Abstract
To ensure care continuity during the COVID-19 pandemic, telehealth has been widely implemented in human immunodeficiency virus (HIV) care. However, participation in and benefits from telehealth were unequal. This study aims to assess the willingness of people living with HIV (PWH) and HIV care providers to use telehealth and perceptions of the future role of telehealth. In-depth interviews with 18 PWH and 10 HIV care providers from South Carolina assessed their willingness to use telehealth, their perspectives on the future of telehealth in HIV care, and recommendations to improve telehealth. Interviews were analyzed using thematic analysis. Most PWH were female (61%), Black/African American (67%), and non-Hispanic (78%). Most PWH (61%) and all providers had used telehealth for HIV care. Most PWH and all providers reported being willing to use or (re-)consider telehealth HIV care services in the future. Providers suggested that telehealth is most suitable for routine HIV care encounters and for established, clinically stable, generally healthy PWH. Attitudes toward telehealth were heterogeneous, with most interviewees valuing telehealth similarly or superior to in-person care, yet >20% perceiving it less valuable. Recommendations to improve telehealth included multilevel strategies to address challenges across four domains: technology, the virtual nature of telehealth, administrative processes, and the sociodemographic profile of PWH. Telehealth in HIV care is here to stay; however, it may not yet be suitable for all PWH and all care encounters. Decision processes related to telehealth versus in-person care need to involve providers and PWH. Existing telehealth options require multilevel adjustments addressing persistent challenges.
Keywords: HIV care services, telehealth, COVID-19, qualitative study, South Carolina
Introduction
During the COVID-19 pandemic, people living with HIV (PWH) faced human immunodeficiency virus (HIV) care interruptions due to clinic closures and social distancing ordinances. For example, in South Carolina (SC), partial or complete HIV care interruption was reported at more than 80% of Ryan White-funded HIV clinics.1 Fragmented and interrupted HIV care jeopardizes the benefits of antiretroviral treatment (ART) and could result in increased HIV-related comorbidities, increased transmission risk, and reduced life expectancy.2–6
To mitigate HIV care interruptions, temporary policy changes facilitated a swift implementation of telehealth for HIV care during the pandemic.7–13
Benefits of telehealth included reduced barriers to HIV care such as transportation or stigma,11,13,14 limited COVID-19 exposure,11,13 and the increased convenience of receiving care at home.9,11,13–15 The Kaiser Family Foundation reported that almost all Ryan White-funded HIV care providers across the United States offered telehealth during the pandemic.16
Despite the widespread implementation of telehealth HIV care services, not everyone was participating in and benefiting from telehealth equally. PWH who experienced housing instability, belonged to historically marginalized racial and ethnic groups, having a substance use history, living in deprived areas, were older, non-native English speakers, or uninsured engaged in fewer telehealth encounters or experienced more challenges with telehealth.8,16–21 To better understand and mitigate these disparities, it is critical to understand telehealth-related decision making, assess providers' and PWHs willingness to use telehealth, and develop strategies to meet their needs.
The implementation of telehealth in HIV care during the pandemic encountered barriers at multiple levels. Individual-level barriers that impacted both PWH and HIV care providers included security concerns, unfamiliarity with virtual visits, difficulties navigating telehealth, and lack of laboratory information or physical exams.9,12,14–17,22–28 Patient-specific barriers further comprised the lack of access to technology, a stable and sufficient internet connection, a private space, digital literacy, and adequate online communication skills.9,11,14–17,22–24,27–31 Social context-level factors included “unequal access to or ability to engage in care using technological means” (i.e., digital divide),16,23 sociodemographic characteristics of PWH such as income and education, health inequalities experienced by PWH, and social distancing and shelter-in-place ordinances.13,15–17,22–24,29,30 Administrative and regulatory barriers included increased administrative burden for HIV care providers, reimbursement issues, and missed appointments.12,13,16,22,24
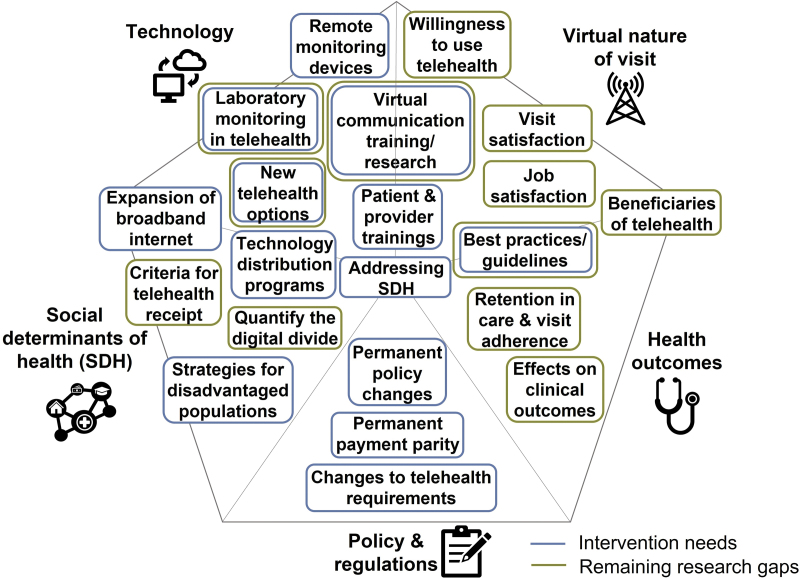
Literature describing telehealth in HIV care during COVID-19 in the Southern United States11–13,17,22,23,32–38 was used to build a telehealth barrier and intervention needs framework (Fig. 1)39 that can be used to guide telehealth research and development. Telehealth barriers were categorized into four domains: technology-related barriers, virtual nature of HIV care visits, policies and regulations, and social determinants of health (SDH). Notably, SDH were reported to amplify other barriers to telehealth HIV care such as limited access to technology, lack of rural connectivity, low digital literacy, and feeling uncomfortable with virtual visits.
