Abstract
Objective
Bipolar disorder (BD) is associated with premature mortality. All-cause and specific mortality risks in this population remain unclear, and more studies are still needed to further understand this issue and guide individual and public strategies to prevent mortality in bipolar disorder Thus, a systematic review and meta‐analysis of studies assessing mortality risk in people with BD versus the general population was conducted. The primary outcome was all‐cause mortality, whilst secondary outcomes were mortality due to suicide, natural, unnatural, and specific‐causes mortality.
Results
Fifty-seven studies were included (BD; n = 678,353). All‐cause mortality was increased in people with BD (RR = 2.02, 95% CI: 1.89–2.16, k = 39). Specific‐cause mortality was highest for suicide (RR = 11.69, 95% CI: 9.22–14.81, k = 25). Risk of death due to unnatural causes (RR = 7.29, 95% CI: 6.41–8.28, k = 17) and natural causes (RR = 1.90, 95% CI: 1.75–2.06, k = 17) were also increased. Among specific natural causes analyzed, infectious causes had the higher RR (RR = 4,38, 95%CI: 1.5–12.69, k = 3), but the analysis was limited by the inclusion of few studies. Mortality risk due to respiratory (RR = 3.18, 95% CI: 2.55–3.96, k = 6), cardiovascular (RR = 1.76, 95% CI: 1.53–2.01, k = 27), and cerebrovascular (RR = 1.57, 95% CI: 1.34–1.84, k = 13) causes were increased as well. No difference was identified in mortality by cancer (RR = 0.99, 95% CI: 0.88–1.11, k = 16). Subgroup analyses and meta-regression did not affect the findings.
Conclusion
Results presented in this meta-analysis show that risk of premature death in BD is not only due to suicide and unnatural causes, but somatic comorbidities are also implicated. Not only the prevention of suicide, but also the promotion of physical health and the prevention of physical conditions in individuals with BD may mitigate the premature mortality in this population. Notwithstanding this is to our knowledge the largest synthesis of evidence on BD-related mortality, further well-designed studies are still warranted to inform this field.
Subject terms: Bipolar disorder, Depression
Background
Bipolar disorder (BD) is a chronic, often progressive, and disabling disorder that has peak and median age at onset at age 19.5 and 33 years old [1], and affects roughly one percent of the global population, regardless of sex, ethnicity, or social income [2–4]. BD is one of the most incapacitating diseases among young and working age adults and is strongly associated with lower productivity levels, functional and social impairment, increased rates of clinical and psychiatric comorbidities and premature mortality [5, 6].
The association between mental disorders and mortality is complex, as the relative risk is the highest for suicide, but the most frequent causes of the death are the physical comorbidities associated to it (e.g., metabolic, cardiovascular, cerebrovascular, infectious, and respiratory diseases) [4, 5]. Although the current literature has focused on major depression [7] and schizophrenia [8], a raising body of evidence have been published suggesting the association between BD and premature death.
Initial studies suggested that higher mortality levels in BD patients were solely attributed to suicide [9, 10]. New research, however, indicates an increase in mortality by natural causes. In fact, compared to the general population, individuals with BD are at a greater risk of physical diseases which contributes to increase the mortality rates [11, 12].
At least part of the increased risk for natural causes of death in people with BD and other mental disorders is due to unhealthy lifestyles, adverse effects of psychiatric medications, limited access to the health care system, and disparities in diagnosis and treatment of comorbid clinical diseases [13]. Additionally, intrinsic mechanisms associated to BD such as inflammatory and oxidative processes, and genetic vulnerability are in turn associated with mortality [11, 14, 15].
To our knowledge, three reviews investigated excess mortality in individuals with BD. In 1998, Harris and Barraclough found an increase of mortality due to violent causes, but only six studies were included (N = 3801) [16]. In their analysis, mortality for suicide was 11 times more prevalent in BD compared to general population [16]. In 2009, Roshanaei-Moghaddam and Katon included 17 studies (N = 331,000), showing that BD were associated with increased premature mortality due to natural causes, mainly cardiovascular disease [11]. Finally, in 2015, Hayes et al. included 31 studies (N = 305,859) and found a twofold increase in the overall mortality in BD compared to the general population [17].
Previous reviews had some limitations as (a) screening in a single database [11], (b) including the absence of exploring all sources of heterogeneity, (c) inclusion of a small range of size effect (SMR), (d) the authors did not perform a quality assessment [17–19]. Due to the above-cited topics and since more studies have been published since the last evidence synthesis, an updated meta-analysis assessing the relative risk of all-cause and cause-specific mortality in those with BD versus the general population is needed. In this review, we aimed to fill this gap and conducting a comprehensive systematic review and meta-analysis on all-cause and cause-specific mortality relative risk in people with BD compared with any control group.
Methods
Protocol and registration
The reporting of this systematic review and meta-analysis was guided by the standards of Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [20] and Meta-analyses Of Observational Studies in Epidemiology (MOOSE) [21]. The PROSPERO protocol was registered on July 14, 2020 (CRD42020192217).
Eligibility criteria
Inclusion criteria were: (1) observational studies that compared risk of any cause of mortality between (2) patients with BD (defined according to DSM/ICD criteria or clinical charts) and a control group, (3) aged 15 years or older or providing estimates in such an age group. No language restrictions were applied. The exclusion criteria were the following: (1) studies that did not specify diagnostic criteria or whose individuals with BD could not be separated from a broader sample (i.e., a group of subjects with mood disorders), (2) studies with less than 50 patients, (3) studies that included solely individuals younger than 15 years old, (4) studies that included only individuals in a very specific subgroup, because this subgroup would not be a representative sample of bipolar disorder (i.e., prison population), (5) duplicated samples (i.e., a smaller sample from a larger cohort published elsewhere), (6) randomized controlled trials, (7) systematic or non-systematic reviews and meta-analysis.
Information sources
Studies were selected by searching in the following databases: PubMed/Medline, Embase, Web of Science and PsycInfo, up to July 20th, 2021. References and bibliography list of relevant papers were examined to track down potential studies that were not identified in the initial search.
Search strategy
Studies were screened using the terms related: (1) to bipolar disorders (e.g., bipolar disorder, bipolar affective disorder, bipolar illness, bipolar depression, and mood disorder), (2) to mortality (e.g., mortality, fatal outcome, life expectancy and death) and (3) to estimates (e.g., standardized mortality ratio or SMR, hazard ratio or HR, odds ratio or OR, and mortality rate ratio or MRR). A complete description of search terms used in each database can be found in Supplementary Table S1. After the database search, duplicated papers and samples were removed, and the study selection started.
Study selection
The studies were first screened based on title and abstract by authors TB and LSR. Selected studies were analyzed in full text by two pairs independently (TB and LSR, LT and GHB) and those that did not met inclusion criteria were removed. Discrepancies in any phase were discussed between the authors TB, GHB, MS, ED and BL until a consensus was reached. The remaining papers were then included in the meta-analysis. The software Covidence was used to conduct the processes from studies screening to data extraction [22].
Data extraction
Data extraction was conducted in pairs independently by TB, LSR, LT and GHB and discrepancies were discussed between authors until a consensus was reached.
We extracted the author, year of publication, country, sex, study design, representativeness, setting (inpatient, outpatient, mixed), BD diagnostic criteria, control group, sample size, outcome, estimates of mortality risk with dispersion measure, adjusted versus non-adjusted analyses, and the information needed to conduct quality assessment.
Statistical analyses
We used RR with 95% CI to describe the summary results of meta-analysis. A RR superior to 1 indicating a higher mortality in individuals with BD, whereas an RR inferior to 1 indicating an increased mortality in the general population or control group [23]. We pooled together SMR, MRR, RR, OR, and HR given that as the event rate was rare, i.e., less frequent than 10%, and the study design, population, comparison, and outcome were comparable [23]. Similar statistical method was used in other meta-analyses regarding mortality in mental diseases groups [8, 24].
Whenever feasible, subgroup analyses were conducted to assess the mortality categorical outcomes stratified by representativeness (whether the sample was representative of the whole population), sample type (outpatient, inpatient or community), study design (prospective, retrospective or case-control), location (Africa, Asia, North America, Europe or other), BD diagnostic criteria (DSM, ICD or other) the use of a structured interview to assess patients adjustment by substance use disorder (SUD) and time-at-risk.
Regarding representativeness, a sample was considered representative when used a populational-based design. It was not considered representative when included inpatients or only individuals with any specific condition (i.e., only BD patients using lithium, or individuals with pre-existing somatic disorders).
We used a random-effects model to calculate the summary RR, based on DerSimonian and Leird method as we could not assume that the same true effect was present in all studies [25]. Statistical analysis was conducted using Comprehensive Meta-Analysis (CMA) version 3. Finally, we calculated the prediction intervals to each meta-analysis to assess the distribution of true effects [26].
Heterogeneity and publication bias
Heterogeneity was assessed using the Q-test and the I2 statistics. Publication bias was calculated using Egger’s regression test and visually assessed by funnel plot [27, 28].
Risk of bias of individual studies
The risk of bias of the included articles was assessed by two independent reviewers independently (TB and GHB) according to the Newcastle-Ottawa Scale (NOS). This instrument is used to evaluate the quality of non-randomized studies in meta-analyses. The NOS consists of 8 items divided into 3 categories: selection, comparability, and outcome (cohort studies) or exposure (case-control studies). Studies scoring 6 or more are considered high-quality, while those scoring 5 or less are considered of low quality [29].
Meta-regression
Meta-regression was performed to assess the influence of confounding factors affecting results and heterogeneity. The continuous variables chosen to be assessed trough meta- regression were sample size, percentage of females, mid-point year of the study, mean follow- up years and NOS score. Since mortality may be affected by social conditions, we additionally included social developing indicators of the countries where the studies were conducted. Hence, both Social Development Index (SDI) and Human Development Index (HDI) were also used as moderators in the meta-regression [30, 31].
Level of certainty of the results
GRADE is a practical to tool evaluate the certainty in the evidence for systematic review authors and decision-makers. Herein, GRADE was used to classify the confidence level in the RR estimates as high, moderate, low, or very low [32].
Results
Study selection
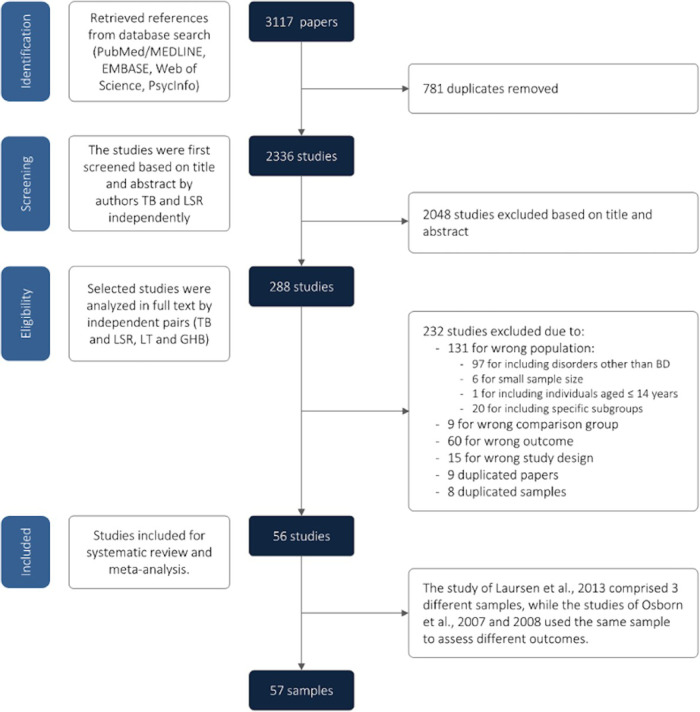
Database search yielded 2336 manuscripts eligible for screening, after the removal of duplicates. Next, 2048 articles were excluded based on title and abstract, and 288 papers were retrieved. After the full-text review, 232 studies were subsequently excluded, resulting in 56 studies included in this meta-analysis. However, the study of Laursen et al., 2013 [33] was comprised of three different samples, while the studies of Osborn et al. 2007 [34] and 2008 [35] used the same sample to assess different outcomes. Hence, the final analysis was composed by 57 samples [36–90]. Figure 1 presents the PRISMA flow diagram for study selection and PRISMA Checklist can be found in suplementar material (Table S6)
Fig. 1. PRISMA flowchart.
