On August 1, 2019, the first cases of electronic cigarette (e-cigarette), or vaping, product use-associated lung injury (EVALI) were reported to the Centers for Disease Control and Prevention (CDC).1 The cluster was an initial signal of an outbreak that, by December 10, 2019, resulted in 2,409 confirmed and probable hospitalized cases reported to CDC. Most EVALI patients are male (67%), under age 35 (78%), and reported using e-cigarette, or vaping, products containing tetrahydrocannabinol (THC) (80%).2
To date, the investigation has predominantly focused on prospectively identifying new hospitalized EVALI cases, following health advisories first issued by the Wisconsin Department of State Health Services on July 25, 2019, Illinois Department of Health on August 2, 2019, and by CDC on August 30, 2019.3 However, questions remain about whether EVALI is a new clinical syndrome or if cases were previously occurring without detection. It is also unknown whether the 86% decline in cases reported to CDC, from 217 people admitted the week of September 15, the apparent peak of the outbreak, to 31 the week of November 17,4,5 represents a drop in active case-finding by states or a true decline in EVALI cases.
Originally developed to detect bioterrorism following the terrorist attacks on September 11, 2001, the National Syndromic Surveillance Program (NSSP)6 has been modernized in recent years and expanded to include data from 47 states (all but Wyoming, South Dakota, and Hawaii) and DC, with participating healthcare facilities eligible for federal incentives. The system captures free-text chief complaints, discharge diagnosis codes, and patient demographics such as age and sex from approximately 70% of ED visits nationwide. Among all visits reported to NSSP, which include more than 100 million annual ED visits, 74% of captured visits are reported within 24 hours, with 75% of discharge diagnoses typically added to the record within 7 days. This allows syndromic surveillance of a wide variety of health exposures and outcomes, including previously unknown ones like EVALI, in real time.7
In this study, we developed queries of NSSP data (Supplement 1) to assess when emergency department (ED) visits associated with possible EVALI began to increase, and whether ED visits associated with these injuries have declined in recent weeks. To visualize the outbreak, time series of ED visits were overlaid with data from Google searches and EVALI cases reported to CDC.
Methods
Syndromic surveillance analysts at state health departments and CDC collaborated to develop two queries of ED data:8 1) exposure to e-cigarette, or vaping, products; and 2) acute lung injury, from January 1, 2017 to December 7, 2019.
Exposure query: e-cigarette, or vaping, product use
The first query was developed to search the chief complaint field for words related to use of e-cigarette, or vaping, products among all people presenting to EDs, including slang (Supplement 2). The query was not limited to lung injuries. The query attempted to exclude injuries unrelated to EVALI, such as device explosions and accidental ingestion of e-liquid; however, it did not exclude potentially related syndromes such as acute intoxication from THC or nicotine poisoning.
Outcome query: acute lung injury
The lung injury query included the ICD-10-CM codes (Supplement 3) recommended by CDC for identifying EVALI that were released on October 17, 2019 (Supplement 4).9 It included people who presented to EDs and were not discharged home, and excluded discharge diagnosis codes and chief complaint terms for infectious diseases, cystic fibrosis, and other potential etiologies. Because 78% of reported cases were age 34 or younger, and 95% were hospitalized,2 the diagnostic query was limited to ages 11–34 who were admitted, transferred, or died in the ED. This age cutoff improved specificity by reducing noise from ED visits with unclear causes, such as unexplained pneumonia, that are more common in older adults.
Confirmed or probable cases
The ED visit trend was overlaid on the trend for confirmed and probable cases reported by state health departments to CDC.4
Google Trends
The weekly time series of ED visits and reported cases were overlaid on Google search engine data, as a measure of public awareness of the outbreak. Data were visualized using Google Trends10, 11 for U.S. searches related to e-cigarettes, or vaping, products (Supplement 1). A Google Trends score of 100 represents peak interest, and 50 means the search term is half as popular.
Analyses
Longer-term trends were assessed as ED visits returned by each query per one million reported ED visits (Supplement 1). To identify weeks when the trend in ED visit rates changed for each query, knots were identified using the segmented package in R version 3.6.12, 13 Piecewise linear splines were fit between knots to estimate the change in visit rates during each period of interest.
For the exposure query, the tidytext package14 in R version 3.6 was used to analyze which symptoms were most commonly described in chief complaints with e-cigarette, or vaping, product use. This method counts adjacent word pairs (bigrams) in chief complaints, excluding uninformative words such as “of” and “the.”
