Abstract
Background
Theophylline is commonly used to control respiratory diseases, especially in developing countries. Theophylline has a narrowed therapeutic index, and its toxicity is associated with morbidity and mortality. Physicians should be aware of the early prediction of the need for intensive care unit admission (ICU) and mechanical ventilation (MV).
Aim
This study aimed to assess the power of the Rapid Emergency Medicine Score (REMS), Modified Early Warning Score (MEWS) and Simple Clinical Score (SCS) in predicting the need for ICU admission and/or MV in acute theophylline-poisoned patients.
Patients and methods
This cross-sectional study included 58 patients with acute theophylline poisoning who were admitted to our Poison Control Center from the 1st of July 2022 to the 31st of January 2023. The REMS, MEWS and SCS were calculated for all patients on arrival at the hospital. The area under the curve (AUC) and receiver operating characteristics were tested to compare scores.
Results
The median values of all studied scores were significantly high among patients who needed MV and/or ICU admission. The AUC of SCS was >0.9, with a sensitivity of 92.9% and specificity of 90.9% for the prediction of ICU admission. Meanwhile, MEWS was an excellent predictor of the need for MV (AUC = 0.996, 95% CI = 0.983–1.000).
Conclusions
We recommend using SCS as an early predictor for ICU admission in acute theophylline-poisoned patients. However, MEWS could effectively predict MV requirements in acute theophylline-poisoned patients.
Keywords: theophylline poisoning, rapid emergency medicine score, modified early warning score, simple clinical score
Introduction
Theophylline drugs are the most often prescribed medications for treating asthma and chronic obstructive pulmonary disease due to their effectiveness, low cost, and easy availability.1 Young children frequently consume theophylline drugs out of curiosity or suicide teenagers.2 The incidence of severe or potentially fatal acute theophylline poisoning ranged from 12%–25% of overdose patients.3 In Egypt, Abuelfadl et al.4 and Elhawary et al.5 reported that 28.57% and 16.7% of patients with acute theophylline toxicity were admitted to the intensive units, respectively.
Theophylline has a limited therapeutic window and variable pharmacokinetics. Theophylline metabolism varies with age, with younger children metabolizing the drug more quickly than older teenagers. Moreover, febrile conditions may slow theophylline clearance.6 Therefore, it frequently causes inadvertent persistent intoxication.3 Acute toxicity can occur if a single dose of more than 10 mg/kg of theophylline is consumed. Moreover, acute poisoning happens in patients chronically using the drug when a risky toxic dose of theophylline is consumed.7
Acute theophylline poisoning causes significant morbidity and mortality. It is associated with many gastrointestinal, neurologic, musculoskeletal, and cardiovascular manifestations.8 Furthermore, life-threatening events such as refractory seizures and cardiac arrhythmias can appear without warning. These events are relatively resistant to standard therapeutic measures, eventually leading to cardiac arrest.9
Treatment of acute theophylline toxicity is generally supportive. However, severely intoxicated patients with life-threatening conditions usually need intensive care. Hence, early prediction of patients requiring mechanical ventilation (MV) and/or intensive care unit (ICU) admission can help physicians improve patient outcomes and reduce resource waste.9
In medical practice, using scoring systems supports clinical judgment. They allow doctors to distinguish diseases, evaluate patients’ conditions, categorize risks, and anticipate outcomes.10 Scoring systems should be simple and mainly focused on clinical data, with little attention to investigations, especially in emergencies.11 Scoring systems should have high levels of reliability and dependability and ideally be easy to calculate at the patient’s bedside by entering the factors into a smartphone application.12 Various scoring systems, including, Rapid Emergency Medicine Score (REMS), Modified Early Warning Score (MEWS) and Simple Clinical Score (SCS), have been created and validated for use in emergency rooms.13
The REMS was introduced by Olsson et al.14 to predict mortality rates among nonsurgical patients. In emergencies, REMS was effective in risk stratification for critically ill patients, which was attributed to its high negative predictive value.15 The MEWS was created to evaluate hospitalized patients for early clinical deterioration detection.16 It consists of simple parameters that the physician can quickly attain to predict outcomes.17 The SCS has several potential uses, including the early identification of patients with a high risk of death who will need care in critical care units, the early identification of patients with a low risk of death who are suitable for early hospital discharge, and assessing the performance of acute medical departments.18
The REMS, MEWS, and SCS scores are commonly used to predict ICU admission and emergency MV, but they are non-specific for theophylline poisoning. However, these scores have been used to assess poisoned patients,13,17,19–21 with reliable findings. Hence, we hypothesized that these scoring systems derived from bedside data such as age, vital signs, mental status, and ECG could aid physicians in spotting patients who are deteriorating early. This is the first study to assess REMS, MEWS, and SCS for the early prediction of the need for ICU admission and/or MV in acute theophylline-poisoned patients.
Patient and methods
Ethical consideration
The present study was carried out following approval of the medical research ethics committee of the Tanta Faculty of Medicine (Approval code: 35563/6/22). After an explanation of the purpose and procedures of the study, all patients or their guardians were asked to provide informed written consent for participation. All data were processed secretly by making code numbers for each patient to maintain the confidentiality of the data.
