Abstract
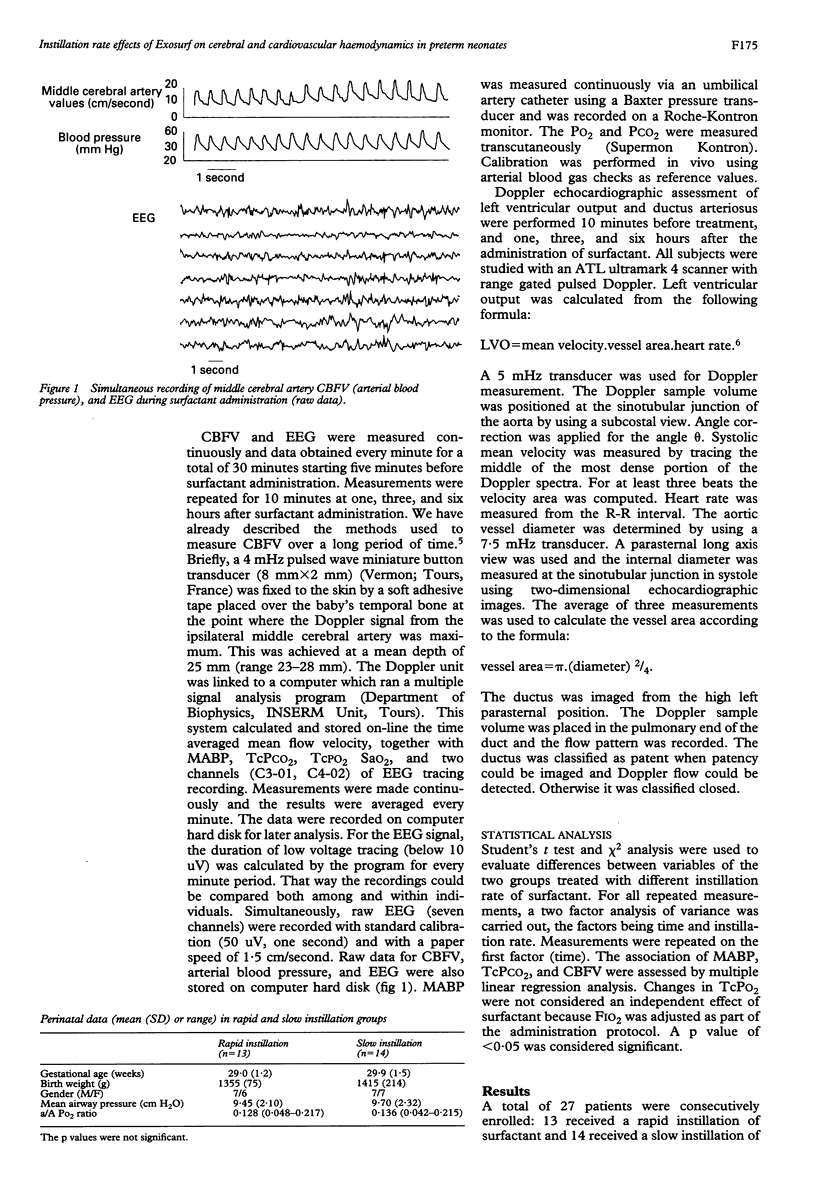
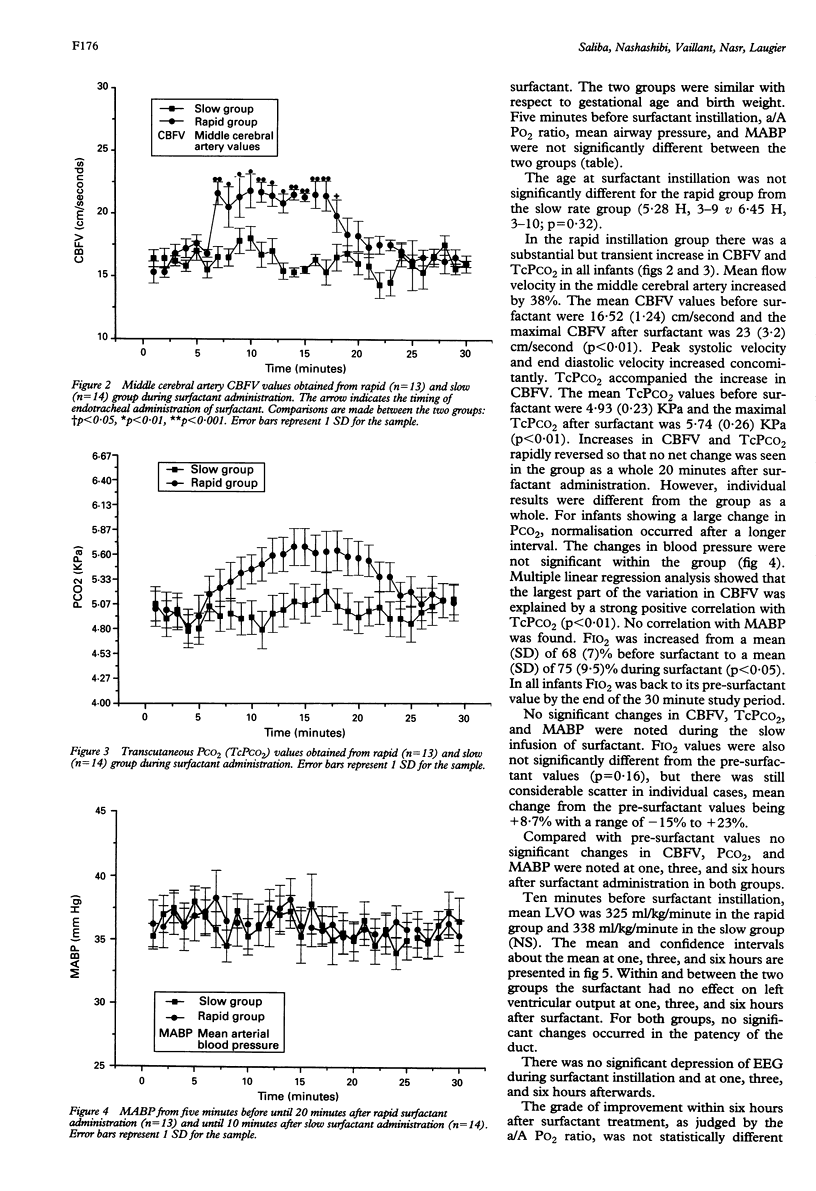
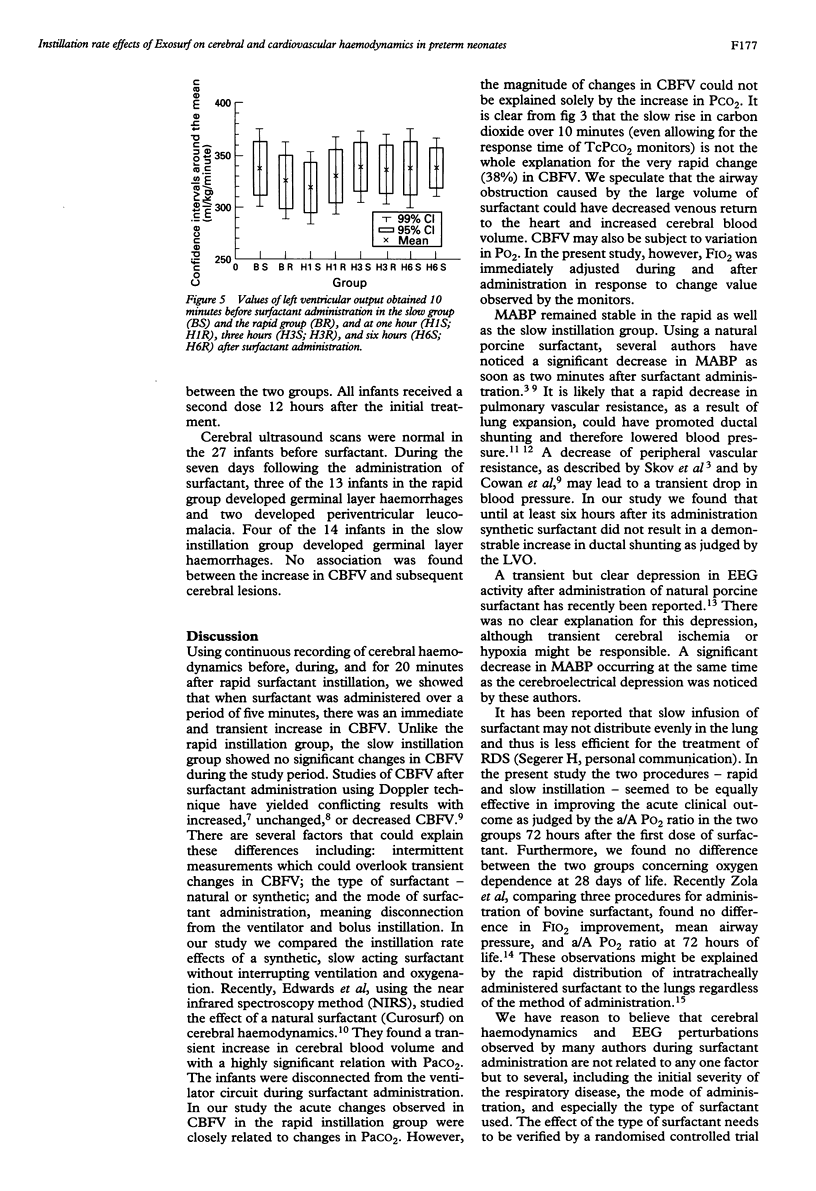
The acute effects of surfactant instillation rate on the cerebral and cardiovascular haemodynamics were studied in a randomised trial of 27 preterm neonates with respiratory distress syndrome (RDS). Cerebral blood flow velocity (CBFV), mean arterial blood pressure (MABP), blood gases and electroencephalogram (EEG) were continuously recorded before, during, and for at least 10 minutes after the administration of surfactant. The measurements were repeated one, three, and six hours later. Left ventricular output (LVO) and ductal patency were assessed 10 minutes before and then one, three, and six hours after surfactant administration. Surfactant (Exosurf) was instilled rapidly over five minutes in 13 infants and slowly over 15 minutes in 14 infants. The rapid group showed a significant but transient increase (mean 38%) in CBFV, a rise strongly related to an increase in carbon dioxide tension. No significant change in CBFV was observed in the slow group. There were no significant changes in EEG, MABP, LVO, or ductal shunting in either group. The findings suggest that rapid instillation of Exosurf leads to an increase in CBFV and partial carbon dioxide pressure (PCO2) and requires a close monitoring of blood gases to maintain adequate ventilation. Furthermore, the findings should alert clinicians to the need for slow infusion of Exosurf.