Abstract
BACKGROUND:
Despite the known mental health burden among children with congenital heart disease (CHD), the literature is constrained by a lack of comparison cohorts and population-based follow-up data. We examined the incidence of mental health conditions among children with CHD, relative to 3 comparison cohorts.
METHODS:
This population-based cohort study identified all children with CHD (<18 years of age; n=16 473) in Denmark from 1996 to 2017, through linkage of individual-level data across national registries. This allowed for complete follow-up of the population. Comparison cohorts included children from the general population (n=162 204), siblings of children with CHD (n=20 079), and children with non-CHD major congenital anomalies (n=47 799). Mental health conditions were identified using inpatient and outpatient hospital discharge codes, prescription data, and data on use of community-based psychology, psychiatry, and psychotherapy services. We computed cumulative incidence by 18 years of age, incidence rates, and adjusted hazard ratios (aHRs) using Cox regression. aHRs accounted for sex, year of CHD diagnosis, parental mental health, and socioeconomic status. All estimates were stratified by age, sex, and CHD complexity.
RESULTS:
The cumulative incidence of mental health conditions by 18 years of age in the CHD cohort was 35.1% (95% CI, 34.0%–36.1%), corresponding to aHRs of 1.64 (95% CI, 1.58–1.71), 1.41 (95% CI, 1.30–1.52), and 1.02 (95% CI, 0.98–1.07) compared with the general population, sibling, and major congenital anomaly cohorts, respectively. Mental health incidence rates showed prominent peaks in early childhood and adolescence. Males and children with severe or single-ventricle CHD demonstrated higher incidence rates of mental health conditions relative to females and children with mild or moderate CHD, respectively. Compared with the general population and sibling cohorts, incidence rates and aHRs in the CHD cohort were highest for severe stress reactions, attention deficit/hyperactivity disorder, intellectual disability, and autism spectrum disorder. Compared with children in the major congenital anomaly cohort, the aHRs were close to 1.
CONCLUSIONS:
More than one-third of children with CHD were diagnosed or treated for a mental health condition by 18 years of age. Mental health conditions began early in life and were most prominent among males and children with severe or single-ventricle heart disease.
Keywords: cardiology, congenital heart defects, epidemiology, mental health, neurodevelopmental disorders
Clinical Perspective.
What Is New?
In this national longitudinal cohort study of the Danish population spanning 22 years of follow-up, 35.1% of children with congenital heart disease (CHD) were diagnosed with or treated for a mental health condition by 18 years of age.
Incidence of mental health conditions in children with CHD was bimodal, with peaks in early childhood and adolescence, and highest in males and children with severe or single-ventricle CHD relative to females and children with mild or moderate CHD.
Relative to the general population and sibling cohorts, children with CHD were at increased risk of mental health conditions, most notably severe stress and neurodevelopmental disorders, including attention-deficit/hyperactivity disorder, intellectual disability, and autism spectrum disorder.
What Are the Clinical Implications?
In one of the most comprehensive assessments of mental health risk in the CHD literature, our findings stress the importance of prevention, early identification, and intervention approaches for neurodevelopmental and mental health conditions as part of congenital cardiac care.
In nations with certain notable differences from Denmark (eg, larger populations of children with severe and single-ventricle CHD and reduced health care equity and access), these findings may underestimate the burden of mental health conditions in children with CHD.
More than 12 million individuals worldwide live with congenital heart disease (CHD).1 Many important complications and comorbidities, including neurodevelopmental and mental health conditions, are now recognized in this growing patient population.2,3 Children and adults with CHD have higher rates of mental health conditions than those reported for the general population.4–8 Among adults with CHD, the lifetime risk of depression and anxiety is approximately 50%, and these conditions are associated with greater health care use and adverse outcomes, including poorer quality of life and greater morbidity and mortality.9–12 Studies including children with CHD (<18 years of age) are limited, but in the general pediatric population, mental health conditions are associated with poorer physical, educational, and social outcomes in childhood,13–15 as well as poorer mental health outcomes in adulthood.16
The need to better understand the incidence of mental health conditions in the pediatric CHD population has become a call to action within the congenital cardiac community.2,17 Limitations of existing research include small samples, lack of longitudinal data and relevant comparison cohorts, and the narrow scope of mental health outcomes examined.2 Use of national population-based registry data can address some of these shortcomings. Denmark registries allow for analysis of a wide spectrum of mental health conditions and relevant risk factors among individuals with CHD, as well as direct comparison of estimates with relevant cohorts, including children in the general population, siblings of children with CHD, and children with non-CHD major congenital anomalies (MCAs). Such comparison cohorts allow a better understanding of estimates of mental health conditions in children with CHD relative to their peers, as well as detection of potential influences of chronic medical illness and family-related factors (eg, parental mental health, genetic and socioeconomic factors).
In this context, we present the first in a series of studies describing the burden of mental health conditions among children with CHD based on Danish national health registry data. In the current population-based cohort study, we aimed to: (1) examine the incidence of mental health conditions and specific hospital-based mental health diagnoses in children with CHD; (2) identify age-, sex-, and CHD severity-based differences in the incidence of mental health conditions in this population; and (3) contextualize these findings by comparison with children in the general population, siblings of children with CHD, and non-CHD MCA cohorts.
METHODS
Study Setting and Population
Denmark has a tax-funded public health care system that ensures free access to health care for all residents.18,19 A personal identification number is assigned to each resident, making it possible to link individual-level data across numerous health, social, and financial registries.18 This facilitates continuous and virtually complete prospective follow-up of the national population. This study was reported to the Danish Data Protection Agency (2016-051-000001-605) by Aarhus University and, as per Danish law, informed consent was waived. The data set is available upon application to the Danish health authorities and is not available to the public.
In this study, children in the CHD and comparison cohorts were identified by the Danish Civil Registration System19 and the Danish National Patient Registry (covering all Danish hospitals.20 The Civil Registration System contains demographic (ie, sex and parental identity) and vital status information. The Danish National Patient Registry contains hospital admission and discharge, procedure, and diagnostic codes from inpatient hospital admissions (1977 to present) and outpatient hospital clinic and emergency room contacts (1995 to present). Discharge diagnoses have been coded according to the International Classification of Diseases, Tenth Revision (ICD-10), since 1994.
Children With CHD
The CHD cohort included children <18 years of age diagnosed with CHD ICD-10 codes Q20–Q26) between January 1996 and December 2017. Children were excluded if a mental health condition was identified before CHD diagnosis or if the CHD was a patent ductus arteriosus associated with prematurity (<37 weeks of gestation), as recorded in the Danish Medical Birth Registry.8,19 CHD complexity was categorized into 5 groups:21,22 (1) mild CHD, defined as all simple congenital heart anomalies not requiring intervention in the first year of life; (2) moderate CHD, defined as simple biventricular malformations requiring surgical or catheter-based intervention (eg, atrial septal defects, ventricular septal defects, coarctation of the aorta); (3) severe CHD, defined as significantly malformed but biventricular heart anomalies requiring surgery in the first year of life (eg, tetralogy of Fallot, transposition of the great arteries, and atrioventricular canal defects); (4) single-ventricle CHD (eg, hypoplastic left heart syndrome); and (5) other (eg, unspecified malformations of cardiac chambers, septa, or valves; Table S1). The index date was defined as the date of CHD diagnosis. CHD complexity was categorized as mild/moderate and severe/single-ventricle CHD to reduce the risk of misclassification of complexity stemming from miscoding or categorization based on timing of interventions.