FIG. 1.
Barrier and intervention needs framework for telehealth in HIV care. Implementation and access barrier to telehealth domains are: technology, virtual nature of HIV care visit, policies and regulations, and SDH. The health outcomes domain was added to map related research gaps and intervention needs. Intervention needs and remaining research gaps may address multiple barrier domains. HIV, human immunodeficiency virus; SDH, social determinants of health. Reproduced from Yelverton et al.39
To effectively address reported telehealth access and uptake barriers, it is crucial to understand PWH and HIV care provider perspectives on the future of telehealth in HIV care and develop tailored telehealth HIV care strategies.
This study's objective is to assess the willingness of PWH and HIV care providers to use telehealth, their perceptions of the role of telehealth in HIV care in the future, and strategies to address telehealth barriers and intervention needs. This study further assessed the perceived value of and attitudes toward telehealth to inform future telehealth decision making and improvements.
Methods
Ethics statement
The study protocol was determined to be exempt from review by the Institutional Review Board at the HIV care providing institution (#1883275). All interviewees consented verbally to participate in in-depth interviews.
Study design and rationale
This study utilized a qualitative study design following a grounded theory approach to assess PWHs and HIV care providers' willingness to use telehealth and their perspectives on the role of telehealth in HIV care in the future. In-depth interviews featuring open-ended question formats were used to collect qualitative data. A quantitative supplemental survey assessed sociodemographic characteristics and measured participants' perceived value of and attitudes toward telehealth. Data analysis and article preparation followed the Standards for Reporting Qualitative Research guidelines.40
Context
The South is the epicenter of the HIV epidemic in the United States, and SC is one of the priority jurisdictions for the End the HIV Epidemic campaign targeting high HIV transmission areas.41 SC ranked among the top 10 states with the highest rates of HIV diagnoses in 2019,42 with a disproportionate burden of HIV among historically marginalized racial and ethnic groups, and people living in rural areas.41,43–47
Study participants, recruitment, and compensation
The study included PWH receiving care from a large HIV clinic in SC and HIV care providers at the same clinic, which serves ∼2400 PWH across 8 counties in SC. PWH were eligible to participate if they were (1) 18 years or older, (2) living with HIV, (3) prescribed ART medication, and (4) received HIV care at the clinic in the year before or during the COVID-19 pandemic. Telehealth use was not an eligibility criterion to capture perspectives on telehealth among people with varying telehealth experiences, including PWH with no telehealth experience. Participants were selected following a stratified purposeful sampling strategy to ensure racial, ethnic, and geographic diversity in PWH participants.48 The target sample composition included at least 25% male PWH, at least 25% female PWH, at least 25% non-Hispanic White PWH, at least 25% people of color who are living with HIV, and at least 25% rural PWH. PWH were identified through a combination of provider referrals, snowball sampling, and study flyers, which were posted in waiting areas of the HIV clinic. HIV care providers and clinic staff assisted with recruitment by distributing information and handouts about the study. Patient participants were compensated with a $30 gift card.
HIV care providers were purposively selected and eligible if they (1) were nontrainee health care providers, and (2) regularly cared for PWH. Providers were recruited in staff meetings and through snowball referrals. In compliance with their institutional policies, providers did not receive compensation for participation.
The sample size was guided by saturation. Interviewers discussed newly introduced themes regularly and determined data saturation once interviews did not introduce any new themes. Prior evidence suggests that data saturation can occur within 12 interviews with primary themes arising as early as 6 interviews in qualitative interviews.49
Study instruments
Semistructured interview guides were developed based on the literature9,14,15,22 and with input from HIV care providers on the study team. Interview guides explored PWHs and HIV care providers' willingness to use telehealth and their perspectives on telehealth in HIV care in the future. To ensure appropriate question content and clear language, separate interview guides were used for PWH and provider participants. Both interview guides were reviewed by experienced HIV care providers in the study team. Interviews were guided by questions formulated in the interview guides and allowed for tailored follow-up questions based on interviewee responses. PWH were asked questions such as: “Thinking of the time after the pandemic, would you want to try/continue receiving HIV care services by phone or using video?” and “What could be done to improve HIV care services by phone or using video?.” Providers were asked questions such as: “Thinking of the time after the pandemic, what role do you see for telehealth in HIV care?.”
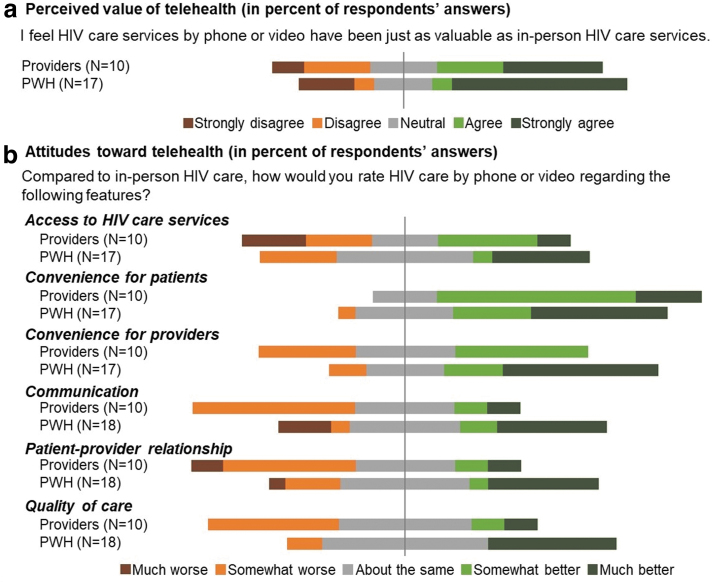
The short quantitative supplemental survey assessed basic sociodemographic characteristics, clinical characteristics (patient version only), work history (provider version only), telehealth utilization, and confidence using digital devices.50 To assess interviewee's perceived value of telehealth, interviewees were asked to respond to the statement, “I feel HIV care services by phone or video have been just as valuable as in-person HIV care services” (answer options were strongly agree, agree, neutral, disagree, strongly disagree, prefer not to answer). To assess interviewee's attitudes toward telehealth, they were asked “Compared to in-person HIV care, how would you rate HIV care by phone or video regarding the following features?” Features included access to HIV care services, convenience for patients, convenience for providers, communication, patient–provider relationship, and quality of care. Response options included: much better, somewhat better, about the same, somewhat worse, much worse, or prefer not to answer.