For the outcome query, to compare the relative frequency of hospitalizations with EVALI-related codes among ages 11–34 beginning June 2, 2019, separate incidence ratios were estimated for males and females using the epiR package15 (R version 3.6).
Results
Exposure query
ED visits with e-cigarette, or vaping, product-related terms in the chief complaint gradually increased between the first week in 2017 and the week of August 11, 2019, particularly among patients ages 10–19 (Figure 1). In this age group, the weekly ED visit rate steadily increased from 4 per one million in the first week of January 2017 to 83 per one million during the week of August 4, 2019. Across all age groups, the trend then sharply increased between August 11, 2019 and September 8, 2019 (Figure 2), by an average of 26 per one million each week (95% CI: 19–32). The weekly visit rate peaked at 116 per one million during the week of September 8, 2019, and then declined by a weekly average of 6 per one million (95% CI: 5–6). The overall trend mirrors the trend in admission dates among EVALI cases reported to CDC, which peaked the week of September 15, and in US Google searches, which peaked during the week of September 8, 2019 (Figure 2).
Figure 1.
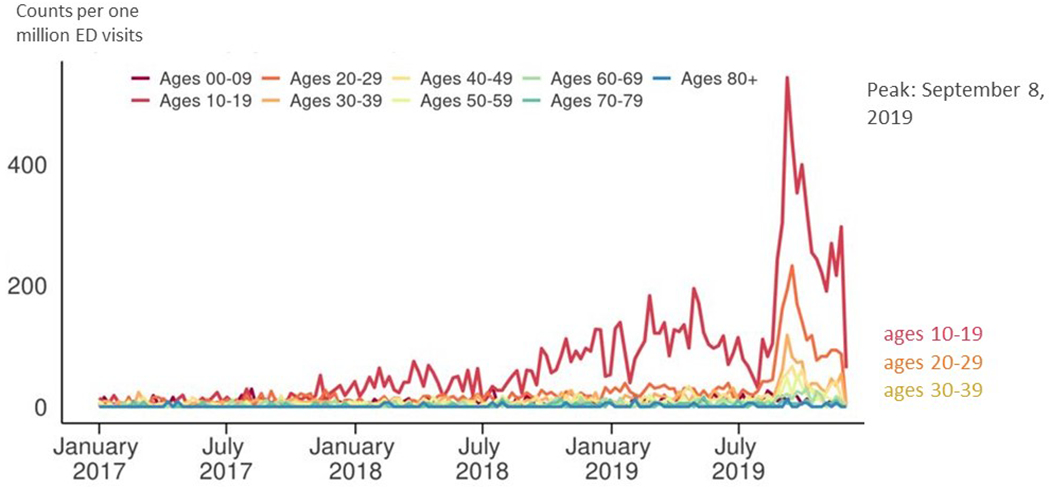
Use emergency department visit with e-cigarette, or vapping, product use in the chirf complaint*, by 10-year age group–National Syndromic Surveillance Program, January 1, 2017–December 7, 2009
*Attempts to exclude injuries unrelated elecrtonic-cigaratte (e-cigaratte), or vaping, product use-associated lung ingury (EVALI), such as device explosions and accidental ingestion of e-liquid, but does not exclude potentially related syndromes such as acute intoxication from tetrahydrocannabinol (THC) or nicotin piosoning.
Figure 2.
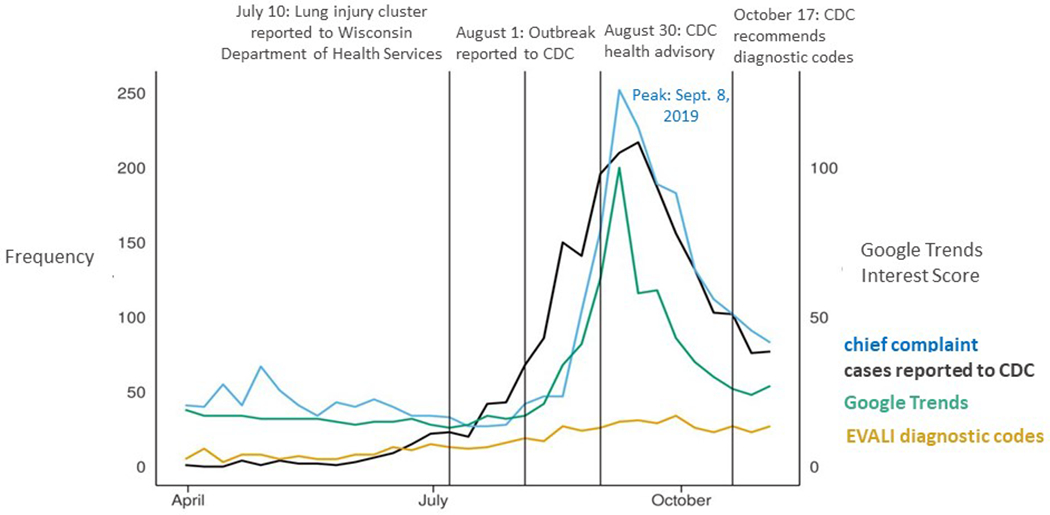
Comparison of weekly counts of US emergency department visits in the National Syndromic Surveillance Program with an e-cigarette, or vaping, product use in the chief complaint, US emergency department visits with EVALI-related diagnosis codes*, Online search interest as measured by Google Trends interest score for terms for e-cigarette, or vaping, from US searches admission date for confirmed or probable cases of EVALI reported to CDC, and April 1, 2019–December 7, 2019.
