Abstract
Background
Kidney failure is common in Ghana. Haemodialysis (HD) is the most common treatment modality for survival. Although, HD has been available in Ghana for 50 years, the majority of patients who develop kidney failure cannot access it. We describe the state of HD, dialysis prevalence, its utilization and cost of HD after fifty years of dialysis initiation in Ghana.
Methods
A situational assessment of HDs centres in Ghana was conducted by surveying nephrologists, doctors, nurses and other health care professionals in HD centres from August to October 2022. We assessed the density of HD centres, number of HD machines, prevalence of nephrologists, number of patients receiving HD treatment and the cost of dialysis in private and government facilities in Ghana.
Results
There are 51 HD centres located in 9 of the 16 regions of Ghana. Of these, only 40 centres are functioning, as 11 had shut down or are yet to operate. Of the functioning centres most (n = 26, 65%) are in the Greater Accra region serving 17.7% of the population and 7(17.5%) in the Ashanti region serving 17.5% of the population in Ghana. The rest of the seven regions have one centre each. The private sector has twice as many HD centers (n = 27, 67.5%) as the public sector (n = 13,32.5%). There are 299 HD machines yielding 9.7 HD machines per million population (pmp) with a median of 6 (IQR 4–10) machines per centre. Ghana has 0.44 nephrologists pmp. Currently, 1195 patients receive HD, giving a prevalence of 38.8 patients pmp with 609(50.9%) in the private sector. The mean cost of HD session is US $53.9 ± 8.8 in Ghana.
Conclusion
There are gross inequities in the regional distribution of HD centres in Ghana, with a low HD prevalence and nephrology workforce despite a high burden of CKD. The cost of haemodialysis remains prohibitive and mainly paid out-of-pocket limiting its utilization.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-023-10154-x.
Keywords: Haemodialysis, Cost of dialysis, Regional distribution, Ghana
Background
Globally, the incidence and prevalence of chronic kidney disease (CKD) are on the increase [1]. The prevalence of CKD in Africa and sub-Saharan Africa are 15.8% and 13.9% respectively [2, 3]. In Ghana, the prevalence of CKD is 13.3%, with chronic glomerulonephritis, diabetes mellitus and hypertension as major causes [4–6]. When CKD progresses to kidney failure (KF), kidney replacement therapy (KRT) is required for survival and to improve quality of life [7, 8]. Kidney transplantation is the best modality of KRT as it improves survival and quality of life compared dialysis [9–11].
Globally, patients in Africa have the lowest access to KRT, with the lowest rates found in Central and Eastern Africa with1-3% of those requiring receiving it [12]. According to the Global Kidney Health Atlas (GKHA), only 4–10% of patients with KF can access KRT in low- and lower middle income countries(LMIC) [13]. Limited access to KRT results from unavailability and high cost in most parts of Africa, including Ghana [14]. Ghana does not have a sustainable kidney transplant program and haemodialysis (HD) is the most common modality for KF management [15, 16]. According to the first Ghana renal registry in 2017, 96.2% were on HD, 0.3% on PD and 3.5% had kidney transplant [15]. There is also inequitable distribution of HD services in Ghana [17]. HD is not reimbursed by the National Health Insurance Scheme (NHIS) [16].
Dialysis is also required in severe cases of acute kidney injury (AKI). AKI accounts for 5.05–24.9% of patients with kidney disease in Ghana [18, 19]. In a single centre study, HD was required in 40.5% of patients with kidney disease on admission, but only 14.5% could afford HD leading to in-hospital mortality of 45.6% [20]. HD requirement for AKI is usually short-term but the cost remains prohibitive with high rates of preventive deaths.
South Africa was the first country to start HD in Africa in 1957, followed by Egypt a year later [21] for AKI management. Countries like Kenya(1961), Nigeria (1965), Sudan (1968) and Libya (1972) then followed [22, 23]. Ghana initiated dialysis in 1972 [22] and by 2015, HD was available in three teaching hospitals and three private facilities [16]. By December 2016 there were 15 dialysis centres with 103 HD machines in the country [17]. However, the rates of transplantation and peritoneal dialysis have however not increased significantly [15].
In this study, we evaluate the current status of HD services in Ghana by regional distribution of services, prevalence of HD patients, cost of HD treatment, utilization of dialysis services and availability of nephrology workforce to deliver HD treatment across centres in Ghana after five decades of HD initiation.
Methods
A cross-sectional situational survey was conducted across all HD centres in Ghana. Questionnaires were circulated and telephone calls were made between August-October 2022. The questionnaire was developed for the survey to understand the current state of dialysis in Ghana (Supplementary file 1). We sought data from nephrologists, doctors, nurses, and health care workers as key informants providing HD care in HD centres in Ghana, to ascertain the number of HD centres, number of HD machines in both public and private facilities, the presence of a resident/locum nephrologist, number of patients on HD and the cost per session of HD. The number of HD units that were previously operational but currently non-functional as well as new HD centres yet to start operation were also documented. The cost of HD was converted to United States dollars (US$) equivalent at the time of study in 2022 using an available currency converter [24]. Data were expressed as proportions, percentages, means ± standard deviation and medians and interquartile ranges as appropriate and analysis done with STATA version 16 [25]. Trends in the data with reference to previous studies conducted in Ghana [16, 17] were analyzed descriptively. Being a survey where no patient or personal data was collected, ethical clearance was waived by the institutional review board.
