Abstract
Introduction
Mental disorders are the leading cause of disability and the second leading cause of death worldwide, which leads to the death of more than 9 million people annually. The global impact of the Coronavirus epidemic on mental health includes insomnia, anxiety, and depression. Therefore, given the current situation, innovations such as telemedicine to provide prevention and treatment services for people with mental disorders seem necessary.
Methods
A literature review was performed according to the preferred items to report in systematic reviews and meta‐analyses (PRISMA). Covering a period from January 2020 to July 2023, we conducted a systematic literature search on five electronic databases (PubMed‐Mesh, Scopus, Web of Science, Science direct, and PsycInfo). The search strategy included three categories of keywords: Mental health, Tele, COVID‐19.
Results
A total of 112 articles were identified by searching the databases of published articles, 13 articles met our inclusion criteria. A total of 76.2% of them were related to patients with stress, anxiety, and depression issues. We found that the real‐time method has been the most common method used to communicate between the physician and the patient (92.3%). The communication technologies used also included telephone, video call, video conference, and E‐mail. During these communications, data was exchanged in text, voice, and video formats. In three studies (27%), interoperability with other systems was mentioned. In addition, 69.2% of the studies reported challenges, the most important of which were access to electronic and communication devices, network connection problems, audio and video problems, and privacy issues.
Conclusions
Considering the many advantages of telemedicine technology in the field of mental health, the need to use this technology in developing countries, including our country, is obvious. But the application of these technologies requires the investigation of technical aspects and challenges related to them as much as possible, which have been seen in few studies.
Keywords: challenges, COVID‐19, mental health, tele
1. INTRODUCTION
Mental disorders are the leading cause of disability and the second leading cause of death worldwide, which leads to the death of more than 9 million people annually. Despite the importance of these disorders, mental health services are scarce in many parts of the world, especially in low‐ and middle‐income countries. Even when the service is available, it does not meet the patient's needs. 1 While mental disorders are recognized as a global burden, the pandemic of coronavirus in 2019 and the implementation of measures such as social distancing, closure of schools and universities, telecommuting, and travel bans had potential effects on the mental health of individuals. 2 , 3 The global impact of the Coronavirus epidemic on mental health includes insomnia, anxiety, and depression among healthcare workers and other populations. 4 In the population, the prevalence of depression, anxiety, insomnia, and acute stress is 27.9%, 31.6, 29.2%, and 24.4%, respectively. Also, people with COVID‐19 have reported a high rate of posttraumatic stress disorder (PTSD) after recovery and hospital discharge. 2 An increase in the number of people affected by the coronavirus is likely to increase the rate of emotional trauma and mental disorders. 4 Therefore, given the current situation, innovations to provide prevention and treatment services for people with mental disorders seem necessary. One of these innovations is telemedicine. The use of information technologies such as telemedicine in mental health provides people with easy access to efficient and effective, yet cost‐effective health services. Telemedicine is an information and communication system for providing and supporting telemedicine services, of which mental health care is a major area. 5 The corona crisis has also increased attention to tele‐mental health. The term tele‐mental health refers to the provision of tele‐mental healthcare using telecommunications, such as telephone, email, video conferencing, digital imaging, and healthcare monitoring devices. 6 Evidence shows that using remote health care for psychotherapy and other psychological services improves patient satisfaction and reduces care costs. 5
Previous systematic studies have focused on various topics in the field of mental health during the COVID‐19 pandemic. Naureen et al. examined the role of tele‐mental health services during the COVID‐19 epidemic. They said that using this innovative method prevents the transmission of infection and provides timely treatment for people. 7 Jing et al., also reviewed data available on the benefits of interventions to reduce the adverse health outcomes of infectious diseases and provide guidance on mental health services' responses to an infectious disease epidemic. They found that telemedicine services are key components of care to manage infectious disease outbreaks and routine support. 2 Appleton et al. investigated the effects of tele‐mental health approaches during COVID‐19 epidemics, facilitators, and barriers to optimal implementation. Their study found that implementing tele‐mental care helps most service users during the COVID‐19 epidemic and is valuable in emergencies. 8
The present study aimed to discuss the description and summary of tele‐mental health during the COVID‐19 epidemic from the published literature and to examine the technical aspects and challenges it is related and investigate the tele‐mental health infrastructure to help further research in this field.
