Abstract
Short-term or long-term CVCs are now considered the standard of practice for the administration of chemotherapy, fluid therapy, antibiotic therapy, and parenteral nutrition. Central venous access catheters are broadly divided into tunneled or non-tunneled catheters. Tunneled catheters can be further subdivided into totally implanted and totally not implanted devices. Device selection generally depends on various factors such as availability of peripheral veins, expected duration of therapy, and desired flow rate. Ultrasound-guided access is the safest technique for central venous access compared to the landmark technique and departments should strive to for a 100% ultrasound guided access. This review gives a basic overview of the differences of CVC catheters including PICCs, Hickman-catheters and port-catheters along with the criteria for CVC selection. It will also describe technical tips on placement of CVCs. Finally, it aims to highlight complications which are associated with CVC placement and options to treat or prevent them.
Introduction
The first insertion of a central venous catheter (CVC) on a human subject was first reported by the German physician Werner Forssmann in a self-experimentation attempt in 1929. 1 In 1953, the Swedish Sven-Ivar Seldinger described a technique that facilitates catheter placement into the arterial system over a guide-wire, that was later also used in the venous system and body cavities. 2 Later, in the 1970s, Broviac et al 3 and Hickman et al 4 designed the first long-term CVCs, and in 1982, Niederhuber et al 5 first reported the insertion of a totally implanted venous port system.
Short-term or long-term CVCs are now considered the standard of practice for various central venous therapies, such as chemotherapy, fluid administration, antibiotic therapy, and parenteral nutrition. In fact, central venous access is one of the most common procedures today, and it is estimated that 8% of hospitalized patients are in need of a CVC. 6 Each year, more than 5 million CVCs are placed in the US alone. 7
Catheter types
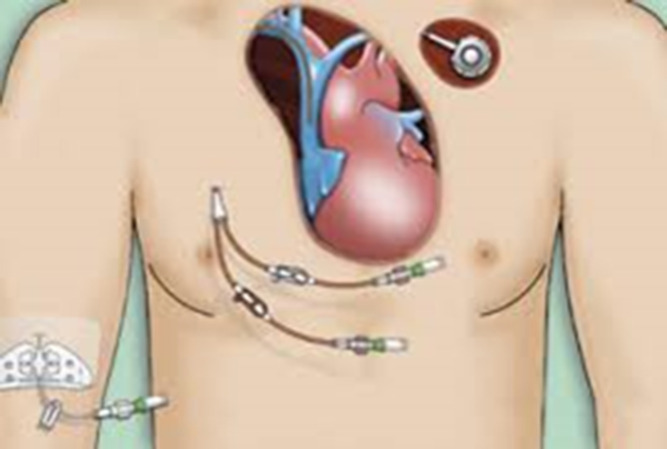
Central venous access catheters are broadly divided in tunneled or non-tunneled catheters (Figure 1). Tunneled catheters can be further subdivided in totally implanted and not totally implanted devices.
Figure 1.
Artistic representation of three common CVCs, from left to right, PICC, Hickman and port. The tip of the CVC in SVC is shown at the center.
Non-tunneled catheters include conventional CVCs, Swan-Ganz catheters, acute dialysis catheters and peripherally inserted central catheters (PICCs). Tunneled catheters are Hickman (double lumen) or Broviac (single lumen) catheters, permanent dialysis catheters, and totally implanted ports. Table 1
Table 1.
Most common catheter types and characteristics
| Catheter type | Size (Fr) | Lumens | Access vein | Tunnel | Totally implanted | Intended dwell time |
|---|---|---|---|---|---|---|
| Conventional | 7–8 | 1–3 | SCV, IJV, CFV | No | No | 3 weeks |
| PICC | 3–6 | 1–3 | BV, BrV, CV | No | No | 6 months |
| Hickman | 7–9 | 2 (1: Broviac) | IJV, SCV, CFV | Yes | No | Years |
| Port | 5–9 | Usually 1, up to 2 | IJV, SCV, CFV | Yes | Yes | Years |
Device selection depends on various factors such as availability of peripheral veins, expected duration of therapy, and desired flow rate. But factors such as availability in an emergency, experience of the health-care professionals with the device, concomitant diseases, and patient preference can also play a role.
As a general rule, a non-tunneled CVC is indicated for a treatment duration of 2–3 weeks. PICCs can generally outlast a conventional CVC and are commonly used for treatment as long as 3 months. Tunneled catheters are expected to be used for more than one month and even for years. Implantable ports are tunneled devices that can last for years and have the added benefit of easy concealment, since they are totally implanted, giving a more discreet appearance. Ports can be placed in the chest or arm, 8,9 A disadvantage of ports is the need for percutaneous access using a special needle, under sterile conditions. 10 On one hand, access is somewhat painful; on the other hand, all flow is directed through the 19–20G needle, which limits the rate of infusion.