PRISMA Flowchart for elegible and included studies.
The main reasons for exclusion were due to population characteristics (mainly when the population was a specific subgroup), or when the statistical analyses for BD as a separate diagnosis. Overall, 124 papers reported data from a broad group, as severe mental illness, mood disorders or affective disorders, rather than specifically on subjects with BD. Other seven studies included a very specific group of bipolar patients, for instance veterans, long-stay psychiatric patients and people without a fixed address. Other nine studies included only individuals with BD but compared physically healthy individuals with BD with subjects with BD and a comorbid organic disease [91–99]. Eight studies reported data from duplicated samples and were not included in the meta-analysis [100–107]. In these cases, we used the most recent and/or the larger sample to choose the included study. Finally, 60 studies did not assess mortality. All excluded articles and the reason for exclusion can be found in the Supplementary Table S2.
Studies characteristics
The 57 samples included in the analysis comprised 678 353 individuals with BD. Assessment data ranged from 1934 to 2016. Ten studies did not report data separately from men and women [108–117] and three studies only included males [118–120]. Sex analysis included 46 studies with males (k = 47 samples, 262 971 individuals) and 43 studies with females (k = 44 samples, 342,493 individuals). As most of the included studies were observational with a longitudinal follow-up with a wide range (1 to 52 years) and there were not at least ten studies reporting mean age with the same outcome, it was not possible to calculate the mean age to use as a moderator in the statistical analysis. The sociodemographic characteristics of the included studies are compiled in Table 1. Additional characteristics are available in Supplementary Table S3.
Table 1.
Demographic characteristics of the included studies.
| Study | Location | Sample size (men/woman) | Recruitment Datea | Outcome | Diagnostic criteria | Sample type | Represen- tativeb | Structured interviewc | NOSd | Type of mortality assessed |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahrens 1995 [36] | Multicentric | 440 (251/189) | 1967–1992 | SMR | NA | Outpatients | No | Yes | 5 | All-cause, suicide, cardiovascular |
| Ajetunmobi 2013 [37] | United Kingdom | 5778 (2159/3619) | 1986–2010 | SMR | ICD-10 | Inpatients | No | No | 7 | All-cause, natural, unnatural, suicide, cardiovascular, cancer, cerebrovascular |
| Almeida 2016 [38] | Australia | 288 (288/0) | 1996–2011 | HR | ICD-8 and 9 | Community | Yes | No | 8 | Suicide |
| Angst 2002 [39] | Switzerland | 220 (73/147) | 1959–1997 | SMR | ICD-8 | Inpatients | No | Yes | 7 | All-cause, suicide, cardiovascular, cancer |
| Angst 2005 [40] | Switzerland | 220 (73/147) | 1959–2003 | SMR | ICD-9 | Inpatients | No | Yes | 6 | All-cause, suicide, cardiovascular, cancer, cerebrovascular |
| Angst 2013 [41] | Switzerland | 190 (132/68) | 1959–2009 | SMR | ICD-10 | Inpatients | No | No | 7 | All-cause, suicide, cardiovascular, cancer, cerebrovascular |
| Black 1987 [42] | United States | 586 (NA/NA) | 1970–1983 | SMR | DSM III | Inpatients | No | No | 6 | All-cause, natural, unnatural, cerebrovascular |
| Bratfos 1968 [9] | Norway | 207 (93/114) | 1952–1963 | SMR | Langfeldt | Inpatients | No | Yes | 6 | All-cause |
| Callaghan 2014 [43] | United States | 76098 (30978/45120) | 1990–2005 | SMR | ICD-9 | Inpatients | No | No | 7 | Cardiovascular, respiratory, cancer |
| Castagnini 2013 [44] | Denmark | 3200 (NA/NA) | 1995–2008 | SMR | ICD-10 | Inpatients | No | No | 6 | All-cause, natural, unnatural, suicide, cardiovascular, respiratory, cancer, infectious, cerebrovascular |
| Chang 2010 [45] | United Kingdom | 2699 (1126/1573) | 2007–2010 | SMR | ICD-10 | Inpatients | No | No | 7 | All-cause, unnatural, suicide |
| Chang 2012 [46] | United Kingdom | 1542 (574/968) | 2007–2010 | HR | ICD-10 | Community | Yes | No | 7 | All-cause, unnatural, suicide |
| Chen 2010 [15, 47] | Taiwan | 1581 (780/801) | 1996–2004 | HR | ICD-9 | Inpatients | No | No | 7 | All-cause, natural, unnatural |
| Chen 2020 [87] | Taiwan | 46490 (23321/23169) | 2001–2016 | SMR | ICD-9 and 10 | Inpatients | No | No | 8 | Sudden cardiac death |
| Choi 2019 [48] | South Korea | 481 (214/267) | 2005–2012 | HR | ICD-10 | Inpatients | No | No | 8 | Suicide |
| Crump 2013 [49] | Sweden | 6618 (2700/3918) | 2003–2009 | HR | ICD-10 | Community | Yes | No | 8 | All-cause, natural, unnatural, suicide, cardiovascular, cancer, cerebrovascular |
| Dutta 2007 [50] | United Kingdom | 235 (102/133) | 1965–1999 | SMR | DSM IV | Inpatients | No | Yes | 6 | All-cause, suicide, cardiovascular, respiratory, cancer, infectious |
| Fekadu 2015 [51] | Ethiopia | 346 (193/153) | 1998–2012 | SMR | SCAN | Community | Yes | No | 7 | All-cause |
| Fiedorowicz 2009 [52] | United States | 435 (185/250) | 1978–2003 | HR | RDC | Outpatients | Yes | Yes | 7 | Cardiovascular |
| Gale 2012 [53] | Sweden | 31 (31/0) | 1950–2004 | HR | ICD-8, 9 and 10 | Inpatients | No | Yes | 8 | Cardiovascular |
| Guan 2013 [54] | Netherlands | 2077 (927/1150) | 1999–2009 | HR | DSM-IV | Community | Yes | No | 7 | All-cause, suicide, cancer |
| Hayes 2017 [55] | United Kingdom | 17314 (7139/10202) | 2000–2014 | HR | ICD-10 | Community | Yes | No | 7 | All-cause, suicide, cardiovascular |
| Hjorthøj 2015 [56] | Denmark | 6799 (2455/4344) | 1969–2011 | SMR | NA | Community | Yes | No | 8 | All-cause |
| Hoang 2011 [57] | United Kingdom | 75720 (29534/46186) | 1999–2006 | SMR | ICD-9 and 10 | Inpatients | No | No | 6 | All-cause, natural, unnatural, cardiovascular, respiratory, cerebrovascular |
| Hoang 2013 [58] | United Kingdom | 14017 (5747/8270) | 2006–2008 | SMR | ICD-10 | Inpatients | No | No | 6 | All-cause |
| Høye 2016 [59] | Norway | 845 (331/514) | 1980–2012 | SMR | ICD-9 and 10 | Inpatients | No | No | 7 | All-cause, suicide, cardiovascular, cancer |
| Kay 1977 [60] | Sweden | 192 (84/108) | 1958–1970 | SMR | NA | Outpatients | Yes | Yes | 5 | All-cause |
| Kim 2018 [61] | South Korea | 1874 (588/1286) | 2002–2013 | HR | ICD-10 | Community | Yes | No | 8 | All-cause, suicide |
| Kodesh 2012 [62] | Israel | 5732 (2539/3193) | 2003–2009 | MRR | ICD-9 | Community | Yes | No | 8 | All-cause |
| Laursen 2007 [90] | Sweden | 11648 (NA/NA) | 1973–2001 | MRR | ICD-8 and 10 | Inpatients | No | No | 8 | Suicide, cardiovascular, respiratory, cancer |
| Laursen 2009 [63] | Denmark | NA (NA/NA) | 1994–2007 | MRR | ICD-8 and 10 | Inpatients | No | No | 8 | Cardiovascular |
| Laursen 2011 [88] | Denmark | 6215 (NA/NA) | 1995–2007 | MRR | ICD-8 and 10 | Community | Yes | No | 8 | Natural |
| Study | Location | Sample size (men/woman) | Recruitment Datea | Outcome | Diagnostic criteria | Sample type | Represen- tativeb | Structured interviewc | NOSd | Type of mortality assessed |
| Laursen 2013a [64] | Denmark | 11101 (4280/6821) | 2000–2007 | SMR | ICD-9 and 10 | community | Yes | No | 8 | All-cause, natural, unnatural, cardiovascular, cerebrovascular |
| Laursen 2013b [64] | Finland | 9919 (4489/5430) | 2000–2007 | SMR | ICD-9 and 10 | Community | Yes | No | 8 | All-cause, natural, unnatural, cardiovascular, cerebrovascular |
| Laursen 2013c [64] | Sweden | 18355 (7367/10988) | 2000–2007 | SMR | ICD-9 and 10 | Community | Yes | No | 8 | All-cause, natural, unnatural, cardiovascular, cerebrovascular |
| Lomholt 2019 [65] | Denmark | 23092 (9510/13582) | 1995–2014 | SMR | ICD-8 and 10 | Community | Yes | No | 8 | All-cause |
| Medici 2015 [66] | Denmark | 15334 (NA/NA) | 1995–2012 | SMR | ICD-10 | Community | Yes | No | 8 | All-cause |
| Mohamed 2019 [67] | United States | 41362 (21632/19730) | 2004–2014 | OR | ICD-9 | Inpatients | No | No | 8 | Cardiovascular |
| Newman 1991 [68] | Canada | 1429 (543/886) | 1976-1985 | SMR | ICD-9 | Community | Yes | No | 8 | All-cause, suicide |
| Norton 1984 [69] | United Kingdom | 791 (NA/NA) | 1967–1977 | SMR | Feighner | Community | No | No | 7 | All-cause, suicide, cardiovascular, cancer |
| Osborn 2007/2008 [70, 89] | United Kingdom | 10742 (5725/5017) | 1987–2002 | HR | Oxmis | Community | Yes | No | 8 | Cardiovascular, cerebrovascular |
| Ösby 2001 [71] | Sweden | 15386 (6578/8808) | 1973–1995 | SMR | ICD-8 and 9 | Inpatients | No | No | 8 | All-cause, natural, unnatural, suicide, cardiovascular, respiratory, cancer, infectious, cerebrovascular |
| Pan 2017 [87] | Taiwan | 77859 (33415/44444) | 2003–2007 | SMR | ICD-9 | Community | Yes | No | 7 | All-cause, natural, unnatural, cerebrovascular |
| Pan 2020 [73] | Taiwan | 103709 (43843/59866) | 2005–2013 | SMR | ICD-9 | Community | Yes | No | 6 | All-cause, natural, unnatural, cerebrovascular |
| Park 2019 [74] | South Korea | 3470 (1706/1764) | 2002–2013 | SMR | ICD-10 | Community | Yes | No | 7 | Suicide |
| Ramsey 2013 | United States | 2519 (1268/1251) | 1980–2007 | OR | DSM III | Community | Yes | No | 7 | All-cause |
| Saku 1995 [76] | Japan | 187 (119/68) | 1948–1985 | SMR | DSM III | Inpatients | No | No | 6 | All-cause, cancer |
| Schaffer 2014 [77] | Canada | 170 (96/74) | 1998–2010 | OR | Coroner | Community | Yes | No | 7 | Suicide |
| Schneider 2001 [78] | Germany | 74 (24/50) | 1983–1993 | SMR | DSM III, ICD-9 | Inpatients | No | Yes | 7 | All-cause, natural, unnatural, cerebrovascular |
| Schulman-Marcus 2016 [79] | United States | 16913 (9353/7560) | 2001–2012 | OR | ICD-9 | Inpatients | No | No | 8 | Cardiovascular |
| Sharma 1994 [80] | United Kingdom | 472 (NA/NA) | 1970–1987 | SMR | DSM III | Inpatients | No | No | 4 | Suicide, cardiovascular, respiratory |
| Tsuang 1980 [81] | United States | 92 (34/58) | 1934–1974 | SMR | Iowa 500 cohort | Inpatients | No | No | 7 | All-cause, natural, unnatural, suicide, cardiovascular, cancer, infectious, cerebrovascular |
| Vinogradova 2010 [82] | United Kingdom | 159 (63/96) | 2000–2005 | HR | Othere | Community | No | No | 6 | All-cause |
| Webb 2014 [83] | Sweden | 15337 (NA/NA) | 1973–2009 | RR | ICD-8, 9 and 10 | Community | Yes | No | 8 | Suicide |
| Weeke 1987 [84] | Denmark | 2662 (2662/0) | 1950–1957 | SMR | ICD-8 | Inpatients | No | No | 5 | All-cause, suicide, cardiovascular |
| Westman 2013 [85] | Sweden | 17101 (NA/NA) | 1987–2006 | SMR | ICD-9 and 10 | Inpatients | No | No | 7 | All-cause, natural, unnatural, suicide, Cardiovascular, cancer, cerebrovascular |
| Yeh 2019 [86] | United States | 213 (102/111) | 2000–2013 | OR | ICD-9 | Community | Yes | No | 8 | Suicide |
HR hazard ratio, MRR mortality rate ratio, NA not available, OR odds ratio, RR risk ratio, SCAN Clinical Assessment in Neuropsychiatry, SMR standardized mortality ratio.
