Abstract
Background
Despite known disparities in health status among older sexual and gender minority adults (OSGM), the prevalence of frailty is unknown. The aim of this study was to develop and validate a deficit-accumulation frailty index (AoU-FI) for the All of Us database to describe and compare frailty between OSGM and non-OSGM participants.
Methods
Developed using a standardized approach, the AoU-FI consists of 33 deficits from baseline survey responses of adults aged 50+. OSGM were self-reported as “not straight” or as having discordant gender and sex assigned at birth. Descriptive statistics characterized the AoU-FI. Regression was used to assess the association between frailty, age, and gender. Validation of the AoU-FI used Cox proportional hazard models to test the association between frailty categories (robust <0.15, 0.15 ≤ pre-frail ≤ 0.25, frail >0.25) and mortality.
Results
There were 9 110 OSGM and 67 420 non-OSGM with sufficient data to calculate AoU-FI; 41% OSGM versus 50% non-OSGM were robust, whereas 34% versus 32% were pre-frail, and 26% versus 19% were frail. Mean AoU-FI was 0.19 (95% confidence interval [CI]: 0.187, 0.191) for OSGM and 0.168 (95% CI: 0.167, 0.169) for non-OSGM. Compared to robust, odds of mortality were higher among frail OSGM (odds ratio [OR] 6.40; 95% CI: 1.84, 22.23) and non-OSGM (OR 3.96; 95% CI: 2.96, 5.29).
Conclusions
The AoU-FI identified a higher burden of frailty, increased risk of mortality, and an attenuated impact of age on frailty among OSGM compared to non-OSGM. Future work is needed to understand how frailty affects the OSGM population.
Keywords: Diversity in Aging, Frailty, LGBTQIA+
In the United States, there are approximately 3 million older sexual and gender minority adults (OSGM), and these numbers are projected to grow to over 5 million by 2030 (1). OSGM face a higher burden of chronic conditions (2–4), mental health issues (2,3,5), subjective cognitive decline (6,7), and health risk behaviors (3,4). These disparities are understood through the minority stress theory that describes that external stressors (eg, stigma and discrimination related to sexual orientation) become internalized, resulting in negative feelings about identity, a need to conceal one’s identity, and expectations of rejection in future interactions. These specific stressors accumulate over everyday stress (8). The minority stress theory has been extended to include the unique experiences of people who are members of gender-minoritized populations (9), individuals with multiple minoritized identities (eg, sexual, gender, and racial) (10), and aging (11). The current generation of OSGM experienced significant events specific to their minority identity, including homosexuality being labeled as a mental illness; the Lavender Scare where there was mass dismissal of SGM workers from U.S. government employment; and the human immunodeficiency virus infection and acquired immunodeficiency syndrome epidemic. Minority stress has been linked to negative health consequences including changes in inflammation, immune, and endocrine function, which contribute to poor cardiovascular, metabolic, and immunologic clinical outcomes (8,12,13) and potentially frailty.
The deficit-accumulation frailty index (FI) is one of 2 prevailing theories of frailty measurement (14,15). FI captures the aggregate burden of age-related health deficits and represents a multidimensional risk state (15). Moreover, the FI is a comprehensive measure that integrates physical and mental health conditions more common among OSGM. However, a lack of available data precludes any systematic characterization of frailty in an OSGM population. The NIH-funded All of Us (AoU) Research Program is well positioned to address this critical need by using multimodal outreach to recruit a diverse cohort of participants who have been historically underrepresented in biomedical research, including OSGM (16). In the present study, we used the AoU database to study frailty in OSGM with 2 goals: First, to develop and validate an FI that can readily be applied to AoU; and second, to estimate the prevalence of frailty among OSGM and compare the burden of frailty in OGSM to a non-SGM older adult (non-OSGM) population. We hypothesized that frailty would be higher in OSGM compared to non-OSGM individuals.
Method
Population
The AoU Program goals, scientific rationale, recruitment methods, and sites have been described previously (16). In brief, eligible participants included U.S. residents over the age of 18, not incarcerated at the time of enrollment, and able to provide informed consent. More than 75% of participants are from populations underrepresented in biomedical research, including 50% from racial and ethnic minority groups. Participants volunteer to complete health surveys, authorize sharing of electronic health records (EHR), share mobile health data (eg Fitbit, Apple HealthKit), and are invited to an in-person visit to contribute biospecimen samples and undergo physical assessment. Structured EHR data are transferred from enrolling sites at least once per quarter (17). All experimental protocols and data collection involving human participants were approved by the Ethics Committee/Institutional Review Board of the AoU Institutional Review Board. The current study was reviewed and deemed exempt by the Northeastern University Institutional Review Board.
We used AoU Version 6 Curated Data Repositories (CDR) of the Registered Tier data set (updated on June 23, 2022, CDR Hotfix for v6 CDRs released January 13, 2023), which has undergone a series of data transformations to protect participant privacy and has been mapped to the Observational Medical Outcomes Partnership common data model (18). At the time of analysis, over 370 000 community-dwelling people in the United States had participated in AoU.
We restricted our older adult cohort to those aged 50 years or older, as conditions of aging have been shown to have higher prevalence at relatively younger ages among other stigmatized populations, such as people living with HIV (19). Data from 5 baseline surveys were used to develop the FI: “The Basics” (participant demographics), “Overall Health” (levels of individual health), “Lifestyle” (health risk behaviors), “Personal Medical History” (medical conditions), and “Health Care Access and Utilization” (access and use of health care).