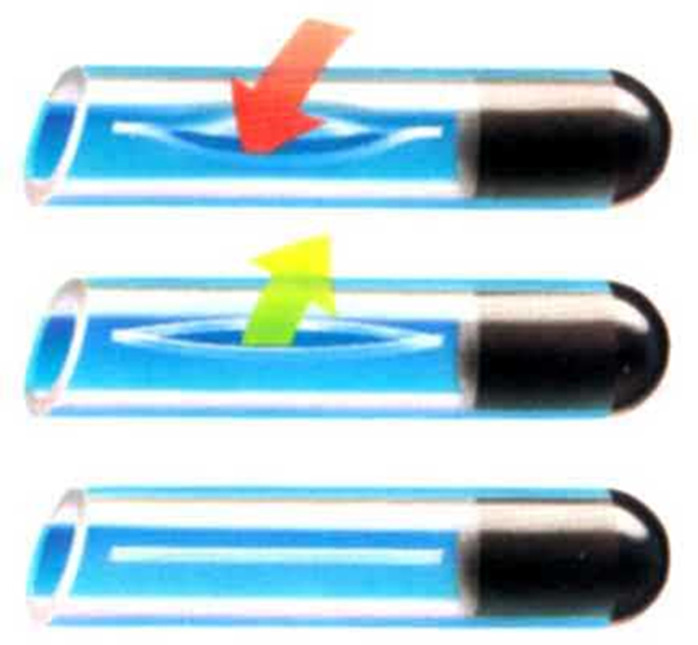
There is a great variety of CVCs offered to cover different needs. Special information on CT- and MR-compatibility can be can be found in the instructions for use, as can the flow rates and maximum pressure for contrast administration. The tip of the CVC may have different configurations which is especially true for dialysis catheters. Some catheter tips are not open-ended, but have a valve, that allows the use of heparin free flush solution. The most commonly used valve, which is essentially a slit in the sidewall of a catheter with a closed end is Groshong valve (Figure 2).
Figure 2.
A Groshong valve at the tip of a CVC.
Contraindications (Relative)
There are no absolute contraindications for central venous catheters placement. Relative contraindications rely upon the urgency of the indication and the presence of an alternative for venous access.
While major bleeding after central venous catheterization is uncommon, moderate-to-severe bleeding diathesis is considered a relative contraindication.
In emergency situations, venous access may be performed in spite of coagulopathy, and the safety of standard and large-bore non-tunneled catheter placement in such circumstances has been documented, 11,12 As a rule of thumb, non-tunneled catheterization at access sites that are easy to control by manual pressure in case of bleeding should be of preference in patients with coagulopathy. In those cases, the subclavian access should be our last choice, due to lack of the ability to safely monitor or compress the venipuncture site. Real-time ultrasound guidance may reduce the amount of venipunctures needed for a successful access and minimize bleeding complication rates. 13
Regarding coagulation factors – platelet count, international normalized ratio (INR), and partial thromboplastin time – there appear to be no cut-off values for safe central venous catheterization. There are no data to support routine correction of coagulopathy prior to CVC insertion, contrary to popular concern and practice. 14,15 There is evidence that thrombocytopenia may be a greater risk than prolonged clotting times, 16,17 Based on available retrospective studies, preprocedural correction for platelet count>20×109 l−1 and INR<3 13 is not indicated For more severe coagulopathy (e.g., platelet count<20×109 l−1 and INR>3), consider administration of blood products (e.g., platelets, fresh-frozen plasma) if time permits.
Access site
Each clinical situation should be individualized for the most appropriate site for central venous access. Important factors to consider may be operator skill, ultrasound findings and availability, relevant anatomy (e.g., easily identified landmarks, documented venous obstruction, presence of lymphedema), factors that increase access risk (e.g., coagulopathy, pulmonary disease), anticipated intravenous therapy needed, frequency and duration of catheter usage, 18–22 There are inherent specific advantages and disadvantages in various access sites, such as jugular, subclavian, or femoral, which determine the risk of varius complications, such as the risk of catheter-related infection. 23 Complications can be minimized with experience of clinician inserting the catheter, use of ultrasound-guided access, adherence to maximum sterile precautions, and training of nurses and related professionals involved in catheter care. 24 According to the guidelines issued by the United States Centers for Disease Control and Prevention (CDC), the femoral access should generally be avoided.
Non-tunneled catheter placement
Non-tunneled percutaneous CVCs can be generally placed at the bedside, while tunneled catheters and ports are preferably inserted in an interventional radiology suite or operating room with use of fluoroscopic guidance.
Before every CVC insertion, informed consent should be given from the patient and/or legal guardian, with the exception of emergency situations where it is implied.
Issues covered in consent include indications, benefits, plan, and potential complications of the procedure (e.g., pneumothorax), the potential need for a second procedure, such as chest tube insertion in case of a pneumothorax.
Continuous cardiac rhythm and pulse oximetry monitoring are essential during central venous access procedures. The room should be equipped with supplemental oxygen in case it becomes necessary, and, for some patients, nasal oxygen administration may be prudent before covering the patient’s head with drapes.
Patient positioning
Patient positioning depends on cardiopulmonary stability and should ensure patient’s and operator’s comfort. Ideally, positioning should help maximize the diameter of the vein to be punctured. Contrary to popular belief, Trendelenburg position is not always necessary or feasible for jugular and subclavian access despite the fact that it may reduce the risk of venous air embolism, 25–29 For high-risk patients, anesthesia with airway control may be required for the safe completion of a central venous access procedure.
Sterile technique
Maximum sterile precautions are indicated for elective and emergency central venous access procedures, in order to reduce infectious complications. These include the use of long enough sterile drapes to cover the entire patient, placing a sterile cover over the ultrasound probe, hand surgical antisepsis, wearing a long-sleeved sterile gown, sterile gloves, a surgical mask and cap. 30–35
Site preparation - Skin antisepsis
Before skin antisepsis, the area should be prepared with hair clipping which is preferable to shaving. 36 The whole area should be prepped using a chlorhexidine antiseptic solution with alcohol and sufficient time should be allowed for it to dry before 30–35 draping the patient. Use of chlorhexidine-based solutions (>0.5% chlorhexidine preparation with alcohol) is desirable compared to aqueous or alcohol-based povidone-iodine, because chlorhexidine offeres increased protection against catheter colonization and catheter-related bloodstream infection (CR-BSI). 37–39
Although common, use of prophylactic antibiotics prior to CVC placement is not supported by literature. A meta-analysis comparing prophylactic antibiotic coverage versus no coverage before totally implanted venous access devices placement, failed to show any significant difference in infection rates. 40
Analgesia and sedation
For CVC placement as for all procedures, effort number of measures should be taken to increase patient cooperation and comfort. Those may include local anesthetic use (topical, infiltrated) and minimal or deeper sedation, in case it is needed. Topical anesthetics may be helpful, particularly in children.
