Abstract
There have been hundreds of millions of cases of coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). With the growing population of recovered patients, it is crucial to understand the long-term consequences of the disease and management strategies. Although COVID-19 was initially considered an acute respiratory illness, recent evidence suggests that manifestations including but not limited to those of the cardiovascular, respiratory, neuropsychiatric, gastrointestinal, reproductive, and musculoskeletal systems may persist long after the acute phase. These persistent manifestations, also referred to as long COVID, could impact all patients with COVID-19 across the full spectrum of illness severity. Herein, we comprehensively review the current literature on long COVID, highlighting its epidemiological understanding, the impact of vaccinations, organ-specific sequelae, pathophysiological mechanisms, and multidisciplinary management strategies. In addition, the impact of psychological and psychosomatic factors is also underscored. Despite these crucial findings on long COVID, the current diagnostic and therapeutic strategies based on previous experience and pilot studies remain inadequate, and well-designed clinical trials should be prioritized to validate existing hypotheses. Thus, we propose the primary challenges concerning biological knowledge gaps and efficient remedies as well as discuss the corresponding recommendations.
Subject terms: Infectious diseases, Immunological disorders
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has brought about an unprecedented scale of burden on health care systems.1,2 More than 770 million cases of COVID-19 and over 6.9 million fatalities have been documented since the outbreak.3 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of COVID-19, gains entry into host cells by combining with angiotensin-converting enzyme 2 (ACE2).4,5 Subsequently, SARS-CoV-2 undergoes replication and provokes damage to multiple organs/tissues, resulting in a complex array of clinical manifestations and potential long-term sequelae.6,7
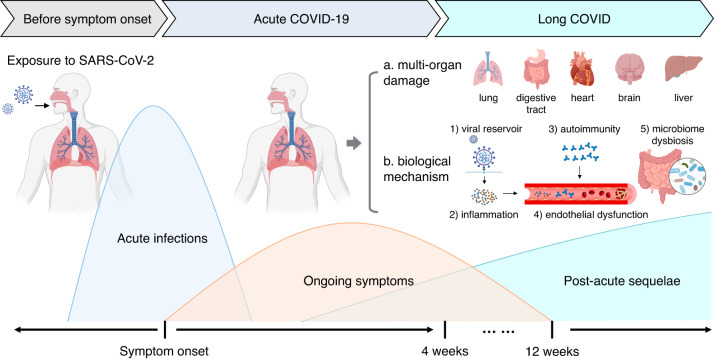
Long COVID, also referred to as ongoing symptomatic COVID-19 and post-acute sequelae of COVID-19 (PASC), is defined as symptoms of COVID-19 that persist for between 4 and 12 weeks or a post-acute syndrome at over 12 weeks after the onset of acute symptoms that cannot be attributed to any other illnesses8–10 (Fig. 1). According to recent research, patients with long COVID exhibit impairment of multiple organs, which manifests as a range of symptoms, including persistent fatigue, diarrhea, dyspnea, limited exercise tolerance, endocrine abnormalities, taste and smell dysfunction, and depression11–16 (Fig. 2). Furthermore, long COVID has been observed in a diverse spectrum of COVID-19 regardless of the mild or severe illness.17–19 Thus, it could be conceivably hypothesized that a more devastating effect could occur in the long COVID period than in the acute period of COVID-19. Nevertheless, the pathophysiological mechanisms and effective therapeutic choices regarding long COVID are unknown.
Fig. 1.
Timeline and multi-organ damage of long COVID. Long COVID is defined as the ongoing symptoms of COVID-19 patients between 4 and 12 weeks, or the post-acute syndrome over 12 weeks after the acute symptoms onset. In addition, the commonly involved organs and biological mechanisms are outlined
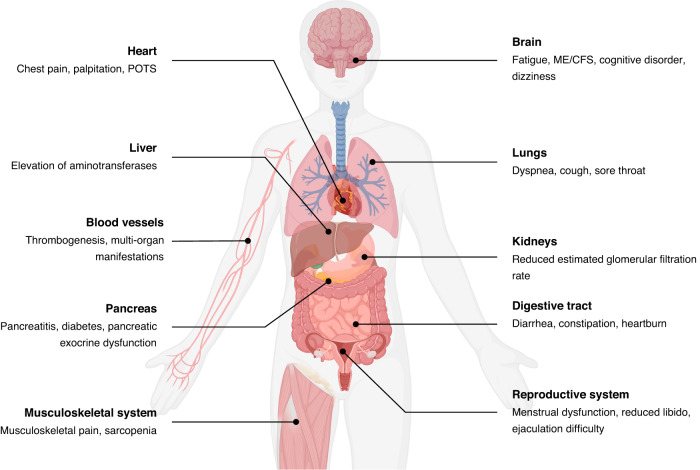
Fig. 2.
Multi-system symptoms/manifestations of long COVID. Long COVID has served as a multi-organ disease which can damage respiratory system, cardiovascular system, neuropsychic system, digestive system, circulatory system, musculoskeletal system, and genitourinary systems. ME/CFS myalgic encephalomyelitis/chronic fatigue syndrome, POTS postural orthostatic tachycardia syndrome
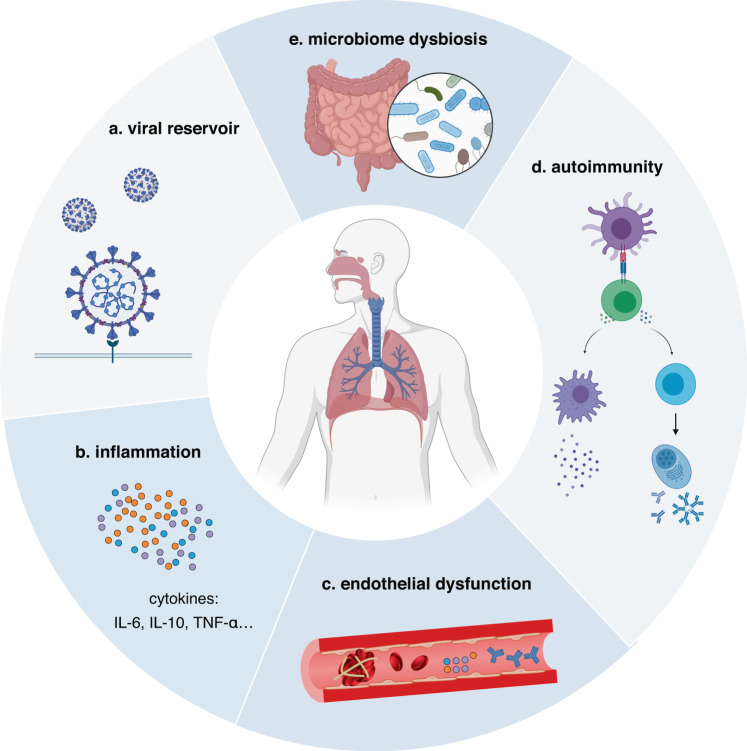
Even so, multiple hypotheses concerning the pathophysiology of long COVID have been recently proposed (Fig. 3). The prevailing theories for underlying mechanisms comprise persisting viral reservoirs,20 sustained inflammation,21 host microbiome factors,22,23 persistent autoimmune responses,24 and endothelial dysfunction and subsequent blood clotting.25 Nevertheless, these studies regarding mechanistic hypotheses are mostly at the preliminary stage, and further research regarding the pathophysiology of long COVID is urgently needed.
Fig. 3.
The potential pathophysiological mechanisms of long COVID. The main hypothesized pathophysiological mechanisms for long COVID include viral reservoir, gut microbiome dysbiosis, endothelial dysfunction, autoimmunity, and inflammation
Herein, we thoroughly describe the current understanding concerning the epidemiology, prevalent manifestations, pathophysiological mechanisms, and potential diagnostic tools and therapeutic options of long COVID. Furthermore, the present obstacles that need to be solved to advance long COVID research are discussed.
Methods
To comprehensively understand the epidemiology, mechanisms, and management of long COVID, extensive literature searches were conducted of reputable databases, including PubMed, the Web of Science, EMBASE, and the Cochrane Library. The search spanned from January 2020 to June 2023, ensuring a thorough collection of relevant articles. The search terms involved “long COVID”, “post-acute sequelae of COVID-19”, “epidemiology”, “symptom”, “mechanism”, “management”, and their relative terms. Two authors screened the studies independently via the titles and abstracts. Afterwards, a meticulous review of the full texts of the eligible studies was performed. All included studies were written in English. Disagreements were reassessed by a third reviewer. Ultimately, the literature was read through and discussed by all authors to yield reliable conclusions.
Epidemiology of long COVID
As the patient population recovering from acute COVID-19 continues to grow, recent studies have increasingly focused on investigating the post-acute effects of SARS-CoV-2 infection.25–35 An international observational study of individuals from 56 countries assessed the outcomes of 3762 confirmed or suspected COVID-19 patients within 6 months of infection via an online survey.26 The overwhelming majority of patients (65.2%) had at least one symptom at 6 months, of which fatigue (80%), post-exertional weakness (73.3%), and cognitive impairment (58.4%) were common clinical manifestations.26
Long COVID symptoms have also been recorded in studies conducted in China, providing significant data on the prevalence and characteristics of these symptoms. Long-term sequelae were evaluated in a cohort study comprising 1733 COVID-19 patients who had been discharged through the utilization of a range of assessments, including questionnaires, physical examinations, blood tests, a 6-minute walk test, ultrasonography, pulmonary function assessments, and imaging of the chest.27 At 6 months after the onset of symptoms, muscle weakness or fatigue was observed in 63% of cases, followed closely by sleep disorders (26%) and depression/anxiety (23%).27 In an identical cohort throughout a 2-year follow-up after acute SARS-CoV-2 infection, the morbidity rate of long COVID exhibited a substantial decline, dropping from 68% at 6 months to 55% after a 2-year period.28 Analogously, fatigue or muscle weakness was the prevailing manifestation, with an incidence of 30%.28 Sleep difficulties, hair loss, dizziness, and palpitations had a high incidence of over 10%.28 Although longitudinal improvements have been witnessed among studies, the prevalence of long COVID sequelae remains stubbornly high, implying that these sequelae may last long and lead to a tremendous burden on patients.
