Abstract
Background
Central venous catheterization is performed for such reasons as hemodynamic monitoring, parenteral nutrition, drug and fluid administration, and extracorporeal treatment. This study aimed to retrospectively review the indications for central venous catheter (CVC) insertion for vascular access and removal by pediatric intensive care unit (PICU) physicians, catheter types, and catheter-associated complications.
Materials and methods
The indications for CVC insertion and removal, catheter insertion site, types of catheters, catheter-associated complications, whether or not insertion was ultrasonographically guided, catheter-associated infections, and duration of use of 1200 catheters used by PICU physicians between 2015 and 2020 were retrospectively reviewed.
Results
In all, 315 (26.3%) hemodialysis catheters and 885 (73.8%) CVCs were inserted. Mean duration of catheter use was 12.33 ± 7.28 days. CVCs were inserted most commonly (28.4% [n = 341]) based on the indication of multiple drug infusions. In total, 44.8% of the CVCs were inserted under ultrasonographic guidance. The most common reason for the removal of catheters was that they were no longer needed (76.8% [n = 921]). Catheter-associated bloodstream infection occurred at the rate of 5.5 days per 1000 catheter days.
Conclusion
Central venous catheterization is becoming more widespread because of the benefits it provides during the follow-up and treatment of children. As central venous catheterization is a more invasive procedure than peripheral localization and is associated with severe complications, especially in pediatric patients, it should be carefully performed under sterile conditions and by experienced personnel based on appropriate indications. Central venous catheters should be removed as soon as the need disappears.
How to cite this article
Misirlioglu M, Yildizdas D, Yavas DP, Ekinci F, Horoz OO, Yontem A. Central Venous Catheter Insertion for Vascular Access: A 6-year Single-center Experience. Indian J Crit Care Med 2023;27(10):748–753.
Keywords: Catheterization, Child, Intensive care, Ultrasonography, Vascular access
Highlights
Central venous catheterization is a method that is increasingly used because of the benefits it provides in the treatment of children.
In pediatric patients, it should be carefully applied in sterile conditions and by experienced people with appropriate indications. It should be removed as soon as the need disappears.
Introduction
Although reliable vascular access in pediatric patients is critical, it can be challenging to achieve in critically ill children. Central venous catheterization is used in intensive care units, operating rooms, emergency services, and other services for monitoring, diagnosis, and treatment purposes. Due to its varied uses and the benefits it provides, its use is consistently increasing. Central venous catheterization is attempted using the femoral, internal jugular, and subclavian veins.1
Central venous catheterization is a more invasive procedure than peripheral catheterization, and is associated with more complications; ventricular arrhythmia, arterial puncture, tamponade, hemothorax, pneumothorax, arterial-vessel lacerations, and catheter malposition can occur.1–3 The present study aimed to retrospectively review the indications for central venous catheter (CVC) insertion and removal by pediatric intensive care unit (PICU) physicians for vascular access, and catheter types, and catheter-associated complications.
Materials and Methods
Central venous catheters inserted by PICU physicians in patients who were being followed-up and treated in the pediatric diseases clinic of a tertiary university hospital were retrospectively reviewed. In general, central venous catheterization is performed by PICU physicians at our hospital. As with all interventional procedures, the patients’ parents were informed about the CVC insertion procedure and their written consent was obtained by the physician prior to performing the procedure.
Central venous catheters were divided into four groups: peripherally inserted CVC, non-tunneled CVC, tunneled CVC, and implanted catheters (also known as ports). In terms of duration of use, there are two types of CVC: permanent and temporary. While temporary catheters are non-tunneled catheters with a peripherally located CVC, tunneled and implanted catheters are permanent.4 In this study, only centrally located temporary non-tunneled catheters were reviewed. Adequate sedation and analgesia were administered before the insertion procedure and the patients were followed-up with monitors measuring heart rate and rhythm, the respiratory rate, and oxygen saturation. The catheterization procedure was performed using the Seldinger method under conditions of asepsis and antisepsis.5 To visualize catheter placement after the insertion procedure and to evaluate complication development, a direct X-ray was obtained.