Implementation and data processing
Most interviews were conducted in-person in a private room at the HIV clinic (24 out of 28 interviews) and 4 PWH interviews were conducted virtually through teleconferencing software following the interviewee's choice. Interviewers and participants did not have a prior relationship. Interviews lasted about 1 h on average. With consent, all interviews were audio recorded. Recordings were transcribed verbatim using Microsoft's 365 Word online version (Microsoft Corporation, Redmond, WA), reread, and corrected if necessary to ensure data accuracy. Names and other identifying information were removed from the transcripts to protect interviewees' identities.
Provider and PWH interviews were analyzed separately. All transcripts were coded line by line in NVivo (released in March 2020; QSR International, Burlington, MA),51 using initial codebooks with predeveloped structural coding categories and subcategories based on the interview guide. Initial codebooks were subsequently expanded by adding new codes that emerged during the coding process. Two members of the research team independently coded each interview. Inter-rater reliability was assessed using Cohen's kappa scores and percentage agreement. Disagreements and differences in coding strategy were resolved in discussion. The final average kappa scores were 0.76 for provider interviews and 0.82 for PWH interview coding, indicating substantial agreement beyond chance.52 The percentage of agreement was high (95.1% agreement for provider interviews; 97.4% for interviews with PWH).
Data analysis
To explore and synthesize constructs within the main domains of interest, data analysis followed a thematic analysis approach.53 We identified themes and subthemes by grouping and categorizing the codes. To map recommended telehealth improvements, we used the telehealth barrier framework described in the introduction,39 with four domains of barriers to telehealth: (1) technology, (2) virtual nature of HIV care visits, (3) administrative processes, and (4) SDH. Results are accompanied by selected representative, verbatim quotes to illustrate key findings. Quotes illustrate the essence of the reported findings and not the frequency with which they were mentioned by interviewees. Quotes were edited for clarity, for example, by removing repeated words or nonlexical utterances. Supplemental survey data were analyzed using descriptive statistics in Stata (Version 16; StataCorp, College Station, TX).
Results
Sample characteristics
We conducted 28 interviews with 18 PWH and 10 HIV care providers. Most PWH were female (61.1%), Black or African American (66.7%), and not of Hispanic or Latinx descent (77.8%), with a mean age of 52 years [standard deviation (SD) = 9.8; Table 1]. The majority lived in an urban area (77.8%) and had public health insurance (61.1%). PWH had been living with HIV for a mean of 19.4 years (SD = 9.8). Most PWH felt very (50%) or somewhat confident (22.2%) in using technology to meet their needs online.
Table 1.
Sample Characteristics
| Characteristic | People living with HIV (N = 18), N (%) | HIV care providers (N = 10), N (%) |
|---|---|---|
| Gender | ||
| Female (vs. male) | 11 (61.11) | 7 (70) |
| Age, years | ||
| Mean (SD) | 52 (9.82) | 43.3 (8.92) |
| Race | ||
| Black or African American | 12 (66.67) | 3 (30) |
| White | 4 (22.22) | 5 (50) |
| Asian | — | 1 (10) |
| Mixed race | 1 (5.56) | — |
| Prefer not to answer | 1 (5.56) | 1 (10) |
| Ethnicity | ||
| Hispanic or Latinx | 1 (5.56) | — |
| Not Hispanic or Latinx | 14 (77.78) | 9 (90) |
| Prefer not to answer | 3 (16.67) | 1 (10) |
| Sexual orientation | ||
| Gay or lesbian | 6 (33.33) | n/a |
| Straight (or heterosexual) | 11 (61.11) | |
| Prefer not to answer | 1 (5.56) | |
| Place of residence | ||
| Urban (vs. rural) | 14 (77.78) | n/a |
| Education | ||
| Less than high school | 2 (11.11) | n/a |
| Highschool diploma or GED | 9 (50) | |
| Some college | 1 (5.56) | |
| Any college degree or higher | 6 (33.33) | |
| Health insurancea | ||
| AIDS Drug Assistance Program | 7 (38.89) | n/a |
| Public insurance | 11 (61.11) | |
| Private insurance | 5 (27.78) | |
| No insurance | 1 (5.56) | |
| Time since HIV diagnosis, years | ||
| Mean (SD) | 19.4 (9.77) | n/a |
| Health status at the day of the interview | ||
| 0–100 (best health), mean (SD) | 82.72 (19.12) | n/a |
| Work experience, years | ||
| Mean (SD) | n/a | 14.65 (10.13) |
| Technological confidence | ||
| Not at all confident | 2 (11.11) | — |
| Only a little confident | 3 (16.67) | — |
| Somewhat confident | 4 (22.22) | 2 (20) |
| Very confident | 9 (50) | 8 (80) |
Multiple responses possible.
GED, General Educational Development Test; HIV, human immunodeficiency virus; n/a, not applicable; SD, standard deviation.
Most HIV care providers were female (70%), White (50%), and not of Hispanic or Latinx descent (90%), with a mean age of 43.3 years (SD = 8.9). Provider participants had a mean work experience in HIV care of 14.7 years (SD = 10.1). All providers felt very (80%) or somewhat confident (20%) in using technology to meet their needs online.