Study design, setting and date
This cross-sectional study was conducted on acute theophylline-poisoned patients admitted to Tanta Poison Control Center, Emergency hospital, Tanta University throughout the period from the 1st of July 2022 to the 31st of January 2023.
Participants
Patients of both sexes aged ≥16 with acute theophylline poisoning were included in this study. Diagnosis of acute theophylline intoxication was based on the history that the patients, or their relatives reported and typical symptoms & signs of acute theophylline toxicity. In addition, identification of the drug using strips or containers brought by patients’ attendants. Drug level was not used for diagnosis as it is unavailable in our poison control center. Acute poisoning was defined as a single exposure to a toxic dose of theophylline without prior use. In contrast, chronic poisoning refers to repeated administration of therapeutic doses of theophylline for at least six months without ingesting a single toxic dose.22,23
Patients with chronic theophylline poisoning or co-ingestion and chronic illnesses (liver, kidney, and cardiac) were excluded. Patients with trauma or burns associated with poisoning and those who received any treatments before admission were also excluded.
Data collection
Demographic data including (age, sex, and residence) and toxicological data including (type, the form of the drug, route of intake, amount of drug taken, mode of poisoning and the elapsed time from intake to hospital admission) were obtained for all patients.
Vital signs, consciousness level and complete physical examination, were reported on admission. Moreover, Arterial blood gases analysis, serum potassium, random blood sugar, blood oxygen saturation, and Electrocardiogram (ECG) were performed on the studied patients at the time of hospital admission.
Calculation of the studied scoring systems
The following scoring systems were calculated at the time of the hospital admission and compared for the prediction of ICU admission and/or the need for MV in acute theophylline-poisoned patients:
1) The REMS comprised pulse rate, mean arterial pressure, respiratory rate, GCS, age, and oxygen saturation. The scoring points ranged from zero to four for each variable except the age, which ranged from zero to six. The lowest score was zero, while the highest score was 26.14
2) The MEWS included systolic blood pressure, heart rate, respiratory rate, temperature, and level of consciousness (using the AVPU scale). These parameters were scored from 0 to 3 according to the severity from normal to abnormal values. The minimum score was 0 and the maximum was 15.24
3) The SCS was calculated based on seven parameters: age, airway, breathing, circulation, disability, ECG, and temperature. The minimum score was 0 and the maximum score was 21.18
Outcomes
The primary outcomes were the need for ICU admission and/or MV among acute theophylline-poisoned patients.
Statistical analysis
MedCalc Statistical Software version 15.8 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2015) was used for conducting the analysis. For numerical variables, the Shapiro-Wilk test for normality was achieved to assess the distribution of data. The variables that followed the normal distribution were summarized as the mean ± standard deviation (SD). The numerical variables that did not follow the normal distribution were summarized as the median and interquartile range (IQR, expressed as 25th–75th percentiles). The Mann-Whitney test was used to compare the scores between two outcome groups (between those admitted to ICU and those who did not, as well as between those requiring MV and those not). The direction, intensity, and significance of the link between the analyzed scores and other numerical variables were examined using Spearman’s rank-order correlation. The categorical variables were expressed as counts and percentages. The appropriate cut-off value, sensitivity, specificity, and positive and negative predictive values (PPV and NPV) for each score were determined using the receiver operating characteristics (ROC) curve. The area under the curve (AUC) was given the following grades: 0.90–1 = excellent; 0.80–0.90 = good; 0.70–0.80 = fair; And 0.60–0.70 = poor. The AUCs of every two scores were compared using the method based on the Mann-Whitney test. A P-value < 0.05 was selected to indicate the significance of the results of statistical tests.
Results
The total number of acute theophylline-poisoned patients admitted to our poison control center was 60 during the study period. Two patients were excluded due to co-ingestion intake of other xenobiotics. Fifty-eight patients were included. Of these 58 patients, 44 did not admit to ICU or needed mechanical ventilation. Meanwhile, 14 patients required ICU admission, of which only two required MV and the remaining 12 patients were admitted to the ICU without needing MV (Fig. 1).
Fig. 1.
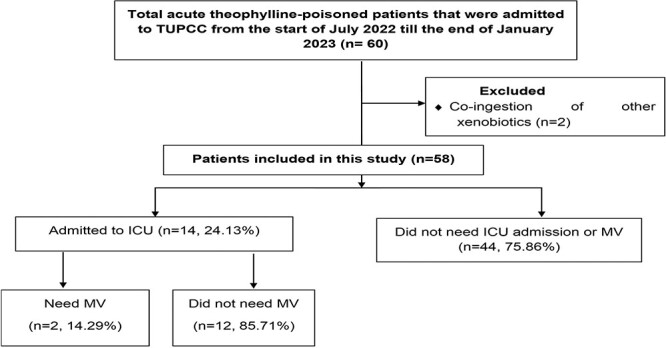
Flow chart of the studied patients.
