Abstract
Background:
This study reviews the patient demographics, functional outcomes, and complications of trapeziometacarpal arthrodesis as a treatment for arthritis of the first carpometacarpal joint.
Methods:
A literature search was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines using PubMed and Google Scholar. Articles located by the search were independently assessed by title, abstract, or full article review for inclusion or exclusion. Demographic, outcome, and complication data from included articles were extracted, compiled, and analyzed. Frequency-weighted means and proportions were generated.
Results:
In total, 21 articles met inclusion and exclusion criteria accounting for 802 patients and 914 thumbs. Average age at time of surgery was 55.4 years, and mean follow-up time was 72.7 months. Arthrodesis techniques include Kirschner-wire fixation (51.3%), plate fixation (24.6%), screw fixation (9.8%), tension band technique (7.1%), staple fixation (7.0%), and none (<0.1%). Mean preoperative Disabilities of the Arm, Shoulder and Hand score was 58 and 25.4 postoperatively (∆ = -32.6 points). Mean preoperative visual analogue scale score was 6.8 and 1.9 postoperatively (∆ = -4.9 points). Mean preoperative grip strength was 15.7 kg, and 23.0 kg postoperatively (∆ = +7.3 kg). In all, 48.7% of thumbs had complications, 15.1% of which were major, while 33.6% were minor. The most common major complication was symptomatic hardware (8.6%) requiring return to the operating room, and the most common minor complications were peritrapezial arthritis (8.5%) and nonunion (8.4%).
Conclusions:
Arthrodesis for arthritis of the trapeziometacarpal joint is associated with good functional outcomes and low to moderate patient-reported disability and pain scores, but a high complication rate.
Level of Evidence:
IV
Keywords: trapeziometacarpal arthrodesis, arthrodesis, fusion, carpometacarpal arthritis, thumb, arthritis
Introduction
Carpometacarpal joint (CMCJ) arthritis is a common, often debilitating disease of the basal joint of the thumb, affecting nearly 17.7% of men and 21% of women. 1 Arthritis of the first CMCJ, also known as the trapeziometacarpal joint, is often symptomatic and presents with pain and limitations in daily functional activities. 2 A common radiographic classification system for CMCJ arthritis was proposed by Eaton and Glickel in 1987 and stages the pathological changes of the basal joint of the thumb. 3 This classification system serves as an objective measurement of disease progression, provides prognostic information, and aids in the determination of optimal treatment methods. 4 Initial treatment for trapeziometacarpal arthritis involves conservative measures such as rest, splinting, occupational therapy, and intra-articular steroid injections. 5 When these measures fail to provide relief, surgical intervention is typically considered. There are a number of surgical options for management of trapeziometacarpal arthritis including ligament reconstruction (LR), interposition (using tendon, bone graft, or spacer), trapeziectomy, metacarpal osteotomy, arthroplasty, and arthrodesis.6-12 Each intervention can have multiple modifications as well as its associated benefits and risk, and for this reason there is no established gold standard.
Since its initial description in 1949, arthrodesis has been one of the most frequently used surgical techniques for CMCJ arthritis, in addition to LR.13,14 Arthrodesis is typically indicated for young, active patients, or for heavy laborers, typically with an Eaton-Glickel stage III arthritis, 15 although its efficacy has been demonstrated in older patients with lower stages of arthritis. 16 Arthrodesis has been suggested to provide a stable CMCJ with minimal postoperative pain. 12 Common disadvantages to arthrodesis include decreased range of motion (ROM) and the potential for nonunion. 15 Although many studies, in mostly smaller case series, have individually investigated the various surgical techniques previously described for treatment of trapeziometacarpal arthritis, there is no comprehensive review of the literature specific to arthrodesis. This study aims to systematically review the current literature to assess patient demographics, clinical outcomes, and complications of trapeziometacarpal arthrodesis in the treatment of arthritis of the first CMCJ.
