruciate ligament rupture: a case-control study in the five biggest football nations in Europe. Scand J Med Sci Sports. 2018;28(10):2226-2233. [DOI] [PubMed] [Google Scholar]
- 53. Oliphant JG, Drawbert JP. Gender differences in anterior cruciate ligament injury rates in Wisconsin intercollegiate basketball. J Athl Train. 1996;31(3):245-247. [PMC free article] [PubMed] [Google Scholar]
- 54. Patras K, Zampeli F, Ristanis S, et al. Hamstring-dominant strategy of the bone-patellar tendon-bone graft anterior cruciate ligament-reconstructed leg versus quadriceps-dominant strategy of the contralateral intact leg during high-intensity exercise in male athletes. Arthroscopy. 2012;28(9):1262-1270. [DOI] [PubMed] [Google Scholar]
- 55. Pfeiffer TR, Kanakamedala AC, Herbst E, et al. Female sex is associated with greater rotatory knee laxity in collegiate athletes. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1319-1325. [DOI] [PubMed] [Google Scholar]
- 56. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320-1325.e6. [DOI] [PubMed] [Google Scholar]
- 57. Raines B, Naclerio E, Sherman S. Management of anterior cruciate ligament injury? What’s in and what’s out? Indian J Orthop. 2017;51(5):563-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Roos H, Ornell M, Gärdsell P, Lohmander Ls, Lindstrand A. Soccer after anterior cruciate ligament injury - an incompatible combination? A national survey of incidence and risk factors and a 7-year follow-up of 310 players. Acta Orthop Scand. 1995;66(2):107-112. [DOI] [PubMed] [Google Scholar]
- 59. Salem HS, Varzhapetyan V, Patel N, Dodson CC, Tjoumakaris FP, Freedman KB. Anterior cruciate ligament reconstruction in young female athletes: patellar versus hamstring tendon autografts. Am J Sports Med. 2019;47(9):2086-2092. [DOI] [PubMed] [Google Scholar]
- 60. Sandon A, Engström B, Forssblad M. High risk of further anterior cruciate ligament injury in a 10-year follow-up study of anterior cruciate ligament-reconstructed soccer players in the Swedish National Knee Ligament Registry.J Arthrosc Relat Surg. 2020;36(1):189-195. [DOI] [PubMed] [Google Scholar]
- 61. Sandon A, Werner S, Forssblad M. Factors associated with returning to football after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2514-2521. [DOI] [PubMed] [Google Scholar]
- 62. Schiffner E, Latz D, Grassmann JP, et al. Anterior cruciate ligament ruptures in German elite soccer players: epidemiology, mechanisms, and return to play. Knee. 2018;25(2):219-225. [DOI] [PubMed] [Google Scholar]
- 63. Shakked R, Weinberg M, Capo J, Jazrawi L, Strauss E. Autograft choice in young female patients: patella tendon versus hamstring. J Knee Surg. 2017;30(3):258-263. [DOI] [PubMed] [Google Scholar]
- 64. Shelbourne KD, Sullivan AN, Bohard K, Gray T, Urch SE. Return to basketball and soccer after anterior cruciate ligament reconstruction in competitive school-aged athletes. Sports Health. 2009;1(3):236-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. [DOI] [PubMed] [Google Scholar]
- 66. Sonnery-Cottet B, Saithna A, Cavalier M, et al. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI study group. Am J Sports Med. 2017;45(7):1547-1557. [DOI] [PubMed] [Google Scholar]
- 67. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 68. Sugimoto D, Myer GD, Bush HM, Klugman MF, Medina McKeon JM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47(6):714-723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sutton KM, Bullock JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg. 2013;21(1):41-50. [DOI] [PubMed] [Google Scholar]
- 70. The female ACL: why is it more prone to injury? J Orthop. 2016;13(2):A1-A4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Thomson A, Einarsson E, Hansen C, Bleakley C, Whiteley R. Marked asymmetry in vertical force (but not contact times) during running in ACL reconstructed athletes <9 months post-surgery despite meeting functional criteria for return to sport. J Sci Med Sport. 2018;21(9):890-893. [DOI] [PubMed] [Google Scholar]
- 72. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Soft. 2010;36(3):1-48. [Google Scholar]
- 73. Volpi P, Bisciotti GN, Chamari K, Cena E, Carimati G, Bragazzi NL. Risk factors of anterior cruciate ligament injury in football players: a systematic review of the literature. Muscles Ligaments Tendons J. 2016;6(4):480-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Waldén M, Hägglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50(12):744-750. [DOI] [PubMed] [Google Scholar]
- 75. Waldén M, Hägglund M, Werner J, Ekstrand J. The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee Surg Sports Traumatol Arthrosc. 2011;19(1):3-10. [DOI] [PubMed] [Google Scholar]
- 76. Warner SJ, Smith MV, Wright RW, Matava MJ, Brophy RH. Sport-specific outcomes after anterior cruciate ligament reconstruction. J Arthrosc Relat Surg. 2011;27(8):1129-1134. [DOI] [PubMed] [Google Scholar]
- 77. Welling W, Benjaminse A, Lemmink K, Dingenen B, Gokeler A. Progressive strength training restores quadriceps and hamstring muscle strength within 7 months after ACL reconstruction in amateur male soccer players. Phys Ther Sport. 2019;40:10-18. [DOI] [PubMed] [Google Scholar]
- 78. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Yoo JC, Ahn JH, Lee SH, Yoon YC. Increasing incidence of medial meniscal tears in nonoperatively treated anterior cruciate ligament insufficiency patients documented by serial magnetic resonance imaging studies. Am J Sports Med. 2009;37(8):1478-1483. [DOI] [PubMed] [Google Scholar]
- 80. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Return to sport after anterior cruciate ligament reconstruction in professional soccer players. Knee. 2014;21(3):731-735. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_19417381231160167 for Clinical Outcomes After ACL Reconstruction in Soccer (Football, Futbol) Players: A Systematic Review and Meta-Analysis by Ian S. Hong, Lauren A. Pierpoint, Justin E. Hellwinkel, Alexander N. Berk, Jonathan M. Salandra, Joshua D. Meade, Dana P. Piasecki, James E. Fleischli, Christopher S. Ahmad, David P. Trofa and Bryan M. Saltzman in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-2-sph-10.1177_19417381231160167 for Clinical Outcomes After ACL Reconstruction in Soccer (Football, Futbol) Players: A Systematic Review and Meta-Analysis by Ian S. Hong, Lauren A. Pierpoint, Justin E. Hellwinkel, Alexander N. Berk, Jonathan M. Salandra, Joshua D. Meade, Dana P. Piasecki, James E. Fleischli, Christopher S. Ahmad, David P. Trofa and Bryan M. Saltzman in Sports Health: A Multidisciplinary Approach