Abstract
Background:
Much has been written about the diagnosis and treatment of soft tissue mallet injuries. However, there has been little regarding the characteristics of this injury affecting patients’ prognosis. The purpose of this prospective study was to identify factors influencing the outcome of treatment of soft tissue mallet injuries.
Methods:
Patients diagnosed with soft tissue mallet injuries were enrolled prospectively in a protocol of dorsal splinting for 6 to 12 weeks, followed by weaning over 2 weeks and then evaluated at 6, 9, and ≥12 months.
Results:
Thirty-seven patients (38 digits) completed the study. Treatment success was defined as a final extensor lag of <15° and failure as a final extensor lag of ≥15°. Those failing splint treatment were older compared with those successfully treated. Patient compliance was significantly associated with a successful outcome. Factors that did not significantly affect success included time to treatment, initial injury severity, splinting duration, sex, and ligamentous laxity. Disabilities of Arm, Shoulder, and Hand scores >0 were not associated with treatment failure. Radiographic and clinical extension lag were statistically comparable.
Conclusions:
This study shows strong association between the success of splint treatment, younger patient age, and compliance with the treatment protocol. Despite this finding, most patients did not report any functional limitations, irrespective of the treatment success. In contrast to prior results, time to treatment and initial extensor lag did not significantly affect treatment success.
Keywords: soft tissue mallet, splinting, hand surgery, extensor lag
Introduction
Mallet finger is an injury to the terminal extensor tendon of the finger, which results in an extensor lag of the distal interphalangeal (DIP) joint. This commonly results from an axial loading or forced flexion moment at the DIP joint.1,2 Mallet fingers are classified as soft tissue, involving disruption of the tendon itself, or bony, which refers to an avulsion fracture at the site of the extensor tendon insertion on the distal phalanx.
Doyle classified these injuries into 4 types: type 1 is a closed injury with or without a small avulsion fracture; type 2 is an open laceration of the terminal extensor tendon; type 3 is an open injury with loss of skin, subcutaneous tissue, and tendon; and type 4 is a mallet fracture. 3 Type 1 is the most common injury pattern and the focus of this study. Treatment of soft tissue mallet injuries is largely nonoperative as studies comparing operative and nonoperative treatments have shown comparable outcomes, but higher complication rates with surgery.2,4-7 There are several variations of mallet finger splints with similar efficacy. Pike et al 8 found no difference in outcome between treatment with noncustom dorsal, noncustom volar, and custom thermoplastic splints. O’Brien and Bailey 9 showed statistically comparable extensor lag and DIP joint motion 20 weeks after treatment with stack, dorsal alumifoam, or custom thermoplastic splints.
Although closed management of mallet fingers usually leads to successful outcomes, this is not always the case. Certain factors that potentially affect outcomes have been identified. Patient compliance has correlated with superior results.9,10 Delay in treatment may also affect outcomes. Abouna and Brown found that initiation of splinting within 4 weeks of injury led to a “cure rate” (defined as an extension lag <5°, no stiffness, and normal flexion and extension) of 70% to 78% and a “failure rate” (defined as an extension lag >15° and the presence of stiffness or impairment of flexion) of 9% to 14.5%. The “cure rate” was 62.5% and the “failure rate” was 37.5% for splinting initiated more than 4 weeks from injury. 1 In contrast, Garberman et al 11 compared splinting within 2 weeks of injury with a delay of greater than 4 weeks and found similar satisfaction outcomes.
O’Brien and Bailey 9 looked at the effect of patient age on outcome and found strong and moderate correlations at 12 and 20 weeks, respectively, between older age and greater residual extensor lag. A number of other studies found a similar correlation. Pike et al 8 found that increasing age correlated moderately with greater residual extensor lag at 12 weeks. Abouna and Brown 1 reported “cure rates” of 100%, 92%, 59%, and 0% in patients 0-21, 21-40, 41-60, and ≥ 61 years of age, respectively. Warren et al 12 showed a greater failure rate in older individuals. Maitra and Dorani found a failure rate of 85.2% in patients aged ≥41 years. 13
The severity of initial extensor lag has also been shown to be associated with outcomes. Abouna and Brown 1 found “cure rates” of 100%, 74%, and 59% for initial extensor lag measurements of <30°, 31°-50°, and >50°, respectively. Warren et al 12 found that when the initial extensor lag was >30°, failures outnumbered successes. Of note, both these studies lacked statistical analysis and included a cohort of both soft tissue and bony mallet injuries.