Studies from European countries have proclaimed similar results.29–34 In a French cohort with 150 confirmed COVID-19 patients, long COVID symptoms were collected via electronic medical records or telephone follow-up.29 At 60 days after symptom onset, 66% of patients had at least one sequela. Among these symptoms, the most frequent manifestation was asthenia (40%), followed by dyspnea (30%) and anosmia/ageusia (23%).29 According to a prospective cohort study from Spain, 50.9% of COVID-19 patients suffered from long COVID symptoms 10 to 14 weeks after illness onset.30 Furthermore, more detailed information regarding respiratory manifestations was assessed by spirometry or chest radiology. Reduced pulmonary function was noted in 9.3% of cases, and abnormal imaging results were found in 18.9% of patients.30 Analogously, data from the northern Netherlands involving 4231 COVID-19 patients and 8462 matched controls revealed that 21.4% of COVID-19 individuals and 8.7% of controls experienced persistent symptoms, including dyspnea, chest pain, painful muscles, lump in throat, ageusia/anosmia, heavy extremities, tingling extremities, paresthesia, and fatigue.32 In another study from the United Kingdom, a telephone screening instrument was designed to attain the post-acute COVID-19 sequelae and quality of life of patients with or without intensive care unit (ICU) care.31 Emerging COVID-19-related fatigue had the highest prevalence of 72% in ICU patients and 60.3% in non-ICU patients, and the alarming incidence of breathlessness as well as psychological distress was also emphasized.31
In an observational cohort study reporting 60-day outcomes from 38 hospitals in Michigan, the United States, medical records and telephone follow-up were adopted to aggregate longer-term consequences.35 After a 60-day period following discharge, 488 (41.8%) patients completed the follow-up, of whom 159 (32.6%) had persistent symptoms related to COVID-19, 75 (15.4%) had a sustained cough, 81 (16.6%) had wheezing/chest tightness/breathlessness, 44 (9.0%) experienced difficulty in ambulation, and 112 (23.0%) suffered from breathlessness when walking up stairs.35 In addition, according to the Morbidity and Mortality Weekly Report (MMWR) from the United States, 38.2% of participants with SARS-CoV-2 infection versus 16.0% of controls had long-term sequelae.36 Notably, the occurrence of long COVID was significantly more prevalent in individuals aged ≥65 years (45.4%) than in patients aged 18–64 years (35.4%).36 Thus, prevention strategies for long COVID sequelae should be emphasized, particularly in elderly individuals with COVID-19.
The aforementioned evidence has significantly enhanced our understanding of the manifestations of long COVID and aided in the identification of individuals at a heightened risk of developing sequelae following SARS-CoV-2 infection. Due to a number of factors, such as follow-up time, heterogeneity in self-reported data, variations in SARS-CoV-2 strains, and race and ethnicity, there are differences in long COVID epidemiology in distinct investigations. In addition, symptomatic differences are present in hospitalized and non-hospitalized individuals. Recent studies have indicated that participants allocated to general wards or ICUs had a higher likelihood of experiencing long COVID symptoms than individuals who were not hospitalized.37,38 However, hospitalization seems to be the only risk factor for complication probability rather than the severity of long COVID.39 These outcomes indicate that a large number of patients are likely to have long COVID, and efficient prevention and treatment strategies are warranted for combating numerous clinical manifestations. Moreover, the association between plentiful hazard factors and morbidity of long COVID remains to be investigated.
Impact of variants and vaccines on long COVID
Since the COVID-19 pandemic, multiple variants have emerged with enhanced transmissibility, which may contribute to the increased number of patients with severe illness and even long COVID manifestations.40–42 The data from the Israeli nationwide health care organization revealed that long COVID symptoms associated with infections with all variants, including prototype, Alpha, and Delta variants, remained consistent.43 Nevertheless, another study revealed that infection with the prototype variant was associated with a higher prevalence of long COVID symptoms than infection with the Alpha or Delta variant.44 Among these variants, dyspnea was found to be more prevalent in patients infected with the prototype variant, while hair loss was more commonly observed in patients infected with the Delta variant.44 Interestingly, the prevalence of fatigue was found to be similar across both variants.44 Compared to these variants, the current data suggested that the Omicron variant possibly led to fewer clinical manifestations of long COVID.45 A study from Eastern India revealed that approximately 8.2% of patients infected with the Omicron variant self-reported experiencing long COVID manifestations, which is relatively lower than estimates for those infected with the Delta variant.46 Similarly, 4.5% of patients with an Omicron variant infection and 10.8% of those infected with the Delta variant in an observational study in the United Kingdom (UK) had long COVID.47 Despite the relatively low morbidity, the increased transmissibility of the Omicron variant may result in a larger number of potential patients with long COVID.48 Thus, it is essential to develop medications with special effects against long COVID to alleviate its clinical manifestations.
The approved vaccines have been proven to be highly effective in preventing COVID-19, especially severe illness.49,50 Notably, these vaccines also exhibit the capacity to prevent long COVID.51 In participants who received an mRNA or adenovirus vector COVID-19 vaccine, 12.8% and 8.8% decreases in long COVID morbidity were initially observed after one dose and two doses, respectively.52 Similarly, in a study involving 739 COVID-19 participants from Italy, the prevalence of long COVID was found to be 41.8% in unvaccinated individuals, 30.0% in those with one dose, 17.4% in those with two doses, and 16.0% in those with three doses, showing a correlation between the number of vaccine doses and long COVID prevalence.53 Compared to one dose, two vaccination doses also lower the risk of a larger range of manifestations, including myocarditis, myalgia, cerebral hemorrhage, anosmia, and interstitial lung disease within six months after infection, among other symptoms.54 In addition to reducing morbidity, a sentinel cohort study conducted in the United Kingdom emphasized the crucial role of vaccination in lowering the mortality rate among long COVID patients,55 further implying the importance of vaccination. However, the data from the Israeli nationwide health care organization indicated that, among the sequelae of long COVID, the administration of a vaccine led to merely a reduced prevalence of dyspnea in cases with a breakthrough infection.43 The differences in vaccines and races may be the underlying cause of the inconsistent results above. Despite the potential protective effect of vaccines, a higher antibody titer is correlated with worse sequelae,56 suggesting that an excessive immune response should be considered during vaccination.
Notably, increasing reinfection is extensively associated with the additional morbidity of long COVID sequelae involving cardiovascular, pulmonary, endocrine, hematological, gastrointestinal, mental, urinary, neurological, and musculoskeletal disorders.57 Therefore, adopting adequate strategies to prevent reinfection is necessary. Although vaccine administration holds a remarkably protective effect, the risk of long COVID remains high.57,58 Moreover, breakthrough SARS-CoV-2 infection (BTI), which refers to the occurrence of SARS-CoV-2 infection within 14 days of vaccination, increases the risk of experiencing various long COVID manifestations, including coagulation and hematologic, cardiovascular, kidney, gastrointestinal, neurologic, metabolic, and musculoskeletal disorders.59 Thus, reliance on vaccines is incapable of optimally mitigating the persistent sequelae of COVID-19, and prevention strategies for SARS-CoV-2 infection and treatment options for sequelae should be emphasized to enhance the quality of life of patients.
Symptoms and possible mechanisms
Neuropsychiatric system
The clinical manifestations of the neuropsychiatric system, which primarily include memory loss, sensorimotor aberration, cognitive disorder, paresthesia, loss of smell or taste, dizziness, and audiovestibular symptoms,60–66 seem to be the prominent features of long COVID, severely impeding the daily activities of patients. Among multiple neuropsychiatric symptoms, a meta-analysis indicated that fatigue and cognitive manifestations were the most prevalent symptoms of long COVID, with proportions of 32% and 22%, respectively.67 Cognitive disorder is a complicated neuropsychological syndrome characterized by the impairment of thinking, perceiving, and remembering.68 According to a recent study of 236,379 patients, the estimated incidences of parkinsonism, dementia, anxiety, and psychotic syndromes among cognitive disorders following six months of SARS-CoV-2 infection were 0.11%, 0.67%, 17.39%, and 1.40%, respectively.69 Within the field of cognitive symptoms, approximately a quarter of patients suffer from “brain fog”, a newly proposed syndrome encompassing attention deficits, processing speed issues, language fluency difficulties, memory problems, and executive function disorders.70,71 Even though these symptoms have low morbidity, cognitive impairments still require sufficient attention. A cohort study with a follow-up period up to 2 years after COVID-19 onset implied that common psychiatric manifestations such as mood disorders and anxiety returned to normal within 2 months, whereas the risks of brain fog, dementia, epilepsy, and psychotic disorders were still increasing at the end of 2 years.72 Additionally, sufficient emphasis should be placed on children due to the higher risk of persistent seizures/epilepsy and psychotic disorders compared with adults.72 Therefore, fully understanding the pathophysiological mechanisms of these manifestations is critical for prevention and treatment.
There are several possible hypotheses for their pathophysiology. The first explanation is the existence of an active-virus reservoir in the nervous system and neuronal injury.73–75 An in vitro experiment assessed SARS-CoV-2 infection in nerve cells and brain organoids and found that viral proteins and infectious particles of the virus were profiled in brain organoids.73 Simultaneously, cortical neurons and neural precursor cells were verified to be the direct binding site of SARS-CoV-2,73 suggesting that the virus probably invades the human brain and contributes to neuropsychiatric symptoms such as anosmia, ageusia, encephalitis, and Guillain‒Barre syndrome. Among nonhuman primates, sporadic SARS-CoV-2 has been detected in the brains of infected animals.74 Moreover, the pathophysiological processes of neuroinflammation, hypoxia, and microhemorrhages have also been observed,74 providing novel perspectives on the neuropsychiatric manifestations of long COVID. Aside from animal experiments, complete autopsies and sampling from the central nervous system of COVID-19 patients have shown that viral replication widely occurs in tissues/organs, including the brain, at 7 months after acute infection.75 In ORF6 and ORF10 of the SARS-CoV-2 proteome, two amyloidogenic subsequences with self-assembled structures were screened to have high toxicity for neurons by means of nanoscale imaging, spectroscopy, molecular modeling, kinetic assays, and X-ray scattering,76 triggering the neurologic symptoms of patients and further supporting the impact of persistent SARS-CoV-2 in neuropsychiatric symptoms of long COVID.