Central venous catheter-associated infection is diagnosed when the catheter has been in place for >48 hours and there is no source of infection other than the catheter, and bacteremia/fungemia is diagnosed based on ≥1 positive peripheral blood culture result and accompanying clinical findings of infection. When blood cultures taken from the catheter and periphery are compared, catheter blood culture grows ≥2 hours earlier and the number of colonies is five-fold greater, and the difference is significant. CVC-associated bloodstream infection is diagnosed according to the Clinical Practice Guidelines for the Diagnosis and Treatment of Intravascular Catheter-Associated Infection published by the American Infectious Diseases Society.6
Data for 1200 CVCs inserted by PICU physicians in patients followed-up and treated in the pediatric clinic inpatient service between January 1, 2015 and December 31, 2020 were obtained from patient’ medical records. The study included only successful catheter insertions in patients aged <18 years. Patients aged >18 years, those patients whose data were unavailable, unsuccessful catheterization attempts, and catheters inserted by departments other than the PICU were excluded from the study. Indications for catheter insertion and removal, the insertion site, the vessel used, catheter size, whether or not insertion was performed under ultrasonographic guidance, duration of catheter use, and the presence of catheter-associated bloodstream infection were examined. The study protocol was approved by the Non-Invasive Clinical Research Ethics Committee.
Statistical Analysis
Data were analyzed using IBM SPSS Statistics for Windows v.20.0 (IBM Corp., Armonk, NY). Descriptive statistics are presented as mean ± SD and median (range). In terms of quantitative data, Student's t-test was used for data with normal distribution and the Mann–Whitney U test was used for data not normally distributed. The Chi-square test was used to evaluate categorical data. The receiver operating characteristic curve (ROC) was used to evaluate the ability of the duration of catheter use to predict the development of catheter-associated infection, and the area under the curve (AUROC) was calculated. The best cut-off scores according to ROC analysis were calculated using YOUDEN's index. The level of statistical significance was set at p < 0.05.
Results
Data for 1200 CVCs inserted by PICU physicians between January 1, 2015 and December 31, 2020 in patients treated and followed-up in the pediatric clinic inpatient service were retrospectively reviewed. Mean age of the patients was 5.25 ± 4.64 years (range: 0–18 years). In total, 54.8% (n = 657) of the 1200 catheters were inserted in male patients, and 26.3% (n = 315) of all the catheters were hemodialysis catheters. The mean duration of catheter use was 12.33 ± 7.28 days (range: 1–41 days). The mean duration of hospitalization was 27.6 ± 21.2 days (range: 2–119 days). The most common indication for CVC insertion was multiple drug infusion (28.4% [n = 341]). The right internal jugular vein was most commonly used for CVC insertion (43.8% [n = 526]) (Fig. 1). In all, 76.8% (n = 921) of the catheters were removed because they were no longer needed. Table 1 presents the features of the inserted catheters, indication for catheterization, catheter type and dimensions, insertion vessel, whether or not ultrasonographic guidance was used during insertion, and indications for CVC removal. During the catheter insertion attempt; 96.8% (n = 484) did not develop complications. It was found that complications, such as 1.4% (n = 7) arterial puncture, 1.0% (n = 5) catheter malposition, 0.4% (n = 2) pneumothorax, and 0.4% (n = 2) ventricular arrhythmia developed.
Fig. 1.
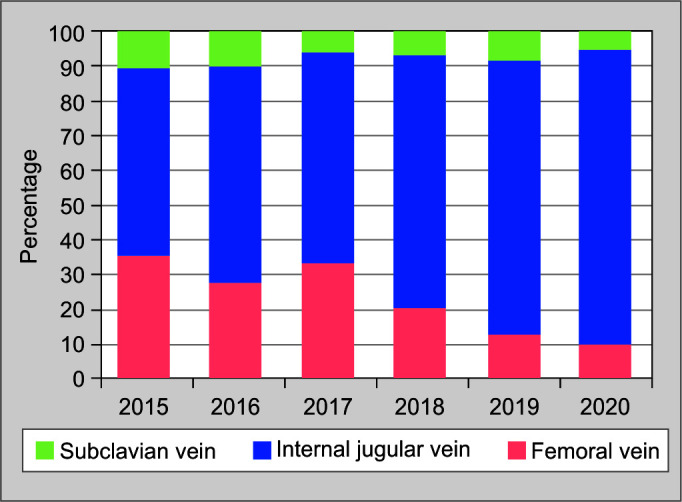
Distribution of catheter insertion sites according to year
Table 1.