Venous access
It cannot be stressed enough that ultrasound guided access is the safest technique for central venous access compared to the landmark technique. Departments should strive to for a 100% ultrasound guided access, 41,42 Use of micropuncture access sets can minimize the risk of access-related complications. A very advantageous access technique for the IJV, especially for patients with short necks or children is the “lateral in-plane technique”. 43
Femoral vein access can be used as an alternative when standard access veins are inaccessible or cannot be recanalized. It is always useful to perform a preoperative ultrasound assessment of the vein of the proposed access site, and of the opposite side, if feasible. Other options reported include transcaval or transhepatic central venous access.
Intraprocedural complications
Operators should be aware of the possibility of aspiration causing venous air embolism due to negative venous pressure. Risk can be minimized by decreasing the time for aspiration by closing the opening of the peel-away sheath with a finger after removing the dilator or by tilting the table to a Trendelenburg’s position so that the head is lower than the right atrium. Venous pressure can be increased by application of the Valsalva maneuver, but can prove counterproductive if the patient cannot follow breathing commands. Some manufacturers have equipped larger peel-away sheaths with valves.
Arterial puncture should be recognized promptly, before introducing larger sheaths or the catheter. When the sheath or catheter is actually in the artery, manual compression usually is sufficient; if the site is not suitable for compression, closure devices, balloon-assisted removal, or surgery can be considered.
Pneumothorax is a rare occurrence using ultrasound-guided access technique and rarely can lead to cardiopulmonary instability. Careful advancement of the access guide-wire under fluoroscopy, ideally in the IVC, will prevent most cases of arrhythmia. In case, supraventricular tachycardia develops compression of the carotid bifurcation can be tried before medical treatment.Tables 2 and 3.
Table 2.
Peri-interventional complications for jugular/subclavian approach; complication rates for peripheral access are smaller 44
| Complication | Incidence |
|---|---|
| Pneumothorax | 1–3% |
| Hemothorax | 1% |
| Hematoma | 1–3% |
| Perforation | 0.5–1% |
| Air embolism | 1% |
| Wound dehiscence | 1% |
| Procedure-induced sepsis | 1–3% |
| Thrombosis | 1–5% |
Table 3.
Early (within 30d) and late complications. 45,46 Complications per 1,000 catheter-days
| CVC | Tunneled CVC | PICC | Port | |
|---|---|---|---|---|
| Complication | 1.08 | 1.01 | 2.02 | 0.52 |
| Systemic infection | 0.22 | 0.34 | 0.11 | 0.16 |
| Local infection | 0.35 | 0.36 | 0.25 | 0.14 |
| Thrombotic dysfunction | 0.08 | 0.06 | 0.40 | 0.06 |
| Non-thrombotic dysfunction | 0.39 | 0.23 | 0.98 | 0.16 |
| Other | 0.04 | 0.02 | 0.00 | 0.00 |
Catheter tip placement
The ideal tip position of central venous catheters is a subject of continuous controversy. 47 Imaging observation shows that the catheter tip of tunneled lines moves head wards with the patient upright. 44 Arm VADs, on the other hand, tend to move catheter tip inwards with arm adduction and elbow flexion. 45 A good compromise for CVC tip positioning is one vertebral body-height distance below the carina in the recumbent patient, minimizing the risk for thrombosis and arrhythmia. An exception to this rule would be neonates (where the carina level would be a safer option for tip positioning) and hemodialysis catheters (where the catheter should enter the RA for better function). Manufacturers have introduced various techniques for correct placement of catheter tip based on ECG guidance. 46
Specific procedure details
Conventional CVCs
Conventional CVCs are usually 2- or 3-lumen 7–8 Fr, 20–30 cm in length catheters. Conventional CVCs are placed using the Seldinger technique, preferably using real-time ultrasound guidance, in the IJV, SCV, and common femoral vein. Tunneling is possible as a more advanced version of the conventional CVC technique. 48 More expensive catheters may have additional antithrombotic antimicrobial coatings and/or power injection capability, a very useful feature that allows them to be connected to a contrast power injector used for contrast medium injection during a CT scan.