* CDC recommended codes for EVALI, including J68.0 (Bronchitis and pneumonitis due to chemicals, gases, fumes and vapors), J69.1 (Pneumonitis due to inhalation of oils and essences; includes lipoid pneumonia), J80 (Acute respiratory distress syndrome), J82 (Pulmonary eosinophilia, not elsewhere classified), J84.114 (Acute interstitial pneumonitis), J84.89 (Other specified interstitial pulmonary disease), J68.9 (Unspecified respiratory condition due to chemicals, gases, fumes, and vapors). Abbreviations: CDC, EVALI. Source for Google Trends: trends.google.com. A value of 100 for the Google interest score represents peak popularity for the search terms. A value of 50 means the term is half as popular. Search terms were: “vaping”, “vap”, “e-cig”, “e-cigarette”, “ecig”, and “electronic cigarette.”
From January 1, 2017 to December 7, 2019, the adjacent word pairs for symptoms that appeared most frequently in the query for use of e-cigarette, or vaping, products were “shortness breath” and “chest pain.” Within records for use of e-cigarette, or vaping, products, “shortness” and “breath” appeared together in 21% (95% CI: 20–23%) of visits during June 2, 2019–December 7, 2019 an increase from 8% (95% CI: 7–9%) during January 1, 2017–June 1, 2019 (Figure 3). Use of the word pair “chest pain” similarly increased to 18% (95% CI: 16–19%) after June 2, 2019 from 8% (95% CI: 6–9%) before June 2, 2019.
Figure 3.
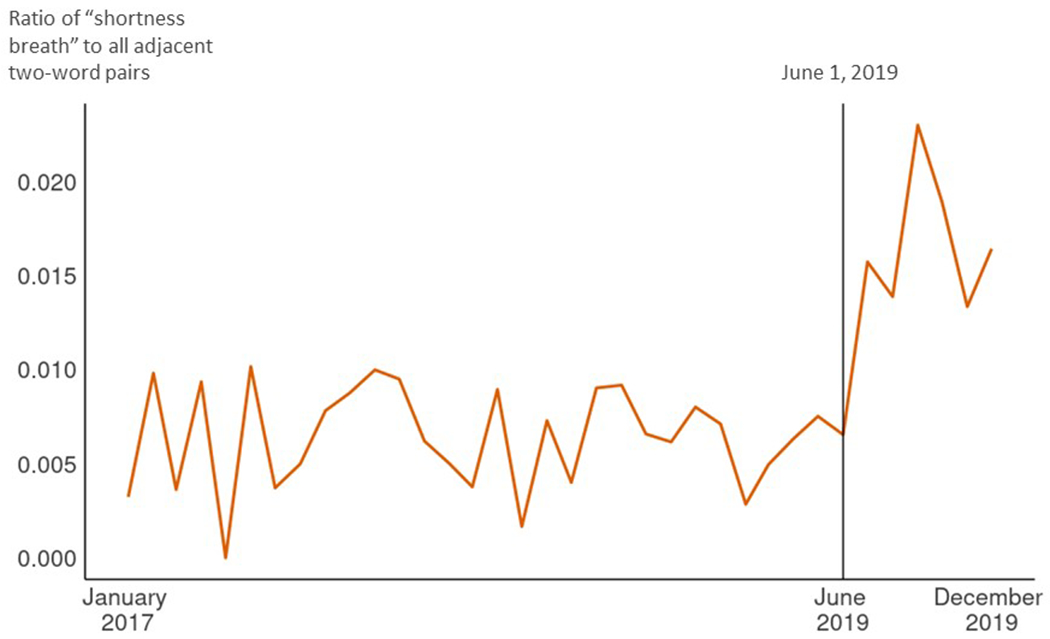
Within records returned by the search for electronic cigarette, or vaping, product use in the chief complaint, trend in the adjacent word pair (bigram) “shortness breath,” January 1, 2017–December 7, 2019. The trend is represented as the monthly count of the word pair “shortness breath” divided by the total number of all adjacent word pairs (bigrams) in records returned by the search that month
Outcome query
The trend in ED visits with EVALI-related diagnosis codes changed in the first week of June 2019. From the week of June 2, 2019 to the week of September 29, 2019, use of these codes increased weekly by an average of 47 per one million visits (95% CI: 36–57). Among males, the incidence of ED visits for EVALI-related codes was higher after June 2, 2019 than during January 1, 2017–June 1, 2019 (Incidence Ratio: 3.4, 95% CI: 2.9–4.0). Incidence was also higher for females after June 2, 2019 than during January 1, 2017–June 1, 2019, although the increase was not as large as for males (Incidence Ratio: 2.0, 95% CI: 1.7–2.3).