Neuroinflammation has also been confirmed as an imperative mechanism for the neuropathology of long COVID.77 An investigation based on the UK Biobank comprising 401 COVID-19 participants showed that a reduction in brain size as well as reduced gray matter thickness in the parahippocampal gyrus and orbitofrontal cortex were noted via magnetic resonance imaging (MRI) at 141 days after infection.78 Similar structural changes were also observed in a German study,79 indicating the possibility of neuroinflammatory events and degenerative hallmarks in patients with long COVID. To elucidate the underlying mechanisms, an in vivo experiment illustrated that inflammation-associated cytokines/chemokines such as CCL11 might promote hippocampal microglial activity and inhibit neurogenesis, which was comparable to the neuropathophysiology of cancer therapy and contributed to cognitive impairment.80,81 Inflammasome activation induced by viral infection also facilitates the activation of transforming growth factor beta (TGF-β) signaling as well as oxidative overload, thus resulting in Alzheimer’s disease-like features and cognitive disorders.82 Furthermore, a study on golden hamsters revealed immune cell activation and the production of proinflammatory cytokines in the olfactory bulb and olfactory epithelium, which even existed one month after SARS-CoV-2 clearance.83 These outcomes underscore the role of neuroinflammation in persistent neuropsychiatric symptoms.
Injury to blood vessels is likewise involved in the pathophysiology of the neuropsychiatric manifestations of long COVID. The impaired vessel density of retinal capillary microcirculation was shown to be more noticeable in long COVID patients than in controls,84 validating that blood vessel damage might promote persistent symptoms. Furthermore, endothelial dysfunction has been proven to facilitate long COVID. A retrospective study revealed that elevated levels of endothelial cell markers, such as von Willebrand factor (VWF) antigen and VWF propeptide, were observed in COVID-19 patients after an average of 68 days following infection,85 signifying sustained endothelial dysfunction in long COVID patients. Similarly, another study indicated that patients with COVID-19 developed endothelial dysfunction over 6 months after discharge compared with healthy participants.86 Nevertheless, the impact of endothelial dysfunction on cerebrovascular manifestations of long COVID merits further investigation.
Myalgic encephalomyelitis/chronic fatigue syndrome
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a neuroimmune illness characterized by intolerance to systemic exertion and chronic fatigue that cannot be alleviated via rest.87,88 The diagnostic criteria of ME/CFS comprise substantial impairment in daily activities for a minimum of 6 months and profound fatigue of new/definite onset that cannot be relieved by rest, accompanied by post-exertional malaise and unrefreshing sleep, cognitive impairment and/or orthostatic intolerance.89 For most patients with ME/CFS, ‘infectious-like’ manifestations involving fever, respiratory and digestive symptoms, myalgia, and lymphadenopathy universally emerge before illness onset.60,87,89
Fatigue syndromes after confirmed infection that might meet the diagnostic criteria of ME/CFS have been reported for multiple pathogens, including Ebola virus, Epstein-Barr virus, herpesvirus-6, SARS-CoV, and Mycoplasma pneumoniae.90–94 The potential correlation between long COVID and ME/CFS has also been commented by many researchers. A systematic review of 21 studies revealed that the clinical manifestations of ME/CFS exhibited many overlaps with long COVID.95 The presence of ME/CFS has also been observed in both children and adults with confirmed long COVID.96,97 Among participants over 18 years old with long COVID, 58.7% met the criteria for ME/CFS.96 In a cross-sectional survey, 40% of children and adolescents with COVID-19 were reported to have documented ME/CFS.97
The pathophysiological processes of ME/CFS could be summarized as initial immune and inflammatory responses, vascular dysregulation, and autonomic/metabolic adaptation.89,98 The widespread inflammatory response triggered by SARS-CoV-2 infection has been reported in patients with varying degrees of illness severity,80,99 which could occur in the nervous system and contribute to neuropsychiatric symptoms.80,83 The interaction networks of ME/CFS and long COVID, including inflammatory cytokines comprising interleukin (IL)-6 and IL-1B, common genes, and microRNAs, have recently been depicted,100 revealing the potential mechanism of ME/CFS in the occurrence of long COVID and further emphasizing the significance of the inflammatory response. Meanwhile, the dysregulation of endothelin-1 has been found in long COVID patients and cases presenting exertion intolerance and persistent fatigue, suggesting the emergence of endothelial dysfunction and its effect on ME/CFS.101 Moreover, metabolic disorders of energy probably promote exercise intolerance and nervous symptoms. The dysregulation of mitochondrial membrane potential and plasma metabolites related to mitochondria-dependent lipid catabolism are manifested in patients with long COVID,102,103 perhaps conducive to ME/CFS development. Intriguingly, a study implementing machine learning to assess antibody-binding data revealed that the microbiota-immune axis was involved in the pathophysiology of ME/CFS,104 suggesting that the microbiota could serve as a novel direction for investigating ME/CFS in post-COVID-19 syndromes.
Under certain circumstances, several diseases, such as mast cell activation syndrome, postural orthostatic tachycardia syndrome (POTS), intracranial hypertension, and craniocervical obstructions, are generally comorbid with ME/CFS.105–107 Quite a few studies have also documented the corresponding manifestations in patients with long COVID.26,95 However, the comorbid diseases of ME/CFS in long COVID remain enigmatic and worth further investigation.
Cardiovascular system
Cardiovascular system symptoms remain one of the dominating persistent manifestations of long COVID. The prevalence of cardiac symptoms differs among current studies.26,108–110 In a study integrating data for individuals from 56 countries, the main symptoms of chest pain, palpitations, and fainting occurred in 86.04% of individuals with long COVID.26 For COVID-19 patients, a study of 153,760 patients showed that the burden of cardiovascular outcome per 1000 persons was 49.37 for dysrhythmia, 2.44 for inflammatory heart disease, and 18.47 for ischemic heart disease at 12 months after the COVID-19-positive test.110 Furthermore, POTS, a specific subtype of cardiovascular manifestation, was observed in approximately 30% of patients with.111
Several potential hypotheses of cardiovascular manifestations caused by long COVID have been proposed recently. Cardiac injury could occur in the acute or post-acute phase after viral infection. During the acute stage, the elevation of cardiac markers such as cardiac troponin signifies myocardial ischemia and injury.112 Regarding the mechanism, it has been confirmed that direct viral toxicity plays a crucial role in mediating myocardial injury by affecting angiotensin-converting enzyme 2 (ACE2) receptors.113 A pathological analysis of autopsy indicated that cardiac thrombi were observed in 78.6% of patients, and microthrombi in small muscular arteries, capillaries, and arterioles were noted in 64.3% of patients with myocyte necrosis.114 Thus, thrombosis is also an essential mechanism resulting in myocardial injury. The potential explanation of thrombosis is that SARS-CoV-2 directly targets pericytes with high ACE2 expression and consequently induces endothelial cell dysfunction,115,116 contributing to increased microvascular endothelial permeability and ultimately leading to thrombotic complications in microcirculation. Furthermore, the upregulation of cytokines IL-6, IL-1, and tumor necrosis factor (TNF)-α might also trigger endothelial dysfunction and platelet activation to facilitate thrombosis,99 which could eventually cause myocardial damage.
The mechanisms of persistent cardiac injury in the post-acute and chronic disease stages are still unclear. One possible mechanism is that the persistent presence of the virus may contribute to the development of cardiac symptoms in individuals with long COVID. Several studies have revealed that SARS-CoV-2 is detectable in plasma, stool, urine, and multiple organs for more than 4 months,117–119 causing persistent damage. Apart from viral persistence, autoantibodies also exert vital effects on cardiovascular system symptoms. Multiple studies have verified the high level of autoantibodies in patients with long COVID, such as antibodies against ACE2, β2-adrenoceptors, and M2 receptors.60,117,120,121 Hence, autoimmunity against cardiac antigens may cause chronic damage to the cardiovascular system.
Respiratory system
Respiratory symptoms such as cough and dyspnea are common clinical manifestations of long COVID.26,122–124 An Italian study demonstrated that 43.4% of COVID-19 patients had persisting dyspnea at 60 days following onset.122 In addition, an international study reported that approximately 40% and 20% of patients with long COVID had dyspnea and dry cough over 6 months, respectively.26 This evidence shows that the respiratory manifestations of COVID-19 may persist for an extended duration and be worth heeding.
On account of acute respiratory disease, quite a number of COVID-19 patients, especially those with severe/critical disease, may suffer from diffuse alveolar damage, severe endothelial injury, and thrombosis,125 accordingly causing substantial and persistent injury to the lungs. Nevertheless, many patients with mild/moderate illness develop small airway dysfunction in the post-acute phase via quantitative chest computed tomography (CT) evaluation.126 A probable explanation is persistent SARS-CoV-2 in lung tissue.119 Thus, direct viral toxicity could constantly cause damage to the respiratory system. In some COVID-19 patients with ongoing dyspnea, increased expression levels of cytokines such as IL-1β, IL-6, and IL-8 have been observed,99,127 which may also contribute to pulmonary fibrosis. Furthermore, the dynamics of the airway immune microenvironment could induce respiratory manifestations. In assessments of the immune-proteomic landscape between healthy controls and long COVID patients, the expression levels of proteins correlated with apoptosis and epithelial injury have been shown to be higher in long COVID patients, and ongoing cytotoxic T-cell activation probably facilitated long-term lung injury.128 Likewise, another study revealed a positive correlation between SARS-CoV-2-specific T cells and systemic inflammation, while a negative correlation was observed with lung function,129 signifying that SARS-CoV-2-specific T cells may play an essential role in respiratory symptoms.