Materials and Methods
This analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. 17
Identification and Selection of Studies
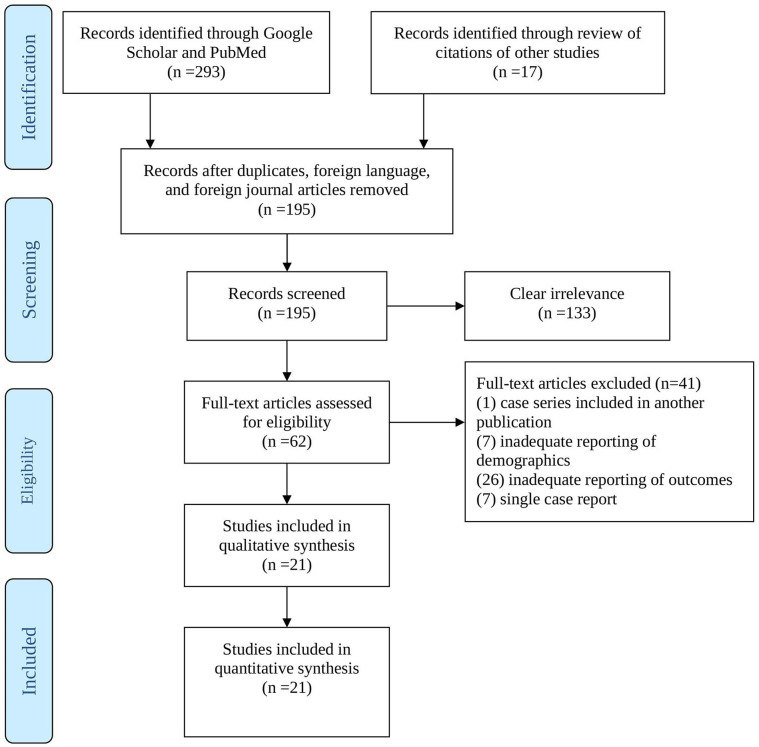
A systematic review of the current available literature was performed using various combinations of multiple search terms including “trapeziometacarpal arthrodesis,” “trapeziometacarpal fusion,” “carpometacarpal arthritis,” and “carpometacarpal osteoarthritis” in PubMed and Google Scholar. Articles located by the search were independently assessed by title, abstract, or full article review by the 2 senior authors for inclusion or exclusion (Figure 1). Articles that met inclusion criteria were reviewed and mined for subjective outcome, objective outcome, and complication data. Weighted means and proportions were produced based on homogeneous data from studies which met the inclusion and exclusion criteria.
Figure 1.
Identification of articles for trapeziometacarpal arthrodesis systematic review.
Eligibility
Articles included in this systematic review met the following inclusion criteria: assessed results of trapeziometacarpal arthrodesis for arthritis of the first CMCJ of the hand; published in English in a North American or European peer-reviewed journal; and reported at least one subjective or objective outcome such as ROM, strength, or functional outcome scores. Studies were excluded if they were a technique description, biomechanical analysis, or a review; were not written in English; reported no numerical subjective or objective data; were single case reports; analyzed patient data contained in other included studies; involved surgical treatments including other joints such as wrist arthrodesis; and were published in a non-American or non-European journal.
Data Extraction and Analysis
The authors extracted, compiled, and analyzed demographic characteristics and all relevant surgical and functional outcomes and complications. Data bias was assessed independently by 2 authors (M.S.D. and A.F.) where results from the available studies were examined for potential missing studies in the form of publication bias, as well as in missing data within the included studies in the form of selective reporting bias. Outcome data were analyzed if the variable was reported by 5 or more articles and included pre- and postoperative Disabilities of the Arm, Shoulder, and Hand (DASH) scores, visual analogue scale (VAS) scores, and grip strength; postoperative Kapandji scores, ROM of thumb extension/radial abduction, ROM of thumb palmar abduction, tip pinch strength, and lateral/key pinch strength. Complications were divided into major and minor, with major defined as requiring return to the operating room (OR) for additional surgery and minor defined as asymptomatic or requiring only conservative management. Of note, this simplified stratification system designates some complications, such as superficial nerve neuropathies, as minor, though some may consider them to be major complications. The authors calculated frequency-weighted means and proportions for homogenous data.
