ABSTRACT
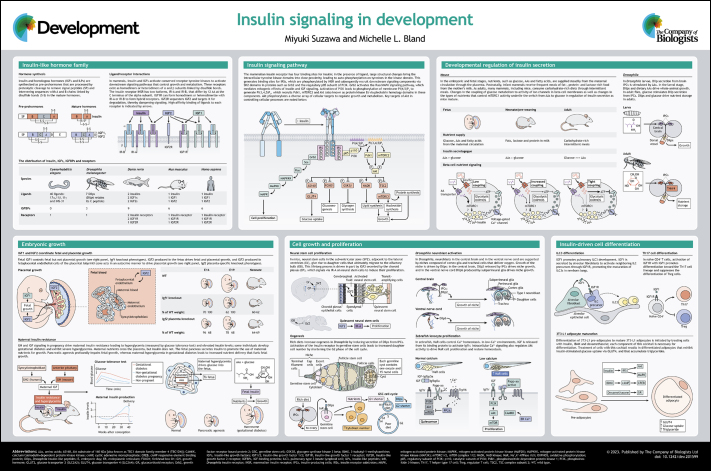
Nutrient intake is obligatory for animal growth and development, but nutrients alone are not sufficient. Indeed, insulin and homologous hormones are required for normal growth even in the presence of nutrients. These hormones communicate nutrient status between organs, allowing animals to coordinate growth and metabolism with nutrient supply. Insulin and related hormones, such as insulin-like growth factors and insulin-like peptides, play important roles in development and metabolism, with defects in insulin production and signaling leading to hyperglycemia and diabetes. Here, we describe the insulin hormone family and the signal transduction pathways activated by these hormones. We highlight the roles of insulin signaling in coordinating maternal and fetal metabolism and growth during pregnancy, and we describe how secretion of insulin is regulated at different life stages. Additionally, we discuss the roles of insulin signaling in cell growth, stem cell proliferation and cell differentiation. We provide examples of the role of insulin in development across multiple model organisms: Caenorhabditis elegans, Drosophila, zebrafish, mouse and human.
Keywords: IGF, Development, Insulin
Summary: This Development at a glance article summarizes insulin hormone family signaling and highlights the roles of individual hormones in regulating growth, cell proliferation and differentiation.
Introduction
Nutrient-sensing pathways allow animals to integrate developmental and physiological processes with nutrient availability. Insulin and insulin-like hormones coordinate nutrient supply with anabolic metabolism, cell growth and proliferation, and aging and lifespan (Kenyon, 2010). The crucial roles of insulin in regulating metabolism are well known (James et al., 2021; Saltiel, 2021), but insulin and insulin-like hormones are also important regulators of development. Here, we summarize the insulin hormone family, describe the conserved insulin signaling pathway, discuss the regulation of insulin production and highlight the roles of individual hormones in regulating growth, cell proliferation and differentiation.
See Supplementary information for a high-resolution version of the poster.
Insulin-like hormone family
Insulin and homologous hormones [insulin-like growth factors (IGFs) and insulin-like peptides (ILPs)] transmit information about nutrient availability to regulate energetically demanding processes, such as growth and nutrient storage. Discovered in late 1921 (Banting et al., 1922), insulin revolutionized the treatment of diabetes and our understanding of metabolic homeostasis, growth control and hormone signaling.
Insulin, IGFs and ILPs are synthesized as pre-prohormones. They typically consist of a signal peptide followed by contiguous B, C and A domains for insulin with additional D and E domains for IGFs. The C peptide for insulin and the E domain of IGFs are removed and disulfide bonds linking the A and B chains are formed during processing to generate the mature hormones.
The number of insulins, IGFs and ILPs varies across animals. In mammals, insulin is produced by beta cells in the islets of Langerhans in the pancreas. IGF1 is produced throughout the body in response to growth hormone (GH), with hepatocytes secreting the majority of circulating IGF1 (Stratikopoulos et al., 2008). IGF2 is highly expressed in the placenta, throughout the fetus, and in fetal and adult liver (Ekström et al., 1995; Sandovici et al., 2022). Danio rerio have two insulins that are expressed in the pancreas and four IGFs: Igf1a (now known as Igf1) and Igf2a are broadly expressed in the embryo; Igf1b (now known as Igf3) is expressed primarily in adult gonads, and Igf2b is expressed in adult liver (Papasani et al., 2006; Zou et al., 2009). Drosophila melanogaster have seven ILPs (Dilp1-Dilp7; now known as Ilp1-Ilp7) that bind and activate a single insulin receptor (Brogiolo et al., 2001; Grönke et al., 2010). Dilps are produced in distinct organs; Dilps 2, 3 and 5 are secreted by 14 insulin-like producing cells (IPCs) in the brain (Ikeya et al., 2002), whereas Dilp6 is produced by the fat body, a liver- and adipose-like organ (Okamoto et al., 2009; Slaidina et al., 2009). The Caenorhabditis elegans genome encodes 40 ILPs and a single insulin receptor, DAF-2 (Pierce et al., 2001; Zheng et al., 2018). C. elegans ILPs are grouped as α-, β- and γ-insulins based on their structures and are classified as agonists or antagonists of daf-2 phenotypes (Zheng et al., 2018).
IGF signaling is modulated by high-affinity IGF-binding proteins (IGFBPs). Six IGFBPs are encoded in mouse and human, nine in D. rerio (Daza et al., 2011), and three secreted proteins bind Dilps in Drosophila (Arquier et al., 2008; Honegger et al., 2008; Okamoto et al., 2013). No IGFBPs have yet been described in C. elegans. The majority of mammalian IGFs form ternary complexes with one of the six IGFBPs and acid labile subunit (Clemmons, 2018). IGFBPs have four major modes of action (Allard and Duan, 2018): (1) inhibiting signaling by sequestering IGFs; (2) promoting signaling following proteolytic cleavage of IGFBP that liberates bound IGF; (3) enhancing IGF signaling by locally concentrating IGFs; and (4) acting as transcriptional regulators independently of IGF.
Insulin, IGF1 and IGF2 activate downstream signaling by binding conserved receptor tyrosine kinases (RTKs). In mammals, insulin binds with high affinity to a dedicated insulin receptor with two splice forms: IR-A and IR-B. IGF1 and IGF2 bind the IGF1 receptor (IGF1R) with high affinity, and IGF2 also binds and activates IR-A. IGF2 also binds IGF2R, which primarily sequesters and internalizes IGF2, dampening IGF2 signaling. Insulin receptor and IGF1R subunits can form heterodimers with significantly higher affinity for IGF1 than for insulin (LeRoith et al., 2021).
Insulin signaling pathway
Insulin and its homologs activate a conserved intracellular signal transduction pathway to regulate anabolic processes (Haeusler et al., 2018). Insulin and IGF1 receptors are dimeric RTKs composed of two alpha and two beta subunits linked by disulfide bonds (De Meyts and Whittaker, 2002). Each alpha subunit contains two insulin-binding sites. Binding of a single insulin to the dimeric receptor at site 1 partially activates signaling, and binding of four insulins initiates structural changes that bring the intracellular tyrosine kinase domains into proximity for full receptor activation (Li et al., 2022; Scapin et al., 2018), leading to trans-phosphorylation of receptor tyrosine residues proximal to the inner membrane and in the kinase activation loop. This phosphorylation fully activates the receptor kinase domain and recruits insulin receptor substrates (IRSs) via their phosphotyrosine-binding domains. IRS proteins are phosphorylated by insulin/IGF receptors, generating Src homology 2 (SH2) domain-binding sites. Proteins recruited to IRS via SH2 domains include phosphoinositide 3-kinase (PI3K, via its regulatory p85 subunit), the adaptor Grb2, and the tyrosine phosphatase SHP2 (PTPN11) (Schmelzle et al., 2006; White, 2002).
PI3K mediates many actions of the pathway via activation of the serine-threonine kinase Akt (also known as protein kinase B). Upon recruitment to the IRS, the catalytic p110 subunit of PI3K phosphorylates phosphatidylinositol 4,5-bisphosphate [PI(4,5)P2] in the plasma membrane to generate PI(3,4,5)P3. The lipid phosphatases PTEN and SHIP2 (INPPL1) inhibit insulin signaling by dephosphorylating PI(3,4,5)P3 (Maehama and Dixon, 1998; Wada et al., 2001). PI(3,4,5)P3 recruits Akt and its upstream kinases, Pdk1 and the mTOR complex 2 (mTORC2), to the plasma membrane via their pleckstrin homology domains (Ebner et al., 2017; Franke et al., 1995; Liu et al., 2015). Pdk1 phosphorylates Akt's activation loop (Thr308 in mice) (Alessi et al., 1997), and mTORC2 phosphorylates Akt's carboxy-terminal hydrophobic motif (Ser473 in mice) (Sarbassov et al., 2005), thus activating Akt (Alessi et al., 1996).
Akt phosphorylates diverse substrates to regulate metabolism and growth (Manning and Toker, 2017); key mammalian targets are described here. Akt drives glucose uptake in muscle and adipose tissue by phosphorylating and inhibiting the Rab GTPase-activating protein AS160 (TBC1D1), a negative regulator of the insulin-sensitive glucose transporter GLUT4 (SLC2A4) (Kane et al., 2002). Akt suppresses hepatic gluconeogenesis by inactivating the transcriptional regulators FOXO1 and PGC1α (PPARGC1A) (Biggs et al., 1999; Rena et al., 1999) (Li et al., 2007), leading to reduced gluconeogenic enzyme expression. Insulin promotes glycogen storage via Akt-dependent phosphorylation and inhibition of GSK3β, a negative regulator of glycogen synthase (Cross et al., 1995). Akt stimulates cell growth by phosphorylating and inhibiting TSC2, a negative regulator of the mTOR complex 1 (mTORC1) (Inoki et al., 2002; Manning et al., 2002; Potter et al., 2002). In turn, mTORC1 phosphorylates multiple substrates to drive protein, nucleotide and lipid synthesis (Ben-Sahra and Manning, 2017). Akt activates NAD kinase to supply NADPH needed for lipogenesis (Hoxhaj et al., 2019). Akt promotes cell survival by inhibiting the pro-apoptotic transcription factor FKHRL1 (FOXO3a) and the pro-apoptotic Bcl-2 family member Bad (Brunet et al., 1999; Datta et al., 1997).