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cowan F., Whitelaw A., Wertheim D., Silverman M. Cerebral blood flow velocity changes after rapid administration of surfactant. Arch Dis Child. 1991 Oct;66(10 Spec No):1105–1109. doi: 10.1136/adc.66.10_spec_no.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis J. M., Russ G. A., Metlay L., Dickerson B., Greenspan B. S. Short-term distribution kinetics of intratracheally administered exogenous lung surfactant. Pediatr Res. 1992 May;31(5):445–450. doi: 10.1203/00006450-199205000-00006. [DOI] [PubMed] [Google Scholar]
- Edwards A. D., McCormick D. C., Roth S. C., Elwell C. E., Peebles D. M., Cope M., Wyatt J. S., Delpy D. T., Reynolds E. O. Cerebral hemodynamic effects of treatment with modified natural surfactant investigated by near infrared spectroscopy. Pediatr Res. 1992 Nov;32(5):532–536. doi: 10.1203/00006450-199211000-00007. [DOI] [PubMed] [Google Scholar]
- Evans N., Moorcraft J. Effect of patency of the ductus arteriosus on blood pressure in very preterm infants. Arch Dis Child. 1992 Oct;67(10 Spec No):1169–1173. doi: 10.1136/adc.67.10_spec_no.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg S. J., Sahn D. J., Allen H. D., Valdes-Cruz L. M., Hoenecke H., Carnahan Y. Evaluation of pulmonary and systemic blood flow by 2-dimensional Doppler echocardiography using fast Fourier transform spectral analysis. Am J Cardiol. 1982 Dec;50(6):1394–1400. doi: 10.1016/0002-9149(82)90481-7. [DOI] [PubMed] [Google Scholar]
- Hellström-Westas L., Bell A. H., Skov L., Greisen G., Svenningsen N. W. Cerebroelectrical depression following surfactant treatment in preterm neonates. Pediatrics. 1992 Apr;89(4 Pt 1):643–647. [PubMed] [Google Scholar]
- Horbar J. D., Soll R. F., Schachinger H., Kewitz G., Versmold H. T., Lindner W., Duc G., Mieth D., Linderkamp O., Zilow E. P. A European multicenter randomized controlled trial of single dose surfactant therapy for idiopathic respiratory distress syndrome. Eur J Pediatr. 1990 Mar;149(6):416–423. doi: 10.1007/BF02009663. [DOI] [PubMed] [Google Scholar]
- Jorch G., Rabe H., Garbe M., Michel E., Gortner L. Acute and protracted effects of intratracheal surfactant application on internal carotid blood flow velocity, blood pressure and carbondioxide tension in very low birth weight infants. Eur J Pediatr. 1989 Aug;148(8):770–773. doi: 10.1007/BF00443108. [DOI] [PubMed] [Google Scholar]