Identifying Older Sexual and Gender Minority Participants
Self-reported sex assigned at birth was assessed in “The Basics” survey with the question “What was your biological sex assigned at birth?” (responses “Male | Female | Intersex | None of these describe me | Prefer not to answer”), and gender was assessed with “What terms best express how you describe your gender identity?” (responses “Man | Woman | Non-binary | Transgender | None of these describe me and I’ve like to consider additional options | Prefer not to answer”). In the Registered Tier Data Set, responses for both sex and gender were aggregated by AoU administrators for participant privacy into “Male | Female | Not male/Not female/prefer not to answer/skip.” Sexual orientation was assessed by the question “Which of the following best represents how you think of yourself?” responses “Gay | Lesbian | Straight | Bisexual | None of these describe me and I’d like to see additional options | Prefer not to answer” were aggregated by AoU administrators into “Straight” or “Not Straight.” We divided participants into 2 mutually exclusive groups: OSGM and non-OSGM, based on concordance between sex assigned at birth, gender, and “straight” status (Table 1). For example, anyone reporting male sex assigned at birth, male gender, and “straight” was considered non-OSGM. However, an individual reporting male sex assigned at birth, male gender, and “not straight” was considered an OSGM man. Anyone reporting male or female sex assigned at birth and gender as not male/not female/prefer not to answer/skip was considered OSGM gender-diverse, regardless of “straight” status. Consistent with culturally appropriate gender identity language (20), we use the terms “Man,” “Woman,” and “Gender-diverse,” to refer to AoU gender responses “Male,” “Female,” and “Not male/Not female/prefer not to answer/skip.” As such, our sample consisted of the following subgroups: non-OSGM men, non-OSGM women, OSGM men, OSGM women, and OSGM gender-diverse. We compared the baseline demographic characteristics of OSGM and non-OSGM people using means and proportions.
Table 1.
Sex Assigned at Birth and Gender Categories by Sexual and Gender Minority Status
| Population | Sex Assigned at Birth | Gender* | n (%) | Final Population | n (%) |
|---|---|---|---|---|---|
| Non-OSGM (n = 67 420) | Male | Male | 25 572 (38%) | Non-OSGM, Man | 25 572 (38%) |
| Female | Female | 41 850 (62%) | Non-OSGM, Woman | 41 850 (62%) | |
| OSGM (n = 9 110) | Male | Male | 2 712 (29.8%) | OSGM, Man | 2 712 (29.8%) |
| Female | Female | 2 480 (27.2%) | OSGM, Woman | 2 480 (27.2%) | |
| Male | Not man only, not woman only, prefer not to answer, or skipped | 305 (3.3%) | OSGM, gender-diverse | 3 918 (43%) | |
| Female | 386 (4.2%) | ||||
| No matching concept | Male or Female | <30 (~0.3%) | |||
| Not man only, not woman only, prefer not to answer, or skipped | 2 639 (29%) | ||||
| Not male, not female, prefer not to answer, or skipped | Male | 185 (2%) | |||
| Female | 294 (3.2%) | ||||
| Not man only, not woman only, prefer not to answer, or skipped | <100 (~1%) |
Notes: OSGM = older sexual and gender minority.
*Gender was recoded from male and female to man and woman in the analyses.
Measures
We developed an AoU deficit-accumulation frailty index (AoU-FI) using methods outlined by Searle et al. (21). We matched AoU survey items with deficits used in other validated frailty indices (21,22). Each deficit was given a value between 0 and 1. Any item with more than 2 answer options had equally distributed graded values between 0 and 1. We assessed 33 deficits across 7 domains of health (Supplementary Table 1): cognition (concentration and dementia), morbidity (cancer, hypertension, peripheral vascular disease, stroke/transient ischemic attack, atrial fibrillation, heart failure, coronary artery disease, diabetes, kidney disease, asthma, and chronic lung disease), physical function (transportation, bathing, running errands alone, walking/climbing stairs, average pain in past 7 days, and everyday activities), geriatric syndromes (fractured bone, osteoporosis, and arthritis), general health status (general health, general social health, health literacy, general social satisfaction, and average fatigue in past 7 days), mental health (anxiety, depression, emotional problems in past 7 days, and general mental health), and sensory impairment (hearing and blindness). Principal components analysis was used to estimate the independent contributions of the 33 deficits. The AoU-FI is calculated as the sum of the conditions present for each participant divided by the number of deficits evaluated for an individual. Participants were excluded if they were missing more than 20% of the AoU-FI deficits or if the available data for the AoU-FI was >70% comorbidities (21). The second criterion ensured a more accurate estimation of frailty rather than a comorbidity index.
Describing and Validating the AoU-FI
We used histograms and summary statistics to characterize the continuous AoU-FI for the OSGM and non-OSGM groups. Consistent with Searle et al. (21), we assessed the skew and density of the AoU-FI distribution, as well as the association between AoU-FI and age. To do this, we used linear regression to evaluate the association between log-transformed AoU-FI and age for OSGM and non-OSGM, as well as stratified by gender within each group. We conducted an unequal variance t-test to compare the AoU-FI to the nationally representative U.S. community using the National Health and Nutritional Examination Survey (NHANES) FI from Pridham et al. (23). We also categorized the AoU-FI using the following cut-points: robust <0.15, ≥0.15 pre-frail, and >0.25 as frail (24).