In the mitogen-activated protein kinase (MAPK) arm of the insulin pathway, Grb2 binding to IRS promotes the interaction between the guanine nucleotide exchange factor Sos and its target, the small GTPase Ras, causing MAPK pathway activation and stimulating cell proliferation (Myers et al., 1994; Skolnik et al., 1993). IGF1 has higher mitogenic potential than insulin (Pozios et al., 2001; Sasaoka et al., 1996). Some insulin receptor agonists induce biased signaling to the PI3K-Akt or the Grb2-MAPK arms (Jensen et al., 2007; Sciacca et al., 2010; Wu et al., 2022), raising the possibility that distinct analogs could be developed to control metabolism versus growth.
Developmental regulation of insulin secretion
Control of insulin secretion in mammals differs between the fetal and the adult pancreas, allowing animals to adapt to the prevailing nutrient supply. In utero, fetuses receive a steady supply of nutrients from the maternal circulation, and circulating glucose is lower and circulating amino acids are higher in fetal rodents compared with adults (Girard et al., 1973; Helman et al., 2020). The switch to intermittent feeding postnatally requires that insulin secretion is suppressed between meals to prevent hypoglycemia. Glucose-stimulated insulin secretion (GSIS) is a feature of mature pancreatic beta cells that permits responses to dietary nutrients (Ashcroft and Rorsman, 2013). Understanding how human beta cells mature is crucial for the generation of functional beta cells from induced pluripotent stem cells as a therapy for type 1 diabetes (Alvarez-Dominguez and Melton, 2022).
In humans and rodents, amino acids greatly potentiate glucose-driven insulin secretion from the fetal pancreas (Hoffman et al., 1982; Kervran and Randon, 1980), but glucose plays an increasingly dominant role in driving insulin secretion as animals mature (Bliss and Sharp, 1992; Helman et al., 2020). Changes in nutrient control of insulin release are paralleled by changes in nutrient control of mTORC1 activity. Fetal mouse and human pancreatic islets exhibit constitutive mTORC1 activity, whereas adult islets exhibit intermittent mTORC1 activity in response to dietary intake of glucose and amino acids. Constitutive activation of mTORC1 in adult mouse beta cells restores the fetal pattern of insulin secretion in response to amino acids (Helman et al., 2020) and increases beta cell mass and basal insulin secretion in vivo and in cultured islets ex vivo (Jaafar et al., 2019; Mori et al., 2009). Interestingly, weaning mice onto a fat-rich diet rather than carbohydrate-rich chow maintains elevated basal activity of mTORC1 and increases basal insulin secretion but blunts GSIS (Jaafar et al., 2019; Stolovich-Rain et al., 2015).
The control of insulin secretion in juvenile and adult stages also differs in Drosophila. The larval stage is characterized by near-constant food consumption, whereas adult flies eat intermittent meals. Amino acids are the main driver of growth in Drosophila larvae (Rodrigues et al., 2015; Shingleton et al., 2017), and the secretion of Dilps from larval IPCs is responsive to dietary protein but not to sugar (Géminard et al., 2009; Koyama and Mirth, 2016; Manière et al., 2016). However, adult IPCs secrete Dilps in response to dietary sugar (Alfa et al., 2015; Kréneisz et al., 2010; Park et al., 2014), and this switch requires activity of the transcription factor Hnf4 (Barry and Thummel, 2016; Palanker et al., 2009). Similarly, in mammals, Hnf4 acts cell-autonomously to drive beta cell maturation and GSIS (Arda et al., 2013; Gupta et al., 2005).
Embryonic growth
Mammalian embryonic and fetal growth requires a functional placenta for nutrient delivery and gas exchange. IGF signaling drives expansion of placental surface area to support fetal development in both normal pregnancy and in adverse gestational environments (Fowden et al., 2009; Sferruzzi-Perri et al., 2017). IGF2 produced by the fetus and by fetoplacental endothelial cells in the placental labyrinthine zone promotes expansion and remodeling of the placental vasculature, enhancing nutrient delivery from the maternal circulation to the fetus (Sandovici et al., 2022). Global or placental-specific deletion of Igf2 in mice results in reduced placental growth and function, leading to fetal growth restriction and a 30-40% decrease in birth weight (DeChiara et al., 1990; Liu et al., 1993; Louvi et al., 1997; Constância et al., 2002; Sibley et al., 2004). Global Igf2 deletion also leads to fetal hepatic steatosis, a phenotype observed in response to in utero nutrient deprivation (Galvan-Martinez et al., 2023; Lopez et al., 2018). In most mammals, except monotremes, IGF2 is expressed solely from the paternal allele (DeChiara et al., 1991; Giannoukakis et al., 1993; Killian et al., 2001). In humans, paternally inherited, heterozygous mutations in IGF2 impair prenatal and postnatal growth (Begemann et al., 2015; Rockstroh et al., 2019). Two human genetic disorders, Beckwith–Wiedemann and Russell–Silver syndromes, alter growth by interfering with IGF2 imprinting. Correcting prenatal IGF2 levels restores growth in mouse models of these conditions (Liao et al., 2021). IGF2R modulates IGF2 signaling. In mice, Igf2r is imprinted and expressed from the maternal allele (Kalscheuer et al., 1993). Consistent with its role in sequestering IGF2, mice with homozygous or maternally inherited, heterozygous null mutations in Igf2r exhibit fetal overgrowth (Lau et al., 1994; Louvi et al., 1997; Wang et al., 1994).
IGF1 and insulin-like hormone signaling drive growth across vertebrate and invertebrate species. In humans, loss-of-function mutations in IGF1 or IGF1R are associated with intrauterine growth impairment and postnatal growth failure (Abuzzahab et al., 2003; Woods et al., 1996). Mice lacking Igf1 are 40% smaller than wild-type littermates at birth, but placental growth is not impaired (Baker et al., 1993; Liu et al., 1993; Louvi et al., 1997; Powell-Braxton et al., 1993). Mice lacking Igf1r are 55% smaller than wild type, consistent with activation of IGF1R by IGF1 and IGF2 (Baker et al., 1993; Liu et al., 1993; Louvi et al., 1997). IGF1 plays a crucial role in determining the size of dogs, wolves, foxes, coyotes, donkeys and whales (Lai et al., 2021; Plassais et al., 2022; Silva et al., 2023; Sutter et al., 2007). In zebrafish, Igf1ra and Igf1rb double knockdown reduces embryo growth and increases apoptosis (Schlueter et al., 2007). In Drosophila, loss-of-function mutations in Dilps or components of the insulin signaling pathway lead to reduced animal size (Böhni et al., 1999; Brogiolo et al., 2001; Ikeya et al., 2002; Okamoto et al., 2009; Slaidina et al., 2009; Zhang et al., 2009). Infection and innate immune signaling inhibit growth in larvae by suppressing Dilp6 production (Suzawa et al., 2019). Similarly, young children who experience early enteric infections exhibit growth impairment and decreased circulating IGF1 (DeBoer et al., 2017). In C. elegans, DAF-2 signaling mediates body size increase in worms fed a high-quality diet (So et al., 2011; You et al., 2008).
Humans become insulin resistant during healthy pregnancy, an adaptation that spares maternal nutrients for fetal growth. Increased GH and IGF signaling during pregnancy alter maternal insulin signaling and glucose homeostasis to promote fetal glucose uptake (Napso et al., 2018). In humans, GH is encoded by GH1, expressed in anterior pituitary somatotropes, and GH2, expressed in placental syncytiotrophoblast cells. After 20 weeks of gestation, GH2 replaces GH1 in circulation (Liao et al., 2018) and stimulates maternal IGF1 secretion (Caufriez et al., 1993). Unlike primates, most mammals do not produce GH in the placenta (Papper et al., 2009). However, maternal GH and IGF1 are elevated in pregnant mice, and transgenic expression of human GH2 in pregnant mice drives maternal insulin resistance (Barbour et al., 2002; Gatford et al., 2017; Liao et al., 2016). In mice, IGF2 secreted by endocrine placental junctional zone cells is required to induce the maternal insulin resistance that supports fetal growth (Lopez-Tello et al., 2023).
During human pregnancy, gestational diabetes mellitus (GDM) can develop with hyperinsulinemia and hyperglycemia that revert after delivery (Ryan et al., 1985). In humans, obesity strongly correlates with GDM, affecting 14% of pregnancies worldwide (Wang et al., 2022). Pregnancies with GDM are associated with increased birth weight, a condition termed ‘macrosomia’ (Castillo-Castrejon and Powell, 2017; Desoye and Nolan, 2016). Maternal insulin does not cross the placenta (Adam et al., 1969); instead, maternally supplied glucose and amino acids stimulate fetal insulin secretion (Obenshain et al., 1970). Hyperglycemia that accompanies GDM leads to elevated fetal insulin levels and, consequently, increased fetal growth. These infants are at increased risk of developing obesity, type 2 diabetes and high blood pressure in adulthood (Dabelea and Crume, 2011). The mechanisms by which GDM influences fetal development may involve epigenetic changes in offspring that predispose them to disease (Sales et al., 2017). In contrast, impaired fetal insulin secretion reduces growth in utero. Complete loss of fetal insulin production occurs in individuals with pancreatic agenesis, resulting in neonatal type 1 diabetes. Loss of the fetal pancreas, congenitally in humans and mice or via pancreatectomy in animals such as mice and sheep, profoundly impairs fetal growth (Fowden, 1992; Hughes et al., 2023). Reduced fetal insulin production is associated with increased risk for type 2 diabetes in adulthood (Hughes et al., 2021).
Cell growth and proliferation
Organisms grow through coordinated increases in cell size and cell number (Jorgensen and Tyers, 2004), and insulin signaling acts in a cell-autonomous manner to promote both processes. In Drosophila, for example, loss-of-function mutations in PI3K and the IRS homolog chico lead to reduced rates of cell growth and division, leading to decreased cell size and number (Böhni et al., 1999; Britton et al., 2002), whereas activation of insulin signaling leads to increased cell size and number (Gao et al., 2000; Verdu et al., 1999). Epistasis experiments in Drosophila and in mouse embryonic fibroblasts show that control of cell size and cell number by Akt requires mTORC1 activity (Potter et al., 2002; Skeen et al., 2006). Insulin signaling also promotes hypertrophy in post-mitotic cells, such as mouse skeletal muscle (Musarò et al., 2001) and Drosophila larval fat body cells, which grow via endoreplication (Britton et al., 2002).