Comparison Cohorts
Members of the general population cohort were individually matched 10:1 to patients with CHD by calendar year, age, and sex. Follow-up for children in the general population cohort began at the same age as their matched patient with CHD. The sibling cohort included all siblings of children with CHD. Siblings were identified through the Civil Registration System and defined as all additional children born to the mother of the child with CHD.23 Follow-up of siblings already born began on the index date of their matched sibling with CHD, and follow-up of siblings not yet born began on their birth dates. For all analyses related to the sibling comparison cohort, a subcohort was created that included only members of the CHD cohort with siblings. The MCA cohort included children with non-CHD MCAs, as defined by the EUROCAT (European Concerted Action on Congenital Anomalies and Twins) categorization of congenital anomalies (eg, genetic anomalies, neural tube defects, and cleft palate; Table S2).24,25 Patients in the MCA cohort were individually matched 3:1 to patients with CHD based on calendar year, age on the index date, and sex. Follow-up began on the MCA index date, defined as the date of MCA diagnosis. Children in the comparison cohorts were excluded if they had a mental health condition before their index date or if their matched CHD subject was excluded.
Mental Health Conditions
The Danish Psychiatric Central Research Register records data from all psychiatric hospital admissions (1969 to present), outpatient hospital-associated psychiatric clinics (1995 to present), and emergency department visits (1995 to present).26 Diagnostic codes from primary care providers, psychiatrists in private practice, and psychologists are not collected in the register. To identify cases managed outside of the inpatient setting and outpatient hospital clinics, we used prescription and psychotherapy code data. The Danish National Prescription Registry collects data on all prescription drugs dispensed in Danish community pharmacies (1994 to present).27 The National Health Insurance Service Registry collects data on numerous services, such as psychotherapy services rendered by any provider, including primary care practitioners, community-based psychologists, and community-based psychiatrists who are supported by the health insurance system (1990 to present for adult services and 1996 to present for pediatric services).
As we aimed to sensitively estimate the mental health burden and specific mental health diagnoses, we broadly defined mental health condition as a composite variable based on: (1) ICD codes for specific hospital-based mental health diagnoses; (2) prescriptions for psychotropic medications; and (3) use of community-based psychology, psychiatry, and psychotherapy services.
Specific hospital-based mental health diagnoses were grouped into 11 categories, incorporating 10 categories from previously published approaches and an 11th category capturing self-harm and suicidality.25,28,29 We used the World Health Organization Anatomical Therapeutic Chemical code system to identify relevant psychotropic medications (Table S2).30 Because a single medication can be used for different conditions, medications were not mapped to specific diagnoses. Finally, we identified all mental health–related encounters using specific health insurance codes associated with a primary care (or general) practitioner visit for mental health concerns, psychotherapy encounters with a psychologist, and any visit to a psychiatrist (Table S2).
The date of mental health condition onset was considered the first contact with a hospital-based provider associated with a relevant ICD code, redemption of a relevant medication prescription, or a psychology, psychiatry, or psychotherapy visit associated with a relevant health insurance code.
Covariates
We evaluated 4 main categories of potential factors associated with mental health diagnoses: (1) child demographic characteristics; (2) child clinical history; (3) parent socioeconomic status; and (4) parent health history. Demographic characteristics included age on the index date (<1 year, 1 to <5 years, and ≥5 years), sex, and immigration status (Danish citizen versus immigrant). Clinical risk factors included CHD complexity, gestational age and weight at birth (further categorized as small for gestational age, defined as <10th percentile for infants of the same gestational age, sex, and birth year), and diagnosis of a non-CHD major congenital anomaly or genetic syndrome before or within the first year after CHD diagnosis (Table S2). To estimate the potential effect of early exposures on the incidence of mental health conditions and to clearly define the mild CHD subcohort, we analyzed the number of surgeries and catheterizations, length of index hospitalization (defined as the first hospitalization associated with CHD or MCA diagnosis), total number of hospitalizations, and cumulative hospitalization duration in the first year after CHD diagnosis. Admissions were only included for children who were in the hospital on day 5 of life or later, up to the first year after CHD diagnosis. Parental factors included maternal marital status and residence (rural versus urban), age, educational level, income, and employment status of both parents. Data on income and employment status were obtained from the Integrated Database for Labor Market Research, and data on the highest level of education completed were obtained from the Educational Attainment Register.31 Parental income was analyzed for mothers and fathers separately. The parental income earned in the year before the index date was adjusted for inflation to an equivalent 2015 income and then categorized into quartiles based on the distribution of income among individuals of the same age and sex in 2015. A composite socioeconomic status score was created using a previously published methodology.32 Parental health history was evaluated at the time of the index date using Danish National Patient Registry data, including hospital-based mental health diagnoses, substance use disorders, and Charlson Comorbidity Index scores.21 Additional covariates were collected and will be reported elsewhere.
Statistical Analysis
We followed members of the study cohorts from their index dates until an outcome of interest, 18 years of age, emigration, death, or end of follow-up (December 31, 2018). We computed incidence rates (incident cases per 1000 person-years) and cumulative incidence (%) by age 18 years of mental health conditions and specific mental health diagnoses, treating death as a competing event. To account for differences in outcomes by age, we used age as a time scale and divided the follow-up periods into successive age groups (0 to <1 years, 1 to <3 years, 3 to <5 years, 5 to <10 years, and 10 to <18 years). For example, a child diagnosed with CHD at birth and followed for 11 years was included in all 5 age groups, whereas a child diagnosed with CHD at 4 years of age and followed for 2 years was included in the 3- to <5-year and 5- to <10-year age groups.
We used Cox proportional hazard regression stratified on matched pairs to compute crude and adjusted hazard ratios (aHRs). The proportional hazards assumption was checked by log-minus-log plots and was found to be satisfied. The CHD versus general population and the CHD versus MCA comparison cohort analyses were adjusted by design for sex and year of CHD diagnosis as a result of matching and further adjusted for immigration status, maternal marital status, maternal residence, maternal composite socioeconomic status score, parental mental health history, and parental chronic illnesses based on Charlson Comorbidity Index scores. The CHD versus sibling comparison cohort analysis was adjusted for sex and calendar year. Patients with missing data for a covariate were excluded from the Cox regression, but given the nature of this data set, this affected only a minimal number of cases. Incidence rates and aHRs were stratified by age groups, sex, and CHD complexity. Sex and CHD complexity subgroups were further stratified by age groups to examine age-based subgroup differences. In the age group–stratified aHR computations, follow-up was left-truncated at the age of entry and censored at the age of last known follow-up or end of the age group period.
All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC). We support interpretation of point estimates and CIs without reliance on statistical tests and thus do not report P values.33 One author (D.K.F.) had full access to all study data and takes responsibility for its integrity and analysis. This article conforms to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for observational studies.