2. METHOD
2.1. Search strategy
We adhered to the protocol to review articles, based on preferred items to report in systematic reviews and meta‐analyses (PRISMA). The PICO framework (population, intervention, comparator, and outcome) was used to structure the research question. The population includes people with mental disorders caused by COVID‐19. The intervention includes a variety of telemedicine methods (real‐time, store and forward) that provide remote services such as counseling, diagnosis, and treatment for this category of patients. The comparator is not considered in this study. The outcome includes the methods of technology evaluation, the type of remote communication, and the challenges in using the technology. Covering a period from January 2020 to July 2023, we conducted a systematic literature search on five electronic databases (PubMed‐Mesh, Scopus, Web of Science, Science direct, and PsycInfo). The search strategy included three categories of keywords: Mental health, Tele, and COVID‐19. These keywords should be appeared in conjunction in the title of the article. The keywords and search strategy are described in Table 1.
Table 1.
Keywords and search strategy.
| Tele | Mental health | Covid | |||||
|---|---|---|---|---|---|---|---|
| Tele* | AND | Mental health | AND | Covid19 | |||
| OR | Remote | OR | Psych* | OR | Covid‐19 |
2.2. Study selection
First, duplicate citations across databases were identified and excluded using EndNote X7.8 (Thomson Reuters) software and a manual revision was done for verification. If a study was reported in more than one publication and presented the same data, we only included the most recent publication. In the next step, the abstract and title of articles were studied according to the inclusion/exclusion criteria. Screening of titles and abstracts was conducted independently by two researchers. The disagreement between researchers was resolved by consensus. The full texts of articles, which seemed relevant to the objectives, were reviewed by the same two researchers. Any disagreement was resolved by consensus.
2.2.1. Inclusion criteria
We included articles in this review if they: (1) were full‐text journal articles (we excluded abstracts); (2) were published in English; (3) were published during the COVID‐19 pandemic (2020–July 2023); (4) reported tele‐mental health implementation.
2.2.2. Exclusion criteria
We excluded articles from this review if they: (1) were reviews or gray literature (e.g., conference papers); (2) not relevant with mental health domain; (3) reported tele‐mental health's adoption from patients' or providers' perspectives; (4) did not mention the implementation and use of tele‐mental health technology; (5) Specifically report guidelines, strategies and challenges for tele‐mental health.
2.3. Data extraction
To conduct a systematic and accurate extraction of data, we developed a data extraction form in Excel software. Similar to the study selection process, two reviewers (S. Z. and M. N.) independently conducted the process of data extraction. The third author (S. H. K.) then checked the accuracy of the extracted data. In case of any discrepancies, meetings were held to compare our findings and resolve disagreements by discussion.
2.4. Quality evaluation
Due to the variety of articles and existing methods, the mixed methods appraisal tool (MMAT) was used to evaluate studies. 9 MMAT is a valid tool for evaluating all study designs. Report the percentage of criteria for each study based on MMAT (e.g., 20% represents 1/5 criteria, while 80% represents 4/5 criteria). Studies if they have 20% or less, of poor quality, if they have 40%–60% criteria, medium quality, and if they have at least 80% of the criteria, high quality is considered. The quality of the studies was evaluated by S. K. and approved by S. Z. Disputes were resolved by discussion.
3. RESULTS
3.1. Search results
A total of 112 articles were identified by searching the databases of published articles. Of these, 53 duplicates were removed. Of the remaining 59 articles, 28 articles were deleted after reviewing the title and abstract, and 18 articles after reviewing the full text. Finally, 13 articles met our inclusion criteria. PRISMA flow diagram of the screening and selection process is presented in Figure 1.
Figure 1.
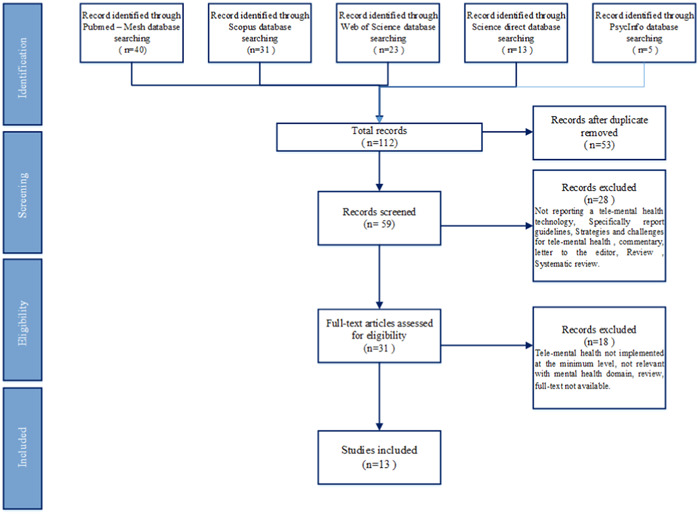
Literature search flow diagram.