Systemic and local insulin signaling and nutrient availability are important regulators of stem cell renewal and differentiation (Diehl et al., 2023; Shim et al., 2013). Stem cells reside in niches that supply local signals that maintain stem cells and their progeny. In adult mice, neuronal stem cells (NSCs) in the subventricular zone (SVZ) adjacent to the lateral ventricles give rise to new neurons that migrate rostrally to the olfactory bulb where they differentiate into interneurons (Obernier and Alvarez-Buylla, 2019). IGF2, secreted by the choroid plexus epithelium and the brain vasculature into cerebrospinal fluid in the lateral ventricle, signals through IR-A to promote proliferation and maintenance of SVZ NSCs (Chidambaram et al., 2022; Lehtinen et al., 2011; Ziegler et al., 2012). Insulin signaling also promotes NSC proliferation in Drosophila. At hatching, most fly NSCs (neuroblasts) are quiescent but begin proliferating after larvae consume food (Britton and Edgar, 1998). In response to dietary protein, Dilps are released locally in the brain, activating insulin signaling in neuroblasts, leading to their reactivation from quiescence (Chell and Brand, 2010; Sousa-Nunes et al., 2011). Glial-derived Dilp6 acts in the ventral nerve cord to drive membrane expansion in cortex glia, which is crucial for neuroblast niche formation (Spéder and Brand, 2018). Following injury in the ventral nerve cord, Dilp6 also stimulates proliferation of glia and their reprogramming to become neuroblasts that promote regeneration (Harrison et al., 2021). In the larval central brain, IPC-derived Dilp2 drives cortex glia and trachea growth and promotes neuroblast reactivation from quiescence in newly hatched larvae (Yuan et al., 2020).
In Drosophila, endocrine insulin signaling links nutrient availability with germline stem cell (GSC) proliferation and maintenance, supporting fecundity. The adult Drosophila ovary consists of multiple ovarioles, each containing a sequence of progressively more mature egg chambers. Egg chamber assembly takes place in a germarium that contains GSCs, which give rise to oocytes and their niche (comprised of terminal filament, cap and escort cells) (Kirilly and Xie, 2007). Protein-rich diets drive oogenesis in an insulin-dependent manner. IPC-derived Dilps increase GSC proliferation rate, thereby increasing daughter cell numbers without affecting total stem cell numbers (Drummond-Barbosa and Spradling, 2001; Hsu et al., 2008; Ikeya et al., 2002; LaFever and Drummond-Barbosa, 2005). Insulin signaling indirectly regulates GSCs by increasing cap cell numbers in the stem cell niche and promoting interaction between cap cells and GSCs (Hsu and Drummond-Barbosa, 2009, 2011).
Insulin signaling also drives proliferation of differentiated cells, such as zebrafish ionocytes, which maintain ion homeostasis. Ionocytes in the gills in adults or in the yolk sac epithelium in zebrafish embryos and larvae actively take up ions from the water, reduce passive ion loss and excrete waste ions (Yan and Hwang, 2019). Na+,K+-ATPase-rich (NaR) cells maintain calcium (Ca2+) homeostasis. In response to low environmental Ca2+, IGF1 signaling induces NaR cell proliferation to increase Ca2+ uptake. NaR cells specifically express Igfbp5a that binds IGF1, and low Ca2+ levels lead to increased Igfbp5a expression (Dai et al., 2014). Low Ca2+ activates the zinc metalloproteinase Papp-aa, which is constitutively expressed by NaR cells and cleaves Igfbp5a, freeing IGF1 to bind to its receptor (Li et al., 2021; Liu et al., 2020). NaR cell proliferation is also regulated by modulating intracellular insulin signaling. Ca2+ entry through the TrpV6 Ca2+ channel in normal conditions activates the serine-threonine phosphatase PP2A to inhibit Akt (Xin et al., 2019), and release of Ca2+ from endoplasmic reticulum stores in low Ca2+ environments promotes Akt activation (Xin et al., 2021).
Insulin signaling and coordination of developmental timing
In multiple contexts, insulin-like hormones coordinate the timing of developmental processes. For example, signaling through IGF1R regulates timing of hair cell differentiation in the mouse cochlea. Reduced IGF1R signaling delays expression of the transcription factor Atoh1, leading to reduced cochlear hair cell number and altered development of the vestibular system (Okano et al., 2011). Similarly, in the Drosophila eye imaginal disc, increased insulin signaling leads to precocious differentiation of photoreceptors, and decreased insulin signaling delays differentiation (Bateman and McNeill, 2004). In Drosophila and C. elegans, insulin signaling regulates developmental timing and maturation of the whole animal (Baugh, 2013; Tennessen and Thummel, 2011). Insulin signaling in the prothoracic gland of Drosophila larvae promotes production of the steroid hormone ecdysone, which drives progression through each stage of the fly life cycle (Colombani et al., 2005; Layalle et al., 2008; Mirth et al., 2005). Similarly, the insulin receptor homolog DAF-2 acts non-cell-autonomously to direct progression of C. elegans larvae to adulthood (Apfeld and Kenyon, 1998; Hung et al., 2014; Kimura et al., 1997).
Insulin-driven cell differentiation
Insulin signaling directly influences differentiation in multiple cell types. For example, in developing mouse lung, IGF1 secreted by alveolar fibroblasts activates IGF1R in neighboring innate lymphoid cell precursors to instruct expansion and maturation of pulmonary type 3 innate lymphoid cells (Oherle et al., 2020). IGF1 acts early in differentiation of naïve CD4+ T cells to bias cell fate toward the T helper type 17 (Th17) lineage and suppress differentiation of regulatory T (Treg) cells (DiToro et al., 2020). In Drosophila, larval hematopoietic progenitor cells are induced to differentiate into mature blood cells in response to starvation. In fed animals, Dilp2 secreted by IPCs stimulates mTORC1 signaling, which maintains hematopoietic progenitors in an undifferentiated, proliferative state (Shim et al., 2013).
Insulin promotes differentiation of mammalian white adipocytes, which store excess nutrients as triglycerides. Mechanisms of adipocyte differentiation from mesenchymal stem cells were defined in 3T3-L1 mouse fibroblast cells, which can differentiate into triglyceride-laden adipocytes. Factors driving 3T3-L1 differentiation include insulin and IGF1, acting through their respective receptors, and cAMP and the glucocorticoid receptor agonist dexamethasone (Green and Kehinde, 1975; Rubin et al., 1978; Smith et al., 1988). Insulin regulates adipocyte differentiation by promoting lipid storage, both by increasing glucose uptake and by inhibiting lipolysis (Czech et al., 2013). Subsequent work has revealed the transcriptional programs underlying differentiation of preadipocytes into mature adipocytes (Cristancho and Lazar, 2011).
Perspectives
Insulin signaling connects nutrient availability with growth and development. Some animals change the nutrient control of insulin secretion to match the prevailing nutrient supply. However, even in nutrient-rich environments, impaired insulin signaling leads to growth defects and developmental delay. Adverse conditions, such as starvation and infection, lead to reduced insulin signaling that slows growth and allows animals to conserve energy or redirect nutrients to processes such as immunity. Whether crosstalk between signaling pathways or changes in nutrient availability disrupt insulin signaling in response to stressors, such as infection, remains to be determined.
Insulin signaling in development impacts not only animal growth in the short term but also metabolic physiology well after the growth period. Both increased and decreased fetal insulin production in utero predispose individuals to metabolic disease later in life. A key question is what mechanisms contribute to such similar long-term outcomes in individuals with opposite in utero growth environments.
How the diversity of insulin-like hormones, IGFBPs and insulin/IGF receptors contributes to the many roles of insulin signaling in development is under investigation. What information do distinct IGFs and ILPs convey to their target tissues? Do distinct hormones differentially activate PI3K-Akt or MAPK signaling downstream of the insulin receptor? How does cellular context affect the outcome of insulin signaling? The most downstream effectors of insulin signaling in development are not as well understood as those that participate in metabolic processes controlled by insulin, such as glucose uptake. Do developmental roles of insulin employ known or novel effectors to control processes such as proliferation and differentiation? Answering these questions will expand our understanding of development and the myriad roles played by this crucial hormone family.
Poster
Acknowledgements
We thank Joseph J. Hill for assistance with graphic design. We regret that we were unable to cite other important original research papers owing to space limitations.
Footnotes
Funding
Research in the Bland lab is supported by the National Institutes of Health (1R01DK123433 to M.L.B.). Deposited in PMC for release after 12 months.