For validation analyses, we restricted our sample to participants who consented to share EHR data and used data on death from any cause recorded in the EHR. We validated the AoU-FI association against risk of mortality using Cox proportional hazards models. We included an a priori interaction term between groups (OSGM and non-OSGM) and categorical frailty (robust, pre-frail, frail) while adjusting for the following baseline characteristics as covariates: age group, race/ethnicity, alcohol consumption, smoking status, income, marital status, and HIV status. The prevalence of alcohol use, smoking, and HIV tend to be higher in OSGM (4) and have previously been shown to affect frailty (25). Analyses were done using R version 4.2.2 (26) in the AoU Researcher Workbench cloud-based platform.
Results
Population Characteristics
Of the 200 793 participants aged 50 and older, 124 263 were excluded for missing more than 20% of AoU-FI deficits. All remaining participants had <70% comorbidity-related deficits. This resulted in a final sample of 76 530 participants consisting of 67 420 non-OSGM and 9 110 OSGM. The OSGM had a mean age of 64.8 years (standard deviation [SD] 8.3), 2 480 (27%) were women, 4 896 (54%) identified as White, 3 195 (35%) are married or living with a partner, and 355 (4%) report with living with HIV. The non-OSGM had a mean age (SD) of 65.7 (8.2) years, 41 850 (62%) were women, 54 244 (80%) identified as White, 43 963 (65%) are married or living with a partner, and 237 (0.4%) report with living with HIV (Table 2).
Table 2.
Characteristics of All of Us Participants by Sexual and Gender Minority Status
| Characteristics | Non-OSGM, n (%) | OSGM, n (%) |
|---|---|---|
| Sample size | 67 420 | 9 110 |
| Age | ||
| Mean (SD) | 65.7 (8.2) | 64.8 (8.3) |
| Age group | ||
| 50–59 | 18 901 (28%) | 2 992 (33%) |
| 60–69 | 27 079 (40%) | 3 540 (39%) |
| 70–79 | 18 705 (28%) | 2 230 (24%) |
| 80+ | 2 735 (4.1%) | 348 (3.8%) |
| Race/ethnicity | ||
| Hispanic or Latino | 4 132 (6.1%) | 521 (5.7%) |
| Black or African American, not Hispanic or Latino | 5 363 (8.0%) | 543 (6.0%) |
| White, not Hispanic or Latino | 54 244 (80%) | 4 896 (54%) |
| Other | 2 664 (4.0%) | 274 (3.0%) |
| Choose not to answer | 1 017 (1.5%) | 2 876 (32%) |
| Education | ||
| College graduate or advanced degree | 42 910 (64%) | 4 090 (45%) |
| Highest grade: college one to three | 16 141 (24%) | 1 477 (16%) |
| Highest grade: twelve or GED | 6 118 (9.1%) | 529 (5.8%) |
| Less than a high school degree or equivalent | 1 766 (2.6%) | 219 (2.4%) |
| Choose not to answer | 485 (0.7%) | 2 795 (31%) |
| Annual income | ||
| <50K | 17 562 (26%) | 2 354 (26%) |
| >100K | 23 931 (35%) | 1 851 (20%) |
| Between 50 and 100K | 18 452 (27%) | 1 565 (17%) |
| Choose not to answer | 7 475 (11%) | 3 340 (37%) |
| Marital status | ||
| Divorced or separated | 12 199 (18%) | 1 092 (12%) |
| Married or living with partner | 43 963 (65%) | 3 195 (35%) |
| Never married | 5 708 (8.5%) | 1 593 (17%) |
| Widowed | 5 052 (7.5%) | 415 (4.6%) |
| Choose not to answer | 498 (0.7%) | 2 815 (31%) |
| Smoked 100 cigarettes (lifetime) | ||
| 100 cigarette lifetime: No | 39 281 (58%) | 4 766 (52%) |
| 100 cigarette lifetime: Yes | 27 206 (40%) | 4 170 (46%) |
| Skip choose not to answer | 933 (1.4%) | 174 (1.9%) |
| Alcohol use (past year) | ||
| Drink frequency past year: 2 or more per week | 22 154 (33%) | 2 841 (31%) |
| Drink frequency past year: 4 or less per month | 30 510 (45%) | 4 027 (44%) |
| Ever drinker | 11 381 (17%) | 1 744 (19%) |
| Nondrinkers | 3 130 (4.6%) | 429 (4.7%) |
| Choose not to answer | 245 (0.4%) | 69 (0.8%) |
| Concerned about stable housing | ||
| No | 62 895 (93%) | 5 598 (61%) |
| Yes | 4 202 (6.2%) | 773 (8.5%) |
| Choose not to answer | 323 (0.5%) | 2 739 (30%) |
| HIV status | ||
| HIV/AIDS recorded | 237 (0.4%) | 355 (3.9%) |
| No HIV/AIDS recorded | 67 183 (99.6%) | 8 755 (96%) |
| Frailty index | ||
| Mean (SD) | 0.17 (0.10) | 0.19 (0.11) |
| Median (IQR) | 0.15 (0.09, 0.22) | 0.17 (0.11, 0.25) |
| 99% | 0.47 | 0.49 |
Notes: AIDS = acquired immunodeficiency syndrome; GED = General Education Development; HIV = human immunodeficiency virus; IQR = interquartile range; OSGM = older sexual and gender minority; SD = standard deviation.