Ghana’s demography and economy
Ghana is a country located in West Africa bounded by Burkina Faso (north), Togo (east), Côte d'Ivoire (west) and the Gulf of Guinea (south). Ghana has a surface area of 238,533km2, 16 regions and a population of 30.8 million people according to the 2021 Population and Housing Census [26]. Greater Accra is the smallest region measuring 3,245 km2 and hosts the national capital Accra with a population of 5,455,692 [27]. The Savannah region is the largest with a surface area of 35,862 km2 and located in the middle belt of Ghana, with a population of 658,946 people. The Ashanti region is also in the middle belt with a population of 5440,463 and a surface area of 24,869 km2 [27].
According to the World Bank, Ghana has a gross domestic product (GDP) of US$77.59 billion and a GDP per capita of US$2,445.39 in 2021 [28]. Hence Ghana is categorized as a LMIC. The daily minimum wage at the time of the study was GHS13.53(US$2.06) per day or GHS365.31(US$55.7) per month [29].
Ghana spent 7.6% of its budget and 1.38% of its GDP on health in 2022 [30] which is less than the recommended 15% by the Abuja declaration [31]. Healthcare is financed largely by progressive taxes for 50% of health care funding, however with out-of-pocket payment accounting for about 45% of health services funding in Ghana [32]. The national health insurance scheme does not reimburse for HD care [16, 17] leading to low utilization of HD services in Ghana.
Results
There are 51 HD centres in Ghana including 37(72.5%) private centres and 14(27.5%) public centres. The majority of the HD centres are in the Greater Accra region 33(64.7%) with 9(17.7%) in the Ashanti region of Ghana. Only 40(78.4%) centres are currently functional, 9(17.7%) centres are not operational and 2(3.9%) new centres have been set up but not yet operational at the time of the survey (Table 1). Haemodialysis services offered in Ghana is mainly intermittent in-centre haemodialysis.
Table 1.
The distribution of haemodialysis centres, patient prevalence, nephrologists and cost of dialysis in Ghana
| Variable | Measure |
|---|---|
| Haemodialysis machines in Ghana (n) | 299 |
| Haemodialysis machines—(pmp) | 9.7 |
| Private centres [n (%)] | 27 (67.5) |
| State owned centres [n (%)] | 13 (32.5) |
| Haemodialysis centres without nephrologist [n (%)] | 23 (57.5) |
| Prevalence of nephrologists in Ghana (pmp) | 0.44 |
| Haemodialysis machines in Ghana | 6 (4–10)a |
| Haemodialysis machines in private centres | 6 (4–10)a |
| Haemodialysis centres in state-owned sector | 8 (3–10)a |
| Patients per haemodialysis centres | 20 (11.5–36.5)a |
| Patients per haemodialysis centres in private centres | 14 (10–25)a |
| Patients per haemodialysis centres in state-owned centres | 25 (14–53)a |
| Mean cost of haemodialysis session in Ghana | 53.9 ± 8.8b |
| Mean cost of haemodialysis in private centres | 56.7 ± 7.9b |
| Cost of haemodialysis in state-owned centres | 48.2 ± 7.9b |
Abbreviations: n number, IQR interquartile range, US $ United States Dollars, SD standard deviation, per million population, pmp [Median; (IQR)]a, (mean ± SD)b
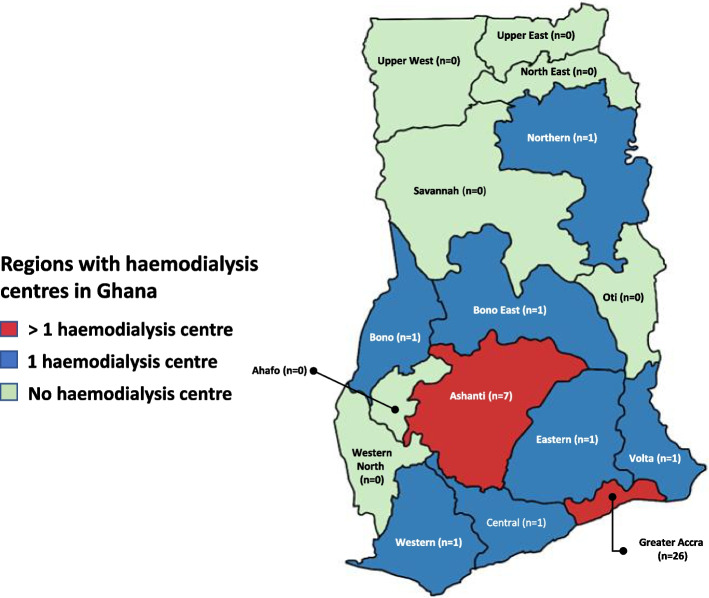
Of the 40 functional centres in Ghana, the majority are in the Greater Accra region and Ashanti regions with 26(65%) and 7(17.5%) respectively. The seven other regions have one HD centre each (Fig. 1).
Fig. 1.
