Abstract
Objective
To assess the feasibility and outcomes of implementing a hospital-based “opt-out” tobacco-cessation service.
Methods
In 2014, the Medical University of South Carolina adopted a policy that all hospitalized patients who self-report using tobacco be referred to tobacco-cessation service. This is a descriptive study of a real-world effort to implement guidelines for a hospital-based cessation service consistent with Joint Commission’s standards. Between February 2014 and May 2015, 42 061 adults were admitted to the Medical University of South Carolina Hospital. Eligible current cigarette smokers were referred to the tobacco-cessation service, which consisted of a bedside consult and phone follow-up 3, 14, and 30 days after hospital discharge using interactive-voice-response. The primary study outcomes evaluated the proportions of smokers reached by the bedside counselor and/or phone follow-up, smokers who opted out, and smokers who self-reported not smoking when last contacted by phone.
Results
Records identified 8423 smokers, of whom 69.4% (n = 5843) were referred into the service. One full-time bedside counselor was able to speak with 1918 (32.8%) patients, of whom 96 (5%) denied currently smoking and 287 (14.9%) refused counselling. Reach at follow-up was achieved for 703 (55%) smokers who received bedside counselling and 1613 (49%) who did not, yielding an overall follow-up reach rate of 60%. Of those reached by phone, 36.4% reported not smoking (51% vs. 27% for those who did and did not receive bedside counselling, respectively). Intent-to-treat abstinence rate was 13.5% according to the last known smoking status.
Conclusions
Findings from this study suggest that an inpatient smoking-cessation service with an “opt-out” approach can positively impact short-term cessation outcomes.
Implications
(1)The findings demonstrate the feasibility of implementing an automated large-scale opt-out tobacco-cessation service for hospitalized patients that is consistent with the Joint Commission recommended standards for treating tobacco dependence. (2) Receiving a bedside tobacco-cessation consult while hospitalized increased the use of stop smoking medications and abstinence from smoking after discharge from the hospital. (3) Even in those patients who did not receive a bedside consult, 5% accepted a referral to the South Carolina Tobacco Quitline to get help to stop smoking.
Introduction
In 2012, the Joint Commission (JC), which sets quality standards for hospitals in the United States, recommended that all current tobacco users identified upon hospitalization receive tobacco-cessation services as an inpatient and be followed-up within 1-month after hospital discharge.1,2 Most studies, but not all, have reported an increase in long-term quit rates when an in-hospital tobacco-cessation intervention is combined with phone follow-up support after discharge.3–8 Despite evidence generally supporting the benefits of providing smoking cessation services to hospitalized patients, few hospitals have fully implemented the JC quality standards.2,9 Most inpatient tobacco services rely on health care providers to refer patients into the service, with various strategies used to encourage providers to make referrals (eg, in-service programs, prompts built into the electronic health records), however not all service follow-up with patients after discharge from the hospital.2,9 Unfortunately, evidence suggests that only a fraction of eligible smokers receive referral to evidence-based smoking cessation support, which has led some researchers and healthcare organizations to recommend the employment of an “opt-out” referral system,10–12 in which patients are automatically enrolled unless they opt-out of the service.13 Also, few hospital cessation service outside of a research context routinely follow-up with patients after hospital discharge to assess tobacco use status and offer referrals to cessation support service as recommended JC.9
In 2014, the Medical University of South Carolina (MUSC) implemented a policy, consistent with the JC’s recommendation, requiring that (1) all hospitalized patients be screened for tobacco use, (2) all patients who report current smoking receive referral to an evidence-based tobacco-cessation treatment service, with (3) phone follow-up cessation support for 30 days after hospital discharge. Unique to this service was the development of an “opt-out” approach, where referrals to the cessation service occurred automatically without requiring any input or decision from either providers or patients. We report herein the reach and impact of the service over the first 15 months of implementation.