High-resolution poster
A high-resolution version of the poster is available for downloading at https://journals.biologists.com/dev/article-lookup/doi/10.1242/dev.201599#supplementary-data
References
- Abuzzahab, M. J., Schneider, A., Goddard, A., Grigorescu, F., Lautier, C., Keller, E., Kiess, W., Klammt, J., Kratzsch, J., Osgood, D.et al. (2003). IGF-I receptor mutations resulting in intrauterine and postnatal growth retardation. N. Engl. J. Med. 349, 2211-2222. 10.1056/NEJMoa010107 [DOI] [PubMed] [Google Scholar]
- Adam, P. A., Teramo, K., Raiha, N., Gitlin, D. and Schwartz, R. (1969). Human fetal insulin metabolism early in gestation. Response to acute elevation of the fetal glucose concentration and placental transfer of human insulin-I-131. Diabetes 18, 409-416. 10.2337/diab.18.6.409 [DOI] [PubMed] [Google Scholar]
- Alessi, D. R., Andjelkovic, M., Caudwell, B., Cron, P., Morrice, N., Cohen, P. and Hemmings, B. A. (1996). Mechanism of activation of protein kinase B by insulin and IGF-1. EMBO J. 15, 6541-6551. 10.1002/j.1460-2075.1996.tb01045.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alessi, D. R., James, S. R., Downes, C. P., Holmes, A. B., Gaffney, P. R., Reese, C. B. and Cohen, P. (1997). Characterization of a 3-phosphoinositide-dependent protein kinase which phosphorylates and activates protein kinase Balpha. Curr. Biol. 7, 261-269. 10.1016/S0960-9822(06)00122-9 [DOI] [PubMed] [Google Scholar]
- Alfa, R. W., Park, S., Skelly, K.-R., Poffenberger, G., Jain, N., Gu, X., Kockel, L., Wang, J., Liu, Y., Powers, A. C.et al. (2015). Suppression of insulin production and secretion by a decretin hormone. Cell Metab. 21, 323-334. 10.1016/j.cmet.2015.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allard, J. B. and Duan, C. (2018). IGF-binding proteins: why do they exist and why are there so many? Front. Endocrinol. 9, 117. 10.3389/fendo.2018.00117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez-Dominguez, J. R. and Melton, D. A. (2022). Cell maturation: hallmarks, triggers, and manipulation. Cell 185, 235-249. 10.1016/j.cell.2021.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apfeld, J. and Kenyon, C. (1998). Cell nonautonomy of C. elegans daf-2 function in the regulation of diapause and life span. Cell 95, 199-210. 10.1016/S0092-8674(00)81751-1 [DOI] [PubMed] [Google Scholar]
- Arda, H. E., Benitez, C. M. and Kim, S. K. (2013). Gene regulatory networks governing pancreas development. Dev. Cell 25, 5-13. 10.1016/j.devcel.2013.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arquier, N., Géminard, C., Bourouis, M., Jarretou, G., Honegger, B., Paix, A. and Léopold, P. (2008). Drosophila ALS regulates growth and metabolism through functional interaction with insulin-like peptides. Cell Metab. 7, 333-338. 10.1016/j.cmet.2008.02.003 [DOI] [PubMed] [Google Scholar]
- Ashcroft, F. M. and Rorsman, P. (2013). K(ATP) channels and islet hormone secretion: new insights and controversies. Nat. Rev. Endocrinol. 9, 660-669. 10.1038/nrendo.2013.166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker, J., Liu, J. P., Robertson, E. J. and Efstratiadis, A. (1993). Role of insulin-like growth factors in embryonic and postnatal growth. Cell 75, 73-82. 10.1016/S0092-8674(05)80085-6 [DOI] [PubMed] [Google Scholar]
- Banting, F. G., Best, C. H., Collip, J. B., Campbell, W. R. and Fletcher, A. A. (1922). Pancreatic extracts in the treatment of diabetes mellitus. Can. Med. Assoc. J. 12, 141-146. [PMC free article] [PubMed] [Google Scholar]
- Barbour, L. A., Shao, J., Qiao, L., Pulawa, L. K., Jensen, D. R., Bartke, A., Garrity, M., Draznin, B. and Friedman, J. E. (2002). Human placental growth hormone causes severe insulin resistance in transgenic mice. Am. J. Obstet. Gynecol. 186, 512-517. 10.1067/mob.2002.121256 [DOI] [PubMed] [Google Scholar]
- Barry, W. E. and Thummel, C. S. (2016). The Drosophila HNF4 nuclear receptor promotes glucose-stimulated insulin secretion and mitochondrial function in adults. eLife 5, e11183. 10.7554/eLife.11183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateman, J. M. and Mcneill, H. (2004). Temporal control of differentiation by the insulin receptor/tor pathway in Drosophila. Cell 119, 87-96. 10.1016/j.cell.2004.08.028 [DOI] [PubMed] [Google Scholar]
- Baugh, L. R. (2013). To grow or not to grow: nutritional control of development during Caenorhabditis elegans L1 arrest. Genetics 194, 539-555. 10.1534/genetics.113.150847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begemann, M., Zirn, B., Santen, G., Wirthgen, E., Soellner, L., Büttel, H.-M., Schweizer, R., Van Workum, W., Binder, G. and Eggermann, T. (2015). Paternally inherited IGF2 mutation and growth restriction. N. Engl. J. Med. 373, 349-356. 10.1056/NEJMoa1415227 [DOI] [PubMed] [Google Scholar]
- Ben-Sahra, I. and Manning, B. D. (2017). mTORC1 signaling and the metabolic control of cell growth. Curr. Opin. Cell Biol. 45, 72-82. 10.1016/j.ceb.2017.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggs, W. H., Meisenhelder, J., Hunter, T., Cavenee, W. K. and Arden, K. C. (1999). Protein kinase B/Akt-mediated phosphorylation promotes nuclear exclusion of the winged helix transcription factor FKHR1. Proc. Natl. Acad. Sci. USA 96, 7421-7426. 10.1073/pnas.96.13.7421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bliss, C. R. and Sharp, G. W. (1992). Glucose-induced insulin release in islets of young rats: time-dependent potentiation and effects of 2-bromostearate. Am. J. Physiol. 263, E890-E896. [DOI] [PubMed] [Google Scholar]
- Böhni, R., Riesgo-Escovar, J., Oldham, S., Brogiolo, W., Stocker, H., Andruss, B. F., Beckingham, K. and Hafen, E. (1999). Autonomous control of cell and organ size by CHICO, a Drosophila homolog of vertebrate IRS1-4. Cell 97, 865-875. 10.1016/S0092-8674(00)80799-0 [DOI] [PubMed] [Google Scholar]
- Britton, J. S. and Edgar, B. A. (1998). Environmental control of the cell cycle in Drosophila: nutrition activates mitotic and endoreplicative cells by distinct mechanisms. Development 125, 2149-2158. 10.1242/dev.125.11.2149 [DOI] [PubMed] [Google Scholar]
- Britton, J. S., Lockwood, W. K., Li, L., Cohen, S. M. and Edgar, B. A. (2002). Drosophila’s insulin/PI3-kinase pathway coordinates cellular metabolism with nutritional conditions. Dev. Cell 2, 239-249. 10.1016/S1534-5807(02)00117-X [DOI] [PubMed] [Google Scholar]
- Brogiolo, W., Stocker, H., Ikeya, T., Rintelen, F., Fernandez, R. and Hafen, E. (2001). An evolutionarily conserved function of the Drosophila insulin receptor and insulin-like peptides in growth control. Curr. Biol. 11, 213-221. 10.1016/S0960-9822(01)00068-9 [DOI] [PubMed] [Google Scholar]
- Brunet, A., Bonni, A., Zigmond, M. J., Lin, M. Z., Juo, P., Hu, L. S., Anderson, M. J., Arden, K. C., Blenis, J. and Greenberg, M. E. (1999). Akt promotes cell survival by phosphorylating and inhibiting a Forkhead transcription factor. Cell 96, 857-868. 10.1016/S0092-8674(00)80595-4 [DOI] [PubMed] [Google Scholar]
- Castillo-Castrejon, M. and Powell, T. L. (2017). Placental nutrient transport in gestational diabetic pregnancies. Front. Endocrinol. 8, 306. 10.3389/fendo.2017.00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caufriez, A., Frankenne, F., Hennen, G. and Copinschi, G. (1993). Regulation of maternal IGF-I by placental GH in normal and abnormal human pregnancies. Am. J. Physiol. 265, E572-E577. [DOI] [PubMed] [Google Scholar]
- Chell, J. M. and Brand, A. H. (2010). Nutrition-responsive glia control exit of neural stem cells from quiescence. Cell 143, 1161-1173. 10.1016/j.cell.2010.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chidambaram, S., Velloso, F. J., Rothbard, D. E., Deshpande, K., Cajuste, Y., Snyder, K. M., Fajardo, E., Fiser, A., Tapinos, N., Levison, S. W.et al. (2022). Subventricular zone adult mouse neural stem cells require insulin receptor for self-renewal. Stem Cell Rep. 17, 1411-1427. 10.1016/j.stemcr.2022.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemmons, D. R. (2018). Role of IGF-binding proteins in regulating IGF responses to changes in metabolism. J. Mol. Endocrinol. 61, T139-T169. 10.1530/JME-18-0016 [DOI] [PubMed] [Google Scholar]
- Colombani, J., Bianchini, L., Layalle, S., Pondeville, E., Dauphin-Villemant, C., Antoniewski, C., Carré, C., Noselli, S. and Léopold, P. (2005). Antagonistic actions of ecdysone and insulins determine final size in Drosophila. Science 310, 667-670. 10.1126/science.1119432 [DOI] [PubMed] [Google Scholar]
- Constância, M., Hemberger, M., Hughes, J., Dean, W., Ferguson-Smith, A., Fundele, R., Stewart, F., Kelsey, G., Fowden, A., Sibley, C.et al. (2002). Placental-specific IGF-II is a major modulator of placental and fetal growth. Nature 417, 945-948. 10.1038/nature00819 [DOI] [PubMed] [Google Scholar]
- Cristancho, A. G. and Lazar, M. A. (2011). Forming functional fat: a growing understanding of adipocyte differentiation. Nat. Rev. Mol. Cell Biol. 12, 722-734. 10.1038/nrm3198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross, D. A., Alessi, D. R., Cohen, P., Andjelkovich, M. and Hemmings, B. A. (1995). Inhibition of glycogen synthase kinase-3 by insulin mediated by protein kinase B. Nature 378, 785-789. 10.1038/378785a0 [DOI] [PubMed] [Google Scholar]