The distribution of functional haemodialysis centres by region in Ghana in 2022. Created with mapchart.net
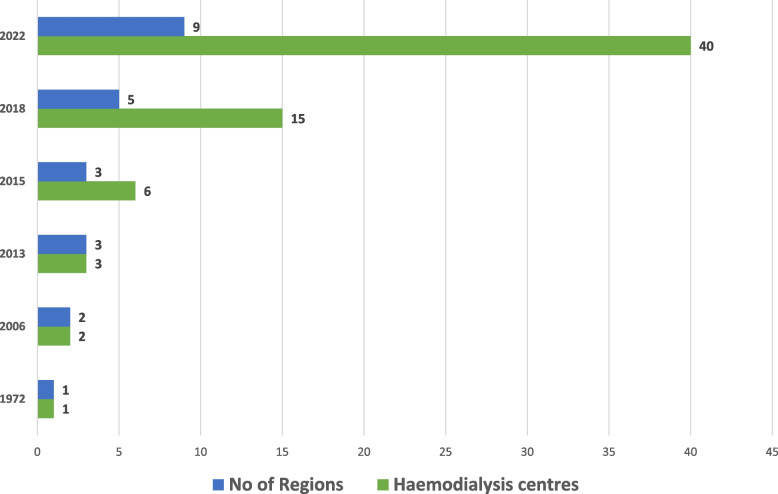
There has been a steady increase in regional distribution of HD centres from one centre in the greater Accra region in 1972 to centers being present in 9 out of the 16 regions in 2022 (Fig. 2).
Fig. 2.
Growth of the number of hemodialysis centers across regions in Ghana from 1972
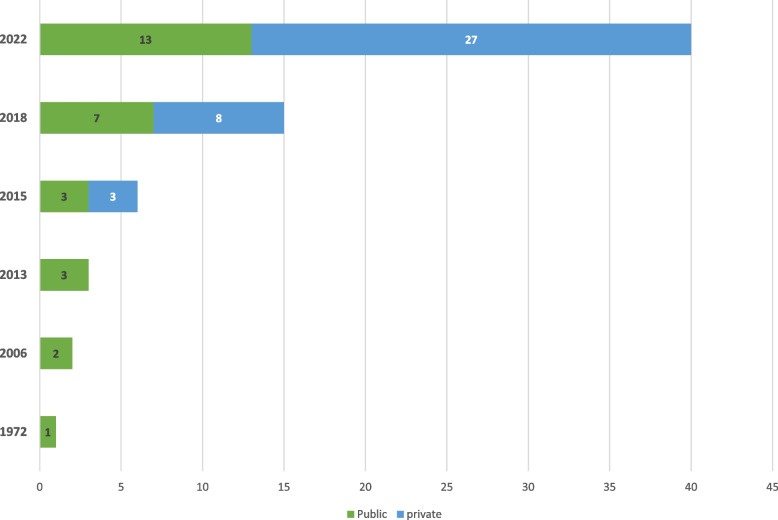
Private facilities were introduced in 2015 and have been increasing much faster than public facilities which were introduced in 1972 (Fig. 3).
Fig. 3.
Trend in haemodialysis centres for private and state-owned centres from 1972 in Ghana
There are 0.17 HD centres per 1000km2 in Ghana (assuming equitable distribution). Greater Accra again has the highest density of HD centres (8.01 per 1000km2) followed by the Ashanti region (0.29 per 1000km2). Bono East and Northern regions have the lowest density of centres (0.04 HD centres per 1000km2 each). The seven regions without HD centres make up 5,702,791(18.5%) of the population and cover 98,587km2 (41.3%) surface area of Ghana (Table 2).
Table 2.
Regional distribution of functional dialysis centres and patients per million population in Ghana
| Region | Population (%) | Population (n) | Surface area km2 | No. of HD centres | No of HD machines | No. of patients | Patients prevalence (pmp) | Dialysis machines (pmp) | Dialysis centres per 1000km2 |
|---|---|---|---|---|---|---|---|---|---|
| Greater Accra | 17.69 | 5,455,692 | 3,245 | 26 | 227 | 875 | 160.4 | 50.77 | 8.01 |
| Ashanti | 17.64 | 5,440,463 | 24,389 | 7 | 39 | 96 | 17.6 | 7.17 | 0.29 |
| Bono East | 3.92 | 1,203,400 | 23,257 | 1 | 3 | 12 | 9.97 | 2.49 | 0.04 |
| Bono | 3.90 | 1,208,649 | 11,107 | 1 | 2 | 4 | 3.3 | 1.65 | 0.09 |
| Central | 9.28 | 2,859,821 | 9,826 | 1 | 10 | 53 | 18.5 | 3.50 | 0.10 |
| Eastern | 9.49 | 2,925,653 | 19,323 | 1 | 8 | 25 | 8.5 | 2.73 | 0.05 |
| Northern | 7.50 | 2,310,939 | 25,448 | 1 | 5 | 90 | 3.9 | 2.16 | 0.04 |
| Volta | 5.38 | 1,659,040 | 9,504 | 1 | 3 | 20 | 12.1 | 1.81 | 0.11 |
| Western | 6.68 | 2,060,585 | 13,847 | 1 | 2 | 20 | 9.7 | 0.97 | 0.07 |
| Upper East | 4.22 | 1,301,226 | 8,842 | 0 | 0 | 0 | 0 | 0 | 0 |
| Upper west | 2.92 | 901,502 | 18,476 | 0 | 0 | 0 | 0 | 0 | 0 |
| Western North | 2.86 | 880,921 | 10,074 | 0 | 0 | 0 | 0 | 0 | 0 |
| Oti | 2.42 | 747,248 | 11,066 | 0 | 0 | 0 | 0 | 0 | 0 |
| North-East | 2.14 | 658,946 | 9,074 | 0 | 0 | 0 | 0 | 0 | 0 |
| Savanna | 2.12 | 653,266 | 35,862 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ahafo | 1.83 | 554,668 | 5,193 | 0 | 0 | 0 | 0 | 0 | 0 |
| Regions without dialysis | 18.52 | 5,702,791 | 98,587 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 100 | 30,792,608 | 238,533 | 40 | 299 | 1195 | 38.8 | 9.7 | 0.17 |
Abbreviations: HD haemodialysis, pmp per million population, km kilometers
There are 299 HD machines with 6(IQR 4–10) machines per centre, yielding 9.7 HD machines per million population(pmp) in Ghana (Table 1).