Table 1 shows the sociodemographic data, toxicological data, vital signs, and results of the scoring systems of the participants. The patients’ age ranged between 16 and 50 years old, with a mean age of 24 ± 8.1 years. Female patients outnumbered males (70.7% versus 29.3%, respectively). Most patients (62.1%) were from rural areas. All patients were presented with suicidal attempts by oral ingestion of theophylline tablets with a median dose of 2,800 mg and a median delay of 4 h before arrival. At admission, the mean systolic blood pressure was 102.3 ± 14.3 mmHg. The mean diastolic blood pressure was 65 ± 12.2 mmHg. The mean arterial blood pressure was 77.5 ± 12.4 mmHg. The mean respiratory rate was 22.8 ± 5.7 cycles/min. The mean temperature was 37 ± 0.3 °C. The mean pulse rate was 113.4 ± 15 beats/min. The mean oxygen saturation was 94.1 ± 4.6%. The median values of REMS, MEWS, and SCS were 2.5, 4 and 5, respectively.
Table 1.
Patients’ demographic data, toxicological data, vital signs, scoring systems results and clinical outcomes (Total n = 58).
| Variables | All patients (n = 58) | |
|---|---|---|
| Age, years | Mean ± SD | 24.0 ± 8.1 |
| Minimum–Maximum | 16.0–50.0 | |
| Sex | Female | 41 (70.7%) |
| Male | 17 (29.3%) | |
| Residence | Rural | 36 (62.1%) |
| Urban | 22 (37.9%) | |
| Mode | Suicidal | 58 (100.0%) |
| Route | Oral | 58 (100.0%) |
| Delay, hours | Median [IQR] | 4.0 [3.0–8.0] |
| Dose, mg | Median [IQR] | 2800.0 [2000.0–3600.0] |
| GCS | Median [IQR] | 15.0 [15.0–15.0] |
| Systolic blood pressure, mmHg | Mean ± SD | 102.8 ± 14.3 |
| Diastolic blood pressure, mmHg | Mean ± SD | 65.0 ± 12.2 |
| Mean blood pressure, mmHg | Mean ± SD | 77.5 ± 12.4 |
| Respiratory rate, cycles/minute | Mean ± SD | 22.8 ± 5.7 |
| Temperature, °C | Mean ± SD | 37.0 ± 0.3 |
| Pulse, beats/minute | Mean ± SD | 113.4 ± 15.0 |
| O2 saturation, % | Mean ± SD | 94.1 ± 4.6 |
| REMS | Median [IQR] | 2.5 [2.0–5.0] |
| MEWS | Median [IQR] | 4.0 [2.0–6.0] |
| SCS | Median [IQR] | 5.0 [1.0–8.0] |
| Outcomes | ICU admission | 14 (24.1%) |
| Mechanical Ventilation | 2 (3.4%) | |
| Duration of hospital stay, hours | Median [IQR] | 24.0 [24.0–48.0] |
Data are presented as mean ± SD, number (%), or median (IQR). SD: standard deviation; IQR: interquartile range; B/p: blood pressure; O2: oxygen; GCS: Glasgow coma score; REMS: Rapid Emergency Medicine Score; MEWS: Modifies Early Warning Score; SCS: Simple Clinical Score; IQR: interquartile range.
Figure 2 clarifies the clinical manifestations of the participants. The most common gastrointestinal presentations included vomiting (67.2%) and abdominal pain (51.7%). Tachycardia was the most common cardiovascular presentation (82.8%). Regarding neurological manifestations, tremors occurred among 31% of patients. While 22.4% of patients presented with agitation, only three developed seizures. Abnormal ECG was reported among 24.1% of acute theophylline-poisoned patients.
Fig. 2.
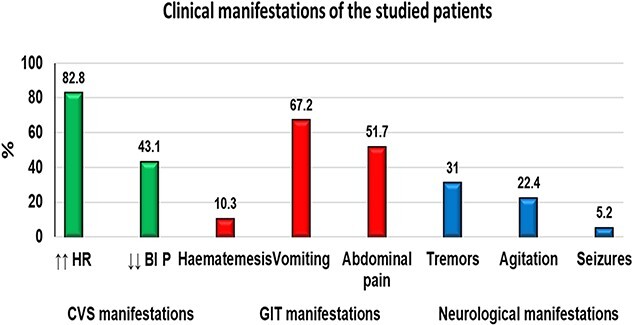
Clinical manifestations of acute theophylline-poisoned patients (n = 58).
Table 2 compares the studied scores for needing MV and ICU on admission. All the median scores were significantly elevated in patients requiring MV and ICU access compared to those who did not need MV and ICU entry (P ≤ 0.001*).
Table 2.
Correlation of calculated rapid emergency medicine score (REMS), modified early warning score (MEWS) and simple clinical score (SCS) with the outcomes.
| Calculated scores | ICU admission (n = 58) | Mechanical ventilation (n = 58) | |||||
|---|---|---|---|---|---|---|---|
| No (n = 44) | Yes (n = 14) | P | No (n = 56) | Yes (n = 2) | P | ||
| REMS | Median [IQR] | 2 [0–3] | 6 [4–7] | <0.001a | 2 [2–5] | 8 [7–8] | 0.011a |
| Min—Max | 0–7 | 2–9 | 0–9 | 7–8 | |||
| MEWS | Median [IQR] | 3 [2–5] | 6.5 [5–8] | <0.001a | 4 [2–6] | 10 [9–10] | 0.001a |
| Min—ax | 0–7 | 3–10 | 0–9 | 9–10 | |||
| SCS | Median [IQR] | 2 [0–5] | 11 [8–12] | <0.001a | 5 [0.5–8] | 13 [12–13] | 0.005a |
| Min—Max | 0–9 | 5–13 | 0–13 | 12–13 | |||
Data are presented as median and IQR. IQR: interquartile range; min: minimum; max: maximum; ICU: intensive care unit; REMS: Rapid Emergency Medicine Score; SCS: Simple Clinical Score; MEWS: Modified Early Warning Score. P-values are based on the Mann-Whitney test.
aSignificant at P < 0.05.