Results
Review of the literature resulted in 21 articles meeting inclusion and exclusion criteria accounting for 802 patients and 914 thumbs as some patients underwent bilateral procedures. Average age at the time of surgery was 55.4 years (ranging from age 20 to 84) with a mean follow-up time of 72.7 months (ranging from 3 to 336 months). A minority of the patients were male (26.3%) and 56% of the procedures were conducted on the patient’s dominant hand (data reported by 17 out of 21 articles). With regard to arthrodesis technique, Kirschner wire (K-wire) fixation was most used (51.3%), followed by plate fixation (24.6%), screw fixation (9.8%), tension band technique (7.1%), staple fixation (7.0%), and none (<0.1%). Among the 10 studies that reported numerical data regarding bone graft usage, 66.4% of patients received bone graft. Demographic data are summarized in Table 1.
Table 1.
Demographics.
| Demographic | a Articles reported | N (patients) | N (thumbs) | Count | Percent (%) | Weighted mean |
|---|---|---|---|---|---|---|
| Age (years) | 21 | 802 | 914 | 55.4 | ||
| Male | 21 | 802 | 211 | 26.3 | ||
| Follow-up (months) | 21 | 802 | 914 | 72.7 | ||
| Dominant hand | 17 | 727 | 407 | 56.0 | ||
| Surgical technique | ||||||
| 1. Kirschner wire | 10 | 914 | 469 | 51.3 | ||
| 2. Plate | 10 | 914 | 225 | 24.6 | ||
| 3. Screw only | 6 | 914 | 90 | 9.8 | ||
| 4. Tension band | 4 | 914 | 65 | 7.1 | ||
| 5. Staple | 5 | 914 | 64 | 7.0 | ||
| 6. None | 1 | 914 | 1 | <0.1 | ||
| Bone graft usage | 10 | 277 | 184 | 66.4 | ||
Articles that reported this information with clear numerical data.
Mean preoperative DASH score was 58 (N thumbs = 149), while mean postoperative DASH score was 25.4 (N thumbs = 427), representing a difference in DASH scores of -32.6 points. Mean VAS score was 6.8 (N thumbs = 279) preoperatively and improved to 1.9 (N thumbs = 529) postoperatively, with a difference of -4.9 points. Mean postoperative Kapandji score was 8.6.
Mean preoperative grip strength was 15.7 kg (N thumbs = 228), while mean postoperative grip strength was 23.0 kg (N thumbs = 561), with a difference of +7.3 kg. Mean postoperative tip pinch strength and lateral or key pinch strength were 4.7 kg and 5.9 kg, respectively. With regard to ROM of the first metacarpophalangeal joint, mean postoperative extension/radial abduction and palmar abduction were 40.3 degrees and 36.6 degrees, respectively. Functional outcomes and ROM data are represented in Table 2.
Table 2.
Functional Outcomes and Range of Motion.
| Functional Outcome | a Articles reported | N (thumbs) | Weighted mean | |
|---|---|---|---|---|
| DASH score | Preoperative | 5 | 149 | 58.0 |
| Postoperative | 12 | 427 | 25.4 | |
| Delta ∆ | –32.6 | |||
| Pain VAS | Preoperative | 5 | 279 | 6.8 |
| Postoperative | 10 | 529 | 1.9 | |
| Delta ∆ | -4.9 | |||
| Kapandji score | Postoperative | 8 | 223 | 8.6 |
| b Extension/radial abduction (Degrees) | 13 | 472 | 40.3 | |
| b Palmar abduction (Degrees) | 11 | 413 | 36.6 | |
| Grip strength (kg) | Preoperative | 5 | 228 | 15.7 |
| Postoperative | 14 | 561 | 23.0 | |
| Delta ∆ | +7.3 | |||
| Tip pinch strength (kg) | Postoperative | 11 | 528 | 4.7 |
| Lateral/key pinch strength (kg) | Postoperative | 10 | 446 | 5.9 |
Note. DASH = Disabilities of the Arm, Shoulder and Hand; VAS = Visual Analogue Scale; MCP = Metacarpophalangeal.
