Abstract
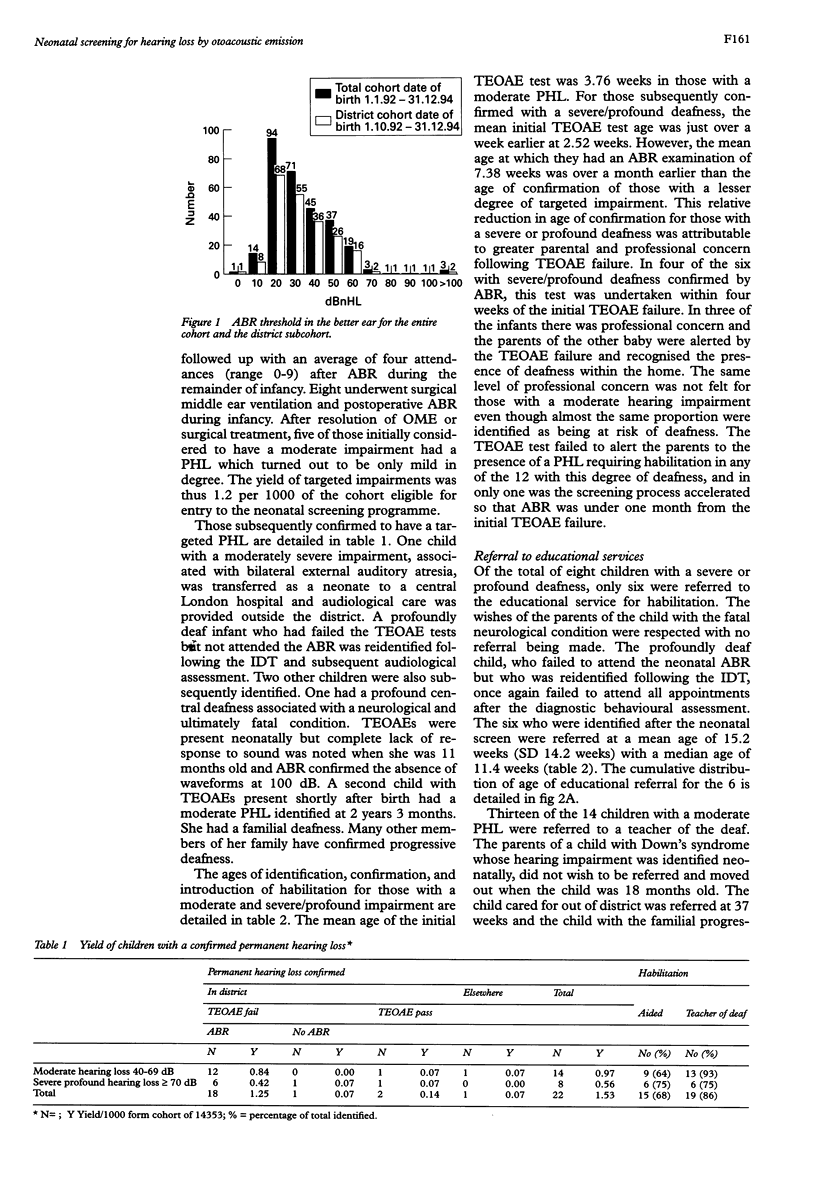
AIM: To assess universal neonatal screening for bilateral hearing impairments averaging 40 dBHL or worse in the better ear, using transient evoked otoacoustic emission screening (TEOAE) testing. METHODS: A three year cohort (14,353 infants born from January 1992 to 1995) was screened and subsequently followed up by hearing surveillance methods, including a distraction test screen from 7 months of age. The entire cohort was used to evaluate the outcome of the screen. A subcohort of 8172 district residents was used to evaluate the continuing worth of the distraction test programme. RESULTS: Nineteen infants (1.3/1000) with a targeted hearing impairment failed the neonatal TEOAE test. Six profoundly deaf infants identified by the TEOAE screen, were fitted with hearing aids at a median age of 16 weeks. One remained without an aid. Of 12 infants with a moderate impairment, only seven accepted hearing aid fitting and the median age of being fitted with an aid increased to 42 weeks. By the time of the analysis 22 children with a targeted hearing impairment (1.5/1000) had been identified from the cohort. Of the three missed neonatally, one was cared for elsewhere, another had a progressive loss, and the third had central deafness. Twenty children were ascertained with a congenital peripheral deafness. Of these, eight (40%) had risk factors identifiable neonatally. Only the child with central deafness was missed by TEOAE screening and subsequently identified by behavioural tests in infancy. The TEOAE screen outperformed the distraction test in terms of processes and yield and was 25% less expensive. CONCLUSIONS: The analysis confirmed the worth within the district of the TEOAE hearing screen. It will thus be continued as a universal neonatal screen with the distraction test being retained as a selective screen in the latter half of infancy.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Gandy G., Rennie J. Antibiotic treatment of suspected neonatal meningitis. Arch Dis Child. 1990 Jan;65(1 Spec No):1–2. doi: 10.1136/adc.65.1_spec_no.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber S. E. Review of a high risk register for congenital or early-onset deafness. Br J Audiol. 1990 Oct;24(5):347–356. doi: 10.3109/03005369009076575. [DOI] [PubMed] [Google Scholar]
- Howie V. M. Natural history of otitis media. Ann Otol Rhinol Laryngol. 1975 Mar-Apr;84(2 PT2):67–72. doi: 10.1177/00034894750840S215. [DOI] [PubMed] [Google Scholar]