Spearman’s rank-order correlation showed a moderately positive correlation between the ingested theophylline dose and the studied scores. REMS and SCS had a strong positive correlation with the hospitalization period. Meanwhile, MEWS was moderately significantly positively correlated to the hospitalization duration (Table 3).
Table 3.
Spearman’s rank-order correlation between the studied scores on admission and the delay time before reaching the hospital, dose, and duration of hospitalization (Total n = 58).
| REMS | MEWS | SCS | ||
|---|---|---|---|---|
| Delay, hours | rs | 0.259 | 0.176 | 0.149 |
| p | 0.050 | 0.187 | 0.264 | |
| Dose, mg | rs | 0.507 | 0.371 | 0.349 |
| p | <0.001* | 0.004* | 0.007* | |
| Duration of hospital stay, hours | rs | 0.748 | 0.680 | 0.721 |
| p | <0.001* | <0.001* | <0.001* |
mg: milligram; REMS: Rapid Emergency Medicine Score; SCS: Simple Clinical Score; MEWS: Modified Early Warning Score; P-values are based on Spearman’s rank-order correlation; *: Significant at p < 0.05.
Figure 3 displays the ROC curve analysis for predicting ICU admission using the studied scores. The SCS had the best AUC (AUC = 0.96), followed by REMS (AUC = 0.891) and finally, MEWS (AUC = 0.877). Pairwise comparisons of AUCs revealed a statistically significant difference between MEWS versus SCS (P = 0.015). The optimal cut-off levels for each score and their associated sensitivities, specificities, PPV, and NPP were revealed in Table 4.
Fig. 3.
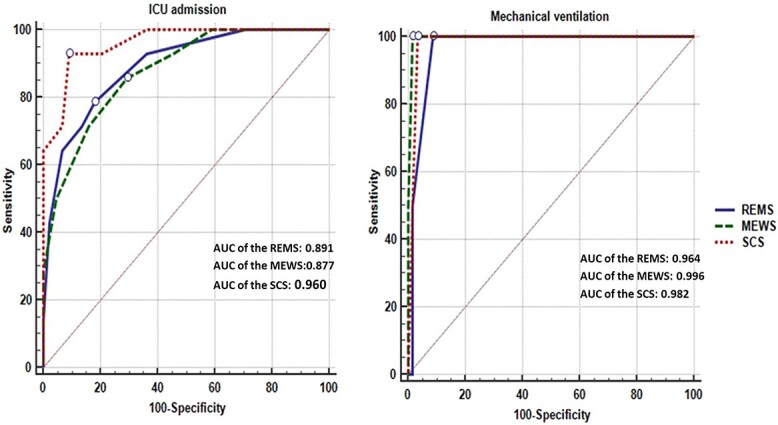
The receiver operating characteristics (ROC) curves for rapid emergency medicine score (REMS), modified early warning score (MEWS) and simple clinical score (SCS) for prediction of the need for intensive care unit (ICU) and mechanical ventilation (MV) in acute theophylline poisoned patients.
Table 4.
The area under the curve, cut-off values, sensitivity, specificity, negative predictive value, and positive predictive value & pairwise comparison of scoring systems for prediction of ICU admission.
| Outcome | ICU admission | ||
|---|---|---|---|
| Scores | REMS | MEWS | SCS |
| AUC | 0.891 | 0.877 | 0.960 |
| 95% CI of AUC | 0.798 to 0.984 | 0.779 to 0.974 | 0.912 to 1.000 |
| P-value | <0.001a | <0.001a | <0.001a |
| Cut-off | >3 | >4 | >7 |
| Sens (%) | 78.6 | 85.7 | 92.9 |
| Spec (%) | 81.8 | 70.5 | 90.9 |
| PPV (%) | 57.9 | 48.0 | 76.5 |
| NPV (%) | 92.3 | 93.9 | 97.6 |
| Accuracy (%) | 81.0 | 74.1 | 91.4 |
| Pairwise comparisons of AUCs | REMS vs. MEWS = 0.678 REMS vs. SCS = 0.112 MEWS vs. SCS = 0.015a |
||
AUC: area under the curve; ICU: intensive care unit; CI: confidence interval; PPV: positive predictive value; NPV: negative predictive value; REMS: rapid emergency medicine score; SCS: simple clinical score; MEWS: Modified Early Warning Score; P-values are based on the Mann-Whitney test.
aSignificant at p < 0.05.
Figure 3 displays the ROC curve analysis for predicting the MV requirement using the studied scores. All the analyzed scores had an AUC > 0.9, indicating they are excellent predictors for requiring MV. The MEWS had the best AUC (AUC = 0.996), followed by SCS (AUC = 0.982) and finally REMS (AUC = 0.964). However, no statistically significant difference was reported among the AUCs of the studied scores (all P values > 0.05). The optimal cut-off levels for each score and their associated sensitivities, specificities, PPV, and NPP were revealed in Table 5.