PICC placement
Peripherally inserted central catheters or PICCs use a venous access in the middle third of the inner aspect of the arm. The difference in patient placement is that the arm should lye extended on an arm table with the forearm supinated. Using a tourniquet, we interrogate with ultrasound the arm veins on both sides working from the elbow up. Important factors to consider are vein size and compressibility (Rapid Peripheral Vein Assesment – RaPeVA). 44
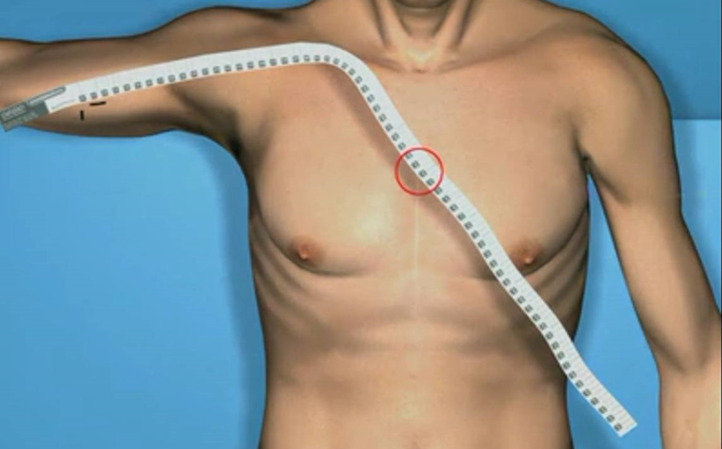
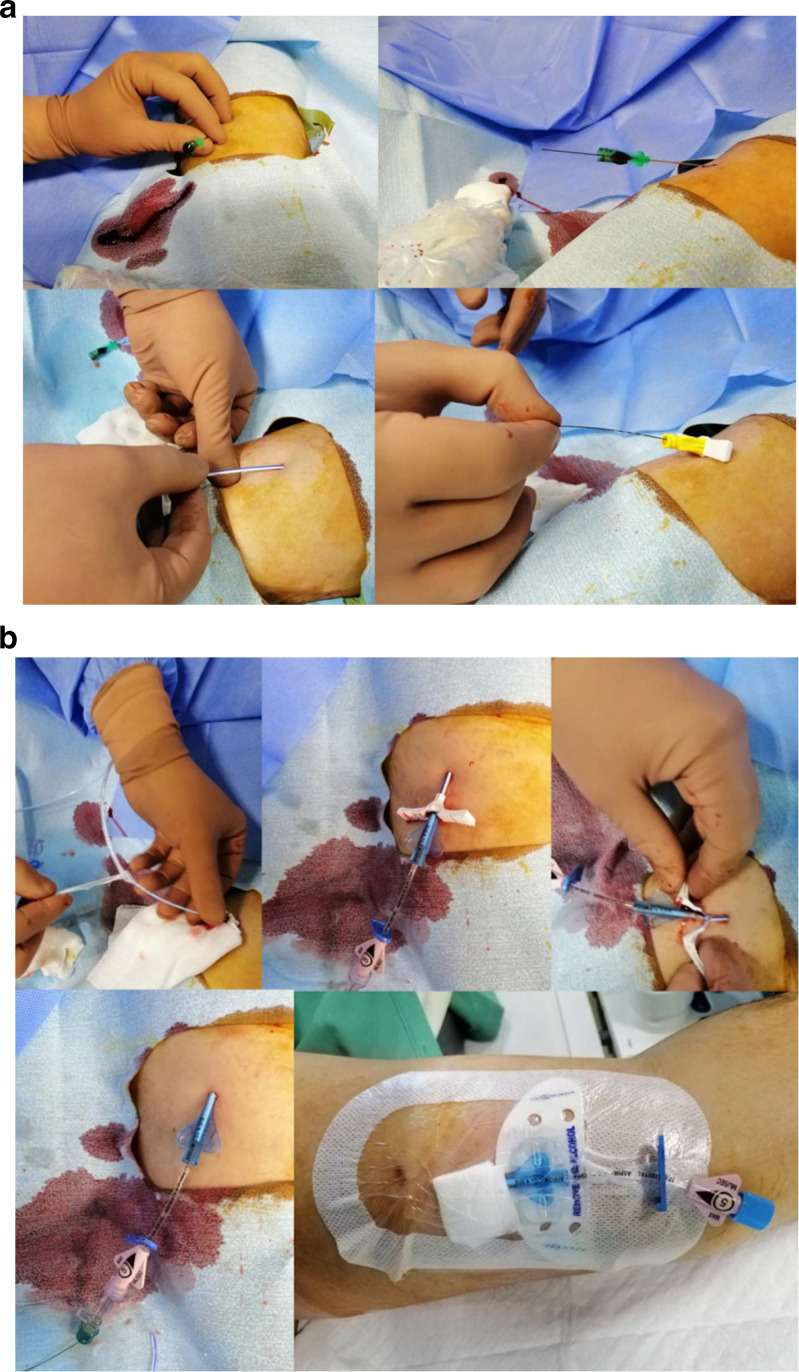
The non-dominant arm is selected, if feasible. The vein access of choice of is the basilic vein, due to its straight course to the axillary vein and its distance from the artery, followed by the brachial veins. Cephalic vein is rarely a good choice, due to its superficial location, angled course to the subclavian and possible use for an AV fistula in the future. Measurement of a PICC’s length is usually carried out with the arm extended, following the anticipated course of the veins to the third intercostal (Figure 3). The vein is accessed in the out-of-plane view and the sheath is introduced over the guide-wire. After removing the dilator and wire, the catheter is threaded to the desirable position (Figure 4). When the catheter is directed in the IJV, ipsilateral head turning and supraclavicular pressure will help position it in the SVC. Manufacturers have developed devices for PICC placement without fluoroscopy based on ECG tracing52. Simple traction and compression of the access point is enough for PICC removal.
Figure 3.
PICC measurement from access site to the 3rdintercostal.
Figure 4.
Various stages of PICC placement. A) Placing the peel-away sheath, B) Inserting the catheter.
Hickman catheter placement
The respective hemithorax is prepared. A low jugular access may help to improve the functional and cosmetic result with different techniques reported. 9,47,48 Alternative access sites include but are not limited to the IJV higher in the neck, the EJV, the brachiocephalic vein, and the supraclavicular and infraclavicular SCV. The catheter is tunneled and the subcutaneous cuff is placed 2–3 fingers from the exit site for easier removal. The peel-away sheath is introduced over the guide wire. The catheter is placed over the chest, following the anticipated course of the SVC and cut over the third intercostal, or one vertebral body height below the carina using fluoroscopy (Figures 5 and 6).