- Kennedy C. R., Kimm L., Dees D. C., Evans P. I., Hunter M., Lenton S., Thornton R. D. Otoacoustic emissions and auditory brainstem responses in the newborn. Arch Dis Child. 1991 Oct;66(10 Spec No):1124–1129. doi: 10.1136/adc.66.10_spec_no.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides A. Age at fitting of hearing aids and speech intelligibility. Br J Audiol. 1986 May;20(2):165–167. doi: 10.3109/03005368609079011. [DOI] [PubMed] [Google Scholar]
- McCormick B., Wood S. A., Cope Y., Spavins F. M. Analysis of records from an open-access audiology service. Br J Audiol. 1984 Aug;18(3):127–132. doi: 10.3109/03005368409078940. [DOI] [PubMed] [Google Scholar]
- Ramkalawan T. W., Davis A. C. The effects of hearing loss and age of intervention on some language metrics in young hearing-impaired children. Br J Audiol. 1992 Apr;26(2):97–107. doi: 10.3109/03005369209077877. [DOI] [PubMed] [Google Scholar]
- Robinshaw H. M. Early intervention for hearing impairment: differences in the timing of communicative and linguistic development. Br J Audiol. 1995 Dec;29(6):315–334. doi: 10.3109/03005369509076750. [DOI] [PubMed] [Google Scholar]
- Stuart A., Yang E. Y., Green W. B. Neonatal auditory brainstem response thresholds to air- and bone-conducted clicks: 0 to 96 hours postpartum. J Am Acad Audiol. 1994 May;5(3):163–172. [PubMed] [Google Scholar]
- Sutton G. J., Gleadle P., Rowe S. J. Tympanometry and otoacoustic emissions in a cohort of special care neonates. Br J Audiol. 1996 Feb;30(1):9–17. doi: 10.3109/03005369609077925. [DOI] [PubMed] [Google Scholar]
- Thompson G., Weber B. A. Responses of infants and young children to behavior observation audiometry (BOA). J Speech Hear Disord. 1974 May;39(2):140–147. doi: 10.1044/jshd.3902.140. [DOI] [PubMed] [Google Scholar]
- Tucker S. M., Bhattacharya J. Screening of hearing impairment in the newborn using the auditory response cradle. Arch Dis Child. 1992 Jul;67(7):911–919. doi: 10.1136/adc.67.7.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkin P. M., Baldwin M., Laoide S. Parental suspicion and identification of hearing impairment. Arch Dis Child. 1990 Aug;65(8):846–850. doi: 10.1136/adc.65.8.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkin P. M., Baldwin M., McEnery G. Neonatal at risk screening and the identification of deafness. Arch Dis Child. 1991 Oct;66(10 Spec No):1130–1135. doi: 10.1136/adc.66.10_spec_no.1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkin P. M. Neonatal otoacoustic emission screening and the identification of deafness. Arch Dis Child Fetal Neonatal Ed. 1996 Jan;74(1):F16–F25. doi: 10.1136/fn.74.1.f16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb H. D., Stevens J. C. Auditory screening in high risk neonates: selection of a test protocol. Clin Phys Physiol Meas. 1991 Feb;12(1):75–86. doi: 10.1088/0143-0815/12/1/006. [DOI] [PubMed] [Google Scholar]


