Abstract
Background:
When a water pipe breaks, contaminants can enter the drinking water system and cause waterborne illnesses such as acute gastrointestinal illness. In May 2010, a major water pipe broke near Boston, Massachusetts, and a boil water order was issued to nearly two million residents.
Methods:
Using a case-crossover study design, we examined the association between the water pipe break and subsequent emergency department visits for acute gastrointestinal illness. We identified cases of illness according to ICD-9-CM diagnosis codes and selected control dates two weeks before and after each case. We estimated the risk of visiting the emergency department during the 0–3 and 4–7 days following the water pipe break using conditional logistic regression models.
Results:
Our analysis included 5,726 emergency department visits for acute gastrointestinal illness from April 3, 2010 through June 5, 2010. Overall, there was a 1.25-fold increased odds for visiting the emergency department for acute gastrointestinal illness during the 0–3 days after the water pipe break (Odds Ratio, OR=1.25; 95% Confidence Interval, CI: 1.11–1.41) compared to referent dates selected two weeks before and after. During the 4–7 days after the break, the association diminished overall (OR=1.09; 95% CI: 0.96–1.23). However, in communities over 12 miles from the break, the 4–7 day association was elevated (OR= 1.39; 95% CI: 1.10, 1.75).
Conclusion:
This study suggests that a major water pipe break was associated with emergency department visits for acute gastrointestinal illness, particularly during the 0–3 days after the break, when a boil water order was in effect.
Keywords: Drinking Water, Water Supply, Acute Gastrointestinal Illness, Gastroenteritis, Emergency Department, Case-Crossover Study
Introduction
On the morning of Saturday, May 1, 2010, a major water pipe broke near Boston, Massachusetts, releasing millions of gallons of water and disrupting the drinking water supply for nearly two million residents.1,2 Specifically, a coupling that secured segments of a 10-foot diameter water pipe broke along a major distribution line serving the greater Boston area.1 By the late afternoon, Massachusetts Governor Deval Patrick issued a boil water order for the City of Boston and 29 nearby communities (Figure 1) and declared a state of emergency.1,3 Affected residents were instructed to boil their water prior to consumption through several modes of communication including the local media (e.g., radio, television, local papers), reverse 911 calls or texts, and highway signs.1,4 In some communities, emergency officials drove through neighborhoods using bullhorns and loudspeakers to inform residents.1,4 Within a week of the pipe break, a survey conducted in waiting rooms at Boston Medical Center revealed that the most common ways of learning about the boil water order were by word of mouth, television, and telephone/cellphone calls.5 By the early morning of May 4th, the boil water order had been lifted for all affected communities.1
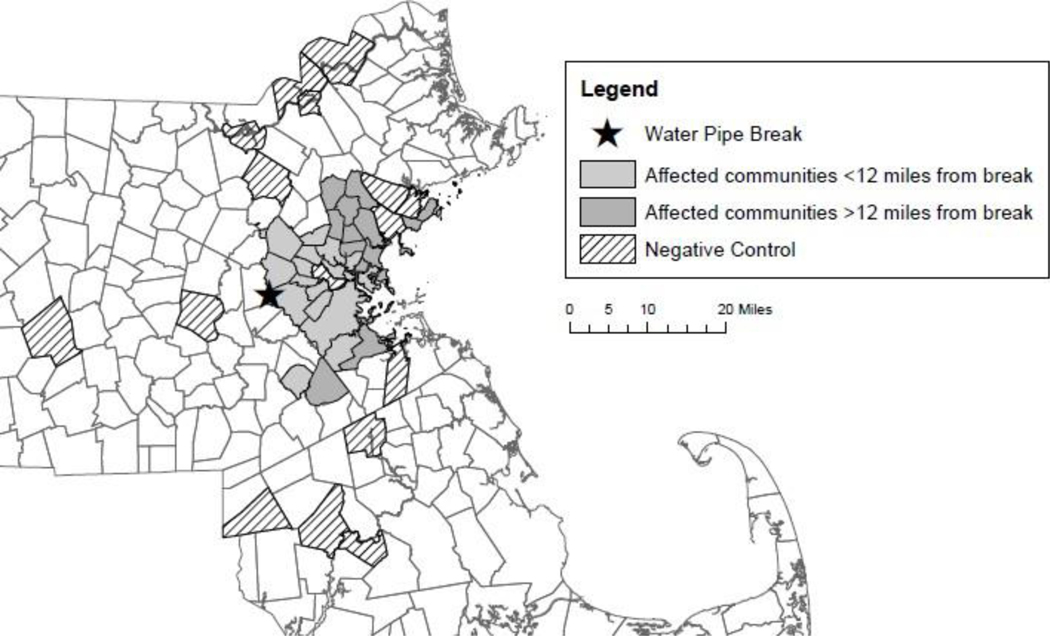
Figure 1.
Massachusetts communities studied in relation to the 2010 water pipe break.