Patient demographic characteristics (n = 1,200)
| n (%) | |
|---|---|
| Patient clinics | PICU: 294 (24.5%) |
| Pediatric oncology: 175 (14.6%) | |
| Pediatric bone marrow transplantation unit: 139 (11.6%) | |
| Pediatric hematology: 112 (9.3%) | |
| Pediatric metabolism: 93 (7.8%) | |
| Pediatric infection: 92 (7.7%) | |
| Pediatric nephrology: 83 (6.9%) | |
| Pediatrics: 77 (6.5%) | |
| Pediatric allergy and immunology: 30 (2.5%) | |
| Pediatric gastroenterology: 28 (2.3%) | |
| Newborn intensive care unit: 27 (2.3%) | |
| Pediatric cardiology: 21 (1.8%) | |
| Pediatric neurology: 13 (1.1%) | |
| Pediatric endocrinology: 10 (0.8%) | |
| Pediatric rheumatology: 6 (0.5%) | |
| Indications for CVC insertion | Multiple drug infusions: 341 (28.4%) Extracorporeal treatment: 305 (25.4%) |
|
|
| Vascular access problem: 304 (25.3%) | |
| Bone marrow transplantation: 135 (11.3%) | |
| Hemodynamic monitoring: 66 (5.5%) | |
| Total parenteral nutrition: 27 (2.3%) | |
| Other: 22 (1.8%) | |
| Indications for CVC removal | No longer needed: 921 (76.8%) |
| Catheter infection: 168 (14%) | |
| Catheter occlusion: 70 (5.8%) | |
| Thrombosis: 41 (3.4%) |
PICU, pediatric intensive care unit; CVC, central venous catheters
The catheter-associated bloodstream infection rate was 6.8% (n = 82); 5.5 days in 1000 catheter days. The cultured microorganisms were as follows: gram-negative bacteria: 46.3%; fungi: 31.7%; gram-positive bacteria: 22%. The frequency of infection according to 1000 catheter days showed that there were more infections in the CVC according to the type of CVC and in the femoral region according to the catheter insertion site, in cases in which ultrasonographic guidance was not used (Table 2). In total, 44.8% of the CVCs were inserted under ultrasonographic guidance. The use of ultrasonographic guidance increased over the course of the study and its use by year is shown in Figure 2. While infection and thrombosis development were observed more frequently in cases of catheter insertion without ultrasonographic guidance, their frequency did not differ significantly between insertion with and without ultrasonographic guidance (p > 0.05) (Table 3).
Table 2.
Catheter-associated bloodstream infection frequencies
| Duration of use, daysMean ± SD | p | Frequency n (%) | p | Per 1000 catheter days | |
|---|---|---|---|---|---|
| Central venous catheter (n = 885) | 13.82 ± 7.13 | <0.001 | 70 (7.9%) | 0.013 | 5.7 |
| Hemodialysis catheter (n = 315) | 8.14 ± 5.96 | 12 (3.8%) | 4.7 | ||
| Femoral vein catheter (n = 269) | 10.88 ± 6.94 | <0.001 | 20 (7.4%) | 0.716 | 6.8 |
| Subclavian vein catheter (n = 96) | 14.43 ± 7.43 | 8 (8.3%) | 5.8 | ||
| Internal jugular vein catheter (n = 835) | 12.55 ± 7.30 | 54 (6.5%) | 5.2 | ||
| Without ultrasonographic guidance (n = 663) | 12.46 ± 7.12 | 0.464 | 52 (7.8%) | 0.123 | 6.3 |
| With ultrasonographic guidance (n = 537) | 12.15 ± 7.49 | 30 (5.6%) | 4.6 |
Fig. 2.