Table 5.
The area under the curve, cut-off values, sensitivity, specificity negative predictive value, and positive predictive value & pairwise comparison of scoring systems for predicting mechanical ventilation (Total n = 58).
| Outcome | Mechanical Ventilation | ||
|---|---|---|---|
| Scores | REMS | MEWS | SCS |
| AUC | 0.964 | 0.996 | 0.982 |
| 95% CI of AUC | 0.912 to 1.000 | 0.983 to 1.000 | 0.950 to 1.000 |
| P-value | <0.001a | <0.001a | <0.001a |
| Cut-off | >6 | >8 | >11 |
| Sens (%) | 100.0 | 100.0 | 100.0 |
| Spec (%) | 91.1 | 98.2 | 96.4 |
| PPV (%) | 28.6 | 66.7 | 50.0 |
| NPV (%) | 100.0 | 100.0 | 100.0 |
| Accuracy (%) | 91.4 | 98.3 | 96.6 |
| Pairwise comparisons of AUCs | REMS vs. MEWS = 0.130 REMS vs. SCS = 0.152 MEWS vs. SCS = 0.218 |
||
AUC: area under the curve; ICU: intensive care unit; CI: confidence interval; PPV: positive predictive value; NPV: negative predictive value; REMS: rapid emergency medicine score; SCS: simple clinical score; MEWS: Modified Early Warning Score; P-values are based on the Mann-Whitney test.
aSignificant at p < 0.05.
Discussion
Acute theophylline poisoning can cause consequences that need ICU admission and MV. Emergency physicians should be able to expect the need for ICU admission and MV in acute theophylline-poisoned patients.8 Several clinical scores were studied to predict the need for MV and/or ICU admission and mortality in medical and poisoning conditions.13,19,25–28 However, the present study was the first to evaluate different scoring systems to predict the need for MV and/or ICU admission in acute theophylline poisoning.
Our main findings revealed that the REMS, MEWS and SCS were simple, rapid, reliable, and effective scores that do not need sophisticated steps at the time of admission of acute theophylline-poisoned patients. The SCS was the best early predictor of the need for ICU admission. Furthermore, MEWS was a practical and simple predictive score for the need for MV.
The Socio-demographic, toxicological and clinical data in the current study agreed with data collected by similar studies in Egypt and worldwide.4,9,29–31
In the present study, the incidence of ICU admission was 24.1%, while patients who needed MV were only 3.4% of acute theophylline-poisoned patients. These results were in line with Abuelfadl et al.4 and Elhawary et al.,5 who reported that 28.57% and 16.7% of patients with acute theophylline toxicity were admitted to ICU respectively.
On the other hand, khalifa and Lashin9 and Abdelwahab and Hussien32 documented that the incidence of ICU admission among acute theophylline-poisoned patients was 9.1% and 4.6%, respectively. However, this difference in the incidence of ICU admission could be explained by the difference in the severity of poisoning among patients in each study.
All the median scores were significantly elevated in patients who needed MV and ICU admission compared to those who did not need MV and ICU admission. Hence, these scoring systems might have a potential role in predicting the need for MV and/or ICU admission. This was in line with El-Sarnagawy and Hafez,27 who recorded that REMS values were significantly higher among mechanically ventilated patients in acutely poisoned patients with drug overdoses. Moreover, Shahin and Hafez21 reported that the median REMS, MEWS, and SCS were higher in mechanically ventilated patients and non-survivors than those who did not need MV and survivors in anticholinesterase pesticide poisoning.
In the current study, ROC curves evaluated the scores’ accuracy as predictors for the need for MV and/or ICU admission in acute theophylline-poisoned patients. Regarding the condition for ICU admission, the SCS had the strongest predictive values for ICU admission with a 91.4% accuracy level. Its AUC was (0.96) at cut-off ˃7 with the highest PPV (76.5%) and specificity (90.9%).
The SCS had already been validated externally25 with a fair level of precision and excellent discrimination for predicting mortality. Furthermore, Li et al.33 used SCS as a risk stratification tool that aids ICU management plans. Despite the dearth of studies examining them in poisoned patients, the SCS was considered a highly accurate outcome predictor in clinical settings. Previous studies have assessed surgical and medical patients presented to the emergency room that is not specific to cases in toxicology. Additionally, researchers were concerned with using of SCS to predict mortality rather than assessing the likelihood of MV and ICU admission.
In this study, the involved parameters of SCS could be the reason for its effectiveness. Age and abnormal ECG are the main constituents of the SCS. Acute theophylline-poisoned patients with underlying severe cardiac disorders and those aged more than 60 years old and children aged less than three years old are more likely to have life-threatening theophylline poisoning.34 Thus, SCS was effective in the prediction of ICU admission among acute theophylline-poisoned patients.
Meanwhile, the MEWS and REMS could have been less accurate in the early prediction of ICU admission compared to SCS. It could be attributed to the fact that MEWS and REMS do not depend on the ECG in their calculations.14,24 While cardiac manifestations and abnormal ECG changes are common clinical findings in acute theophylline poisoning35,36 On the other hand, El-Sarnagawy et al.19 showed that the MEWS was easy and capable of predicting ICU admission for patients with organophosphorus poisoning.