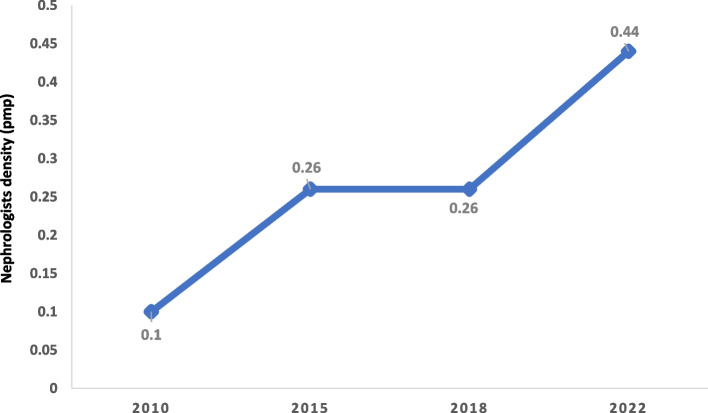
Regionally, Greater Accra has the highest number of HD machines pmp with 50.8pmp followed by Ashanti region with 7.2 HD machines pmp. The Western region has the lowest number of HD machines with 0.97pmp. Ghana has 15 nephrologists for a population of 30.8million with a prevalence of 0.44 nephrologists pmp (Table 1). Over half 23(57.5%) of the functional dialysis centres do not have a resident or locum nephrologist associated with the centre. The prevalence of nephrologists pmp has increased marginally since 2010 (Fig. 4).
Fig. 4.
Prevalence of nephrologists per million population in Ghana from 2010—2022
There are 1195 patients (private—609; public—586) receiving HD in Ghana. The HD prevalence is 38.8pmp in Ghana. The Greater Accra region has the highest prevalence of patients receiving HD (160.4pmp), followed by the Ashanti region (17.6 pmp). The least prevalent region is Bono East with a patient prevalence of 3.3pmp. There are no dialysis services for seven regions with a population of 5.7million people (Table 2). The mean cost of HD session in Ghana is US $53.9 ± 8.8. The cost in public centres is US$48.2 ± 7.9 and US$56.7 ± 7.9 in private centres.
Discussion
After 50 years of HD initiation in Ghana, this study assessed the regional distribution, status of HD services, patient prevalence on HD, nephrology workforce, and cost of HD in Ghana. Since 2016, the number of functional HD centres have increased from 15 to 40 and HD machines have increased from 103 to 299 in 2022 [17]. Gross inequities persist in the distribution of HD centres with very low nephrology workforce and high cost of HD.
The HD machines pmp have increased from 4.2pmp in 2016 [17] to 9.7pmp in 2022. The increase in HD centres has been largely contributed by the private sector expansion by 237.5% as compared to 85.7% increase in the public sector. Though patients are almost equally distributed in private and public centres, the median number of patients are higher in public centres compared to private centres. This likely reflects the higher cost of HD in the private centres. Seven regions occupying 41.3% of Ghana’s surface area and inhabited by 18.5% of the population have no HD centres [27]. Patients in these areas have to travel very long distances to access HD adding on to the cost of care lower utilization leading to poor quality of life, morbidity and mortality [7, 33].
Geographically, there is inequitable distribution of HD centres in Ghana. Countrywide, there are 17 HD centres per 100,000km2 while Greater Accra has 8 HD centres per 1000km2. This inequity is driven by population density and the ability to pay for services, hence HD is not accessible or affordable for the majority. Accessibility, availability, affordability, acceptability and accommodation make up the Penchansky’s conceptual model required for health service utilization [34]. Access refers to all the factors between the perception of need for the HD service to the utilization of the service [35].
The HD patient prevalence in Ghana is 38.8pmp, a marginal increase from 23.6pmp reported in 2017 [15]. This remains lower than the average prevalence in Africa of 79pmp and a global average of 296 in a systematic review [12]. Ghana’s prevalence is lower than the average for LMIC(68pmp). Ghana is comparable with some countries in sub-Saharan Africa and low income settings with a prevalence of less than 20pmp [36].
From global ballpark figures, it may be estimated that around 0.05% of the population in LMICs would develop KF [12]. With a population of 30.8 million people, Ghana has about 15,400 patients with KF. The 1,195 patients on HD in our survey represents only 7.8% of estimated patients with KF requiring HD in Ghana. Hence, some 92% of patients with KF have no access to KRT, consistent with the 90% reported for LMIC by GKHA [13] as PD and kidney transplants are in the minority [15].