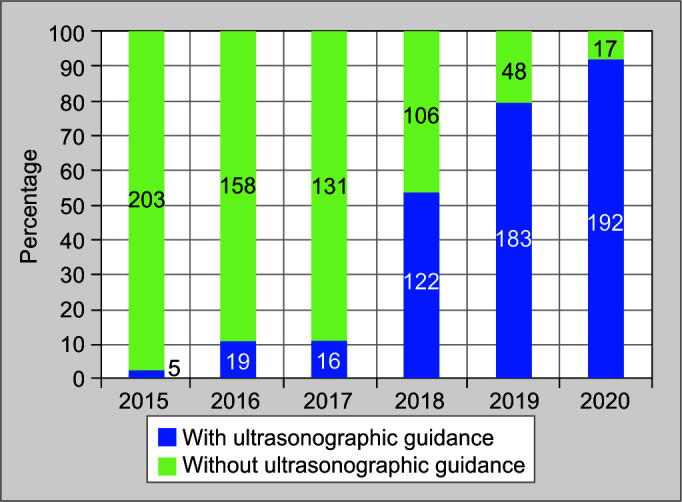
Distribution of ultrasonographic guidance according to year
Table 3.
Infections, thrombosis, and duration of catheter usage according to ultrasonographic guidance
| With ultrasonographic guidance (n = 537) | Without ultrasonographic guidance (n = 663) | p | |
|---|---|---|---|
| Catheter-associated bloodstream infection | 30 (5.6%) | 52 (7.8%) | 0.123 |
| Catheter-associated venous thrombosis | 12 (2.2%) | 21 (3.2%) | 0.326 |
| Duration of catheter usage, days | 12.2 ± 7.5 | 12.5 ± 7.1 | 0.464 |
The effects of some clinical features on the development of catheter-associated bloodstream infection were evaluated (Table 4). The incidence of catheter-associated bloodstream infection was higher in patients that received total parenteral nutrition and in those with catheter size ≤7 Fr (p = 0.008 and p = 0.005, respectively). The mortality rate was higher in patients that developed catheter-associated bloodstream infections. Duration of hospitalization was longer in patients that developed catheter-associated bloodstream infections, as compared with those that did not (Table 5).
Table 4.
Catheter-associated blood circulation infections according to patient clinical features
| Catheter-associated bloodstream infection n (%) | p | |
|---|---|---|
| Gender | ||
| Male (n = 657) | 43 (6.5) | 0.730 |
| Female (n = 543) | 39 (7.2) | |
| Total parenteral nutrition | ||
| Yes (n = 27) | 6 (22.2) | 0.008 |
| No (n = 1173) | 76 (6.5) | |
| Catheter size | ||
| ≤7 F (n = 904) | 72 (8.0) | 0.005 |
| >7 F (n = 296) | 10 (3.4) | |
| Catheter insertion vessel | ||
| Internal jugular vein (n = 835) | 54 (6.5) | 0.716 |
| Subclavian vein (n = 96) | 8 (8.3) | |
| Femoral vein (n = 269) | 20 (7.4) | |
| Ultrasonographic guidance | ||
| Yes (n = 537) | 30 (5.6) | 0.123 |
| No (n = 663) | 52 (7.8) | |
| Mortality | ||
| Yes (n = 212) | 22 (10.4) | 0.024 |
| No (n = 988) | 60 (6.1) |
Table 5.
Duration of catheter use and hospital stay in patients with and without catheter-related bloodstream infection
| Catheter-related bloodstream infection | |||
|---|---|---|---|
|
Yes (n = 82)
Mean ± SD Median (range) |
No (n = 1118)
Mean ± SD Median (range) |
p | |
| Duration of catheter usage, days | 19.0 ± 6.3 18.0 (7–41) |
11.8 ± 7.1 11.0 (1–33) |
<0.001 |
| Duration of hospital stay, days | 53.3 ± 48.8 38.0 (10–285) |
30.2 ± 30.5 22.0 (1–285) |
<0.001 |
The duration of catheter use was significantly longer in the patients who developed catheter-associated bloodstream infections than in those who did not (19.0 days and 11.8 days, respectively) (p < 0.001). The AUROC analysis was performed (AUROC 0.78) to evaluate the relationship between the duration of catheter use and the development of catheter-associated bloodstream infections, and the ROC curve showed that the best cut-off point for the risk of infection was 14 days (sensitivity: 81; specificity: 67). The catheter-associated bloodstream infection rate was 2.1% in patients with catheter use for <15 days, versus 15.2% in those with ≥15 days of catheter use (p < 0.001).