An increase in the number of visits among people with a potential EVALI-related discharge diagnosis began the week of June 2, 2019 (Figure 4), the same time that shortness of breath was increasingly seen in records with chief complaints related to e-cigarette, or vaping, products (Figure 3) While visits with these codes have declined since peaking the week of September 29, they remain higher than any time before June 2019.
Figure 4.
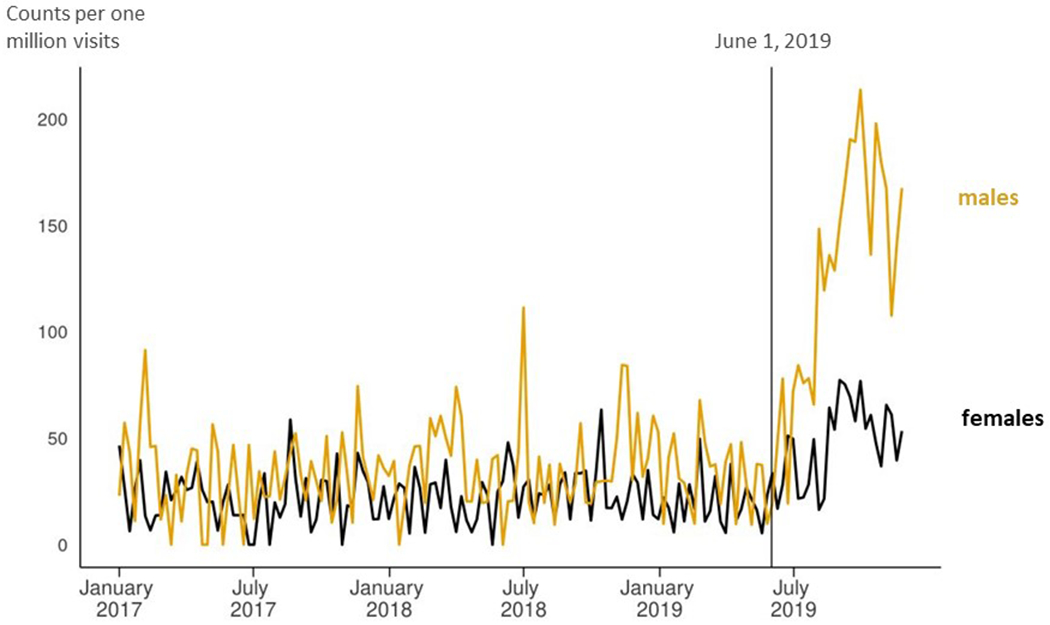
US emergency department visits among patients aged 11–34 with potential EVALI-related diagnoses who were admitted, transferred or died, by sex — National Syndromic Surveillance Program, January 1, 2017–December 7, 2019
*CDC recommended codes for EVALI, including J68.0 (Bronchitis and pneumonitis due to chemicals, gases, fumes and vapors), J69.1 (Pneumonitis due to inhalation of oils and essences; includes lipoid pneumonia), J80 (Acute respiratory distress syndrome), J82 (Pulmonary eosinophilia, not elsewhere classified), J84.114 (Acute interstitial pneumonitis), J84.89 (Other specified interstitial pulmonary disease), J68.9 (Unspecified respiratory condition due to chemicals, gases, fumes, and vapors). Abbreviation: EVALI.