Mallet fingers can have both aesthetic and functional consequences. The success of nonoperative treatment may be dependent on various patient and injury factors. The purpose of this study is to identify patient and injury factors associated with the successful nonoperative management of soft tissue mallet injuries.
Materials and Methods
Institutional review board approval was obtained for this study. Informed consent was obtained from each patient upon enrollment. Patients presenting to the practice of 3 fellowship-trained hand and upper extremity surgeons who were older than 18 years of age and diagnosed with a soft tissue mallet injury represented by a DIP joint extension lag greater than 0° and less than 3 months after the date of injury were offered the opportunity to participate in the study. Exclusion criteria included open soft tissue mallet injuries, any history of collagen vascular or connective tissue disease, chronic pain, prior injury with surgical or nonsurgical treatments involving the DIP joint, radiographic confirmation of a bony mallet including minor avulsions, and a positive urine pregnancy test.
A questionnaire of patient demographic characteristics (age, sex, hand dominance, etc) was obtained at the initial visit. A Visual Analogue Scale (VAS) for pain and a Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire were given to each patient on their initial and all subsequent visits. The DASH questionnaire was selected as it is a validated, commonly used, and well-accepted outcome measure to assess upper extremity function. It captures many activities that are considered activities of daily living and therefore provides an effective assessment of impairment due to upper extremity pathology. At each visit, a physical examination was performed by the treating physician, which included goniometer measurements of extensor lag and range of motion of the metacarpophalangeal, proximal interphalangeal (PIP), and DIP joint of the affected digits and contralateral digit for comparison after the appropriate course of splinting. The presence of upper extremity ligamentous laxity (thumb-to-forearm, elbow hyperextension), swelling graded by attending physician (scale: 0 [no swelling], 1 + [mild], 2 + [moderate], or 3 + [severe]), and swan-neck deformity was also documented. At visits during the continuous splinting protocol, patients were asked about their compliance with continuous splint wear. Patients who removed their splint themselves during this time were classified as noncompliant.
Splinting Protocol
At the initial visit, an alumifoam splint bent into mild hyperextension was applied to the dorsum of the affected digit extending from the tip of the finger to a point just distal to the PIP joint. This splint was worn continuously during the first 6 weeks. During this time, patients were seen back at 2-week intervals for splint change, evaluation of the integrity of the dorsal skin, and assessment of physical examination study parameters. Four patients in this study experienced minor skin complications of hyperemia and maceration. These all occurred at the end of the continuous splinting protocol, and patients were switched to removable splints according to the splint weaning protocol.
After a minimum of 6 weeks of splinting, patients with no residual extension lag began a 2-week splint weaning protocol. During the first week, this consisted of removing the splint 3 times per day to perform 6 repetitions of gentle DIP flexion exercises. During the second weaning week, the frequency of exercise was increased to 4 times per day to doing 12 repetitions. After the 2-week splint weaning protocol, patients were instructed to continue night splinting for an additional 4 weeks. If at any point during the splint weaning protocol the patients were unable to achieve full active extension, or if after the initial splinting period any patient had a persistent extensor lag, they were splinted continuously for an additional 2 weeks. Physical examination study parameters were then repeated. Measurements were made with a goniometer. If an extension lag of 5° or greater persisted, continuous splinting continued at 2-week intervals until the extension lag resolved or until a total of 12 weeks of continuous splinting had been completed, whichever came first. No patient was splinted longer than 12 weeks. All study measurements were completed by 1 of the 3 attending hand surgeons or 1 of the 6 hand surgery fellows.
In addition to the described physical examination assessments that were made at each follow-up visit, at the final 12-month assessment, the patients completed a final VAS of pain, DASH assessment, and radiography of the injured finger and the corresponding contralateral uninjured finger to evaluate the extension lag radiographically.
Statistical Analysis
Patients were divided into 2 groups based on the final outcome of their treatment. “Success” was defined as a residual extension lag <15° at the final follow-up (>1 year), compared with the contralateral side. “Failure” was defined as a residual extension lag ≥15°. Between these 2 groups, normally distributed continuous variables were compared by t test. Continuous variables not normally distributed were compared by Wilcoxon rank-sum test. Categorical variables were compared by the Fisher exact test. Extension lag was compared between various follow-up time points by the Student t test to assess significant trends in improvement of worsening over time. Radiography and clinical measurements of extension lag were compared with Pearson correlation. Correlation was also assessed between final visit extension lag and DASH score, loss of DIP flexion and DASH score, and age and extension lag.