Methods
The MUSC hospital inpatient tobacco-cessation service is based in part upon the program previously implemented at the Ottawa Heart Institute which utilized bedside counselling and interactive voice response (IVR) follow-up calls to patients after hospital discharge.5,14,15 The MUSC service is unique because the treatment policy requires enrollment of all eligible current smokers, defined as having smoked within 30 days of their hospitalization, as well as referral to phone follow-up whether or not the patients received a bedside consult. This is a descriptive study of a real-world effort to implement standard guidelines for a hospital-based cessation service in a large academic medical center. All current adult cigarette smokers are enrolled in the service with the following exclusions: (1) died during hospitalization; (2) receiving hospice care; (3) unable to communicate due to language or medical condition; (4) not discharged back home, and (5) patients without a phone number. Patients who were readmitted but had an active follow-up call schedule were also excluded. Psychiatric inpatients were excluded from our paper because when we launched the service in February 2014, we were not cleared to provide bedside consults to psychiatric inpatients. When we were given permission to provide tobacco cessation support to this patient group, we utilized a group counselling approach rather than meeting with patients at their bedside. All eligible patients are automatically enrolled in the service, but are given the option to “opt-out” of the service. Patients can “opt-out” of the service either by refusing the bedside consult or by refusing and/or not responding to post-discharge phone calls.
The MUSC inpatient tobacco-cessation service includes three steps. In step 1 (screening): all hospitalized patients are asked about whether or not they use cigarettes. Smoking status is identified through the electronic medical record (EMR). Only patients who self-identify as current smokers are referred to the tobacco-cessation service. Most data are obtained from admission records, but in some instances smoking is identified using data obtained at patient discharge, the latter not seen by bedside counselor. We developed an explicit feature to allow patients who are identified as current smokers by the medical staff, but not through their EMR, to be manually referred to bedside counselling. Patients reporting current smoking are identified and referred through a daily census to a certified tobacco-treatment specialist, who then makes rounds throughout the hospital to engage all patients. In step 2 (bedside counselling): At the time that these data were collected, the MUSC tobacco-cessation service employed one full-time tobacco-treatment specialist who provided bedside consults to as many patients as could be reached while hospitalized. The bedside consult averaged about 15 minutes and involved asking patients to confirm their smoking status, obtaining a tobacco use history, assessment of nicotine dependence, readiness to quit, and the development of an individualized tobacco-treatment plan tailored to the patients’ readiness to quit and level of nicotine dependence. Information from the bedside consult was captured on an electronic tablet. The tablet generated an automated summary of the consult that included the patient’s smoking history and tobacco-treatment plan. Recommendations from the bedside counselor for stop smoking medications for patients were provided to the patient’s attending physician as a note in the medical record where they were encouraged to act upon the recommendation or modify it. A hospital charity account was established to provide access to stop smoking medications to patients who did not have insurance coverage for such medications. In step 3 (follow-up): All eligible patients, whether seen by the bedside counselor or not, are followed-up by IVR phone calls at 3, 14, and 30 days after discharge to assess their smoking status and provide additional support through the offer of a direct immediate referral “warm transfer” to the South Carolina Quitline. IVR calls are about 2-minutes long and are timed to occur at 3, 14, and 30 days post-discharge in an attempt to reinforce the importance of smoking abstinence during a high risk period for relapse. At each of the three follow-up contact days, at least six callback attempts are made at multiple times of the day, on varied days, to maximize the response rate. Service reach was defined as having been “touched” by the service intervention which delivers an opportunity to receive support to stop smoking. This includes being seen by the bedside counselor and/or receiving the phone follow-up call which not only assesses the patient’s smoking status, but also allows the patient to be connected to the South Carolina Tobacco Quitline if interested. The intervention is outlined in Supplementary Appendix 1 and includes the bedside counselling form and follow-up call script.
Data on all smokers are secured in a database that allows staff to track the status of patients enrolled into the service. A physician-led oversight committee meets monthly to track five quality indicators associated with the standards recommended by the JC: (1) the proportion of adult (18 years old and older) patients screened for tobacco use, (2) the proportion of current smokers reached by the bedside counselor, (3) the proportion of current smokers who receive pharmacotherapy support for their nicotine addiction, (4) the proportion of smokers reached by a follow-up call within a month after discharge, and (5) the proportion of smokers who report abstinence after discharge. The annual budget for the service which included expenses for the bedside counselor, printed materials, equipment, and the IVR system for making phone calls was approximately $170 000.
