Abstract
Introduction and importance:
This case report presents an intriguing instance of a 35-year-old nonsmoker female who exhibited a convergence of acute necrotizing pneumonia (ANP) and squamous cell carcinoma (SCC), two distinct pulmonary conditions. ANP involves severe lung infection and tissue necrosis, while SCC is a non-small cell lung carcinoma originating from the bronchial epithelium. Such a unique combination in a nonsmoker female patient emphasizes the intricate interplay of diverse pulmonary pathologies and the importance of comprehensive diagnostic evaluation and effective patient management strategies.
Case presentation:
The patient’s symptoms include fever, pain, cough, and sporadic hemoptysis. Initial imaging suggested ANP due to a multilobulated necrotic lung mass. Despite empirical antibiotic therapy, no improvement occurred, prompting further investigation. Positron emission tomography and computed tomography revealed intense fluorodeoxyglucose avidity in the lesion. A computer tomography-guided Tru-cut biopsy confirmed non-small cell carcinoma with squamous differentiation in the necrotic mass.
Clinical discussion:
ANP is a severe manifestation of pneumonia, predominantly affecting young, healthy individuals, while SCC, commonly linked to smoking, presents as non-small cell lung carcinoma. Overlapping symptoms and radiological findings complicate diagnosis. Early diagnosis and appropriate management are crucial for both conditions to prevent progression and complications.
Conclusion:
This case highlights the significance of precise diagnosis and adaptable treatment approaches. The coexistence of ANP and SCC in a nonsmoker female patient underscores the necessity of meticulous diagnostic evaluation and personalized treatment strategies. The scarcity of such presentations emphasizes the need for further research to comprehend the mechanisms underlying these occurrences.
Keywords: acute necrotizing pneumonia, non-small cell carcinoma, squamous cell carcinoma, surgical resection, Tru-cut biopsy
Introduction
Highlights
This case report unveils a remarkable convergence of acute necrotizing pneumonia (ANP) and squamous cell carcinoma (SCC) within a single clinical scenario, shedding light on the intricate interplay of diverse pulmonary pathologies.
Nonsmoker female affected: The rarity of this case lies in the fact that the patient is a 35-year-old nonsmoker female, challenging conventional expectations regarding SCC diagnosis.
Diagnostic challenges: Initial imaging suggested ANP, but empirical antibiotics proved ineffective, highlighting the complexities in differentiating these conditions with overlapping symptoms.
PET-CT (positron emission tomography and computed tomography) revelation: Fluorodeoxyglucose (FDG) PET-CT played a pivotal role, revealing intense FDG avidity in the necrotic lung mass akin to primary malignant lesions.
Surgical and cisplatin-based therapy: Successful surgical resection followed by cisplatin-based therapy demonstrated the effectiveness of this tailored treatment approach in achieving remission.
Acute necrotizing pneumonia (ANP) and squamous cell carcinoma (SCC) are distinct medical entities, each representing a different aspect of pulmonary pathology. While ANP is a severe form of lung infection characterized by rapid tissue necrosis1, SCC is a type of non-small cell lung carcinoma originating from the bronchial epithelium2. The convergence of these two conditions in a single clinical scenario is indeed a rare finding, particularly when considering the demographics of a nonsmoker female patient. This case report presents a unique and intriguing instance in which a 35-year-old nonsmoker female presented with clinical and radiological features suggestive of ANP; however, further investigations led to the unexpected diagnosis of SCC within a necrotic lung mass. The rarity of such a presentation underscores the complex interplay between diverse pulmonary pathologies and emphasizes the need for meticulous diagnostic workup, tailored treatment approaches, and comprehensive patient management.
Methods
We report this case in line with the updated consensus-based Surgical CAse REport (SCARE) 2020 criteria3.
The complete Case Timeline (Fig. 1).
Figure 1.
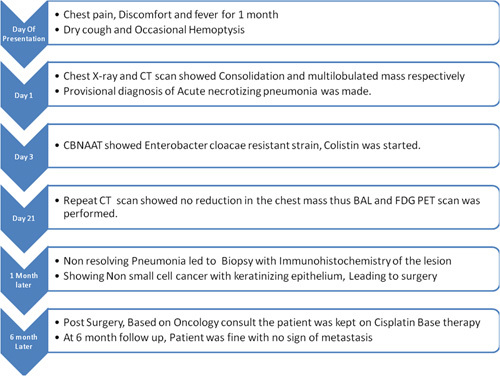
Complete patient timeline from admission to follow-up.