The identified articles were implemented in eight countries. Among the articles that have identified a country, most of the articles are related to Italy (4, 30.7%), 10 , 11 , 12 , 13 followed by India, 14 , 15 with three articles. 14 , 15 , 16 Most articles focused on the high‐income countries of the World Bank (7, 53.8%) 10 , 11 , 12 , 17 , 18 , 19 and high‐middle income (2, 15.3%). 20 , 21 Four articles focused on low‐middle‐income countries 14 , 15 , 16 , 22 and one article focused on low‐income countries. 23
Four groups of participants involved in the use of tele‐mental health were identified in the articles, the most common participants being patients and caregivers (11, 84.6%). 10 , 11 , 12 , 13 , 14 , 15 , 17 , 19 , 20 , 21 , 23 Among these articles, five articles were for patients only 11 , 14 , 16 , 19 , 22 and two articles were for caregivers only. 4 , 10 In addition, two articles for patients and/or their relatives. 13 , 20
The method of communication in mental health remotely described in the articles includes two types real‐time and store and forward. The real‐time method has been the most used among these methods (12, 92.3%), 10 , 12 , 14 , 15 , 17 , 19 , 20 , 21 , 23 and one article has only used the store and forward method. 11 Four articles used both methods. 12 , 20 , 21 , 23 The communication technologies used also included telephone, video call, video conference, and E‐mail. Nine articles used telephone and video calls, 10 , 14 , 15 , 16 , 17 , 19 , 21 , 22 four articles from video conferences, 12 , 13 , 20 , 23 and one article from E‐mail to communicate. 11 During these communications, data was exchanged in text, voice, and video formats.
The articles identified in our review were written with the purpose of using tele‐mental health. According to the tree diagram in Figure 2, there were seven specific purposes among the articles, the most of which was the use of tele‐mental health in the field of psychological support and counseling (11, 84.6%). 10 , 11 , 12 , 14 , 15 , 16 , 17 , 20 , 21 , 22 , 23 In addition to psychological support and counseling, two articles described the field of educational counseling/cognitive behavior therapy. 14 , 23 Three articles described treatment and diagnosis, 13 , 19 , 20 and one article focused on monitoring 11 and another on psychiatric follow‐up focus. 23
Figure 2.
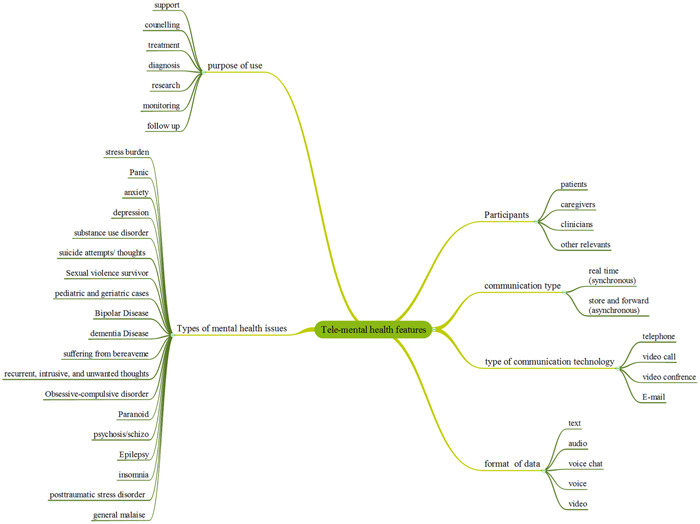
Tree diagram of tele‐mental health features.
The articles addressed a variety of issues in tele‐mental health, which are listed in Table 2. Among these issues, stress, anxiety, and depression were the most considered (10, 76.9%). 10 , 11 , 12 , 13 , 14 , 15 , 16 , 19 , 20 , 21 , 22 One article reviewed remote mental health for patients with dementia disease. 17 Another article examined the adoption, acceptability, appropriateness, and perceptions of the potential sustainability of tele‐mental health for chronic progressive neurologic conditions using combined methods. 18 Ibragimov et al.'s article also discusses issues such as survivors of sexual violence/cases of children and the elderly/severe mental illness in humanitarian, critical, or other low‐resource settings. 23
Table 2.