Data Sources
Data for this paper come from three sources: (1) EMRs, (2) the bedside consult questionnaire, and (3) the phone follow-up survey (copies of the follow-up surveys can be obtained from the corresponding author). EMRs contain information on the patients’ admission and discharge dates and times, unit, demographics (age, race, sex, type of insurance), smoking status, and identifying information such as full name, address, and phone number. Data on daily admissions are extracted from EMRs and deposited via a secure, HIPAA-compliant transfer to TelASK Technologies (Ottawa, Canada) which identifies current smokers eligible for the tobacco-cessation service. Each morning the list of inpatient smokers from the prior day’s admissions is made available to the bedside counselor through a secure web-interface provided by TelASK that can be accessed using a desktop computer and a tablet. The interface loads each patient’s identifying information to a task list that informs the bedside counselor where patients are located in the hospital. For patients seen by the bedside counselor, information on the consult is captured on the tablet and securely downloaded to the patient database system. Data from the EMRs received daily also allow the patient database system to detect smokers who have been discharged and are eligible to start receiving IVR calls, which are initiated 3 days after discharge. Based on the patient’s hospital-assigned medical record number, the system identifies patients who have been readmitted to the hospital within 6-months of the original admission, and excludes them from the service. Data from EMRs, bedside consult, and IVR calls are kept in separate databases and linked together for analysis via the patient’s medical record number and hospital admission date.
Statistical Analyses
We summarized data on the overall reach of the service, response to follow-up telephone calls, and self-reported smoking status 1-month after hospital discharge for patients hospitalized at MUSC between February 2014 and May 2015. Service reach was defined as eligible current cigarette smokers who received either a bedside consult and/or responded to at least one of the three follow-up callbacks after discharge from the hospital. Response to the telephone callback is defined as answering at least one of the three follow-up calls made 3, 14, and 30 days after hospital discharge. Self-reported smoking abstinence is measured as last-known-status self-reported during the most recent follow-up call, excluding those who did not use tobacco in the 30 days preceding hospitalization. When applying intent-to-treat analysis of quit rates, all those not reached by phone were considered to be still smoking, allowing all eligible smokers to be included in the denominator and conservatively estimating overall quitting behavior. Frequencies and percentages were reported for categorical variables whereas medians and ranges, means and standard deviations (SD) were reported for continuously measured variables. All statistical analyses were performed in SAS 9.4 (SAS Institute, Cary, NC).
Results
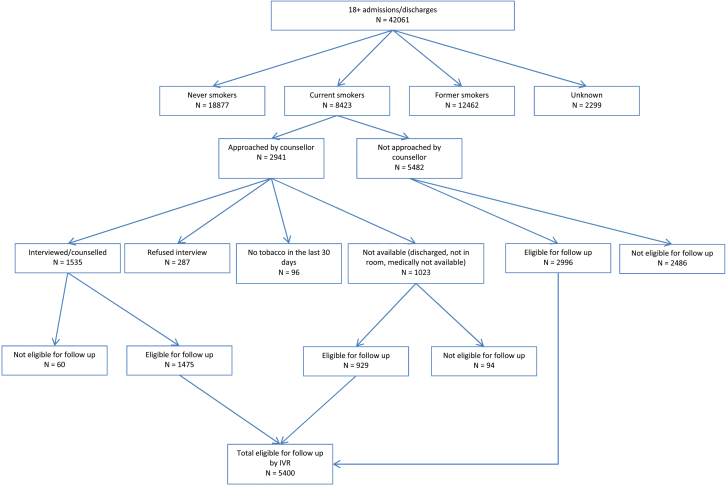
Between February 2014 and May 2015 there were 42 061 adult admissions to the MUSC hospital, of who 8423 (20%) reported current smoking (Figure 1). Of identified current smokers 69.4% (5843/8423) were deemed eligible for referral to the tobacco-cessation service. The bedside counselor attempted to interview 2941 patients, of whom 1918 were reached while in the hospital and 1023 were not reached. Of those not reached by the bedside counselor most were discharged from the hospital before the bedside counselor could see them while some patients were deemed medically unavailable (eg, intubated, comatose). Of those reached by the bedside counselor, 80% (1535/1918) were successfully counseled, 15% (287/1918) opted out of counselling, and 5% (96/1918) denied using any tobacco products within the past 30 days.
Figure 1.
Flow of patients from screening to follow-up of adult admissions to the Medical University of South Carolina (MUSC) hospital Feb 2014–May 2015.