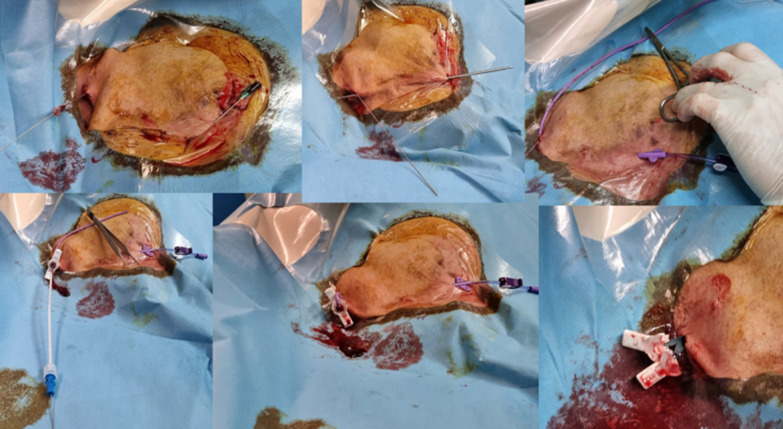
Figure 5.
Stages of Hickman catheter placement.
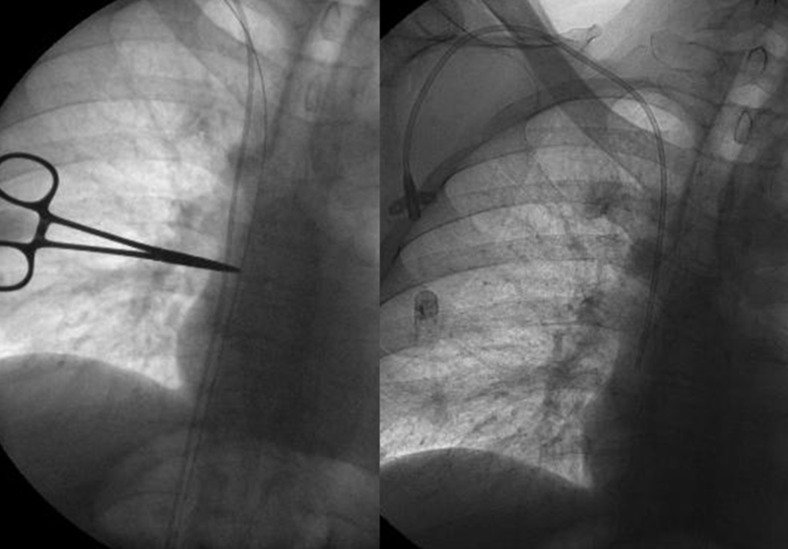
Figure 6.
Hickman trimming using fluoroscopy (left), placing the catheter over the patient’s chest and marking the 3rd intercostal with a hemostat. Final fluoroscopic result (right).
Port catheter placement
Preparation and ultrasound-guided venous access are the same with a Hickman catheter.
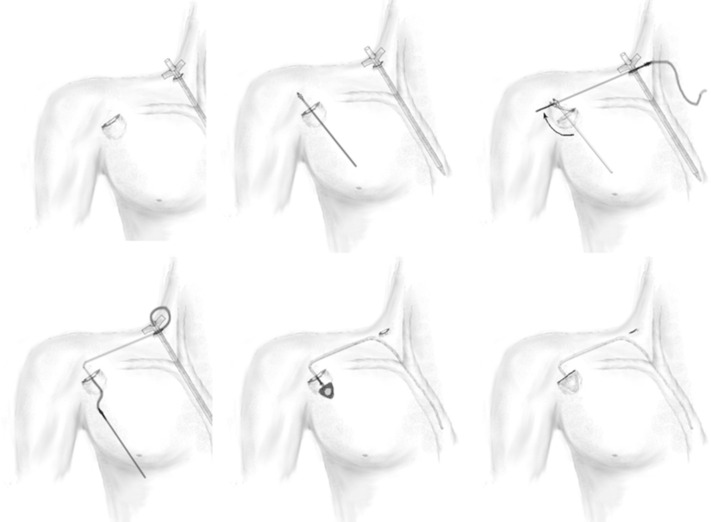
There are several variations of placing the port pouch. A more discreet option follows the skin tension lines about one to two fingers medial to the deltoid crease and one to two fingers caudal to the clavicular bone. A subcutaneous pouch is created caudal to the incision, making sure that the incision will not overlay the port puncture area. The dissection is made above the pectoralis major aponeurosis. We propose the “L-shaped” tunneling technique, for avoidance of catheter kinking. 49 The incision and pouch of the port should be as narrow as possible for a snug fit, ensuring a better cosmetic result and good hemostasis, avoiding skin tension above the port (Figures 7–9). Suturing the port to the aponeurosis to prevent rotation within the pouch is not usually necessary.
Figure 7.
Stages of port placement using the “L-shaped tunneling technique”
Figure 8.
Immediate postoperative result of a port placed using the “L-shaped tunneling technique”
Figure 9.
The respective fluoroscopic image of patient in Fig. 6 (right). Compare with a port placed with conventional technique on the left.
After peeling of the sheath, the catheter tip is positioned using fluoroscopy and the port is connected. While positioning the tip, the effect of an upright position on anatomy should be anticipated. Before pouch suturing, the port is aspirated and flushed.