The characteristics of the reviewed articles.
| Reference | Country | Purpose | Participants | Communication type | Type of communication technology | Format of data | Types of mental health issues | Purpose of use | Type of evaluation | Interoperability with other systems | Challenges | Score based on MMAT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Akhunzad et al. 22 | Pakistan | To find out the frequencies of Psychiatric disorders in the general population during COVID‐19 and to compare the genderbased association between newly diagnosed patients during COVID‐19 with already existing psychiatric patients in Peshawar to provide patient care on priority bases | Patients | Real time | Video call | Video | Anxiety, Depression, Bipolar disease, Dissociative, Obsessive‐compulsive disorder, Paranoid, psychosis/schizo, stress burden, Epilepsy, substance use disorder, Phobic symptoms, and Others | Psychological Support and counseling | Not mentioned | Not mentioned | Not reported | 5/5 |
| 2. Biagianti et al. 13 | Italy | To evaluate intervention feasibility and to assess the impact of the intervention by means of pre post pre‐psychological changes | Patients and other relatives | Real time | Video conference | Video/audio | Anxiety, depression, insomnia, posttraumatic stress disorder, and general malaise | Treatment | Not mentioned | Not mentioned | The lack of follow‐up data | 5/5 |
| 3. Ganesan et al. 16 | India | To assess the effect of telecounseling in reducing anxiety in patients admitted to isolation wards. | Patients | Real time | Telephone | Audio | Anxiety | Psychological Support and counseling | Not mentioned | Not mentioned | “The nonavailability of cell phones, not knowing how to use the cell phone, network and connectivity issues, hearing disability in the older adults“ | 5/5 |
| 4. Ibragimov et al. 23 | Sub‐Saharan Africa/the Middle East and North Africa/Asia | To evaluate the altered service provision in an effort to understand the challenges and successes of implementing tele‐MH care in a tumultuous period, and to better prepare for similar remote care needs in the future. | Patients/caregivers | Store and forward/real time | Video conference | Audio/voice chat/video | Sexual violence survivor/pediatric and geriatric cases/severe mental illness | Psychosocial support and counseling/Educational counseling/Psychiatric follow‐up/cognitive behavior therapy | Mixed methods (Qualitative & quantitive assessment) | Not reported | Access to communication devices/Poor local infrastructure/Patients security and confidentiality/Delivery of MH care from home/Transferability of interventions/Low acceptance by patients/Sudden lockdown/Budget/logistical/Human resource constraints/…. | 4/5 |
| 5. Zhang et al. 19 | USA | To quantify overall trends in patients treated for mental health disorders and adverse events, including via tele‐mental health (TMH) and psychopharmacology during pandemic related health care transformation | Patients | Real time | Telephone | Voice | Depression/posttraumatic stress disorder (PTSD)/substance use disorder/severe mental illness/suicide attempts | Treatment/diagnosis | Not reported | Electronic medical records | Not reported | 4/5 |
| 6. Hazarika et al. 14 | India | To evaluate the sociodemographic profile of the distress callers, their psychosocial concerns, the interventions provided by the service provider, and whether the service users were satisfied with the intervention(s) or not | Patients | Real time | Telephone | Voice | Anxiety/depression/suicidal thoughts | Psychosocial support and counseling/Educational counseling/cognitive behavior therapy | Not reported | Not reported | Resistance to change from the old system to the new | 5/5 |
| 7. Rotondoa et al. 10 | Italy | To give tele‐psychological support to caregivers and evaluate the effect of this intervention by quantifying stress burden and quality of life during the first COVID‐19 lockdown. | Caregivers | Real time | Telephone | Voice | Stress burden | Psychological Support and counseling | Not reported | Not reported | The average of drop out was high/the study was biased by other variables (number of family members, social condition, economic status. Etc)/need a larger and better‐defined populations | 4/5 |
| 8. Di Lorito et al. 17 | England | To present preliminary evidence on tele‐rehabilitation for people with dementia and identify the type of clients with dementia tele‐rehabilitation works for, how, and under which conditions; the benefits for the clients receiving telerehabilitation and the therapists delivering tele‐rehabilitation; and the challenges of telerehabilitation and how to potentially address these | patients/caregivers | Real time | Video call | Video | Dementia Disease | Psychological support and counseling | Not reported | Not reported | Could not challenge participants/required their physical presence/Q Health did not cater to participants with dementia because of their cognitive issues/the digital exclusion that participants lacking basic IT knowledge would face | 5/5 |
| 9. Biancalani et al. 12 | Italy | To contribute preliminary data on client perceptions of change after tele‐psychodrama interventions in time of global crisis. | Patients/caregivers | Store and forward/real time | Video conference | Audio/voice chat/video | Anxiety/depression/panic disorders | Psychological support and counseling | Not reported | Not reported | Electronic devices, the internet, and/or network connection difficulties/communicating online remains a limited medium of expression/social distancing measures to limit the spread of COVID‐19. | 4/5 |