For early prediction of the need for MV, the MEWS recorded the best discriminatory power, followed by SCS and REMS, with no significant differences. The MEWS had the best AUC (0.996) with a cut-off value >8, 100% sensitivity and 98.2% specificity. It had the highest accuracy level, PPV and specificity for prediction of the MV than other scores. In the current study, MEWS’s positive predictive value and cut-off level were higher than previous studies.37,38 In accordance, Helmy et al.17 supposed MEWS was a valuable scoring system for the prediction of MV in organophosphate-poisoned patients (AUC was 0.927 at a 2.5 cut-off value with an 88.64% accuracy level). Moreover, Elhawary and Sagah20 detected that the AUC of MEWS was 0.923 with a cut-off value ˃4 for MV prediction among carbon monoxide-poisoned patients.
In the current study, two patients were mechanically ventilated. Early MV protected the airway and enabled the successful delivery of enteral charcoal in patients whose vomiting persists despite using an anti-emetic and a nasogastric tube.39 The MEWS score depends mainly on the vital signs and neurological assessment by the AVPU scale.24 The adopted scores’ discriminatory power can be attributed to their constituents. Thus, the MEWS was an effective predictor of MV compared to REMS and SCS.
Regarding SCS as predictors for MV, it had AUC (0.982) with a cut-off value >11, 100% sensitivity and 96.4% specificity. Elhawary and Sagah20 recorded that SCS at a cut-off value >9 with a specificity of 100% was a good predictor for MV requirement in carbon monoxide poisoning. Moreover, Shahin and Hafez21 registered that SCS at cut-off >3 was an effective predictor tool for MV in anticholinesterase poisoning. The SCS was less effective than the MEWS score for predicting the need for MV early.
The REMS is a clinical score that does not require laboratory parameters, staff training or extra skills.40,41 The AUC of REMS was 0.772 for predicting geriatric ICU admission with a cut-off level >7.26 In the emergency department, the REMS was an accurate score for the prediction of non-surgical patients’ outcomes.42 In a multicenter study, Bulut et al.43 reported that the AUC of REMS was superior to MEWS in predicting hospitalization and mortality of emergency medical and surgical patients.
In the current study, REMS was the least effective score compared to the SCS and MEWS for predicting both the ICU admission and MV, respectively. The REMS score was evaluated in different poisoning conditions with reliable findings. El-Sarnagawy and Hafez27 reported that REMS had good overall accuracy in predicting the need for ICU admission and MV in poisoned patients. Elhawary and Sagah20 found that REMS at a cut-off value >4 was a good predictor for MV among carbon monoxide-poisoned patients. Lashin and Sharif44 reported that REMS had a comparable discrimination power of ICU admission and MV with MEWS in acute clozapine poisoning. Different types of poisoning and clinical conditions could explain these contradictory findings.
As the lack of using different scoring systems for early prediction of the need for ICU admission and MV in acute theophylline-poisoned patients, it could be helpful for residents to utilize SCS, MEWS and REMS scores. Hence, the need for ICU admission and MV would be controlled, saving hospital resources.
Limitation
This cross-sectional study was performed on a small number of patients. However, our results may pave the way for a more extensive multicenter study recruiting many patients. Moreover, it is preferable that we measure theophylline serum concentrations in theophylline poisoning patients. This approach is pricey and not usually accessible in many hospitals.
Conclusion
The REMS, SCS and MEWS are simple, applicable, and effective scores that do not need sophisticated steps at admission. We recommend using SCS as an early predictor for ICU admission in acute theophylline-poisoned patients. Furthermore, MEWS can effectively predict MV requirements in acute theophylline-poisoned patients.
Contributor Information
Ghada Attia Sagah, Forensic Medicine and Clinical Toxicology Department, Faculty of Medicine, Medical collages complex, 6 th Floor, Al-Geish Street, Tanta University, Tanta, Elgharbya 31527, Egypt.
Alshaimma Mahmoud Elmansy, Forensic Medicine and Clinical Toxicology Department, Faculty of Medicine, Medical collages complex, 6 th Floor, Al-Geish Street, Tanta University, Tanta, Elgharbya 31527, Egypt.
Acknowledgments
Authors extend their appreciation to Tanta University Poison Control Center (TUPCC) for facilitating this work.
Author contributions
Both authors contributed equally to the study. The corresponding author is responsible for communication during and after the manuscript submission.
Funding
There was no funding support to this research.
Conflict of interest statement. None declared.
Data availability
The corresponding author will provide data sets collected and used in the current work upon reasonable request.