Digestive system
The gastrointestinal symptoms of long COVID mainly include heartburn, gastrointestinal disorders, constipation, loss of appetite, and abdominal pain.130–133 An online survey of individuals from 56 countries showed that 20.5% of participants with long COVID experienced persistent diarrhea, and 13.7% of long COVID patients had loss of appetite, even 7 months after infection.26 A prospective study of 749 COVID-19 survivors revealed that gastrointestinal symptoms were experienced by approximately 29% of participants after a period of 6 months following viral infection.134 Among them, the leading digestive manifestations included reflux/heartburn (16.3% of cases), constipation (11.1% of cases), diarrhea (9.6% of cases), abdominal pain (9.4% of cases), and nausea/vomiting (7.1% of cases).134 Thus, the effect of digestive system manifestations on the quality of life of patients with long COVID cannot be neglected.
The probable hypotheses of the mechanisms regarding gastrointestinal symptoms comprise the persistent viral component or active virus and alterations in gut microbiota. Multiple studies have been undertaken to validate persistent SARS-CoV-2 in the gastrointestinal tract and found that viral RNAs and proteins in stool and gut tissue could be detected up to 12 months after diagnosis.135–137 By performing an endoscopy study, it was observed that a significant number of patients still had detectable levels of the nucleocapsid protein of SARS-CoV-2 in the gut epithelium even 7 months after the initial infection.137 Furthermore, most patients with antigen persistence were reported to have long COVID, which did not occur in the participants without persistent antigens.137
The gut microbiota is considered a complicated ecosystem that significantly affects human health and multiple diseases.138 Recent evidence has also revealed that the gut microbiota exerts a critical function in gastrointestinal symptoms of long COVID.22,139–141 The microbiome of long COVID patients is characterized by elevated levels of Bacteroides vulgatus and Ruminococcus gnavus, along with a decreased abundance of Faecalibacterium prausnitzii,22 which may facilitate the digestive manifestations of long COVID. Intriguingly, the gut microbiota has recently been validated to have predictive potential. Opportunistic pathogens of the gut are related to respiratory symptoms, while nosocomial pathogens such as Actinomyces naeslundii and Clostridium innocuum may contribute to neuropsychiatric manifestations, and butyrate-producing bacteria present an inverse association with long COVID.22 Analogously, patients with persistent reduction in pulmonary diffusing capacity for carbon monoxide have an altered gut microbiota composition characterized by the reduced abundance of dozens of bacterial taxa and increased levels of several taxa involving Veillonella.142 Therefore, the gut microbiome should serve as a promising research focus to elucidate the mechanisms of long COVID among multiple systems beyond the digestive system.
Vascular and organ impairment
Despite initial recognition as a disease of the respiratory system, COVID-19 is capable of inducing multiple systemic and organic lesions. Damage to the circulatory system includes endothelial dysfunction, subsequent bleeding and thrombogenesis among long COVID patients. The level of arterial stiffening in the aorta, carotid artery, and brachial artery in COVID-19 patients was shown to be notably superior to that in the control group,143 indicating that the impairment of great vessels is a universal phenomenon in COVID-19. In regard to microcapillaries, participants with long COVID presented persistent microclots that were resistant to fibrinolysis,144 which exert a crucial role in blocking microcirculation. In addition, persistent capillary rarefication was found in patients at 18 months following SARS-CoV-2 infection,25 emphasizing the impaired microcirculation in individuals with long COVID. Vascular impairment at different sites might result in diverse manifestations. Neurovascular damage and endothelial cell activation, accompanied by subsequent platelet aggregation and microthrombi, have been reported in COVID-19 patients,145 which possibly causes sustained neuropsychiatric symptoms. With respect to the cardiovascular system, microthrombi are the major reason for myocardial damage in COVID patients.114 Furthermore, the risk of lung embolism, deep venous thromboembolism, and bleeding was still dramatically elevated after a long infection period compared to a control period,146 highlighting the role of vascular impairment in multisystem damage.
Recent evidence has focused on the multiorgan impairment of long COVID. Compared to controls, German patients who recovered from mild/moderate COVID-19 illness have been observed to have a higher risk of long-term sequelae, which includes multiorgan damage associated with renal, thrombotic, cardiac, and pulmonary functions.147 Furthermore, an observational cohort study noted that 70% of individuals with long COVID exhibited evidence of damage to at least one organ.148 Of them, the lungs (11%), heart (26%), kidneys (4%), pancreas (40%), liver (28%), and spleen (4%) suffered from mild impairment, with 29% of patients presenting with multiorgan damage.148 For certain organic impairments, the symptoms may be specific. Elevation of aminotransferases serves as the representative symptom of long COVID patients with liver impairment, which is perhaps caused by viral infection of the liver and supported by pathological manifestations.149 Analogously, SARS-CoV-2 has been observed to potentially have a direct impact on the pancreas by binding to ACE2 receptors and causing pancreatitis, diabetes, and pancreatic exocrine dysfunction.150–152 For kidney impairment, a study of 478 follow-up patients reported a reduced estimated glomerular filtration rate in 29.7% of patients who had no manifestations of acute kidney injury.153 However, the correlation between long COVID and chronic kidney disease is still obscure.154
Reproductive system
Although studies exploring the potential correlation between long COVID and reproductive manifestations are relatively insufficient, reproductive symptoms have been frequently reported in individuals experiencing the post-acute syndrome of COVID-19. Menstrual alterations are the leading morbidity of reproductive symptoms in women with COVID-19. In a study involving 1031 women, 53% of participants experienced worse premenstrual symptoms, 18% had new onset of menorrhagia, and 30% had new dysmenorrhea after the COVID-19 pandemic.155 In the CoVHORT study, approximately 16% of COVID-19 participants had alterations in their menstrual cycle, which encompassed irregular menstruation, infrequent menstruation, and heightened premenstrual symptoms, persisting for a prolonged period.156 In addition, ovarian impairment, including reproductive endocrine disorder and decreased ovary reserve, was observed in COVID-19 patients.157 Mechanistically, follicular fluid from women who had previously been infected with SARS-CoV-2 exhibited decreased levels of IL-1β and vascular endothelial growth factor (VEGF), which subsequently influenced the expression of estrogen receptor β and the migration of endothelial cells,158 perhaps contributing to ovarian dysfunction. Nonetheless, another observational study held an inverse outcome that the function of the ovary was not adversely affected following SARS-CoV-2 infection, and the menstrual alterations might be attributed to inflammation or psychological factors.159 Thus, in-depth investigation with a larger sample size on the relationship between long COVID and ovarian impairment is necessary.
Regarding the male reproductive system, recent studies have exhibited the impairment of spermatogenic function and sperm quality in patients with COVID-19, which was potentially led by direct SARS-CoV-2 attack or immune activation.160,161 A large retrospective study compared the risk of many manifestations of long COVID in 486,149 cases who experienced the SARS-CoV-2 infection with 1,944,580 participants without evidence of infection and indicated that the morbidity of reproductive symptoms such as ejaculation difficulty and reduced libido was increased in COVID-19 patients.162 As another typical reproductive manifestation, erectile dysfunction was likewise documented in patients experiencing COVID-19.163 To elucidate its biological mechanism, transmission electron microscopy was conducted on penile tissue and revealed that persistent viral particles of SARS-CoV-2 were found to remain in the vascular endothelial cells of the penis, potentially playing a role in the development of erectile dysfunction.163
It is worth noting that patients with well-documented ME/CFS commonly have several reproductive manifestations, including menstrual cycle fluctuations, polycystic ovary syndrome (PCOS), and hyperprolactinemia.164–166 Because over 50% of patients with long COVID have the classic symptoms of ME/CFS,96 some of them probably also have reproductive comorbidities. Therefore, future studies should lay emphasis on the comorbidity with reproductive manifestations and ME/CFS in long COVID patients to better elucidate its pathophysiology.
Musculoskeletal system
The musculoskeletal manifestations of long COVID, including musculoskeletal pain, sarcopenia and decreased skeletal muscle mass, have recently attracted much attention.130,167–171 The Linköping COVID-19 Study reported that 28.5% of individuals had weakness in the extremities, and 10.5% of individuals had muscle weakness among patients with long COVID symptoms.172 In addition, another study indicated that approximately 18.59% and 15.09% of survivors developed joint pain and myalgia at 6 months following hospitalization, respectively.173 In spite of the relatively low morbidity, these symptoms are classified into one of four major subphenotypes (nervous and musculoskeletal system manifestations) of long COVID and supported as core symptoms by 92% of patients with long COVID and their family members/caregivers,169,174 which signifies that delving deeply into their pathophysiological mechanisms might assist in the precise management of long COVID.
Similar to other systems, the direct attack of SARS-CoV-2 is considered a significant contributing factor to musculoskeletal system disorders. Multiple cellular types in skeletal muscle tissue, such as pericytes and smooth muscle cells, have been validated to express AEC2 and TMPRSS2 via analysis of transcriptional data,175 which indicates that SARS-CoV-2 has the potential to directly invade these cells, leading to detrimental effects on the musculoskeletal system. However, the autopsy studies found that the load of SARS-CoV-2 was low or even negative in tissue samples of COVID-19 patients who exhibited obvious musculoskeletal symptoms,176–178 demonstrating that the directly viral attack is difficult to comprehensively elucidate the musculoskeletal manifestations of long COVID. Moreover, inflammation and microvascular injury are also hypothesized to be crucial pathophysiological mechanisms. Systemic inflammation, characterized by persistently elevated levels of cytokines, including IFN-γ, TNF-α, IL-6, and IL-10, has been observed in numerous COVID-19 patients and could persist for over 6 months following SARS-CoV-2 infection.179,180 In this way, inflammatory cytokines potentially trigger abnormal catabolic pathways and result in muscle wasting.181 Interestingly, the studies of muscle biopsy showed that musculoskeletal injury ought to be the secondary outcome of microvascular damage, and substantial persistent circulating microclots with inflammatory molecules were profiled in patients with long COVID.144,178 Hence, the synergistic effect between inflammation and vascular injury could be an important element for maintaining musculoskeletal injury. Notably, other than catabolic pathways, inflammatory cytokines also promote the sensitization of the nervous system, offering a novel perspective for understanding the musculoskeletal symptoms of long COVID.182
Increasing evidence has pointed out the importance of hypoxia in skeletal muscle alterations.167 For patients with hypoxia, metabolic alterations and muscle wasting are common characteristics.167 Some patients with acute respiratory distress syndrome (ARDS) have been reported to develop skeletal muscle weakness and were unable to fully recover even after a 5-year follow-up after discharge.183 Intriguingly, a similar finding has been observed in hospitalized COVID-19 patients, especially those assigned to the ICU,184,185 which might be interpreted as hypoxia being widespread in patients with severe COVID-19 and probably facilitating skeletal muscle weakness. In mechanism, the hypoxia-induced factor (HIF) and related regulatory factors that stimulate hypoxia can delay muscle regeneration and cause the loss of skeletal muscle.186 Nevertheless, further elucidation is required to understand the underlying mechanisms of hypoxia in long COVID. Apart from the mechanisms above, several other factors, such as muscle disuse, malnutrition and medication, might also contribute to the reduced muscle mass and should be considered to explain the musculoskeletal manifestations of long COVID.