AoU Deficit-Accumulation Frailty Index
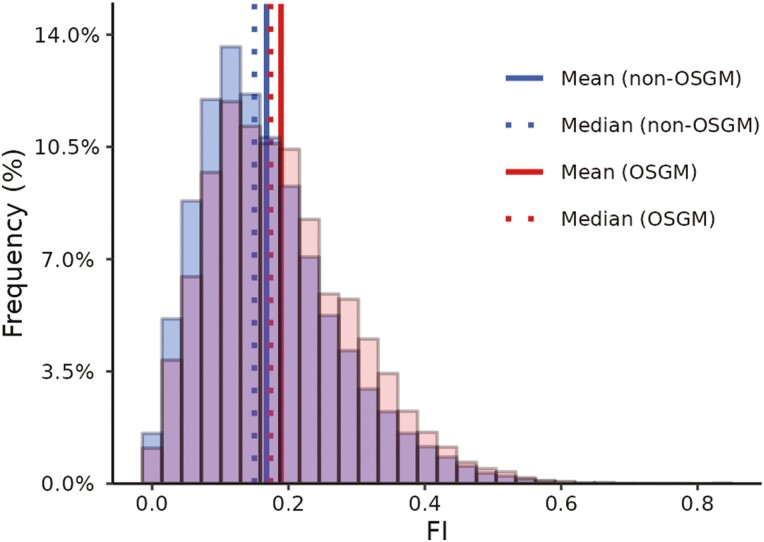
Of the 33 deficits included, principal components analysis demonstrated that each deficit independently contributed to the variance of the AoU-FI (Supplementary Figure1). The AoU-FI distribution for both OSGM and non-OSGM groups was right-skewed, resembling a gamma distribution, as with previous FIs (27,28) (Figure 1). Comparing the AoU-FI to the NHANES FI, both had similar means (SD), AoU-FI 0.170 (0.10), and NHANES 0.176 (0.073), yet there was a significant difference between the means with a t(2 111) = −3.32, 95% confidence interval (CI; −0.009, −0.002), and p < .001, likely due to large sample sizes.
Figure 1.
Distribution of AoU-FI for OSGM, n = 9 110 and non-OSGM, n = 67 420. AoU-FI = All of Us frailty index; OSGM = older sexual and gender minority. The AoU-FI distribution for both populations with mean (solid line) and median (dashed line).
Comparing Frailty Between OSGM and Non-OSGM
Among OSGM there were 3 711 (41%) robust, 3 064 (34%) pre-frail, and 2 335 (26%) frail, and among non-OSGM, there were 33 401 (50%) robust, 21 277 (32%) pre-frail, and 12 742 (19%) frail (Table 2). The median, mean (95% CI), and 99% of the AoU-FI for OSGM compared to non-OSGM were 0.17, 0.19 (0.187, 0.191), and 0.47 and 0.15, 0.168 (0.167, 0.169), and 0.49 respectively (Table 2 and Figure 1).
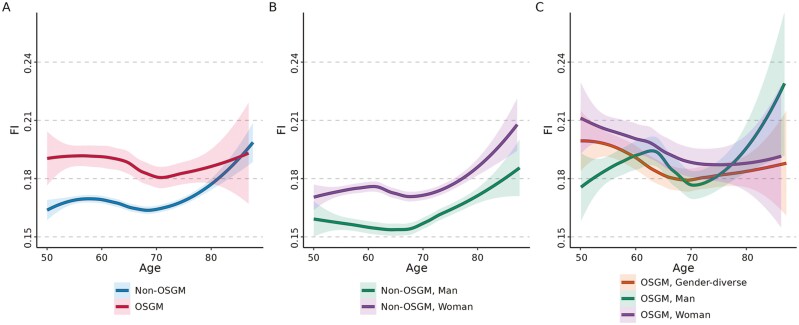
There was a significant association between frailty and age (ß = 0.005, p < .001). Further, the age-by-OSGM status interaction term was significant (ß = −0.005, p < .001), suggesting that the association with age is stronger for non-OSGM compared to OSGM (Figure 2). When stratified by gender, non-OSGM women had higher frailty than non-OSGM men (ß = 0.30, p < .001) and a significant age-by-gender interaction (ß = −0.003, p < .001; Figure 2. For OSGM, OSGM women had higher frailty than OSGM men (ß = 0.41, p = .007) and frailty for OSGM gender-diverse and OSGM men were similar (ß = 0.19, p = .16). Further, the interaction of age-by-gender among OSGM was significant for OSGM women compared to OSGM men (ß = −0.005, p < .001), but not for OSGM gender-diverse compared to OSGM men (ß = −0.003, p = .14; Figure 2). The 3 OSGM gender categories had similar median and mean (SD) frailty, OSGM men 0.17, 0.19 (0.1), OSGM women 0.18, 0.2 (0.11), and OSGM gender-diverse 0.17, 0.19 (0.11) (Supplementary Table 2).
Figure 2.
Association of AoU-FI values by age and gender for non-OSGM and OSGM. AoU-FI = All of Us frailty index; OSGM = older sexual and gender minority adults. (A) The association between AoU-FI by age (ß = 0.005, p < .001), with separate lines for OSGM n = 9 110 and non-OSGM n = 67 420. (B) Non-OSGM association between AoU-FI by age and gender (age × gender: ß = −0.003, p < .001), non-OSGM men, n = 25 572 (ref) and non-OSGM women n = 41 850. (C) OSGM association between AoU-FI by age and gender, OSGM gender-diverse, n = 3 918 (age × compared to OSGM men: ß = −0.003, p = .14), OSGM men n = 2 712 (ref), and OSGM women n = 2 480 (age × compared to OSGM men: ß = −0.005, p < .001). For all panels, a trend line was added using the generalized additive models.
Mortality
There were 378 deaths during follow-up: 346 among non-OSGM and 32 among OSGM. In the adjusted analysis, the adjusted hazard ratio (HR; 95% CI) for mortality among non-OSGM was 3.99 (2.99, 5.33), and among OSGM was 6.34 (1.83, 21.98) for frail compared to robust. However, a likelihood-ratio test comparing nested models with and without the a priori interaction between SGM status and FI category was not statistically significant (p = .4; Table 3).
