Abstract
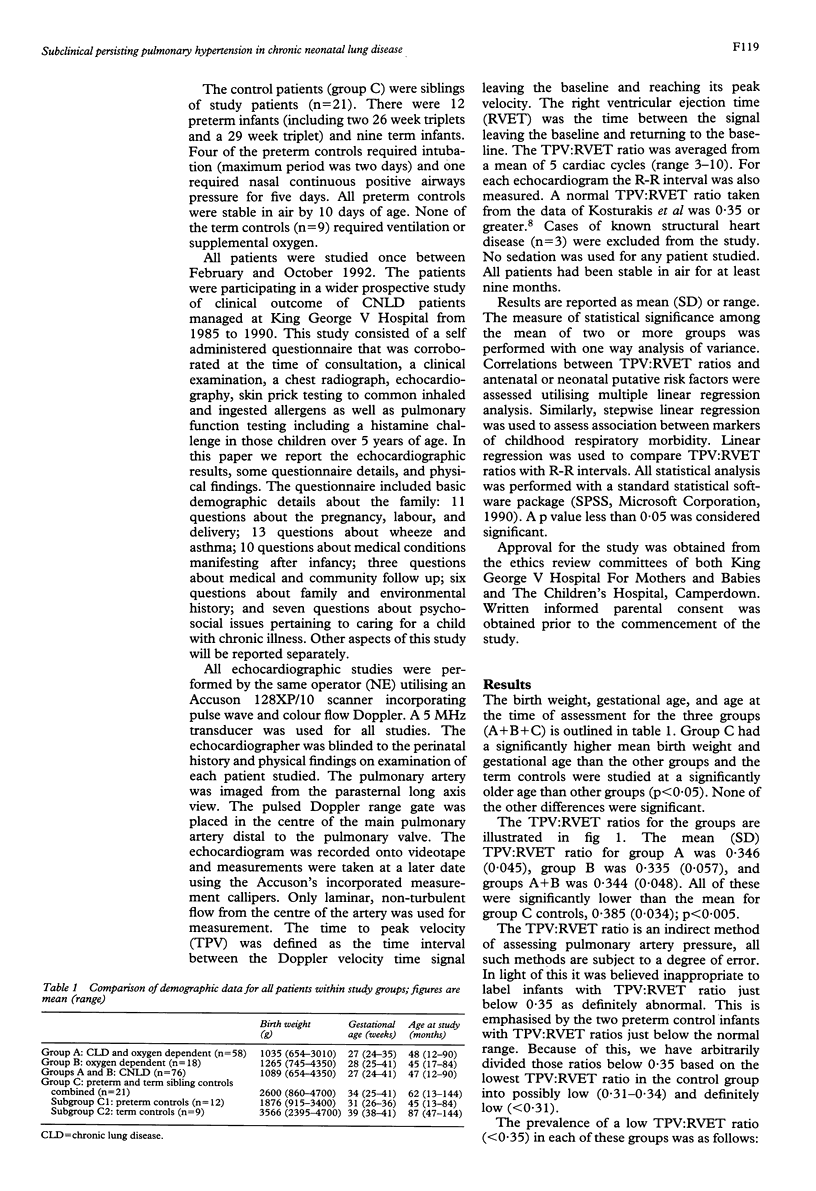
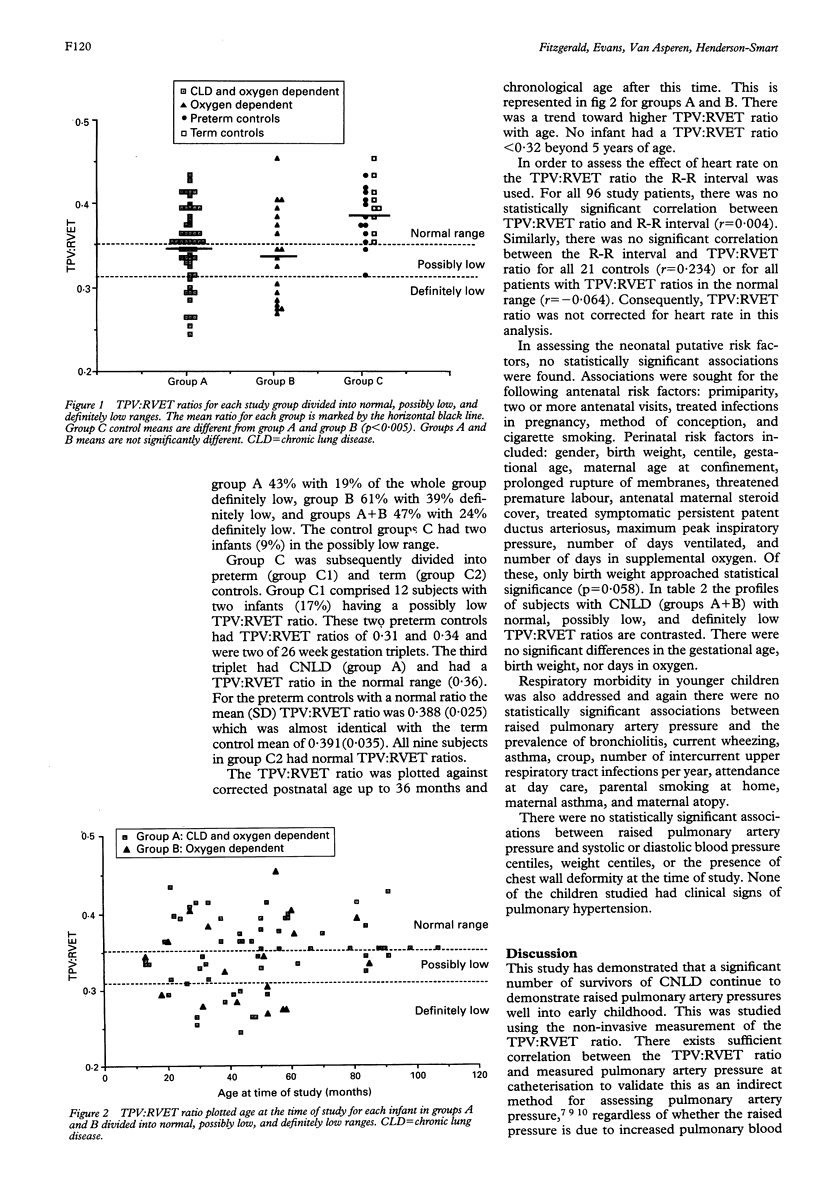
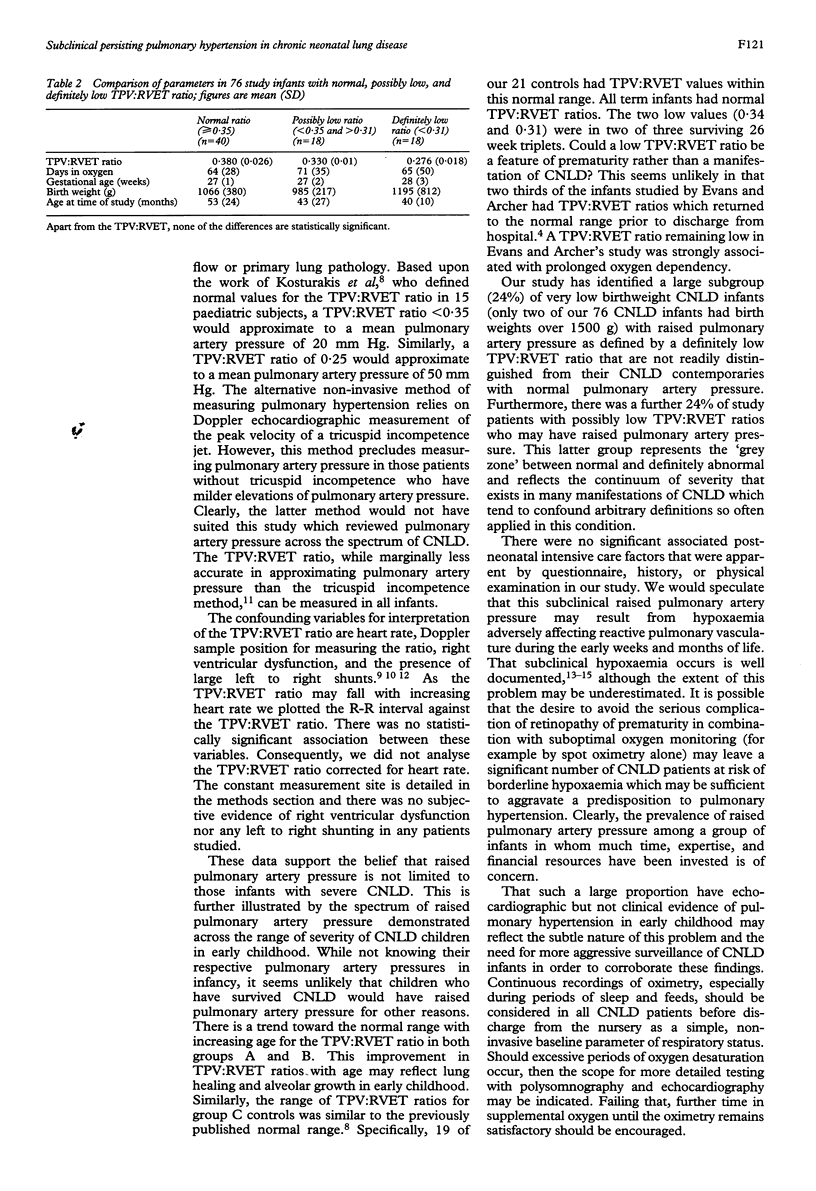
The development of pulmonary hypertension is one of the adverse factors in the outcome of infants with chronic neonatal lung disese (CNLD). The purpose of this cross sectional study was to evaluate the prevalence and degree of pulmonary hypertension in a cohort of survivors of CNLD stable in air. Pulmonary artery pressure was assessed using its inverse correlation with the ratio of time to peak velocity and right ventricular ejection time (TPV:RVET) as measured from Doppler velocity time signals in the main pulmonary artery. A normal ratio is > or = 0.35, a possibly low ratio lies between 0.31 and 0.35, and a definitely low ratio is < 0.31. The subjects were divided into three groups. Group A comprised 58 infants with oxygen dependence and an abnormal chest radiograph at 28 days of age; group B comprised 18 infants with oxygen dependence and a normal chest radiograph at 28 days of age; and group C (controls) comprised 21 siblings without oxygen dependence by 10 days and a normal chest radiograph. There were significant differences in mean (SD) TPV:RVET ratio between group A 0.346 (0.045), group B 0.335 (0.057), and groups A + B 0.344 (0.048) when compared with group C controls 0.385 (0.034). The prevalence of a definitely low TPV:RVET ratio suggesting a raised pulmonary artery pressure was 19% in group A, 39% in group B, 24% in groups A + B, and none in group C. There were no clinical signs of pulmonary hypertension in any patient studied. Stepwise multiple linear regression failed to find significant associations with antenatal or neonatal putative risk factors. Additionally, there were no associations with childhood respiratory morbidity. These data suggest a high prevalence of subclinical pulmonary hypertension in CNLD patients. It is speculated that occult hypoxaemia may be occurring in this group of infants.