Discussion
These analyses suggest that ED visits associated with EVALI began to spike in June 2019, peaked with cases reported to CDC in September, and have since declined. From January 2017 to June 2019, there was a gradual rise in ED visits with e-cigarette, or vaping, product use mentions. In the first week of June 2019, chief complaints that included these products and shortness of breath began a sharp increase, suggesting that this EVALI-related symptom was appearing more often in people using e-cigarette, or vaping, products. That same week in June, discharge diagnoses with codes that CDC would later recommend for EVALI began to rise nationwide among ages 11–34. These increases in June 2019 coincide with the first known EVALI cluster.1 As with cases reported to CDC2 and a previous analysis in Illinois,1 ED visit rates were higher in males. This analysis of ED data suggests that EVALI sharply increased in the summer of 2019 and had not been occurring at the same level over a longer period without detection.
The gradual increase in chief complaints with e-cigarette, or vaping, product use during January 1, 2017–June 1, 2019, especially among ages 10–19, could reflect sporadic cases from the same products or substances that later contributed to the wider outbreak when they became more commonly used. This gradual increase could also be caused by the increasing use of e-cigarettes containing nicotine. The percentage of U.S. high school students reporting e-cigarette use in the past 30 days increased from 11.7% in 2017 to 27.5% in 2019. 16 Newer generation e-cigarettes use nicotine salts,17 which allow more nicotine to be inhaled with less irritation.18 This may increase the risk of adverse effects to the lungs due to more frequent and stronger inhalation, or other health effects, such as nicotine poisoning or effects from other potential toxicants such as flavoring agents. The increase also coincided with the use of cannabinoid (CBD) oil in these products.19 The rise in these ED visits may also be driven by acute intoxication from THC, which increased in availability over this time period, synthetic cannabinoids, or other drugs. More study is needed to understand the increase between 2017 and June 2019.
The number of ED visits with the use of e-cigarette, or vaping, products in the chief complaint peaked during the week of September 8, 2019, the same week as a peak in Google searches for similar terms, following widespread national media attention. This could reflect a real increase in the occurrence of incident EVALI cases over time. The lung injury outcome query, which relies on use of specific diagnostic codes, increased beginning the first week in June 2019 and peaked during the week of September 29, 2019, before CDC recommended these codes for use on October 17. This slower rise and later peak might be caused by more gradual uptake of certain diagnostic codes. Alternatively, some of the ED visits with e-cigarette product use in the chief complaint but no EVALI-associated diagnosis may represent less severe effects or were early signs of more serious injury, such as shortness of breath that later progressed to respiratory failure.
This report has limitations. First, both the exposure and outcome searches return records unrelated to the current injury and where e-cigarette use is incidental to the visit. Second, the exposure query is as likely affected by public and clinical awareness of the outbreak, which increases the likelihood that e-cigarette product is mentioned in the chief complaint. Third, the outcome query relies on the use of specific codes and likely underestimates the number of EVALI visits. While the magnitude of the underestimate cannot be assessed at the national level, an analysis of confirmed and probable cases in Illinois found 23% of 159 patients ages 11–34 had a CDC-recommended discharge diagnosis so would have been captured by the outcome query. Finally, NSSP coverage is not uniform across or within all states, and healthcare facilities contributing data to the system change over time as new hospitals are added to the system, and more rarely when they close. Between the first week of June and first week of November, the number of facilities sending data to NSSP increased from 3,109 to 3,247.
Despite these limitations, syndromic surveillance also has important strengths, including timeliness, automated reporting, the ability to rapidly examine local and national trends, and the flexibility to rapidly change syndrome definitions without changing data collection, which make ED data a valuable complement to traditional epidemiologic investigations. In the future, ED data can be used in combination with reports from clinicians to understand any spikes that may be caused by increasing exposure to e-cigarette, or vaping, products. CDC announced in November 2019, that it would no longer request EVALI case reports for patients who were not hospitalized; data from ED visits that do not lead to hospitalization can thus offer insight on trends in less severe cases.
Conclusion
ED data suggest that EVALI sharply increased between early June and early September 2019, particularly among males and young people. While ED visits with chief complaint terms and discharge diagnosis codes associated with EVALI have declined since their peak, they have not fallen to the rates observed before June 2019, demonstrating a need for continued monitoring and prevention.