aData since the first individual from the last individual entered and do not necessarily correspond to the data of the last assessment of mortality.
bWhether the sample is representative from the general population or not.
cWhether the researchers used a structured interview to recruit individuals to the study.
dThe NOS (Newcastle-Ottawa Scale) is used to assess the risk of bias.
eStandard computer codes (Read codes) for general practice in the UK.
The samples were obtained from 16 different countries, mainly from western Europe (k = 35), followed by North America (k = 10) and Asia (k = 9). Africa [121] and Oceania [118] were represented by one study each, while another study was multicentric [122]. Most of studies used retrospective (k = 28) or prospective cohorts (k = 26), while few of them were case-control studies (k = 3). Studies included samples of inpatients (k = 28), community (k = 26) or outpatient (k = 3). Follow-up time ranged from 1 to 52 years.
Regarding estimates, 35 studies reported SMR, while 12 used HR, five used OR, four used MRR and one used RR. From the 58 samples included in the final analysis, 26 were considered representative of the population, while 31 were considered not representative.
Risk of bias of individual studies
The scores in the NOS ranged from four to eight in the included studies. Only four up to 56 studies were considered at high risk of bias [108, 120, 122, 123]. The remaining studies scored six or more and were considered at a low risk of bias. Individual risks of each study are presented in Table 1, whereas a detailed scoring is described in the Supplementary Table S4. Supplementary Figure S1 shows a visual distribution of risk of bias of individual studies and Supplementary Figure S2 summarizes the distribution of biases regarding all included studies.
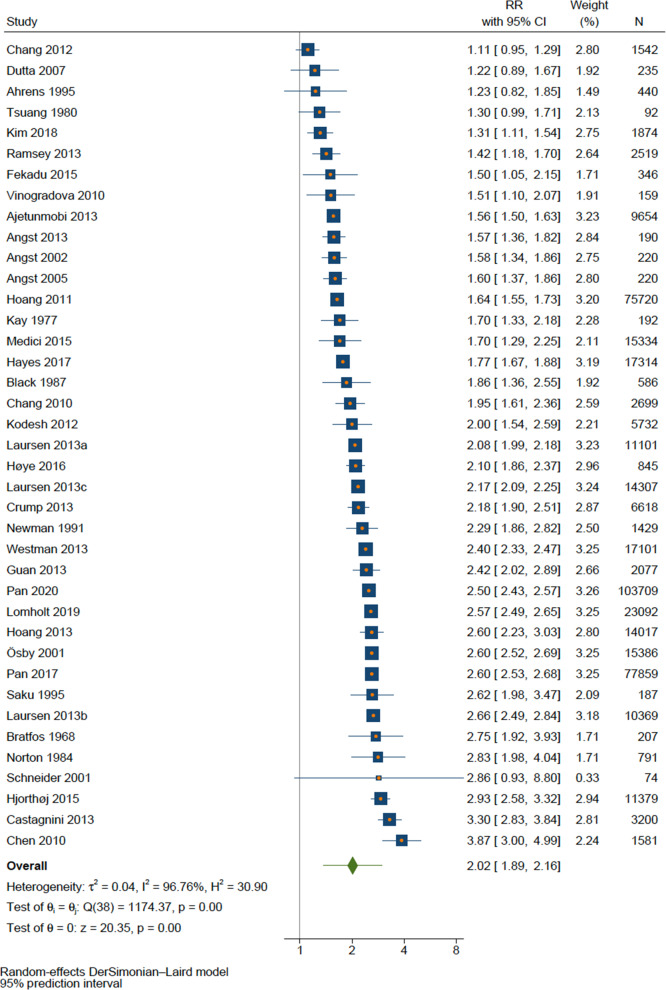
Overall mortality
All-causes mortality was assessed in 39 samples comprising 450 397 individuals with BD. The pooled RR for overall mortality in the total population was RR = 2.02 (95%CI 1.89–2.16, p < 0.001, k = 39). The RR was similar between men (RR = 2.27, 95%CI 2.13–2.43, p < 0.001, k = 23) and women (RR = 2.26, 95%CI 2.08–2.46, p < 0.001, k = 22).
There was a high between-study heterogeneity, either for total population (Q = 1174.2, p < 0.001, I2 = 96.8%) or sex analysis of men (Q = 180.8, p < 0.001, I2 = 87.8%) and women (Q = 317.5, p < 0.001, I2 = 93.4%). The forest plot for all-cause mortality is shown in Fig. 2.
Fig. 2.
Forest plot of all-cause mortality.
Although a high heterogeneity was found, when prediction interval was calculated, the true effect size remained significant and ranged from 1.37 in some populations to 2.98 in others, regardless the sex (1.73 to 2.98 for males and 1.57 to 3.27 for females). The results and graphs of prediction interval are presented in Supplementary Fig. S3.
A significant publication bias was found in the analysis of overall mortality (Egger’s test p = 0.036). Funnel plot showed that most of the studies presents a low standard error, which is a consequence of the large sample sizes of the included studies. However, there is a homogeneous distribution between results that does not favor any group, whether the general population or BD (Supplementary Fig. S4). Both Egger’s test and forest plots revealed no publication bias for male (p = 0.360) or female (p = 0.328). Summary results for all-cause mortality are presented in Table 2.
Table 2.
Summary of results.
| Sex | K | N | Effect size [95%CI] | I2 (%) | Egger’s test p value | GRADE |
|---|---|---|---|---|---|---|
| All-cause mortality | ||||||
| Total | 39 | 450397 | 2.02 [1.89–2.16] | 96.8 | 0.036 | ⨁⨁⨁◯ |
| Male | 23 | 158752a | 2.27 [2.13–2.43] | 87.8 | 0.360 | ⨁⨁⨁◯ |
| Female | 22 | 215505a | 2.26 [2.08–2.46] | 93.4 | 0.328 | ⨁⨁⨁◯ |
| Mortality by natural causes | ||||||
| Total | 17 | 354417 | 1.91 [1.76–2.07] | 96.1 | 0.588 | ⨁⨁◯◯ |
| Male | 11 | 103783a,d | 2.03 [1.88–2.19] | 87.9 | 0.893 | ⨁⨁⨁◯ |
| Female | 12 | 138050a,d | 2.05 [1.95–2.16] | 71.5 | 0.848 | ⨁⨁⨁◯ |
| Mortality by unnatural causes | ||||||
| Total | 17 | 349744 | 7.29 [6.42–8.28] | 94.1 | 0.128 | ⨁⨁⨁⨁ |
| Male | 10 | 103783a | 6.69 [5.85–7.66] | 87.3 | 0.454 | ⨁⨁⨁⨁ |
| Female | 11 | 138050a | 9.33 [8.07–0.78] | 86.1 | 0.082 | ⨁⨁⨁⨁ |
| Mortality by suicide | ||||||
| Total | 25 | 180210 | 11.6 [9.23–14.81] | 94.6 | 0.103 | ⨁⨁⨁⨁ |
| Male | 11 | 47568b,e,h | 14.02 [11.16–17.60] | 87.1 | 0.146 | ⨁⨁⨁⨁ |
| Female | 11 | 71175b,e | 17.53 [10.76–28.54] | 97.5 | 0.258 | ⨁⨁⨁⨁ |
| Mortality by cardiovascular causes | ||||||
| Total | 27 | 387963c | 1.76 [1.53–2.02] | 98.0 | 0.528 | ⨁⨁◯◯ |
| Male | 13 | 96411b | 1.82 [1.69–1.97] | 73.3 | 0.735 | ⨁⨁◯◯ |
| Female | 14 | 154499c | 1.69 [1.44–1.99] | 95.4 | 0.637 | ⨁⨁◯◯ |
| Mortality by cerebrovascular causes | ||||||
| Total | 13 | 165787 | 1.57 [1.34–.84] | 85.6 | 0.931 | ⨁⨁◯◯ |
| Male | 7 | 56494 | 1.70 [1.54–1.88] | 0.0 | 0.434 | ⨁⨁◯◯ |
| Female | 7 | 77620 | 1.70 [1.30–2.23] | 90.9 | 0.254 | ⨁⨁◯◯ |
| Mortality by infectious causes | ||||||
| Total | 3 | 91341f | 4.38 [1.51–12.70] | 94.7 | NA** | ⨁⨁◯◯ |
| Male | 2 | 6680 | 3.24 [1.90–5.52] | 0.0 | NA** | ⨁⨁◯◯ |
| Female | 2 | 8941 | 2.62 [1.61–4.28] | 0.0 | NA** | ⨁⨁◯◯ |
| Mortality by respiratory causes | ||||||
| Total | 6 | 106661g | 3.18 [2.56–3.97] | 77.4 | 0.200 | ⨁⨁⨁◯ |
| Male | 5 | 67192b | 3.29 [2.37–4.58] | 94.7 | 0.606 | ⨁⨁⨁◯ |
| Female | 5 | 100247b | 2.86 [2.05–3.98] | 95.6 | 0.507 | ⨁⨁⨁◯ |
| Mortality by cancer | ||||||
| Total | 16 | 203181 | 0.99 [0.88–1.11] | 75.0 | 0.854 | ⨁⨁◯◯ |
| Male | 9 | 73004b | 0.99 [0.93–1.06] | 0.0 | 0.681 | ⨁⨁◯◯ |
| Female | 9 | 104805c | 1.03 [0.87–1.21] | 79.2 | 0.901 | ⨁⨁◯◯ |
Legend. K, number of samples; N, sample size; The following authors did not report sample size: aBlack 1987, Laursen b2007, c2009 and (d) 2011, and eCastagnini 2013; Results of the following studies were excluded from analysis due to excessive asymmetry in the 95%CI: fTsuang 1980, gCallaghan 2014 and hAhrens 1995; * Based on Cochrane’s GRADE (Grading of Recommendations Assessment, Development and Evaluation). ** Not enough studies to calculate. GRADE: ⨁◯◯◯: very low; ⨁⨁◯◯: Low; ⨁⨁⨁◯: Moderate; ⨁⨁⨁⨁: High.