Discussion
Vascular access in pediatric patients is the most critical difficult step in treatment, because it is more laborious and difficult to obtain than in adults. Intravenous treatments are administered to patients through peripheral and central veins. Central venous catheterization is an interventional procedure that is becoming more common in clinics for various indications.7 Central venous catheterization is indicated for hemodynamic monitoring, extracorporeal treatments, parenteral nutrition, blood collection, multiple drug and fluid treatments, and administration of blood and blood products, and when peripheral vascular access is not possible.1 A study that included 120 catheters inserted over the course of 4 years in PICU patients reported that the most common reason for catheterization was the lack of peripheral vascular access (47.5%), followed by hemodynamic monitoring (22.5%).8 In the present study, the most common indication for catheterization was multiple fluid and drug administration (28.4%), followed by extracorporeal treatments (25.4%), and lack of peripheral vascular access (25.3%).
In total, 26.3% of the catheters inserted in the present study were temporary non-tunneled hemodialysis catheters, and mean duration of use of all catheters was 11 days (range: 1–41 days). In the present study, the internal jugular vein was most commonly used for CVC insertion and the frequency of femoral catheter insertion decreased throughout the study period. Furthermore, only 8% of CVCs were inserted in the subclavian vein. A study on 196 catheters inserted in the PICU over 2 years reported that hemodialysis catheters were used in 21% of the patients, CVCs were inserted in the internal jugular vein in 77% of the patients and in the femoral vein in 11%, and mean duration of catheter use was 22 days (range: 11–33 days).9 Physicians choose the site for CVC insertion based on patient’ clinical condition and experience. The subclavian region was used for CVC insertion in the present study at the lowest rate due to lack of experience and the associated technical difficulties and high incidence of such life-threatening complications as hemothorax and pneumothorax.10 Our catheter usage time is lower than the average, as catheters are attempted in patient services due to treatments, such as bone marrow transfer, erythrocytapheresis, and leukapheresis.
Various complications can occur during and after catheterization. Whereas mechanical complications occur in 5–19% of cases, infectious complications occur in 5–26%, and thromboembolic complications in 2–26% of cases.11 Arterial puncture, vascular injuries, catheter malposition, pneumothorax, hemothorax, and arrhythmias are among the mechanical complications associated with catheterization.11,12 Mechanical complications occur due to repetitive unsuccessful attempts at insertion, misdirection of the puncture needle, and insertion of the guide wire without aspiration of blood.11,13 To reduce the likelihood of these complications, the physician performing CVC insertion should be experienced and new practitioners should perform it in the presence of an experienced physician. The American Board of Internal Medicine does not provide clear advice on the number of procedures that a physician must perform to be considered experienced, but acknowledges that there is a learning curve that varies according to individual and procedure. It is estimated that a physician should perform 10–20 CVC insertions before feeling comfortable with the procedure.11 A literature review reported that catheter insertion by a physician who has performed ≥50 catheterizations is half as likely to result in a mechanical complication as when performed by a physician that has performed <50 CVC insertions.14 In the present study, catheterization procedures were performed by PICU physicians.
The mortality rate associated with CVC insertion in the present study was 0%. Furthermore, 98.3% of the patients did not have mechanical complications, whereas the most common mechanical complication was arterial puncture, followed by pneumothorax, hemothorax, catheter malposition, and ventricular arrhythmia. We think the present study's mechanical complication rate was low because CVCs were inserted only by experienced physicians. Whereas the present study's thrombosis rate was 3.4% (consistent with the literature), thrombosis did not occur in any of the patients with subclavian CVC insertion, and 90% of the instances of thrombosis occurred in cases of femoral vein catheterization. No complications secondary to thromboembolic events were observed in any of the patients due to early diagnosis, early removal of the catheter, and early treatment.