Case presentation
A 35-year-old female patient presented to the clinic with a history of fever, chills, lower back and right-sided pain, dry cough, palpitations, and occasional hemoptysis. Chest radiography revealed consolidation in the right lower lobe and inhomogeneous opacities with central lucency. The patient was then sent for a computed tomography (CT) scan, which showed a sizeable multilobulated mass with central necrosis and air-filled spaces with multiple internal septa of 9×6.2×9.1 cm (Fig. 2). The lesion was adherent to the costal pleura, without rib erosion (Fig. 3). There was no evidence of interstitial thickening or honeycombing. Based on these findings, the patient was diagnosed with ANP.
Figure 2.
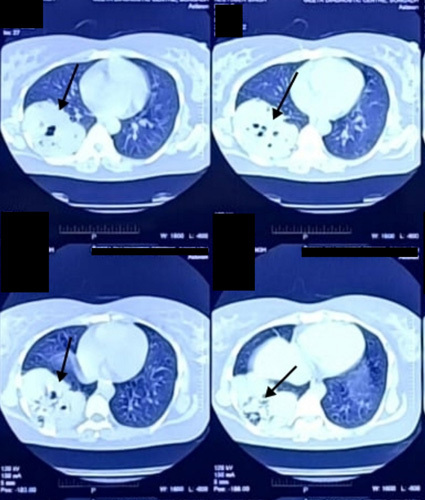
Computed tomography scan at the level of lungs showing large multilobulated and smooth marginated soft tissue lesion and internal non-enhancing necrotic areas with air bronchograms (black arrow).
Figure 3.
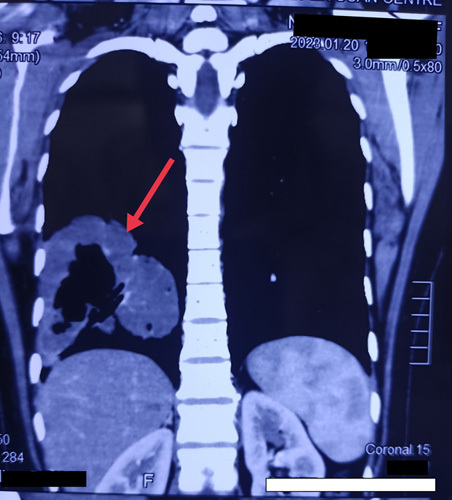
Computed tomography scan showing right lower lobe mass with central leucencies (red arrow).
The patient started empirical therapy consisting of intravenous antibiotics, including macrolides and fluoroquinolones, while awaiting laboratory results regarding the causative agent. However, no improvement was observed on subsequent CT scans, and bronchoscopy with bronchoalveolar lavage (BAL) was performed. The BAL samples were sent for Cartridge-based amplification technique (CBNAT) testing, which revealed the presence of Enterobacter cloacae, which were found to be resistant to ceftazidime, imipenem, amikacin, and gentamicin. This bacterial resistance presented a challenge as the patient’s condition deteriorated further, and the symptoms worsened with frequent hemoptysis. The patient was admitted to the intensive care unit (ICU), and treatment was switched to colistin to prevent aspiration and dehydration. After 15 days, a repeat CT revealed no reduction in the mass. Fluorodeoxyglucose (FDG) positron emission tomography and computed tomography (PET-CT) showed intense FDG avidity in the multilobulated, non-enhancing, centrally necrotic mass in the right lower pulmonary lobe (9.5×7.4×9.7 cm) (Fig. 4).
Figure 4.
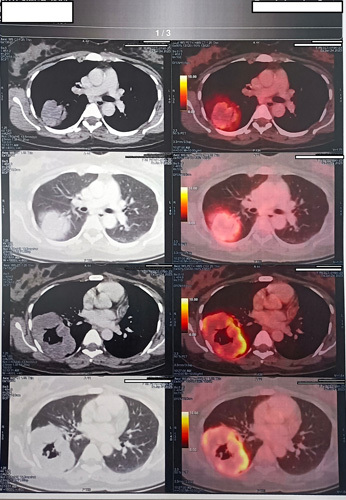
Intense hypermetabolism, like in the case of a primary malignant lesion in the right lower lobe of the lung as seen in FDG (fluorodeoxyglucose) PET-CT (positron emission tomography and computed tomography).