Articles that reported this information with clear numerical data.
Movements at the MCP joint of the thumb.
In total, 445 out of 914 thumbs had complications, representing a complication rate of 48.7% among all 21 studies. In all, 15.1% of complications were considered major (defined as requiring a nonroutine return to the OR), and 33.6% of complications were minor (defined as requiring either nonoperative treatment or no treatment). One study described return to the OR for K-wire removal for 3 patients that was not attributed to complications or symptoms—these were not considered complications for the purposes of the present study. The most common major complication was symptomatic hardware necessitating additional surgery (8.6%), while the second most common was nonunion requiring additional surgery (4.3%). “Other” major complications requiring return to the OR comprised 2.2% of major complications and are listed below in Table 3. The most common minor complications were peritrapezial arthritis (8.5%), followed by nonunion (8.4%; asymptomatic and/or not requiring surgical management), radial nerve neuropathies (5.5%), superficial infections (1.9%), and complex regional pain syndrome (1.2%). “Other” minor complications comprised 8.1% of the total minor complications and are specified below Table 3, which summarizes all complication data.
Table 3.
Complications.
| Complication | a Articles reported | N (thumbs) | Count | Percent (%) |
|---|---|---|---|---|
| Major | 17 | 914 | 138 | 15.1 |
| 1. Nonunion revision | 13 | 914 | 39 | 4.3 |
| 2. Symptomatic hardware | 9 | 914 | 79 | 8.6 |
| 3. b Other return to operating room | 11 | 914 | 20 | 2.2 |
| Minor | 19 | 914 | 307 | 33.6 |
| 1. Nonunion | 11 | 914 | 77 | 8.4 |
| 2. Superficial infection | 8 | 914 | 17 | 1.9 |
| 3. Radial nerve neuropathies | 13 | 914 | 50 | 5.5 |
| 4. Complex regional pain syndrome | 6 | 914 | 11 | 1.2 |
| 5. c Peritrapezial arthritis | 8 | 914 | 78 | 8.5 |
| 6. d Other | 12 | 914 | 74 | 8.1 |
| Total complications | 21 | 914 | 445 | 48.7 |
Articles that reported this information with clear numerical data.
Flexor pollicus longus rupture (1), difficulty removing Kirschner wire (K-wire) in clinic (1), deep infection (1), malpositioned hardware (2), general pain (4), scaphotrapeziotrapezoidal (STT) arthritis (3), painful osteophytes (2), radial nerve neuropathy (2), and unspecified complaints or complications (4).
STT arthritis, trapezial-trapezoid arthritis, trapezial-index metacarpal arthritis.
Metacarpophalangeal (MCP) joint arthritis (26), reactive Dupuytren’s contracture (1), extensor indicis proprius rupture (1), dysesthetic scar (1), migration or loosening of hardware (5), intraoperative fracture (1), MCP synovitis (1), delayed union (12), scar pain (20), inadvertently buried K-wires (2), loss of digit length (1), K-wire fracture (2), and “other” (1).
Discussion
The trapeziometacarpal joint is a common location of arthritis in the hand and can cause pain in addition to compromising hand function. While nonsurgical treatments are available, patients experiencing significant symptoms resistant to conservative management may pursue surgical intervention. There are multiple surgical options available, including but not limited to LR, LR with tendon interposition (LRTI), trapeziectomy, arthroplasty, and arthrodesis (fusion), and others. However, there is no widely agreed upon gold standard treatment. A systematic review from 2011 comparing 8 surgical techniques, 16 a 2015 Cochrane review comparing 7 different surgical techniques, 18 as well as a recent meta-analysis comparing 5 techniques, found no single method to be superior. 19 The present review analyzes the demographic characteristics, functional outcomes, and complications of trapeziometacarpal arthrodesis as a treatment for arthritis of the first CMCJ. It was concluded that although arthrodesis is associated with good functional outcomes; however, the procedure has a high complication rate.