Among the 5482 patients not seen by the bedside counselor, 2996 were eligible for enrollment in the follow-up IVR cessation service while 2486 were not due to failure to provide a phone number or being discharged to places other than home (eg, discharged to a rehabilitation facility, hospice, prison, etc.). Overall, a total of 5400 patients were deemed eligible to receive phone follow-up calls.
Table 1 provides information on patient characteristics by smoking status. Current smoking was more common among males than females and those who were uninsured or on Medicaid than those with commercial insurance. Current smokers tended to be younger and have slightly longer lengths of stay in the hospital compared to former and never smokers. Current smoking was most common in those with a diagnosed psychiatric disorder (56.9%) and those treated for injury and poisoning (29.8%), but less prevalent among women admitted to the maternity ward (11.9%) and those with a diagnosis of cancer (13.9%) (data not shown).
Table 1.
Patient Characteristics by Smoking Status
| Patient characteristics | Current smokers (n = 8423, 20.0%) | Former smokers (n = 12 462, 29.6%) | Never smokers (n = 18 877, 44.9%) | Unknown status (n = 2299, 5.5%) | Total N = 42 061 |
|---|---|---|---|---|---|
| Sex, n (%)a | |||||
| Females | 3761 (16.1) | 5759 (24.7) | 12 559 (53.9) | 1214 (5.2) | 23 293 |
| Males | 4661 (24.8) | 6703 (35.7) | 6317 (33.7) | 1080 (5.8) | 18 761 |
| Missing | 1 (14.3) | 0(0.0) | 1 (14.3) | 5 (71.4) | 7 |
| Age in year; median, mean (SD)b | 48, 46.8 (15.5) | 62, 59.5 (16.6) | 50, 49.5 (19.4) | 53, 52.3 (20.0) | 54, 52.1 (18.6) |
| Length of hospitalization in days; median, mean (SD)c € | 4, 6.3 (14.8) | 3, 5.8 (10.3) | 3, 5.4 (9.6) | 3, 7.2 (29.3) | 3, 5.8 (12.5) |
| Race, n (%)a | |||||
| Black | 2300 (20.5) | 2685 (23.9) | 5593 (49.8) | 662 (5.9) | 11 240 |
| White | 3658 (20.5) | 5953 (33.4) | 7249 (40.7) | 964 (5.4) | 17 824 |
| Other | 159 (12.6) | 244 (19.3) | 783 (61.8) | 80 (6.3) | 1266 |
| Missingd | 2281 (19.4) | 3592 (30.6) | 5261 (44.8) | 597 (5.1) | 11 731 |
| Insurance, n (%)a | |||||
| Medicare | 1701 (14.4) | 4604 (39.0) | 4914 (41.6) | 592 (5.0) | 11 811 |
| Medicaid | 1319 (28.0) | 967 (20.5) | 2215 (46.9) | 218 (4.6) | 4719 |
| Commercial | 1209 (15.3) | 2040 (25.8) | 4292 (54.3) | 360 (4.6) | 7901 |
| Uninsured | 1174 (36.2) | 634 (19.5) | 1081 (33.3) | 357 (11) | 3246 |
| Missingd | 2995 (20.8) | 4229 (29.4) | 6384 (44.4) | 776 (5.4) | 14 384 |
SD = standard deviation.
aChi-square test of independence p < .0001.
bChi-square test of median equality p < .0001.
cDuration of hospitalization was missing for 2007 patients.
dAbout one-third cases are missing information on race and insurance status because data linkage was not completed at the time of writing the paper. However, we do not believe that the smoking status rates as presented in the table above will vary much between the obtained partial sample and the full sample. Our plan is to add in the missing data when available.
Table 2 summarizes data for the 1535 patients who completed the bedside consult and who partially comprise the sample eligible for IVR follow-up. Ninety-four percent of patients reported that they were daily smokers, and most reported smoking their first cigarette within 5 minutes of waking up (79%). Few smokers (n = 156; 11%) had tried to quit in the past year for at least 24 hours, and of those only 63% were successful in quitting for at least 1 day. About 40% had high intention for quitting smoking, but only 8% were very confident that they would remain smoke-free after discharge. Unassisted quitting (ie, “cold turkey”) was the most common patient reported method of quitting, followed by e-cigarettes. Approximately 44% experienced craving to smoke while hospitalized, and the majority of those (81%) were interested in receiving NRT during their stay.
Table 2.