A CT-guided Tru-cut biopsy was obtained from the lesion, with polygonal cells and extensively necrotic non-small cell carcinoma that showed keratinizing squamous differentiation at low power (Fig. 5) and high power (Fig. 6). Based on the oncology consult, the tumor was surgically resected with posterolateral thoracotomy and was continued with cisplatin-based therapy for 3 weeks. Follow-up after 6 months showed no mass or lymph node involvement.
Figure 5.
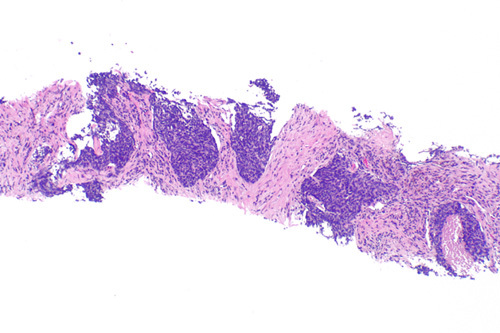
Low magnification image of the biopsy showing necrotic cells.
Figure 6.
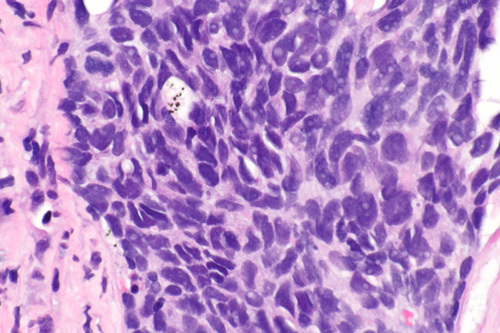
High magnification image of the biopsy consistent with non-small cell carcinoma.
Discussion
ANP is an uncommon yet severe manifestation of community-acquired pneumonia (CAP), characterized by rapid and extensive necrosis of lung tissue1. The condition primarily affects young, immunocompetent individuals and typically presents with fever, cough, pleuritic chest pain, and sometimes hemoptysis4. Radiological findings, such as multilobulated necrotic lung masses with air-filled spaces, can mimic other lung pathologies, making accurate diagnosis challenging. The etiology of ANP is often related to aggressive bacterial infections, with Streptococcus pneumoniae and Staphylococcus aureus being the common causative agents5. However, other microorganisms, including E. cloacae, have rarely been observed, as in the present case, and can also contribute to its development6,7. Prompt diagnosis and aggressive management, including antibiotic therapy and surgical intervention, are crucial to prevent disease progression and associated complications.
SCC is a prevalent type of non-small cell lung carcinoma primarily linked to cigarette smoking and carcinogenic exposure. SCC typically arises from the bronchial epithelium and manifests in older individuals with a smoking history2. SCC is characterized by the abnormal proliferation of squamous cells, leading to the formation of a malignant tumor that can invade surrounding tissues and metastasize to distant sites8. Patients with SCC often present with symptoms such as persistent cough, hemoptysis, chest pain, and weight loss. Imaging studies, including CT and PET-CT, play a crucial role in identifying the extent of the tumor and guiding treatment decisions.
The clinical presentation of fever, chills, pain, and respiratory symptoms in the context of lung pathology prompted comprehensive diagnostic evaluation. Initial chest X-ray imaging and subsequent CT revealed a distinctive multilobulated mass with central necrosis and air-filled spaces located in the right lower lung lobe. While the clinical presentation and radiological findings initially raised suspicion of infectious etiologies such as ANP, the subsequent course of events revealed a more intricate underlying condition. Despite empirical therapy with intravenous antibiotics, including macrolides and fluoroquinolones, the patient failed to show improvement. This lack of a response prompted further investigation. Thus, the utilization of FDG PET-CT scanning revealed intense FDG avidity in the necrotic mass, resembling patterns seen in primary malignant lesions.