Mortality for specific causes
Mortality also was increased for infectious (RR = 4.38, 95%CI 1.51–12.70, p = 0.007, k = 3), respiratory (RR = 3.18, 95%CI 2.55–3.96, p < 0.001, k = 6), cardiovascular (RR = 1.76, 95%CI 1.53–2.02, p < 0.001, k = 27), and cerebrovascular (RR = 1.57, 95%CI 1.34–1.84, p < 0.001, k = 13), and causes. Mortality by cancer was the only specific cause that was not elevated in BD when compared to general population (RR = 0.99, 95%CI 0.88–1.11, p = 0.894, k = 16), as shown in Fig. 3. When stratified by sex, results were not significant for cancer but remained significant for all other causes of mortality. Although mortality by infectious (k = 3) and respiratory (k = 6) causes were found to be nearly twofold higher than cardiovascular (k = 27) and cerebrovascular (k = 13), their results came from a smaller number of studies, making a comparison not reliable.
Fig. 3.
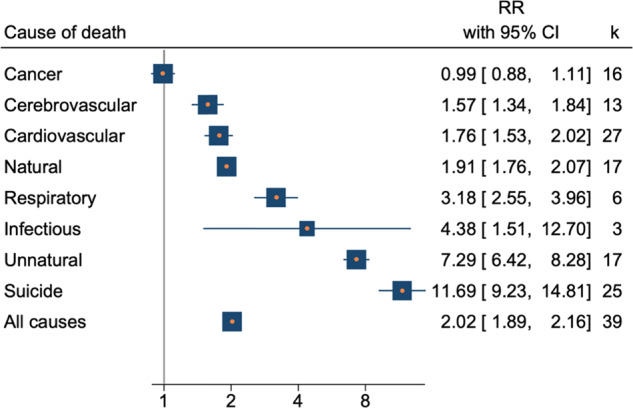
Forest plot of summary results.
A higher SMR was observed for suicide and unnatural causes in BD when compared to general population. RR for suicide was 11.69 (95%CI 9,22–14,81, p < 0.001, k = 25), When stratified by gender, suicide SMR was higher in woman (17.52 95%CI, 10.76–28.54, p < 0.001, k = 11) than in men (14,02, 95%CI 11.16–17.60, p < 0.001, k = 11). The SMR total for unnatural causes was 7,29 (IC95% 6.42-8.28, p < 0.001, k = 17). For males the RR for unnatural causes was 6.69 (95%CI 5.85–7.66, p < 0.001, k = 10), and for females the RR was 9.33 (8.07–10.78, p < 0.001, K = 11).
Only four of the main results were not considered statistically heterogeneous: mortality from cancer (Q = 7.9, p = 0.443, I2 = 0.0%), cerebrovascular (Q = 4.9, p = 0.559, I2 = 0.0%) and infectious (Q = 0.4, p = 0.521, I2 = 0.0%) causes in men, and mortality from infectious causes in women (Q = 0.3, p = 0.589, I2 = 0.0%). None of the meta-analyses of mortality for specific causes were found to present publication bias.
Prediction intervals showed that the range of the true effects remained significant only for mortality from natural causes, unnatural causes, and suicide. Cardiovascular and cerebrovascular causes were homogeneous distributed only in men with BD. Summary results for specific mortality are presented in Table 2.
Meta-regression and subgroup analysis
There was no difference in mortality between subgroups when analyzed by location, sample type, representativeness, study design, diagnostic criteria, use of structured interview, adjustment by substance use disorder and adjustment by time at risk (Table 3).
Table 3.
Results from subgroup analysis.
| Group | Sub-group | Population | Number of studies (k) | Risk ratio [95% CI] | I2 (%) | Group | Sub-group | Population | Number of studies (k) | Risk ratio [95% CI] | I2 (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Location | Africa | Total | 1 | NA | NA | Study design | Case–control | Total | 1 | NA | NA |
| Male | 0 | NA | NA | Male | 1 | NA | NA | ||||
| Female | 0 | NA | NA | Female | 1 | NA | NA | ||||
| Asia | Total | 6 | 2.33 [2.07–2.62] | 93.8 | Prospective | Total | 21 | 2.02 [1.84–2.21] | 94.0 | ||
| Male | 5 | 2.49 [2.36–2.63] | 46.3 | Male | 9 | 2.27 [2.02–2.56] | 84.7 | ||||
| Female | 5 | 2.67 [2.44–2.93] | 73.1 | Female | 10 | 2.32 [2.11–2.55] | 78.4 | ||||
| Europe | Total | 26 | 2.02 [1.85–2.20] | 97.2 | Retrospective | Total | 17 | 1.95 [1.76–2.17] | 98.1 | ||
| Male | 15 | 2.25 [2.06–2.46] | 89.5 | Male | 13 | 2.21 [2.04–2.41] | 89.4 | ||||
| Female | 13 | 2.17 [1.94–2.42] | 94.4 | Female | 11 | 2.13 [1.87–2.43] | 96.0 | ||||
| North America | Total | 5 | 1.83 [1.40–2.39] | 81.9 | Diagnostic criteria | DSM | Total | 5 | 1.83 [1.37–2.46] | 86.4 | |
| Male | 2 | 1.99 [1.53–2.59] | 12.5 | Male | 3 | 1.93 [1.45–2.58] | 30.6 | ||||
| Female | 3 | 2.14 [1.73–2.64] | 0.0 | Female | 3 | 1.95 [1.09–3.49] | 78.9 | ||||
| Other | Total | 1 | NA | NA | ICD | Total | 25 | 2.07 [1.91–2.24] | 97.8 | ||
| Male | 1 | NA | NA | Male | 17 | 2.30 [2.15–2.47] | 90.0 | ||||
| Female | 1 | NA | NA | Female | 15 | 2.31 [2.11–2.54] | 95.2 | ||||
| Sample type | Community | Total | 20 | 2.05 [1.90–2.21] | 95.8 | Other | Total | 6 | 1.90 [1.40–2.58] | 74.8 | |
| Male | 11 | 2.25 [2.08–2.44] | 89.9 | Male | 0 | NA | NA | ||||
| Female | 11 | 2.32 [2.11–2.56] | 94.1 | Female | 1 | NA | NA | ||||
| Inpatient | Total | 17 | 2.05 [1.80–2.34] | 97.5 | Blank | Total | 3 | 1.88 [1.12–3.13] | 92.5 | ||
| Male | 10 | 2.44 [2.12–2.80] | 87.2 | Male | 3 | 1.72 [0.94–3.14] | 86.8 | ||||
| Female | 9 | 2.26 [1.81–2.83] | 94.4 | Female | 3 | 2.17 [1.40–3.35] | 81.0 | ||||
| Outpatient | Total | 2 | 1.51 [1.11–2.05] | 42.7 | |||||||
| Male | 2 | 1.29 [0.70–2.37] | 61.4 | ||||||||
| Female | 2 | 1.74 [1.31–2.31] | 0.0 | ||||||||
| Representative | Yes | Total | 18 | 2.04 [1.88–2.21] | 96.2 | Use of structured interview | SI Yes | Total | 7 | 1.63 [1.39–1.92] | 58.8 |
| Male | 11 | 2.25 [2.08–2.44] | 89.9 | Male | 4 | 2.07 [0.86–5.00] | 92.8 | ||||
| Female | 11 | 2.30 [2.08–2.54] | 94.2 | Female | 3 | 1.51 [1.15–2.00] | 24.1 | ||||
| No | Total | 21 | 2.01 [1.78–2.27] | 96.9 | SI No | Total | 32 | 2.08 [1.94–2.24] | 97.2 | ||
| Male | 12 | 2.31 [2.01–2.64] | 86.6 | Male | 19 | 2.27 [2.13–2.41] | 87.1 | ||||
| Female | 11 | 2.22 [1.82–2.70] | 93.1 | Female | 19 | 2.34 [2.14 - 2.55] | 94.0 | ||||
| Adjusted by SUD | SUD Yes | Total | 4 | 1.95 [1.41–2.70] | 95.0 | Adjusted by time-at-risk | Time Yes | Total | 7 | 1.94 [1.60–2.35] | 98.8 |
| Male | 2 | 2.37 [1.71–3.28] | 89.8 | Male | 4 | 2.37 [2.20–2.54] | 78.3 | ||||
| Female | 2 | 2.62 [2.05–3.37] | 85.0 | Female | 3 | 2.66 [2.49–2.84] | 66 | ||||
| SUD No | Total | 35 | 2.03 [1.89–2.17] | 96.9 | Time No | Total | 32 | 2.04 [1.90–2.19] | 95.3 | ||
| Male | 21 | 2.26 [2.11–2.43] | 88.1 | Male | 19 | 2.25 [2.05–2.46] | 88.0 | ||||
| Female | 20 | 2.22 [2.02–2.44] | 93.9 | Female | 19 | 2.19 [1.99–2.42] | 92.2 |
Meta-regression showed no influence in results in proportion of females (p = 0.577) and sample size (p = 0.228). Sociodemographic variables could not be considered a source of heterogeneity: SDI (p = 0.319), HDI (p = 0.398) and mid-point year (p = 0.578). None of the variables that affect the quality of the studies were significantly related to RR: NOS (p = 0.433) and mean follow-up years (p = 0.219). When analyzed separately, SMR heterogeneity was 96.7% and HR heterogeneity was 94.4%. Finally, the exclusion of different outcomes did not decrease heterogeneity.
Level of certainty of the results
Based on the GRADE, the mortality for unnatural causes and suicide showed a high level of certainty, while mortality for all causes and respiratory causes were rated as moderate level of certainty. Evidence for cancer, cardiovascular and cerebrovascular mortality reached a low level of certainty (Table 2). A summary of findings of the GRADE evidence profile can be found as Supplementary Material in Table S6.
Discussion
The current meta-analysis aimed to systematically review studies regarding mortality by any and specific causes in BD. Results found that individuals with BD have a twofold increased risk of premature mortality when compared to the general population. The largest effect size emerged for suicide, whose risk was 11 times higher in BD, especially in women (17 times higher). Mortality by natural, infectious, respiratory, cardiovascular, and cerebrovascular causes was also elevated in BD. Cancer was the only studied cause with a mortality rate that was not significatively higher in BD.
Over the last years, more attention has been paid to the study of mortality in mental disorders. Although less studied when compared to other disorders (such as schizophrenia and unipolar depression), more evidence has emerged on the increased mortality in individuals with BD [11, 16, 17, 124–126]. Previous studies have assessed mortality in individuals with BD, however a novel and robust systematic review and meta-analysis of mortality in BD was needed, given that the previous reviews did not include the quality assessment, certainty of evidence, rigorous inclusion criteria and a robust assessment of heterogeneity. In contrast to earlier studies, our study provides a detailed analysis about general and specific mortality causes in BD, including not only studies that provided SMR, but a range of studies with other effect measures as RR, HR, MRR, and OR. This approach allows the inclusion of a larger sample, hence better representing the general population of individuals with BD. Our research was able to include 57 studies from 16 different countries (while the meta-analysis from Hayes included 31 studies) and comprised more than twice as many subjects with BD than the previous largest meta-analysis (678 353 vs. 305 859) [17]
In 2020 World Health Organization reported that the leading causes of death in the general population were ischemic heart disease and stroke [127]. In our study, we found an increase of mortality 1.76 and 1.91 times by cardiovascular and cerebrovascular causes in the BD population, respectively. Although different cardiovascular diseases (coronary disease, atherosclerotic disease, arrhythmias, and valvular diseases) can have a different impact on mortality we could not analyze separately the weight of each cause in mortality mainly because the assessment of these causes within the studies were through ICD groups that did not differentiate specific cardiovascular diseases (i.e., I00-I52; I70-I79). Unfortunately, most systems of healthcare are not configured to adequately prevent, diagnose, and treat medical comorbidity in the mood disorder population [128, 129]. Indeed, people with mental disorder do receive lower quality of screening and care for cardiovascular diseases [130].