Central venous catheter insertion under ultrasonographic guidance significantly reduces the catheter-associated complication rate.15,16 The safest way to prevent CVC-associated complications is to perform the procedure under the guidance of ultrasonography, fluoroscopy, or X-rays. Fluoroscopy is often used for interventional radiology procedures. To increase the success rate of catheterization and reduce the complication rate, it is recommended to insert the catheter while visualizing the central vein and adjacent structures via ultrasonography. Dynamic or static methods are preferred during ultrasonography-guided catheter insertion. Using the dynamic method, the target vessel structure is displayed on a screen, and then insertion is performed. With the static method, the vessel structure and surrounding structures are displayed via ultrasonography before the procedure, and after the marking is made, the ultrasonography probe is removed and insertion is performed.17–19
In the present study, 44.8% of CVCs were inserted under ultrasonographic guidance, with its frequency of use increasing over the course of the study. In addition, whereas the development of infection and thrombosis were observed more frequently when CVCs were inserted without ultrasonographic guidance, the rates did not differ significantly between CVCs inserted with and without ultrasonographic guidance (p > 0.05). Moreover, the duration of catheter use did not differ significantly between CVCs inserted with and without ultrasonographic guidance (p > 0.05). No mechanical complications were observed in cases of ultrasonographically guided CVC insertion. Earlier studies report that performing CVC insertion with ultrasonographic guidance significantly decreases the incidence of complications.20–22 By ultrasonographically imaging the vein for insertion, insertion of a suitably sized catheter and in the presence of canalized thrombus in the lumen of the vein, intervention in that area should be avoided. While the use of ultrasonography was examined regarding complications during the intervention, no studies were found comparing the imaging in terms of complications developed during follow-up.20–22 In the present study, the high frequency of thrombosis and infection observed during follow-up in cases of CVC insertion without ultrasonographic guidance might have been due to use of an inappropriately sized catheter for the relevant vessel, inserting the CVC it into a vessel with canalized thrombus, or repeated CVC insertion attempts.
CVC-associated bloodstream infection is diagnosed according to the Clinical Practice Guidelines for the Diagnosis and Treatment of Intravascular Catheter-Associated Infection published by the American Infectious Diseases Society.6 In the present study, CVC-associated bloodstream infection was 5.5 per 1000 catheter days. The most common cultured microorganisms were gram-negative bacteria. The frequency of infection according to 1000 catheter days showed that infections were more common in the femoral region according to the catheter intervention site, and in cases of CVCs inserted without ultrasonographic guidance.
Topal et al. examined 196 catheters inserted in the PICU and reported a catheter-associated bloodstream infection rate of 6.2 per 1000 catheter days, mostly in the femoral region.9 A multicenter CVC-associated infection study based on 6 years of PICU data that included 66,194 CVCs reported an infection rate of 4.97 per 1000 catheter days.23 Another study based on data for 255 CVCs reported a CVC-associated bloodstream infection rate of 13.5 per 1000 catheter days and that gram-negative bacteria were the most common reproducing microorganism, as in the present study.24 In the present study, the CVC-associated bloodstream infection rate was higher in the patients with a catheter size ≤7 Fr and in those receiving total parenteral nutrition. The lipid and dextrose content of total parenteral nutrition fluids might contribute to the development of infection. A study that included 196 CVCs inserted in the PICU over a 2-year period observed that the total parenteral nutrition support was significantly associated with the risk of infection and that the risk increased with the use of CVCs for >10 days.8 Patients who develop infection have a longer hospital stay and an increased risk of mortality than those who do not. In the present study, the CVC-associated bloodstream infection rate was 2.1% in patients with catheter use for <15 days, vs 15.2% in those with catheter use ≥15 days. McLaws et al. observed that the incidence of infection in catheters used for 1–5 days was 2.1 per 1000 catheter days and increased to 10.2 per 1000 catheter days in catheters used for 16–30 days.25 Another PICU-based study reported that the critical period for the development of CVC-associated bloodstream infection was 7 days.24
The present study has several limitations. As the data were obtained retrospectively, the duration of catheter insertion and the number of insertion attempts are unknown. In addition, there may have been some complications that were not recorded. Although our clinic's experience using ultrasonography while inserting CVCs increased during the course of the study, its low rate of use early in the study might have negatively affected the results. Additional prospective studies on the effects of multiple CVC insertion attempts in PICU patients, with and without ultrasonographic guidance, are needed.