Particular patient anatomies may necessitate applying gentle caudal traction to the breast for the entire implantation, moving the incision to a site in the mid-clavicular line just below the clavicle or dissecting the subcutaneous fat only about 1 cm deep, for easier port access.
Arm port catheter placement
Conventional technique for placing arm ports (also called “PICC ports”) involves accessing an arm vein in a manner similar to PICC placement (usually upper Basilic, upper Brachial or Axillary without a tourniquet). Then, the line is tunneled lower in the arm where a pouch is created. 50,51 One must be careful not to damage the ulnar and median nerve and to use a bony counterpart under the port for puncture support.
Advanced techniques for arm VAD placement
Specifically for arm VADs, the Arm-to-Chest Tunneling technique (ACT) has been described. 9 It is a technique for placement of arm VADs (ports, PICCs and cuffed lines) using IJV access, particularly useful for patients with occluded or small arm veins, or even children. This technique has the advantages that it is easier, quicker, and less-expensive than, for example, trying a recanalization of an occluded subclavian vein using a glide wire. ACT is the only method the authors use for arm port placement.
Conclusion
Central venous catheters are an essential service for any modern hospital. The operator should be familiar with placement, complication management, and use of different types of central venous catheters following the motto “the right catheter for the right patient”. Strict sterile technique, adoption of ultrasound access for all cases, and attention to detail are the mainstay for a successful venous access.
Contributor Information
Elias Kehagias, Email: eliaskmd@gmail.com.
Nikolaos Galanakis, Email: eliaskmd@gmail.com.
Dimitrios Tsetis, Email: eliaskmd@gmail.com.
REFERENCES
- 1. Forssmann W. Die sondierung des rechten herzens. [Probing of the right heart]. Klin Wochenschr 1929; 8: 2085–87. doi: 10.1007/BF01875120 [DOI] [Google Scholar]
- 2. SELDINGER SI. Catheter replacement of the needle in percutaneous Arteriography: a new technique. Acta Radiol 1953; 39: 368–76. doi: 10.3109/00016925309136722 [DOI] [PubMed] [Google Scholar]
- 3. Broviac JW, Cole JJ, Scribner BH. A silicone rubber atrial catheter for prolonged parenteral Alimentation. Surgery, Gynecology & Obstetrics 1973; 136: 602–6. [PubMed] [Google Scholar]
- 4. Hickman RO, Buckner CD, Clift RA, Sanders JE, Stewart P, Thomas ED. A modified right atrial catheter for access to the venous system in marrow transplant recipients. Surgery, Gynecology & Obstetrics 1979; 148: 871–75. [PubMed] [Google Scholar]
- 5. Niederhuber JE, Ensminger W, Gyves JW, Liepman M, Doan K, Cozzi E. Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery 1982; 92: 706–12. [PubMed] [Google Scholar]
- 6. Ruesch S, Walder B, Tramèr MR. Complications of central venous catheters: internal jugular versus Subclavian access--a systematic review. Crit Care Med 2002; 30: 454–60. doi: 10.1097/00003246-200202000-00031 [DOI] [PubMed] [Google Scholar]
- 7. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 2003; 348: 1123–33. doi: 10.1056/NEJMra011883 [DOI] [PubMed] [Google Scholar]
- 8. Kehagias E, Tsetis D. The "arm-to-chest Tunneling" technique: a modified technique for arm placement of Implantable ports or central catheters. J Vasc Access 2019; 20: 771–77. doi: 10.1177/1129729819826039 [DOI] [PubMed] [Google Scholar]
- 9. Annetta MG, Ostroff M, Marche B, Emoli A, Musarò A, Celentano D, et al. Chest-to-arm tunneling: a novel technique for medium/long term venous access devices. J Vasc Access 2023; 24: 92–98. doi: 10.1177/11297298211026825 [DOI] [PubMed] [Google Scholar]
- 10. Kehagias E, Tsetis D. Proper technique of port puncture in the deltopectoral groove: the `` Port pinning technique.'' J Vasc Access 2017; 18: FB002E19-43F8-4F4C-A321-7601E5F61463. doi: 10.5301/jva.5000635 [DOI] [PubMed] [Google Scholar]
- 11. Frykholm P, Pikwer A, Hammarskjöld F, Larsson AT, Lindgren S, Lindwall R, et al. Clinical guidelines on central venous catheterisation. Acta Anaesthesiol Scand 2014; 58: 508–24. doi: 10.1111/aas.12295 [DOI] [PubMed] [Google Scholar]
- 12. Weigand K, Encke J, Meyer FJ, Hinkel UP, Munder M, Stremmel W, et al. Low levels of prothrombin time (Inr) and platelets do not increase the risk of significant bleeding when placing central venous catheters*. Med Klin 2009; 104: 331–35. doi: 10.1007/s00063-009-1070-2 [DOI] [PubMed] [Google Scholar]
- 13. Tercan F, Ozkan U, Oguzkurt L. US-guided placement of central vein catheters in patients with disorders of hemostasis. European Journal of Radiology 2008; 65: 253–56. doi: 10.1016/j.ejrad.2007.04.002 [DOI] [PubMed] [Google Scholar]