In Ghana, the monthly minimum wage (US$55.7) can pay for only a session of HD (US$53.9) [29]. The cost of dialysis imposes substantial household burden on HD patients [37]. In a single centre study in Ghana, only 14.5% were able to utilize HD [20] resulting in high mortality of 32.9–45.6% [20, 33]. Due to high cost, most patient are unable to afford the prescribed three-times a week haemodialysis and settle for twice-a-week or even once-a-week haemodialysis in most cases.
The cost of HD excludes other direct medical costs which can be categorized as (i) medications such as oral haematinics, intravenous iron, subcutaneous erythropoietin, anti-hypertensives, medications for the management of mineral bone disease and (ii) vascular access-related such as arteriovenous fistula, arteriovenous graft, HD tunneled and temporary catheter costs. The average annual cost of HD for the required three sessions per week in Ghana is US$8,408.4 and US$5,605.6 for two sessions/week per person. The cost of HD services can be grouped into four categories. These are direct medical, direct non-medical, indirect and intangible costs [38, 39]. For HD treatment, the direct medical costs include staff, dialyzers, dialysis tubing, nephrologist consultation, capital cost for HD machines, cost of hospitalization and associated laboratory investigations, medications and vascular access. Direct non-medical costs include building costs, facility utilities such as electricity, water, administrative and overhead costs. Indirect costs are related to loss of productivity by the patients and caregivers as a result of the disease, transport cost and relocation. Intangible cost is related to the pain, symptoms and quality of life [37].
The cost of HD in Ghana is higher than in India (annual cost of US $3,423.79) and lower than in Nigeria (US $42,784.91) and Kenya (US$16,845.10) [40]. The cost per HD session is also lower than in Tunisia (US$65) and South Africa (US$140) [41]. In Ghana, the cost of HD is borne directly by most patients out-of-pocket as the NHIS does not reimburse for HD. Some private insurance and philanthropists support some patients with KF in some HD centres in Ghana [42]. NHIS reimburses admission cost, some medications and laboratory tests [16].
Increasingly, countries in sub-Saharan Africa even with lower GDP per capita than Ghana (US$2,445.5) such as Kenya (US$2,006.8) and Tanzania (US$1,135.5) [43, 44] have initiated universal coverage with twice-a-week dialysis services. This has led to a dramatic increase in dialysis utilization and prevalence in these countries.
Countries in sub-Saharan Africa adopt various approaches to provide HD services for patients with KF. This includes universal coverage of dialysis for AKI and KF (Kenya, Sudan, Malawi), government subsidy for HD (Senegal, Ethiopia, Cameroun), universal coverage for AKI only (South Africa, Ethiopia) and state coverage for chronic HD under limited conditions (South Africa), while others like Ghana, Nigeria, Burundi and Democratic republic of Congo provide no state coverage [45].
With the desired political will, Ghana could support the management of patients with KF far more than in its current state. If the expected 15,400 patients with KF are treated with twice-a-week HD at US $53 per session, about 100 sessions will be required per person per year. It will cost US $81,620,000 per year (US $5,300 per patient) which is 7.4% of the health budget. This might overburden the health budget considering other disease conditions of similar importance, hence governments may consider about 2% or more of the health budget (US $22 million) which can manage about 4,150 patients with KF per year initial rationing of dialysis like in South Africa [46] bearing in mind its challenges. The cost per unit of HD can also substantially be reduced if the import duties were reduced, and with large volume purchases decreasing further the cost per session. Pricing should also be further negotiated with dialysis companies. Local production of dialysis supplies should be explored to improve dialysis service utilization.
In 2022, US$1.1 billion was allocated to health in Ghana which is 7.6% of budget spending and 1.38% of GDP [30]. This is less than the 15% recommended by the Abuja declaration [31]. There is the need to increase the overall budgetary allocation to health as the cost of KRT for all who require it would have significant opportunity costs for other diseases [45].
Despite the limited availability of HD services, some existing HD facilities are folding up due to multiple reasons including unavailability or high cost of HD consumables due to high import duties and weak local currency, patients’ inability to pay realistic prices per session for HD, high property cost, administrative and labour costs making it difficult to break even to remain viable as well as the shortage of trained personnel such as dialysis nurses, technicians and nephrologists. The majority of HD centres do not have an attending nephrologist. Though the nephrologist prevalence has increased to 0.44 pmp in 2022 from 0.26 pmp in 2016 [17], it is still lower than the average of 0.5pmp in sub-Saharan Africa [13]. Ghana like most countries in sub-Saharan Africa needs more nephrologists to improve kidney care [47]. The nephrologists pmp in Ghana, a LMIC is currently only higher than in LIC (0.2pmp) but lower than in average LMIC (1.6pmp), UMIC (10.8pmp) and HIC (23.2 pmp) [13]. To improve the care and management of kidney disease, and to achieve kidney health for all in Africa, efforts should be put into investment in kidney health care, training of more nephrologists, task shifting in areas with less nephrology workforce, improving access to KRT all across the country and most importantly improving community engagement with education on disease prevention [47, 48]. The International Society of Nephrology (ISN) has improved the nephrology workforce in sub-Saharan Africa through the ISN fellowship program with positive impact [49] but there is still the need for more nephrology workforce in Ghana and most parts of sub-Saharan Africa [50].