Trapeziometacarpal arthrodesis has been commonly used in the past, particularly for individuals with significant instability of the CMC joint.15,20,21 The procedure was typically reserved for younger patients, those with posttraumatic arthritis, or those requiring a high functional capacity of the hand. 22 However, more recent studies demonstrated that arthrodesis can also be used in older patients with stage II or III osteoarthritis. 16 Arthrodesis is known to increase thumb stability and durability.12,23,24 Additionally, the procedure generally provides adequate pain relief and strength.13,25 However, concerns remain with regard to complications, including nonunion, ROM limitations, and peritrapezial arthritis. 24
Generally, functional outcomes following arthrodesis are considered to be comparable to other surgical techniques.18,19 The current study found that arthrodesis has been associated with good clinical outcomes. Following surgical intervention, DASH score decreased by a mean of 32.6 points to 25.4 points postoperatively, and VAS score by 4.9 points to 1.9 points postoperatively, while grip strength increased by 7.3 kg to 23.0 kg postoperatively (46.5% increase). In comparison, a prospective study of 56 women who underwent either trapeziectomy alone or LRTI found that trapeziectomy resulted in postoperative DASH and VAS scores of 33 and 3.25, respectively, with a 47% increase in grip strength. 26 LR with tendon interposition resulted in postoperative DASH and VAS scores of 27 and 2.41, respectively, with a 74% increase in grip strength. With regard to ROM, a prospective study of 53 thumbs comparing LR versus LRTI also showed similar ROM outcomes to the present study. 27 Mean radial abduction was 43 degrees and mean palmar abduction was 42 for LR, while mean radial abduction was 39 degrees and mean palmar abduction was 38 degrees for LRTI. The present study demonstrated that arthrodesis results in a mean radial abduction of 40.3 degrees and a mean palmar abduction of 36.6 degrees. Additionally, the mean postoperative Kapandji score of 8.6 indicates adequate oppositional mobility of the thumb. A comparative study of tendon position arthroplasty to arthrodesis also determined that tip pinch, key pinch, and grip strength outcomes were not significantly different, although ROM was higher in the tendon position arthroplasty group. 28 However, 1 study found that patients who underwent LRTI had significantly better improvements to pain and function compared to arthrodesis. 29 Despite largely satisfactory functional outcomes, the controversy surrounding arthrodesis stems from its associated complications. 25
The present study showed a mean 48.7% complication rate, almost a third of which required return to the OR. The most common major complication was symptomatic hardware (8.6%), while common minor complications included peritrapezial arthritis (8.5%), nonunion (8.4%), and radial nerve neuropathies (5.5%). Knightly and Sullivan stated in their metanalysis that arthrodesis had an unacceptably high complication rate. When compared to trapeziectomy and trapeziectomy with LRTI, arthrodesis is associated with a higher rate of complications and additional surgeries. 16 The previously mentioned study comparing LR to LRTI noted only 5 complications in 53 thumbs representing only a 9.4% complication rate, none of which required reoperation. 27 Mureau et al 28 showed that tendon interposition arthroplasty had a 12% lower complication rate than arthrodesis. Hattori et al 30 performed arthrodesis in 38 patients using tension band fixation method and reported painful hardware necessitating removal in 82% of the patients. The authors went on to recommend routine hardware removal which they noted as a significant disadvantage as compared to other procedures. Given the findings of the present study and previous literature, arthrodesis should be employed cautiously, as other surgical methods can provide equivalent functional outcomes with a lower risk of complications.