- 14. Estcourt LJ, Desborough M, Hopewell S, Doree C, Stanworth SJ. Comparison of different platelet transfusion thresholds prior to insertion of central lines in patients with thrombocytopenia. Cochrane Database Syst Rev 2015; 2015(): CD011771. doi: 10.1002/14651858.CD011771.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hall DP, Lone NI, Watson DM, Stanworth SJ, Walsh TS, Intensive Care Study of Coagulopathy (ISOC) Investigators . Factors associated with prophylactic plasma transfusion before vascular catheterization in non-bleeding critically ill adults with prolonged prothrombin time: a case-control study. Br J Anaesth 2012; 109: 919–27. doi: 10.1093/bja/aes337 [DOI] [PubMed] [Google Scholar]
- 16. Doerfler ME, Kaufman B, Goldenberg AS. Central venous catheter placement in patients with disorders of hemostasis. Chest 1996; 110: 185–88. doi: 10.1378/chest.110.1.185 [DOI] [PubMed] [Google Scholar]
- 17. Polderman KH, Girbes AJ. Central venous catheter use. part 1: mechanical complications. Intensive Care Med 2002; 28: 1–17. doi: 10.1007/s00134-001-1154-9 [DOI] [PubMed] [Google Scholar]
- 18. Heckmann JG, Lang CJ, Kindler K, Huk W, Erbguth FJ, Neundörfer B. Neurologic manifestations of cerebral air embolism as a complication of central venous catheterization. Crit Care Med 2000; 28: 1621–25. doi: 10.1097/00003246-200005000-00061 [DOI] [PubMed] [Google Scholar]
- 19. Toung TJ, Rossberg MI, Hutchins GM. Volume of air in a lethal venous air embolism. Anesthesiology 2001; 94: 360–61: 360. doi: 10.1097/00000542-200102000-00031 [DOI] [PubMed] [Google Scholar]
- 20. Brull SJ, Prielipp RC. Vascular air embolism: A silent hazard to patient safety. J Crit Care 2017; 42: 255–63. doi: 10.1016/j.jcrc.2017.08.010 [DOI] [PubMed] [Google Scholar]
- 21. Flanagan JP, Gradisar IA, Gross RJ, Kelly TR. Air Embolus--a lethal complication of Subclavian Venipuncture. N Engl J Med 1969; 281: 488–89. doi: 10.1056/NEJM196908282810907 [DOI] [PubMed] [Google Scholar]
- 22. Gordy S, Rowell S. Vascular air embolism. Int J Crit Illn Inj Sci 2013; 3: 73–76. doi: 10.4103/2229-5151.109428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McCarthy CJ, Behravesh S, Naidu SG, Oklu R. Air embolism: practical tips for prevention and treatment. J Clin Med 2016; 5: : 93. doi: 10.3390/jcm5110093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bowdle A. Vascular complications of central venous catheter placement: evidence-based methods for prevention and treatment. Journal of Cardiothoracic and Vascular Anesthesia 2014; 28: 358–68. doi: 10.1053/j.jvca.2013.02.027 [DOI] [PubMed] [Google Scholar]
- 25. Guilbert M-C, Elkouri S, Bracco D, Corriveau MM, Beaudoin N, Dubois MJ, et al. Arterial trauma during central venous catheter insertion: case series, review and proposed algorithm. J Vasc Surg 2008; 48: 918–25. doi: 10.1016/j.jvs.2008.04.046 [DOI] [PubMed] [Google Scholar]
- 26. Dixon OGB, Smith GE, Carradice D, Chetter IC. A systematic review of management of inadvertent arterial injury during central venous catheterisation. J Vasc Access 2017; 18: 97–102. doi: 10.5301/jva.5000611 [DOI] [PubMed] [Google Scholar]
- 27. Nicholson T, Ettles D, Robinson G. Managing inadvertent arterial catheterization during central venous access procedures. Cardiovasc Intervent Radiol 2004; 27: 21–25. doi: 10.1007/s00270-003-0043-8 [DOI] [PubMed] [Google Scholar]
- 28. Kander T, Frigyesi A, Kjeldsen-Kragh J, Karlsson H, Rolander F, Schött U. Bleeding complications after central line insertions: relevance of pre-procedure coagulation tests and institutional transfusion policy. Acta Anaesthesiol Scand 2013; 57: 573–79. doi: 10.1111/aas.12075 [DOI] [PubMed] [Google Scholar]
- 29. Hall DP, Estcourt LJ, Doree C, Hopewell S, Trivella M, Walsh TS. Plasma transfusions prior to insertion of central lines for people with abnormal coagulation. Cochrane Database Syst Rev 2016; 9(): CD011756. doi: 10.1002/14651858.CD011756.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Oliver WC Jr, Nuttall GA, Beynen FM, Raimundo HS, Abenstein JP, Arnold JJ. The incidence of artery puncture with central venous cannulation using a modified technique for detection and prevention of arterial cannulation. J Cardiothorac Vasc Anesth 1997; 11: 851–55. doi: 10.1016/s1053-0770(97)90119-1 [DOI] [PubMed] [Google Scholar]
- 31. Boyd R, Saxe A, Phillips E. Effect of patient position upon success in placing central venous catheters. Am J Surg 1996; 172: 380–82. doi: 10.1016/s0002-9610(96)00198-5 [DOI] [PubMed] [Google Scholar]
- 32. Tripathi M, Dubey PK, Ambesh SP. Direction of the J-tip of the guidewire, in Seldinger technique, is a significant factor in misplacement of subclavian vein catheter: a randomized, controlled study. Anesthesia & Analgesia 2005; 100: 21–24. doi: 10.1213/01.ANE.0000139349.40278.77 [DOI] [PubMed] [Google Scholar]