Water pipe breaks are a public health concern because they can cause a rapid change in water pressure and allow contaminants from the surrounding environment to enter the distribution system through openings such as leakage points, submerged air valves, and faulty seals.6–10 Depending on the physical condition of the distribution network, abrupt changes in water pressure following a pipe break can lead to the intrusion of contaminants throughout the network, not just at the location of the pipe break.10 Fecal indicator bacteria and culturable human viruses have been detected in the soil and water external to drinking water pipelines, thus creating the potential for them to enter the water system during a negative pressure event.9,11 Intestinal parasites (e.g., Cryptosporidium, Giardia) have also been found in soil and could enter the water system.12,13
An estimated 240,000 water main breaks occur each year, wasting over two trillion gallons of treated drinking water.14 From 2012 to 2017, Folkman (2018) reported that overall main break rates increased by 27% in the United States and Canada.15 Regardless of factors such as pipe age, pipe material, weather (i.e., extreme cold, droughts), and soil types, main breaks are a concern in all types of water systems.15,16
Several studies have reported an association between tap water consumption in faulty distribution networks and gastrointestinal illness.17 In the United States, Shortridge et al. (2014) found an association between the number of pipe breaks and the internet search volume for symptoms of gastrointestinal illness.18 In the United Kingdom, Hunter et al. (2005) suggested that up to 15% of gastrointestinal illness in the general population could be related to drinking water contaminated by low water pressure events such as a burst water pipe.19 In Norway, Nygard et al. (2007) observed that reports of gastrointestinal illness increased during the week after the occurrence of main breaks or maintenance work on the water distribution system.20
Few epidemiology studies have explicitly studied how distribution failure events may contribute to the occurrence of waterborne illnesses.6 The major water pipe break near Boston in May 2010 provided an opportunity to study this using existing healthcare data. The aim of this analysis was to estimate the association between the pipe break and the risk for visiting the emergency department for acute gastrointestinal illness.
Methods
Study Population
Approximately two million residents living in 30 Boston metropolitan communities were affected by the boil water order and considered exposed to the water pipe break.1,2,4 Figure 1 highlights these communities, which included Arlington, Belmont, Boston, Brookline, Canton, Chelsea, Everett, Hanscom Air Force Base, Lexington, Lynnfield, Malden, Marblehead, Medford, Melrose, Milton, Nahant, Newton, Norwood, Quincy, Reading, Revere, Saugus, Somerville, Stoneham, Swampscott, Wakefield, Waltham, Watertown, Winchester, and Winthrop. These communities were located approximately 3 to 23 miles from the water pipe break.
Negative Control Exposure
In a separate analysis, communities unaffected by the pipe break and subsequent boil water order served as a negative control to assess whether acute gastrointestinal illness also increased at the time of the event.21 Communities receiving water unaffected by the pipe break were selected as a negative control exposure if they were 1) located in relatively close proximity (<40 miles) of the break and 2) had a Census population of at least 40,000 residents to ensure a sample size comparable to the truly exposed communities. These communities included Attleboro, Billerica, Brockton, Cambridge, Framingham, Haverhill, Lawrence, Lowell, Lynn, Methuen, Peabody, Salem, Taunton, Weymouth, and Worcester. Figure 1 highlights these 15 communities serving as negative controls. These communities were located approximately 7 to 31 miles away from the water pipe break.
Emergency Department Visits for Acute Gastrointestinal Illness
Acute gastrointestinal illness is often the most common recognizable health endpoint following infection with waterborne pathogens.22,23 Incubation periods can vary by type of pathogen – from less than a day for some viruses (e.g., norovirus) to a few days for some bacteria (e.g., Campylobacter).24,25 Some parasites (e.g., Cryptosporidium, Giardia) have a longer incubation period on average (~7 days), though it can range from a day to two weeks.26–28 These different types of pathogens often cause similar symptoms such as diarrhea, vomiting, nausea, and cramps.22,23 Acute gastrointestinal illness is also a convenient measure because it does not usually require any sample collection or analytical test.22 Acute gastrointestinal illness was defined using the primary and five associated diagnosis codes (International Classification of Disease, Version 9 Clinical Modification, ICD-9-CM). Several prior studies assessing drinking water quality and gastrointestinal illness have used ICD-9-CM codes.29–32 Building on what has been used in the literature, the following ICD-9-CM diagnosis codes were used to define acute gastrointestinal illness: 001–009.9 (intestinal infectious diseases); 558.9 (other and unspecified noninfectious gastroenteritis and colitis); 787.01 (nausea with vomiting); 787.03 (vomiting alone); and 787.91 (diarrhea).
Emergency department data, including hospital outpatient data, were obtained from the Commonwealth of Massachusetts Center for Health Information and Analysis for the year 2010. Emergency department data included visits to emergency departments in Massachusetts’ acute care hospitals and satellite emergency facilities. Hospital outpatient data included patients who received observation services but were not admitted to the hospital. Patients receiving observation services are usually transferred from the emergency department, though they are not included in the emergency department database to avoid duplicate reporting.33–35 Only 6% of the persons with acute gastrointestinal illness were diagnosed during hospital outpatient visits.
Massachusetts hospitals are required to file emergency department visit data for administrative purposes. These data do not contain any personally identifiable information and were therefore determined exempt from Institutional Review Board evaluation by the Office of Human Research Ethics at the University of North Carolina at Chapel Hill, as well as the U.S. Environmental Protection Agency’s Human Subjects Research Protocol Officer.