References
- 1. Henriksen DP, Davidsen JR, Laursen CB. Nationwide use of theophylline among adults-a 20-year danish drug utilisation study. Respir Med. 2018:140:57–62. [DOI] [PubMed] [Google Scholar]
- 2. Kapoor S, Thakkar J, Aggarwal V. Theophylline toxicity leading to suicidal ideation in a patient with no prior psychiatric illness. SAGE Open Med Case Rep. 2015:3:2050313X15583208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hocaoğlu N, Yıldıztepe E, Bayram B, Aydın B, Tunçok Y, Kalkan Ş. Demographic and clinical characteristics of theophylline exposures between 1993 and 2011. Balkan Med J. 2014:31(4):322–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Abuelfadl AA, Shahin MM, Alghazaly GM. Ecg changes as predictor of mortality and major outcome events in theophylline acutely intoxicated patients. MJFMCT. 2017:25(1):15–26. [Google Scholar]
- 5. Elhawary A, Elgazzar F, El-Ebiary A. Predictors of acute theophylline toxicity outcomes. MJFMCT. 2015:23(1):29–49. [Google Scholar]
- 6. Ellis EF, Koysooko R, Levy G. Pharmacokinetics of theophylline in children with asthma. Pediatrics. 1976:58(4):542–547. [PubMed] [Google Scholar]
- 7. Singh N, Shreshtha AK, Thakur MS, Patra S. Xanthine scaffold: scope and potential in drug development. Heliyon. 2018:4(10):e00829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Greene SC, Halmer T, Carey JM, Rissmiller BJ, Musick MA. Theophylline toxicity: an old poisoning for a new generation of physicians. Turk J Emerg Med. 2018:18(1):37–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khalifa H, Lashin H. Predictors for intensive care unit admission in acute theophylline intoxicated patients. Ain Shams J Forensic Med Clin Toxicol. 2018:31(2):77–86. [Google Scholar]
- 10. Oprita B, Aignatoaie B, Gabor-Postole DA. Scores and scales used in emergency medicine. Practicability in toxicology. J Med Life. 2014:7(Spec Iss 3):4–7. [PMC free article] [PubMed] [Google Scholar]
- 11. Kornbluth J, Bhardwaj A. Evaluation of coma: a critical appraisal of popular scoring systems. Neurocrit Care. 2011:14(1):134–143. [DOI] [PubMed] [Google Scholar]
- 12. Schwarz ES, Kopec KT, Wiegand TJ, Wax PM, Brent J. Should we be using the poisoning severity score? J Med Toxicol. 2017:13(2):135–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Valiollahzadeh S, Ostadi A, Rahmani F. Predictive value of national early warning score and modified early warning score in outcome of patients with poisoning: prediction of mortality in suicide patients. Int J Med Toxicol Forensic Med. 2022:12(4):38299. [Google Scholar]
- 14. Olsson T, Terent A, Lind L. Rapid emergency medicine score: a new prognostic tool for in-hospital mortality in nonsurgical emergency department patients. J Intern Med. 2004:255(5):579–587. [DOI] [PubMed] [Google Scholar]
- 15. Hu H, Yao N, Qiu Y. Comparing rapid scoring systems in mortality prediction of critically ill patients with novel coronavirus disease. Acad Emerg Med Off J Soc Acad Emerg Med. 2020:27(6):461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yu M, Huang B, Liu P, Wang A, Ding W, Zhai Y, Huang Y, Zhong Y, Jian Z, Huang H, et al. . Detection of deteriorating patients after whipple surgery by a modified early warning score (mews). Ann Transl Med. 2019:7(20):574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Helmy M, Farahat AMA, Ismael M, Mahmoud S, Ghanem AA. Assessment of acute physiology and chronic health evaluation, modified early warning and worthing physiological scores as predictor for mechanical ventilation in acute organophosphorus toxicity patients. MJFMCT. 2022:30:17–27. [Google Scholar]
- 18. Subbe CP, Jishi F, Hibbs RA. The simple clinical score: a tool for benchmarking of emergency admissions in acute internal medicine. Clin Med (Lond). 2010:10(4):352–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. el-Sarnagawy GN, Abdelnoor AA, Abuelfadl AA, el-Mehallawi IH. Comparison between various scoring systems in predicting the need for intensive care unit admission of acute pesticide-poisoned patients. Environ Sci Pollut Res. 2022:29(23):33999–34009. [DOI] [PubMed] [Google Scholar]
- 20. Elhawary A, Sagah G. Evaluation of various scoring systems in prediction of acute carbon monoxide poisoning outcome. Ain Shams J Forensic Med Clin Toxicol. 2022:38(1):79–86. [Google Scholar]
- 21. Shahin M, Hafez A. Comparison of different scoring systems in poisoning with cholinesterase inhibitors. MJFMCT. 2020:28:25–42. [Google Scholar]
- 22. Shannon M. Predictors of major toxicity after theophylline overdose. Ann Intern Med. 1993:119(12):1161–1167. [DOI] [PubMed] [Google Scholar]
- 23. Geib A-J. Theophylline and other methylxanthines. In: Brent J, Burkhart K, Dargan PI, et al., editors. Critical care toxicology: diagnosis and management of the critically poisoned patient. 2nd ed. Cham: Springer International Publishing, Imprint Springer; 2019. pp. 883–890 [Google Scholar]