Patient Characteristics Assessed During the Bedside Consult
| N = 1535 | |
|---|---|
| Have you used cigarettes in the past 30 days? | |
| No | 9 (1%) |
| Yes | 1451 (94%) |
| Missing | 75 (5%) |
| Before coming to the hospital did you use cigarettes…a | |
| Daily | 1333 (92%) |
| Non-daily | 88 (6%) |
| Missing | 30 (2%) |
| How many years did you use cigarettes?a | |
| Median (Range) | 23.5 (80) |
| Mean (Standard Deviation) | 24.8 (13.9) |
| Missing (n) | 75 |
| On the days that you used cigarettes how many did you use?a | |
| Median (Range) | 10 (80) |
| Mean (Standard Deviation) | 15 (11.1) |
| Missing (n) | 116 |
| How soon after you wake up do you use cigarettes?a | |
| <5 min | 1147 (79%) |
| 6–30 min | 126 (9%) |
| 31–60 min | 29 (2%) |
| >60 min | 15 (1%) |
| Missing | 134 (9%) |
| How many quit attempts of at least 24 h have you made in the past year?a | |
| 0 | 1295 (89%) |
| 1 | 112 (8%) |
| 2 or more | 44 (3%) |
| How long did your quit attempt last? (in days)a,b | |
| 0 | 58 (37%) |
| 1 | 13 (8%) |
| 2–30 | 51 (33%) |
| >30 | 34 (22%) |
| On a scale of 1–5 with 5 being the strongest, how much do you intend to quit tobacco once you are discharged from the hospital?a | |
| 1 | 116 (8%) |
| 2 | 192 (13%) |
| 3 | 550 (38%) |
| 4 | 160 (11%) |
| 5 | 413 (29%) |
| Missing | 20 (1%) |
| On a scale of 1–5 with 5 being the strongest, how confident are you to remain quit once you are discharged from the hospital?a | |
| 1 | 259 (18%) |
| 2 | 485 (33%) |
| 3 | 560 (39%) |
| 4 | 46 (3%) |
| 5 | 79 (5%) |
| Missing | 22 (2%) |
| Methods used to quit during most recent quit attempta,b | |
| Unassisted quitting | 94 (60%) |
| Class | 2 (1%) |
| Quit line | 1 (1%) |
| Prescription medication | 11 (7%) |
| Over the counter medication | 13 (8%) |
| E-cigarette | 28 (18%) |
| Have you experienced strong cravings to smoking since admission?a | |
| No | 806 (56%) |
| Yes | 626 (44%) |
| Missing | 19 (1%) |
| Would patient be interested in getting some nicotine medication while in hospital?a,c | |
| No | 83 (13%) |
| Yes | 506 (81%) |
| Missing | 37 (6%) |
| Cessation aid recommendeda | |
| Patch | 762 (53%) |
| Gum | 70 (5%) |
| Lozenge | 557 (38%) |
| Zyban/Wellbutrin | 18 (1%) |
| Chantix/Varenicline | 47 (3%) |
aAmong those who have used cigarettes in the past 30 days.
bAmong those who had at least one quit attempt.
cAmong those who had cravings to smoking.
Of the 5400 patients enrolled in the IVR follow-up calls, 42.8% (n = 2316) were reached at least once within 30 days post discharge. Of the 3084 patients who did not respond to the follow-up calls, 796 (25.8%) were mostly not reached because of wrong or non-working numbers while the balance (n = 2288, 74.2%), had apparently valid phone numbers but did not respond to any of the 18 callback attempts made to them and thus were classified as passively “opted out” of the service. Of the 2316 individuals who responded to at least one of the phone follow-up calls, only 18 (0.77%) affirmatively opted out of future calls. Combined, 60.4% (3531/5843) of the smokers were reached by the service, either by inpatient contact with the bedside counselor and/or by IVR follow-up calls.
Among those who were reached by phone, 36.4% self-reported not smoking at the time of their last phone contact. Based on intent-to-treat, 13.5% of patients were classified as not smoking based on their most recent follow-up call. Overall, of the 1824 patients reached by phone and who acknowledged that they were still currently smoking, 19.6% (n = 357) selected the option of being transferred to the South Carolina Quitline to receive additional cessation support. Acceptance of the Quitline referral was higher in those who only received the IVR call compared to those that received both the bedside consult while hospitalized plus the IVR follow-up call (35% [281/1121] vs. 11% [76/703]).
