Abstract
V-A ECMO during bilateral lung transplantation is routinely used when extracorporeal support is needed, in particular in case of patients affected by pulmonary hypertension. We report the case of a patient successfully transplanted with V-A ECMO assistance using a percutaneous double lumen cannula as venous drainage (Protek Duo, CardiacAssist Inc., Pittsburgh, PA) and central aortic cannulation. The double lumen cannula allowed an optimal drainage of the venous system and effective emptying of right heart chambers.
Keywords: lung transplant, VA-ECMO, double lumen cannula, cardio pulmonary bypass, pulmonary hypertension
Introduction
Extracorporeal support is often necessary in patients undergoing lung transplant (LT) for pulmonary arterial hypertension (PAH) because of right ventricle (RV) failure, inability to tolerate one lung ventilation and/or hemodynamic instability caused by surgical manoeuvres during hilar dissection. 1 Protek Duo (CardiacAssist Inc., Pittsburgh, PA) device is a dual lumen cannula in which proximal inflow lumen is positioned in the right atrium and the distal outflow lumen is positioned in the main pulmonary artery. It is inserted percutaneously via right internal jugular veins into the pulmonary artery (PA). Originally designed as a V-V ECMO cannula for pulmonary support it can also be used in case of acute right-heart failure as RV support. 2
Case report
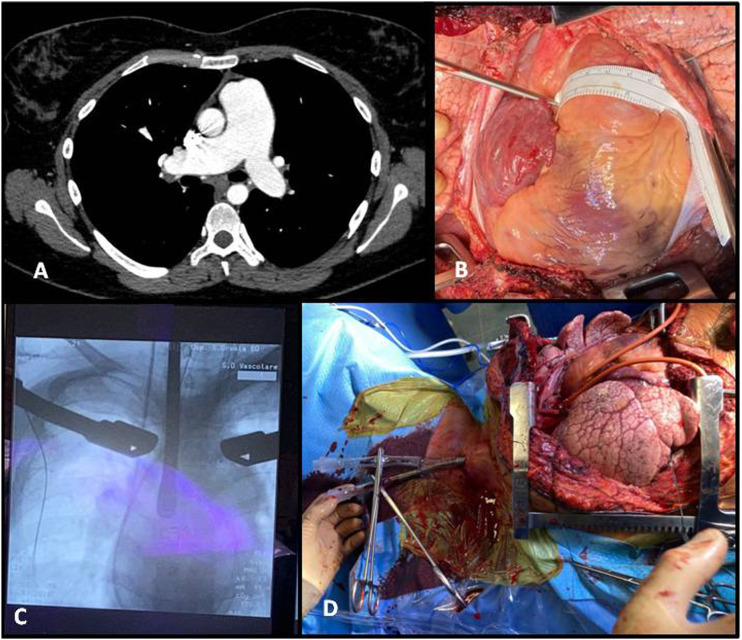
We report the case of a 32 years-old woman affected by idiopathic PAH with history of percutaneously treated atrial septal defect, who underwent bilateral LT. On screening cardiac-ultrasound showed signs of severe PAH (70 mmHg), dilation of right atrium (53 × 57 mm) and ventricle (31 × 51 mm) with preserved left ventricle ejection fraction (68%); on right heart catheterization systolic PA pressure was 94 mmHg, cardiac index was 2.3 L/min/m, right atrial pressure was 10 mmHg, pulmonary vascular resistances were 12.3WU and right heart failure was observed; CT showed enlarged PA with main trunk measuring 6 cm (Figure 1(a)). We usually perform LT for PAH on V-A ECMO, in this case, considering the extremely dilated right heart chambers and PA, we opted for VV-A ECMO to allow an improved venous drainage and right heart emptying.3,4 On arrival in the operatory room hemodynamic was stable (blood pressure: 90/60 mmHg, heart rate: 95, oxygen saturation: 93% on room air), lactates were 3.8 mmol/L. Clamshell incision was performed. Main PA was enlarged (6 cm) and right heart chambers severely dilated (Figure 1(b)). Central cannulation was performed in the ascending aorta. Venous cannulation was performed percutaneously under fluoroscopic and TEE guidance (Figure 1(c)) through the right jugular vein and a flexible dual lumen cannula (Protek Duo) was inserted (Figure 1(d)). The tip of the cannula was pushed till the main PA while the other aspiration site was positioned in right atrium. Protek Duo is originally designed to work as a double lumen cannula in V-V ECMO circuit for pulmonary support, but it is also used as RV support. 2 Approval from our Institutional Research Ethical Board was obtained and written informed consent for the use of anonymized clinical data and intraoperative images was waived accordingly. VV-A ECMO was started, using both lumen of the cannula as venous drainage, at 2.5 L/min with Activated Clotting Time of 150 s. We observed right heart and pulmonary artery decompression allowing a manageable bilateral LT. Patient remained stable throughout the procedure (blood pressure: 90/60, heart rate: 70, lactates: 1.8 mmol/L). Total ischemic time was 5 h for the left lung and 6 h 40 m for the right. VV-A ECMO was then switched to femoral-femoral V-A ECMO. Following the experience reported by the Lung Transplant Group of Vienna we assist the patient with V-A ECMO postoperatevely in order to allow prolonged controlled graft reperfusion and prevent fluid extravasation, reducing Primary Graft Dysfunction risk. 5
Figure 1.