| 10. Biagianti et al. 20 | China | To present the development of a brief remote psychotherapy program for COVID‐19 patients and/or their relatives | Patients and/or their relatives | Store and forward/real time | Video conference | Audio/voice chat/video | Posttraumatic stress disorder (PTSD)/suffering from bereaveme/recurrent, intrusive, and unwanted thoughts/traumatic experience/depersonalization and derealization | Treatment/Psychological support and counseling/research | Not reported | Reimbursement system of the regional health service | Not reported | 5/5 |
| 11. Ravindran et al. 15 | India | To describe the preliminary experience in providing psychosocial support amid the COVID‐19 pandemic from a Tertiary Care Centre in India | Patients/caregivers | Real time | Telephone | Voice | Panic/anxiety/depression/substance use disorder | Psychological Support and counseling | Not reported | Not reported | Being unable to see a distressed individual real time/Use of video‐ conferencing may not be feasible while addressing a large population/Getting calls concerning logistical issues/networks and technological issues | 5/5 |
| 12. Ghazanfarpouri et al. 21 | Iran | To investigate the effectiveness of telecounseling on the mental health of staff in hospitals and coronavirus reference clinics where the screening and referral of suspected individuals are carried out in Iran | Caregivers | Real time/store and forward | Vdeo call | Text, voice | Depression/anxiety | Psychological support and counseling | Not reported | Not reported | Not reported | 5/5 |
| 13. Carmassi et al. 11 | Italy | To investigate acute posttraumatic stress symptoms (PTSS) reported by patients with Bipolar Disorder followed in the framework of a telepsychiatry service, | Patients | Store and forward | Text | Acute PTSS/anxiety/depression/bipolar disease | Monitoring/psychological support and counseling | Not reported | Not reported | Evaluation of efficacy was not an aim of the study | 5/5 |
The interoperability with other systems was only mentioned in three articles, two of which had the ability to connect and access the tele‐mental health system to the electronic medical record, 18 , 19 and one article reported the ability to connect the reimbursement system of the regional health service. 20
According to the results in Table 2, except for four articles, the rest of the articles addressed the challenges of using tele‐mental health. These challenges primarily included technological barriers and technical issues, which were stated in six articles. 12 , 15 , 16 , 17 , 18 , 23 These barriers included access to electronic and communication devices, the Internet and/or network connection problems, audio and video problems, and lack of access to mobile phones and local infrastructure. Other challenges were mainly focused on acceptance and privacy issues. Two articles reported unacceptability or low acceptance by patients regarding the use of tele‐mental health, 14 , 23 and three articles also had physical presence limitations. 15 , 18 , 23 One article referred to budget problems, logistics, human resource constraints patients' security, and confidentiality issues. 23 An article presented the hearing disorders of the elderly as a challenge. 16
3.2. Quality of included studies
MMAT quality assessment was done for 13 studies. All studies scored “yes” to the two screening questions, indicating that the MMAT is appropriate for their assessment. Four out of five qualitative studies scored “yes” in five methodological criteria. 14 , 15 , 17 , 20 One study with a mixed method, 23 clinical trial, 19 and quantitative description scored “yes” on four of the five criteria. The rest of the studies scored “yes” for all five criteria. Therefore, in general, out of 13 studies, four studies have 80% criteria (high quality), and nine studies have 100% criteria (high quality). The results of the quality assessment are presented in the attachment file 1 (Supporting Information: Appendix 1).
4. DISCUSSION
In our review, we briefly describe tele‐mental health during the COVID‐19 epidemic and examine its challenges. The main findings of this study showed that video conferencing, telephone, or video calling are popular communication methods in remote mental health during the pandemic. Additionally, tele‐mental health during the COVID‐19 pandemic has been chiefly for stress, anxiety, and depression disorders and with the purpose of providing psychological support and counseling. Challenges tele‐mental health extracted from selected studies mostly described technical challenges.
According to the results of our study, almost half of tele‐mental health studies are described in developed and high‐income countries, and evidence is scarce in underdeveloped/developing and middle/low‐income countries. While the situation of undeveloped/developing and middle/low‐income countries due to uncertainty about the health status, follow‐up of patients, and medical care in these countries, increases the vulnerability of such societies to the psychological effects of COVID‐19. 24 Therefore, this issue highlights the importance of collecting data from undeveloped/developing and middle/low‐income countries.