- Czech, M. P., Tencerova, M., Pedersen, D. J. and Aouadi, M. (2013). Insulin signalling mechanisms for triacylglycerol storage. Diabetologia 56, 949-964. 10.1007/s00125-013-2869-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dabelea, D. and Crume, T. (2011). Maternal environment and the transgenerational cycle of obesity and diabetes. Diabetes 60, 1849-1855. 10.2337/db11-0400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai, W., Bai, Y., Hebda, L., Zhong, X., Liu, J., Kao, J. and Duan, C. (2014). Calcium deficiency-induced and TRP channel-regulated IGF1R-PI3K-Akt signaling regulates abnormal epithelial cell proliferation. Cell Death Differ. 21, 568-581. 10.1038/cdd.2013.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datta, S. R., Dudek, H., Tao, X., Masters, S., Fu, H., Gotoh, Y. and Greenberg, M. E. (1997). Akt phosphorylation of BAD couples survival signals to the cell-intrinsic death machinery. Cell 91, 231-241. 10.1016/S0092-8674(00)80405-5 [DOI] [PubMed] [Google Scholar]
- Daza, D. O., Sundström, G., Bergqvist, C. A., Duan, C. and Larhammar, D. (2011). Evolution of the insulin-like growth factor binding protein (IGFBP) family. Endocrinology 152, 2278-2289. 10.1210/en.2011-0047 [DOI] [PubMed] [Google Scholar]
- De Meyts, P. and Whittaker, J. (2002). Structural biology of insulin and IGF1 receptors: implications for drug design. Nat. Rev. Drug Discov. 1, 769-783. 10.1038/nrd917 [DOI] [PubMed] [Google Scholar]
- Deboer, M. D., Scharf, R. J., Leite, A. M., Férrer, A., Havt, A., Pinkerton, R., Lima, A. A. and Guerrant, R. L. (2017). Systemic inflammation, growth factors, and linear growth in the setting of infection and malnutrition. Nutrition 33, 248-253. 10.1016/j.nut.2016.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeChiara, T. M., Efstratiadis, A. and Robertson, E. J. (1990). A growth-deficiency phenotype in heterozygous mice carrying an insulin-like growth factor II gene disrupted by targeting. Nature 345, 78-80. 10.1038/345078a0 [DOI] [PubMed] [Google Scholar]
- DeChiara, T. M., Robertson, E. J. and Efstratiadis, A. (1991). Parental imprinting of the mouse insulin-like growth factor II gene. Cell 64, 849-859. 10.1016/0092-8674(91)90513-X [DOI] [PubMed] [Google Scholar]
- Desoye, G. and Nolan, C. J. (2016). The fetal glucose steal: an underappreciated phenomenon in diabetic pregnancy. Diabetologia 59, 1089-1094. 10.1007/s00125-016-3931-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl, F. F., Sapp, K. M. and Vander Heiden, M. G. (2023). The bidirectional relationship between metabolism and cell cycle control. Trends Cell Biol. 10.1016/j.tcb.2023.05.012 [DOI] [PubMed] [Google Scholar]
- Ditoro, D., Harbour, S. N., Bando, J. K., Benavides, G., Witte, S., Laufer, V. A., Moseley, C., Singer, J. R., Frey, B., Turner, H.et al. (2020). Insulin-like growth factors are key regulators of T helper 17 regulatory T cell balance in autoimmunity. Immunity 52, 650-667.e10. 10.1016/j.immuni.2020.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond-Barbosa, D. and Spradling, A. C. (2001). Stem cells and their progeny respond to nutritional changes during Drosophila oogenesis. Dev. Biol. 231, 265-278. 10.1006/dbio.2000.0135 [DOI] [PubMed] [Google Scholar]
- Ebner, M., Sinkovics, B., Szczygieł, M., Ribeiro, D. W. and Yudushkin, I. (2017). Localization of mTORC2 activity inside cells. J. Cell Biol. 216, 343-353. 10.1083/jcb.201610060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekström, T. J., Cui, H., Li, X. and Ohlsson, R. (1995). Promoter-specific IGF2 imprinting status and its plasticity during human liver development. Development 121, 309-316. 10.1242/dev.121.2.309 [DOI] [PubMed] [Google Scholar]
- Fowden, A. L. (1992). The role of insulin in fetal growth. Early Hum. Dev. 29, 177-181. 10.1016/0378-3782(92)90135-4 [DOI] [PubMed] [Google Scholar]
- Fowden, A. L., Sferruzzi-Perri, A. N., Coan, P. M., Constancia, M. and Burton, G. J. (2009). Placental efficiency and adaptation: endocrine regulation. J. Physiol. 587, 3459-3472. 10.1113/jphysiol.2009.173013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franke, T. F., Yang, S. I., Chan, T. O., Datta, K., Kazlauskas, A., Morrison, D. K., Kaplan, D. R. and Tsichlis, P. N. (1995). The protein kinase encoded by the Akt proto-oncogene is a target of the PDGF-activated phosphatidylinositol 3-kinase. Cell 81, 727-736. 10.1016/0092-8674(95)90534-0 [DOI] [PubMed] [Google Scholar]
- Galvan-Martinez, D. H., Bosquez-Mendoza, V. M., Ruiz-Noa, Y., Ibarra-Reynoso, L. D. R., Barbosa-Sabanero, G. and Lazo-De-La-Vega-Monroy, M.-L. (2023). Nutritional, pharmacological, and environmental programming of NAFLD in early life. Am. J. Physiol. Gastrointest. Liver Physiol. 324, G99-G114. 10.1152/ajpgi.00168.2022 [DOI] [PubMed] [Google Scholar]
- Gao, X., Neufeld, T. P. and Pan, D. (2000). Drosophila PTEN regulates cell growth and proliferation through PI3K-dependent and -independent pathways. Dev. Biol. 221, 404-418. 10.1006/dbio.2000.9680 [DOI] [PubMed] [Google Scholar]
- Gatford, K. L., Muhlhausler, B. S., Huang, L., Sim, P. S.-L., Roberts, C. T., Velhuis, J. D. and Chen, C. (2017). Rising maternal circulating GH during murine pregnancy suggests placental regulation. Endocr. Connect. 6, 260-266. 10.1530/EC-17-0032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Géminard, C., Rulifson, E. J. and Léopold, P. (2009). Remote control of insulin secretion by fat cells in Drosophila. Cell Metab. 10, 199-207. 10.1016/j.cmet.2009.08.002 [DOI] [PubMed] [Google Scholar]
- Giannoukakis, N., Deal, C., Paquette, J., Goodyer, C. G. and Polychronakos, C. (1993). Parental genomic imprinting of the human IGF2 gene. Nat. Genet. 4, 98-101. 10.1038/ng0593-98 [DOI] [PubMed] [Google Scholar]
- Girard, J. R., Cuendet, G. S., Marliss, E. B., Kervran, A., Rieutort, M. and Assan, R. (1973). Fuels, hormones, and liver metabolism at term and during the early postnatal period in the rat. J. Clin. Invest. 52, 3190-3200. 10.1172/JCI107519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green, H. and Kehinde, O. (1975). An established preadipose cell line and its differentiation in culture. II. Factors affecting the adipose conversion. Cell 5, 19-27. 10.1016/0092-8674(75)90087-2 [DOI] [PubMed] [Google Scholar]
- Grönke, S., Clarke, D.-F., Broughton, S., Andrews, T. D. and Partridge, L. (2010). Molecular evolution and functional characterization of Drosophila insulin-like peptides. PLoS Genet. 6, e1000857. 10.1371/journal.pgen.1000857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta, R. K., Vatamaniuk, M. Z., Lee, C. S., Flaschen, R. C., Fulmer, J. T., Matschinsky, F. M., Duncan, S. A. and Kaestner, K. H. (2005). The MODY1 gene HNF-4alpha regulates selected genes involved in insulin secretion. J. Clin. Invest. 115, 1006-1015. 10.1172/JCI200522365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeusler, R. A., Mcgraw, T. E. and Accili, D. (2018). Biochemical and cellular properties of insulin receptor signalling. Nat. Rev. Mol. Cell Biol. 19, 31-44. 10.1038/nrm.2017.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison, N. J., Connolly, E., Gascón Gubieda, A., Yang, Z., Altenhein, B., Losada Perez, M., Moreira, M., Sun, J. and Hidalgo, A. (2021). Regenerative neurogenic response from glia requires insulin-driven neuron-glia communication. eLife 10, e58756. 10.7554/eLife.58756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helman, A., Cangelosi, A. L., Davis, J. C., Pham, Q., Rothman, A., Faust, A. L., Straubhaar, J. R., Sabatini, D. M. and Melton, D. A. (2020). A nutrient-sensing transition at birth triggers glucose-responsive insulin secretion. Cell Metab. 31, 1004-1016.e5. 10.1016/j.cmet.2020.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman, L., Mandel, T. E., Carter, W. M., Koulmanda, M. and Martin, F. I. (1982). Insulin secretion by fetal human pancreas in organ culture. Diabetologia 23, 426-430. 10.1007/BF00260956 [DOI] [PubMed] [Google Scholar]
- Honegger, B., Galic, M., Köhler, K., Wittwer, F., Brogiolo, W., Hafen, E. and Stocker, H. (2008). Imp-L2, a putative homolog of vertebrate IGF-binding protein 7, counteracts insulin signaling in Drosophila and is essential for starvation resistance. J. Biol. 7, 10. 10.1186/jbiol72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoxhaj, G., Ben-Sahra, I., Lockwood, S. E., Timson, R. C., Byles, V., Henning, G. T., Gao, P., Selfors, L. M., Asara, J. M. and Manning, B. D. (2019). Direct stimulation of NADP+ synthesis through Akt-mediated phosphorylation of NAD kinase. Science 363, 1088-1092. 10.1126/science.aau3903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu, H.-J. and Drummond-Barbosa, D. (2009). Insulin levels control female germline stem cell maintenance via the niche in Drosophila. Proc. Natl. Acad. Sci. USA 106, 1117-1121. 10.1073/pnas.0809144106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu, H.-J. and Drummond-Barbosa, D. (2011). Insulin signals control the competence of the Drosophila female germline stem cell niche to respond to Notch ligands. Dev. Biol. 350, 290-300. 10.1016/j.ydbio.2010.11.032 [DOI] [PubMed] [Google Scholar]
- Hsu, H.-J., Lafever, L. and Drummond-Barbosa, D. (2008). Diet controls normal and tumorous germline stem cells via insulin-dependent and -independent mechanisms in Drosophila. Dev. Biol. 313, 700-712. 10.1016/j.ydbio.2007.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, A. E., Hattersley, A. T., Flanagan, S. E. and Freathy, R. M. (2021). Two decades since the fetal insulin hypothesis: what have we learned from genetics? Diabetologia 64, 717-726. 10.1007/s00125-021-05386-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, A. E., De Franco, E., Freathy, R. M., Fetal Insulin and Growth Consortium, Flanagan, S. E. and Hattersley, A. T. (2023). Monogenic disease analysis establishes that fetal insulin accounts for half of human fetal growth. J. Clin. Invest. 133, e165402. 10.1172/JCI165402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung, W. L., Wang, Y., Chitturi, J. and Zhen, M. (2014). A Caenorhabditis elegans developmental decision requires insulin signaling-mediated neuron-intestine communication. Development 141, 1767-1779. 10.1242/dev.103846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeya, T., Galic, M., Belawat, P., Nairz, K. and Hafen, E. (2002). Nutrient-dependent expression of insulin-like peptides from neuroendocrine cells in the CNS contributes to growth regulation in Drosophila. Curr. Biol. 12, 1293-1300. 10.1016/S0960-9822(02)01043-6 [DOI] [PubMed] [Google Scholar]