Risk of natural causes death was almost two times higher in BD, even though natural causes account for most deaths in this population. It is essential that prevention strategies, such as investment in measures to reduce cardiovascular risk factors, begin to be implemented in this population early on. Some ways to reduce these risk factors are through psychoeducation of the target population, encouraging measures that impact adherence to drug treatment, as well as the implementation of programs that engage this population in physical activity, investment in a healthy diet, tobacco cessation, and obesity control. Thus, aiming to better establish functional and effective public health policies, may yield a possible reduction in the impact of modifiable risk factors on mortality in the BD population. Although, it is important to emphasize that this review did not evaluate the weight of risk factors in all and specific-cause mortality in the BD population.
We hypothesize that the increase in respiratory mortality is mainly due to the high index of tobacco use in this population. It is well known that tobacco smoking is 2–3 times higher in bipolar disorder, with estimates ranging from 60–70% in bipolar patients compared to 25–30% in the general population [131]. Unfortunately, the studies included in this meta-analysis did not report rates of smokers, so we could not calculate the weight of tobacco use in the mortality among bipolar disorder individuals. Regarding the increase of infectious mortality in the bipolar disorder population, one possible mechanism is the vulnerability that the lifestyle of the BD population is involved, such as a higher prevalence of substance use, such as alcohol and tobacco, poor diet, and higher rates of sedentarism. These behaviors can negatively impact the immune system response, contributing to a mortality increase in this population.
Cancer was the only cause of death without increase in BD population. Previous metanalyses have shown similar results, however new evidence of increase of mortality by cancer in BD has emerged in the last years [54, 132]. Our main hypothesis is that the factors involved in our findings were related to lower survival in BD subjects than in the general population associated to the fact that cancer is a disease affecting predominantly the late adult or elderly population, and the underdiagnosis of cancer in this population related to disease stigma, lower seeking for medical help, and the difficulties of a proper stage treatment [132, 133]. The lack of significance difference in mortality risk in the analyzed samples might be due to lower screening rates and the risk of missed cancer diagnoses in people with mental disorders compared with the general population. Although, more studies are needed to confirm this hypothesis.
As showed by our data, in agreement with previous literature, the RR for suicide and unnatural causes of death was significative higher in BD than in the general population, namely 11 times increased in BD individuals. Suicide is the leading cause of preventable death [117]. Our findings lead us to an understanding that is necessary an effort to prevent suicide mainly
in the high-risk BD. The improvement of these indices can occur by public health policies implementation through access to information about suicide, training of health professionals to evaluate and manage risk cases, early diagnosis, and implementation of public health policies to prevent suicide [134, 135].
Considering the findings of this study, it is essential to think in how early diagnosis in BD may have an impact on the prevention of disease episodes, clinical comorbidities, adherence to treatment and, consequently, reducing mortality in this group.
Some limitations should be considered. Observational studies in the field of psychiatry are often fraught with several biases (e.g., reverse causation) and also by a poor control of confounders even in large-scale, nationwide, studies [136]. Factors such as disease subtype or symptomatic burden, were not reported in the majority of the included studies. Because of this limitation we were not able to take into account these factors in statistical analysis. Another limitation we could not calculate the mean age of the sample to perform a meta-regression as most of the samples were from observational studies (only eight studies provide mean age), then age was not explored as a source of heterogeneity.
From the statistical point of view, we were not able to find clear sources of heterogeneity based on the classical meta-regression method. Interpreting heterogeneity has been a persistent difficulty in meta-analyses of prevalence studies, which often present high I2 values. Even though, a high I2 value is not always synonymous with high heterogeneity. In meta-analyses of prevalence, I2 statistics may not be discriminative and should be interpreted with caution, avoiding arbitrary thresholds [26].
Prediction intervals predict the range of effect size for any subject randomly assigned from the population in 95% of the time [28] and reflect the variation in treatment effects over different settings, including over future patients [29]. They have been proposed to have a better appreciation of the uncertainty around the effect estimate than CI when heterogeneity is substantial [30] and has been currently recommended in meta-analyses, especially from prevalence studies [27–29]. The prediction Interval of all-cause mortality was 1.37 to 2.98. This interval is entirely above 1 and shows that mortality is elevated when applied in at least 95% of the individual setting. The same rationale can be applied to mortality for suicide (prediction interval 3.71 to 36.90) and respiratory causes (prediction interval 1.65 to 6.12). On the other hand, the prediction interval for cardiovascular (0.87 to 3.58), cerebrovascular (0.91 to 2.70) and cancer (0.67 to 1.46) contain values below 1 and so, although on average the mortality seems to be higher, it may not always be true in an individual setting. In these cases, further research is needed to identify sources of heterogeneity.
The CI higher than one indicates that there is robust evidence to conclude that mortality is higher in most individuals with BD. However, the prediction interval containing it indicates that mortality is heterogeneously distributed, and this result does not apply to 95% of individuals with BD, as CI would suggest. Consequently, there must be factors that hinder mortality for cardiovascular, cerebrovascular, and natural causes to be higher. This rationale has important clinical implications. Now, it is an important topic to explore which characteristics make an individual with BD less susceptible to premature death.
We then conducted meta-regressions to test whether sociodemographic and methodological factors could represent such characteristics. Our study found an I2 of 96.8%, and I2 tells us what proportion of the variance is due to variation in real effects rather than sampling error [27]. It can be interpreted as 3.2% of the differences in mortality are due to sampling or population differences. Hence, it was expected beforehand that meta-regression of sociodemographic characteristics would fail to find differences in heterogeneity. Then, methodological aspects are expected to be relevant. Although not measurable herein, some methodological features can be quoted as potential sources of heterogeneity and further included in studies on mortality in BD, namely: quality of epidemiological data (are databases complete and reliable?), quality of care (could an efficient and accessible health system counterbalance the increased mortality risk in individuals with BD?), and assessment of clinical and psychiatric comorbidities (is there any confounding factor moderating the mortality risk in individuals with BD?).
Conclusion
According to this meta-analysis, the highest RR for mortality in individuals with BD emerged for suicide, infectious, respiratory, cardiovascular, and cerebrovascular causes. Large-scale and well-designed studies are still needed to identify the main moderators and mediators of premature mortality in the population. Also, efforts must be made to prevent suicide and unnatural mortality causes in the high-risk BD population and to investigate and treat physical comorbidities. Further research should be undertaken to identify modifiable factors that might be targeted by interventions to reduce this gap.
Supplementary information
Acknowledgements
TBB and GHB are joint first authors of this paper. BL and MS contributed equally as senior authors to this work. LSR was supported by CAPES Scholarship 88887.475730/2020-00 during the preparation of this manuscript. CAPES Scholarship had no role in writing the manuscript or the decision to submit it for publication. This research received support from the Baszucki Brain Research Fund for publication-related expenses.
Author contributions
TBB, GHB and BL were responsible for the study concept and design. TBB, GHB, LT and LSR were responsible for the literature search, study selection, data extraction and quality assessment. TBB, GHB, BL, MS, ED and AFC were responsible for planning and performing the statistical analysis. All authors interpreted the data and wrote the manuscript. BL and MS were responsible for the supervision of the work.
Competing interests
MS has received honoraria/has been a consultant for Angelini, Lundbeck, Otsuka.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Taís Boeira Biazus, Gabriel Henrique Beraldi, Marco Solmi, Beny Lafer.
Supplementary information
The online version contains supplementary material available at 10.1038/s41380-023-02109-9.
References
- 1.Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27:281–95. doi: 10.1038/s41380-021-01161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alonso J, Petukhova M, Vilagut G, Chatterji S, Heeringa S, Stün U¨, et al. Days out of role due to common physical and mental conditions: results from the WHO World Mental Health surveys. Mol Psychiatry. 2011;16:1234–46. doi: 10.1038/mp.2010.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, et al. Bipolar disorders. Nat Rev Dis Primers. 2018;4. https://pubmed.ncbi.nlm.nih.gov/29516993/. [DOI] [PubMed]
- 4.Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet. 2016;387:1561–72. doi: 10.1016/S0140-6736(15)00241-X. [DOI] [PubMed] [Google Scholar]
- 5.Colton CW, Manderscheid RW. PEER REVIEWED: congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3:1–14. [PMC free article] [PubMed] [Google Scholar]
- 6.Vieta E, Salagre E, Grande I, Carvalho AF, Fernandes BS, Berk M, et al. Early intervention in bipolar disorder. Am J Psychiatry. 2018;175:411–26. doi: 10.1176/appi.ajp.2017.17090972. [DOI] [PubMed] [Google Scholar]
- 7.Machado MO, Veronese N, Sanches M, Stubbs B, Koyanagi A, Thompson T, et al. The association of depression and all-cause and cause-specific mortality: An umbrella review of systematic reviews and meta-analyses. BMC Med. 2018;16:1–13. doi: 10.1186/s12916-018-1101-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Correll CU, Solmi M, Croatto G, Schneider LK, Rohani-Montez SC, Fairley L, et al. Mortality in people with schizophrenia: a systematic review and meta- analysis of relative risk and aggravating or attenuating factors. World Psychiatry. 2022 Jun [cited 2022 Jul 16];21:248–71. https://pubmed.ncbi.nlm.nih.gov/35524619/. [DOI] [PMC free article] [PubMed]
- 9.Bratfos O, Haug JO. The course of manic-depressive psychosis: a follow-up investigation of 215 patients. Acta Psychiatr Scand. 1968;44:89–112. doi: 10.1111/j.1600-0447.1968.tb07637.x. [DOI] [PubMed] [Google Scholar]
- 10.Guze SB, Robins E. Suicide and primary affective disorders. Br J Psychiatry. 1970;117:437–8. doi: 10.1192/bjp.117.539.437. [DOI] [PubMed] [Google Scholar]
- 11.Roshanaei-Moghaddam B, Katon W. Premature mortality from general medical illnesses among persons with bipolar disorder: a review. Psychiatr Serv. 2009;60:147–56. doi: 10.1176/ps.2009.60.2.147. [DOI] [PubMed] [Google Scholar]
- 12.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet. 2013;382:1575–86. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 13.Solmi M, Fiedorowicz J, Poddighe L, Delogu M, Miola A, Høye A, et al. Disparities in screening and treatment of cardiovascular diseases in patients with mental disorders across the world: systematic review and meta- analysis of 47 observational studies. Am J Psychiatry. 2021;178:793–803. doi: 10.1176/appi.ajp.2021.21010031. [DOI] [PubMed] [Google Scholar]
- 14.Vancampfort D, Correll CU, Galling B, Probst M, de Hert M, Ward PB, et al. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta-analysis. World Psychiatry. 2016;15:166–74. doi: 10.1002/wps.20309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldstein BI, Baune BT, Bond DJ, Chen PH, Eyler L, Fagiolini A, et al. Call to action regarding the vascular-bipolar link: A report from the Vascular Task Force of the International Society for Bipolar Disorders. Bipolar Disord. 2020;22:440–60. doi: 10.1111/bdi.12921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry. 1998;173:11–53. doi: 10.1192/bjp.173.1.11. [DOI] [PubMed] [Google Scholar]
- 17.Hayes JF, Miles J, Walters K, King M, Osborn DP. A systematic review and meta-analysis of premature mortality in bipolar affective disorder. Acta Psychiatr Scand. 2015;131:417–25. doi: 10.1111/acps.12408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Delgado M. Critique of a systematic review and meta-analysis of premature mortality in bipolar affective disorder. Acta Psychiatr Scand. 2015;132:315. doi: 10.1111/acps.12432. [DOI] [PubMed] [Google Scholar]
- 19.Dreier M. Quality assessment in meta-analysis. 2013;213–28. https://link.springer.com/chapter/10.1007/978-3-642-37131-8_13.