(a): preoperative CT showing enlarged pulmonary artery. (b): intraoperative image showing enlarged pulmonary artery. (c): intraoperative fluoroscopic/trans esophageal echo guidance for cannula positioning. (d): Protek Duo cannula in place.
V-A ECMO was removed 72 h after surgery. Postoperative course was characterized by a slow physical recovery mainly due to an episode of stroke, on the 14th postoperative day, in close proximity to large bore central venous catheter removal. This episode was likely due to air reflux during central venous catheter removal. This resulted in left emiplegia. Upper extremity plegia promptly regressed while lower extremity paralysis needed prolonged physiotherapy. Brain CT and MRI showed minor frontal ischemic lesions of possible microembolic origin. The patient was discharged to a rehabilitation clinic 62 days after surgery in good clinical condition. On arterial blood gases pO2 was 94 mmHg, pCO2 36 mmHg.
Discussion
There is considerable variability in practice concerning the use of extracorporeal support during LT. 6
ECMO as a standard extracorporeal support during LT has demonstrated better results compared to cardio-pulmonary bypass (CPB) in terms of reduced intraoperative and postoperative morbidity. The main advantage of ECMO, compared to CPB, is a miniaturized circuit without air-blood interaction, lower priming volume, and lesser inflammatory activation with minimal coagulative disorders.7,8
Nevertheless CPB with bi-caval cannulation and venting of the PA is necessary in patients affected by PAH with severe cardiomegaly and over-systemic pulmonary pressure in order to achieve a complete heart emptying, moreover in case of pulmonary arteries dilatation, the only way to have an optimal access to the pulmonary hilum and to safely manage the PA is to work with the heart completely assisted and emptied. 1
Starting from this evidence we hypothesised that a double lumen cannula, such as the Protek Duo, used with both lumen as venous drainage would have overcome the issues encountered in PAH patients. In particular, the aspiration site of the cannula placed in the main PA allowed an easier and safer vascular dissection maintaining the arteries decongested. This VV-A ECMO configuration allowed to achieve a peculiar feature of CPB such as PA venting avoiding its drawbacks. Moreover, when performing pneumonectomy, a lower blood pressure in the PA allows to cut down the artery before the vein, so that the pulmonary vascular bed is emptied and a significant blood loss is avoided.
The use of Protek Duo cannula as double venous drainage has been previously reported in only one case in literature by Budd with satisfactory results, allowing hemodynamic stability and protection of RV function. 2
Conclusion
The use of Protek Duo as double site aspiration cannula during LT assisted by VV-A ECMO has shown satisfactory outcome. This is a case report and further experience is mandatory in order to confirm our promising preliminary results.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The work reported in this publication was funded by the Italian Ministry of Health, RC-2022-2774143 project.
ORCID iD
Filippo Antonacci https://orcid.org/0000-0003-3048-8281
References
- 1.Dell’Amore A, Campisi A, Congiu S, et al. Extracorporeal life support during and after bilateral sequential lung transplantation in patients with pulmonary artery hypertension. Artif Organs 2020; 44: 628–637. [DOI] [PubMed] [Google Scholar]
- 2.Budd AN, Kozarek K, Kurihara C, et al. Use of ProtekDuo as veno-arterial and veno-venous extracorporeal membrane oxygenation during bilateral lung transplantation. J Cardiothorac Vasc Anesth 2019; 33(8): 2250–2254. [DOI] [PubMed] [Google Scholar]
- 3.Conrad SA, Broman LM, Taccone FS, et al. The extracorporeal life support organization Maastricht treaty for nomenclature in extracorporeal life support. A position paper of the extracorporeal life support organization. Am J Respir Crit Care Med 2018; 198(4): 447–451. DOI: 10.1164/rccm.201710-2130CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broman LM, Taccone FS, Lorusso R, et al. The ELSO Maastricht treaty for ECLS nomenclature: abbreviations for cannulation configuration in extracorporeal life support - a position paper of the extracorporeal life support organization. Crit Care 2019; 23(1): 36. DOI: 10.1186/s13054-019-2334-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoetzenecker K, Schwarz S, Muckenhuber M, et al. Intraoperative ECMO and the possibility of postoperative prolongation improve survival in bilateral lung transplantation. J Thorac Cardiovasc Surg 2018; 155(5): 2193–2206.e3. [DOI] [PubMed] [Google Scholar]
- 6.Schaheen L, D’Cunha J. ECMO in lung transplantation: no longer a four letter word. J Thorac Cardiovasc Surg 2018; 155: 2191–2192. [DOI] [PubMed] [Google Scholar]
- 7.Machuca TN, Collaud S, Mercier O, et al. Outcomes of intraoperative extracorporeal membrane oxygenation versus cardiopulmonary bypass for lung transplantation. J Thorac Cardiovasc Surg 2015; 149: 1152–1157. [DOI] [PubMed] [Google Scholar]
- 8.Bermudez CA, Shiose A, Esper SA, et al. Outcomes of intraoperative venoarterial extracorporeal membrane oxygenation versus cardiopulmonary bypass during lung transplantation. Ann Thoracic Surg 2014; 98: 1936–1943. [DOI] [PubMed] [Google Scholar]