Conclusion
In conclusion, central venous catheterization should be performed when appropriately indicated under sterile conditions and by experienced physicians. To increase the CVC insertion success rate and minimize complications, catheter placement should be performed while visualizing the central vein and adjacent structures under ultrasonographic guidance. Patients should be carefully monitored for complications that can occur during the procedure and catheters should be removed as soon as they are no longer needed.
Orcid
Merve Misirlioglu https://orcid.org/0000-0002-9554-841X
Dincer Yildizdas https://orcid.org/0000-0003-0739-5108
Damla Pinar Yavas https://orcid.org/0000-0002-0424-4155
Faruk Ekinci https://orcid.org/0000-0001-6675-3150
Ozden Ozgur Horoz https://orcid.org/0000-0001-7590-650X
Ahmet Yontem https://orcid.org/0000-0002-9982-0310
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Javeri Y, Jagathkar G, Dixit S, Chaudhary D, Zirpe KG, Mehta Y, et al. Indian Society of Critical Care Medicine Position Statement for central venous catheterization and management 2020. Indian J Crit Care Med. 2020;24(Suppl 1):S6–S30. doi: 10.5005/jp-journals-10071-G23183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bagwell CE, Salzberg AM, Sonnino RE, Haynes JH. Potentially lethal complications of central venous catheter placement. J Pediatr Surg. 2000;35(5):709–713. doi: 10.1053/jpsu.2000.6029. [DOI] [PubMed] [Google Scholar]
- 3.Misirlioglu M, Horoz OO, Yildizdas D, Ekinci F, Yontem A, Pehlivan UA. A rare complication of central venous catheterization interventions: subdural effusion. Indian J Crit Care Med. 2022;26(3):384–386. doi: 10.5005/jp-journals-10071-24132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith SR. Vascular (venous) access for pediatric resuscitation and other pediatric emergencies. Up To Date. This topic last updated: Feb 24, 2022. [Google Scholar]
- 5.Seldinger SI. Catheter replacement of the needle in percutaneous arteriography: a new technique. Acta Radiol. 1953;39(5):368. doi: 10.3109/00016925309136722. [DOI] [PubMed] [Google Scholar]
- 6.Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, Grady NPO, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;49:1–45. doi: 10.1086/599376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatt S, Dahat A, Jain N, Nayak U, Patel V. Indications and complications of central venous catheterization in critically ill children in intensive care unit. Natl J Med Res. 2012;2(1):85–88. [Google Scholar]
- 8.Isguder R, Gulfidan G, Agin H, Devrim I, Karaarsan U, Unal N. Central venous catheterization in pediatric intensive care unit: a four-years’ experience. J Pediatr Emerg Intens Care Med. 2014;1(1):31–38. doi: 10.5505/cayb.2014.22932. [DOI] [Google Scholar]
- 9.Topal S, Sarac Sandal O, Ceylan G, Atakul G, Colak M, Soydan E, et al. Central venous catheter types and association with bloodstream infection in the pediatric intensive care unit: experience of two years. J Dr. Behcet Uz Chidren's Hospital. 2021;11(3):247–254. doi: 10.5222/buchd.2021.78736. [DOI] [Google Scholar]
- 10.Rey C, Alvarez F, De La Rua V, Medina A, Concha A, Diaz JJ, et al. Mechanical complications during central venous cannulations in pediatric patients. Intensive Care Med. 2009;35:1438–1443. doi: 10.1007/s00134-009-1534-0. [DOI] [PubMed] [Google Scholar]
- 11.Eisen LA, Narasimhan M, Berger JS, Mayo PH, Rosen MJ, Schneider RF, et al. Mechanical complications of central venous catheters. J Intensive Care Med. 2006;21(1):40–46. doi: 10.1177/0885066605280884. [DOI] [PubMed] [Google Scholar]