Table 3.
Association of Frailty Category and Morality by Sexual and Gender Minority Status
| Sample Size | Crude Analysis | Adjusted Analysis† | ||||
|---|---|---|---|---|---|---|
| n (%) | HR | 95% CI | HR | 95% CI | ||
| Non-OSGM | Robust | 33 401 (49.5%) | Reference | Reference | ||
| Pre-frail | 21 277 (31.6%) | 2.47* | 1.87, 3.27 | 2.18* | 1.64, 2.89 | |
| Frail | 12 742 (18.9%) | 4.71* | 3.58, 6.19 | 3.99* | 2.99, 5.33 | |
| OSGM | Robust | 3 711 (40.7%) | Reference | Reference | ||
| Pre-frail | 3 064 (33.6%) | 5.68* | 1.63, 19.78 | 4.81* | 1.38, 16.76 | |
| Frail | 2 335 (25.6%) | 7.94* | 2.30, 27.42 | 6.34* | 1.83, 21.98 | |
Notes: AoU-FI = All of Us Frailty Index; CI = confidence interval; HR = hazard ratio; OSGM = older sexual and gender minority.
†Adjusted for age, race/ethnicity, alcohol use, smoking status, HIV status, and marital status.
* p value < .05. The p value for the OSGM-frailty interaction was .4.
Discussion
Using the AoU survey data to construct an FI, we found that OSGM compared to non-OSGM have a higher burden of frailty maintained across the life span and a higher magnitude of mortality risk. To our knowledge, this is the first study to examine frailty among OSGM.
Overall, OSGM had higher rates of frailty, at younger ages and continuing into older age, compared to non-OSGM in our study, made evident by the significant association between frailty and age-by-OSGM status. It may be that among frail OSGM, those in the oldest age groups (70–79 and 80+) are less likely to participate or died earlier than frail non-OSGM. Additionally, this finding is analogous to the literature regarding people living with HIV, another vulnerable minority population who have been shown to have higher levels of frailty at relatively younger ages and among whom more than 50% also identify as SGM (29,30). This may be due to the minority stress experience of chronic additive stress associated with social stigmatization and discrimination which may lead to systemic inflammation (13) and contribute to the development of frailty at relatively younger ages. Considering this, HIV status was included as a covariate in the adjusted analysis, and the association between frailty and mortality remained significant. Among people living with HIV, 79% experienced stigma when receiving medical care (31), and stigma was associated with reduced access to care, no regular source of HIV care, and suboptimal adherence to life-critical medication (32). Similarly for OSGM, those with internalized stigma or discrimination were less likely to have a routine physical exam in the past year (33), screening pap smear (34), sexual minority women are less likely to have a usual place of care, and both sexual minority men and women report difficulties with affording care (35). Despite the consistent association between minority stress and health care utilization, little is known to date about how utilization affects health outcomes (36) or frailty among OSGM.
The magnitude of association between frailty and mortality was higher for OSGM compared to non-OSGM, potentially reflecting health disparities and may also contribute to the age difference in frailty between OSGM and non-OSGM. OSGM mortality rates are understudied and not well defined. For women, despite no differences in all-cause mortality, sexual minority women had a higher mortality risk due to self-harm (37) and breast cancer (38) compared to non-sexual minority women. In contrast, research on mortality for sexual minority men has shown both higher (39) and no difference (37) in HIV-related mortality risk. Beyond sexual minorities, there is growing interest in understanding transgender mortality rates given exaggerated disparities in morbidity, mental health issues, and discrimination compared to non-transgender individuals (40–43). Hughes and colleagues found the mortality rate of privately insured transgender people was almost double compared to non-transgender people and highest in transfeminine and unclassified transgender individuals (42). Together, these findings highlight that OSGM heterogeneity may give rise to differences in frailty and mortality of OSGM subpopulations, emphasizing that OSGM research will require discerning subpopulations to elucidate disparities in frailty.
As expected, we demonstrated differences in the association between frailty and age across genders among non-OSGM (44–46). By extending this to the OSGM population, our results demonstrated that the association between frailty and age was reduced for all OSGM genders compared to non-OSGM genders. Consistent with the minority stress theory, our results suggest that OSGM status may have a larger affect on frailty development compared to age. Clinically, this finding emphasizes the need for early frailty assessment among OSGM.
Strengths and Limitations
The major strength of our study is the implementation of a novel AoU-FI on a large OSGM population with detailed health information available. Despite this, there are limitations to our study. We used Searle et al. methods to develop the AoU-FI, but not all the original FI items were available and substitutions were made. Even still, the resulting AoU-FI had the expected distribution (21), and association between age (47,48), gender (48–50), and mortality (21,27) reinforcing our confidence in its effectiveness as an FI. Additionally, the AoU database is a convenience sample of healthy volunteers, which may limit generalizability and introduce sampling bias. However, the AoU research program was designed to focus on those underrepresented in biomedical research, including sexual and gender minorities, enabling studies like ours. In this study, we identified distributions of OSGM baseline characteristics including age, race/ethnicity, annual income, and marital status that were consistent with the literature describing the OSGM population (2,3,6,49) despite a higher proportion of OSGM who chose not to answer. OSGM reported lower proportions of college or advanced degrees, some college, and high school/GED compared to non-OSGM. Studies have reported both higher (3,5) and lower (2) levels of education for OSGM participants. The similarity in the characteristics of the AoU OSGM with previously published OSGM populations is encouraging for external validity, despite being a convenience sample. Given these limitations, future work should also assess selection bias and the impact that missing data have on measures such as the AoU-FI.