- 20.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. https://pubmed.ncbi.nlm.nih.gov/33782057/. [DOI] [PMC free article] [PubMed]
- 21.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 22.Covidence systematic review software. Melbourne, Australia: Veritas Health Innovation.
- 23.George A, Stead TS, Ganti L What’s the risk: differentiating risk ratios, odds ratios, and hazard ratios? Cureus. 2020;12. https://pubmed.ncbi.nlm.nih.gov/32983737/. [DOI] [PMC free article] [PubMed]
- 24.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 26.Borges Migliavaca C, Stein C, Colpani V, Timothy, Barker H, Ziegelmann PK, et al. Meta-analysis of prevalence: I2 statistic and how to deal with heterogeneity. Res Synth Methods. 2022 Feb [cited 2022 Apr 23]; https://onlinelibrary.wiley.com/doi/full/10.1002/jrsm.1547. [DOI] [PubMed]
- 27.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sterne JAC, Becker BJ, Egger M The Funnel Plot. In 2006.
- 29.Wells GA, Wells G, Shea B, Shea B, O’Connell D, Peterson J, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. In 2014.
- 30.Human Development Index (HDI) by Country 2022 [Internet]. [cited 2022 Oct 14]. https://worldpopulationreview.com/country-rankings/hdi-by-country.
- 31.Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019 | GHDx [Internet]. [cited 2022 Oct 14]. https://ghdx.healthdata.org/record/ihme-data/gbd-2019-socio-demographic-index-sdi-1950-2019.
- 32.Schünemann HJ. Interpreting GRADE’s levels of certainty or quality of the evidence: GRADE for statisticians, considering review information size or less emphasis on imprecision? Journal of clinical epidemiology. 2016;75:6–15. doi: 10.1016/j.jclinepi.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 33.Laursen TM, Wahlbeck K, Hällgren J, Westman J, Ösby U, Alinaghizadeh H, et al. Life Expectancy and Death by Diseases of the Circulatory System in Patients with Bipolar Disorder or Schizophrenia in the Nordic Countries. PLoS One. 2013;8. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L369200131. [DOI] [PMC free article] [PubMed]
- 34.Osborn DPJ, Levy G, Nazareth I, Petersen I, Islam A, King MB Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s general practice research database. Arch Gen Psychiatry. 2007;64:242–9. http://ezproxy.libproxy.db.erau.edu/login?url=https://www.proquest.com/docview/621873129?accountid=27203. [DOI] [PubMed]
- 35.Osborn D, Levy G, Nazareth I, King M. Suicide and severe mental illnesses. Cohort study within the UK general practice research database. Schizophr Res. 2008;99:134–8. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L50023537. [DOI] [PubMed]
- 36.Ahrens B, Müller-Oerlinghausen B, Schou M, Wolf T. Excess cardiovascular and suicide mortality of affective disorders may be reduced by lithium prophylaxis. J Affect Disord. 1995;33:67–75. doi: 10.1016/0165-0327(94)00074-j. [DOI] [PubMed] [Google Scholar]
- 37.Ajetunmobi O, Taylor M, Stockton D, Wood R. Early death in those previously hospitalised for mental healthcare in Scotland: a nationwide cohort study, 1986- 2010. BMJ Open. 2013;3:9. doi: 10.1136/bmjopen-2013-002768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Almeida OP, McCaul K, Hankey GJ, Yeap BB, Golledge J, Flicker L Suicide in older men: The health in men cohort study (HIMS). Prev Med (Baltim) [Internet]. 2016;93((Almeida O.P., osvaldo.almeida@uwa.edu.au) School of Psychiatry & Clinical Neurosciences, University of Western Australia, Perth, Australia(Almeida O.P., osvaldo.almeida@uwa.edu.au; McCaul K.; Flicker L.) WA Centre for Health & Ageing of Centre for Medica):33–8. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L612350152. [DOI] [PubMed]
- 39.Angst F, Stassen HH, Clayton PJ, Angst J Mortality of patients with mood disorders: follow-up over 34-38 years. J Affect Disord. 2002;68:167–81. http://ezproxy.libproxy.db.erau.edu/login?url=https://www.proquest.com/docview/71810101?accountid=27203. [DOI] [PubMed]
- 40.Angst J, Angst F, Gerber-Werder R, Gamma A. Suicide in 406 mood-disorder patients with and without long-term medication: A 40 to 44 years’ follow-up. Arch Suicide Res. 2005;9:279–300. doi: 10.1080/13811110590929488. [DOI] [PubMed] [Google Scholar]
- 41.Angst J, Hengartner MP, Gamma A, D VZ, Angst F. Mortality of 403 patients with mood disorders 48 to 52 years after their psychiatric hospitalisation. Eur Arch Psychiatry Clin Neurosci. 2013;263:425–34. doi: 10.1007/s00406-012-0380-1. [DOI] [PubMed] [Google Scholar]
- 42.Black DW, Winokur G, Nasrallah A. Mortality in patients with primary unipolar depression, secondary unipolar depression, and bipolar affective disorder: A comparison with general population mortality. Int J Psychiatry Med. 1987;17:351–60. http://ezproxy.libproxy.db.erau.edu/login?url=https://search.proquest.com/docview/617514164?accountid=27203. [DOI] [PubMed]
- 43.Callaghan RC, Veldhuizen S, Jeysingh T, Orlan C, Graham C, Kakouris G, et al. Patterns of tobacco-related mortality among individuals diagnosed with schizophrenia, bipolar disorder, or depression. J Psychiatr Res. 2014;48:102–10. doi: 10.1016/j.jpsychires.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 44.Castagnini A, Foldager L, Bertelsen A. Excess mortality of acute and transient psychotic disorders: comparison with bipolar affective disorder and schizophrenia. Acta Psychiatr Scand. 2013;128:370–5. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L52406024. [DOI] [PubMed]
- 45.C.-K. C, Hayes RD, Broadbent M, Fernandes AC, Lee W, Hotopf M, et al. All- cause mortality among people with serious mental illness (SMI), substance use disorders, and depressive disorders in southeast London: a cohort study. BMC Psychiatry. 2010;10 ((Chang C.-K., chin-kuo.chang@kcl.ac.uk; Hayes R.D., richard.hayes@kcl.ac.uk; Broadbent M., matthew.broadbent@kcl.ac.uk; Fernandes A.C., andrea.1.fernandes@kcl.ac.uk; Stewart R., robert.stewart@kcl.ac.uk) King’s College London, Section of Epidemiology, Dep). http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L51096081. [DOI] [PMC free article] [PubMed]
- 46.J-C C, H-H C, Yen AMF, Chen SLS, C-S L. Survival of bipolar depression, other type of depression and comorbid ailments: Ten-year longitudinal follow- up of 10,922 Taiwanese patients with depressive disorders (KCIS no. PSY1) J Psychiatr Res. 2012;46:1442–8. doi: 10.1016/j.jpsychires.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 47.Chen YH, Lee HC, Lin HC. Mortality among psychiatric patients in Taiwan- Results from a universal National Health Insurance programme. Psychiatry Res. 2010;178:160–5. doi: 10.1016/j.psychres.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 48.Choi JW, Lee KS, Kim TH, Choi J, Han E. Suicide risk after discharge from psychiatric care in South Korea. J Affect Disord. 2019;251:287–92. doi: 10.1016/j.jad.2019.03.079. [DOI] [PubMed] [Google Scholar]
- 49.Crump C, Sundquist K, Winkleby MA, Sundquist J Comorbidities and mortality in bipolar disorder: A Swedish national cohort study. JAMA Psychiatry. 2013;70:931–9. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L369754127. [DOI] [PubMed]
- 50.Dutta R, Boydell J, Kennedy N, VAN Jim OS, Fearon P, Murray RM. Suicide and other causes of mortality in bipolar disorder: a longitudinal study. Psychol Med. 2007;37:839–47. doi: 10.1017/S0033291707000347. [DOI] [PubMed] [Google Scholar]
- 51.Fekadu A, Medhin G, Kebede D, Alem A, Cleare AJ, Prince M, et al. Excess mortality in severe mental illness: 10-year population-based cohort study in rural Ethiopia. Br J Psychiatry. 2015;206:289–96. doi: 10.1192/bjp.bp.114.149112. [DOI] [PubMed] [Google Scholar]
- 52.Fiedorowicz JG, Solomon DA, Endicott J, Leon AC, Li C, Rice JP, et al. Manic/hypomanic symptom burden and cardiovascular mortality in bipolar disorder. Psychosom Med. 2009;71:598–606. doi: 10.1097/PSY.0b013e3181acee26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gale CR, Batty GD, Osborn DPJ, Tynelius P, Whitley E, Rasmussen F. Association of mental disorders in early adulthood and later psychiatric hospital admissions and mortality in a cohort study of more than 1 million men. Arch Gen Psychiatry. 2012;69:823–31. doi: 10.1001/archgenpsychiatry.2011.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guan NC, Termorshuizen F, Laan W, Smeets HM, Zainal NZ, Kahn RS, et al. Cancer mortality in patients with psychiatric diagnoses: A higher hazard of cancer death does not lead to a higher cumulative risk of dying from cancer. Soc Psychiatry Psychiatric Epidemiol. 2013;48:1289–95. doi: 10.1007/s00127-012-0612-8. [DOI] [PubMed] [Google Scholar]
- 55.Hayes JF, Marston L, Walters K, King MB, Osborn DPJ. Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000- 2014. British Journal of Psychiatry. 2017;211:175–81. doi: 10.1192/bjp.bp.117.202606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hjorthøj C, Østergaard MLD, Benros ME, Toftdahl NG, Erlangsen A, Andersen JT, et al. Association between alcohol and substance use disorders and all-cause and cause-specific mortality in schizophrenia, bipolar disorder, and unipolar depression: A nationwide, prospective, register-based study. Lancet Psychiatry. 2015;2:801–8. doi: 10.1016/S2215-0366(15)00207-2. [DOI] [PubMed] [Google Scholar]
- 57.Hoang U, Stewart R, Goldacre MJ Mortality after hospital discharge for people with schizophrenia or bipolar disorder: Retrospective study of linked English hospital episode statistics, 1999-2006. BMJ (Online). 2011;343. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L362626739. [DOI] [PMC free article] [PubMed]
- 58.Hoang U, Goldacre MJ, Stewart R Avoidable mortality in people with schizophrenia or bipolar disorder in England. Acta Psychiatr Scand. 2013;127:195–201. [DOI] [PubMed]
- 59.Høye A, Nesvåg R, Reichborn-Kjennerud T, Jacobsen BK. Sex differences in mortality among patients admitted with affective disorders in North Norway: A 33-year prospective register study. Bipolar Disord. 2016;18:272–81. doi: 10.1111/bdi.12389. [DOI] [PubMed] [Google Scholar]
- 60.Kay DWK, Petterson U. VI. Mortality. Acta Psychiatr Scand. 1977;56:55–60. doi: 10.1111/j.1600-0447.1977.tb10824.x. [DOI] [Google Scholar]
- 61.Kim W, S.-Y. J, T.-H. L, Lee JE, E.-C. P. Association between continuity of care and subsequent hospitalization and mortality in patients with mood disorders: Results from the Korea National Health Insurance cohort. PLoS One. 2018;13. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L624971680. [DOI] [PMC free article] [PubMed]
- 62.Kodesh A, Goldshtein I, Gelkopf M, Goren I, Chodick G, Shalev V. Epidemiology and comorbidity of severe mental illnesses in the community: findings from a computerized mental health registry in a large Israeli health organization. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1775–82. doi: 10.1007/s00127-012-0478-9. [DOI] [PubMed] [Google Scholar]