To definitively ascertain the nature of the lesion, a CT-guided Tru-cut biopsy was performed. The biopsy revealed a non-small cell carcinoma with keratinizing squamous differentiation9, a finding that redefined the diagnosis and prompted oncology consultation. Surgical resection of the tumor through posterolateral thoracotomy was followed by cisplatin-based therapy10. The subsequent 6-month follow-up, characterized by the absence of mass or lymph node involvement, underscored the success of the treatment regimen in achieving remission.
Conclusion
This case report highlights the intricate diagnostic journey and management challenges encountered in patients with initially ambiguous symptoms and imaging findings. This experience underscores the value of clinical vigilance, prompt adaptation of treatment strategies, and the integration of advanced diagnostic modalities to achieve accurate diagnoses and favorable clinical outcomes. The mechanisms underlying SCC development in nonsmokers, particularly within the context of ANP, remain poorly understood and warrant further investigation.
Ethical approval
It is not required at our institution, as this is a case report.
Consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
None.
Author contribution
K.M., D.M., and S.M.: topic conception, data gathering and analysis, manuscript preparation, review, revisions, and editing; K.M. and D.M.: manuscript preparation, review, revisions, and editing; S.M. and P.O.T.: data gathering and analysis, manuscript preparation, revisions, and editing.
Conflicts of interest disclosure
The authors declare no conflicts of interest.
Research registration unique identifying number (UIN)
Name of the registry: not applicable.
Unique identifying number or registration ID: not applicable.
Hyperlink to your specific registration (must be publicly accessible and will be checked): not applicable.
Guarantor
Kahan Mehta, research.kahan@gmail.com.
Data availability statement
The data generated are in the article above.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
Assistance with the study: None taken.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 2 October 2023
Contributor Information
Kahan Mehta, Email: research.kahan@gmail.com.
Deep Modh, Email: akshatwala5109@gmail.com.
Samir Mehta, Email: drsamirnmaheta@gmail.com.
Pearl O. Tenkorang, Email: pearltenkorang3@gmail.com.
References
- 1.Chatha N, Fortin D, Bosma KJ. Management of necrotizing pneumonia and pulmonary gangrene: a case series and review of the literature. Can Respir J 2014;21:239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sabbula BR, Gasalberti DP, Anjum F. Squamous Cell Lung Cancer Accessed 2023 May 6 StatPearls. StatPearls Publishing; 2023.https://www.ncbi.nlm.nih.gov/books/NBK564510/ [PubMed]
- 3.Agha RA, Franchi T, Sohrabi C, et al. for the SCARE Group . The SCARE 2020 Guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 2020;84:226–230. [DOI] [PubMed] [Google Scholar]
- 4.Tsai Y-F, Ku Y-H. Necrotizing pneumonia: a rare complication of pneumonia requiring special consideration. Curr Opin Pulm Med 2012;18:246–252. [DOI] [PubMed] [Google Scholar]
- 5.Hodina M, Hanquinet S, Cotting J, et al. Imaging of cavitary necrosis in complicated childhood pneumonia. Eur Radiol 2002;12:391–396. [DOI] [PubMed] [Google Scholar]
- 6.Chou DW, Wu SL, Lee CT. Intensive care unit-acquired complicated necrotizing pneumonia caused by Enterobacter cloacae: a case report. Intractable Rare Dis Res 2018;7:283–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al Tassan RS, Al Alola S, Al Shaalan H, et al. Necrotizing pneumonia following cardiac surgery in a neonate. J Infect Public Health 2013;6:154–157. [DOI] [PubMed] [Google Scholar]
- 8.Yan W, Wistuba II, Emmert-Buck MR, et al. Squamous cell carcinoma – similarities and differences among anatomical sites. Am J Cancer Res 2011;1:275–300. [PMC free article] [PubMed] [Google Scholar]
- 9.Travis WD, Brambilla E, Noguchi M, et al. Diagnosis of lung cancer in small biopsies and cytology: implications of the 2011 International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification. Arch Pathol Lab Med 2013;137:668–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paoletti L, Pastis NJ, Denlinger CE, et al. A decade of advances in treatment of early-stage lung cancer. Clin Chest Med 2011;32:827–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated are in the article above.