Rates of nonunion vary significantly in the literature. 24 Singh et al 31 compared K-wire fixation with internal fixation and found that K-wire was more often associated with nonunion. The majority of cases in the present review used K-wire fixation. It has been proposed that early removal of K-wires was associated with decreased joint stability and increased risk of nonunion. 31 When compared to other fixation methods such as plate and screw, K-wire may result in less stability and delayed rehabilitation given its lesser rigidity and lack of permanent fixation.32,33 Nonunion has been associated with a need for additional surgery in some cases, but also with higher postoperative DASH scores. 31
Peritrapezial arthritis is another known complication of arthrodesis. In fact, Carroll recommended in 1987 that arthrodesis be limited to patients under the age of 50 due to increased risk of arthritis of the surrounding trapezial joints. Although not always symptomatic, in some cases peritrapezial arthritis requires medical or even surgical intervention.22,24 Rizzo et al noted a particularly high rate of peritrapezial arthritis at 31% but attributed this to a lengthy mean follow-up time of 11.2 years. The increased risk of peritrapezial arthritis is somewhat expected given that CMC arthrodesis redistributes axial load on to the scaphotrapeziotrapezoidal joint. 34
The main limitation of this systematic review was heterogeneity of the outcome data. Inconsistencies in variable outcome measures, as well as outcome reporting limited both data analysis and article inclusion. Second, the varying arthrodesis surgical techniques may limit the external validity of our results. In addition to the risk of underreporting complications among retrospective cohort studies, the discrepancies in follow-up time may have further influenced reported complication rates, especially for those that may take many years to develop, such as peritrapezial arthritis. Finally, many of the articles of inclusion were case series, and therefore constitute lower levels of evidence according to Grading of Recommendations, Assessment, Development and Evaluations (GRADE) criteria.
Nevertheless, this review analyzes the patient demographics, functional outcomes, and complications of trapeziometacarpal arthrodesis as a treatment for arthritis of the first CMCJ. It is concluded that although trapeziometacarpal arthrodesis is associated with good functional outcomes and low to moderate patient-reported disability and pain scores, the procedure has a high 48.7% complication rate. The results of this study suggest that trapeziometacarpal arthrodesis should not be considered a first-line treatment for individuals diagnosed with carpometacarpal arthritis requiring surgical management. Future, well-powered studies that report standardized outcome measures are needed to assess trapeziometacarpal arthrodesis, as well as other procedures for carpometacarpal arthritis, in order to generate foundational datasets for comparative meta-analyses.
Footnotes
Ethical Approval: Ethics approval was not required for this systematic review.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This article does not include any individual participants.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Miraal S. Dharamsi  https://orcid.org/0000-0002-8107-7012
https://orcid.org/0000-0002-8107-7012
Data Availability: The data that support the findings of this study are available from the corresponding author, MSD, upon reasonable request.
References
- 1. Wilder FV, Barrett JP, Farina EJ. Joint-specific prevalence of osteoarthritis of the hand. Osteoarthritis Cartilage. 2006;14(9):953-957. doi: 10.1016/j.joca.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 2. Dahaghin S, Bierma-Zeinstra SM, Ginai AZ, et al. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study). Ann Rheum Dis. 2005;64(5):682-687. doi: 10.1136/ard.2004.023564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eaton RG, Glickel SZ. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin. 1987;3(4):455-471. [PubMed] [Google Scholar]