Full text
PDF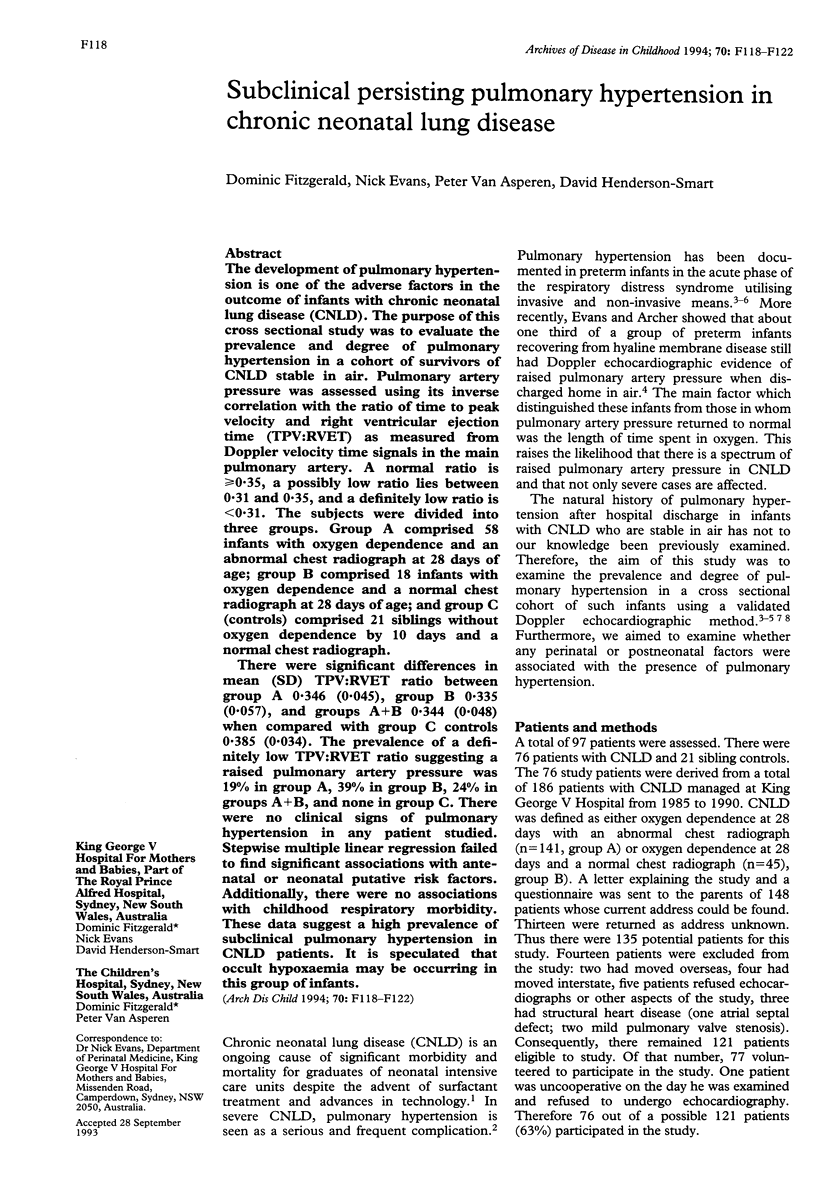
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blayney M., Kerem E., Whyte H., O'Brodovich H. Bronchopulmonary dysplasia: improvement in lung function between 7 and 10 years of age. J Pediatr. 1991 Feb;118(2):201–206. doi: 10.1016/s0022-3476(05)80483-4. [DOI] [PubMed] [Google Scholar]
- Chan K. L., Currie P. J., Seward J. B., Hagler D. J., Mair D. D., Tajik A. J. Comparison of three Doppler ultrasound methods in the prediction of pulmonary artery pressure. J Am Coll Cardiol. 1987 Mar;9(3):549–554. doi: 10.1016/s0735-1097(87)80047-5. [DOI] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Doppler assessment of pulmonary artery pressure and extrapulmonary shunting in the acute phase of hyaline membrane disease. Arch Dis Child. 1991 Jan;66(1 Spec No):6–11. doi: 10.1136/adc.66.1_spec_no.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Doppler assessment of pulmonary artery pressure during recovery from hyaline membrane disease. Arch Dis Child. 1991 Jul;66(7 Spec No):802–804. doi: 10.1136/adc.66.7_spec_no.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill A. B., Weindling A. M. Pulmonary artery pressure changes in the very low birthweight infant developing chronic lung disease. Arch Dis Child. 1993 Mar;68(3 Spec No):303–307. doi: 10.1136/adc.68.3_spec_no.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman G., Perkin R. M., Anas N. G., Sperling D. R., Hicks D. A., Rowen M. Pulmonary hypertension in infants with bronchopulmonary dysplasia. J Pediatr. 1988 Jan;112(1):67–72. doi: 10.1016/s0022-3476(88)80125-2. [DOI] [PubMed] [Google Scholar]
- Hakulinen A. L., Heinonen K., Länsimies E., Kiekara O. Pulmonary function and respiratory morbidity in school-age children born prematurely and ventilated for neonatal respiratory insufficiency. Pediatr Pulmonol. 1990;8(4):226–232. doi: 10.1002/ppul.1950080404. [DOI] [PubMed] [Google Scholar]
- Kitabatake A., Inoue M., Asao M., Masuyama T., Tanouchi J., Morita T., Mishima M., Uematsu M., Shimazu T., Hori M. Noninvasive evaluation of pulmonary hypertension by a pulsed Doppler technique. Circulation. 1983 Aug;68(2):302–309. doi: 10.1161/01.cir.68.2.302. [DOI] [PubMed] [Google Scholar]
- Kosturakis D., Goldberg S. J., Allen H. D., Loeber C. Doppler echocardiographic prediction of pulmonary arterial hypertension in congenital heart disease. Am J Cardiol. 1984 Apr 1;53(8):1110–1115. doi: 10.1016/0002-9149(84)90646-5. [DOI] [PubMed] [Google Scholar]