In sub-Saharan Africa, efforts should be channeled towards sustainable preventive programs, health education and community engagement [48] to improve early detection and improve kidney health for all with optimal support for those who develop kidney failure [47].
This study has multiple strengths and few limitations. A major strength is that this situational survey results represents the most up-to-date source of information. Information represents a cross-sectional snapshot at the time of the survey which may change with time. It also possible that there may be a few patients who were on acute dialysis in some centres during the survey. Estimates of the locations of these dialysis centres per 1000 km square were based on the assumptions of equal distribution of the present dialysis centres. However, these fluctuations and estimations are unlikely to fundamentally change the overall message of poor access to HD and geographic inequities. This study therefore provides essential data for advocacy to improve kidney care in Ghana and sub-Saharan Africa.
Recommendation
There is the need for more state support for patients with KF in Ghana. This could include complete funding of some patients with KF, subsidization of cost of HD consumables, strengthening the nephrology workforce, improving renal transplantation programs, establishment of dialysis centres in regions without any and supporting defunct HD centres to restart operations. Ghana should adopt strategies to support HD services through the NHIS as practiced in Kenya, Tanzania and South Africa [43–45]. Until then, efforts should be channeled towards prevention of kidney disease through public health approaches [48]. Universal health coverage for all is critical for early identification of risk factors and the provision of equitable access to early interventions to delay the progression of kidney diseases. There is the need for good governance, multiple stake-holder engagements, transparency and a universal commitment to improve the right to kidney care in Ghana [51].
Conclusion
There have been advances in kidney care in Ghana for the past 50 years but gross inequity still exists. The HD prevalence in Ghana is below the average for LMICs and Africa. Cost of HD is still prohibitive but with more government support kidney care in Ghana and sub-Saharan Africa will substantially improve.
Supplementary Information
Additional file 1. Survey questionnaire on the state of haemodialysis in Ghana.
Acknowledgements
We appreciate the effort and contribution of the doctors and other health workers across dialysis facilities in Ghana who contributed data towards this manuscript. We like to specially acknowledge Emily Ampadu Nyarko, Lauretta Dede Lartey and Augustina Amankwah-Idris who were very instrumental in data collection.
Informed consent statement
Informed consent was also waived by the institutional review board of the Committee On Human Research Publication and Ethics (CHRPE) of the Kwame Nkrumah University of Science and Technology as there was no interaction with patients and personal data was not collected.
Abbreviations
- HD
Haemodialysis
- PMP
Per million population
- USD
United States Dollars
- CKD
Chronic kidney disease
- KF
Kidney failure
- KRT
Kidney replacement therapy
- GKHA
Global Kidney Health Atlas
- LMIC
Low and lower middle income countries
- AKI
Acute kidney injury
- GDP
Gross domestic product
- NHIS
National health insurance scheme
- ISN
International Society of Nephrology
Authors’ contributions
EKT initiated the study and put together the initial draft with ideas and inputs from VL and IO. KHM, POA, MKA, KFG, AJI, KAA and BIN were involved in the collection and cleaning of the data. Data analysis was initiated by EKT and improved by VL and IO. Figures were designed by IO after the initial concepts were drafted by EKT. VL and IO contributed to the write-up of the discussion in the manuscript. All authors contributed equally to critical revision of the manuscript. All authors read and approved the final manuscript.
Funding
This study is self-funded by the authors.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Ethical clearance was waived by the institutional review board of the Committee On Human Research Publication and Ethics (CHRPE) of the Kwame Nkrumah University of Science and Technology as there was no patient or personal data collection. We confirm that all methods were carried out in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 2.Stanifer JW, Jing B, Tolan S, Helmke N, Mukerjee R, Naicker S, et al. The epidemiology of chronic kidney disease in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(3):e174–e181. doi: 10.1016/S2214-109X(14)70002-6. [DOI] [PubMed] [Google Scholar]
- 3.Kaze AD, Ilori T, Jaar BG, Echouffo-Tcheugui JB. Burden of chronic kidney disease on the African continent: a systematic review and meta-analysis. BMC Nephrol. 2018;19(1):125. doi: 10.1186/s12882-018-0930-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adjei DN, Stronks K, Adu D, Beune E, Meeks K, Smeeth L, et al. Chronic kidney disease burden among African migrants in three European countries and in urban and rural Ghana: the RODAM cross-sectional study. Nephrol Dial Transplant. 2018;33(10):1812–1822. doi: 10.1093/ndt/gfx347. [DOI] [PubMed] [Google Scholar]