Supplementary Material
Footnotes
Publisher's Disclaimer: Author: This file is the accepted version of your manuscript, and it shows any changes made by the Editor-in-Chief and the Deputy Editor since you submitted your last revision. This is the version that is being sent to Manuscript Editing for further editing in accordance with NEJM style. You will receive proofs of the edited manuscript, by e-mail. The proofs will contain queries from the manuscript editor, as well as any queries that may be present in this file. The proof stage will be your next opportunity to make changes; in the meantime, please do not make any changes or send any new material to us.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Layden J, Ghinai I, Pray I, et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin — preliminary report. N Engl J Med 2019. Sep 6. [DOI] [PubMed] [Google Scholar]
- 2.Lozier MJ, Wallace B, Anderson K, et al. Demographic, Product, and Substance-Use Characteristics of Hospitalized Patients in a Nationwide Outbreak of E-cigarette, or Vaping, Product Use–Associated Lung Injuries — United States, December 2019. MMWR Morb Mortal Wkly Rep 2019;68:1142–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Severe pulmonary disease associated with using e-cigarette products. Health Alert Network. August 30, 2019. CDCHAN-00421. https://emergency.cdc.gov/han/han00421.asp.
- 4.Perrine CG, Pickens CM, Boehmer TK, et al. Characteristics of a Multistate Outbreak of Lung Injury Associated with E-cigarette use, or Vaping – United States, 2019. MMWR Morb Mortal Wkly Rep 2019; 68:860–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products: Dates of symptom onset and hospital admission for patients with lung injury associated with e-cigarette use, or vaping — United States, March 31–November 16, 2019. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
- 6.Gould DW, Walker D, Yoon PW. The Evolution of BioSense: Lessons Learned and Future Directions. Public Health Reports. 2017. Volume: 132 issue: 1_suppl, page(s): 7S–11S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoon PW, Ising AI, Gunn JE. Using Syndromic Surveillance for All-Hazards Public Health Surveillance: Successes, Challenges, and the Future. Public Health Reports 2017;I32(Supplement I): 3S–6S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. National Syndromic Surveillance Program (NSSP): BioSense Platform. https://www.cdc.gov/nssp/biosense/index.html.
- 9.CDC. ICD-10-CM Official Coding Guidelines – Supplement. Coding encounters related to E-cigarette, or Vaping, Product Use. https://www.cdc.gov/nchs/data/icd/Vapingcodingguidance2019_10_17_2019.pdf.
- 10.Google. FAQ about Google Trends data. https://support.google.com/trends/answer/4365533?hl=en.
- 11.Mavragani A and Ochoa G. Google Trends in Infodemiology and Infoveillance. JMIR Public Health Surveill 2019. May;5(2):e13439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muggeo VMR Estimating regression models with unknown break-points. Statistics in Medicine 2003. September: 22(19): 3055–3071. [DOI] [PubMed] [Google Scholar]
- 13.Muggeo VM. Segmented: an R package to fit regression models with broken-line relationships. R News. 2008. May;8(1):20–25. [Google Scholar]
- 14.Silge J, Robinson D (2016). “tidytext: Text Mining and Analysis Using Tidy Data Principles in R.” JOSS, 1(3). doi: 10.21105/joss.00037, 10.21105/joss.00037. [DOI] [Google Scholar]
- 15.Stevenson M epiR: Tools for the Analysis of Epidemiological Data. https://cran.r-project.org/web/packages/epiR/index.html.
- 16.Cullen KA, Gentzke AS, Sawdey MD. E-Cigarette Use Among Youth in the United States, 2019. JAMA, published online November 5. https://jamanetwork.com/journals/jama/article-abstract/2755265. [DOI] [PMC free article] [PubMed]
- 17.Surgeon General’s Advisory on E-cigarette Use Among Youth. https://e-cigarettes.surgeongeneral.gov/documents/surgeon-generals-advisory-on-e-cigarette-use-among-youth-2018.pdf.
- 18.Yingst JM, Hrabovsky S, Hobkirk et al. Nicotine absorption profile among regular users of a pod-based electronic nicotine delivery system. JAMA Netw Open. 2019;2(11):e1915494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.VanDolah HJ, Bauer BA, Mauck KF. Clinicians’ Guide to Cannabidiol and Hemp Oils. Mayo Clin Proc. 2019. Sep;94(9):1840–1851. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Outbreak of Lung Injury Associated with the Use of E-cigarette, or Vaping, Products: What CDC Recommends. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html#key-facts-vit-e.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