Immune system
While the complete understanding of the immunobiology of long COVID remains elusive, the possible mechanisms in multiple systems have underscored its importance. The dominant hypotheses include persistent SARS-CoV-2 and corresponding antigens and/or nucleic acids involved in the inflammatory response, persistent autoantibodies triggering autoimmunity during the post-acute stage, and an imbalance in the microbiome and immune microenvironment.60,136,187–189 Several studies have confirmed the presence of SARS-CoV-2 RNAs and proteins in the cardiovascular system, brain, lung tissue, plasma, and urine for a long time after initial infection,60,117–119 which probably results in chronic inflammation and multiple systemic manifestations. In a study of 37 long COVID participants, the circulating spike emerged in more than 70% of patients with ongoing cardiovascular, gastrointestinal, neuropsychiatric, systemic, and musculoskeletal symptoms,136 supporting the explanation that a reservoir of active SARS-CoV-2 or its components persists in COVID-19 patients. Nonetheless, the limitation of sample size makes it difficult to ensure reliability, and future research with larger sample sizes is necessitated to be conducted.
Autoimmunity plays a vital role in the development of long COVID. Multiple recent studies have documented the upregulation of autoantibodies such as antibodies to ACE2, anti-nuclear autoantibodies, and immunomodulatory factors (including complement components, chemokines, cytokines, and cell-surface proteins) in patients with persistent symptoms following SARS-CoV-2 infection.120,121,190–192 An observational study indicated that the upregulation of IgG antibodies against ACE2 was found in 1.5% of patients with COVID-19,191 implying the widespread existence of autoantibodies to ACE2. However, the duration of increased levels of anti-ACE2 antibodies and their relationship with long COVID still require further elucidation. In terms of anti-nuclear autoantibodies, the expression of anti-nuclear/extractable-nuclear antibodies (ANAs/ENAs) was higher in COVID-19 patients at 6 months after recovery than in healthy participants or patients with other respiratory infections, and persistent positive titers were relatively associated with the severity of clinical manifestations,192 implying that anti-ANA/ENA antibodies could facilitate long COVID. Furthermore, the elevated level of specific autoantibodies against immunomodulatory factors has been reported to contribute to particular immune-cell population depletion and worse clinical outcomes,121 and multiomics data analysis of 309 COVID-19 patients revealed cross-correlations between neutralizing antibodies against SARS-CoV-2 and autoantibodies.120 For instance, there was a negative correlation between the expression of anti-nuclear and anti-IFN-α2 autoantibodies and the levels of anti-SARS-CoV-2 IgG,120 suggesting a potential interconnection between these factors and the development of long COVID. Intriguingly, several autoantibodies have been found to be correlated with disorders of specific organs. For instance, long COVID patients with neurological manifestations show a higher level of nucleocapsid protein IgG against SARS-CoV-2, while some other autoantibodies have been associated with sputum production and gastrointestinal symptoms,120 manifesting their potential as diagnostic biomarkers.
The dynamics in the immune microenvironment could also be associated with long COVID.193 For patients who go on to develop long COVID, TNF-α and IFN-γ-induced protein 10 are significantly elevated during early recovery (<90 days), while IL-6 is upregulated among patients with long COVID,194 demonstrating that persistent immune activation potentially leads to long COVID and could be utilized to develop novel remedies. An in-depth study indicated that long COVID patients had a typical immune microenvironment featuring activated innate immunocytes, poor abundance of naïve lymphocytes (T and B cells), and overexpression of IFN-β and IFN-λ1 at 8 months following infection.195 Furthermore, the patterns of plasma-cell-related expression and monocyte alterations at the acute stage of COVID-19 were also correlated with persistent symptoms,196,197 providing early insights into the etiologies and pathophysiology of long COVID. However, there remain numerous unknown fields concerning the immune microenvironment of long COVID, and further investigation may shed light on its prevention and treatment.
Psychological disorders and long COVID
Although most studies on long COVID are predominantly concerned with somatic manifestations and enrich the understanding of its pathophysiology to a certain extent,7,42,60 the effect of psychological and psychosomatic factors has been almost neglected. In fact, psychological disorders may affect a substantial proportion of those who develop long COVID.198–205 A previous study reported that both COVID-19 patients and control individuals develop clinical manifestations consistent with PASC.198 Despite the relatively superior morbidity among COVID-19 patients, no evidence of autoimmunity, abnormal immune activity or persistent infection was found in the entire study population.198 Hence, the underlying contributing factors rather than the somatic factors mentioned above deserve to be underlined. Significantly, individuals with perceived fatigue in the long COVID group did not exhibit any additional objective fatigability compared to those without long COVID symptoms,199 signifying that mental factors probably serve as critical modifiers or even causes of long COVID. Analogously, another study showed that 64% of patients after mild COVID-19 with persistent neurological symptoms met the criteria of somatic symptom disorder (SSD),200 and psychiatric conditions were confirmed to contribute to the prolonged duration of COVID-19 symptoms,206 which suggests that psychosomatic disorders should be emphasized when investigating the mechanisms of long COVID. Consequently, the identification of psychological or psychosomatic disorders is encouraged to assist in multidisciplinary care and better cure long COVID.201,207
With the accumulation of clinical evidence, the mechanisms of psychological/psychosomatic disorders in long COVID have also been highlighted. Psychiatric consequences have been proven to affect the immune system via multiple pathways, such as the hypothalamic-pituitary adrenal (HPA) axis and microglial activation, which subsequently might delay the recovery of COVID-19.208,209 In addition, somatic symptoms have been verified to lead to worse mental health and poor quality of life, while mental disorders could aggravate the physical symptoms of long COVID patients in turn.134,210 Under these circumstances, the positive feedback loop between somatic symptoms and psychological disorders probably exacerbates both mental and physical manifestations, which further facilitates long COVID.134 However, although the importance of psychological disorders has been underlined, the mechanisms are still unclear. There are several reasons why psychological disorders in long COVID have not yet been well studied. First, it is difficult for clinicians to investigate the underlying pathology by ascribing psychological disorders.211 Second, the explanations of physical symptoms from the perspective of psychology are usually considered a stigma for patients.212 Third, the roles of psychosomatic medicine in other diseases have not yet been clarified,213 making it more difficult to elucidate the progression of long COVID. Therefore, thoroughly illustrating the psychological mechanisms of long COVID remains an enormous challenge. Notably, a cross-sectional analysis of 26,823 participants suggested that self-reported SARS-CoV-2 infection was correlated with the presence of long COVID symptoms, while seropositivity was merely associated with anosmia instead of other physical symptoms.202 Thus, it is speculated that persistent somatic symptoms may be related more to self-reported infection than to laboratory-confirmed SARS-CoV-2 infection. Consequently, misdiagnosis might occur, and patients with a diagnosis of long COVID are prone to experiencing multilayered stigmas, further exacerbating their mental symptoms.214 Therefore, a careful evaluation is indispensable to prevent the manifestations caused by psychological disorders being incorrectly ascribed to PASC or long COVID.
Despite the huge challenge of elucidating its psychological mechanisms, it is assured that psychological and psychosomatic factors exert an indispensable role in the progression of long COVID manifestations, and adopting multidisciplinary therapeutic strategies, including psychotherapy, is potentially beneficial for persistent symptoms.
Management of long COVID
Diagnostic tools for long COVID
For early detection of long COVID, routine auxiliary inspections such as medical imaging techniques and laboratory examinations are currently indispensable. Among them, echocardiography, cardiac biomarkers and MRI are utilized to assess cardiac injury and arrhythmia,215 and chest imaging examination and pulmonary function tests are adopted for evaluating lung damage and the degree of dyspnea.216 However, for certain neuropsychiatric manifestations, such as fatigue and cognitive impairment, the evidence is mainly based on self-report of patients rather than objective tests.26,217 Although (18)F-FDG PET has a satisfactory performance in predicting hyposmia, cognitive impairment, and insomnia via the identification of bilateral hypometabolism of the bilateral rectal or orbital gyrus in previous research,218 no apparent change in glucose metabolism of the brain has been observed in another study.219 Therefore, it is necessary to develop more accurate laboratory tests to enhance the sensitivity and specificity for predicting long COVID.
In addition to traditional examination methods, the microbiome has recently been reported to be associated with long COVID.104,220–222 Early research into the gut microbiome suggested that opportunistic gut pathogens were correlated with persistent respiratory manifestations. The common nosocomial pathogens, including Actinomyces naeslundii and Clostridium innocuum, were related to fatigue and neuropsychiatric symptoms (p < 0.05).22 Simultaneously, multikingdom microbiota identified by metagenomic-based clustering exhibit potential utility in long COVID prediction.141 Moreover, the alteration of tens of bacterial taxa, including Veillonella, has been validated to be related to fibrosis and could be utilized to diagnose the long-term pulmonary manifestations of long COVID.142 In a similar manner, the abundance of certain oral microbiota, including members of the Veillonella and genera Prevotella, is significantly increased in long COVID patients, which exhibits the potential for predicting persistent symptoms after SARS-CoV-2 infection.222 The available evidence indicates that the composition of the microbiome can be potentially used to predict the occurrence of long COVID, even specific symptoms.