Use of telehealth in HIV care
Telehealth in HIV care during the COVID-19 pandemic underwent several stages. Providers described that they provided most telehealth HIV care visits between March and September of 2020, when public health measures limited in-person patient care, and that those services reverted to more in-person care after this initial phase of the pandemic. While in-person care never stopped entirely at the HIV clinic, preventative measures were implemented, and nonurgent visits were rescheduled or provided through telehealth. One provider explained,
“The pandemic didn't stop people from living. And so, it changed the way how they had to do things by wearing a mask and staying separated, however, care continued. Care will not stop because of a pandemic, and so people need to realize with telehealth that care was continued, and patients continued to receive care” (Provider interview #010).
Among our interviewees, most PWH (61.1%) used telehealth for HIV care during the COVID-19 pandemic. Of the remaining PWH, 27.8% reported that telehealth was never offered or discussed and 11.1% reported that they refused to do telehealth. All providers had some experience with telehealth in HIV care; however, the intensity varied. While most providers reported frequent telehealth encounters, some providers reported having fewer than five telehealth encounters.
Perceived value of telehealth
There was heterogeneity in the perceived value of telehealth. Most interviewees (58.8% of PWH and 50% of providers) agreed or strongly agreed that telehealth was as valuable as in-person HIV care. Yet, almost one in four PWH (23.5%) and almost one in three providers (30%) disagreed or strongly disagreed with the comparability of value between visit types (Fig. 2).
FIG. 2.
PWHs' and HIV care providers' perceived value of and attitudes toward telehealth. HIV, human immunodeficiency virus, PWH, people living with HIV.
Several differences emerged between PWH and provider ratings of the value of telehealth. Both groups were split on the value of telehealth for improving access to HIV care and its convenience for patients. PWH rated the convenience for providers higher than providers (64.7% of PWH vs. 40% of providers responded with much or somewhat better). Around 44.4% of PWH versus 20% of providers responded that communication through telehealth was much or somewhat better than in in-person care, whereas 22.3% of PWH and 50% of providers rated communication to be much or somewhat worse in telehealth. Similar heterogeneity was observed regarding the patient–provider relationship and quality of care. While almost two in five PWH (38.9%) and only one in five providers (20%) perceived the relationship much or somewhat better in telehealth, 22.3% of PWH and 50% of providers perceived it much or somewhat worse.
While most respondents (50% of PWH and 40% of providers) perceived the quality of care in telehealth as comparable to in-person care, PWH rated the quality of care higher than providers: 38.8% of PWH versus 20% of providers rated it much or somewhat better; 11.1% of PWH and 40% of providers perceived it as somewhat worse.
Willingness to use telehealth and the future role of telehealth in HIV care
PWH's willingness to use or consider telehealth in HIV care in the future varied. While few PWH reported that they prefer telehealth, many PWH perceived it as an option when in-person care is not possible. One person explained,
“If I didn't have transportation or if I broke my foot or broke my leg and I couldn't drive to an appointment, telehealth would be very, very beneficial. So, I think it's something that is and can be beneficial and can continue to be beneficial in the future” (PWH interview #104).
Other PWH were not interested in using telehealth in the future as one person said, “I don't have it. […] It's like, it's good to, you know, to have that interaction in the same room, so you know you can talk” (PWH interview #106). Another person shared, “I don't think anything would make me [want to] use it. I like to see my doctor because he can look at you and tell if something is wrong” (PWH interview #113).
All providers reported being willing to continue or revisit telehealth HIV care services in the future. Many believed that telehealth in HIV care will increase or continue in the future as one provider said, “I think the bells been rung. I think that once you ring the bell, it's hard to unring it” (Provider interview #008). To guide successful telehealth in HIV care, providers suggested that telehealth may be most beneficial when used as a care complement rather than a substitute for in-person care. One provider said that they
“see telehealth really being a good instrument when someone is used to seeing their doctor every six months because they have pretty significant issues, and they might need that three-month follow-up or something in between to get them through. I think that's where it's going to have its most utility” (Provider interview #008).
Other providers suggested alternating telehealth and in-person care. One provider explained,
“If they're a stable HIV patient and I know they're adherent with their HIV medication. I don't mind doing a telehealth visit, you know, once a year. But I definitely want to see them in person, at least once a year. Just to make sure you know everything is OK” (Provider interview #007).
Telehealth improvements
Recommendations to improve telehealth in HIV care were organized by the telehealth barriers framework39 and addressed barriers related to (1) technology, (2) the virtual nature of HIV care visits, (3) administrative processes, and (4) the SDH.
Strategies to address technological barriers
PWH and providers recommended user-friendly telehealth platforms and telehealth training to address technological barriers. One person living with HIV recommended, “Make your platform that you're [going to] use more friendly usable, so that even the little child know how to do it. OK? Take the kinks out of it” (PWH interview #102). Another person explained the need for hands-on training to navigate telehealth and technology,
“Honey, I'm 59, I graduated high school in 79, OK? So, you see that gap? Thank you. But now they do telehealth. […] You can send me the instructions but I'm a visual learner. You understand what I'm saying? I'm a visual learner I can read it, but I still don't get it” (PWH interview #105).
A provider explained that they needed “someone [to] actually sit down with me and to go through the process. I think that's a big one. And actually show, walk me through the process instead of sending bits and pieces through emails” (Provider interview #005). Providers further suggested technological support and an enhanced telehealth setup at the HIV clinic. One provider explained,
“If there were stations like this [tablet name] where you can just click on the patient name and connect with them, that would be easy, but trying to expect people to know which software to use on the computer or on their handheld devices and how to do this securely and safely […] I don't think that's ideal in my opinion” (Provider interview #009).