Pipe Break Exposure
Pipe break exposure was based on the community of residence reported at the emergency department visit. It was hypothesized that any emergency department visit for acute gastrointestinal illness caused by the water pipe break would occur within a week of the break. Despite the magnitude of the situation, the broken pipe was repaired in less than two days and the boil water order was lifted within 3 days.1 The one-week hazard period encompassed the time it would take for contaminated water to enter the distribution system and reach the consumer, the pathogen incubation period, and the time for an affected person to visit the emergency department. The hazard period was examined as two mutually exclusive intervals, which were defined a priori: 0–3 days and 4–7 days. The 0–3 day period encompassed the duration of the boil water order. The day of the water pipe break (day 0) was included because the water pipe break occurred in the morning and the boil water order was not issued until late in the afternoon.1 In addition, contamination may have occurred prior to the actual pipe break if there were any pressure fluctuations due to the pipe becoming compromised.10 The later 4–7-day hazard period accounted for a longer time lag from the pipe break to account for water distribution time, and resident exposure, infection, onset of acute gastrointestinal symptoms, and visiting the emergency department. The length of these hazard periods was optimal for capturing the effect of pathogens with an incubation period of no more than a few days.
Statistical Analysis
A case-crossover study design was used to examine the association between the major water pipe break and acute gastrointestinal illness. This type of study design, in which patients of interest effectively serve as their own control at different point(s) in time, was applicable because the water pipe break was a brief exposure with potentially transient effects on gastrointestinal illness.36,37 Specifically, the pipe break was fixed within two days and the onset of gastrointestinal illness, if any, was expected to be rapid and short-lived.1,22,36 Control times were selected bidirectionally, two weeks before and two weeks after the pipe break.38,39 By having patients with acute gastrointestinal illness essentially serve as their own control, the self-matching design eliminated confounding by individual characteristics that do not vary over a short time period, such as sex, race, and socioeconomic status.36,40 Selecting control times on the same day of week as the case time controlled for any confounding due to day of week.38 Also, the two week gap between case and control times ensured that exposure during the 0–3 and 4–7 day hazard periods was independent of exposure during the control period, thus preventing any autocorrelation between case and control periods.40 See eFigure 1, which illustrates how controls were selected and how exposure was assigned.
Conditional fixed-effects logistic regression models were used to estimate the risk of visiting the emergency department for acute gastrointestinal illness following the pipe break. This type of regression model is the standard for case-crossover studies.37 Only case-control groups with discordant exposures contribute information to the analysis; therefore, this analysis was confined to a 64-day period (April 3, 2010 through June 5, 2010) based on all possible discordant exposure scenarios.40 Results are reported as odds ratios (OR) and 95% confidence intervals (CI) and interpreted as the relative increase in odds of visiting the emergency department for acute gastrointestinal illness after the water pipe break.
The analysis was also stratified by potential effect modifiers. Age and sex were considered potential effect modifiers due to possible differences in immune status, risk for gastrointestinal illness, and drinking water intake.41–43 In addition, the analysis was stratified by the median distance (12 miles) from the pipe break to the centroid of each community in order to examine whether closer communities were impacted earlier, or more severely, than more distant communities. A sensitivity analysis in which acute gastrointestinal illness was defined based on only the primary diagnosis code was conducted to examine the robustness of results. Lastly, attributable fractions and population attributable fractions were calculated using a case-based approach described by Hanley.44 This approach uses the attributable fraction in the exposed (approximated by (OR-1)/OR because emergency department visits for acute gastrointestinal illness are rare) and the case fraction (number of exposed cases divided by the overall number of cases). Data management and statistical analyses were conducted using Stata SE Version 13 and the xtlogit command was used to fit the conditional logistic regression models.45
Results
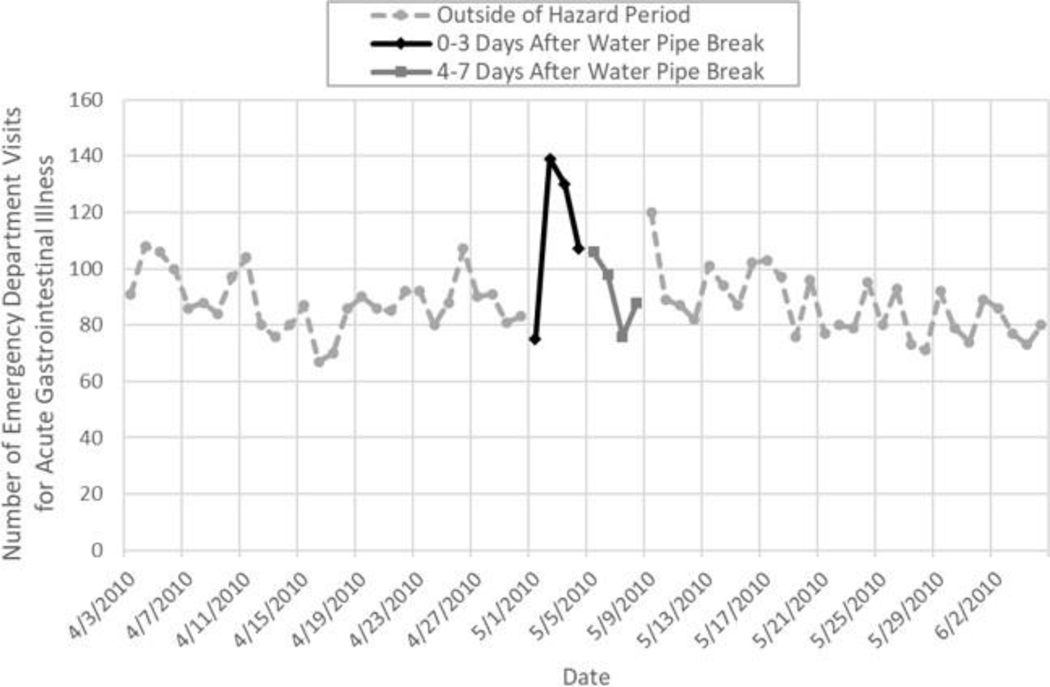
Among residents of the 30 communities affected by the water pipe break, there were 5,726 emergency department visits with at least one diagnosis code for acute gastrointestinal illness during the study period (April 3, 2010 through June 5, 2010). Over half (n=2,960; 52%) had a primary diagnosis of an acute gastrointestinal symptom. The majority (79%) of all visits were among adults (19–64 years) and young children (≤5 years) and there were slightly more females (n=3,410; 60%) than males. The most common diagnosis codes were for vomiting (n=3,652), followed by diarrhea (n=1,795), other and unspecified noninfectious gastroenteritis and colitis (n=1,005), and intestinal infectious diseases (n=381). Table 1 summarizes characteristics of emergency department visits for acute gastrointestinal illness in the communities affected by the pipe break; the table also reports the same characteristics in the communities selected as the negative control. Figure 2 depicts the total number of patients with acute gastrointestinal illness by day in the communities affected by the pipe break.