- Inoki, K., Li, Y., Zhu, T., Wu, J. and Guan, K.-L. (2002). TSC2 is phosphorylated and inhibited by Akt and suppresses mTOR signalling. Nat. Cell Biol. 4, 648-657. 10.1038/ncb839 [DOI] [PubMed] [Google Scholar]
- Jaafar, R., Tran, S., Shah, A. N., Sun, G., Valdearcos, M., Marchetti, P., Masini, M., Swisa, A., Giacometti, S., Bernal-Mizrachi, E.et al. (2019). mTORC1 to AMPK switching underlies β-cell metabolic plasticity during maturation and diabetes. J. Clin. Invest. 129, 4124-4137. 10.1172/JCI127021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James, D. E., Stöckli, J. and Birnbaum, M. J. (2021). The aetiology and molecular landscape of insulin resistance. Nat. Rev. Mol. Cell Biol. 22, 751-771. 10.1038/s41580-021-00390-6 [DOI] [PubMed] [Google Scholar]
- Jensen, M., Hansen, B., De Meyts, P., Schäffer, L. and Ursø, B. (2007). Activation of the insulin receptor by insulin and a synthetic peptide leads to divergent metabolic and mitogenic signaling and responses. J. Biol. Chem. 282, 35179-35186. 10.1074/jbc.M704599200 [DOI] [PubMed] [Google Scholar]
- Jorgensen, P. and Tyers, M. (2004). How cells coordinate growth and division. Curr. Biol. 14, R1014-R1027. 10.1016/j.cub.2004.11.027 [DOI] [PubMed] [Google Scholar]
- Kalscheuer, V. M., Mariman, E. C., Schepens, M. T., Rehder, H. and Ropers, H. H. (1993). The insulin-like growth factor type-2 receptor gene is imprinted in the mouse but not in humans. Nat. Genet. 5, 74-78. 10.1038/ng0993-74 [DOI] [PubMed] [Google Scholar]
- Kane, S., Sano, H., Liu, S. C. H., Asara, J. M., Lane, W. S., Garner, C. C. and Lienhard, G. E. (2002). A method to identify serine kinase substrates. Akt phosphorylates a novel adipocyte protein with a Rab GTPase-activating protein (GAP) domain. J. Biol. Chem. 277, 22115-22118. 10.1074/jbc.C200198200 [DOI] [PubMed] [Google Scholar]
- Kenyon, C. J. (2010). The genetics of ageing. Nature 464, 504-512. 10.1038/nature08980 [DOI] [PubMed] [Google Scholar]
- Kervran, A. and Randon, J. (1980). Development of insulin release by fetal rat pancreas in vitro: effects of glucose, amino acids, and theophylline. Diabetes 29, 673-678. 10.2337/diab.29.9.673 [DOI] [PubMed] [Google Scholar]
- Killian, J. K., Nolan, C. M., Stewart, N., Munday, B. L., Andersen, N. A., Nicol, S. and Jirtle, R. L. (2001). Monotreme IGF2 expression and ancestral origin of genomic imprinting. J. Exp. Zool. 291, 205-212. 10.1002/jez.1070 [DOI] [PubMed] [Google Scholar]
- Kimura, K. D., Tissenbaum, H. A., Liu, Y. and Ruvkun, G. (1997). daf-2, an insulin receptor-like gene that regulates longevity and diapause in Caenorhabditis elegans. Science 277, 942-946. 10.1126/science.277.5328.942 [DOI] [PubMed] [Google Scholar]
- Kirilly, D. and Xie, T. (2007). The Drosophila ovary: an active stem cell community. Cell Res. 17, 15-25. 10.1038/sj.cr.7310123 [DOI] [PubMed] [Google Scholar]
- Koyama, T. and Mirth, C. K. (2016). Growth-blocking peptides as nutrition-sensitive signals for insulin secretion and body size regulation. PLoS Biol. 14, e1002392. 10.1371/journal.pbio.1002392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kréneisz, O., Chen, X., Fridell, Y.-W. C. and Mulkey, D. K. (2010). Glucose increases activity and Ca2+ in insulin-producing cells of adult Drosophila. Neuroreport 21, 1116-1120. 10.1097/WNR.0b013e3283409200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafever, L. and Drummond-Barbosa, D. (2005). Direct control of germline stem cell division and cyst growth by neural insulin in Drosophila. Science 309, 1071-1073. 10.1126/science.1111410 [DOI] [PubMed] [Google Scholar]
- Lai, Z., Wu, F., Li, M., Bai, F., Gao, Y., Yu, J., Li, H., Lei, C. and Dang, R. (2021). Tissue expression profile, polymorphism of IGF1 gene and its effect on body size traits of Dezhou donkey. Gene 766, 145118. 10.1016/j.gene.2020.145118 [DOI] [PubMed] [Google Scholar]
- Lau, M. M., Stewart, C. E., Liu, Z., Bhatt, H., Rotwein, P. and Stewart, C. L. (1994). Loss of the imprinted IGF2/cation-independent mannose 6-phosphate receptor results in fetal overgrowth and perinatal lethality. Genes Dev. 8, 2953-2963. 10.1101/gad.8.24.2953 [DOI] [PubMed] [Google Scholar]
- Layalle, S., Arquier, N. and Léopold, P. (2008). The TOR pathway couples nutrition and developmental timing in Drosophila. Dev. Cell 15, 568-577. 10.1016/j.devcel.2008.08.003 [DOI] [PubMed] [Google Scholar]
- Lehtinen, M. K., Zappaterra, M. W., Chen, X., Yang, Y. J., Hill, A. D., Lun, M., Maynard, T., Gonzalez, D., Kim, S., Ye, P.et al. (2011). The cerebrospinal fluid provides a proliferative niche for neural progenitor cells. Neuron 69, 893-905. 10.1016/j.neuron.2011.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leroith, D., Holly, J. M. P. and Forbes, B. E. (2021). Insulin-like growth factors: ligands, binding proteins, and receptors. Mol. Metab. 52, 101245. 10.1016/j.molmet.2021.101245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, X., Monks, B., Ge, Q. and Birnbaum, M. J. (2007). Akt/PKB regulates hepatic metabolism by directly inhibiting PGC-1alpha transcription coactivator. Nature 447, 1012-1016. 10.1038/nature05861 [DOI] [PubMed] [Google Scholar]
- Li, S., Liu, C., Goldstein, A., Xin, Y., Ke, C. and Duan, C. (2021). Calcium state-dependent regulation of epithelial cell quiescence by stanniocalcin 1a. Front. Cell Dev. Biol. 9, 662915. 10.3389/fcell.2021.662915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, J., Park, J., Mayer, J. P., Webb, K. J., Uchikawa, E., Wu, J., Liu, S., Zhang, X., Stowell, M. H. B., Choi, E.et al. (2022). Synergistic activation of the insulin receptor via two distinct sites. Nat. Struct. Mol. Biol. 29, 357-368. 10.1038/s41594-022-00750-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao, S., Vickers, M. H., Stanley, J. L., Ponnampalam, A. P., Baker, P. N. and Perry, J. K. (2016). The placental variant of human growth hormone reduces maternal insulin sensitivity in a dose-dependent manner in C57BL/6J mice. Endocrinology 157, 1175-1186. 10.1210/en.2015-1718 [DOI] [PubMed] [Google Scholar]
- Liao, S., Vickers, M. H., Stanley, J. L., Baker, P. N. and Perry, J. K. (2018). Human placental growth hormone variant in pathological pregnancies. Endocrinology 159, 2186-2198. 10.1210/en.2018-00037 [DOI] [PubMed] [Google Scholar]
- Liao, J., Zeng, T.-B., Pierce, N., Tran, D. A., Singh, P., Mann, J. R. and Szabó, P. E. (2021). Prenatal correction of IGF2 to rescue the growth phenotypes in mouse models of Beckwith-Wiedemann and Silver-Russell syndromes. Cell Rep. 34, 108729. 10.1016/j.celrep.2021.108729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, J. P., Baker, J., Perkins, A. S., Robertson, E. J. and Efstratiadis, A. (1993). Mice carrying null mutations of the genes encoding insulin-like growth factor I (Igf-1) and type 1 IGF receptor (Igf1r). Cell 75, 59-72. [PubMed] [Google Scholar]
- Liu, P., Gan, W., Chin, Y. R., Ogura, K., Guo, J., Zhang, J., Wang, B., Blenis, J., Cantley, L. C., Toker, A.et al. (2015). PtdIns(3,4,5)P3-dependent activation of the mTORC2 kinase complex. Cancer Discov. 5, 1194-1209. 10.1158/2159-8290.CD-15-0460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, C., Li, S., Noer, P. R., Kjaer-Sorensen, K., Juhl, A. K., Goldstein, A., Ke, C., Oxvig, C. and Duan, C. (2020). The metalloproteinase Papp-aa controls epithelial cell quiescence-proliferation transition. eLife 9, e52322. 10.7554/eLife.52322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez, M. F., Zheng, L., Miao, J., Gali, R., Gorski, G. and Hirschhorn, J. N. (2018). Disruption of the Igf2 gene alters hepatic lipid homeostasis and gene expression in the newborn mouse. Am. J. Physiol. Endocrinol. Metab. 315, E735-E744. 10.1152/ajpendo.00048.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Tello, J., Yong, H. E. J., Sandovici, I., Dowsett, G. K. C., Christoforou, E. R., Salazar-Petres, E., Boyland, R., Napso, T., Yeo, G. S. H., Lam, B. Y. H.et al. (2023). Fetal manipulation of maternal metabolism is a critical function of the imprinted Igf2 gene. Cell Metab. 35, 1195-1208.e6. 10.1016/j.cmet.2023.06.007 [DOI] [PubMed] [Google Scholar]
- Louvi, A., Accili, D. and Efstratiadis, A. (1997). Growth-promoting interaction of IGF-II with the insulin receptor during mouse embryonic development. Dev. Biol. 189, 33-48. 10.1006/dbio.1997.8666 [DOI] [PubMed] [Google Scholar]
- Maehama, T. and Dixon, J. E. (1998). The tumor suppressor, PTEN/MMAC1, dephosphorylates the lipid second messenger, phosphatidylinositol 3,4,5-trisphosphate. J. Biol. Chem. 273, 13375-13378. 10.1074/jbc.273.22.13375 [DOI] [PubMed] [Google Scholar]