Studies have shown that telemedicine is effective and increases access to care. There are various communication methods to access remote care, each with its own advantages and disadvantages. Tele‐mental health communication methods such as video conference, telephone, or video call were more popular in selected studies. Video conferencing and telephone services can facilitate access to remote geographical locations and patient access to mental health services. 5 In addition, telephones provide an excellent means of communication for patients and therapists. They can send and receive text, audio, and video messages that improve the clinical interaction between therapists and patients. Although communication technologies can expand the scope of healthcare services, there are still certain concerns that need to be addressed. For example, video conferencing and video calling eliminate the full‐scale physical presence and some behavioral cues. Mobile phones do not remove visual cues, but text messages remove both audio and visual cues, which can affect the quality of service delivery. 5 , 24
Studies show that the COVID‐19 pandemic can affect people's mental health and cause anxiety, depression, and posttraumatic stress symptoms. 24 , 25 , 26 , 27 For this reason, most of the selected studies in this research describe issues such as stress, anxiety, and depression in the provision of tele‐mental health during the COVID‐19 epidemic. In this regard, the prevalence of stress, anxiety, and depression as a result of the epidemic in the general population, was announced as 29.6, 31.9, and 33.7, 24 which respectively, indicate the widespread impact of the COVID‐19 epidemic on mental health. COVID‐19 is new and unknown, and its rapid transmission, high mortality rate, and concern about the future can be reasons for anxiety. 28 Mental health experts recommend promoting healthy behaviors, avoiding exposure to negative news, and using alternative communication methods such as social networks and digital communication platforms to prevent social isolation and reduce mental disorders caused by COVID‐19. 24
4.1. Challenges
Remote areas with inadequate healthcare providers have difficulty providing primary care to the mentally ill. The use of information technologies such as telemedicine in the management of mental patients provides them with easy access to modern and efficient health services and reliable and affordable diagnoses. 5 , 29 According to studies, using telemedicine for psychotherapy and other psychological services improves patient satisfaction and lowers costs of care. In addition, tele‐mental health can be effective in minimizing direct exposure to Covid‐19 outbreaks and rapid access to health care. 5 However, there are barriers and challenges that prevent the rapid development of tele‐mental health services.
4.1.1. Technical challenges
Technical challenges were the most mentioned challenges in the selected studies. Technical challenges include access to electronic and communication devices, Internet and/or network connectivity issues, audio and video issues, and overall IT infrastructure. Technical concerns should be considered as part of the implementation challenges. 30 It is very important to pay attention to these concerns and challenges because these challenges are one of the main problems in adopting remote mental health. For example, a challenge such as the lack of equal access to telecommunication facilities for the general public is one of the barriers to adoption. 31 On the other hand, access to high‐quality broadband or internet is another technical challenge. The effectiveness of telemedicine depends on the quality of the video, audio, and as well as seamless connectivity. To achieve this goal, good bandwidth and secure connection are very important. 32 According to studies, it has been shown that the development of medical technology with good and accessible bandwidth improves technical issues. 31
4.1.2. Reception challenge
Patient satisfaction is very important in the adoption and use of telemedicine technologies such as tele‐mental health. Therefore, to obtain their consent, they must be informed of the possible risks that may occur during the use of tele‐mental health. On the other hand, the laws regarding consent for the use of telemedicine vary from country to country, and the doctor must check the patient's consent according to the laws of his country. 31
4.1.3. The privacy challenges
Maintaining privacy and ensuring the protection of patients' personal data is one of the most important factors of trust and success in medicine. 33 Telemedicine technology services require the collection and use of sensitive medical information between the physician and the patient. 34 Therefore, there are ethical concerns regarding the use of telehealth services and privacy protection for patients and physicians. They are not sure who might hear the conversation between doctors and patients. 5 This is important to note because patients will be reluctant to use tele‐mental health technology if they are unsure and concerned about privacy. To solve this challenge, technical controls such as data encryption, use of authentication devices, real time authentication of patients, and application of HIPPA rules compatible with telemedicine technology can be used. 35 Additionally, a password can be set for each telemedicine session to be used only by the patient and the physician. Also, to ensure patient privacy, telemedicine sessions should be held in a private space. 31
Gutierrez et al. in a study, suggested the following five steps to reduce the challenges and implement telemedicine systems faster. 36 According to the results of the present study and the challenges extracted for tele‐mental health, we believe that these steps can also be used to improve tele‐mental health:
-
1.
Preparation and training: The system, its needs, and expectations should be taught to patients and doctors.
-
2.
Standardization and acceleration of validation: Processes should be standardized and test sessions with test patients should be conducted for validation.
-
3.
Technology: A basic rule of telemedicine is to use the simplest technology to meet the need. Regardless of the technology used, a backup plan is required.
-
4.
Bandwidth: Having broadband capabilities with unlimited data is very important. Technology support must be provided to ensure adequate Internet connectivity at all locations.
-
5.