Although we were able to develop the AoU-FI, we were unable to assess a frailty phenotype using the AoU survey data; however, given the extent of OSGM health disparities, FI provides a multidimensional assessment of aging. Further, we validated the AoU-FI with mortality with death from any cause recorded in the EHR, notably not all deaths are captured by the EHR, and deaths are not currently confirmed by next of kin contact or linked to the National Death Index. Despite this limitation, we were able to establish an association between AoU-FI and mortality to support that AoU-FI is a new representation of the frailty concept within the common data model that can be used by other investigators and can expand our understanding of frailty by applying it to underresearched and underrepresented populations.
Finally, the OSGM population is heterogeneous and consists of but is not limited to those who identify as gay, lesbian, bisexual, transgender, and nonbinary. Subpopulations of OSGM (eg bisexual or transgender individuals) have differences in health disparities (41,50), mortality (42), and likely frailty. Further, sexual minority and gender minority identities are not mutually exclusive so it is possible that individuals who belong to both gender and sexual minority groups (eg, transgender woman and lesbian) may be more frail than their cisgender, sexual minority counterparts as a result of stigma and discrimination from multiple minoritized identities. The AoU Registered Tier Data lacked the granularity to study the individual sexual orientation subpopulations, but we did assess gender subpopulations of OSGM. Future work should evaluate frailty among subpopulations of OSGM as these differences may have significant implications for OSGM care strategies. Despite these limitations, this study was a necessary first step to understanding frailty among OSGM.
Conclusion
We successfully developed and validated an AoU-FI and describe frailty among OSGM for the first time. Our results support the hypothesis that OSGM have a higher burden of frailty, particularly at younger ages, and have a higher risk of mortality compared to non-OSGM. This highlights the need to consider aging physiology for OSGM populations, even at younger ages. Future work should assess how and when frailty develops among OSGM to identify potential targets for intervention.
Supplementary Material
Contributor Information
Chelsea N Wong, Division of Gerontology, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA.
Michael P Wilczek, Roux Institute, Northeastern University, Portland, Maine, USA.
Louisa H Smith, Roux Institute, Northeastern University, Portland, Maine, USA; Department of Health Sciences, Bouvé College of Health Sciences, Northeastern University, Boston, Massachusetts, USA.
Jordon D Bosse, School of Nursing, Northeastern University, Boston, Massachusetts, USA.
Erin L Richard, Herbert Wertheim School of Public Health and Human Longevity Science, University of California San Diego, San Diego, California, USA.
Robert Cavanaugh, Roux Institute, Northeastern University, Portland, Maine, USA.
Justin Manjourides, Roux Institute, Northeastern University, Portland, Maine, USA; Department of Health Sciences, Bouvé College of Health Sciences, Northeastern University, Boston, Massachusetts, USA.
Ariela R Orkaby, New England Geriatric Research, Education, and Clinical Center, Veterans Affairs Boston Healthcare System, Boston, Massachusetts, USA; Division of Aging, Department of Medicine, Brigham & Women’s Hospital, Harvard Medical School, Boston, Massachusetts, USA.
Brianne Olivieri-Mui, Roux Institute, Northeastern University, Portland, Maine, USA; Department of Health Sciences, Bouvé College of Health Sciences, Northeastern University, Boston, Massachusetts, USA.
Funding
Dr. Orkaby is supported by VA CSR&D CDA-2 award IK2-CX001800. The All of Us Research Program is supported (or funded) by grants through the National Institutes of Health, Office of the Director: Regional Medical Centers: 1 OT2 OD026549, 1 OT2 OD026554, 1 OT2 OD026557, 1 OT2 OD026556, 1 OT2 OD026550, 1 OT2 OD 026552, 1 OT2 OD026553, 1 OT2 OD026548, 1 OT2 OD026551, and 1 OT2 OD026555; IAA #: AOD 16037; Federally Qualified Health Centers: HHSN 263201600085U; Data and Research Center: 5 U2C OD023196; Biobank: 1 U24 OD023121; The Participant Center: U24 OD023176; Participant Technology Systems Center: 1 U24 OD023163; Communications and Engagement: 3 OT2 OD023205 and 3 OT2 OD023206; and Community Partners: 1 OT2 OD025277, 3 OT2 OD025315, 1 OT2 OD025337, and 1 OT2 OD025276. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. All of Us Research Program would not be possible without the contributions made by its participants.
Conflict of Interest
None.
Author Contributions
Study design: All authors. Analysis: M.P.W., L.H.S., R.C., C.N.W., B.O.M. Data interpretation: All authors. Manuscript drafting: C.N.W., B.O.M. Manuscript editing: All authors.