Table 1.
Descriptive summary of emergency department visits for acute gastrointestinal illness (April 3, 2010 - June 5, 2010).
| Communities affected by pipe break (n=30) | Communities serving as negative control exposure (n=15) | |||
|---|---|---|---|---|
|
|
||||
| N | % | N | % | |
| Total | 5,726 | 100% | 4,975 | 100% |
| Type of Visit Emergency Department |
5,373 | 94% | 4,674 | 94% |
| Hospital Outpatient* | 353 | 6% | 301 | 6% |
| Primary Diagnosis | 2,960 | 52% | 2,600 | 52% |
| Age Children (≤5 yrs) |
1,189 | 21% | 1,156 | 23% |
| Youth/Adolescents (6–18 yrs) | 674 | 12% | 689 | 14% |
| Adults (19–64 yrs) | 3,336 | 58% | 2,794 | 56% |
| Elderly (≥65 yrs) | 527 | 9% | 336 | 7% |
| Sex Female |
3,410 | 60% | 3,004 | 60% |
| Male | 2,316 | 40% | 1,971 | 40% |
| Race White |
2,881 | 50% | 2,420 | 49% |
| Black | 1,126 | 20% | 485 | 10% |
| Hispanic | 1,042 | 18% | 1,436 | 29% |
| Other | 565 | 10% | 579 | 12% |
| Missing | 112 | 2% | 55 | 1% |
Hospital outpatient visits included patients who received observation services but were not admitted to the hospital.
Figure 2.
Number of Emergency Department Visits for Acute Gastrointestinal Illness in 30 Boston Metropolitan Communities, April 3, 2010 - June 5, 2010.
There was a 1.25-fold increased odds for visiting the emergency department for acute gastrointestinal illness during the 0–3 days after the pipe break (OR=1.25; 95% CI: 1.11–1.41; Table 2). When day 0 was excluded, results were similar (OR=1.33; 95% CI: 1.18–1.49). This association was of a smaller magnitude during the 4–7 day hazard period (OR=1.09; 95% CI: 0.96–1.23). The associations were similar in males and females. When the analysis was restricted to visits with a primary diagnosis for acute gastrointestinal illness, the association remained similar as when using all diagnosis codes for both the 0–3 day hazard period (OR=1.29; 95% CI: 1.10–1.51) and the 4–7 day hazard period (OR=1.09; 95% CI: 0.91–1.30).
Table 2.
Association between the major water pipe break and emergency department visits for acute gastrointestinal illness in Boston metropolitan communities.
| Odds Ratio (95% Confidence Interval) |
|||
|---|---|---|---|
| Number of visits | 0–3 days after pipe break | 4–7 days after pipe break | |
| Acute Gastrointestinal Illness* | 5,726 | 1.25 | 1.09 |
| (1.11, 1.41) | (0.96, 1.23) | ||
| Among Young Children (≤5 years) | 1,189 | 1.31 | 0.96 |
| (1.02, 1.68) | (0.72, 1.27) | ||
| Among Youth/Adolescents (6–18 years) | 674 | 1.46 | 1.31 |
| (1.05, 2.02) | (0.90, 1.92) | ||
| Among Adults (19–64 years) | 3,336 | 1.27 | 1.04 |
| (1.09, 1.48) | (0.88, 1.23) | ||
| Among Elderly (≥65 years) | 527 | 0.76 | 1.47 |
| (0.49, 1.20) | (0.99, 2.16) | ||
| Among Females | 3,410 | 1.22 | 1.01 |
| (1.05, 1.43) | (0.86, 1.19) | ||
| Among Males | 2,316 | 1.29 | 1.21 |
| (1.08, 1.55) | (0.99, 1.47) | ||
| Among Residents Living <12 miles from the break | 4,212 | 1.32 | 0.98 |
| (1.15, 1.51) | (0.84, 1.14) | ||
| Among Residents Living >12 miles from the break | 1,514 | 1.07 | 1.39 |
| (0.84, 1.36) | (1.10, 1.75) | ||
| Any Primary Diagnosis for Acute Gastrointestinal Illness | 2,960 | 1.29 | 1.09 |
| (1.10, 1.51) | (0.91, 1.30) | ||
Primary and associated diagnoses
As shown in Table 2, the increased odds for visiting the emergency department during the 0–3 days after the water pipe break was consistent across all age groups except the elderly (≥65 years). The elderly, however, did have an elevated odds ratio during the 4–7 day hazard period (OR=1.47; 95% CI: 0.99–2.16). Similarly, the odds ratio among youth/adolescents (6–18 years) was elevated during the 4–7 day hazard periods (OR=1.31; 95% CI: 0.90–1.92). Due to fewer visits among these age groups, results were more imprecise for the elderly and youth/adolescents.