Results
A total of 82 patients were enrolled in the study. Ten were excluded due to an interruption of the splinting protocol (eg, patient not returning for follow-up appointments/splint changes before protocol was completed). Thirty-six did not return for 1-year follow-up visits. Therefore, 37 patients (38 digits) completed the study. Table 1 lists the patient demographics. Of note, in our cohort, the male-to-female ratio was 2:1. The patient’s age ranged from 25 to 79, with the greatest number of soft tissue mallet injuries in the 45- to 54-year category (n = 12 of 37, 32%). The most common injury mechanism was performing housework or other activities of daily living (n = 11 of 37, 30%), followed by sports (n = 10 of 37, 27%). Table 2 provides the additional descriptive information about the study population at the time of injury.
Table 1.
Patient Demographics.
| Patient Demographics | No. of patients (N = 37) | % |
|---|---|---|
| Sex | ||
| Female | 13 | 35 |
| Male | 24 | 65 |
| Age, y | ||
| 25-34 | 6 | 16 |
| 35-44 | 5 | 14 |
| 45-54 | 12 | 32 |
| 55-64 | 5 | 14 |
| 65-74 | 5 | 14 |
| >75 | 4 | 11 |
| Mean | 51 | |
| Range | 25-79 | |
| Occupation | ||
| Professional/office work | 19 | 51 |
| Arts | 7 | 19 |
| Homemaker | 3 | 8 |
| Hospitality/retail | 2 | 5 |
| Student | 2 | 5 |
| Unknown | 2 | 5 |
| Retired | 2 | 5 |
| Ligamentous laxity | ||
| Any laxity present | 8 | 22 |
| Thumb-to-forearm | 4 | 11 |
| Elbow hyperextension | 4 | 11 |
| Swan neck deformity of other digit | 1 | 3 |
Table 2.
Injury Characteristics.
| Injury Characteristics | No. of patients (N = 37) | % |
|---|---|---|
| Mechanism of injury | ||
| Housework/ADLs | 11 | 30 |
| Sports | 10 | 27 |
| Dressing | 5 | 14 |
| Unknown | 5 | 14 |
| Childcare | 3 | 8 |
| Fall | 2 | 5 |
| Direct blow (unspecified) | 1 | 3 |
| No. of digits (N = 38) | % | |
| Digit injured | ||
| Index | 1 | 3 |
| Middle | 16 | 42 |
| Ring | 12 | 32 |
| Small | 9 | 24 |
| Injured side | ||
| Right | 18 | 47 |
| Left | 20 | 53 |
| Dominant | 20 | 53 |
| Nondominant | 18 | 47 |
| Mean | ||
| Time between injury and treatment, d | 6 | |
| Initial extensor lag, deg a | 31 | |
| Swan neck deformity present, % | 22 | |
Note. ADLs = activities of daily living.
Compared with contralateral side extension.
Table 3 provides the descriptive information of the cohort comparing treatment success and treatment failure, defined by a modification of the Abouna and Brown 1 criteria as a final extensor lag <15° and a final extensor lag >15°, respectively. Those who failed splint treatment for soft tissue mallet injuries were older (mean age = 64 years) compared with those who were successfully treated with a splint (mean age = 48 years) (P = .005). This correlation between patient age and treatment success is shown in Figure 1, demonstrating greater extensor lag at final follow-up in older patients. Patients who were compliant with continuous splint use were more likely to have a successful outcome (P = .02).
Table 3.
Comparison of Characteristics Between Treatment Failure and Treatment Success.
| Mean | |||
|---|---|---|---|
| Treatment failure (N = 10) |
Treatment success (N = 28) |
P value | |
| Age, y | 64 | 48 | .005* |
| Time between injury and treatment, d | 10 | 4.7 | .39 |
| Initial extensor lag, deg | 36 | 29 | .51 |
| Duration of dorsal splint, wk | 8 | 8.2 | .73 |
| Male | 8 | 17 | .23 |
| Female | 2 | 11 | |
| Compliant | 3 | 20 | .02* |
| Noncompliant | 7 | 8 | |
| Ligamentous laxity | 2 | 6 | 1 |
| No ligamentous laxity | 8 | 22 | |
P < .05 considered significant.
Figure 1.