Strategies to address barriers related to the virtual nature of telehealth
PWH requested to ensure that they can see their regular HIV care provider and that there is an option for multidisciplinary telehealth visits, including their case manager, nurse, mental health care providers, and other HIV care providers. One person explained,
“You [got to] bring all the team players in, like especially when it comes to healthcare. Make sure that all the doctors [are going to] participate, all the nurses, all the case managers that they know exactly what they're doing when they come online” (PWH interview #102).
To improve communication barriers, PWH suggested using language free of medical jargon as PWH may not know its meaning and offering language interpretation services for telehealth for PWH whose primary language is not English or PWH who have trouble hearing. PWH suggested incorporating nonhealth care-related conversations to build and maintain a personal provider–patient relationship. One person shared, “From my experience, at least let's get [an] opportunity to know each other first before you try to ask me my business. Let's get comfortable with each other, then let's get to know one [another]” (PWH interview #105). A provider recommended using technology such as remote monitoring devices and video connections to overcome challenges with physical exam components. They said, “You really can't do a full exam on the patient. Maybe my opinion [about telehealth] would change if I experienced the newer technology” (Provider interview #005).
Strategies to address administrative processes
A person living with HIV recommended implementing interim check-in calls to assess patient needs between scheduled visits. They described the benefits of having
“a liaison, such as someone is saying to call each patient on certain days just calling to see how you're doing. Do you need anything? Do you need to talk to somebody, you know? When is your next appointment, you know? Maybe I can squeeze you in sooner because you got this problem” (PWH interview #112).
Providers recommended streamlining telehealth processes and appointments;
“Different doctors use different versions and the set up for it is different. I guess having more consistency or a better way of communicating so that patients are set up and know how to use it [before their telehealth visit]. Cause that's the biggest issue I think we have” (Provider interview #002).
One provider suggested that it would be helpful to have guidance on identifying what visit type is most appropriate for each patient and visit.
Strategies to address barriers related to SDH
One person living with HIV recommended providing digital devices to PWH to support telehealth access. They stated,
“If they could provide devices […] some type of program, to where a person could even pick up a device or get it mailed to them when it's time for their appointment. But then you know just like leasing it and then be there like you go to the library, you can check out a book and you have it for a certain amount of time. I think that would be very, very beneficial for those that don't have access to a device to have a telehealth appointment” (PWH interview #104).
Discussion
Following the notion that Telehealth is here to stay,54,55 this study provided novel qualitative findings on PWH's and HIV care providers' perceptions of the future of telehealth in HIV care and which adjustments to improve telehealth options will be necessary to meet their needs.
Our findings indicate that the perceived value of and attitudes toward telehealth among and between PWH and HIV care providers are perceived heterogeneously, which is in line with other studies.26,56–58 While most interviewees perceived telehealth HIV care to be as valuable as in-person care, there were PWH and providers who perceived telehealth to be an inferior care modality. Notably, PWH rated the convenience for providers more positive than HIV care providers themselves, which highlights the need for shared decision making to adequately reflect the attitudes and preferences of all parties involved. As our study sample was small and results may not be generalizable beyond our sample, future research needs to assess systematic variation in the perceived value of and attitudes toward telehealth among and between PWH and HIV care providers to better guide tailored visit type allocation.
Interviewees expressed predominantly negative attitudes toward communication and the patient–provider relationship in telehealth HIV care, which echoes reported telehealth challenges related to communication difficulties and telehealth visits feeling impersonal.16,22,24,26,27,57 Recommendations to improve communication challenges included time for personal, nonhealth care-related conversation within telehealth visits, using language free of medical jargon, and offering language interpretation services for telehealth. Future research is needed to evaluate if communication barriers are specific to telehealth or occur in in-person care as well, and if the recommended strategies to improve communication and the patient–provider relationship can improve attitudes toward telehealth.
Providers were unanimously open to considering telehealth HIV care yet imposed limiting parameters for two telehealth dimensions. The first limiting parameter addressed the scope of telehealth HIV care services. Telehealth was described as a complimentary tool in the care of PWH. Interview findings underlined that, in its current form, telehealth cannot fully replace in-person HIV care visits. Innovative telehealth strategies such as remote monitoring devices and telehealth exam kits may be able to widen the perceived suitability of telehealth. The second limitation related to the patient population that was considered suitable for telehealth. Providers perceived telehealth to be suitable for established, stable, and generally healthy PWH. This consideration needs to be further investigated and included in HIV care visit type decisions to ensure adequate HIV care.
Study findings highlight varied willingness to use telehealth among PWH. While many PWH express some level of interest in telehealth for routine HIV care or when in-person care is inconvenient or impossible, others refuse telehealth HIV care services. These results are in line with other studies reporting that a substantial proportion of PWH were interested in continued telehealth HIV care encounters beyond the pandemic.24,27,58 Imbert et al. found that there are two distinctly different preference profiles among PWH. One group of PWH had a strong preference for seeing the same provider at each visit, while other PWH favor care flexibility in telehealth for HIV care.56 Further, research by Wong et al. highlights benefits of telehealth, such as privacy and convenience, for people facing or fearing stigma in response to seeking HIV care services.59 Future research is needed to identify candidates who are open to using telehealth and develop guidelines on including patients in the visit type decision process. Varied and conditional willingness to use telehealth in conjunction with heterogeneous perceptions of value and attitudes toward telehealth underline the well-established need for patient-centered approaches in HIV care.
Building on the proposed patient-centered differentiated service delivery (“DSD 2.0”) model,60 our findings suggest adding a potential new dimension of preference-concordant HIV care visit type to differentiated service delivery models.
In our study, we identified various recommendations to improve telehealth in HIV care. Recommendations addressed challenges related to technology, the virtual nature of telehealth visits, administrative processes, and SDH, suggesting the need for multilevel improvement strategies. Notably, only one interviewee suggested device distribution programs addressing the lack of access to technology. In our scoping review, we found that SDH were reported to amplify other telehealth barriers among PWH, including limited access to technology, lack of rural connectivity, and low digital literacy.39 Structural interventions promoting economic stability, digital literacy, and access to broadband internet for all PWH are needed to unfold the full potential of telehealth and to reduce HIV care inequalities.