The communities less than the median distance (<12 miles) away from the water pipe break were at a 1.32-fold increased odds for visiting the emergency department for acute gastrointestinal illness during the 0–3 day hazard period (OR=1.32; 95% CI: 1.15–1.51) but not during the 4–7 day hazard period (OR=0.98; 95% CI: 0.84–1.14). To assess if this was due to disproportionate effects of Boston’s large population, a sensitivity analysis excluding Boston was conducted and the association remained (OR=1.38; 95% CI: 1.13–1.70). For the communities over 12 miles from the break, there was no association during the 0–3 day hazard period (OR=1.07; 95% CI: 0.84–1.36); however, there was an elevated odds ratio during the 4–7 day hazard period (OR=1.39; 95% CI: 1.10–1.75).
In a separate analysis using the negative control exposure, there was a 1.09-fold increased odds for visiting the emergency department for acute gastrointestinal illness during the 0–3 day hazard period (OR=1.09; 95% CI: 0.95–1.24). There was no association during the 4–7 day hazard period (OR=0.89; 95% CI: 0.77–1.03).
Based on the overall association (OR=1.25), the attributable fraction in the exposed was 20% ((1.25–1)/1.25=0.20), meaning almost a quarter of emergency department visits for acute gastrointestinal illness 0–3 days after the pipe break could be attributed to the break. Using the proportion of emergency department visits that occurred 0–3 days after the break (451/5,762=0.08), the population attributable fraction was approximately 2% (0.08*0.20=0.02).
Discussion
Water pipe break and acute gastrointestinal illness
The major water pipe break in May 2010 provided the opportunity to investigate the association between a water pipe break and emergency department visits for acute gastrointestinal illness. Citing a personal communication from July 2010 with the Massachusetts Department of Public Health (MA DPH), Wang et al. (2011) mentioned that the MA DPH did not observe a notable rise in disease reports after the break.5 The present study, however, found an increased risk for visiting the emergency department for gastrointestinal illness during the week after the pipe break. This association was strongest during the immediate 0–3 days after the break when the boil water order was in effect. Since emergency department visits for acute gastrointestinal illness are rare, the 20% attributable fraction during the 0–3 days after the pipe break amounts to only 90 excess cases of illness in the 30 affected communities (0.20*451=90). This increased risk was further supported by a negative control exposure yielding diminished or null effects.
Age did not appear to modify the risk of visiting the emergency department for acute gastrointestinal illness after the water pipe break. The most apparent differences were among the youth/adolescents (6–18 years) and elderly (≥65 years), which both yielded higher odds ratios during the 4–7 day hazard period. However, these age groups had fewer emergency department visits so results were more imprecise. Consequently, there was not enough evidence to make any meaningful conclusions regarding age modification.
When the analysis was stratified by distance from the water pipe break, the closer communities (i.e., those less than 12 miles away) were at an increased risk for visiting the emergency department for acute gastrointestinal illness during the 0–3 day hazard period (OR=1.32; 95% CI: 1.15–1.51). In the further communities (>12 miles away), there was no association during the 0–3 day hazard period; however, there was an increased risk during the 4–7 day hazard period (OR=1.39; 95% CI: 1.10–1.75).
This may demonstrate a delayed effect reflecting the additional time it takes distributed water to reach these areas.
This study may have underestimated the impact of the pipe break on the burden of acute gastrointestinal illness because emergency department visits only capture the most severe cases of illness requiring immediate medical attention. Since emergency department visits for acute gastrointestinal illness are rare to begin with, it is understandable that the state health department did not observe a substantial increase in reports of acute gastrointestinal illness after the break. Shortridge et al. (2014) provided support that distribution system disturbances may increase mild cases of gastrointestinal illness that do not necessitate a doctor’s visit.18 In Sweden, Tornevi et al. (2013) found an increase in nurse advice calls relating to gastrointestinal illness after precipitation upstream of a drinking water utility.46 Unfortunately, the administrative data used in this study lacks the information necessary to capture such mild cases of gastrointestinal illness. In addition, without routine cultures being performed, the non-specific definition of gastrointestinal illness may dilute associations due to etiologies unrelated to the pipe break. In order to theoretically increase specificity and reduce potential misclassification, gastrointestinal illness was also defined based on only the primary diagnosis code though results did not change (Table 2). Nevertheless, a small increase in risk could have a substantial public health impact, particularly when a large community is affected or among sensitive sub-groups.
This study adds to the existing literature on how disturbances in the drinking water system may play a role in disease transmission in the U.S. Aside from community-wide water emergencies, wet weather events (e.g., precipitation, flooding) have also been associated with increased gastrointestinal illness.17,31,32,47–50 In addition, water pipes can become vulnerable with aging infrastructures and extreme temperature fluctuations.16,51 Understanding the different risk factors involved can help water utilities and health departments establish and improve preparedness and response plans.