- 5.Amoako YA, Laryea DO, Bedu-Addo G, Andoh H, Awuku YA. Clinical and demographic characteristics of chronic kidney disease patients in a tertiary facility in Ghana. Pan Afr Med J. 2014;18:274. doi: 10.11604/pamj.2014.18.274.4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tannor EK, Sarfo FS, Mobula LM, Sarfo-Kantanka O, Adu-Gyamfi R, Plange-Rhule J. Prevalence and predictors of chronic kidney disease among Ghanaian patients with hypertension and diabetes mellitus: A multicenter cross-sectional study. J Clin Hypertens. 2019;21(10):1542–1550. doi: 10.1111/jch.13672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tannor EK, Norman BR, Adusei KK, Sarfo FS, Davids MR, Bedu-Addo G. Quality of life among patients with moderate to advanced chronic kidney disease in Ghana-a single centre study. BMC Nephrol. 2019;20(1):122. doi: 10.1186/s12882-019-1316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tannor EK, Archer E, Kapembwa K, van Schalkwyk SC, Davids MR. Quality of life in patients on chronic dialysis in South Africa: a comparative mixed methods study. BMC Nephrol. 2017;18(1):4. doi: 10.1186/s12882-016-0425-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alvares J, Cesar CC, Acurcio Fde A, Andrade EI, Cherchiglia ML. Quality of life of patients in renal replacement therapy in Brazil: comparison of treatment modalities. Qual Life Res. 2012;21:983–991. doi: 10.1007/s11136-011-0013-6. [DOI] [PubMed] [Google Scholar]
- 10.Purnell TS, Auguste P, Crews DC, Lamprea-Montealegre J, Olufade T, Greer R, et al. Comparison of life participation activities among adults treated by hemodialysis, peritoneal dialysis, and kidney transplantation: a systematic review. Am J Kidney Dis. 2013;62(5):953–973. doi: 10.1053/j.ajkd.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Czyzewski L, Sanko-Resmer J, Wyzgal J, Kurowski A. Assessment of health-related quality of life of patients after kidney transplantation in comparison with hemodialysis and peritoneal dialysis. Ann Transplant. 2014;19:576–585. doi: 10.12659/AOT.891265. [DOI] [PubMed] [Google Scholar]
- 12.Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. The Lancet. 2015;385(9981):1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 13.Bello AK, Levin A, Lunney M, Osman MA, Ye F, Ashuntantang GE, et al. Status of care for end stage kidney disease in countries and regions worldwide: international cross sectional survey. BMJ. 2019;367:l5873. doi: 10.1136/bmj.l5873. [DOI] [PubMed] [Google Scholar]
- 14.Ashuntantang G, Osafo C, Olowu WA, Arogundade F, Niang A, Porter J, et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: a systematic review. Lancet Glob Health. 2017;5(4):e408–e417. doi: 10.1016/S2214-109X(17)30057-8. [DOI] [PubMed] [Google Scholar]
- 15.Boima V, Tannor EK, Osafo C, Awuku YA, Mate-Kole M, Davids MR, et al. The Ghana Renal Registry–a first annual report. Afr J Nephrol. 2021;24(1):19–24. [Google Scholar]
- 16.Antwi S. State of renal replacement therapy services in Ghana. Blood Purif. 2015;39(1–3):137–140. doi: 10.1159/000368942. [DOI] [PubMed] [Google Scholar]
- 17.Tannor E, Awuku Y, Boima V, Antwi S. The geographical distribution of dialysis services in Ghana. Ren Replace Ther. 2018;4(1):3. doi: 10.1186/s41100-018-0143-1. [DOI] [Google Scholar]
- 18.Adu D, Okyere P, Boima V, Matekole M, Osafo C. Community-acquired acute kidney injury in adults in Africa. Clin Nephrol. 2016;86(Suppl 1):S48. doi: 10.5414/CNP86S121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okyere P, Okyere I, Ephraim RKD, Attakorah J, Osafo C, Arhin B, et al. Spectrum and clinical characteristics of Renal Diseases in Ghanaian Adults: a 13-year retrospective study. Int J of Nephrol. 2020;2020:8967258. doi: 10.1155/2020/8967258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tannor E, Agyei M, Emmanuel A, Kuffour P, Norman B. POS-056 Pattern of kidney disease in medical admissions in Ghana–a single centre study. Kidney Int Rep. 2021;6(4):S25. doi: 10.1016/j.ekir.2021.03.062. [DOI] [Google Scholar]
- 21.Barsoum RS. History of dialysis in Africa. Dialysis: history, development and promise: World Scientific. 2012. pp. 599–610. [Google Scholar]
- 22.Abd ElHafeez S, Dounousi E, Barsoum R. A journey through the history of dialysis in sub-Saharan Africa. Arch Hell Med. 2020;37(Suppl 2):203–207. [Google Scholar]
- 23.Barsoum RS, Khalil SS, Arogundade FA. Fifty years of dialysis in Africa: challenges and progress. Am J Kidney Dis. 2015;65(3):502–512. doi: 10.1053/j.ajkd.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 24.Xe Currency Converter. Convert Ghana Cedis to US Dollars 2022. Available from: https://www.xe.com/currencyconverter/convert/?Amount=1&From=GHS&To=USD. [Cited 24th November 2022].
- 25.StataCorp. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC; 2019. [Google Scholar]
- 26.Wikipedia. The administrative regions of Ghana. Last updated 4th November 2022 at 19:24 (UTC). Available from https://en.wikipedia.org/wiki/Regions_of_Ghana. [Cited 20th November, 2022].
- 27.Trading Economics. Gross domestic product of Ghana in 2022. Last updated 31st October 2022. Availble from https://tradingeconomics.com/ghana/indicators. [Cited 2nd November, 2022].
- 28.Ghana Statistical Service. Ghana Population and Housing Census 2021. Ghana Statistical Service. 021. Population and Housing Census]. Available from: https://census2021.statsghana.gov.gh/index.php. [Cited 2022 November 27].
- 29.Papaya Global. Monthly minimum wage in Ghana 2022. Last updated on 30th November 2022. Available from: https://www.papayaglobal.com/countrypedia/country/ghana/. [Cited 2022 December 17].