Table 3 compares outcomes for patients who received bedside counselling and post-discharge IVR phone follow-up calls and those who received post-discharge IVR calls only. Bedside tobacco-cessation counselling was associated with a 13% increase in response to the follow-up calls, a 90% increase in reported tobacco abstinence, and an over two-fold increase in the reported use of stop smoking medications.
Table 3.
Outcomes for Patients Who Received Bedside Counseling and IVR Versus IVR Follow-up only
| Bedside + IVR | IVR Only | RR (95% CI) | |
|---|---|---|---|
| Reached within 1-month post-discharge (of those eligible to receive calls) | 703/1280 = 55% | 1613/3324 = 49% | 1.13 (1.07–1.20) |
| Used medications within 1-month post-discharge (of those who were reached by phone)a | 144/703 = 21% | 92/1121 = 8% | 2.5 (1.96–3.20) |
| Abstinent from smoking within 1-month post-discharge (of those reached by phone)a,b | 359/703 = 51% | 304/1121 = 27% | 1.9 (1.67–2.12) |
| Abstinence within 1-month applying intent-to-treat (of those activated for follow-up)a,b | 359/1475 = 24% | 304/3443 = 9% | 2.8 (2.39–3.16) |
CI = confidence interval; EMR = electronic medical record; IVR = interactive voice response.
aExcluding 492 false positives (defined as those individuals identified by EMR as smokers who upon phone follow-up denied that they had been a smoker at the time of hospitalization) identified during follow-up calls among the IVR only group.
bLast known smoking status.
Discussion
The findings from this study demonstrate the feasibility of implementing an “opt-out” tobacco-cessation service for hospitalized patients that is consistent with the JC recommended standards for treating tobacco dependence.1 With one full-time bedside tobacco-treatment specialist counselor and an automated IVR telephone support service, 60.4% of eligible patients received evidence-based cessation support. The majority of patients reached by phone within 30 days of hospital discharge reported that they had returned to smoking again, although abstinence rates were almost three-fold higher among those who had received a bedside consult while hospitalized. These findings are consistent with other studies which have reported that receiving an inpatient bedside tobacco-cessation consult is associated with a greater likelihood of using stop smoking medications and refraining from smoking after discharge from the hospital.3–8 Other studies have suggested that IVR follow-up alone can also improve cessation outcomes,7,14,15 although in this study we do not have a no IVR comparison group.
The “opt-out” smoking cessation policy adopted by MUSC is novel since nearly all of the published studies on hospital-based cessation services rely on physician and/or patient self-referrals to trigger the delivery of tobacco-cessation support.3–9 However, “opt-out” strategies have also been recommended by the National Institute for Health and Care Excellence in the United Kingdom.16 Our tobacco-cessation service attempted to reach all smokers, regardless of their motivation to quit. Consistent with other studies describing “opt-out” programs, we found that the vast majority of patients accepted the service when offered.17 For example, 80% (1535/1918) of hospitalized smokers who were approached by the counselor accepted the bedside consult. This percentage is slightly lower than what Warren et al.12 found, where over 90% of cancer patients accepted tobacco-cessation treatment when offered. Of the 4112 patients who were eligible to receive our automated follow-up calls, less than 1% (18/4112) explicitly asked to be removed from the service suggesting that patients are highly receptive to the “opt-out” policy. These findings suggest that patient resistance to smoking cessation support may not be a significant barrier in hospitalized patients. These results significantly strengthen the argument to expand “opt-out” “approaches for cessation support in both the inpatient and outpatient setting.10,11 In this case, automated evidence-based cessation support was provided without any additional clinical burden on hospital staff or admission teams. Thus implementation was well received by both patients and clinicians.