There are several limitations to this study. First, there may be limited generalizability as this study focused on a small sample of PWH and HIV care providers from SC; however, data saturation for both PWH and HIV care provider interviews was reached. Second, our sampling quotas aiming to include at least 25% of PWH who are non-Hispanic White and at least 25% of PWH who live in rural areas were missed by 2.8% each. Further, most PWH participating in our study were female, while only 27% of PWH in SC are female.45 While we included a diverse sample of PWH in our study, perspectives of rural, non-Hispanic White, and male PWH may be underrepresented. Third, our study identified heterogeneous perceptions of willingness to use telehealth, the value of telehealth HIV care, and attitudes toward telehealth. Extending this work through the collection of quantitative survey data with a large and diverse sample of PWH and HIV care providers would be useful to examine the relationship between willingness to use telehealth, the perceived value of and attitudes toward telehealth, and sociodemographic and clinical characteristics.
In conclusion, telehealth in HIV care is here to stay yet not blankly suitable for all PWH and care encounters in its current form. Visit type decision processes need to be shared and patient centered, that is, it is crucial to involve PWH, and consider their preferences and health care needs. Existing telehealth options require multilevel adjustments to achieve high levels of visit and medication adherence and reduce inequalities.
Acknowledgments
The authors greatly appreciate the support from Christina Miller and her colleagues at the HIV clinic for their help with participant recruitment and organization of the interviews. The authors thank all interview participants for their time and insights.
Ethics Approval
The study protocol was determined to be exempt from review by the Institutional Review Board at the HIV care providing institution (#1883275).
Informed Consent
All interviewees consented verbally to participate in in-depth interviews.
Data, Materials, and/or Code Availability
Due to the qualitative nature of this research, participants of this study did not agree for their data to be shared publicly, therefore supporting data are not available.
Authors' Contributions
V.Y., J.O., S.W., C.D., and H.A. contributed to the study conception and design. Study instruments were developed by V.Y., J.O., S.W., C.D., N.N., N.L.H., B.O., O.O., S.Q., X.L., and H.A. Data collection and analysis were performed by V.Y., S.G., D.A., and C.C. The first draft of the article was written by V.Y. and all authors commented on previous versions of the article. All authors read and approved the final article.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Research reported in this publication was supported by the Agency for Healthcare Research and Quality (AHRQ) Grants for Health Services Research Dissertation Program (1R36HS029267), the 2022 Health Sciences Center at Prisma Health Research Seed Grant Program, the SPARC Graduate Research Program from the Office of the Vice President for Research at University of South Carolina, and the Student Opportunities for Academic Achievement Through Research (SOAR) program from the University of South Carolina School of Medicine Columbia. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, Prisma Health, and the University of South Carolina.
References
- 1. Qiao S, Li Z, Weissman S, et al. Disparity in HIV service interruption in the outbreak of COVID-19 in South Carolina. AIDS Behav 2021;25(1):49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. Behavioral and clinical characteristics of persons receiving medical care for HIV infection—Medical Monitoring Project, United States, 2015 Cycle. 2019. Available from: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-special-report-number-20.pdf [Last accessed: October 12, 2018].
- 3. Siddiqi AE, Hall HI, Hu X, et al. Population-based estimates of life expectancy after HIV diagnosis: United States 2008–2011. J Acquir Immune Defic Syndr 2016;72(2):230–236; doi: 10.1097/qai.0000000000000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jewell BL, Smith JA, Hallett TB. Understanding the impact of interruptions to HIV services during the COVID-19 pandemic: A modelling study. EClinicalMedicine 2020;26:100483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cornelius T, Jones M, Merly C, et al. Impact of food, housing, and transportation insecurity on ART adherence: A hierarchical resources approach. AIDS Care 2017;29(4):449–457; doi: 10.1080/09540121.2016.1258451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maqutu D, Zewotir T. Optimal HAART adherence over time and time interval between successive visits: their association and determinants. AIDS Care 2011;23(11):1417–1424; doi: 10.1080/09540121.2011.565028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weerasuria M, Ko C, Ehm A, et al. The impact of the COVID-19 pandemic on people living with HIV in Victoria, Australia. AIDS Res Hum Retroviruses 2021;37(4):322–328; doi: 10.1089/aid.2021.0007. [DOI] [PubMed] [Google Scholar]
- 8. Spinelli MA, Hickey MD, Glidden DV, et al. Viral suppression rates in a safety-net HIV clinic in San Francisco destabilized during COVID-19. AIDS 2020;34(15):2328–2331; doi: 10.1097/qad.0000000000002677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rogers BG, Coats CS, Adams E, et al. Development of telemedicine infrastructure at an LGBTQ+ Clinic to support HIV prevention and care in response to COVID-19, Providence, RI. AIDS Behav 2020;24(10):2743–2747; doi: 10.1007/s10461-020-02895-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hoagland B, Torres TS, Bezerra DRB, et al. High acceptability of PrEP teleconsultation and HIV self-testing among PrEP users during the COVID-19 pandemic in Brazil. Braz J Infect Dis 2021;25(1)101037; doi: 10.1016/j.bjid.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dandachi D, Freytag J, Giordano TP, et al. It is time to include telehealth in our measure of patient retention in HIV care. AIDS Behav 2020;24(9):2463–2465; doi: 10.1007/s10461-020-02880-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Armstrong WS, Agwu AL, Barrette E-P, et al. Innovations in human immunodeficiency virus (HIV) care delivery during the coronavirus disease 2019 (COVID-19) pandemic: Policies to strengthen the ending the epidemic initiative—A policy paper of the Infectious Diseases Society of America and the HIV Medicine Association. Clin Infect Dis 2021;72(1):9–14; doi: 10.1093/cid/ciaa1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Budak JZ, Scott JD, Dhanireddy S, et al. The impact of COVID-19 on HIV care provided via telemedicine—past, present, and future. Curr HIV/AIDS Rep 2021;18:98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Coppock D, Quimby C, Nunez J, et al. People living with human immunodeficiency virus during the COVID-19 pandemic: Experiences with telemedicine. Health Promot Pract 2021;22(3):298–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Auchus IC, Jaradeh K, Tang A, et al. Transitioning to telehealth during the COVID-19 pandemic: Patient perspectives and attendance at an HIV Clinic in San Francisco. AIDS Patient Care STDS 2021;35(7):249–254; doi: 10.1089/apc.2021.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dawson L, Kates J. Delivering HIV Care and Prevention in the COVID Era: A National Survey of Ryan White Providers. Kaiser Family Foundation. 2020. Available from: https://www.kff.org/report-section/delivering-hiv-care-prevention-in-the-covid-era-a-national-survey-of-ryan-white-providers-issue-brief/ [Last accessed: September 25, 2021].