Although it is also possible that the boil water order and widespread media attention increased the rate of emergency department visits for psychosomatic illnesses, residents were explicitly told not to panic if they drank water before boiling and to call their doctor rather than visit the emergency room if they had any gastrointestinal symptoms.1 The Boston Mayor’s 24-hour hotline had a scripted response for concerned residents:
“Please do not go to an emergency room unless you are seriously ill and/or have been advised by your health care provider to seek immediate care. Please do not go to an emergency room to be checked out because you drank tap water and are concerned. There is no testing that can be done at emergency rooms for patients who are not in need of emergency care.”1
Water exposure after pipe break
A strength of this analysis was that the pipe break and subsequent boil order were clearly defined events that help determine exposure to potential water contamination. Estimating the association between drinking water contamination and risk of illness is difficult due to the many assumptions that have to be made.9,52 For example, a contamination event is contingent on a sequence of events, from the occurrence of an adverse pressure condition, to the presence of an outside contamination source, to the availability of an external pathway for contamination.9,52 In addition, population exposure depends on factors such as the type and concentration of pathogen entering the system and then reaching the consumers’ taps, the duration and magnitude of contamination, and the consumers’ drinking habits.9,52
While the pipe was being repaired, water pressure had to be maintained throughout the system in order to sustain sanitation needs (e.g., flushing toilets), to keep up with fire protection requirements, and to prevent contamination from backflow.1 As a result, the distribution system was reconfigured to use backup water supplies treated only with emergency chlorination.1 This meant that water was always available at the tap and uninformed or preoccupied residents could easily consume it without first boiling it. Furthermore, the boil water order focused on direct ingestion through eating and drinking.1 Exposure through other pathways was still possible, such as through bathing/showering. Despite aggressive efforts to inform the public about the boil water order, there would inevitably be residents who do not get the message in time.1,4 A survey conducted the week after the pipe break among a convenience sample (n=533) at Boston Medical Center found that 97% were aware of the order.5 However, the authors estimated that 34% of those who lived in affected communities were potentially exposed to contaminated water.5 Potential exposure was defined according to three criteria: 1) awareness of the order; 2) timing of receipt of the message; and 3) action taken upon receipt of the message.5
Due to the large number of water samples that needed to be tested (over 800 each day), only presence/absence tests were performed for the fecal indicator bacteria, total coliform and E. coli.1 The water authority claimed that, according to samples taken from throughout the affected area, the water quality was not atypical for a normal day at that time of year with only a few samples testing positive for total coliform and none testing positive for E. coli.1,53 However, due to the logistics of responding to the break, water samples were not collected on the day of the break.1 There are numerous potential pathogens in the environment and in untreated water that can contaminate drinking water supplies under conditions such as a distribution system failure.22,54 The association during the 0–3 day period after the break suggests that the pathogens involved had a short incubation period (e.g., enteric viruses). Since the backup water supplies were treated only with chlorine, parasites like cryptosporidium could be a concern since their outer shell can protect them from chlorine disinfection.26 Apart from the ineffectiveness of chlorine treatment for some parasites in the backup water supplies, those parasites may also be present in the soil surrounding the distribution pipes and could infiltrate the system when the pressure initially drops.12,13 Given that parasites generally have a longer incubation period (2–10 days), it is possible that the slightly elevated association during the 4–7 day hazard period (OR=1.09; 95% CI: 0.96–1.23) was driven by parasitic infections.26,28 Unfortunately, a limitation of the case-crossover study design is the inability to examine longer incubation periods and still control for seasonality.37,55
A limitation of this study is that exposure was based on community of residence even though people likely commute to other communities for work and other activities. This would result in some mixing and misclassification of exposure. However, since the pipe break occurred on a Saturday, fewer people would be commuting to work or school. In the survey study conducted within a week of the break, the majority (>75%) of potentially exposed respondents learned about the boil water order after dinner on Saturday or else on Sunday.5 Aside from not knowing the exact location of exposure, information on individual water consumption, such as bottled water use and in-home filter use, was unavailable.