Implementation of MUSC’s “opt-out” tobacco-cessation service was not accomplished without learning some lessons. First, developing an automated system using EMR to consistently identify tobacco users admitted to the hospital on a daily basis was challenging. It took several months to develop and test a system that would reliably identify patient records and work out logistics for downloading, transferring, and reporting patient information in a way that was easily accessible by the bedside counselor and usable by the IVR phone follow-up system. This effort was further complicated by the MUSC’s implementation of a new EMR system in July 1 2014. The switch to a new EMR system resulted in a brief interruption in our ability to identify records, which resulted in the suspension of the IVR follow-up calls for 2 months (ie, on July and August, 2015). Second, before the service was implemented we did not know how many eligible smokers we would be able to reach. With only one full-time bedside tobacco-treatment specialist and automated IVR telephone follow-up calls, the service was able to intervene in person with about one-third of eligible smoker and when combined with IVR phone follow-up with 60% of eligible adult smokers. Third, while most of the 5400 patients who were enrolled in the service had phones, about 8.5% of them were unreachable due to providing a wrong number on their medical record. Even with these challenges, the “opt-out” approach led to a significant proportion of patients receiving evidence-based tobacco-cessation support in-person, by phone, or via both service modalities.
An important strength of this implementation study was its use of existing clinical staff, rather than research personnel, to deliver the intervention. We did not know in advance of launching the service the required staffing capacity for our inpatient population. With just one full-time bedside counselor and an automated IVR telephone follow-up system, we were able to intervene with over 60% of eligible current smokers admitted to a large academic medical center, at a cost of about $36 per eligible patient. In January 2016 we hired a second bedside counsellor. Preliminary data support an increased number of counselled patients and higher follow-up reach rates. Like many real-world implementation studies there are important weaknesses that may reduce the internal validity of the reported findings. For example, there is no data from either a pre-implementation period or a comparison hospital to assess the relative impact of the “opt-out” approach on cessation outcomes. In addition, many patients failed to respond to follow-up phone calls and cessation outcomes were short-term (30 days) and based on self-report. Prior studies suggest that smoking status tends to be underreported by some categories of patients.18–20 Another weakness of the study has to do with our reliance on the EMR system to capture patients’ tobacco use behavior, which is not standardized. We acknowledge that we likely missed some smokers by relying on self-reported smoking status identified via the EMR. In fact, the service did enroll about 150 tobacco-users who were not identified as current smokers by the EMR, but were referred into the service by medical staff (ie, floor referrals). However, the overall 20% prevalence of smoking for our hospitalized patient is consistent with the population survey for South Carolina which shows a 21.5% smoking prevalence among adults.21 Finally, we only had limited information on the characteristics of patients enrolled in IVR follow-up but who did not receive bedside counselling, which makes it difficult to understand the lower abstinence rate observed in this subgroup of patients. The better outcomes seen among patients who received bedside counselling suggests that the service’s impact could be enhanced by hiring a second counsellor, which was recently done.
Despite these weaknesses, the findings from this study suggest that an inpatient smoking-cessation service with an “opt-out” approach can positively impact short-term cessation outcomes. The “opt-out” approach is novel in that patients were eligible for cessation counselling support during and after hospitalization regardless of whether they were ready to quit or not.
Supplementary Material
Supplementary data are available at Nicotine & Tobacco Research online.
Funding
Medical University of South Carolina Health.
Declaration of Interests
MUSC Health provided the sole funding for the service reported. All co-authors are either employed or contracted by MUSC. KMC and BAT have received separate grant funding from Pfizer, Inc., and both have received payments as expert witnesses in litigation filed against the tobacco industry. All other authors have no conflicts to report.
Supplementary Material
Acknowledgments
We would like to acknowledge support provided by Mark Daniels and Patricia Wagstaff who provided IT support for the service and James Brook, RN, MBA Oncology Service Line Director at the Hollings Cancer Center and Danielle Bowen Scheurer, MD, MSCR, Chief Quality Officer at MUSC, who provided both administrative and financial support to implement the inpatient tobacco-cessation service. We would also like to acknowledge the contribution of Danny Woodard, MS who served as the bedside counselor for the Tobacco-cessation Service during the period covered by this report.
Contributor Information
Georges J Nahhas, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC;.
Dianne Wilson, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC;.
Vince Talbot, TelASK Technologies Inc., Ottawa, Canada;.
Kathleen B Cartmell, College of Nursing, Medical University of South Carolina, Charleston, SC;.
Graham W Warren, Department of Radiation Oncology, Medical University of South Carolina, Charleston, SC;; Department of Cell and Molecular Pharmacology, Medical University of South Carolina, Charleston, SC;
Benjamin A Toll, Department of Public Health Sciences, Medical University of South Carolina, Charleston, SC.
Matthew J Carpenter, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC;.
K Michael Cummings, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC;.