- 30.UNICEF. Ghana Health Budget Brief. UNICEF; 2022. Available from https://www.unicef.org/ghana/media/4581/file/2022%20Health%20Budget%20Brief%20.pdf. [Cited 2022 December 29].
- 31.World Health Organization. The Abuja declaration: Ten years on. 2010 and Available from https://apps.who.int/iris/bitstream/handle/10665/341162/WHO-HSS-HSF-2010.01-eng.pdf. [Cited on 21st November 2022].
- 32.Akazili J, Gyapong J, McIntyre D. Who pays for health care in Ghana? Int Journal Equity Health. 2011;10(1):1–13. doi: 10.1186/1475-9276-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eghan BA, Amoako-Atta K, Kankam CA, Nsiah-Asare A. Survival pattern of hemodialysis patients in Kumasi, Ghana: a summary of forty patients initiated on hemodialysis at a new hemodialysis unit. Hemodial Int. 2009;13(4):467–471. doi: 10.1111/j.1542-4758.2009.00379.x. [DOI] [PubMed] [Google Scholar]
- 34.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Medical care. 1981;19:127–40. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 35.Joseph AE, Phillips DR. Accessibility and utilization: geographical perspectives on health care delivery. New York City: Harper and Row; 1984. [Google Scholar]
- 36.El Matri A. ESRD management in Africa during the last decade. Clin Nephrol. 2015;83(7 Suppl 1):11–13. doi: 10.5414/CNP83S011. [DOI] [PubMed] [Google Scholar]
- 37.Kumah E, Agyei-Baffour P, Acheampong MK, Boateng KA, Larbie D, Afriyie EK, et al. Household cost of chronic kidney disease care among patients presenting at Komfo Anokye Teaching Hospital. Ghana Afr J Nephrol. 2022;25(1):182–191. [Google Scholar]
- 38.Just PM, De Charro FT, Tschosik EA, Noe LL, Bhattacharyya SK, Riella MC. Reimbursement and economic factors influencing dialysis modality choice around the world. Nephrol Dial Transplant. 2008;23(7):2365–2373. doi: 10.1093/ndt/gfm939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Letsios A. The effect of the expenditure increase in the morbidity and the mortality of patients with end stage renal disease: the USA case. Hippokratia. 2011;15(Suppl 1):16. [PMC free article] [PubMed] [Google Scholar]
- 40.Mushi L, Marschall P, Fleßa S. The cost of dialysis in low and middle-income countries: a systematic review. BMC Health Serv Res. 2015;15(1):1–10. doi: 10.1186/s12913-015-1166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matri A, Elhassan E, Abu-Aisha H. Renal replacement therapy resources in Africa. Arab J Nephrol Transplant. 2008;1(1):9–14. [Google Scholar]
- 42.Kankam A. First Sky Group provides free medical treatment for kidney patients: Ghanaweb. 2016. Available from: https://www.ghanaweb.com/GhanaHomePage/NewsArchive/First-Sky-Group-provides-free-medical-treatment-for-kidney-patients-494892. [Cited 2022 November 22]
- 43.Maritim P, Twahir A, Davids MR. Global Dialysis Perspective: Kenya. Kidney360. 2022;3(11):1944–7. doi: 10.34067/KID.0006662021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mushi L, Krohn M, Flessa S. Cost of dialysis in Tanzania: evidence from the provider’s perspective. Heal Econ Rev. 2015;5(1):1–10. doi: 10.1186/s13561-015-0064-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Luyckx VA, Miljeteig I, Ejigu AM, Moosa MR, editors. Ethical challenges in the provision of dialysis in resource-constrained environments. Semin Nephrol. 2017;37(3):273–286. 10.1016/j.semnephrol.2017.02.007 [DOI] [PubMed]
- 46.Moosa M, Kidd M. The dangers of rationing dialysis treatment: the dilemma facing a developing country. Kidney Int. 2006;70(6):1107–1114. doi: 10.1038/sj.ki.5001750. [DOI] [PubMed] [Google Scholar]
- 47.Tannor EK, Nlandu YM, Elrggal ME, Chika OU, Nzana V. Kidney Health for All-Bridging the gap to better kidney care in Africa. Afr J Nephrol. 2022;25(1):108–115. [Google Scholar]
- 48.Tannor EK, Calice-Silva V. Kidney health for all-Efforts in low-income settings to enhance community engagement, kidney health awareness and screening. Kidney Int Reports. 2022;7(3):359. doi: 10.1016/j.ekir.2021.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harris DC, Dupuis S, Couser WG, Feehally J. Training nephrologists from developing countries: does it have a positive impact? Kidney Int Suppl. 2012;2(3):275–278. doi: 10.1038/kisup.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Riaz P, Caskey F, McIsaac M, Davids R, Htay H, Jha V, et al. Workforce capacity for the care of patients with kidney failure across world countries and regions. BMJ Glob Health. 2021;6(1):e004014. doi: 10.1136/bmjgh-2020-004014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ashu JT, Mwangi J, Subramani S, Kaseje D, Ashuntantang G, Luyckx VA. Challenges to the right to health in sub-Saharan Africa: reflections on inequities in access to dialysis for patients with end-stage kidney failure. Int J Equity Health. 2022;21(1):1–1. doi: 10.1186/s12939-022-01715-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Survey questionnaire on the state of haemodialysis in Ghana.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.