Liquid biopsy research into the clinical manifestations of long COVID has shown satisfactory prognostic and diagnostic potential.223–232 For example, kynurenine has been validated to be upregulated in the serum and saliva of long COVID-19 patients over 20 weeks,223 and vascular transformation biomarkers, including P-SEL and ANG-1, have excellent specificity and sensitivity for long COVID and may serve as promising biomarkers for long COVID diagnosis and monitoring.228 In addition, several biomarkers have the capacity to predict neuropsychiatric manifestations that are difficult to detect in traditional inspection. Neurofilament light chain, glial fibrillary acidic protein, SARS-CoV-2 nucleocapsid antigen, and immune-inflammation indicators in plasma have been verified to be correlated with persistent depression/anxiety and cognitive impairment.225,227 The neurofilament light and 14-3-3 protein from cerebrospinal fluid were significantly related to neurologic disability at 18 months after neurologic symptom onset.224 Remarkably, extracellular vesicles derived from neurocytes contain the crucial components particularly relevant to occult neural damage and indicate the capacity for monitoring the neuropsychiatric manifestations of long COVID.229,231
The relevance of noncoding RNAs to many human diseases, such as malignant tumors, cardiovascular disorders, and infectious diseases, including COVID-19, has been well studied.233,234 In a pilot study, miR-29a-3p, miR-155-5p and miR-146a-3p exhibited excellent performance in COVID-19 diagnosis, and miR-29a-3p and miR-146a-3p could be utilized to distinguish the post-acute phase of SARS-CoV-2 infection from the acute phase.235 Hence, noncoding RNAs are also hypothesized to possess the potential to detect and monitor long COVID.
Although the diagnostic performance of liquid biopsy for long COVID has been observed, most of the evidence is based on preliminary studies with limited sample sizes. Therefore, the importance of exploring biomarkers suitable for clinical practice cannot be overemphasized.
Remedies for long COVID
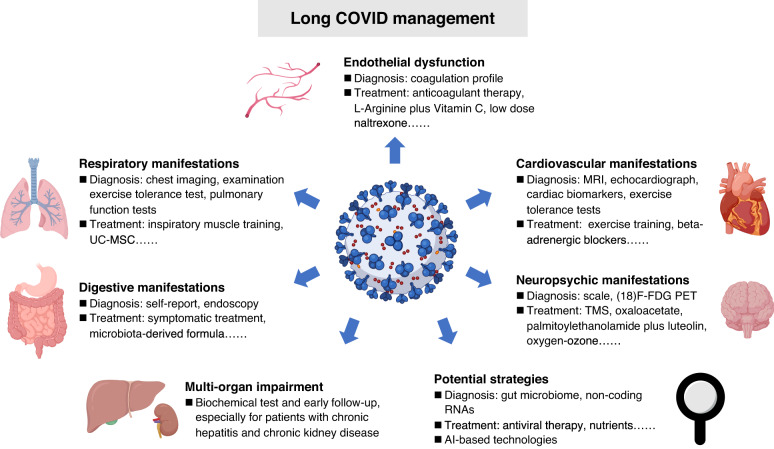
To help clinicians better manage long COVID manifestations, the National Institute for Health and Care Excellence (NICE) of England developed guidelines on the care of patients with persistent effects of COVID-19.9,236 Although there is no documented evidence regarding effective remedies for patients with long COVID, abundant therapeutic regimens based on previous experiences for certain symptoms and pilot studies have been proposed as the means to effectively address the post-acute symptoms of COVID-199,237 (Table 1) (Fig. 4).
Table 1.
Major candidate treatments for long COVID
| Manifestations | Treatment options | Supporting evidence | references |
|---|---|---|---|
| Respiratory symptoms | Self-management including stopping smoking and regular exercise | COPD and long COVID literatures | 239,240 |
| Inspiratory muscle training | Long COVID RCT | 241 | |
| Music-based approaches | Long COVID RCT | 242 | |
| UC-MSC treatment | COVID-19 RCT | 243 | |
| Cardiovascular symptoms | β-adrenergic blockers | Heart disease literature | 245 |
| POTS |
Non-pharmacological interventions: health education and exercise training Pharmacological treatments: β-blockers and vasoactive agents |
POTS literature | 246 |
| Chronic fatigue | Self-management | NICE guideline for long COVID | 236 |
| ME/CFS | Energy management, personalized exercise or physical activity, personalized sleep management, and dietary management | ME/CFS literature | 247 |
| Anhydrous enol-oxaloacetate | Long COVID pilot study | 248 | |
| Hyperbaric oxygen therapy | Long COVID pilot study | 249 | |
| Oxygen-ozone autohemotherapy | Long COVID pilot study | 250 | |
| Digestive symptoms | SIM01 (a microbiota-derived formula) | COVID-19 pilot study | 252 |
| Endothelial dysfunction | L-Arginine plus Vitamin C | Long COVID pilot study | 253,254 |
| Low dose naltrexone | COVID-19 pilot study | 255 | |
| MASC | H1 and H2 antihistamines | MASC literature | 256 |
| Olfactory disorders | Nasal irrigation (including ambroxol, betamethasone, and rinazine) | Long COVID pilot study | 258 |
| Memory and olfactory dysfunction | Palmitoylethanolamide plus luteolin | Long COVID pilot study | 259 |
| Viral persistence | Nirmatrelvir | Long COVID pilot study | 265 |
| Long COVID | Nutrients treatment | Long COVID pilot study | 263,264 |
COPD chronic obstructive pulmonary disease, MCAS mast cell activation syndrome, ME/CFS myalgic encephalomyelitis/chronic fatigue syndrome, NICE National Institute for Health and Care Excellence, POTS postural orthostatic tachycardia syndrome, RCT randomized controlled trial, UC-MSC umbilical cord-derived mesenchymal stem cell
Fig. 4.
Multidisciplinary management of long COVID. Multidisciplinary management including diagnostic tools and treatment options based on previous experience and pilot studies is essential for recovery of long COVID patients. AI artificial intelligence, MRI magnetic resonance imaging, TMS transcranial magnetic stimulation, UC-MSC umbilical cord-derived mesenchymal stem cell
Respiratory symptoms are frequently reported among individuals with long COVID, which mainly manifest as persistent dyspnea and cough.26 The exercise tolerance test and chest radiograph are recommended in the NICE and ESCMID guidelines to assist in illness evaluation and management.9,236,238 To better control pulmonary manifestations, multidisciplinary approaches should be applied. The recommendations for dyspnea suggest that self-management, including avoiding pollutants, stopping smoking, and regular exercise, could relieve exacerbated dyspnea.42,239,240 For long COVID patients, previous studies showed that inspiratory muscle training and music-based breathing training elicited clinical improvements in chest symptoms and difficult breathing,241,242 which should be recommended for COVID-19 patients. Additional therapeutic regimens proposed for managing the respiratory symptoms of long COVID based on pilot studies also facilitate symptomatic relief. Human umbilical cord-derived mesenchymal stem cell (UC-MSC) administration for patients with COVID-19 has revealed an excellent outcome in symptoms and lung lesion improvement at 1 year after infection compared to a control group.243 Furthermore, the COVID-Rehab study proposed a cardiopulmonary rehabilitation program to treat individuals with long COVID.244
For cardiovascular symptoms, the treatment options for other cardiovascular disorders/syndromes can be used for reference in long COVID. In accordance with the NICE guideline, exercise tolerance tests should be applied routinely for heart function measurement.42,236 β-adrenergic blockers have been amply validated to benefit patients with cardiac arrhythmias, acute coronary syndromes, and angina42,245; thus, it could be implied that β-adrenergic blockers might possess potential efficacy in the treatment of cardiovascular symptoms associated with long COVID. As a special type of cardiovascular symptom, POTS featured as orthostatic intolerance and the excessive increase of heart rate while standing is commonly reported in long COVID.26,246 The treatment of POTS mainly consists of nonpharmacological interventions such as health education and exercise training as well as pharmacological treatments including β-blockers and vasoactive agents.246 Therefore, rational usage of these approaches is perhaps beneficial for long COVID patients. However, few studies have explored the therapeutic effects of these interventions in long COVID.
Chronic fatigue holds the dominant place in morbidity of long COVID, which even accounts for 80% of patients with long COVID.26 Because of the lack of specific treatment, the NICE guideline initially recommended self-management for relieving fatigue.236 Nevertheless, patients with long COVID fatigue are commonly comorbid with ME/CFS; thus, active therapeutic strategies are necessary. Multidisciplinary strategies have also been proposed to manage ME/CFS in current guidelines, which mainly involve energy management, personalized exercise or physical activity, personalized sleep management, and dietary management.247 Hence, these strategies are likely to be effective for managing the ME/CFS symptoms of long COVID. Nevertheless, it should be noted that ME/CFS manifestations cannot currently be cured, and the strategies mentioned merely control symptoms.247 Furthermore, many studies have investigated certain remedies in long COVID patients. A clinical trial evaluated the therapeutic effect of anhydrous enol-oxaloacetate and found that it significantly reduced the fatigue of ME/CFS in long COVID patients.248 However, the data for the control group is from a historical trial and meta-analysis, and further study of oxaloacetate with a rigorous design is warranted. In addition, oxygen-ozone autohemotherapy has exerted the ability to alleviate fatigue and pain in at least 67% of COVID patients, and hyperbaric oxygen therapy with 10 sessions yielded a substantial improvement in fatigue, cognition, executive function, attention, verbal function, and information processing.249,250 In general, these remedies documented in pilot studies demonstrate a favorable effect on ME/CFS of long-COVID and deserve in-depth study.