- 63.Laursen TM, Munk-Olsen T, Agerbo E, Gasse C, Mortensen PB. Somatic hospital contacts, invasive cardiac procedures, and mortality from heart disease in patients with severe mental disorder. Arch Gen Psychiatry. 2009;66:713–20. doi: 10.1001/archgenpsychiatry.2009.61. [DOI] [PubMed] [Google Scholar]
- 64.Laursen TM, Wahlbeck K, Hällgren J, Westman J, Ösby U, Alinaghizadeh H, et al. Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the nordic countries. PLoS One. 2013;8:e67133. doi: 10.1371/journal.pone.0067133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lomholt LH, Andersen DV, Sejrsgaard-Jacobsen C, Øzdemir CM, Graff C, Schjerning O, et al. Mortality rate trends in patients diagnosed with schizophrenia or bipolar disorder: a nationwide study with 20 years of follow- up. Int J Bipolar Disord. 2019;7. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L626706259. [DOI] [PMC free article] [PubMed]
- 66.Medici CR, Videbech P, Gustafsson LN, Munk-Jørgensen P Mortality and secular trend in the incidence of bipolar disorder. J Affect Disord. 2015;183 ((Medici C.R., Clara.reece.medici@post.au.dk; Gustafsson L.N.; Munk-Jørgensen P.) Aarhus University Hospital, Skovagervej 2, Risskov, Denmark(Videbech P.) Psychiatric Center Glostrup, Glostrup, Denmark):1–6. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L604446456. [DOI] [PubMed]
- 67.Mohamed MO, Rashid M, Farooq S, Siddiqui N, Parwani P, Shiers D, et al. Acute myocardial infarction in severe mental illness: prevalence, clinical outcomes, and process of care in US hospitalizations. Can J Cardiol. 2019;35:821–30. doi: 10.1016/j.cjca.2019.04.021. [DOI] [PubMed] [Google Scholar]
- 68.Newman SC, Bland RC. Suicide risk varies by subtype of affective disorder. Acta Psychiatr Scand. 1991;83:420–6. doi: 10.1111/j.1600-0447.1991.tb05568.x. [DOI] [PubMed] [Google Scholar]
- 69.Norton B, Whalley LJ. Mortality of a lithium-treated population. Br J Psychiatry. 1984;145:277–82. doi: 10.1192/bjp.145.3.277. [DOI] [PubMed] [Google Scholar]
- 70.Osborn D, Levy G, Nazareth I, King M. Suicide and severe mental illnesses. Cohort study within the UK general practice research database. Schizophr Res. 2008;99:134–8. doi: 10.1016/j.schres.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 71.Ösby U, Brandt L, Correia N, Ekbom A, Sparén P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58:844–50. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- 72.Pan YJ, Yeh LL, Chan HY, Chang CK. Transformation of excess mortality in people with schizophrenia and bipolar disorder in Taiwan. Psychol Med. 2017;47:2483–93. doi: 10.1017/S0033291717001040. [DOI] [PubMed] [Google Scholar]
- 73.Pan YJ, Yeh LL, Chan HY, Chang CK. Excess mortality and shortened life expectancy in people with major mental illnesses in Taiwan. Epidemiol Psychiatr Sci. 2020;29:e156. doi: 10.1017/S2045796020000694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Park S, Rim SJ, Jo M, Lee MG, Kim CE Comorbidity of Alcohol Use and Other Psychiatric Disorders and Suicide Mortality: Data from the South Korean National Health Insurance Cohort, 2002 to 2013. Alcohol Clin Exp Res. 2019;43:842–9. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L626985240. [DOI] [PubMed]
- 75.Ramsey CM, Spiraa AP, Mojtabai R, Eaton WW, Roth K, Leeb HB. Lifetime manic spectrum episodes and all-cause mortality: 26-year follow-up of the NIMH epidemiologic catchment area study. J Affect Disord. 2013;151:337–42. doi: 10.1016/j.jad.2013.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Saku M, Tokudome S, Ikeda M, Kono S, Makimoto K, Uchimura H, et al. Mortality in psychiatric patients, with a specific focus on cancer mortality associated with schizophrenia. Int J Epidemiol. 1995;24:366–72. doi: 10.1093/ije/24.2.366. [DOI] [PubMed] [Google Scholar]
- 77.Schaffer A, Sinyor M, Reis C, Goldstein BI, Levitt AJ. Suicide in bipolar disorder: Characteristics and subgroups. Bipolar Disord. 2014;16:732–40. doi: 10.1111/bdi.12219. [DOI] [PubMed] [Google Scholar]
- 78.Schneider B, Müller MJ, Philipp M. Mortality in affective disorders. J Affect Disord. 2001;65:263–74. doi: 10.1016/S0165-0327(00)00290-1. [DOI] [PubMed] [Google Scholar]
- 79.Schulman-Marcus J, Goyal P, Swaminathan RV, Feldman DN, S-C W, Singh HS, et al. Comparison of trends in incidence, revascularization, and in- hospital mortality in ST-elevation myocardial infarction in patients with versus without severe mental illness. Am J Cardiol. 2016;117:1405–10. doi: 10.1016/j.amjcard.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 80.Sharma R, Markar HR. Mortality in affective disorder. J Affect Disord. 1994;31:91–6. doi: 10.1016/0165-0327(94)90112-0. [DOI] [PubMed] [Google Scholar]
- 81.Tsuang MT, Woolson RF, Fleming JA. Causes of death in schizophrenia and manic-depression. Br J Psychiatry. 1980;136:239–42. doi: 10.1192/bjp.136.3.239. [DOI] [PubMed] [Google Scholar]
- 82.Vinogradova Y, Coupland C, Hippisley-Cox J, Whyte S, Penny C. Effects of severe mental illness on survival of people with diabetes. Br J Psychiatry. 2010;197:272–7. doi: 10.1192/bjp.bp.109.074674. [DOI] [PubMed] [Google Scholar]
- 83.Webb RT, Lichtenstein P, Larsson H, Geddes JR, Fazel S. Suicide, hospital- presenting suicide attempts, and criminality in bipolar disorder: examination of risk for multiple adverse outcomes. J Clin Psychiatry. 2014;75:E809-+. doi: 10.4088/JCP.13m08899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Weeke A, Juel K, Væth M. Cardiovascular death and manic-depressive psychosis. J Affect Disord. 1987;13:287–92. doi: 10.1016/0165-0327(87)90049-8. [DOI] [PubMed] [Google Scholar]
- 85.Westman J, Hallgren J, Wahlbeck K, Erlinge D, Alfredsson L, Osby U Cardiovascular mortality in bipolar disorder: a population-based cohort study in Sweden. BMJ Open. 2013;3:8. [DOI] [PMC free article] [PubMed]
- 86.H-H Y, Westphal J, Hu Y, Peterson EL, L KW, Prabhakar D, et al. Diagnosed mental health conditions and risk of suicide mortality. Psychiatric Services. 2019;70:750–7. doi: 10.1176/appi.ps.201800346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.P.-H. C, S.-Y. T, C.-H. P, H.-M. C, Y.-L. C, S.-S. S, et al. Incidence and risk factors of sudden cardiac death in bipolar disorder across the lifespan. J Affect Disord. 2020;274 ((Chen P.-H.; Tsai S.-Y.) Department of Psychiatry, Taipei Medical University Hospital, Taipei, Taiwan(Chen P.-H.; Tsai S.-Y.; Kuo C.-J., tcpckuo@seed.net.tw) Psychiatric Research Center, Taipei Medical University Hospital, Taipei, Taiwan(Chen P.-H.; Tsai):210–7. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L2006025669. [DOI] [PubMed]
- 88.Laursen TM, Munk-Olsen T, Gasse C. Chronic somatic comorbidity and excess mortality due to natural causes in persons with schizophrenia or bipolar affective disorder. PLoS One. 2011;6:7. doi: 10.1371/journal.pone.0024597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Osborn DPJ, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s general practice research database. Arch Gen Psychiatry. 2007;64:242–9. doi: 10.1001/archpsyc.64.2.242. [DOI] [PubMed] [Google Scholar]
- 90.Laursen TM, Munk-Olsen T, Nordentoft M, Mortensen PB. Increased mortality among patients admitted with major psychiatric disorders: A register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia. J Clin Psychiatry. 2007;68:899–907. doi: 10.4088/JCP.v68n0612. [DOI] [PubMed] [Google Scholar]
- 91.Alharbi AA, Khan M, Munir B, Agrawal P, Osman M, Patel K, et al. Trends and predictors of inpatient mortality among patients with mood disorders undergoing pci. J Am Coll Cardiol. 2020;75:1395. doi: 10.1016/S0735-1097(20)32022-2. [DOI] [Google Scholar]
- 92.Bodén R, Molin E, Jernberg T, Kieler H, Lindahl B, Sundström J. Higher mortality after myocardial infarction in patients with severe mental illness: A nationwide cohort study. J Intern Med. 2015;277:727–36. doi: 10.1111/joim.12329. [DOI] [PubMed] [Google Scholar]
- 93.Brunner S, Camboni D, Flörchinger B, Kobuch R, Lieb M, Keyser A, et al. Patients under antidepressants undergoing cardiac surgery have a high risk for adverse events. Thoracic and Cardiovascular Surgeon. 2013;61 ((Brunner S.; Camboni D.; Flörchinger B.; Kobuch R.; Keyser A.; Hilker M.; Schmid C.) Universitätsklinikum Regensburg, Klinik und Poliklinik für Herz, Thorax-und herznahe Gefäßchirurgie, Regensburg, Germany(Lieb M.) Universitätsklinikum Regensburg, Klinik). Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L71144971.
- 94.Chander G, Daumit G, Zhang Y, Guallar E, Ford D, Steinwachs D, et al. Is there earlier time to death among hiv infected individualswith severe mental illness? J Gen Intern Med. 2010;25 ((Chander G.) Johns Hopkins University, School of Medicine, Baltimore, MD, United States(Daumit G.) Johns Hopkins University, School of Medicine, Rockville, MD, United States(Zhang Y.; Guallar E.; Ford D.; Steinwachs D.) Johns Hopkins University, Baltimore):S320-. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L70315026.
- 95.Chen PH, Kao YW, Shia BC, Lin HC, Kang JH Adverse stroke outcomes among patients with bipolar disorder. PLoS One. 2019;14:9. [DOI] [PMC free article] [PubMed]
- 96.Laursen TM, Mortensen PB, MacCabe JH, Cohen D, Gasse C. Cardiovascular drug use and mortality in patients with schizophrenia or bipolar disorder: a Danish population-based study. Psychol Med. 2014;44:1625–37. doi: 10.1017/S003329171300216X. [DOI] [PubMed] [Google Scholar]
- 97.Schulman-Marcus J, Goyal P, Swaminathan R, Singh H, Minutello R, Bergman G, et al. Disparities in revascularization for st-elevation myocardial infarction persist for patients with severe mental illness. J Am Coll Cardiol. 2016;67:656. doi: 10.1016/S0735-1097(16)30657-X. [DOI] [PubMed] [Google Scholar]
- 98.Tsai SY, Kuo CJ, Huang SH, Huang YL, Wang YF Risk and protective factors for premature circulatory mortality of bipolar disorder. Bipolar Disord. 2011;13 ((Tsai S.Y.; Kuo C.J.; Wang Y.F.) Department of Psychiatry, School of Medicine, Taipei Medical University, Taipei, Taiwan(Tsai S.Y.; Huang S.H.; Huang Y.L.) Department of Psychiatry, Taipei Medical University Hospital, Taipei, Taiwan(Kuo C.J.) Taipei City):102. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L70569876.
- 99.H.-C. W, F.H.-C. C, K.-Y. T, C.-Y. S, S.-P. S, T.-C. C. The incidence and relative risk of stroke among patients with bipolar disorder: a seven-year follow-up study. PLoS One. 2013;8. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L369734522. [DOI] [PMC free article] [PubMed]
- 100.Aagaard J, Nissen F, Wernlund A, Foldager L, Merinder L Valuable intervention against the excess mortality of psychiatric patients. Bipolar Disord. 2014;16 ((Aagaard J.; Nissen F.; Wernlund A.) Departement Q Anxiety and Depression, Aarhus University Hospital, Risskov, Denmark(Foldager L.; Merinder L.) Departement M, Aarhus University Hospital, Risskov, Denmark):111. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L71430879.