Conclusion
This study provides evidence for an association between a recent major water pipe break and acute gastrointestinal illness in the United States. Understanding the health implications of water pipe breaks will help inform public health prevention and response plans. This is especially pertinent as drinking water systems age and the likelihood of pipe breaks increases.56,57
Supplementary Material
eFigure 1. Figure that illustrates how controls were selected and how exposure was assigned. [.pdf]
References
- 1.Stratus Consulting Inc. Multi-agency Response to a Major Water Pipe Break: A Massachusetts Case Study and Evaluation. Washington, DC: Association of Metropolitan Water Agencies, Water Research Foundation, WaterISAC, 2011. [Google Scholar]
- 2.Levenson M, Daley B. A ‘catastrophic’ rupture hits region’s water system. The Boston Globe. Boston, MA: Globe Newspaper Company, 2010. [Google Scholar]
- 3.Massachusetts Water Resources Authority. MWRA WATER MAIN BREAK REQUIRES BOIL WATER ORDER. Vol. 2017, 2010. [Google Scholar]
- 4.Henry D. Ruptured Pipe Cuts Water in Boston. The New York Times The New York Times Company, 2010. [Google Scholar]
- 5.Wang CJ, Little AA, Holliman JB, Ng CY, Barrero-Castillero A, Fu CM, Zuckerman B, Bauchner H. Communication of Urgent Public Health Messages to Urban Populations: Lessons From the Massachusetts Water Main Break. Disaster Medicine and Public Health Preparedness 2011;5(3):235–241. [DOI] [PubMed] [Google Scholar]
- 6.National Research Council (U.S.). Committee on Public Water Supply Distribution Systems: Assessing and Reducing Risks., National Academies Press (U.S.). Drinking water distribution systems assessing and reducing risks. Washington, D.C.: National Academies Press,, 2006;1 online resource (xii, 391 p.) ill. [Google Scholar]
- 7.Gullick RW, Lechevallier MW, Svindland RC, Friedman MJ. Occurrence of transient low and negative pressures in distribution systems. Journal American Water Works Association 2004;96(11):52–66. [Google Scholar]
- 8.Environmental Protection Agency US. Drinking water infrastructure needs survey and assessment : fifth report to Congress. In: Office of Water, Office of Ground Water and Drinking Water, Drinking Water Protection Division, eds. 2011 drinking water infrastructure needs survey and assessment. Washington, D.C.: U.S. Environmental Protection Agency, 2013. [Google Scholar]
- 9.LeChevallier MW, Gullick RW, Karim MR, Friedman M, Funk JE. The potential for health risks from intrusion of contaminants into the distribution system from pressure transients. J Water Health 2003;1(1):3–14. [PubMed] [Google Scholar]
- 10.Mora-Rodríguez J, Amparo López-Jiménez P, Ramos HM. Intrusion and leakage in drinking systems induced by pressure variation. Journal of Water Supply: Research and Technology - Aqua 2012;61(7):387. [Google Scholar]
- 11.Karim MR, Abbaszadegan M, Lechevallier M. Potential for pathogen intrusion during pressure transients. Journal / American Water Works Association 2003;95(5):134–146. [Google Scholar]
- 12.Dado D, Izquierdo F, Vera O, Montoya A, Mateo M, Fenoy S, Galvan AL, Garcia S, Garcia A, Aranguez E, Lopez L, del Aguila C, Miro G. Detection of zoonotic intestinal parasites in public parks of Spain. Potential epidemiological role of microsporidia. Zoonoses Public Health 2012;59(1):23–8. [DOI] [PubMed] [Google Scholar]
- 13.Hong S, Kim K, Yoon S, Park WY, Sim S, Yu JR. Detection of Cryptosporidium parvum in environmental soil and vegetables. J Korean Med Sci 2014;29(10):1367–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Society of Civil Engineers. 2017 Infrastructure Report Card for Drinking Water. 2017. [Google Scholar]
- 15.Folkman S. Water Main Break Rates in the USA and Canada: A Comprehensive Study. Utah State University, Buried Structures Laboratory, 2018;49. [Google Scholar]
- 16.Rajani B, Kleiner Y, Sink JE. Exploration of the relationship between water main breaks and temperature covariates. Urban Water Journal 2012;9(2):67–84. [Google Scholar]
- 17.Ercumen A, Gruber JS, Colford JM Jr., Water distribution system deficiencies and gastrointestinal illness: a systematic review and meta-analysis. Environ Health Perspect 2014;122(7):651–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shortridge JE, Guikema SD. Public health and pipe breaks in water distribution systems: analysis with internet search volume as a proxy. Water Res 2014;53:26–34. [DOI] [PubMed] [Google Scholar]
- 19.Hunter PR, Chalmers RM, Hughes S, Syed Q. Self-reported diarrhea in a control group: a strong association with reporting of low-pressure events in tap water. Clin Infect Dis 2005;40(4):e32–4. [DOI] [PubMed] [Google Scholar]
- 20.Nygard K, Wahl E, Krogh T, Tveit OA, Bohleng E, Tverdal A, Aavitsland P. Breaks and maintenance work in the water distribution systems and gastrointestinal illness: a cohort study. Int J Epidemiol 2007;36(4):873–80. [DOI] [PubMed] [Google Scholar]
- 21.Lipsitch M, Tchetgen Tchetgen E, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiology 2010;21(3):383–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Messner M, Shaw S, Regli S, Rotert K, Blank V, Soller J. An approach for developing a national estimate of waterborne disease due to drinking water and a national estimate model application. J Water Health 2006;4 Suppl 2:201–40. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. Guidelines for drinking-water quality. 4th ed. Geneva: World Health Organization, 2011. [Google Scholar]
- 24.Centers for Disease Control and Prevention. Norovirus. https://www.cdc.gov/norovirus/about/symptoms.html Accessed Oct. 3, 2017.
- 25.Centers for Disease Control and Prevention. Campylobacter (Campylobacteriosis). https://www.cdc.gov/campylobacter/faq.html Accessed Dec. 10, 2017.
- 26.Centers for Disease Control and Prevention. Parasites - Cryptosporidium: Infection – General Public. https://www.cdc.gov/parasites/crypto/gen_info/infect.html Accessed Dec. 10, 2017.
- 27.Centers for Disease Control and Prevention. Parasites - Giardia. https://www.cdc.gov/parasites/giardia/ Accessed Nov. 3, 2017.
- 28.Centers for Disease Control and Prevention. Giardiasis. https://www.cdc.gov/dpdx/giardiasis/index.html Accessed Jan. 3, 2018.