- 33. Lefrant J-Y, Muller L, De La Coussaye J-E, Prudhomme M, Ripart J, Gouzes C, et al. Risk factors of failure and immediate complication of Subclavian vein catheterization in critically ill patients. Intensive Care Med 2002; 28: 1036–41. doi: 10.1007/s00134-002-1364-9 [DOI] [PubMed] [Google Scholar]
- 34. Pittiruti M, Lamperti M. Late cardiac Tamponade in adults secondary to tip position in the right Atrium: an urban legend? A systematic review of the literature. J Cardiothorac Vasc Anesth 2015; 29: 491–95. doi: 10.1053/j.jvca.2014.05.020 [DOI] [PubMed] [Google Scholar]
- 35. Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different Intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc 2006; 81: 1159–71. doi: 10.4065/81.9.1159 [DOI] [PubMed] [Google Scholar]
- 36. Schiffer CA, Mangu PB, Wade JC, Camp-Sorrell D, Cope DG, El-Rayes BF, et al. Central venous catheter care for the patient with cancer: American Society of clinical oncology clinical practice guideline. JCO 2013; 31: 1357–70. doi: 10.1200/JCO.2012.45.5733 [DOI] [PubMed] [Google Scholar]
- 37. Ng PK, Ault MJ, Ellrodt AG, Maldonado L. Peripherally inserted central catheters in general medicine. Mayo Clin Proc 1997; 72: 225–33. doi: 10.4065/72.3.225 [DOI] [PubMed] [Google Scholar]
- 38. Pongruangporn M, Ajenjo MC, Russo AJ, McMullen KM, Robinson C, Williams RC, et al. Patient- and device-specific risk factors for peripherally inserted central venous catheter-related bloodstream infections. Infect Control Hosp Epidemiol 2013; 34: 184–89. doi: 10.1086/669083 [DOI] [PubMed] [Google Scholar]
- 39. Chopra V, O’Horo JC, Rogers MAM, Maki DG, Safdar N. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 2013; 34: 908–18. doi: 10.1086/671737 [DOI] [PubMed] [Google Scholar]
- 40. Johnson E, Babb J, Sridhar D. Routine antibiotic prophylaxis for totally implantable venous access device placement: meta-analysis of 2,154 patients. J Vasc Interv Radiol 2016; 27: 339–43. doi: 10.1016/j.jvir.2015.11.051 [DOI] [PubMed] [Google Scholar]
- 41. Denys BG, Uretsky BF, Reddy PS. Ultrasound-Assisted cannulation of the internal jugular vein. A prospective comparison to the external landmark-guided technique. Circulation 1993; 87: 1557–62. doi: 10.1161/01.cir.87.5.1557 [DOI] [PubMed] [Google Scholar]
- 42. Skolnick ML. The role of sonography in the placement and management of jugular and subclavian central venous catheters. AJR Am J Roentgenol 1994; 163: 291–95. doi: 10.2214/ajr.163.2.8037017 [DOI] [PubMed] [Google Scholar]
- 43. Rossi UG, Rigamonti P, Tichà V, Zoffoli E, Giordano A, Gallieni M, et al. Percutaneous ultrasound-guided central venous catheters: the lateral in-plane technique for internal jugular vein access. J Vasc Access 2014; 15: 56–60. doi: 10.5301/jva.5000177 [DOI] [PubMed] [Google Scholar]
- 44. Nazarian GK, Bjarnason H, Dietz CA, Bernadas CA, Hunter DW. Changes in tunneled catheter tip position when a patient is upright. Journal of Vascular and Interventional Radiology 1997; 8: 437–41. doi: 10.1016/S1051-0443(97)70585-2 [DOI] [PubMed] [Google Scholar]
- 45. Forauer AR, Alonzo M. Change in peripherally inserted central catheter tip position with abduction and adduction of the upper extremity. J Vasc Interv Radiol 2000; 11: 1315–18. doi: 10.1016/s1051-0443(07)61308-6 [DOI] [PubMed] [Google Scholar]
- 46. Yu C, Shulan L, Juan W, Ling L, Chun-Mei L. The accuracy and safety of using the electrocardiogram positioning technique in localizing the peripherally inserted central catheter tip position: a systematic review and meta-analysis. Nurs Open 2022; 9: 1556–63. doi: 10.1002/nop2.932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Vesely TM. Central venous catheter tip position: a continuing controversy. Journal of Vascular and Interventional Radiology 2003; 14: 527–34. doi: 10.1097/01.RVI.0000071097.76348.72 [DOI] [PubMed] [Google Scholar]
- 48. Ostroff MD, Moureau N, Pittiruti M. Rapid assessment of vascular exit site and tunneling options (ravesto): a new decision tool in the management of the complex vascular access patients. J Vasc Access 2023; 24: 311–17. doi: 10.1177/11297298211034306 [DOI] [PubMed] [Google Scholar]
- 49. Kehagias E, Tsetis D. The L-shaped tunneling technique: a modified technique facilitating a more discreet implantable port positioning. J Vasc Access 2016; 17: 195–99. doi: 10.5301/jva.5000496 [DOI] [PubMed] [Google Scholar]
- 50. Bertoglio S, Cafiero F, Meszaros P, Varaldo E, Blondeaux E, Molinelli C, et al. PICC-port totally implantable vascular access device in breast cancer patients undergoing chemotherapy. J Vasc Access 2020; 21: 460–66. doi: 10.1177/1129729819884482 [DOI] [PubMed] [Google Scholar]
- 51. Bertoglio S, Annetta MG, Brescia F, Emoli A, Fabiani F, Fino M, et al. A multicenter retrospective study on 4480 implanted picc-ports: a gavecelt project. J Vasc Access 2022: 11297298211067683. doi: 10.1177/11297298211067683 [DOI] [PubMed] [Google Scholar]