Rapid feedback and improvement: After a few days of system deployment, collect feedback to improve quality and address concerns. 36
5. CONCLUSIONS
Tele‐mental health is an import step to provide advanced care to the mentally ill alongside conventional care. Considering the many advantages of telemedicine technology in the field of mental health, the need to use this technology in developing countries, including our country, is obvious. The findings of this research can play an effective role in the successful implementation of such systems by increasing the awareness of managers and policy makers of the healthcare sector.
According to the results of the present study, it is suggested that future directions for remote mental health research for COVID‐19 patients include investigating various challenges in this field, investigating and tracking the longer‐term effects of using this method and providing solutions to increase adoption and improve privacy. In addition, considering that most of the studies were conducted in high‐income countries. Analysis is recommended for the provision of mental health services in different settings, especially in low‐ and middle‐income countries, as this method is a promising approach to increase access to mental health care.
AUTHOR CONTRIBUTIONS
Maryam Nazemi: Data curation, formal analysis, investigation, methodology, software, visualization, writing—original draft. Shamim Kiani: Methodology, visualization, writing—original draft. Somayyeh Zakerabasali: Conceptualization, data curation, formal analysis, project administration, supervision, validation, visualization, writing—original draft, writing—review and editing.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Somayyeh Zakerabasali affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
We express our gratitude to Shiraz University of Medical Sciences. This study received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors.
Nazemi M, Kiani S, Zakerabasali S. Tele‐mental health during the COVID‐19 pandemic: a systematic review of the literature focused on technical aspects and challenges. Health Sci Rep. 2023;6:e1637. 10.1002/hsr2.1637
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article and/or its Supporting Information.
REFERENCES
- 1. Larsen A, Tele A, Kumar M. Mental health service preferences of patients and providers: a scoping review of conjoint analysis and discrete choice experiments from global public health literature over the last 20 years (1999–2019). BMC Health Serv Res. 2021;21(1):589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yue JL, Yan W, Sun YK, et al. Mental health services for infectious disease outbreaks including COVID‐19: a rapid systematic review. Psychol Med. 2020;50(15):2498‐2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Johnson S, Dalton‐Locke C, Vera San Juan N, et al. Impact on mental health care and on mental health service users of the COVID‐19 pandemic: a mixed methods survey of UK mental health care staff. Soc Psychiatry Psychiatr Epidemiol. 2021;56(1):25‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zaçe D, Hoxhaj I, Orfino A, Viteritti AM, Janiri L, Di Pietro ML. Interventions to address mental health issues in healthcare workers during infectious disease outbreaks: a systematic review. J Psychiatr Res. 2021;136:319‐333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Langarizadeh M, Tabatabaei M, Tavakol K, Naghipour M, Moghbeli F. Telemental health care, an effective alternative to conventional mental care: a systematic review. Acta Inform Med. 2017;25(4):240‐246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mazziotti R, Rutigliano G. Tele‐mental health for reaching out to patients in a time of pandemic: provider survey and meta‐analysis of patient satisfaction. JMIR Ment Health. 2021;8(7):e26187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ali NA, Khoja A, Kazim F. Role of the telemental health services during the COVID‐19 pandemic: a systematic review. Turkish J Psychiatry. 2021;32(4):275‐282. [DOI] [PubMed] [Google Scholar]
- 8. Appleton R, Williams J, Vera San Juan N, et al. Implementation, adoption, and perceptions of telemental health during the COVID‐19 pandemic: systematic review. J Med Internet Res. 2021;23(12):e31746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hong QN, Fàbregues S, Bartlett G, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34:1‐7. [Google Scholar]
- 10. Rotondo E, Galimberti D, Mercurio M, et al. Caregiver tele‐assistance for reduction of emotional distress during the COVID‐19 pandemic. Psychological support to caregivers of people with dementia: the Italian experience. J Alzheimer's Dis. 2022;85(3):1045‐1052. [DOI] [PubMed] [Google Scholar]