- 17. Ennis N, Armas L, Butame S, et al. Factors impacting video telehealth appointment completion during covid-19 pandemic among people living with HIV in a community-based health system. AIDS Behav 2022;26(2):407–414; doi: 10.1007/s10461-021-03394-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. El-Nahal WG, Chander G, Jones JL, et al. Telemedicine use among people with HIV in 2021: The hybrid-care environment. J Acquir Immune Defic Syndr 2023;92(3):223–230; doi: 10.1097/qai.0000000000003124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Friedman EE, Devlin SA, Gilson SF, et al. Age and racial disparities in telehealth use among people with HIV during the COVID-19 pandemic. AIDS Behav 2022;26(8):2686–2691; doi: 10.1007/s10461-022-03607-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wood BR, Lan KF, Tao Y, et al. Visit trends and factors associated with telemedicine uptake among persons with HIV during the COVID-19 pandemic. Open Forum Infect Dis 2021;8(11):ofab480; doi: 10.1093/ofid/ofab480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Trepka MJ, Ward MK, Ladner RA, et al. HIV care access during the COVID-19 Pandemic as perceived by racial/ethnic minority groups served by the Ryan White Program, Miami-Dade County, Florida. J Int Assoc Provid AIDS Care 2022;21:23259582221084536; doi: 10.1177/23259582221084536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yelverton V, Qiao S, Weissman S, et al. Telehealth for HIV care services in South Carolina: Utilization, barriers, and promotion strategies during the covid-19 pandemic. AIDS Behav 2021;25(12):3909–3921; doi: 10.1007/s10461-021-03349-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wood BR, Young JD, Abdel-Massih RC, et al. Advancing digital health equity: A Policy Paper of the Infectious Diseases Society of America and the HIV Medicine Association. Clin Infect Dis 2021;72(6):913–919; doi: 10.1093/cid/ciaa1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Walker D, Moucheraud C, Butler D, et al. Experiences with telemedicine for HIV care in two federally qualified health centers in Los Angeles: A qualitative study. BMC Health Serv Res 2023;23(1):156; doi: 10.1186/s12913-023-09107-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Eaton LA, Cherry C, Cain D, et al. A novel approach to prevention for at-risk HIV-negative men who have sex with men: Creating a teachable moment to promote informed sexual decision-making. Am J Public Health 2011;101(3):539–545; doi: 10.2105/ajph.2010.191791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Galaviz KI, Shah NS, Gutierrez M, et al. Patient experiences with telemedicine for HIV care during the first COVID-19 wave in Atlanta, Georgia. AIDS Res Hum Retroviruses 2022;38(5):415–420; doi: 10.1089/aid.2021.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hickey MD, Sergi F, Zhang K, et al. Pragmatic randomized trial of a pre-visit intervention to improve the quality of telemedicine visits for vulnerable patients living with HIV. J Telemed Telecare 2023;29(3):187–195; doi: 10.1177/1357633x20976036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rosen JG, Zhang L, Pelaez D, et al. Provider perspectives on HIV pre-exposure prophylaxis service disruptions and adaptations during the COVID-19 pandemic in Baltimore, Maryland: A qualitative study. AIDS Patient Care STDS 2022;36(8):313–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lesko CR, Bengtson AM. HIV and COVID-19: Intersecting epidemics with many unknowns. Am J Epidemiol 2021;190(1):10–16; doi: 10.1093/aje/kwaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gwadz M, Campos S, Freeman R, et al. Black and latino persons living with hiv evidence risk and resilience in the context of covid-19: A mixed-methods study of the early phase of the pandemic. AIDS Behav 2021;25(5):1340–1360; doi: 10.1007/s10461-021-03177-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Eaton EF, Burgan K, McCollum G, et al. Expanding access to substance use services and mental health care for people with HIV in Alabama, a technology readiness assessment using a mixed methods approach. BMC Health Serv Res 2022;22(1):919; doi: 10.1186/s12913-022-08280-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Algarin AB, Varas-Rodríguez E, Valdivia C, et al. Symptoms, stress, and HIV-related care among older people living with HIV during the COVID-19 pandemic, Miami, Florida. AIDS Behav 2020;24(8):2236–2238; doi: 10.1007/s10461-020-02869-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Edelman EJ, Aoun-Barakat L, Villanueva M, et al. Confronting another pandemic: Lessons from HIV can inform our covid-19 response. AIDS Behav 2020;24(7):1977–1979; doi: 10.1007/s10461-020-02908-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Guaraldi G, Milic J, Martinez E, et al. HIV care models during the COVID-19 era. Clin Infect Dis 2021;73(5):e1222–e1227; doi: 10.1093/cid/ciaa1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mgbako O, Miller EH, Santoro AF, et al. COVID-19, telemedicine, and patient empowerment in HIV care and research. AIDS Behav 2020;24(7):1990–1993; doi: 10.1007/s10461-020-02926-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rhodes SD, Mann-Jackson L, Alonzo J, et al. A rapid qualitative assessment of the impact of the COVID-19 pandemic on a racially/ethnically diverse sample of gay, bisexual, and other men who have sex with men living with HIV in the US South. AIDS Behav 2021;25(1):58–67; doi: 10.1007/s10461-020-03014-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Smith E, Badowski ME. Telemedicine for HIV care: Current status and future prospects. HIV AIDS Res Palliat Care 2021;13:651–656; doi: 10.2147/hiv.S277893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Young SD, Schneider J. Clinical care, research, and telehealth services in the era of social distancing to mitigate COVID-19. AIDS Behav 2020;24(7):2000–2002; doi: 10.1007/s10461-020-02924-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Yelverton V, Weissman S, Qiao S, et al. Social Determinants of Health Exacerbate Implementation and Access Barriers to Telehealth HIV Care in the Southern United States. In: Results from a Scoping Review of Research and Intervention Needs [Poster Presentation]. International AIDS Society: Montreal, Canada; 2022. [Google Scholar]
- 40. O'Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: A synthesis of recommendations. Acad Med 2014;89(9):1245–1251. [DOI] [PubMed] [Google Scholar]
- 41. HIV.gov About ending the HIV epidemic: Plan for America. 2023. Available from: https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview [Last accessed: September 25, 2021].