RESULTS
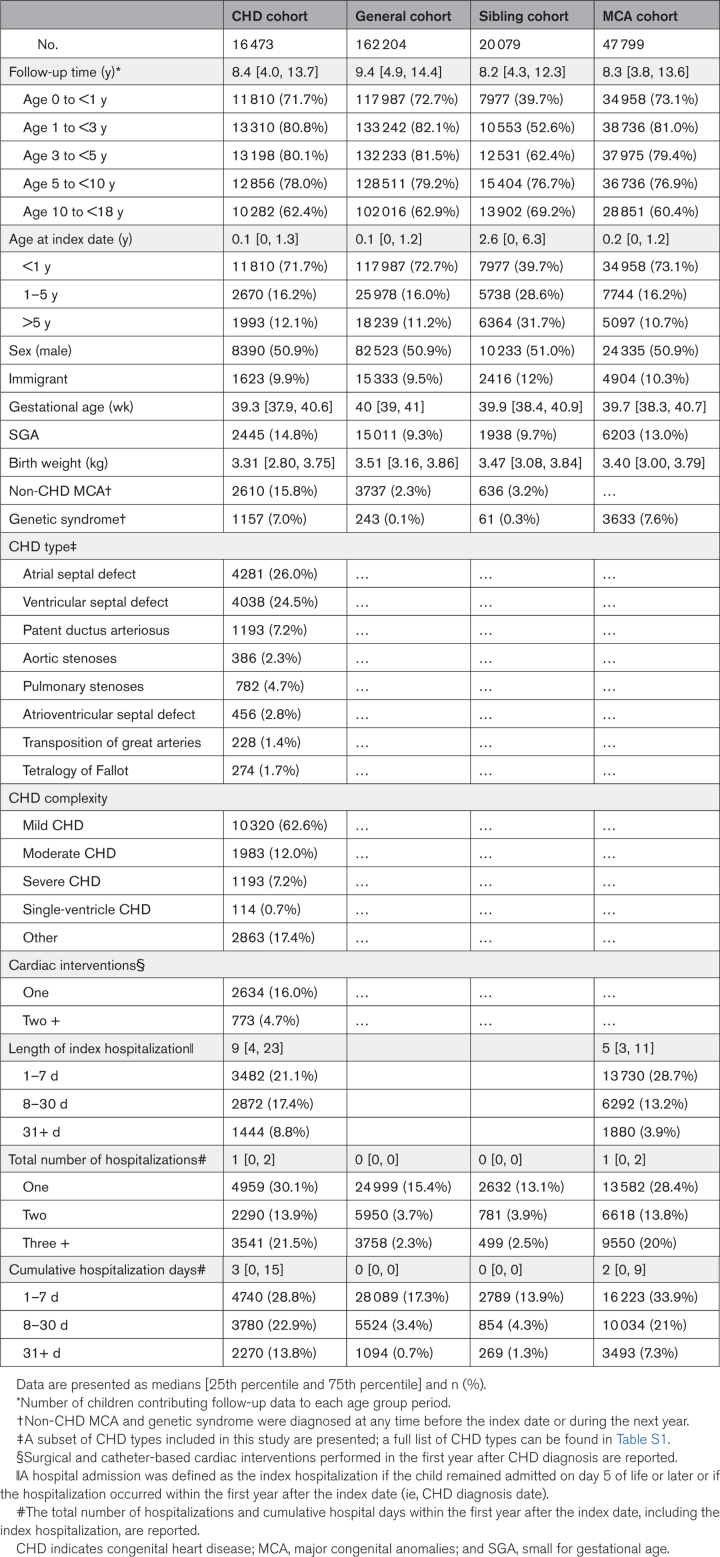
We identified 17 114 children diagnosed with CHD by 18 years of age. Of these, 641 (3.7%) were excluded due to history of a mental health condition (composite score) before the index date. Thus, the final CHD cohort included 16 473 children with a median follow-up of 8.4 years (25th percentile [Q1], 75th percentile [Q3]: 4.0, 13.7 years]. The matched comparison cohorts included 162 204 children from the general population (median follow-up = 9.4 years [Q1, Q3: 4.9, 14.4 years]) after exclusion of 3060 (1.8%) children; 20 079 siblings of children with CHD (median follow-up = 8.2 years [Q1, Q3: 4.3, 12.3 years]) after exclusion of 891 (4.1%) children; and 47 799 children with non-CHD MCAs (median follow-up = 8.3 years [Q1, Q3: 3.8, 13.6 years]) after exclusion of 1820 (3.5%) children. Within both the CHD and comparison cohorts, <3.5% died or were lost to follow-up due to emigration during the study period (Figure S1).
CHD Cohort Characteristics
CHD was diagnosed in most subjects within the first year of life (71.7%; median age at diagnosis = 0.1 years [Q1, Q3: 0, 1.3 years]), with slight male predominance (50.9%; Table 1). The CHD cohort had the lowest gestational age (median, 39.3 weeks [Q1, Q3: 37.9, 40.6 weeks]) and lowest weight at birth (3.31 kg [Q1, Q3: 2.80, 3.75 kg]), with the highest prevalence of small for gestational age at birth (14.8%) relative to all 3 comparison cohorts. Within the CHD cohort, 74.6% of children had mild or moderate CHD, and 7.9% had severe or single-ventricle CHD. Non-CHD MCAs were present in 2610 (15.8%) children with CHD, including 1157 (7.0%) children with a genetic syndrome. Within the first year after CHD diagnosis, 3407 children (20.7%) underwent cardiac surgery or catheterization, and 10 790 (65.5%) were hospitalized. For those hospitalized within the first year after CHD diagnosis, median index hospitalization duration was 9 days (Q1, Q3: 4, 23 days), with a cumulative hospitalization duration of 10 days (Q1, Q3: 3, 25 days). Cox regression analyses adjusted for parental socioeconomic status, mental health conditions, and Charlson Comorbidity Index (Table S3).
Table 1.
Characteristics of the CHD, General Population, Sibling, and Non-CHD Major Congenital Anomaly Cohorts, Denmark, 1996 to 2017
Mental Health Conditions
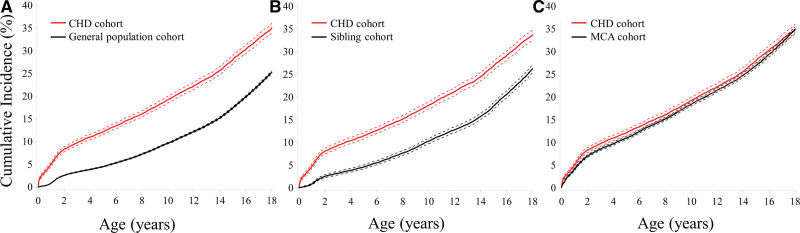
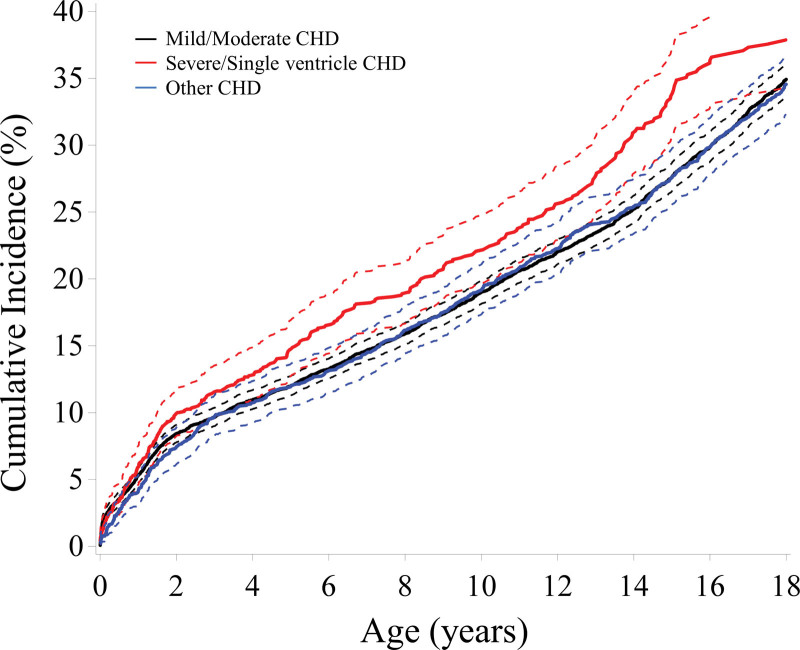
A total of 3316 children with CHD, 21 398 children from the general population, 2646 children in the sibling cohort, and 9913 children in the MCA cohort had a mental health condition (54.0% were detected by ICD code, 27.9% by prescription code, and 18.1% by first contact for community-based psychology, psychiatry, or psychotherapy services). The cumulative incidence of mental health conditions by 18 years of age in the CHD cohort was 35.1% (95% CI, 34.0%–36.1%) compared with 25.3% (95% CI, 25.0%–25.6%) in the general population cohort, 26.2% (95% CI, 25.4%–27.1%) in the sibling cohort, and 34.9% (95% CI, 34.2%–35.5%) in the MCA cohort (Figure 1). aHRs were 1.64 (95% CI, 1.58–1.71), 1.41 (95% CI, 1.30–1.52), and 1.02 (95% CI, 0.98–1.07) when the CHD cohort was compared with the general population, sibling, and MCA cohorts, respectively (Table 2). These associations remained consistent across age group–stratified comparisons.
Figure 1.
Cumulative incidence of mental health conditions in the CHD cohort relative to the comparison cohorts. The cumulative incidence of mental health conditions by 18 years of age in the CHD cohort exceeded that in the general population cohort (A) and sibling cohort (B) but was similar to that in the non-CHD MCA cohort (C). Mental health conditions were defined as a composite outcome of a first medical contact yielding an associated International Classification of Diseases, Tenth Revision (ICD-10) diagnosis, prescription of a psychotropic medication, or provision of psychotherapy. The solid line represents the point estimate, and the dashed lines represent 95% CIs. CHD indicates congenital heart disease; and MCA, major congenital anomaly.