- 11. Carmassi C, Bertelloni CA, Dell'Oste V, et al. Tele‐psychiatry assessment of post‐traumatic stress symptoms in 100 patients with bipolar disorder during the COVID‐19 pandemic social‐distancing measures in Italy. Front Psychiatry. 2020;11:580736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Biancalani G, Franco C, Guglielmin MS, et al. Tele‐psychodrama therapy during the COVID‐19 pandemic: participants' experiences. Arts Psychotherapy. 2021;75:101836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Biagianti B, Lisi I, Di Liberto A, et al. Feasibility and preliminary efficacy of brief tele‐psychotherapy for COVID‐19 patients and their first‐degree relatives. J Affect Disord. 2023;330:300‐308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hazarika M, Das B, Das S, et al. Profile of distress callers and service utilisation of tele‐counselling among the population of Assam, India: an exploratory study during COVID‐19. Open J Psychiatry Allied Sci. 12(1)2021:7‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ravindran S, Nirisha P L, Channaveerachari NK, et al. Crossing barriers: role of a tele‐outreach program addressing psychosocial needs in the midst of COVID‐19 pandemic. Asian J Psychiatry. 2020;53:102351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ganesan S, Balasubramanian B, Krishnamurthy P, Govindan R, Mani N. Effects of tele‐counseling on reducing anxiety levels of COVID‐19 patients in isolation wards: an observational study. Indian J Psychol Med. 2023;45(1):43‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Di Lorito C, Duff C, Rogers C, et al. Tele‐Rehabilitation for people with dementia during the COVID‐19 pandemic: a case‐study from england. Int J Environ Res Public Health. 2021;18(4):1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Saliba‐Gustafsson EA, Miller‐Kuhlmann R, Kling SMR, et al. Rapid implementation of video visits in neurology during COVID‐19: mixed methods evaluation. J Med Internet Res. 2020;22(12):e24328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang J, Boden M, Trafton J. Mental health treatment and the role of tele‐mental health at the veterans health administration during the COVID‐19 pandemic. Psychol Serv. 2022;19(2):375‐385. [DOI] [PubMed] [Google Scholar]
- 20. Biagianti B, Zito S, Fornoni C, et al. Developing a brief tele‐psychotherapy model for COVID‐19 patients and their family members. Front Psychol. 2021;12:784685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ghazanfarpour M, Ashrafinia F, Zolala S, Ahmadi A, Jahani Y, Hosseininasab A. Investigating the effectiveness of tele‐counseling for the mental health of staff in hospitals and COVID‐19 clinics: a clinical control trial. Trends Psychiatry Psychother. 2022;44:e20200176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Akhunzada WA, Laghari DK, Rasheed H, et al. Tele‐psychiatry during COVID‐19 at HMC Peshawar. J Liaquat Univ Med Health Sci. 2023;22(01):64‐67. [Google Scholar]
- 23. Ibragimov K, Palma M, Keane G, et al. Shifting to tele‐mental health in humanitarian and crisis settings: an evaluation of médecins sans frontières experience during the COVID‐19 pandemic. Confl Health. 2022;16(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Salari N, Hosseinian‐Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID‐19 pandemic: a systematic review and meta‐analysis. Global Health. 2020;16(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID‐19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cénat JM, Blais‐Rochette C, Kokou‐Kpolou CK, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID‐19 pandemic: a systematic review and meta‐analysis. Psychiatry Res. 2021;295:113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shah SMA, Mohammad D, Qureshi MFH, Abbas MZ, Aleem S. Prevalence, psychological responses and associated correlates of depression, anxiety and stress in a global population, during the coronavirus disease (COVID‐19) pandemic. Community Ment Health J. 2021;57(1):101‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Banerjee D. The COVID‐19 outbreak: crucial role the psychiatrists can play. Asian J Psychiatry. 2020;50:102014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pandya A, Shah K, Chauhan A, Saha S. Innovative mental health initiatives in India: a scope for strengthening primary healthcare services. J Family Med Prim Care. 2020;9(2):502‐507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Portnoy J, Waller M, Elliott T. Telemedicine in the era of COVID‐19. J Allergy Clin Immunol Practice. 2020;8(5):1489‐1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alipour J, Hayavi‐Haghighi MH. Opportunities and challenges of telehealth in disease management during COVID‐19 pandemic: a scoping review. Appl Clin Inform. 2021;12(4):864‐876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID‐19 pandemic. J Am Coll Surg. 2020;231(2):216‐222e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mahajan V, Singh T, Azad C. Using telemedicine during the COVID‐19 pandemic. Indian Pediatr. 2020;57(7):658‐661. [PubMed] [Google Scholar]
- 34. Shokri T, Lighthall JG. Telemedicine in the era of the COVID‐19 pandemic: implications in facial plastic surgery. Facial Plastic Surgery Aesthetic Med. 2020;22(3):155‐156. [DOI] [PubMed] [Google Scholar]
- 35. Costa M, Reis G, Pavlo A, Bellamy C, Ponte K, Davidson L. Tele‐mental health utilization among people with mental illness to access care during the COVID‐19 pandemic. Community Ment Health J. 2021;57(4):720‐726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gutierrez J, Kuperman E, Kaboli PJ. Using telehealth as a tool for rural hospitals in the COVID‐19 pandemic response. J Rural Health. 2021;37(1):161‐164. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and/or its Supporting Information.