- 42. Elflein J. U.S. states with the highest rates of HIV diagnoses in 2019. statista.com 2023. Available from: https://www.statista.com/statistics/257734/us-states-with-highest-aids-diagnosis-rates/ [Last accessed December 5, 2021].
- 43. Centers for Disease Control and Prevention. Social determinants of health among adults with diagnosed HIV infection, 2016. Part A: Census tract-level social determinants of health among adults with diagnosed HIV infection—13 states, the District of Columbia, and Puerto Rico. HIV Surveillance Supplemental Report. Volume 23 (No. 6, pt A); September 27, 2021. Available from: https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Last accessed September 27, 2021].
- 44. Reif SS, Whetten K, Wilson ER, et al. HIV/AIDS in the Southern USA: A disproportionate epidemic. AIDS Care 2014;26(3):351–359. [DOI] [PubMed] [Google Scholar]
- 45. South Carolina Department of Health and Environmental Control. An Epidemiologic Profile of HIV and AIDS in South Carolina. Available from: https://scdhec.gov/hiv-aids-std-data-reports [Last accessed September 27, 2021].
- 46. Centers for Disease Control and Prevention. HIV Surveillance Report; 2017. Available from: www.cdcgov/hiv/library/reports/hivsurveillancehtml [Last accessed September 27, 2021].
- 47. Division of Surveillance and Technical Support Bureau of Disease Control [SCDHEC]. An Epidemiologic Profile of HIV and AIDS in South Carolina; 2018. Available from: https://scdhec.gov/hiv-aids-std-data-reports [Last accessed September 27, 2021].
- 48. Patton MQ. Qualitative Research & Evaluation Methods, 4th ed. Sage Publications: Thousand Oaks, CA; 2015. [Google Scholar]
- 49. Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006;18(1):59–82. [Google Scholar]
- 50. Pew Research Center. The American Trends Panel. Available from: https://www.pewresearch.org/our-methods/u-s-surveys/the-american-trends-panel/ [Last accessed May 1, 2023].
- 51. QSR International Pty Ltd. NVivo (released in March 2020). https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- 52. McHugh ML. Interrater reliability: The kappa statistic. Biochem Med 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- 53. Terry G, Hayfield N, Clarke V, et al. Thematic Analysis. In: The Sage Handbook of Qualitative Research in Psychology. (Willig C, Rogers WS. eds.) Sage: Los Angeles, CA; 2017; pp. 17–37. [Google Scholar]
- 54. Henry T. Telehealth is here to stay, but payment is key to future use. 2021. Available from: https://www.ama-assn.org/practice-management/digital/telehealth-here-stay-payment-key-future-use [Last accessed May 1, 2023].
- 55. Telehealth is here to stay. Nat Med 2021;27(7):1121–1121; doi: 10.1038/s41591-021-01447-x. [DOI] [PubMed]
- 56. Imbert E, Hickey MD, Del Rosario JB, et al. Brief report: Heterogeneous preferences for care engagement among people with HIV experiencing homelessness or unstable housing during the COVID-19 pandemic. J Acquir Immune Defic Syndr 2022;90(2):140–145; doi: 10.1097/qai.0000000000002929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Baim-Lance A, Angulo M, Chiasson MA, et al. Challenges and opportunities of telehealth digital equity to manage HIV and comorbidities for older persons living with HIV in New York State. BMC Health Serv Res 2022;22(1):609; doi: 10.1186/s12913-022-08010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Harsono D, Deng Y, Chung S, et al. Experiences with telemedicine for HIV care during the COVID-19 pandemic: A mixed-methods study. AIDS Behav 2022;26(6):2099–2111; doi: 10.1007/s10461-021-03556-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wong KYK, Stafylis C, Klausner JD. Telemedicine: A solution to disparities in human immunodeficiency virus prevention and pre-exposure prophylaxis uptake, and a framework to scalability and equity. Mhealth 2020;6:21; doi: 10.21037/mhealth.2019.12.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ehrenkranz P, Grimsrud A, Holmes CB, et al. Expanding the vision for differentiated service delivery: A call for more inclusive and truly patient-centered care for people living with HIV. J Acquir Immune Defic Syndr 2021;86(2):147–152; doi: 10.1097/qai.0000000000002549. [DOI] [PMC free article] [PubMed] [Google Scholar]