- 29.Schwartz J, Levin R, Goldstein R. Drinking water turbidity and gastrointestinal illness in the elderly of Philadelphia. J Epidemiol Community Health 2000;54(1):45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tinker SC, Moe CL, Klein M, Flanders WD, Uber J, Amirtharajah A, Singer P, Tolbert PE. Drinking water turbidity and emergency department visits for gastrointestinal illness in Atlanta, 1993– 2004. J Expo Sci Environ Epidemiol 2010;20(1):19–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang LY, Wang YC, Liu CM, Wu TN, Chou CH, Sung FC, Wu CC. Water outage increases the risk of gastroenteritis and eyes and skin diseases. BMC Public Health 2011;11:726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wade TJ, Lin CJ, Jagai JS, Hilborn ED. Flooding and Emergency Room Visits for Gastrointestinal Illness in Massachusetts: A Case-Crossover Study. PLoS ONE 2014;9(10):e110474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Downey C. EDTUs (emergency diagnostic and treatment units): last line of defense against costly inpatient stays. Manag Care 2001;10(4):44–6. [PubMed] [Google Scholar]
- 34.Massachusetts Division of Health Care Finance and Policy. Fiscal Year 2010 Outpatient Hospital Emergency Department Database Documentation Manual. 2011. [Google Scholar]
- 35.Massachusetts Division of Health Care Finance and Policy. Fiscal Year 2010 Outpatient Hospital Observation Database Documentation Manual. 2011. [Google Scholar]
- 36.Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 1991;133(2):144–53. [DOI] [PubMed] [Google Scholar]
- 37.Maclure M, Mittleman MA. Should we use a case-crossover design? Annu Rev Public Health 2000;21:193–221. [DOI] [PubMed] [Google Scholar]
- 38.Janes H, Sheppard L, Lumley T. Case-crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology 2005;16(6):717–26. [DOI] [PubMed] [Google Scholar]
- 39.Navidi W. Bidirectional case-crossover designs for exposures with time trends. Biometrics 1998;54(2):596–605. [PubMed] [Google Scholar]
- 40.Mittleman MA, Mostofsky E. Exchangeability in the case-crossover design. Int J Epidemiol 2014;43(5):1645–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Giefing-Kroll C, Berger P, Lepperdinger G, Grubeck-Loebenstein B. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell 2015;14(3):309–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sebastian RS, Enns CW, Goldman JD. Drinking Water Intake in the U.S. Food Surveys Research Group Dietary Data Brief, 2011;8. [Google Scholar]
- 43.Spellman FR. The handbook of environmental health [electronic resource]. Lanham, Md.: Scarecrow Press, Inc., 2013. [Google Scholar]
- 44.Hanley JA. A heuristic approach to the formulas for population attributable fraction. J Epidemiol Community Health 2001;55(7):508–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP, 2013. [Google Scholar]
- 46.Tornevi A, Axelsson G, Forsberg B. Association between precipitation upstream of a drinking water utility and nurse advice calls relating to acute gastrointestinal illnesses. PLoS One 2013;8(7):e69918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gargano JW, Freeland AL, Morrison MA, Stevens K, Zajac L, Wolkon A, Hightower A, Miller MD, Brunkard JM. Acute gastrointestinal illness following a prolonged community-wide water emergency. Epidemiol Infect 2015;143(13):2766–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Drayna P, McLellan SL, Simpson P, Li SH, Gorelick MH. Association between rainfall and pediatric emergency department visits for acute gastrointestinal illness. Environ Health Perspect 2010;118(10):1439–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jagai JS, Li Q, Wang S, Messier KP, Wade TJ, Hilborn ED. Extreme Precipitation and Emergency Room Visits for Gastrointestinal Illness in Areas with and without Combined Sewer Systems: An Analysis of Massachusetts Data, 2003–2007. Environ Health Perspect 2015;123(9):873–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tornevi A, Barregard L, Forsberg B. Precipitation and primary health care visits for gastrointestinal illness in Gothenburg, Sweden. PLoS One 2015;10(5):e0128487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morris RE. Principal Causes and Remedies of Water Main Breaks. Journal (American Water Works Association) 1967;59(7):782–798. [Google Scholar]
- 52.Besner MC, Prevost M, Regli S. Assessing the public health risk of microbial intrusion events in distribution systems: conceptual model, available data, and challenges. Water Res 2011;45(3):961–79. [DOI] [PubMed] [Google Scholar]
- 53.Daley B, Gil G. Tests confirm it — water was OK to drink all weekend. The Boston Globe. Boston: Globe Newspaper Company., 2010. [Google Scholar]
- 54.Reynolds KA, Mena KD, Gerba CP. Risk of waterborne illness via drinking water in the United States. Rev Environ Contam Toxicol 2008;192:117–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bateson TF, Schwartz J. Control for seasonal variation and time trend in case-crossover studies of acute effects of environmental exposures. Epidemiology 1999;10(5):539–44. [PubMed] [Google Scholar]
- 56.U.S. Environmental Protection Agency. Drinking Water Distribution Systems. https://www.epa.gov/dwsixyearreview/drinking-water-distribution-systems Accessed Oct. 25, 2016.
- 57.Olson E. WHAT’S ON TAP? Grading Drinking Water in U.S. Cities. 2003. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Figure that illustrates how controls were selected and how exposure was assigned. [.pdf]