- Manière, G., Ziegler, A. B., Geillon, F., Featherstone, D. E. and Grosjean, Y. (2016). Direct sensing of nutrients via a LAT1-like transporter in Drosophila insulin-producing cells. Cell Rep. 17, 137-148. 10.1016/j.celrep.2016.08.093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning, B. D. and Toker, A. (2017). AKT/PKB signaling: navigating the network. Cell 169, 381-405. 10.1016/j.cell.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning, B. D., Tee, A. R., Logsdon, M. N., Blenis, J. and Cantley, L. C. (2002). Identification of the tuberous sclerosis complex-2 tumor suppressor gene product tuberin as a target of the phosphoinositide 3-kinase/akt pathway. Mol. Cell 10, 151-162. 10.1016/S1097-2765(02)00568-3 [DOI] [PubMed] [Google Scholar]
- Mirth, C., Truman, J. W. and Riddiford, L. M. (2005). The role of the prothoracic gland in determining critical weight for metamorphosis in Drosophila melanogaster. Curr. Biol. 15, 1796-1807. 10.1016/j.cub.2005.09.017 [DOI] [PubMed] [Google Scholar]
- Mori, H., Inoki, K., Opland, D., Münzberg, H., Villanueva, E. C., Faouzi, M., Ikenoue, T., Kwiatkowski, D. J., Macdougald, O. A., Myers, M. G.et al. (2009). Critical roles for the TSC-mTOR pathway in β-cell function. Am. J. Physiol. Endocrinol. Metab. 297, E1013-E1022. 10.1152/ajpendo.00262.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musarò, A., Mccullagh, K., Paul, A., Houghton, L., Dobrowolny, G., Molinaro, M., Barton, E. R., Sweeney, H. L. and Rosenthal, N. (2001). Localized Igf-1 transgene expression sustains hypertrophy and regeneration in senescent skeletal muscle. Nat. Genet. 27, 195-200. 10.1038/84839 [DOI] [PubMed] [Google Scholar]
- Myers, M. G., Wang, L. M., Sun, X. J., Zhang, Y., Yenush, L., Schlessinger, J., Pierce, J. H. and White, M. F. (1994). Role of IRS-1-GRB-2 complexes in insulin signaling. Mol. Cell. Biol. 14, 3577-3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napso, T., Yong, H. E. J., Lopez-Tello, J. and Sferruzzi-Perri, A. N. (2018). The role of placental hormones in mediating maternal adaptations to support pregnancy and lactation. Front. Physiol. 9, 1091. 10.3389/fphys.2018.01091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obenshain, S. S., Adam, P. A., King, K. C., Teramo, K., Raivio, K. O., Räihä, N. and Schwartz, R. (1970). Human fetal insulin response to sustained maternal hyperglycemia. N. Engl. J. Med. 283, 566-570. 10.1056/NEJM197009102831104 [DOI] [PubMed] [Google Scholar]
- Obernier, K. and Alvarez-Buylla, A. (2019). Neural stem cells: origin, heterogeneity and regulation in the adult mammalian brain. Development 146, dev156059. 10.1242/dev.156059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oherle, K., Acker, E., Bonfield, M., Wang, T., Gray, J., Lang, I., Bridges, J., Lewkowich, I., Xu, Y., Ahlfeld, S.et al. (2020). Insulin-like growth factor 1 supports a pulmonary niche that promotes type 3 innate lymphoid cell development in newborn lungs. Immunity 52, 275-294.e9. 10.1016/j.immuni.2020.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto, N., Yamanaka, N., Yagi, Y., Nishida, Y., Kataoka, H., O'connor, M. B. and Mizoguchi, A. (2009). A fat body-derived IGF-like peptide regulates postfeeding growth in Drosophila. Dev. Cell 17, 885-891. 10.1016/j.devcel.2009.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto, N., Nakamori, R., Murai, T., Yamauchi, Y., Masuda, A. and Nishimura, T. (2013). A secreted decoy of InR antagonizes insulin/IGF signaling to restrict body growth in Drosophila. Genes Dev. 27, 87-97. 10.1101/gad.204479.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okano, T., Xuan, S. and Kelley, M. W. (2011). Insulin-like growth factor signaling regulates the timing of sensory cell differentiation in the mouse cochlea. J. Neurosci. 31, 18104-18118. 10.1523/JNEUROSCI.3619-11.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palanker, L., Tennessen, J. M., Lam, G. and Thummel, C. S. (2009). Drosophila HNF4 regulates lipid mobilization and beta-oxidation. Cell Metab. 9, 228-239. 10.1016/j.cmet.2009.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papasani, M. R., Robison, B. D., Hardy, R. W. and Hill, R. A. (2006). Early developmental expression of two insulins in zebrafish (Danio rerio). Physiol. Genomics 27, 79-85. 10.1152/physiolgenomics.00012.2006 [DOI] [PubMed] [Google Scholar]
- Papper, Z., Jameson, N. M., Romero, R., Weckle, A. L., Mittal, P., Benirschke, K., Santolaya-Forgas, J., Uddin, M., Haig, D., Goodman, M.et al. (2009). Ancient origin of placental expression in the growth hormone genes of anthropoid primates. Proc. Natl. Acad. Sci. USA 106, 17083-17088. 10.1073/pnas.0908377106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, S., Alfa, R. W., Topper, S. M., Kim, G. E. S., Kockel, L. and Kim, S. K. (2014). A genetic strategy to measure circulating Drosophila insulin reveals genes regulating insulin production and secretion. PLoS Genet. 10, e1004555. 10.1371/journal.pgen.1004555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce, S. B., Costa, M., Wisotzkey, R., Devadhar, S., Homburger, S. A., Buchman, A. R., Ferguson, K. C., Heller, J., Platt, D. M., Pasquinelli, A. A.et al. (2001). Regulation of DAF-2 receptor signaling by human insulin and ins-1, a member of the unusually large and diverse C. elegans insulin gene family. Genes Dev. 15, 672-686. 10.1101/gad.867301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plassais, J., vonholdt, B. M., Parker, H. G., Carmagnini, A., Dubos, N., Papa, I., Bevant, K., Derrien, T., Hennelly, L. M., Whitaker, D. T.et al. (2022). Natural and human-driven selection of a single non-coding body size variant in ancient and modern canids. Curr. Biol. 32, 889-897.e9. 10.1016/j.cub.2021.12.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter, C. J., Pedraza, L. G. and Xu, T. (2002). Akt regulates growth by directly phosphorylating Tsc2. Nat. Cell Biol. 4, 658-665. 10.1038/ncb840 [DOI] [PubMed] [Google Scholar]
- Powell-Braxton, L., Hollingshead, P., Warburton, C., Dowd, M., Pitts-Meek, S., Dalton, D., Gillett, N. and Stewart, T. A. (1993). IGF-I is required for normal embryonic growth in mice. Genes Dev. 7, 2609-2617. 10.1101/gad.7.12b.2609 [DOI] [PubMed] [Google Scholar]
- Pozios, K. C., Ding, J., Degger, B., Upton, Z. and Duan, C. (2001). IGFs stimulate zebrafish cell proliferation by activating MAP kinase and PI3-kinase-signaling pathways. Am. J. Physiol. Regul. Integr. Comp. Physiol. 280, R1230-R1239. 10.1152/ajpregu.2001.280.4.R1230 [DOI] [PubMed] [Google Scholar]
- Rena, G., Guo, S., Cichy, S. C., Unterman, T. G. and Cohen, P. (1999). Phosphorylation of the transcription factor forkhead family member FKHR by protein kinase B. J. Biol. Chem. 274, 17179-17183. 10.1074/jbc.274.24.17179 [DOI] [PubMed] [Google Scholar]
- Rockstroh, D., Pfäffle, H., Le Duc, D., Rößler, F., Schlensog-Schuster, F., Heiker, J. T., Kratzsch, J., Kiess, W., Lemke, J. R., Abou Jamra, R.et al. (2019). A new p.(Ile66Serfs*93) IGF2 variant is associated with pre- and postnatal growth retardation. Eur. J. Endocrinol. 180, K1-K13. 10.1530/EJE-18-0601 [DOI] [PubMed] [Google Scholar]
- Rodrigues, M. A., Martins, N. E., Balancé, L. F., Broom, L. N., Dias, A. J. S., Fernandes, A. S. D., Rodrigues, F., Sucena, É. and Mirth, C. K. (2015). Drosophila melanogaster larvae make nutritional choices that minimize developmental time. J. Insect Physiol. 81, 69-80. 10.1016/j.jinsphys.2015.07.002 [DOI] [PubMed] [Google Scholar]
- Rubin, C. S., Hirsch, A., Fung, C. and Rosen, O. M. (1978). Development of hormone receptors and hormonal responsiveness in vitro. Insulin receptors and insulin sensitivity in the preadipocyte and adipocyte forms of 3T3-L1 cells. J. Biol. Chem. 253, 7570-7578. 10.1016/S0021-9258(17)34541-6 [DOI] [PubMed] [Google Scholar]
- Ryan, E. A., O'sullivan, M. J. and Skyler, J. S. (1985). Insulin action during pregnancy. Studies with the euglycemic clamp technique. Diabetes 34, 380-389. 10.2337/diab.34.4.380 [DOI] [PubMed] [Google Scholar]
- Sales, V. M., Ferguson-Smith, A. C. and Patti, M.-E. (2017). Epigenetic mechanisms of transmission of metabolic disease across generations. Cell Metab. 25, 559-571. 10.1016/j.cmet.2017.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saltiel, A. R. (2021). Insulin signaling in health and disease. J. Clin. Invest. 131, e142241. 10.1172/JCI142241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandovici, I., Georgopoulou, A., Pérez-García, V., Hufnagel, A., López-Tello, J., Lam, B. Y. H., Schiefer, S. N., Gaudreau, C., Santos, F., Hoelle, K.et al. (2022). The imprinted Igf2-Igf2r axis is critical for matching placental microvasculature expansion to fetal growth. Dev. Cell 57, 63-79.e8. 10.1016/j.devcel.2021.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarbassov, D. D., Guertin, D. A., Ali, S. M. and Sabatini, D. M. (2005). Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science 307, 1098-1101. 10.1126/science.1106148 [DOI] [PubMed] [Google Scholar]
- Sasaoka, T., Ishiki, M., Sawa, T., Ishihara, H., Takata, Y., Imamura, T., Usui, I., Olefsky, J. M. and Kobayashi, M. (1996). Comparison of the insulin and insulin-like growth factor 1 mitogenic intracellular signaling pathways. Endocrinology 137, 4427-4434. 10.1210/endo.137.10.8828504 [DOI] [PubMed] [Google Scholar]
- Scapin, G., Dandey, V. P., Zhang, Z., Prosise, W., Hruza, A., Kelly, T., Mayhood, T., Strickland, C., Potter, C. S. and Carragher, B. (2018). Structure of the insulin receptor-insulin complex by single-particle cryo-EM analysis. Nature 556, 122-125. 10.1038/nature26153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlueter, P. J., Peng, G., Westerfield, M. and Duan, C. (2007). Insulin-like growth factor signaling regulates zebrafish embryonic growth and development by promoting cell survival and cell cycle progression. Cell Death Differ. 14, 1095-1105. 10.1038/sj.cdd.4402109 [DOI] [PubMed] [Google Scholar]