References
- 1. Fredriksen-Goldsen KI, Kim HJ, Shiu C, Goldsen J, Emlet CA.. Successful aging among LGBT older adults: physical and mental health-related quality of life by age group. Gerontologist. 2015;55(1):154–168. doi: 10.1093/geront/gnu081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fredriksen-Goldsen KI, Kim HJ, Shui C, Bryan AE.. Chronic health conditions and key health indicators among lesbian, gay, and bisexual older US adults, 2013–2014. Am J Public Health. 2017;107(8):1332–1338. doi: 10.2105/ajph.2017.303922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gonzales G, Przedworski J, Henning-Smith C.. Comparison of health and health risk factors between lesbian, gay, and bisexual adults and heterosexual adults in the United States: results from the National Health Interview Survey. JAMA Intern Med. 2016;176(9):1344–1351. doi: 10.1001/jamainternmed.2016.3432 [DOI] [PubMed] [Google Scholar]
- 4. Han BH, Duncan DT, Arcila-Mesa M, Palamar JJ.. Co-occurring mental illness, drug use, and medical multimorbidity among lesbian, gay, and bisexual middle-aged and older adults in the United States: a nationally representative study. BMC Public Health. 2020;20(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nelson CL, Andel R.. Does sexual orientation relate to health and well-being? Analysis of adults 50+ years of age. Gerontologist. 2020;60(7):1282–1290. doi: 10.1093/geront/gnz187 [DOI] [PubMed] [Google Scholar]
- 6. Flatt JD, Cicero EC, Lambrou NH, et al. Subjective cognitive decline higher among sexual and gender minorities in the United States, 2015–2018. Alzheimers Dement Transl Res Clin Interv. 2021;7(1):e12197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fredriksen-Goldsen KI, Jung H, Kim HJ, Petros R, Emlet C.. Disparities in subjective cognitive impairment by sexual orientation and gender in a national population based study of U.S. adults, 2013–2018. J Aging Health. 2022;34(4–5):519–528. doi: 10.1177/08982643211046466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hendricks ML, Testa RJ.. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Prof Psychol Res Pract. 2012;43:460–467. doi: 10.1037/a0029597 [DOI] [Google Scholar]
- 10. Cyrus K. Multiple minorities as multiply marginalized: applying the minority stress theory to LGBTQ people of color. J Gay Lesbian Ment Health. 2017;21(3):194–202. doi: 10.1080/19359705.2017.1320739 [DOI] [Google Scholar]
- 11. Levy BR, Slade MD, Chang ES, Kannoth S, Wang SY.. Ageism amplifies cost and prevalence of health conditions. Gerontologist. 2020;60(1):174–181. doi: 10.1093/geront/gny131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Flentje A, Heck NC, Brennan JM, Meyer IH.. The relationship between minority stress and biological outcomes: a systematic review. J Behav Med. 2020;43(5):673–694. doi: 10.1007/s10865-019-00120-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Diamond LM, Dehlin AJ, Alley J.. Systemic inflammation as a driver of health disparities among sexually-diverse and gender-diverse individuals. Psychoneuroendocrinology. 2021;129:105215. doi: 10.1016/j.psyneuen.2021.105215 [DOI] [PubMed] [Google Scholar]
- 14. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M157. doi: 10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- 15. Mitnitski AB, Mogilner AJ, Rockwood K.. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal. 2001;1:323–336. doi: 10.1100/tsw.2001.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. The “All of Us” Research Program. N Engl J Med. 2019;381(7):668–676. doi: 10.1056/NEJMsr1809937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Data Methods—All of Us Research Hub. Accessed December 17, 2022. https://www.researchallofus.org/data-tools/methods/
- 18. OMOP Common Data Model. Accessed February 14, 2023. https://ohdsi.github.io/CommonDataModel/
- 19. Olivieri-Mui B, Shi S, McCarthy EP, et al. Categorizing comorbid risk for people living with HIV: a latent profile analysis. JAIDS J Acquir Immune Defic Syndr. 2022;90(4):449–455. doi: 10.1097/qai.0000000000002999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Flatt JD, Cicero EC, Kittle KR, Brennan-Ing M.. Recommendations for advancing research with sexual and gender minority older adults. J Gerontol B Psychol Sci Soc Sci. 2022;77(1):1–9. doi: 10.1093/geronb/gbab127 [DOI] [PubMed] [Google Scholar]
- 21. Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K.. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8(1):1–10. doi: 10.1186/1471-2318-8-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim DH, Afilalo J, Shi SM, et al. Evaluation of changes in functional status in the year after aortic valve replacement. JAMA Intern Med. 2019;179(3):383–391. doi: 10.1001/jamainternmed.2018.6738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pridham G, Rockwood K, Rutenberg A.. Strategies for handling missing data that improve Frailty Index estimation and predictive power: lessons from the NHANES dataset. GeroScience. 2022;44(2):897–923. doi: 10.1007/s11357-021-00489-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shi SM, McCarthy EP, Mitchell SL, Kim DH.. Predicting mortality and adverse outcomes: comparing the frailty index to general prognostic indices. J Gen Intern Med. 2020;35(5):1516–1522. doi: 10.1007/s11606-020-05700-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Crane HM, Ruderman SA, Whitney BM, et al. ; Centers for AIDS Research Network of Integrated Clinical Systems (CNICS) Cohort Study. Associations between drug and alcohol use, smoking, and frailty among people with HIV across the United States in the current era of antiretroviral treatment. Drug Alcohol Depend. 2022;240:109649. doi: 10.1016/j.drugalcdep.2022.109649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. R Core Team. R: A Language and Environment for Statistical Computing. Published online 2022. Accessed February 14, 2023. https://cran.r-project.org/ [Google Scholar]