- 24. Chang SH, Hsieh CH, Weng YM, Hsieh MS, Goh ZNL, Chen HY, Chang T, Ng CJ, Seak JC, Seak CK, et al. . Performance assessment of the mortality in emergency department sepsis score, modified early warning score, rapid emergency medicine score, and rapid acute physiology score in predicting survival outcomes of adult renal abscess patients in the emergency department. Biomed Res Int. 2018:2018:6983568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stræde M, Brabrand M. External validation of the simple clinical score and the hotel score, two scores for predicting short-term mortality after admission to an acute medical unit. PLoS One. 2014:9(8):e105695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dundar ZD, Karamercan MA, Ergin M, Colak T, Tuncar A, Ayrancı K, Kocak S, Cander B. Rapid emergency medicine score and hotel score in geriatric patients admitted to the emergency department. Int J Gerontol. 2015:9(2):87–92. [Google Scholar]
- 27. el-Sarnagawy GN, Hafez AS. Comparison of different scores as predictors of mechanical ventilation in drug overdose patients. Hum Exp Toxicol. 2017:36(6):539–546. [DOI] [PubMed] [Google Scholar]
- 28. Abd Elghany S, Heshmat M, Oreby M, Elsarnagawy G. Evaluation of various scoring systems in prediction of acute aluminum phosphide (alp) poisoning outcome. Ain Shams J Forensic Med Clin Toxicol. 2018:30(1):117–127. [Google Scholar]
- 29. Hayes TM, Hayes E. Assessment of diabetic control: a comparison between home and clinic blood glucose levels. Diabetes Care. 1978:1(3):166–167. [DOI] [PubMed] [Google Scholar]
- 30. Hodeib AA, Ghonem MM. Troponine i versus creatinine kinase-mb as predictor markers of the severity and outcomes in acute theophylline toxicity. MJFMCT. 2019:27(2):57–72. [Google Scholar]
- 31. Naguib S, el Sayed A, el Helaly H, Said S. Retrospective study of acute theophylline intoxicated cases admitted to poison control center, Ain-Shams University Hospitals from January 2007 to December 2008. Ain Shams J Forensic Med Clin Toxicol. 2013:21(2):129–140. [Google Scholar]
- 32. Abdelwahab W, Hussien R. Construction of a predictive score for hemodialysis in acute theophylline intoxicated patients. MJFMCT. 2020:28:97–109. [Google Scholar]
- 33. Li JY, Yong TY, Hakendorf P, Roberts S, O'Brien L, Sharma Y, Ben-Tovim D, Thompson CH. Simple clinical score is associated with mortality and length of stay of acute general medical admissions to an australian hospital. Intern Med J. 2012:42(2):160–165. [DOI] [PubMed] [Google Scholar]
- 34. Visitsunthorn N, Punnakan L. Theophylline toxicity in thai children. Asian Pac J Allergy Immunol. 2001:19:177–182. [PubMed] [Google Scholar]
- 35. Sessler CN, Cohen MD. Cardiac arrhythmias during theophylline toxicity. A prospective continuous electrocardiographic study. Chest. 1990:98(3):672–678. [DOI] [PubMed] [Google Scholar]
- 36. Amin S, el Seidy A, Hammad S, Habib N. Relation between theophylline serum level with ecg changes and poison severity score (pss) among some theophylline intoxicated patients in menofia poison control center (mpcc) a prospective study. Ain Shams J Forensic Med Clin Toxicol. 2013:20(1):170–179. [Google Scholar]
- 37. Wei X, Ma H, Liu R, Zhao Y. Comparing the effectiveness of three scoring systems in predicting adult patient outcomes in the emergency department. Medicine. 2019:98(5):e14289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gök RGY, Gök A, Bulut M. Assessing prognosis with modified early warning score, rapid emergency medicine score and worthing physiological scoring system in patients admitted to intensive care unit from emergency department. Int Emerg Nurs. 2019:43:9–14. [DOI] [PubMed] [Google Scholar]
- 39. Henderson A, Wright DM, Pond SM. Management of theophylline overdose patients in the intensive care unit. Anaesth Intensive Care. 1992:20(1):56–62. [DOI] [PubMed] [Google Scholar]
- 40. Bidari A, Talachian E. Rapid emergency medicine score (rems) as a predictor of early mortality in the setting of emergency department. Iran J Med Sci. 2022:47(2):81–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ruangsomboon O, Boonmee P, Limsuwat C, Chakorn T, Monsomboon A. The utility of the rapid emergency medicine score (rems) compared with sirs, qsofa and news for predicting in-hospital mortality among patients with suspicion of sepsis in an emergency department. BMC Emerg Med. 2021:21(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ghaffarzad A, Vahed N, Shams Vahdati S, Ala A, Jalali M. The accuracy of rapid emergency medicine score in predicting mortality in non-surgical patients: a systematic review and meta-analysis. Iran J Med Sci. 2022:47(2):83–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bulut M, Cebicci H, Sigirli D, Sak A, Durmus O, Top AA, Kaya S, Uz K. The comparison of modified early warning score with rapid emergency medicine score: a prospective multicentre observational cohort study on medical and surgical patients presenting to emergency department. Emerg Med J. 2014:31(6):476–481. [DOI] [PubMed] [Google Scholar]
- 44. Lashin HI, Sharif AF. Evaluation of various scoring systems as predictors of the need for intensive care unit admission and other adverse outcomes among patients with acute clozapine poisoning. Toxicol Res (Camb). 2023:12(3):468–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The corresponding author will provide data sets collected and used in the current work upon reasonable request.