- 101.Bodén R, Molin E, Jernberg T, Kieler H, Lindahl B, Sundström J Myocardial infarction survival in patients with bipolar disorder or schizophrenia spectrum disorders-a nationwide cohort study. Bipolar Disord. 2014;16 ((Bodén R.; Molin E.) Neuroscience Psychiatry, Uppsala University, Uppsala, Sweden(Jernberg T.) Medicine Section of Cardiology Huddinge, Karolinska Institute, Stockholm, Sweden(Kieler H.) Centre for Pharmacoepidemiology, Department of Medicine, Karolinska):62–3. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L71430741.
- 102.Laursen TM, Wahlbeck K, Hällgren J, Westman J, Alinaghizadeh H, Gissler M, et al. Life expectancy and cardiovascular deaths of patients with bipolar disorder or schizophrenia in the nordic countries. Schizophr Bull. 2013;39 ((Laursen T.M.) Aarhus University, Aarhus, Denmark(Wahlbeck K.; Gissler M.) THL National Institute for Health and Welfare, Helsinki, Finland, THL, Helsinki, Finland(Hällgren J.; Alinaghizadeh H.) Karolinska Institute, Stockholm, Sweden(Laursen T.M.; Wahlbe):S67–8. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L71120220.
- 103.Ramsey C, Spira PA, Eaton W, Lee HB Lifetime manic spectrum syndromes and all-cause mortality: A26-year follow-up of the us national epidemiological catchment area study. J Am Geriatr Soc. 2012;60 ((Ramsey C.; P. Spira A.; Eaton W.; Lee H.B.) Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States(Lee H.B.) Psychiatry, Yale University, New Haven, CT, United States):S148-. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L70737837.
- 104.Staudt Hansen P, Frahm Laursen M, Grøntved S, Puggard Vogt Straszek S, Licht RW, Nielsen RE Increasing mortality gap for patients diagnosed with bipolar disorder—a nationwide study with 20 years of follow‐up. Bipolar Disord. 2018; Available from: http://ezproxy.libproxy.db.erau.edu/login?url=https://search.proquest.com/docview/2082682034?accountid=27203. [DOI] [PubMed]
- 105.Tsuang MT, Woolson RF. Mortality in patients with schizophrenia, mania, depression and surgical conditions: a comparison with general population mortality. Br J Psychiatry. 1977;130:162–6. doi: 10.1192/bjp.130.2.162. [DOI] [PubMed] [Google Scholar]
- 106.Tsuang MT, Woolson RF. Excess mortality in schizophrenia and affective disorders: do suicides and accidental deaths solely account for this excess? Arch Gen Psychiatry. 1978;35:1181–5. doi: 10.1001/archpsyc.1978.01770340031002. [DOI] [PubMed] [Google Scholar]
- 107.Tsuang MT. Suicide in schizophrenics, manics, depressives, and surgical controls: A comparison with general population suicide mortality. Arch Gen Psychiatry. 1978;35:153–5. doi: 10.1001/archpsyc.1978.01770260031002. [DOI] [PubMed] [Google Scholar]
- 108.Sharma R, Markar HR. Mortality in affective disorder. J Affect Disord. 1994;31:91–6. doi: 10.1016/0165-0327(94)90112-0. [DOI] [PubMed] [Google Scholar]
- 109.Webb RT, Lichtenstein P, Larsson H, Geddes JR, Fazel S. Suicide, hospital- presenting suicide attempts, and criminality in bipolar disorder: examination of risk for multiple adverse outcomes. J Clin Psychiatry. 2014;75:E809-+. doi: 10.4088/JCP.13m08899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Westman J, Hallgren J, Wahlbeck K, Erlinge D, Alfredsson L, Osby U. Cardiovascular mortality in bipolar disorder: a population-based cohort study in Sweden. BMJ Open. 2013;3:8. doi: 10.1136/bmjopen-2012-002373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Medici CR, Videbech P, Gustafsson LN, Munk-Jørgensen P Mortality and secular trend in the incidence of bipolar disorder. J Affect Disord. 2015;183 ((Medici C.R., Clara.reece.medici@post.au.dk; Gustafsson L.N.; Munk-Jørgensen P.) Aarhus University Hospital, Skovagervej 2, Risskov, Denmark(Videbech P.) Psychiatric Center Glostrup, Glostrup, Denmark):1–6. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L604446456. [DOI] [PubMed]
- 112.Norton B, Whalley LJ. Mortality of a lithium-treated population. Br J Psychiatry. 1984;145::277–82. doi: 10.1192/bjp.145.3.277. [DOI] [PubMed] [Google Scholar]
- 113.Laursen TM, Munk-Olsen T, Gasse C. Chronic somatic comorbidity and excess mortality due to natural causes in persons with schizophrenia or bipolar affective disorder. PLoS One. 2011;6:7. doi: 10.1371/journal.pone.0024597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Laursen TM, Munk-Olsen T, Agerbo E, Gasse C, Mortensen PB. Somatic hospital contacts, invasive cardiac procedures, and mortality from heart disease in patients with severe mental disorder. Arch Gen Psychiatry. 2009;66:713–20. doi: 10.1001/archgenpsychiatry.2009.61. [DOI] [PubMed] [Google Scholar]
- 115.Laursen TM, Munk-Olsen T, Nordentoft M, Mortensen PB. Increased mortality among patients admitted with major psychiatric disorders: a register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia. J Clin Psychiatry. 2007;68:899–907. doi: 10.4088/JCP.v68n0612. [DOI] [PubMed] [Google Scholar]
- 116.Castagnini A, Foldager L, Bertelsen A. Excess mortality of acute and transient psychotic disorders: Comparison with bipolar affective disorder and schizophrenia. Acta Psychiatr Scand. 2013;128:370–5. doi: 10.1111/acps.12077. [DOI] [PubMed] [Google Scholar]
- 117.Black DW, Winokur G, Nasrallah A. Mortality in patients with primary unipolar depression, secondary unipolar depression, and bipolar affective disorder: A comparison with general population mortality. Int J Psychiatry Med. 1987;17:351–60. doi: 10.2190/VL1B-7YEE-91J5-MWRA. [DOI] [PubMed] [Google Scholar]
- 118.Almeida OP, McCaul K, Hankey GJ, Yeap BB, Golledge J, Flicker L Suicide in older men: The health in men cohort study (HIMS). Prev Med (Baltim). 2016;93 ((Almeida O.P., osvaldo.almeida@uwa.edu.au) School of Psychiatry & Clinical Neurosciences, University of Western Australia, Perth, Australia(Almeida O.P., osvaldo.almeida@uwa.edu.au; McCaul K.; Flicker L.) WA Centre for Health & Ageing of Centre for Medica):33–8. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L612350152. [DOI] [PubMed]
- 119.Gale CR, Batty GD, Osborn DPJ, Tynelius P, Whitley E, Rasmussen F. Association of mental disorders in early adulthood and later psychiatric hospital admissions and mortality in a cohort study of more than 1 million men. Arch Gen Psychiatry. 2012;69:823–31. doi: 10.1001/archgenpsychiatry.2011.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Weeke A, Juel K, Væth M. Cardiovascular death and manic-depressive psychosis. J Affect Disord. 1987;13:287–92. doi: 10.1016/0165-0327(87)90049-8. [DOI] [PubMed] [Google Scholar]
- 121.Fekadu A, Medhin G, Kebede D, Alem A, Cleare AJ, Prince M, et al. Excess mortality in severe mental illness: 10-year population-based cohort study in rural Ethiopia. Br J Psychiatry. 2015;206:289–96. doi: 10.1192/bjp.bp.114.149112. [DOI] [PubMed] [Google Scholar]
- 122.Ahrens B, Müller-Oerlinghausen B, Schou M, Wolf T. Excess cardiovascular and suicide mortality of affective disorders may be reduced by lithium prophylaxis. J Affect Disord. 1995;33:67–75. doi: 10.1016/0165-0327(94)00074-J. [DOI] [PubMed] [Google Scholar]
- 123.Kay DWK, Petterson U. VI. MORTALITY. Acta Psychiatr Scand. 1977;56:55–60. doi: 10.1111/j.1600-0447.1977.tb10824.x. [DOI] [Google Scholar]
- 124.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72:227–36. doi: 10.1016/S0165-0327(01)00413-X. [DOI] [PubMed] [Google Scholar]
- 125.Saha S, Chant D, Mcgrath J. A Systematic Review of Mortality in Schizophrenia Is the Differential Mortality Gap Worsening Over Time? Population-based studies that re-ported primary data on deaths in people with schizo-phrenia. Arch Gen Psychiatry. 64 2007. [DOI] [PubMed]
- 126.Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, Penninx BW. Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. Am J Psychiatry. 2014;171:453–62. doi: 10.1176/appi.ajp.2013.13030325. [DOI] [PubMed] [Google Scholar]
- 127.The top 10 causes of death. [cited 2022 Aug 7]. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
- 128.Hossain S, Mainali P, Bhimanadham NN, Imran S, Ahmad N, Patel RS. Medical and psychiatric comorbidities in bipolar disorder: insights from national inpatient population-based study. Cureus. 2019;11:8. doi: 10.7759/cureus.5636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Magalhães PV, Kapczinski F, Nierenberg AA, Deckersbach T, Weisinger D, Dodd S, et al. Illness burden and medical comorbidity in the systematic treatment enhancement program for bipolar disorder. Acta Psychiatr Scand. 2012;125:303–8. doi: 10.1111/j.1600-0447.2011.01794.x. [DOI] [PubMed] [Google Scholar]
- 130.Solmi M, Fiedorowicz J, Poddighe L, Delogu M, Miola A, Høye A, et al. Disparities in screening and treatment of cardiovascular diseases in patients with mental disorders across the world: systematic review and meta- analysis of 47 observational studies. Am J Psychiatry. 2021;178:793–803. doi: 10.1176/appi.ajp.2021.21010031. [DOI] [PubMed] [Google Scholar]
- 131.Thomson D, Berk M, Dodd S, Rapado-Castro M, Quirk SE, Ellegaard PK, Berk L, Dean OM. Tobacco use in bipolar disorder. Clin Psychopharmacol Neurosci. 2015;13:1–11. doi: 10.9758/cpn.2015.13.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Grassi L, Stivanello E, Belvederi Murri M, Perlangeli V, Pandolfi P, Carnevali F, et al. Mortality from cancer in people with severe mental disorders in Emilia Romagna Region, Italy. Psychooncology. 2021;30:2039–51. doi: 10.1002/pon.5805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kisely S, Forsyth S, Lawrence D. Why do psychiatric patients have higher cancer mortality rates when cancer incidence is the same or lower? Aust N Z J Psych. 2016;50:254–63. doi: 10.1177/0004867415577979. [DOI] [PubMed] [Google Scholar]
- 134.Schaffer A, Isometsä ET, Tondo L, H Moreno D, Turecki G, Reis C, et al. International Society for Bipolar Disorders Task Force on Suicide: meta- analyses and meta-regression of correlates of suicide attempts and suicide deaths in bipolar disorder. Bipolar Disord. 2015;17:1–16. doi: 10.1111/bdi.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Stone D, Holland K, Bartholow B, Crosby A, Davis S, Wilkins N Preventing Suicide: A Technical Package of Policy, Programs, and Practices.
- 136.Munkholm K, Faurholt-Jepsen M, Ioannidis JPA, Hemkens LG. Consideration of confounding was suboptimal in the reporting of observational studies in psychiatry: a meta-epidemiological study. J Clin Epidemiol. 2020;119:75–84. doi: 10.1016/j.jclinepi.2019.12.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.