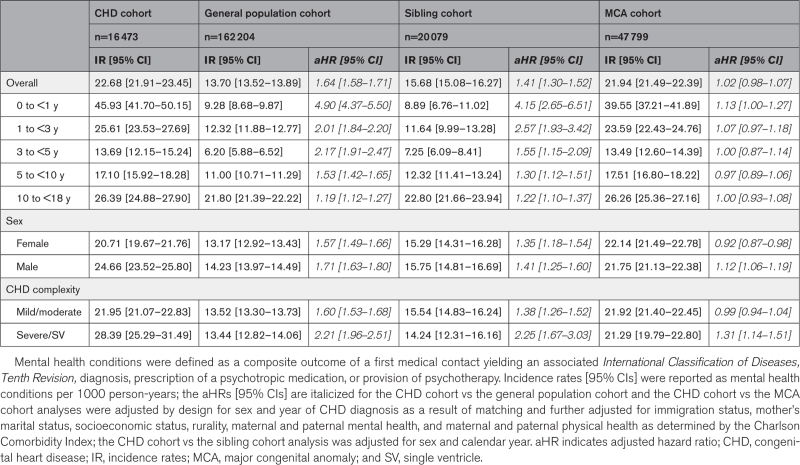
Table 2.
Incidence Rates and aHRs of Mental Health Conditions by Cohort, Stratified by Age Group, Sex, and CHD Complexity
We observed a bimodal pattern of mental health condition incidence rates by age group, with the highest incidence in children with CHD between the ages of 0 and 1 year (45.93 per 1000 person-years [95% CI, 41.70–50.15 per 1000 person-years]) and 10 to 18 years (26.39 per 1000 person-years [95% CI, 24.88–27.90 per 1000 person-years]). Compared with the general population and sibling comparison cohorts, in the CHD cohort, aHRs for mental health conditions were highest in infancy and early childhood (Table 2). In adolescence, the aHRs of mental health conditions in the CHD cohort were higher, but more closely approximated, than those for the general population (aHR, 1.19 [95% CI, 1.12–1.27]) and sibling (aHR, 1.22 [95% CI, 1.10–1.37]) cohorts (Table 2; Figure S2). When we compared the CHD and MCA cohorts, the incidence rates were similar, and aHRs were close to 1 (Table 2).
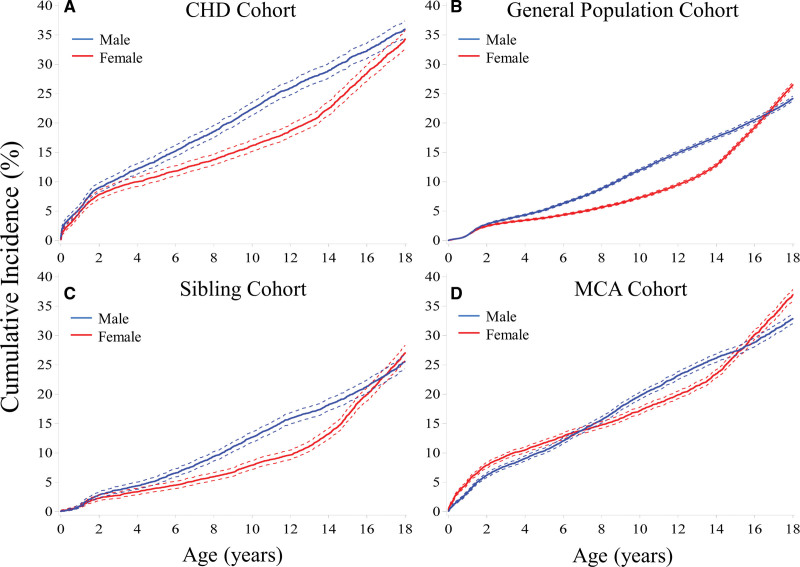
Differences by Sex
The cumulative incidence of mental health conditions by 18 years of age in males with CHD exceeded that of females with CHD (36.0% [95% CI, 34.6%–37.4%] versus 34.3% [95% CI, 32.8%–35.8%]; Figure 2). Across age groups, males had higher incidence rates of mental health conditions than females, except for the adolescent age group (females = 28.38 per 1000 person-years [95% CI, 26.18–30.57 per 1000 person-years] versus males = 24.31 per 1000 person-years [95% CI, 22.24–26.38 per 1000 person-years]; Table S4; Figure S3). Compared with the general population and sibling cohorts, males with CHD had higher aHRs for mental health conditions than females with CHD (Table 2). These associations remained consistent in age group–stratified comparisons (Table S4).
Figure 2.
Cumulative incidence of mental health conditions in the CHD cohort relative to the comparison cohorts, stratified by sex. The cumulative incidence of mental health conditions in males (blue) generally exceeded that in females (red) in all cohorts (A-D), except in adolescence. Mental health conditions were defined as a composite outcome of a first medical contact yielding an associated International Classification of Diseases, Tenth Revision (ICD-10) diagnosis, prescription of a psychotropic medication, or provision of psychotherapy. The solid line represents the point estimate, and the dashed lines represent 95% CIs. CHD indicates congenital heart disease; and MCA, major congenital anomaly.
Differences by CHD Complexity
The cumulative incidence of mental health conditions by 18 years of age in children with severe or single-ventricle CHD exceeded that in children with mild or moderate CHD (37.9% [95% CI, 34.3%–41.4%] versus 34.9% [95% CI, 33.7%–36.2%]; Figure 3). Correspondingly, the aHRs were highest among children with severe or single-ventricle CHD compared with the general population (aHR, 2.21 [95% CI, 1.96–2.51]) and sibling cohorts (aHR, 2.25 [95% CI, 1.67–3.03]; Table 2). aHRs among children with mild or moderate CHD remained notable, with a 60% increased hazard of mental health conditions compared with the general population cohort (aHR, 1.60 [95% CI, 1.53–1.68]) and a 38% increased hazard compared with the sibling cohort (aHR, 1.38 [95% CI, 1.26–1.52]). These associations remained consistent in age group–stratified comparisons (Table S4).
Figure 3.
Cumulative incidence of mental health conditions in the CHD cohort, stratified by CHD complexity. The cumulative incidence of mental health conditions in children with severe or single-ventricle CHD (red) exceeded that in children with mild or moderate CHD and in children with “other” CHD. Children with “other” CHD demonstrated a similar cumulative incidence pattern as children with mild or moderate CHD. Mental health conditions were defined as a composite outcome of a first medical encounter yielding an associated International Classification of Diseases, Tenth Revision (ICD-10) diagnosis, prescription of a psychotropic medication, or provision of psychotherapy. The solid line represents the point estimate, and dashed lines represent 95% CIs. CHD indicates congenital heart disease.
Hospital-Based Mental Health Diagnoses
The cumulative incidence of hospital-based mental health diagnoses by 18 years of age in the CHD cohort was 24.0% (95% CI, 23.0%–24.9%) compared with 15.2% (95% CI, 14.9%–15.4%), 16.5% (95% CI, 15.8%–17.2%), and 23.2% (95% CI, 22.6%–23.7%) in the general population, sibling, and MCA cohorts, respectively. When we stratified the analyses by age group, sex, and CHD severity, the overall mental health diagnosis burden both within the CHD cohort and relative to the comparison cohorts was the same as that found in the composite mental health analyses (Table S5).