- 27. Blodgett J, Theou O, Kirkland S, Andreou P, Rockwood K.. Frailty in NHANES: comparing the frailty index and phenotype. Arch Gerontol Geriatr. 2015;60(3):464–470. doi: 10.1016/j.archger.2015.01.016 [DOI] [PubMed] [Google Scholar]
- 28. Williams DM, Jylhävä J, Pedersen NL, Hägg S.. A frailty index for UK Biobank participants. J Gerontol A Biol Sci Med Sci. 2019;74(4):582–587. doi: 10.1093/gerona/gly094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Guaraldi G, Brothers TD, Zona S, et al. A frailty index predicts survival and incident multimorbidity independent of markers of HIV disease severity. AIDS. 2015;29(13):1633–1641. doi: 10.1097/QAD.0000000000000753 [DOI] [PubMed] [Google Scholar]
- 30. HIV Among Gay and Bisexual Men in the U.S. | Fact Sheets | Newsroom | NCHHSTP | CDC. 2022. Accessed January 19, 2023. https://www.cdc.gov/nchhstp/newsroom/fact-sheets/hiv/HIV-gay-bisexual-men.html
- 31. Baugher AR, Beer L, Fagan JL, et al. ; Medical Monitoring Project. Prevalence of internalized HIV-related stigma among HIV-infected adults in care, United States, 2011–2013. AIDS Behav. 2017;21(9):2600–2608. doi: 10.1007/s10461-017-1712-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE.. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24(10):1101–1108. doi: 10.1007/s11606-009-1068-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kittle KR, Boerner K, Kim K, Fredriksen-Goldsen KI.. The role of contextual factors in the health care utilization of aging LGBT adults. Gerontologist. Published online September 1, 2022:gnac137. doi: 10.1093/geront/gnac137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Johnson MJ, Mueller M, Eliason MJ, Stuart G, Nemeth LS.. Quantitative and mixed analyses to identify factors that affect cervical cancer screening uptake among lesbian and bisexual women and transgender men. J Clin Nurs. 2016;25(23–24):3628–3642. doi: 10.1111/jocn.13414 [DOI] [PubMed] [Google Scholar]
- 35. Heslin K, Alfier J.. Sexual Orientation Differences in Access to Care and Health Status, Behaviors, and Beliefs: Findings From the National Health and Nutrition Examination Survey, National Survey of Family Growth, and National Health Interview Survey. National Center for Health Statistics; 2022. doi: 10.15620/cdc:115982 [DOI] [PubMed] [Google Scholar]
- 36. Gioia SA, Rosenberger JG.. Sexual orientation-based discrimination in us healthcare and associated health outcomes: a scoping review. Sex Res Soc Policy. 2022;19(4):1674–1689. doi: 10.1007/s13178-022-00741-8 [DOI] [Google Scholar]
- 37. Cochran SD, Mays VM.. Mortality risks among persons reporting same-sex sexual partners: evidence from the 2008 General Social Survey—National Death Index Data Set. Am J Public Health. 2015;105(2):358–364. doi: 10.2105/AJPH.2014.301974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cochran SD, Mays VM.. Risk of breast cancer mortality among women cohabiting with same sex partners: findings from the National Health Interview Survey, 1997–2003. J Womens Health. 2012;21(5):528–533. doi: 10.1089/jwh.2011.3134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cochran SD, Mays VM.. Sexual orientation and mortality among us men aged 17 to 59 years: results from the National Health and Nutrition Examination Survey III. Am J Public Health. 2011;101(6):1133–1138. doi: 10.2105/AJPH.2010.300013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Blosnich JR, Brown GR, Shipherd JC, Kauth M, Piegari RI, Bossarte RM.. Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing veterans health administration care. Am J Public Health. 2013;103(10):e27–e32. doi: 10.2105/AJPH.2013.301507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hughes L, Shireman TI, Hughto J.. Privately insured transgender people are at elevated risk for chronic conditions compared with cisgender counterparts. Health Aff (Millwood). 2021;40(9):1440–1448. doi: 10.1377/hlthaff.2021.00546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hughes LD, King WM, Gamarel KE, Geronimus AT, Panagiotou OA, Hughto JM.. Differences in all-cause mortality among transgender and non-transgender people enrolled in private insurance. Demography. 2022;59(3):1023–1043. doi: 10.1215/00703370-9942002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Quinn VP, Nash R, Hunkeler E, et al. Cohort profile: Study of Transition, Outcomes and Gender (STRONG) to assess health status of transgender people. BMJ Open. 2017;7(12):e018121. doi: 10.1136/bmjopen-2017-018121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gordon EH, Hubbard RE.. Differences in frailty in older men and women. Med J Aust. 2020;212(4):183–188. doi: 10.5694/mja2.50466 [DOI] [PubMed] [Google Scholar]
- 45. Hubbard RE, Rockwood K.. Frailty in older women. Maturitas. 2011;69(3):203–207. doi: 10.1016/j.maturitas.2011.04.006 [DOI] [PubMed] [Google Scholar]
- 46. Hubbard RE. Sex differences in frailty. Frailty Aging. 2015;41:41–53. doi: 10.1159/000381161 [DOI] [PubMed] [Google Scholar]
- 47. Mitnitski AB, Song X, Rockwood K.. The estimation of relative fitness and frailty in community-dwelling older adults using self-report data. J Gerontol A Biol Sci Med Sci. 2004;59(6):M627–M632. doi: 10.1093/gerona/59.6.m627 [DOI] [PubMed] [Google Scholar]
- 48. Rockwood K, Howlett SE, MacKnight C, et al. Prevalence, attributes, and outcomes of fitness and frailty in community-dwelling older adults: report from the Canadian Study of Health and Aging. J Gerontol A Biol Sci Med Sci. 2004;59(12):1310–1317. doi: 10.1093/gerona/59.12.1310 [DOI] [PubMed] [Google Scholar]
- 49. Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP.. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–1809. doi: 10.2105/AJPH.2012.301110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Fredriksen-Goldsen KI, Shiu C, Bryan AEB, Goldsen J, Kim HJ.. Health equity and aging of bisexual older adults: pathways of risk and resilience. J Gerontol B Psychol Sci Soc Sci. 2017;72(3):468–478. doi: 10.1093/geronb/gbw120 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.