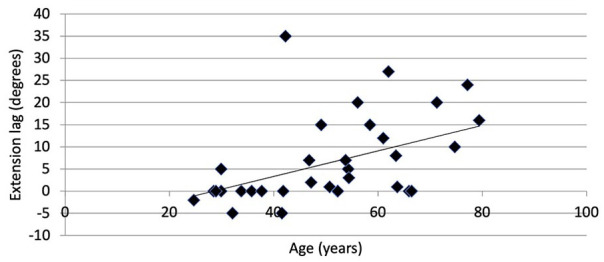
Correlation of extension lag at final visit with age. Spearman correlation coefficient R = 0.57, P = .0002. Extension lag measured clinically, compared with the contralateral side.
The remaining variables tested in this study did not have significant bearing on the success or failure of treatment. Interestingly, a patient’s final extensor lag and loss of DIP joint flexion compared with the contralateral finger showed no correlation with DASH score (R = −0.14, P = .41, and R = 0.33, P = .05, respectively). Furthermore, 83% of patients rated their DASH score at final follow-up as 0/100, indicating no subjective functional deficit despite some having final extensor lags of up to 35° (Figure 2) and loss of DIP flexion of up to 27° (Supplemental Figure 1). The highest DASH score for 2 patients (3 injured digits) was 13 (Figure 2). The final extensor lag measurements for these digits were 0°, 5°, and 24°, with DIP flexion loss of 1° and 5° in 2 digits, whereas the other had 15° greater flexion than the contralateral corresponding finger.
Figure 2.
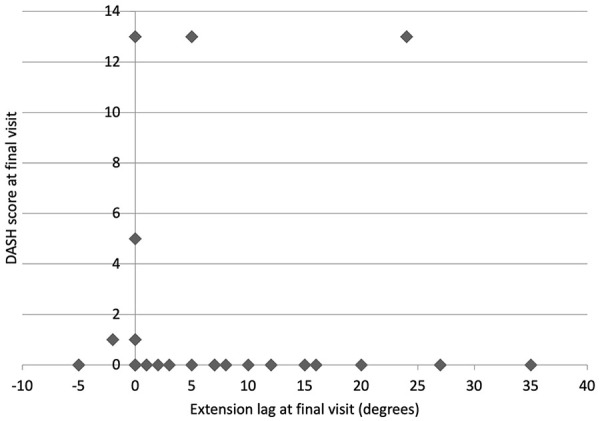
Correlation between extension lag and DASH score at final visit. Spearman correlation coefficient R = −0.14, P = .41. Extension lag measured clinically, compared with the contralateral side. DASH = Disabilities of the Arm, Shoulder, and Hand.
The extensor lag measured radiographically at final follow-up correlated closely to the extensor lag measured clinically (R = 0.84, P < .0001), overestimating the clinical lag by an average of 3° (Supplemental Figure 2).
The injured finger remained swollen, as measured clinically with observation on a 0 to 3 scale, for an average of 6 months after splinting but resolved by 1 year (Figure 3).
Figure 3.
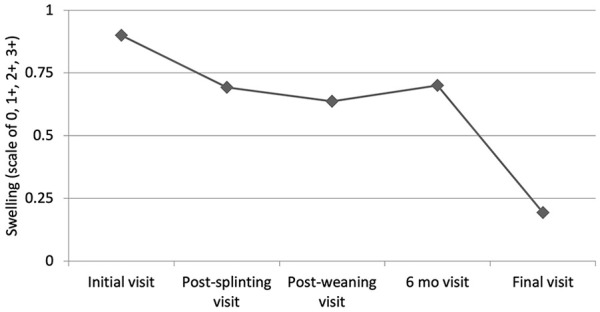
Swelling: average progression over time. Swelling graded by an attending physician on a scale of 0 (no swelling), 1+, 2+, or 3+.
Clinical extensor lag increased 6° during the splint weaning period (P = .0001); however, it subsequently decreased 4° from the end of splint weaning to final follow-up (P = .03) (Figure 4).
Figure 4.
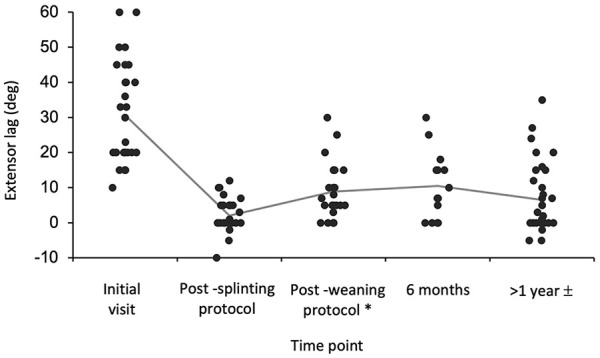
Clinical extensor lag increased during the splint weaning period.