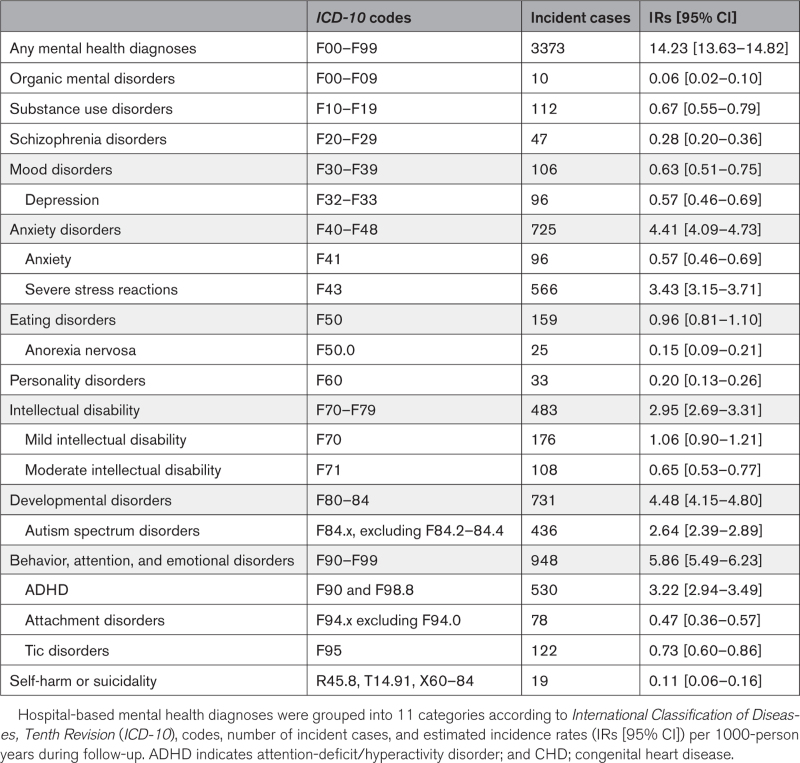
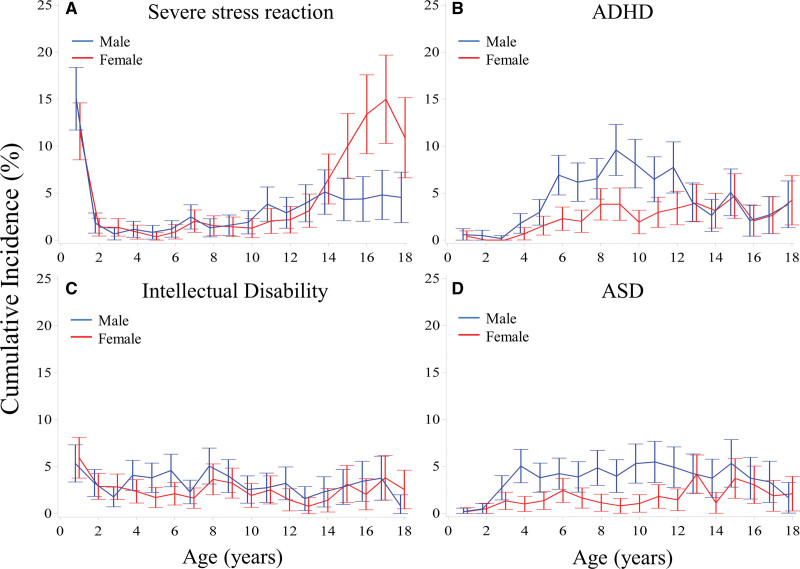
Within the CHD cohort, hospital-based mental health diagnoses with the highest incidence rates were severe stress reaction (3.43 per 1000 person-years [95% CI, 3.15–3.71 per 1000 person-years]), attention-deficit/hyperactivity disorder (ADHD; 3.22 per 1000 person-years [95% CI, 2.94–3.49 per 1000 person-years]), intellectual disability (2.95 per 1000 person-years [95% CI, 2.69–3.31 per 1000 person-years]), and autism spectrum disorder (ASD; 2.64 per 1000 person-years [95% CI, 2.39–2.89 per 1000 person-years]; Table 3; Figure 4A through 4D). Incidence rates of ADHD and ASD were most prominent in males, starting from 6 to 12 years of age, followed by a slow decline in incidence rates in adolescence. In contrast, females demonstrated a higher incidence of anxiety and mood disorders, especially during adolescence (Figure S4). Most anxiety disorders (77.8%) were related to severe stress reactions in a bimodal pattern, with peaks in early childhood and in adolescence (Figure 4A).
Table 3.
Incidence of Hospital-Based Mental Health Diagnoses in the CHD Cohort
Figure 4.
Incidence rates of the four highest incident hospital-based mental health diagnoses in the CHD cohort, stratified by sex. Incidence rates and 95% CIs for females (red) and males (blue) are graphed in 1-year intervals of age. ADHD indicates attention deficit/hyperactivity disorder; ASD, autism spectrum disorder; and CHD, congenital heart disease
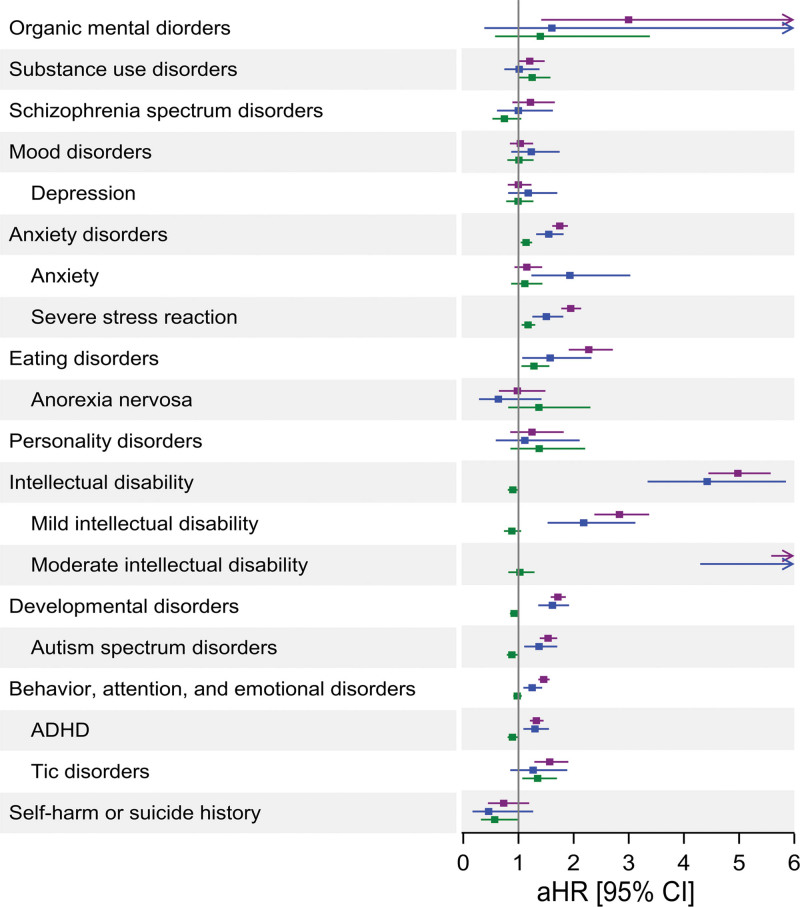
Compared with the general population and sibling cohorts, children with CHD had the highest aHRs for moderate intellectual disability (aHR, 7.23 [95% CI, 5.58–9.36] and aHR, 8.82 [95% CI, 4.30–18.12], respectively), severe stress reaction (aHR, 1.95 [95% CI, 1.78–2.14] and aHR, 1.51 [95% CI, 1.25–1.81], respectively), and ASD (aHR, 1.54 [95% CI, 1.39–1.70] and aHR, 1.37 [95% CI, 1.11–1.70], respectively; Figure 5; Table S6). Incidence rates were similar and aHRs were close to 1 when diagnostic groups and specific diagnoses were compared between the CHD and MCA cohorts.
Figure 5.