References
- 1. Organizations JCoAoH. Tobacco Treatment Measures (TTM). 2011; www.jointcommission.org/assets/1/6/Tobacco%20Treatment%20Measures%20List1.PDF, 2016. Accessed November 3, 2016.
- 2. Fiore MC Goplerud E Schroeder SA. The Joint Commission’s new tobacco-cessation measures–will hospitals do the right thing? N Engl J Med. 2012;366(13):1172–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Freund M Campbell E Paul C et al. Increasing hospital-wide delivery of smoking cessation care for nicotine-dependent in-patients: a multi-strategic intervention trial. Addiction. 2009;104(5):839–849. [DOI] [PubMed] [Google Scholar]
- 4. Katz DA Holman JE Johnson SR et al. Implementing best evidence in smoking cessation treatment for hospitalized veterans: results from the VA-BEST Trial. Jt Comm J Qual Patient Saf. 2014;40(11):493–491. [DOI] [PubMed] [Google Scholar]
- 5. Reid RD Mullen KA Slovinec D’Angelo ME et al. Smoking cessation for hospitalized smokers: an evaluation of the “Ottawa Model”. Nicotine Tob Res. 2010;12(1):11–18. [DOI] [PubMed] [Google Scholar]
- 6. Rigotti NA Clair C Munafo MR Stead LF. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2012(5):CD001837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rigotti NA Regan S Levy DE et al. Sustained care intervention and postdischarge smoking cessation among hospitalized adults: a randomized clinical trial. JAMA. 2014;312(7):719–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smith PM Kraemer HC Miller NH DeBusk RF Taylor CB. In-hospital smoking cessation programs: who responds, who doesn’t? J Consult Clin Psychol. 1999;67(1):19–27. [DOI] [PubMed] [Google Scholar]
- 9. Duffy SA Cummins SE Fellows JL et al. Fidelity monitoring across the seven studies in the Consortium of Hospitals Advancing Research on Tobacco (CHART). Tob. Induc. Dis. 2015;13(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kotz D. Implementation of a new ‘opt-out’ default for tobacco treatment is urgently needed, but requires free access to evidence-based treatments. Addiction. 2015;110(3):387–388. [DOI] [PubMed] [Google Scholar]
- 11. Richter KP Ellerbeck EF. It’s time to change the default for tobacco treatment. Addiction. 2015;110(3):381–386. [DOI] [PubMed] [Google Scholar]
- 12. Warren GW Marshall JR Cummings KM et al. Automated tobacco assessment and cessation support for cancer patients. Cancer. 2014;120(4):562–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cummings KM. Smoking Isn’t Cool Anymore: The success and continuing challenge of public health efforts to reduce smoking. J Public Health Manag Pract. 2016;22(1):5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Regan S Reyen M Lockhart AC Richards AE Rigotti NA. An interactive voice response system to continue a hospital-based smoking cessation intervention after discharge. Nicotine Tob Res. 2011;13(4):255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reid RD Pipe AL Quinlan B Oda J. Interactive voice response telephony to promote smoking cessation in patients with heart disease: a pilot study. Patient Educ Couns. 2007;66(3):319–326. [DOI] [PubMed] [Google Scholar]
- 16. Excellence TNIfHaC. Stop smoking services. www.nice.org.uk/guidance/ph10?unlid=2390889542015830183649.
- 17. Nahhas GJ Cummings KM Talbot V Carpenter MJ Toll BA Warren GW. Who opted out of an opt-out smoking-cessation programme for hospitalised patients? J Smoking Cessation. 2016:1–6. [Google Scholar]
- 18. Morales NA Romano MA Michael Cummings K et al. Accuracy of self-reported tobacco use in newly diagnosed cancer patients. Cancer Causes Control. 2013;24(6):1223–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Patrick DL Cheadle A Thompson DC Diehr P Koepsell T Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84(7):1086–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shipton D Tappin DM Vadiveloo T Crossley JA Aitken DA Chalmers J. Reliability of self reported smoking status by pregnant women for estimating smoking prevalence: a retrospective, cross sectional study. BMJ. 2009;339:b4347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Prevention CfDCa. Centers for Disease Control and Prevention’s STATE System State Highlights. 2014. http://nccd.cdc.gov/STATESystem/rdPage.aspx?rdReport=OSH_STATE.Highlights&rdRequestForwarding=Form. Accessed November 3, 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.