- Mallory G. B., Jr, Chaney H., Mutich R. L., Motoyama E. K. Longitudinal changes in lung function during the first three years of premature infants with moderate to severe bronchopulmonary dysplasia. Pediatr Pulmonol. 1991;11(1):8–14. doi: 10.1002/ppul.1950110103. [DOI] [PubMed] [Google Scholar]
- Matsuda M., Sekiguchi T., Sugishita Y., Kuwako K., Iida K., Ito I. Reliability of non-invasive estimates of pulmonary hypertension by pulsed Doppler echocardiography. Br Heart J. 1986 Aug;56(2):158–164. doi: 10.1136/hrt.56.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brodovich H. M., Mellins R. B. Bronchopulmonary dysplasia. Unresolved neonatal acute lung injury. Am Rev Respir Dis. 1985 Sep;132(3):694–709. doi: 10.1164/arrd.1985.132.3.694. [DOI] [PubMed] [Google Scholar]
- Panidis I. P., Ross J., Mintz G. S. Effect of sampling site on assessment of pulmonary artery blood flow by Doppler echocardiography. Am J Cardiol. 1986 Nov 15;58(11):1145–1147. doi: 10.1016/0002-9149(86)90146-3. [DOI] [PubMed] [Google Scholar]
- Parker R. A., Lindstrom D. P., Cotton R. B. Improved survival accounts for most, but not all, of the increase in bronchopulmonary dysplasia. Pediatrics. 1992 Nov;90(5):663–668. [PubMed] [Google Scholar]
- Sekar K. C., Duke J. C. Sleep apnea and hypoxemia in recently weaned premature infants with and without bronchopulmonary dysplasia. Pediatr Pulmonol. 1991;10(2):112–116. doi: 10.1002/ppul.1950100213. [DOI] [PubMed] [Google Scholar]
- Serwer G. A., Cougle A. G., Eckerd J. M., Armstrong B. E. Factors affecting use of the Doppler-determined time from flow onset to maximal pulmonary artery velocity for measurement of pulmonary artery pressure in children. Am J Cardiol. 1986 Aug 1;58(3):352–356. doi: 10.1016/0002-9149(86)90076-7. [DOI] [PubMed] [Google Scholar]
- Shennan A. T., Dunn M. S., Ohlsson A., Lennox K., Hoskins E. M. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988 Oct;82(4):527–532. [PubMed] [Google Scholar]
- Singer L., Martin R. J., Hawkins S. W., Benson-Szekely L. J., Yamashita T. S., Carlo W. A. Oxygen desaturation complicates feeding in infants with bronchopulmonary dysplasia after discharge. Pediatrics. 1992 Sep;90(3):380–384. [PMC free article] [PubMed] [Google Scholar]
- Stahlman M., Blankenship W. J., Shepard F. M., Gray J., Young W. C., Malan A. F. Circulatory studies in clinical hyaline membrane disease. Biol Neonate. 1972;20(3):300–320. doi: 10.1159/000240473. [DOI] [PubMed] [Google Scholar]
- Walther F. J., Benders M. J., Leighton J. O. Persistent pulmonary hypertension in premature neonates with severe respiratory distress syndrome. Pediatrics. 1992 Dec;90(6):899–904. [PubMed] [Google Scholar]