Forest plot of adjusted hazard ratios for hospital-based mental health diagnostic groups and specific hospital-based diagnoses in the CHD cohort, relative to the comparison cohorts. The aHR estimates are reported as a point estimate (dot) and 95% CIs (horizontal bars) for comparisons of the CHD cohort vs the general population cohort (purple), the CHD cohort vs the sibling cohort (blue), and the CHD cohort vs the non-CHD MCA cohort (green). The CHD cohort vs the general population cohort and the CHD cohort vs the MCA cohort analyses were adjusted by design for sex and year of CHD diagnosis as a result of matching and further adjusted for immigration status, maternal marital status, socioeconomic status, rurality, maternal and paternal mental health, and maternal and paternal physical health as determined by the Charlson Comorbidity Index score; the CHD cohort vs the sibling cohort analysis was adjusted for sex and calendar year. ADHD indicates attention deficit/hyperactivity disorder; aHR, adjusted hazard ratio; CHD, congenital heart disease; and MCA, major congenital anomalies
DISCUSSION
This national, longitudinal cohort study of the pediatric Danish population represents a comprehensive assessment of the risk of mental health conditions in the CHD population compared with to multiple reference cohorts. Herein, we report on 4 main findings. First, the cumulative incidence of mental health conditions was 35.1% by 18 years of age in the CHD cohort; this far exceeded the risk found in the general population and sibling cohorts but was similar to the MCA cohort. Second, the incidence of mental health conditions among children with CHD had a bimodal pattern, with prominent peaks in early childhood and adolescence. Third, males and children with severe or single-ventricle CHD had an increased risk of mental health conditions relative to females and to children with mild/moderate CHD. Fourth, relative to the general population and sibling cohorts, children with CHD were at increased risk of severe stress and neurodevelopmental disorders, including ADHD, intellectual disability, and ASD.
The inclusion of multiple comparison cohorts allowed us to better understand and contextualize the incidence of mental health conditions in the CHD cohort. The increased incidence of mental health conditions in the CHD cohort, compared with the general population and CHD sibling cohorts, was consistent using both the composite outcome and hospital-based mental health diagnostic codes for the entire CHD cohort and the CHD cohort stratified by age groups. This demonstrates that children of all ages with CHD are at increased risk of mental health conditions compared with their peers and siblings. The cumulative incidence of hospital-based mental health diagnoses by 18 years of age observed in the general population cohort in our study closely approximated findings in a similar Danish registry study (15.01% [95% CI, 14.48%–14.77%]) and previous global prevalence estimates of ≈13%, substantiating our methodology.28,34 We found that the incidence of mental health conditions in the sibling cohort was slightly higher than in the general population cohort. This is consistent with the limited number of published studies including siblings of children with congenital conditions.35,36 Siblings of children with chronic illnesses may experience familial and personal stressors, and the concept of a “carryover effect” in the sibling cohort may partially explain the increased rates of mental health conditions found in our study.37,38 Finally, the incidence of mental health conditions among children with CHD and children with non-CHD MCAs have not been directly compared in previous research. In our study, we found similar incidence rates in the 2 cohorts; however, children with non-CHD MCAs had a higher mental health burden than children in the general population, as has been found in previous studies.39,40 Using US national survey data spanning ≈10 years, the estimated 2-year cumulative incidence of mental health conditions was 11.5% for children 6 to 25 years of age with chronic physical conditions.39 Our findings extend previous research and suggest the cumulative incidence of hospital-based mental health diagnoses nears 1 in 4 by 18 years of age in children with non-CHD MCAs.
Although the incidence of mental health conditions in the CHD cohort mirrored male-predominant and peak-in-adolescence diagnostic patterns found in the general population, children with CHD also had a high incidence of mental health conditions in early childhood.28 Severe stress reactions were among the conditions with the highest incidence in infants and young children with CHD. Thus, the current study offers important quantitative epidemiological data on early-life stress, which are especially scarce. The cumulative burden of early medical adversity can have profound consequences for mental and physical health across the lifespan.41–43
Later, in mid-childhood and adolescence, neurodevelopmental and anxiety disorders predominated in our study. The lifelong challenges of managing a complex chronic illness, magnified by concomitant neurodevelopmental and behavioral disorders, compound the risk of mental health conditions in adolescence and adulthood.2,44 The causes of neurodevelopmental disorders in children with CHD have been extensively studied.2,3,45,46 Innate individual and environmental factors, such as genetic factors underlying common brain and heart developmental pathways, are now understood to be more important contributors to risk than perioperative factors.45,46 As in the general population, our study demonstrated that males have an increased incidence of ADHD and ASD, especially during mid-childhood, whereas females have an increased incidence of mood and anxiety disorders, especially during adolescence.4,6,14,28,47,48 It is interesting that the high incidence rate of mental health conditions in adolescent females led to nearly equal cumulative incidence curves between sexes by 18 years of age.28 Previous studies have found that <30% of children with CHD received psychotherapy or psychopharmacotherapy for known ADHD or anxiety.4,6 This represents an important opportunity for collaboration among pediatricians, mental health professionals such as psychologists and psychiatrists, and cardiologists to improve mental health outcomes among these patients.4,6
Our findings represent an important step in ongoing efforts to characterize the burden of mental health conditions in CHD. Next steps for our collaboration include identification of clinical, socioeconomic, and parent- and family-related factors associated with mental health conditions in CHD. In previous studies, socioeconomic factors (eg, education, employment, and household income) and parental psychological distress and mental health history have been more strongly associated with mental health conditions in children with CHD than medical factors including disease complexity.2,4–6,8,12,41,49 Our findings suggest that the role of medical complexity merits further investigation.4,6,8 As previously reported, we observed that children with mild or moderate CHD were at increased risk of mental health conditions compared with the general population cohort.7 These findings should raise awareness of a potentially underrecognized burden of mental health conditions among children with otherwise “simple” CHD, such as children with a history of ventricular septal defect repair or ballooned pulmonary stenosis. Children with severe or single-ventricle CHD represented a group at even higher risk, with an ≈2.2-fold increased risk of mental health conditions compared with the general population.
Strengths of this study include the longitudinal analysis of a national population with multiple comparison cohorts and minimal loss to follow-up. However, several limitations must be addressed. First, misclassification of diagnoses cannot be ruled out. Still, CHD diagnoses in the Danish National Patient Registry have been validated to medical records, with an overall high positive predictive value (95.5%).50 As well, most mental health diagnoses have been similarly validated with acceptable positive predictive values.20,26,27 The Danish Psychiatric Research Registry lacks diagnostic data from patients managed outside hospitals (ie, by general practitioners, psychologists, and psychiatrists in private practice). This prompted our use of a more sensitive composite outcome; however, the use of hospital-based diagnostic codes and the known undertreatment of mental health conditions with psychotherapy and pharmacotherapies limit our ability to estimate the true incidence of mental health conditions and specific mental health diagnoses in the Danish population. In addition, follow-up data were less robust in the adolescent cohort, as ≈70% of CHD diagnoses were made by 12 months of age, and the median follow-up duration after CHD diagnosis was 8 years. Thus, incidence estimates of specific mental health conditions diagnosed at higher rates during adolescence, such as anxiety and depression, are likely underestimated.16,28 In Denmark, routine developmental evaluations are performed in the home by nurses during infancy, in daycare and at school entry by early childhood educators, and by general practitioners as part of regular checkups. For children with CHD, a high number of encounters with the health care system, as well as increased awareness among parents and health professionals, may have resulted in ascertainment bias; however, we do not believe this fully explains the high incidence rates found in young children with CHD in this study. This study lacked adequate follow-up data to investigate the effect of era (in terms of advancement in medical and surgical care of children with CHD during the study period) on the incidence of mental health conditions, as children born in the early versus later periods of the study had different durations of follow-up. Finally, the incidence of mental health conditions reported in our study represents a risk estimate within a specific medical and sociocultural system. The rates of severe and single-ventricle heart disease are comparatively lower in Denmark than in many other countries; thus, the data reported here potentially underestimate the mental health burden in larger, more complex CHD populations. Similarly, children with CHD experiencing food or housing insecurity, systemic racism, or less access to health care may be at increased mental health risk than children with CHD in Denmark who benefit from strong social services and easy access to health care.51 Thus, our findings for Danish children should be reconsidered within the different circumstances of children living in other countries.