*Extensor lag increased 6° during the splint weaning period (P < .0001).
± Extensor lag then decreased 4° from the end of splint weaning to the final follow-up time (P = .03).
Discussion
This study, in agreement with several prior studies, shows that a patient’s age is a significant factor in the success or failure of treatment of soft tissue mallet injuries with dorsal alumifoam splinting.1,8-10,12,13 For the purposes of our study, treatment failure was defined as greater than or equal to 15° of extensor lag at the final follow-up based on a modification of the original article by Abouna and Brown. 1 Based on this definition, those patients who failed treatment in our study were older (mean age = 64 years) compared to those with a successful result (mean age = 48 years). This finding provides helpful prognostic information. Older patients with this injury should be educated about the potential for some degree of residual extensor lag after splint treatment. Interestingly, DASH scores at final follow-up did not correlate with the residual extensor lag or with loss of flexion of the DIP joint. In addition, 83% of our patients had a DASH score of 0 despite some having residual extensor lags of up to 35° and a loss of DIP flexion of up to 27°. Therefore, although older individuals are less likely to obtain full correction of their extensor lag after dorsal splinting, the functional consequences are minimal. Not surprisingly, those patients who were compliant with the splint protocol were more likely to have a successful treatment outcome.
Prior studies have suggested that the time interval between injury and initiation of splinting, and the degree of extensor lag at the time of injury are factors that influence the success of splint treatment for soft tissue mallet injuries.1,9,12 Our study did not support these findings. Intuitively, one would think that these variables would, indeed, play a role in a patient’s response to treatment. The fact that our study did not confirm this may potentially be due to the limited number of patients in our study. A post hoc power analysis suggests that 138 patients would be needed to achieve the appropriate power for the observed differences to achieve statistical significance with respect to the extensor lag at the time of injury, and 612 patients would be needed to properly evaluate the time interval between injury and initiation of splinting. An alternative explanation is that several of the previously mentioned studies grouped soft tissue and bony mallet injuries together in their analysis of these factors; however, our study focused solely on soft tissue mallet injuries.
Additional factors of prognostic importance that can be gleaned from this study are that sex, the presence of ligamentous laxity, and the presence of swan neck deformity at the time of injury do not seem to influence the outcome of splinting. Furthermore, comparing those who had a successful outcome from splinting with those who did not revealed no significant difference in the duration of continuous dorsal splinting. Patients often also ask about swelling of the injured finger, and based on our results, the finger may remain swollen for at least 6 months after initiation of splinting.
Pike et al 8 discovered a relative decrease in extensor lag, indicating clinical improvement, over an interval between 12 and 24 weeks after initiation of a 6-week splinting protocol. Our results were similar; we noted that the extensor lag worsened an average of 6° during splint weaning but then improved an average of 4° from the end of splint weaning to final follow-up.
A limitation of our study is the relatively small sample size. This was due mainly to a higher than anticipated number of patients being unavailable for final follow-up when contacted for scheduling. As most patients in this study felt that they had no functional deficit regardless of the treatment outcome, it is understandable that some would think this final follow-up appointment was not worth the time and effort. The demographics of the cohort that did not return for final follow-up was similar to that of the studied cohort regarding sex (64% men), age (44 years of age), laxity (20%), timing of presentation (7 days), and initial extensor lag (33°). The average duration of follow-up for this group was 23 weeks, and at that time they reported an average VAS of 1 and an extensor lag of 3°. Although there was a high loss to final follow-up, the similarity between these groups strengthens the generalizability of the results. Nonetheless, despite our relatively small sample size, many statistical comparisons were adequately powered to reveal significant results.
In summary, our data show that for individuals treated for soft tissue mallet injuries with a dorsal alumifoam splint, older patients and noncompliant patients are more likely to have some degree of residual extensor lag after treatment; however, this is of little functional significance.