- Schmelzle, K., Kane, S., Gridley, S., Lienhard, G. E. and White, F. M. (2006). Temporal dynamics of tyrosine phosphorylation in insulin signaling. Diabetes 55, 2171-2179. 10.2337/db06-0148 [DOI] [PubMed] [Google Scholar]
- Sciacca, L., Cassarino, M. F., Genua, M., Pandini, G., Le Moli, R., Squatrito, S. and Vigneri, R. (2010). Insulin analogues differently activate insulin receptor isoforms and post-receptor signalling. Diabetologia 53, 1743-1753. 10.1007/s00125-010-1760-6 [DOI] [PubMed] [Google Scholar]
- Sferruzzi-Perri, A. N., Sandovici, I., Constancia, M. and Fowden, A. L. (2017). Placental phenotype and the insulin-like growth factors: resource allocation to fetal growth. J. Physiol. 595, 5057-5093. 10.1113/JP273330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim, J., Gururaja-Rao, S. and Banerjee, U. (2013). Nutritional regulation of stem and progenitor cells in Drosophila. Development 140, 4647-4656. 10.1242/dev.079087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shingleton, A. W., Masandika, J. R., Thorsen, L. S., Zhu, Y. and Mirth, C. K. (2017). The sex-specific effects of diet quality versus quantity on morphology in Drosophila melanogaster. R. Soc. Open Sci. 4, 170375. 10.1098/rsos.170375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley, C. P., Coan, P. M., Ferguson-Smith, A. C., Dean, W., Hughes, J., Smith, P., Reik, W., Burton, G. J., Fowden, A. L. and Constância, M. (2004). Placental-specific insulin-like growth factor 2 (Igf2) regulates the diffusional exchange characteristics of the mouse placenta. Proc. Natl. Acad. Sci. USA 101, 8204-8208. 10.1073/pnas.0402508101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva, F. A., Souza, É. MS., Ramos, E., Freitas, L. and Nery, M. F. (2023). The molecular evolution of genes previously associated with large sizes reveals possible pathways to cetacean gigantism. Sci. Rep. 13, 67. 10.1038/s41598-022-24529-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeen, J. E., Bhaskar, P. T., Chen, C.-C., Chen, W. S., Peng, X., Nogueira, V., Hahn-Windgassen, A., Kiyokawa, H. and Hay, N. (2006). Akt deficiency impairs normal cell proliferation and suppresses oncogenesis in a p53-independent and mTORC1-dependent manner. Cancer Cell 10, 269-280. 10.1016/j.ccr.2006.08.022 [DOI] [PubMed] [Google Scholar]
- Skolnik, E. Y., Batzer, A., Li, N., Lee, C. H., Lowenstein, E., Mohammadi, M., Margolis, B. and Schlessinger, J. (1993). The function of GRB2 in linking the insulin receptor to Ras signaling pathways. Science 260, 1953-1955. 10.1126/science.8316835 [DOI] [PubMed] [Google Scholar]
- Slaidina, M., Delanoue, R., Gronke, S., Partridge, L. and Léopold, P. (2009). A Drosophila insulin-like peptide promotes growth during nonfeeding states. Dev. Cell 17, 874-884. 10.1016/j.devcel.2009.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, P. J., Wise, L. S., Berkowitz, R., Wan, C. and Rubin, C. S. (1988). Insulin-like growth factor-I is an essential regulator of the differentiation of 3T3-L1 adipocytes. J. Biol. Chem. 263, 9402-9408. 10.1016/S0021-9258(19)76555-7 [DOI] [PubMed] [Google Scholar]
- So, S., Miyahara, K. and Ohshima, Y. (2011). Control of body size in C. elegans dependent on food and insulin/IGF-1 signal. Genes Cells 16, 639-651. 10.1111/j.1365-2443.2011.01514.x [DOI] [PubMed] [Google Scholar]
- Sousa-Nunes, R., Yee, L. L. and Gould, A. P. (2011). Fat cells reactivate quiescent neuroblasts via TOR and glial insulin relays in Drosophila. Nature 471, 508-512. 10.1038/nature09867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spéder, P. and Brand, A. H. (2018). Systemic and local cues drive neural stem cell niche remodelling during neurogenesis in Drosophila. eLife 7, e30413. 10.7554/eLife.30413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolovich-Rain, M., Enk, J., Vikesa, J., Nielsen, F. C., Saada, A., Glaser, B. and Dor, Y. (2015). Weaning triggers a maturation step of pancreatic β cells. Dev. Cell 32, 535-545. 10.1016/j.devcel.2015.01.002 [DOI] [PubMed] [Google Scholar]
- Stratikopoulos, E., Szabolcs, M., Dragatsis, I., Klinakis, A. and Efstratiadis, A. (2008). The hormonal action of IGF1 in postnatal mouse growth. Proc. Natl. Acad. Sci. USA 105, 19378-19383. 10.1073/pnas.0809223105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutter, N. B., Bustamante, C. D., Chase, K., Gray, M. M., Zhao, K., Zhu, L., Padhukasahasram, B., Karlins, E., Davis, S., Jones, P. G.et al. (2007). A single IGF1 allele is a major determinant of small size in dogs. Science 316, 112-115. 10.1126/science.1137045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzawa, M., Muhammad, N. M., Joseph, B. S. and Bland, M. L. (2019). The toll signaling pathway targets the insulin-like peptide Dilp6 to inhibit growth in Drosophila. Cell Rep. 28, 1439-1446.e5. 10.1016/j.celrep.2019.07.015 [DOI] [PubMed] [Google Scholar]
- Tennessen, J. M. and Thummel, C. S. (2011). Coordinating growth and maturation - insights from Drosophila. Curr. Biol. 21, R750-R757. 10.1016/j.cub.2011.06.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdu, J., Buratovich, M. A., Wilder, E. L. and Birnbaum, M. J. (1999). Cell-autonomous regulation of cell and organ growth in Drosophila by Akt/PKB. Nat. Cell Biol. 1, 500-506. 10.1038/70293 [DOI] [PubMed] [Google Scholar]
- Wada, T., Sasaoka, T., Funaki, M., Hori, H., Murakami, S., Ishiki, M., Haruta, T., Asano, T., Ogawa, W., Ishihara, H.et al. (2001). Overexpression of SH2-containing inositol phosphatase 2 results in negative regulation of insulin-induced metabolic actions in 3T3-L1 adipocytes via its 5’-phosphatase catalytic activity. Mol. Cell. Biol. 21, 1633-1646. 10.1128/MCB.21.5.1633-1646.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Z. Q., Fung, M. R., Barlow, D. P. and Wagner, E. F. (1994). Regulation of embryonic growth and lysosomal targeting by the imprinted Igf2/Mpr gene. Nature 372, 464-467. 10.1038/372464a0 [DOI] [PubMed] [Google Scholar]
- Wang, H., Li, N., Chivese, T., Werfalli, M., Sun, H., Yuen, L., Hoegfeldt, C. A., Elise Powe, C., Immanuel, J., Karuranga, S.et al. (2022). IDF diabetes atlas: estimation of global and regional gestational diabetes mellitus prevalence for 2021 by international association of diabetes in pregnancy study group's criteria. Diabetes Res. Clin. Pract. 183, 109050. 10.1016/j.diabres.2021.109050 [DOI] [PubMed] [Google Scholar]
- White, M. F. (2002). IRS proteins and the common path to diabetes. Am. J. Physiol. Endocrinol. Metab. 283, E413-E422. 10.1152/ajpendo.00514.2001 [DOI] [PubMed] [Google Scholar]
- Woods, K. A., Camacho-Hübner, C., Savage, M. O. and Clark, A. J. (1996). Intrauterine growth retardation and postnatal growth failure associated with deletion of the insulin-like growth factor I gene. N. Engl. J. Med. 335, 1363-1367. 10.1056/NEJM199610313351805 [DOI] [PubMed] [Google Scholar]
- Wu, M., Carballo-Jane, E., Zhou, H., Zafian, P., Dai, G., Liu, M., Lao, J., Kelly, T., Shao, D., Gorski, J.et al. (2022). Functionally selective signaling and broad metabolic benefits by novel insulin receptor partial agonists. Nat. Commun. 13, 942. 10.1038/s41467-022-28561-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin, Y., Malick, A., Hu, M., Liu, C., Batah, H., Xu, H. and Duan, C. (2019). Cell-autonomous regulation of epithelial cell quiescence by calcium channel Trpv6. eLife 8, e48003. 10.7554/eLife.48003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin, Y., Guan, J., Li, Y. and Duan, C. (2021). Regulation of cell quiescence-proliferation balance by Ca2+-CaMKK-Akt signaling. J. Cell Sci. 134, jcs253807. 10.1242/jcs.253807 [DOI] [PubMed] [Google Scholar]
- Yan, J.-J. and Hwang, P.-P. (2019). Novel discoveries in acid-base regulation and osmoregulation: a review of selected hormonal actions in zebrafish and medaka. Gen. Comp. Endocrinol. 277, 20-29. 10.1016/j.ygcen.2019.03.007 [DOI] [PubMed] [Google Scholar]
- You, Y., Kim, J., Raizen, D. M. and Avery, L. (2008). Insulin, cGMP, and TGF-beta signals regulate food intake and quiescence in C. elegans: a model for satiety. Cell Metab. 7, 249-257. 10.1016/j.cmet.2008.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan, X., Sipe, C. W., Suzawa, M., Bland, M. L. and Siegrist, S. E. (2020). Dilp-2-mediated PI3-kinase activation coordinates reactivation of quiescent neuroblasts with growth of their glial stem cell niche. PLoS Biol. 18, e3000721. 10.1371/journal.pbio.3000721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, H., Liu, J., Li, C. R., Momen, B., Kohanski, R. A. and Pick, L. (2009). Deletion of Drosophila insulin-like peptides causes growth defects and metabolic abnormalities. Proc. Natl. Acad. Sci. USA 106, 19617-19622. 10.1073/pnas.0905083106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng, S., Chiu, H., Boudreau, J., Papanicolaou, T., Bendena, W. and Chin-Sang, I. (2018). A functional study of all 40 Caenorhabditis elegans insulin-like peptides. J. Biol. Chem. 293, 16912-16922. 10.1074/jbc.RA118.004542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegler, A. N., Schneider, J. S., Qin, M., Tyler, W. A., Pintar, J. E., Fraidenraich, D., Wood, T. L. and Levison, S. W. (2012). IGF-II promotes stemness of neural restricted precursors. Stem Cells 30, 1265-1276. 10.1002/stem.1095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou, S., Kamei, H., Modi, Z. and Duan, C. (2009). Zebrafish IGF genes: gene duplication, conservation and divergence, and novel roles in midline and notochord development. PLoS One 4, e7026. 10.1371/journal.pone.0007026 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.