Conclusions
We found that more than 1 in 3 children with CHD were diagnosed with or treated for a mental health condition by 18 years of age. Compared with the general population and siblings, the mental health burden was significantly higher in the CHD population. This disparate risk began early in life and was most prominent among males and children with severe or single-ventricle heart disease. Children with CHD were at increased risk for neurodevelopmental disorders and anxiety disorders (especially severe stress in early childhood) compared with their peers and siblings. Health care professionals should be aware of the substantial mental health burden in this high-risk population. This study supports the growing body of evidence highlighting the importance of prevention, early identification, and intervention approaches for mental health conditions within the congenital cardiac community.
ARTICLE INFORMATION
Sources of Funding
N.A.K. is the recipient of a National Heart Foundation of Australia future leader fellowship (101229) and receives support from the Heart Institute Research Core at Cincinnati Children’s Hospital.
Disclosures
None.
Supplemental Material
Tables S1–S6
Figures S1–S4
Supplementary Material
Nonstandard Abbreviations and Acronyms
- ADHD
- attention deficit hyperactivity disorder
- ASD
- autism spectrum disorder
- CHD
- congenital heart disease
- ICD
- International Classification of Diseases
- MCA
- major congenital anomaly
N.A. Kasparian and N. Madsen contributed equally.
This manuscript was sent to Marc Cribbs, Guest Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCULATIONAHA.123.064705.
For Sources of Funding and Disclosures, see page 1392.
Circulation is available at www.ahajournals.org/journal/circ.
Contributor Information
Dóra Körmendiné Farkas, Email: df@clin.au.dk.
Kristina Laugesen, Email: kristina.laugesen@clin.au.dk.
Henrik Toft Sørensen, Email: hts@clin.au.dk.
Nadine A. Kasparian, Email: nadine.kasparian@cchmc.org.
Nicolas Madsen, Email: nicolas.madsen@utsouthwestern.edu.
REFERENCES
- 1.GBD 2017 Congenital Heart Disease Collaborators. Global, regional, and national burden of congenital heart disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Child Adolesc Health. 2020;4:185–200. doi: 10.1016/S2352-4642(19)30402-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kovacs AH, Brouillette J, Ibeziako P, Jackson JL, Kasparian NA, Kim YY, Livecchi T, Sillman C, Kochilas LK; American Heart Association Council on Lifelong Congenital Heart Disease and Heart Health in the Young; and Stroke Council. Psychological outcomes and interventions for individuals with congenital heart disease: a scientific statement from the American Heart Association. Circ Cardiovasc Qual Outcomes. 2022;15:e000110. doi: 10.1161/HCQ.0000000000000110 [DOI] [PubMed] [Google Scholar]
- 3.Marino BS, Lipkin PH, Newburger JW, Peacock G, Gerdes M, Gaynor JW, Mussatto KA, Uzark K, Goldberg CS, Johnson WH, Jr, et al. ; American Heart Association Congenital Heart Defects Committee, Council on Cardiovascular Disease in the Young, Council on Cardiovascular Nursing, and Stroke Council. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation. 2012;126:1143–1172. doi: 10.1161/CIR.0b013e318265ee8a [DOI] [PubMed] [Google Scholar]
- 4.DeMaso DR, Calderon J, Taylor GA, Holland JE, Stopp C, White MT, Bellinger DC, Rivkin MJ, Wypij D, Newburger JW. Psychiatric disorders in adolescents with single ventricle congenital heart disease. Pediatrics. 2017;139:e20162241. doi: 10.1542/peds.2016-2241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeMaso DR, Labella M, Taylor GA, Forbes PW, Stopp C, Bellinger DC, Rivkin MJ, Wypij D, Newburger JW. Psychiatric disorders and function in adolescents with d-transposition of the great arteries. J Pediatr. 2014;165:760–766. doi: 10.1016/j.jpeds.2014.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holland JE, Cassidy AR, Stopp C, White MT, Bellinger DC, Rivkin MJ, Newburger JW, DeMaso DR. Psychiatric disorders and function in adolescents with tetralogy of fallot. J Pediatr. 2017;187:165–173. doi: 10.1016/j.jpeds.2017.04.048 [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez VJ, Kimbro RT, Cutitta KE, Shabosky JC, Bilal MF, Penny DJ, Lopez KN. Mental health disorders in children with congenital heart disease. Pediatrics. 2021;147:e20201693. doi: 10.1542/peds.2020-1693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olsen M, Sørensen HT, Hjortdal VE, Christensen TD, Pedersen L. Congenital heart defects and developmental and other psychiatric disorders: a Danish nationwide cohort study. Circulation. 2011;124:1706–1712. doi: 10.1161/CIRCULATIONAHA.110.002832 [DOI] [PubMed] [Google Scholar]
- 9.Carazo MR, Kolodziej MS, DeWitt ES, Kasparian NA, Newburger JW, Duarte VE, Singh MN, Opotowsky AR. Prevalence and prognostic association of a clinical diagnosis of depression in adult congenital heart disease: results of the Boston Adult Congenital Heart Disease Biobank. J Am Heart Assoc. 2020;9:e014820. doi: 10.1161/JAHA.119.014820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim YY, Gauvreau K, Bacha EA, Landzberg MJ, Benavidez OJ. Resource use among adult congenital heart surgery admissions in pediatric hospitals: risk factors for high resource utilization and association with inpatient death. Circ Cardiovasc Qual Outcomes. 2011;4:634–639. doi: 10.1161/CIRCOUTCOMES.111.963223 [DOI] [PubMed] [Google Scholar]
- 11.Kovacs AH, Saidi AS, Kuhl EA, Sears SF, Silversides C, Harrison JL, Ong L, Colman J, Oechslin E, Nolan RP. Depression and anxiety in adult congenital heart disease: predictors and prevalence. Int J Cardiol. 2009;137:158–164. doi: 10.1016/j.ijcard.2008.06.042 [DOI] [PubMed] [Google Scholar]
- 12.Marshall KH, D’Udekem Y, Sholler GF, Opotowsky AR, Costa DSJ, Sharpe L, Celermajer DS, Winlaw DS, Newburger JW, Kasparian NA. Health-related quality of life in children, adolescents, and adults with a Fontan circulation: a meta-analysis. J Am Heart Assoc. 2020;9:e014172. doi: 10.1161/JAHA.119.014172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Christensen MK, Lim CCW, Saha S, Plana-Ripoll O, Cannon D, Presley F, Weye N, Momen NC, Whiteford HA, Iburg KM, et al. The cost of mental disorders: a systematic review. Epidemiol Psychiatr Sci. 2020;29:e161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, Hedden SL, Crosby AE, Visser SN, Schieve LA, et al. ; Centers for Disease Control and Prevention (CDC). Mental health surveillance among children—United States, 2005-2011. MMWR Suppl. 2013;62:1–35. [PubMed] [Google Scholar]
- 15.Snell T, Knapp M, Healey A, Guglani S, Evans-Lacko S, Fernandez JL, Meltzer H, Ford T. Economic impact of childhood psychiatric disorder on public sector services in Britain: estimates from national survey data. J Child Psychol Psychiatry. 2013;54:977–985. doi: 10.1111/jcpp.12055 [DOI] [PubMed] [Google Scholar]
- 16.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- 17.Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, Crumb SR, Dearani JA, Fuller S, Gurvitz M, et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e698–e800. doi: 10.1161/CIR.0000000000000603 [DOI] [PubMed] [Google Scholar]
- 18.Laugesen K, Ludvigsson JF, Schmidt M, Gissler M, Valdimarsdottir UA, Lunde A, Sørensen HT. Nordic health registry-based research: a review of health care systems and key registries. Clin Epidemiol. 2021;13:533–554. doi: 10.2147/CLEP.S314959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmidt M, Schmidt SAJ, Adelborg K, Sundbøll J, Laugesen K, Ehrenstein V, Sørensen HT. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. doi: 10.2147/CLEP.S179083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evers PD, Farkas DK, Hjorth CF, Khoury M, Olsen M, Madsen NL. Return to work following adverse cardiovascular events in adults with congenital heart disease. Int J Cardiol Congenital Heart Dis. 2021;4:100160. doi: 10.1016/j.ijcchd.2021.100160 [Google Scholar]