Moreover, multiple additional interventions have been applied to tackle the gastrointestinal, circulatory, neurologic, musculoskeletal and even multiorgan manifestations of long COVID. As a research hotspot of the digestive system, the gut microbiome has long been considered a potential direction for the treatment of gastrointestinal diseases. A previous study proved that 5-hydroxytryptamine signaling mediated by gut microbiome dysregulation probably contributed to the gastrointestinal manifestations of long COVID.251 Thus, certain agents targeting the gut microbiome may alleviate post-COVID manifestations. In this manner, SIM01, a microbiota-derived formula including xylooligosaccharide, galactooligosaccharides, resistant dextrin, and Bifidobacteria strains, relieved the gut dysbiosis and symptoms of COVID-19 patients,252 further validating the effect of the gut microbiome on treating digestive manifestations. Endothelial dysfunction and persistent plasma microclots have been found in the circulatory system, which potentially lead to damage to multiple organs, including the brain, lung, and heart.144,253 Therefore, active anticoagulant therapy is essential for COVID-19 patients in a hypercoagulable state to reduce the risk of thrombogenesis. For oxidation reduction and endothelial function improvement, the administration of L-arginine plus vitamin C for COVID-19 patients was applied in the LINCOLN study and significantly reduced the incidence of long COVID symptoms such as asthenia, dyspnea, chest tightness, dizziness, headache, and concentration difficulty.253,254 In the meanwhile, low-dose naltrexone exhibited a promising effect on reducing the incidence of thrombotic complications.255 Interestingly, naltrexone has also been mentioned in the treatment of ME/CFS.60 The evidence above demonstrates the potential of naltrexone for long COVID treatment. H1 and H2 antihistamines are commonly recommended for mast cell activation syndrome to mitigate the symptoms, but cognitive decline caused by H1 blockers should be noted.256 Various strategies have been proposed for the treatment of neuropsychiatric manifestations. For instance, obvious improvement in fatigue, cognitive function, and depressive symptoms has been observed after transcranial magnetic stimulation (TMS) in long COVID patients.257 With regard to persistent olfactory disorders, a recent study indicated that the combination of nasal irrigation (with ambroxol, betamethasone, and rinazine) and systemic prednisone represented an excellent curative effect to improve dysosmia in long COVID patients,258 and palmitoylethanolamide plus luteolin also ameliorated neuropsychiatric manifestations, including memory and olfactory dysfunction.259 For musculoskeletal pain, regular exercise was suggested to reduce pain and improve physical function.260 It is remarkable that these physical manifestations are perhaps aggravated by psychological symptoms; thus, psychotherapy interwoven with therapy of somatic consequences is of utmost importance to long COVID treatment.261,262
In addition to the L-arginine plus vitamin C mentioned above, nutrients, TGF-β inhibitors, and antiviral therapies exhibit a potential effect on alleviating multisystem or multiorgan symptoms.254,263–266 The proper intake of nutrients is strongly recommended to maintain metabolism and overcome disease during the COVID-19 pandemic.264 Among nutrients, Morinda citrifolia and fermented Carica papaya are hypothesized to diminish the manifestations of long COVID via redox balancing, pro-energy, and immune-modulating mechanisms.263 Regrettably, clinical outcomes are still lacking, so research concerning these nutrients in long COVID therapy is warranted. On account of persistent SARS-CoV-2 in multiple organs,42,60 antiviral therapies perhaps exert promising effects on long COVID symptom relief. With respect to antiviral agents, nirmatrelvir dramatically mitigates the progression of COVID-19 without additional safety concerns.267 Furthermore, patients administered nirmatrelvir presented a 26% reduction in morbidity associated with long COVID symptoms of fatigue, heart disease, blood clots, dyspnea, and cognitive impairment.265 Thus, nirmatrelvir should be routinely recommended to COVID-19 patients. TGF-β inhibitors, modulators of immunity and fibrosis, have also demonstrated favorable potential in attenuating long-term COVID symptoms.266 Nevertheless, their curative effects need further validation.
Overall, current studies have presented a diverse array of therapeutic options for combating long COVID. Nevertheless, the majority of them are based on previous experience in similar diseases and pilot studies with crude designs. Although hundreds of clinical trials have been registered (Table 2), few of them have been widely used in clinical practice. Accordingly, there is an urgent need for well-designed trials with large sample sizes to investigate the potential impact of updated therapeutic regimens, including nutrients, antiviral agents, and anticoagulants, on addressing the challenges of long COVID.
Table 2.
Representative clinical trials for treatment of long COVID
| Therapeutic regimens | NCT identifier | Indications | Phase | Developer |
|---|---|---|---|---|
| Nirmatrelvir-Ritonavir | Multiple symptoms | II | Harlan M Krumholz, Stanford University, Pfizer | |
| Lithium | NCT05618587 | Fatigue and brain fog | II | State University of New York at Buffalo |
| Sodium pyruvate nasal spray | NCT04871815 | Multiple symptoms | II, III | Cellular Sciences, etc. |
| Mitoquinone | NCT05373043 | Vascular endothelial dysfunction | NA | VA Office of Research and Development |
| Imatinib-Infliximab | NCT05220280 | Multiple symptoms | IV | Clinical Urology and Epidemiology Working Group, etc. |
| TNX-102 SL | NCT05472090 | Pain | II | Tonix Pharmaceuticals |
| Remdesivir | NCT04978259 | Multiple symptoms | IV | Clinical Urology and Epidemiology Working Group, etc. |
| Nicotinamide adenine dinucleotide plus naltrexone | NCT04604704 | Fatigue | II | AgelessRx |
| UC-MSC-derived exosomes | NCT05808400 | Chronic cough | I | Huazhong University of Science and Technology, etc. |
| Acupuncture | NCT05212688 | Fatigue | II | Royal Marsden NHS Foundation Trust |
| Sirolimus | NCT04948203 | Pulmonary fibrosis | II, III | University of Chicago |
| Prospekta | NCT05074888 | Fatigue | III | Materia Medica Holding |
| Ivabradine | NCT05481177 | POTS | IV | Uniformed Services University of the Health Sciences |
| Temelimab | NCT05497089 | Neuropsychiatric symptoms | II | GeNeuro SA |
| Metoprolol Succinate | NCT05096884 | Tachycardia, Dyspnea | I | Hackensack Meridian Health |
| Vortioxetine | NCT05047952 | Cognitive impairment | II | Brain and Cognition Discovery Foundation |
| Mind body syndrome therapy | NCT04854772 | Somatic symptoms | NA | Beth Israel Deaconess Medical Center |
| Microbiome immunity formula | NCT04950803 | Multiple symptoms | NA | Chinese University of Hong Kong |
NA not applicable, POTS postural orthostatic tachycardia syndrome, UC-MSC umbilical cord-derived mesenchymal stem cell
Artificial intelligence (AI) in long COVID management
In the past few decades, AI technologies have developed rapidly and paved the way for precise diagnosis and clinical decision-making for multiple diseases, including malignant tumors, respiratory diseases, and pediatric diseases, on the basis of medical image and electronic health record (EHR) data.268–270 In the field of COVID-19, state-of-the-art AI models have also been applied for rapid diagnosis and severe illness prediction.271,272 The above studies demonstrate that AI has the ability to tackle complex clinical tasks and empower personalized medicine.
In spite of the relatively young discipline, cutting-edge AI technologies have been utilized in the management of patients with long COVID. On the one hand, AI technologies enable the accurate identification of long COVID. Liquid biopsy is deemed a potent tool for disease diagnosis and monitoring. A recent study conducted a high-definition single-cell assay to compare long COVID patients with normal donors and identified specific cellular/acellular events of long COVID.273 Using these events, a machine learning classifier was developed to separate long COVID patients from healthy controls, with an accuracy over 90%.273 Apart from blood examination, constructing models based on EHR data could also enable accurate diagnosis.109,274,275 The XGBoost models trained with diagnostic information, health-care utilization, demographics, and medications attained areas under the curve (AUCs) of 0.92 (whole patients), 0.85 (non-hospitalized individuals), and 0.90 (hospitalized individuals) for long COVID identification.275 Interestingly, the symptoms in the acute period after SARS-CoV-2 infection were verified to be related to long COVID,109,276 and a random forest model created using the manifestations at 7 days plus personal characteristics and comorbidities had the capacity to predict individuals with persistent symptoms,109 which offers a powerful tool for the early identification of individuals with a high risk of long COVID. Moreover, a multiclass machine-learning model based on fecal metagenomic data was also reported to hold promising potential in diagnosing PACS.221
On the other hand, AI technologies have been utilized for the stratification of long COVID patients. Researchers have recently proposed an unsupervised machine learning model for semantic phenotypic clustering utilizing EHR data that divides long COVID patients into 6 subtypes, including multisystem symptoms plus laboratory abnormalities (Cluster 1), pulmonary disorders (Cluster 2), neuropsychiatric manifestations (Cluster 3), cardiovascular manifestations (Cluster 4), pain/fatigue (Cluster 5), and multisystem-pain symptoms (Cluster 6).277 Consequently, this method enables the rational allocation of clinical resources and precision clinical management. Nevertheless, another study based on machine learning analysis suggested that long COVID patients should be classified into 4 subphenotypes consisting of renal and cardiac phenotype; respiratory, anxiety and sleep phenotype; musculoskeletal and nervous phenotype; and respiratory and digestive phenotype.169 These differences may be derived from the data bias, selection of cluster number, and variety of machine learning models. Thus, a large sample set from multiple centers is essential for precise subdivision of long COVID phenotypes. Moreover, the instruments for measuring the symptom burden of long COVID individuals have also exhibited the capacity for assessing the effect of interventions and enable precise clinical management.278–280 However, they are presented in the form of questionnaires, and AI-based patterns should be constructed.
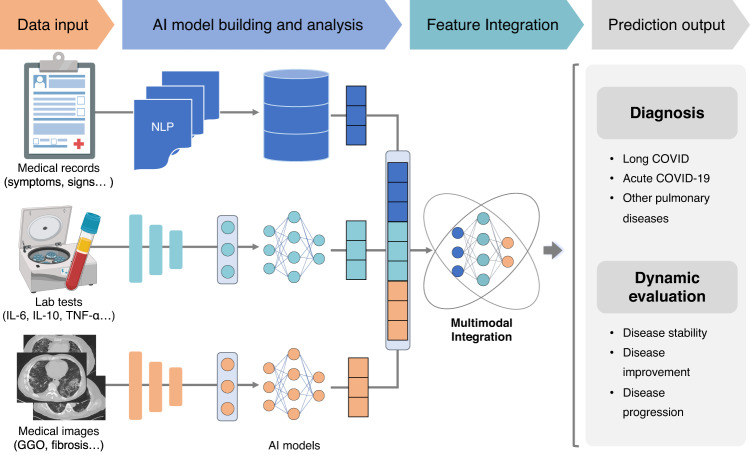
As an essential instrument for the diagnosis and prognosis evaluation of pulmonary diseases, CT examination also exhibits the potential for long COVID assessment.281–286 The CT abnormalities among patients with persistent manifestations following acute COVID-19 manifest as subpleural bands and ground-glass opacity (GGO) at 3 months after infection as well as fibrosis without obvious GGOs at 6 months after infection.283,285 Even worse, fibrotic changes could persist for 1 year in some individuals.281 Thus, the early identification and dynamic evaluation of CT abnormalities is of paramount importance. Although qualitative CT approaches have been applied for assessment of the sequential change in long-term pulmonary manifestations of long COVID, they mostly rely on manual assessment.282,284,287 Therefore, establishing AI-based models to automatically assess the CT images of long COVID patients is extremely meaningful to improve the efficiency of doctors. Moreover, the current AI models for long COVID management are concentrated on single modality, which inevitably diminishes the synergistic effect among multiple clinical modalities. Indeed, multimodal integration (MMI) via AI has been substantiated to enhance the robustness and accuracy of models,288–290 lighting the path to clinical practice of AI production. Hence, further studies harnessing MMI technologies to integrate EHR, laboratory examination, and medical images may enable the individualized management of patients with long COVID (Fig. 5).