- 12.Alemohammad M. Central venous catheter insertion problem solving using intravenous catheter: Technical communication. Tehran Univ Med J. 2013;70(11):724–728. [Google Scholar]
- 13.Schummer W, Schummer C, Fröber R. Internal jugular vein and anatomic relationship at the root of the neck. Anesth Analg. 2003;96:1540–1541. doi: 10.1213/01.ane.0000072448.11064.d8. [DOI] [PubMed] [Google Scholar]
- 14.McGee Dc, Gould MK. Preventing complications of central venous catheterization. New Engl J Med. 2003;348(12):1123–1133. doi: 10.1056/NEJMra011883. [DOI] [PubMed] [Google Scholar]
- 15.Tolunay O, Okuyan MK, Celik T, Mert MK. Use of ultrasound for central venous catheterization in pediatric intensive care unit; a single center experience. J Ped Emerg Intensive Care Med. 2015;2(3):127–132. doi: 10.5505/cayb.2015.68077. [DOI] [Google Scholar]
- 16.Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: A metaanalysis of the literature. Crit Care Med. 1996;24(12):2053–2058. doi: 10.1097/00003246-199612000-00020. [DOI] [PubMed] [Google Scholar]
- 17.American Society of Anesthesiologists Task Force on Central Venous Access, Rupp SM, Apfelbaum JL, Blitt C, Caplan RA, Connis RT, et al. Practice guidelines for central venous access: A report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 2012;116(3):539–573. doi: 10.1097/ALN.0b013e31823c9569. [DOI] [PubMed] [Google Scholar]
- 18.Stone MB, Nagdev A, Murphy MC, Sisson CA. Ultrasound detection of guide wire position during central venous catheterization. Am J Emerg Med. 2010;28(1):82–84. doi: 10.1016/j.ajem.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 19.Resnick JR, Cydulka RK, Donato J, Jones RA, Werner SL. Success of ultrasound-guided peripheral intravenous access with skin marking. Acad Emerg Med. 2008;15(8):783–793. doi: 10.1111/j.1553-2712.2008.00174.x. [DOI] [PubMed] [Google Scholar]
- 20.Hayashi H, Amano M. Does ultrasound imaging before puncture facilitate internal jugular vein cannulation? Prospective randomized comparison with landmark-guided puncture in ventilated patients. J Cardiothorac Vasc Anesth. 2002;16:572–575. doi: 10.1053/jcan.2002.126950. [DOI] [PubMed] [Google Scholar]
- 21.Leung J, Duffy M, Finckh A. Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: a randomized, prospective study. Ann Emerg Med. 2006;48:540–547. doi: 10.1016/j.annemergmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Cakici M, Baran C, Ozcinar E, Hasde AI, Bermede O, Inan MB, et al. Impact of ultrasound guidance on mechanical complications of central venous catheterization: a single centre retrospective analysis. Turkish Journal of Vascular Surgery. 2016;25(3):122–127. doi: 10.9739/uvcd.2017-57731. [DOI] [Google Scholar]
- 23.Patel N, Petersen TL, Simpson PM, Feng M, Hanson SJ. Rates of venous thromboembolism and central line-associated bloodstream infections among types of central venous access devices in critically ill children. Crit Care Med. 2020;48(9):1340–1348. doi: 10.1097/CCM.0000000000004461. [DOI] [PubMed] [Google Scholar]
- 24.Rosado V, Camargos PA, Clemente WT, Romanelli RM. Incidence of infectious complications associated with central venous catheters in pediatric population. Am J Infect Control. 2013;41(9):e81–e84. doi: 10.1016/j.ajic.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 25.McLaws ML, Berry G. Non uniform risk of blood stream infection with increasing central venous catheter-days. Infect Control Hosp Epidemiol. 2005;26(8):715–719. doi: 10.1086/502608. [DOI] [PubMed] [Google Scholar]