- 22.Larsen SH, Olsen M, Emmertsen K, Hjortdal VE. Interventional treatment of patients with congenital heart disease: nationwide Danish experience over 39 years. J Am Coll Cardiol. 2017;69:2725–2732. doi: 10.1016/j.jacc.2017.03.587 [DOI] [PubMed] [Google Scholar]
- 23.Obel C, Zhu JL, Olsen J, Breining S, Li J, Grønborg TK, Gissler M, Rutter M. The risk of attention deficit hyperactivity disorder in children exposed to maternal smoking during pregnancy — a re-examination using a sibling design. J Child Psychol Psychiatry. 2016;57:532–537. doi: 10.1111/jcpp.12478 [DOI] [PubMed] [Google Scholar]
- 24.Larsen H, Nielsen GL, Bendsen J, Flint C, Olsen J, Sørensen HT. Predictive value and completeness of the registration of congenital abnormalities in three Danish population-based registries. Scand J Public Health. 2003;31:12–16. doi: 10.1080/14034940210134194 [DOI] [PubMed] [Google Scholar]
- 25.Rotberg B, Horváth-Puhó E, Vigod S, Ray JG, Sørensen HT, Cohen E. Increased maternal new-onset psychiatric disorders after delivering a child with a major anomaly: a cohort study. Acta Psychiatr Scand. 2020;142:264–274. doi: 10.1111/acps.13181 [DOI] [PubMed] [Google Scholar]
- 26.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39:54–57. doi: 10.1177/1403494810395825 [DOI] [PubMed] [Google Scholar]
- 27.Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M. Data resource profile: the Danish National Prescription Registry. Int J Epidemiol. 2017;46:798–798f. doi: 10.1093/ije/dyw213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dalsgaard S, Thorsteinsson E, Trabjerg BB, Schullehner J, Plana-Ripoll O, Brikell I, Wimberley T, Thygesen M, Madsen KB, Timmerman A, et al. Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiatry. 2020;77:155–164. doi: 10.1001/jamapsychiatry.2019.3523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pedersen CB, Mors O, Bertelsen A, Waltoft BL, Agerbo E, McGrath JJ, Mortensen PB, Eaton WW. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014;71:573–581. doi: 10.1001/jamapsychiatry.2014.16 [DOI] [PubMed] [Google Scholar]
- 30.WHO Collaborating Center for Drug Statistics Methodology. Guidelines for ATC Classification and DDD Assignment, 2023. Oslo, 2022. [Google Scholar]
- 31.Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 2011;39:12–16. doi: 10.1177/1403494811399956 [DOI] [PubMed] [Google Scholar]
- 32.Jørgensen H, Horváth-Puhó E, Laugesen K, Braekkan S, Hansen JB, Sørensen HT. Socioeconomic status and risk of incident venous thromboembolism. J Thromb Haemost. 2021;19:3051–3061. doi: 10.1111/jth.15523 [DOI] [PubMed] [Google Scholar]
- 33.Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature. 2019;567:305–307. doi: 10.1038/d41586-019-00857-9 [DOI] [PubMed] [Google Scholar]
- 34.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: s meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56:345–365. doi: 10.1111/jcpp.12381 [DOI] [PubMed] [Google Scholar]
- 35.Feudtner C, Nye RT, Boyden JY, Schwartz KE, Korn ER, Dewitt AG, Waldman AT, Schwartz LA, Shen YA, Manocchia M, et al. Association between children with life-threatening conditions and their parents’ and siblings’ mental and physical health. JAMA Netw Open. 2021;4:e2137250. doi: 10.1001/jamanetworkopen.2021.37250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wray J, Maynard L. Living with congenital or acquired cardiac disease in childhood: maternal perceptions of the impact on the child and family. Cardiol Young. 2005;15:133–140. doi: 10.1017/S1047951105000302 [DOI] [PubMed] [Google Scholar]
- 37.Deavin A, Greasley P, Dixon C. Children’s perspectives on living with a sibling with a chronic illness. Pediatrics. 2018;142:e20174151. doi: 10.1542/peds.2017-4151 [DOI] [PubMed] [Google Scholar]
- 38.Sjölander A, Frisell T, Kuja-Halkola R, Öberg S, Zetterqvist J. Carryover effects in sibling comparison designs. Epidemiology. 2016;27:852–858. doi: 10.1097/EDE.0000000000000541 [DOI] [PubMed] [Google Scholar]
- 39.Adams JS, Chien AT, Wisk LE. Mental illness among youth with chronic physical conditions. Pediatrics. 2019;144:e20181819. doi: 10.1542/peds.2018-1819 [DOI] [PubMed] [Google Scholar]
- 40.Suryavanshi MS, Yang Y. Clinical and economic burden of mental disorders among children with chronic physical conditions, United States, 2008-2013. Prev Chronic Dis. 2016;13:E71. doi: 10.5888/pcd13.150535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kasparian NA, Kan JM, Sood E, Wray J, Pincus HA, Newburger JW. Mental health care for parents of babies with congenital heart disease during intensive care unit admission: systematic review and statement of best practice. Early Hum Dev. 2019;139:104837. doi: 10.1016/j.earlhumdev.2019.104837 [DOI] [PubMed] [Google Scholar]
- 42.Nelson CA, Scott RD, Bhutta ZA, Harris NB, Danese A, Samara M. Adversity in childhood is linked to mental and physical health throughout life. BMJ. 2020;371:m3048. doi: 10.1136/bmj.m3048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–e246. doi: 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- 44.Robson VK, Stopp C, Wypij D, Dunbar-Masterson C, Bellinger DC, DeMaso DR, Rappaport LA, Newburger JW. Longitudinal associations between neurodevelopment and psychosocial health status in patients with repaired d-transposition of the great arteries. J Pediatr. 2019;204:38–45.e1. doi: 10.1016/j.jpeds.2018.08.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gaynor JW, Stopp C, Wypij D, Andropoulos DB, Atallah J, Atz AM, Beca J, Donofrio MT, Duncan K, Ghanayem NS, et al. ; International Cardiac Collaborative on Neurodevelopment (ICCON) Investigators. Neurodevelopmental outcomes after cardiac surgery in infancy. Pediatrics. 2015;135:816–825. doi: 10.1542/peds.2014-3825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Homsy J, Zaidi S, Shen Y, Ware JS, Samocha KE, Karczewski KJ, DePalma SR, McKean D, Wakimoto H, Gorham J, et al. De novo mutations in congenital heart disease with neurodevelopmental and other congenital anomalies. Science. 2015;350:1262–1266. doi: 10.1126/science.aac9396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shillingford AJ, Glanzman MM, Ittenbach RF, Clancy RR, Gaynor JW, Wernovsky G. Inattention, hyperactivity, and school performance in a population of school-age children with complex congenital heart disease. Pediatrics. 2008;121:e759–e767. doi: 10.1542/peds.2007-1066 [DOI] [PubMed] [Google Scholar]
- 49.McCusker CG, Doherty NN, Molloy B, Casey F, Rooney N, Mulholland C, Sands A, Craig B, Stewart M. Determinants of neuropsychological and behavioural outcomes in early childhood survivors of congenital heart disease. Arch Dis Child. 2006;92:137–141. doi: 10.1136/adc.2005.092320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schwartz SS, Pedersen MGB, Frøslev T, Madsen N, Olsen MS. Positive predictive value of congenital heart disease diagnostic codes in the Danish National Patient Registry. Int J Cardiol Congenital Heart Dis. 2022;8:100372. [Google Scholar]
- 51.Gonzalez VJ, Kimbro RT, Shabosky JC, Kostelyna S, Fasipe T, Villafranco N, Cutitta KE, Lopez KN. Racial disparities in mental health disorders in youth with chronic medical conditions. J Pediatr. 2023;259:113411. doi: 10.1016/j.jpeds.2023.113411 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.