- McCord F. B., Curstedt T., Halliday H. L., McClure G., Reid M. M., Robertson B. Surfactant treatment and incidence of intraventricular haemorrhage in severe respiratory distress syndrome. Arch Dis Child. 1988 Jan;63(1):10–16. doi: 10.1136/adc.63.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saliba E., Autret E., Nasr C., Suc A. L., Laugier J. Perinatal pharmacology and cerebral blood flow. Biol Neonate. 1992;62(4):252–257. doi: 10.1159/000243879. [DOI] [PubMed] [Google Scholar]
- Saliba E., Chantepie A., Autret E., Gold F., Pourcelot L., Laugier J. Effects of indomethacin on cerebral hemodynamics at rest and during endotracheal suctioning in preterm neonates. Acta Paediatr Scand. 1991 Jun-Jul;80(6-7):611–615. doi: 10.1111/j.1651-2227.1991.tb11918.x. [DOI] [PubMed] [Google Scholar]
- Skov L., Bell A., Greisen G. Surfactant administration and the cerebral circulation. Biol Neonate. 1992;61 (Suppl 1):31–36. doi: 10.1159/000243841. [DOI] [PubMed] [Google Scholar]
- Vidyasagar D., Maeta H., Raju T. N., John E., Bhat R., Go M., Dahiya U., Roberson Y., Yamin A., Narula A. Bovine surfactant (surfactant TA) therapy in immature baboons with hyaline membrane disease. Pediatrics. 1985 Jun;75(6):1132–1142. [PubMed] [Google Scholar]
- van de Bor M., Ma E. J., Walther F. J. Cerebral blood flow velocity after surfactant instillation in preterm infants. J Pediatr. 1991 Feb;118(2):285–287. doi: 10.1016/s0022-3476(05)80503-7. [DOI] [PubMed] [Google Scholar]