- 4. Barron OA, Glickel SZ, Eaton RG. Basal joint arthritis of the thumb. J Am Acad Orthop Surg. 2000;8(5):314-323. doi: 10.5435/00124635-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 5. Heyworth BE, Lee JH, Kim PD, et al. Hylan versus corticosteroid versus placebo for treatment of basal joint arthritis: a prospective, randomized, double-blinded clinical trial. J Hand Surg Am. 2008;33(1):40-48. doi: 10.1016/j.jhsa.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 6. Harenberg PS, Jakubietz MG, Jakubietz RG, et al. Treatment of osteoarthritis of the first carpometacarpal joint by resection-suspension-interposition arthoplasty using the split abductor pollicis longus tendon. Oper Orthop Traumatol. 2013;25(1):95-103. doi: 10.1007/s00064-011-0082-2. [DOI] [PubMed] [Google Scholar]
- 7. Trumble T, Rafijah G, Heaton D. Thumb carpometacarpal arthroplasty with ligament reconstruction and interposition costochondral arthroplasty. J Wrist Surg. 2013;2(3):220-227. doi: 10.1055/s-0033-1351375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Desmoineaux P, Delaroche C, Beaufils P. Partial arthroscopic trapeziectomy with ligament reconstruction to treat primary thumb basal joint osteoarthritis. Orthop Traumatol Surg Res. 2012;98(7):834-839. doi: 10.1016/j.otsr.2012.05.018. [DOI] [PubMed] [Google Scholar]
- 9. Parker WL, Linscheid RL, Amadio PC. Long-term outcomes of first metacarpal extension osteotomy in the treatment of carpal-metacarpal osteoarthritis. J Hand Surg Am. 2008;33(10):1737-1743. doi: 10.1016/j.jhsa.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 10. Badia A, Sambandam SN. Total joint arthroplasty in the treatment of advanced stages of thumb carpometacarpal joint osteoarthritis. J Hand Surg Am. 2006;31(10):1605-1614. doi: 10.1016/j.jhsa.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 11. Lee JK, Yoon BH, Lee HI, et al. Prosthetic replacement has a clinical outcome superior to that of trapeziectomy with ligament reconstruction and tendon interposition: a meta-analysis. Orthopedics. 2021;44(2):e151-e157. doi: 10.3928/01477447-20210104-06. [DOI] [PubMed] [Google Scholar]
- 12. Zhang X, Wang T, Wan S. Minimally invasive thumb carpometacarpal joint arthrodesis with headless screws and arthroscopic assistance. J Hand Surg Am. 2015;40(1):152-158. doi: 10.1016/j.jhsa.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 13. Hartigan BJ, Stern PJ, Kiefhaber TR. Thumb carpometacarpal osteoarthritis: arthrodesis compared with ligament reconstruction and tendon interposition. J Bone Joint Surg Am. 2001;83(10):1470-1478. doi: 10.2106/00004623-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 14. Muller GM. Arthrodesis of the trapezio-metacarpal joint for osteoarthritis. J Bone Joint Surg Br. 1949;31B(4):540-542, illust. [PubMed] [Google Scholar]
- 15. Kapoutsis DV, Dardas A, Day CS. Carpometacarpal and scaphotrapeziotrapezoid arthritis: arthroscopy, arthroplasty, and arthrodesis. J Hand Surg Am. 2011;36(2):354-366. doi: 10.1016/j.jhsa.2010.11.047. [DOI] [PubMed] [Google Scholar]
- 16. Vermeulen GM, Slijper H, Feitz R, et al. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011;36(1):157-169. doi: 10.1016/j.jhsa.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 17. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wajon A, Vinycomb T, Carr E, et al. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2015;2015(2):CD004631. doi: 10.1002/14651858.CD004631.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Knightly N, Sullivan P. Surgery for trapeziometacarpal joint osteoarthritis: a meta-analysis on efficacy and safety. J Hand Surg Asian Pac Vol. 2021;26(2):245-264. doi: 10.1142/S2424835521500260. [DOI] [PubMed] [Google Scholar]