Supplemental Material
Supplemental material, sj-pdf-1-han-10.1177_15589447221093674 for A Prospective Analysis of Patient Characteristics Affecting the Outcome of Dorsal Splinting for Soft Tissue Mallet Injuries by Ali Azad, Gary Kegel, James Phelps, Astrid Marshall, Marissa P. Lafer, Madeline Rocks, Louis Catalano, O. Alton Barron and Steven Glickel in HAND
Supplemental material, sj-pdf-2-han-10.1177_15589447221093674 for A Prospective Analysis of Patient Characteristics Affecting the Outcome of Dorsal Splinting for Soft Tissue Mallet Injuries by Ali Azad, Gary Kegel, James Phelps, Astrid Marshall, Marissa P. Lafer, Madeline Rocks, Louis Catalano, O. Alton Barron and Steven Glickel in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This article does not contain any studies with human or animal subjects.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ali Azad  https://orcid.org/0000-0001-7581-8788
https://orcid.org/0000-0001-7581-8788
References
- 1. Abouna JM, Brown H. The treatment of mallet finger the results in a series of 148 consecutive cases and a review of the literature. Br J Surg. 1968;55(9):653-667. doi: 10.1002/bjs.1800550905. [DOI] [PubMed] [Google Scholar]
- 2. Stern PJ, Kastrup JJ. Complications and prognosis of treatment of mallet finger. J Hand Surg Am. 1988;13(3):329-334. doi: 10.1016/S0363-5023(88)80002-9. [DOI] [PubMed] [Google Scholar]
- 3. Doyle JR. Extensor tendons: acute injuries. In: Green DP, Hotchkiss RN, Pederson WC, eds. Green’s operative hand surgery. 4th ed. New York, NY: Churchill Livingstone; 1999:195-198. [Google Scholar]
- 4. Smit JM, Beets MR, Zeebregts CJ, et al. Treatment options for mallet finger: a review. Plast Reconstr Surg. 2010;126(5):1624-1629. doi: 10.1097/PRS.0b013e3181ef8ec8. [DOI] [PubMed] [Google Scholar]
- 5. Auchincloss JM. Mallet-finger injuries: a prospective, controlled trial of internal and external splintage. Hand. 1982;14(2):168-173. doi: 10.1016/S0072-968X(82)80011-9. [DOI] [PubMed] [Google Scholar]
- 6. Wehbe MA, Schneider LH. Mallet fractures. J Bone Jt Surg—Ser A. 1984;66(5):658-669. doi: 10.2106/00004623-198466050-00003. [DOI] [PubMed] [Google Scholar]
- 7. Niechajev IA. Conservative and operative treatment of mallet finger. Plast Reconstr Surg. 1985;76(4):580-585. doi: 10.1097/00006534-198510000-00019. [DOI] [PubMed] [Google Scholar]
- 8. Pike J, Mulpuri K, Metzger M, et al. Blinded, prospective, randomized clinical trial comparing volar, dorsal, and custom thermoplastic splinting in treatment of acute mallet finger. J Hand Surg Am. 2010;35(4):580-588. doi: 10.1016/j.jhsa.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 9. O’Brien LJ, Bailey MJ. Single blind, prospective, randomized controlled trial comparing Dorsal aluminum and custom thermoplastic splints to stack splint for acute mallet finger. Arch Phys Med Rehabil. 2011;92(2):191-198. doi: 10.1016/j.apmr.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 10. Groth GN, Wilder DM, Leroy Young V. The impact of cormpliance on the rehabilitation of patients with mallet finger injuries. J Hand Ther. 1994;7(1):21-24. doi: 10.1016/S0894-1130(12)80037-8. [DOI] [PubMed] [Google Scholar]
- 11. Garberman SF, Diao E, Peimer CA. Mallet finger: results of early versus delayed closed treatment. J Hand Surg Am. 1994;19(5):850-852. doi: 10.1016/0363-5023(94)90200-3. [DOI] [PubMed] [Google Scholar]
- 12. Warren RA, Norris SH, Ferguson DG. Mallet finger: a trial of two splints. J Hand Surg Br. 1988;13(2):151-153. doi: 10.1016/0266-7681(88)90124-6. [DOI] [PubMed] [Google Scholar]
- 13. Maitra A, Dorani B. The conservative treatment of mallet finger with a simple splint: a case report. Arch Emerg Med. 1993;10(3):244-248. doi: 10.1136/emj.10.3.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-han-10.1177_15589447221093674 for A Prospective Analysis of Patient Characteristics Affecting the Outcome of Dorsal Splinting for Soft Tissue Mallet Injuries by Ali Azad, Gary Kegel, James Phelps, Astrid Marshall, Marissa P. Lafer, Madeline Rocks, Louis Catalano, O. Alton Barron and Steven Glickel in HAND
Supplemental material, sj-pdf-2-han-10.1177_15589447221093674 for A Prospective Analysis of Patient Characteristics Affecting the Outcome of Dorsal Splinting for Soft Tissue Mallet Injuries by Ali Azad, Gary Kegel, James Phelps, Astrid Marshall, Marissa P. Lafer, Madeline Rocks, Louis Catalano, O. Alton Barron and Steven Glickel in HAND