- 20. Earp B, Cefalu C, Blazar P. Thumb metacarpophalangeal joint arthritis. J Am Acad Orthop Surg. 2019;27(23):e1029-e1039. doi: 10.5435/JAAOS-D-18-00683. [DOI] [PubMed] [Google Scholar]
- 21. Weiss AC, Goodman AD. Thumb basal joint arthritis. J Am Acad Orthop Surg. 2018;26(16):562-571. doi: 10.5435/JAAOS-D-17-00374. [DOI] [PubMed] [Google Scholar]
- 22. Fulton DB, Stern PJ. Trapeziometacarpal arthrodesis in primary osteoarthritis: a minimum two-year follow-up study. J Hand Surg Am. 2001;26(1):109-114. doi: 10.1053/jhsu.2001.20964. [DOI] [PubMed] [Google Scholar]
- 23. Bamberger HB, Stern PJ, Kiefhaber TR, et al. Trapeziometacarpal joint arthrodesis: a functional evaluation. J Hand Surg Am. 1992;17(4):605-611. doi: 10.1016/0363-5023(92)90302-6. [DOI] [PubMed] [Google Scholar]
- 24. Rizzo M, Moran SL, Shin AY. Long-term outcomes of trapeziometacarpal arthrodesis in the management of trapeziometacarpal arthritis. J Hand Surg Am. 2009;34(1):20-26. doi: 10.1016/j.jhsa.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 25. Jimenez-Diaz V, Cecilia-Lopez D, Porras-Moreno MA, et al. Arthrodesis of the thumb carpometacarpal joint using a quadrangular plate: surgical technique and long-term results of 70 patients. Eur J Orthop Surg Traumatol. 2017;27(7):909-915. doi: 10.1007/s00590-017-1973-1. [DOI] [PubMed] [Google Scholar]
- 26. De Smet L, Sioen W, Spaepen D, et al. Treatment of basal joint arthritis of the thumb: trapeziectomy with or without tendon interposition/ligament reconstruction. Hand Surg. 2004;9(1):5-9. doi: 10.1142/s0218810404001942. [DOI] [PubMed] [Google Scholar]
- 27. Kriegs-Au G, Petje G, Fojtl E, et al. Ligament reconstruction with or without tendon interposition to treat primary thumb carpometacarpal osteoarthritis. A prospective randomized study. J Bone Joint Surg Am. 2004;86(2):209-218. doi: 10.2106/00004623-200402000-00001. [DOI] [PubMed] [Google Scholar]
- 28. Mureau MA, Rademaker RP, Verhaar JA, et al. Tendon interposition arthroplasty versus arthrodesis for the treatment of trapeziometacarpal arthritis: a retrospective comparative follow-up study. J Hand Surg Am. 2001;26(5):869-876. doi: 10.1053/jhsu.2001.26659. [DOI] [PubMed] [Google Scholar]
- 29. Spekreijse KR, Selles RW, Kedilioglu MA, et al. Trapeziometacarpal arthrodesis or trapeziectomy with ligament reconstruction in primary trapeziometacarpal osteoarthritis: a 5-year follow-up. J Hand Surg Am. 2016;41(9):910-916. doi: 10.1016/j.jhsa.2016.07.089. [DOI] [PubMed] [Google Scholar]
- 30. Hattori Y, Doi K, Dormitorio B, et al. Arthrodesis for primary osteoarthritis of the trapeziometacarpal joint in elderly patients. J Hand Surg Am. 2016;41(7):753-759. doi: 10.1016/j.jhsa.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 31. Singh HP, Hoare C, Beresford-Cleary N, et al. Nonunion after trapeziometacarpal arthrodesis: comparison between K-wire and internal fixation. J Hand Surg Eur Vol. 2015;40(4):351-355. doi: 10.1177/1753193414537758. [DOI] [PubMed] [Google Scholar]
- 32. Dreyfuss D, Allon R, Izacson N, et al. A comparison of locking plates and intramedullary pinning for fixation of metacarpal shaft fractures. Hand (N Y). 2019;14(1):27-33. doi: 10.1177/1558944718798854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yoshida R, Obopilwe E, Rodner CM. Biomechanical comparison of fifth carpometacarpal fusion methods: Kirschner wires versus plate and screws. Tech Orthop. 2018;33(4):271-273. doi: 10.1097/BTO.0000000000000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Berger AJ, Meals RA. Management of osteoarthrosis of the thumb joints. J Hand Surg Am. 2015;40(4):843-850. doi: 10.1016/j.jhsa.2014.11.026. [DOI] [PubMed] [Google Scholar]