Fig. 5.
The workflow of multimodal integration (MMI) for precise management of long COVID. MMI systems could identify associations among multimodal data and output the outcomes including diagnosis and dynamic evaluation of patients to empower the precise management. AI artificial intelligence, GGO ground-glass opacity, NLP natural language processing
Conclusions and future directions
The ongoing symptoms and post-acute sequelae of patients with SARS-CoV-2 infection have been increasingly brought to the forefront, which could contribute to multi-system manifestations encompassing cardiovascular, respiratory, neuropsychiatric, gastrointestinal, reproductive, and musculoskeletal symptoms. Moreover, advances in diagnosis and remedies for long COVID have been witnessed recently. Nevertheless, many problems left over from the past still require enough attention and urgently need to be addressed.
The first is the accessibility and accuracy of laboratory tests for SARS-CoV-2. The data from a previous study suggested that only 1–3% of patients had laboratory-confirmed COVID-19 in the first wave due to technical limitations.291 For non-hospitalized individuals with mild to moderate symptoms of COVID-19, PCR or antigen testing might not be applied.60 In addition, despite being the gold standard for diagnosis, the omission diagnostic rate of nucleic acid detection is still worth noting. Approximately 38% of cases underwent an omission diagnosis at symptom onset, and the false-negative rate was still 2% on days 22–24.292,293 However, the majority of patients with nonsevere illness recovered from COVID-19 at that time, possibly resulting in missed diagnosis of numerous long COVID patients. In consideration of the accessibility of self-tests, antigen tests have also been recommended. However, only 64% of confirmed COVID-19 individuals experienced seroconversion, implying a considerably high proportion of omission diagnosis via antigen testing of COVID-19.294 The prevalence of nonseroconversion is more remarkable in mild COVID-19 patients and children.295,296 Among the diverse severity spectrum, the antigen levels of 22.2% mild and 2.6% severe patients with COVID-19 could not be profiled even after an 8-month follow-up.295 To improve the detection rate, cases with COVID-19-related manifestations should receive timely and sustained inspection. Since the combination of IgG and IgM showed promising sensitivity of up to 96%,297 the combination of IgG/IgM, antigen and PCR tests can be assumed to be a precise approach for COVID-19 diagnosis. By these means, long COVID may be better monitored.
In addition, a lack of knowledge and health-care education for sequelae of COVID-19 probably impedes personalized management. For instance, ME/CFS and POTS are common long COVID sequelae that have rarely been studied previously. Only 5.6% of US medical schools cover the clinical, curriculum, and research criteria for ME/CFS,298 suggesting that the proportion might be even lower in developing countries. Furthermore, a cross-sectional survey reported that 75% of POTS cases were misdiagnosed due to the complexity of the illness.299 Therefore, health facilities, medical schools, and government agencies should educate research/health workers on these sequelae and pursue the establishment of a dedicated discipline focused on long COVID research and care to enable the precise management of long COVID manifestations. Moreover, as recommended by researchers from Johns Hopkins University, the establishment of COVID-19 clinics equipped with multidisciplinary specialists is also crucial to afford integrated care for long COVID symptoms.300 Nonetheless, multidisciplinary clinics in low-/middle-income countries remain challenging due to limited resource availability and medical professionals.301
Despite the rapid progress in epidemiological understanding, pathophysiological mechanism and management strategies of long COVID, the available evidence is principally based on pilot studies with finite sample sizes and treatment of similar diseases.60,302,303 To address these problems, future research concerning the critical clinical, epidemiological, serological, and pathological characteristics will assist in understanding the pathophysiology of long COVID. Ultimately, it is imperative that a diverse range of long COVID patients of various races and ethnicities should be meaningfully engaged in clinical trials to facilitate the clinical applications of novel interventions.
There are several strengths in this review. First, we comprehensively summarize the epidemiological understanding, impact of vaccinations and variants, multiorgan manifestations and corresponding pathophysiological mechanisms, and multidisciplinary management of long COVID. Second, as abnormal laboratory examination results were not found in many patients and a considerable percentage of patients suffering from long COVID symptoms meet the criteria for SSD,198,200 the correlation between psychological or psychosomatic factors and long COVID manifestations is underlined in this review. Third, the major challenges concerning biological knowledge gaps and efficient remedies that need to be addressed are also proposed to move the research field of long COVID forward. Despite the advantages above, weaknesses still exist. Multiple therapeutic strategies have presented promising effects on alleviating symptoms of long COVID, but most of them might be overly optimistic because the current studies are mainly based on small sample sizes without rigorous scientific validation. In fact, these measures may bear a risk of serious side effects without medical advice. Hence, correct guidance is necessary to prevent patients with long COVID from being misled by social media platforms. Furthermore, among patients infected with the Omicron variant and/or vaccinated, the morbidity associated with long COVID is noticeably lower, and most of them are resolved in several months.43,45 Thus, some findings may currently be overrated. However, as the transmissibility of the Omicron variant increases,48,304 a larger proportion of patients are likely to develop long COVID. Consequently, sufficient attention still needs to be paid to the pathophysiological mechanisms and therapeutic options of long COVID.
Given the multisystemic illness of long COVID, numerous clinical manifestations, including impairment of multiple organs/systems, vascular damage, dysautonomia, and ME/CFS, have been observed in an extensive number of patients. Simultaneously, the foreseeable requirement of health care for sequelae of COVID-19 will continue to grow due to the global pandemic. However, the diagnostic and treatment strategies remain inadequate currently. To address these challenges, a combination of existing laboratory tests, suitable health education, outpatient infrastructure, and clinical trials with rigorous designs are clearly warranted.
Acknowledgements
This study was supported by the Science and Technology Project of Sichuan (2022ZDZX0018, 2020YFG0473, 2023NSFSC1889); Science and Technology Project of Chengdu (2023-YF09-00007-SN); Sichuan University from “0” to “1” Innovation Project. We acknowledged the BioRender.com for the support of figures design.
Author contributions
C.W., W.L. and Y.Y. conceived the manuscript; J.L., Y.Z., J.M., and Q.Z. wrote the initial draft; J.L. and C.W. contributed to the figure preparation and making; J.S., S.L., Y.Y., W.L. and C.W. revised the manuscript. All authors have read and approved the manuscript.
Competing interests
W.L. is one of the Associate Editors of Signal Transduction and Targeted Therapy, but he has not been involved in the process of the manuscript handling. All authors listed declared that there is no conflict of interest.
Footnotes
These authors contributed equally: Jingwei Li, Yun Zhou, Jiechao Ma, Qin Zhang
Contributor Information
Yizhou Yu, Email: yizhouy@acm.org.
Weimin Li, Email: weimi003@scu.edu.cn.
Chengdi Wang, Email: chengdi_wang@scu.edu.cn.
References
- 1.Halperin SA, et al. Final efficacy analysis, interim safety analysis, and immunogenicity of a single dose of recombinant novel coronavirus vaccine (adenovirus type 5 vector) in adults 18 years and older: an international, multicentre, randomised, double-blinded, placebo-controlled phase 3 trial. Lancet. 2022;399:237–248. doi: 10.1016/S0140-6736(21)02753-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li J, Shao J, Wang C, Li W. The epidemiology and therapeutic options for the COVID-19. Precis. Clin. Med. 2020;3:71–84. doi: 10.1093/pcmedi/pbaa017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. WHO coronavirus (COVID-19) dashboard, https://covid19.who.int (2023).
- 4.Wang C, et al. COVID-19 in early 2021: current status and looking forward. Signal Transduct. Target Ther. 2021;6:114. doi: 10.1038/s41392-021-00527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu M, et al. Potential role of ACE2 in coronavirus disease 2019 (COVID-19) prevention and management. J. Transl. Int. Med. 2020;8:9–19. doi: 10.2478/jtim-2020-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen T, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nalbandian A, et al. Post-acute COVID-19 syndrome. Nat. Med. 2021;27:601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah W, Hillman T, Playford ED, Hishmeh L. Managing the long term effects of COVID-19: summary of NICE, SIGN, and RCGP rapid guideline. BMJ. 2021;372:n136. doi: 10.1136/bmj.n136. [DOI] [PubMed] [Google Scholar]
- 9.Venkatesan P. NICE guideline on long COVID. Lancet Respir. Med. 2021;9:129. doi: 10.1016/S2213-2600(21)00031-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greenhalgh T, et al. Long COVID-an update for primary care. BMJ. 2022;378:e072117. doi: 10.1136/bmj-2022-072117. [DOI] [PubMed] [Google Scholar]
- 11.Pan L, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am. J. Gastroenterol. 2020;115:766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raman B, et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine. 2021;31:100683. doi: 10.1016/j.eclinm.2020.100683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naeije R, Caravita S. Phenotyping long COVID. Eur. Respir. J. 2021;58:2101763. doi: 10.1183/13993003.01763-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petersen MS, et al. Long COVID in the Faroe Islands: a longitudinal study among nonhospitalized patients. Clin. Infect. Dis. 2021;73:e4058–e4063. doi: 10.1093/cid/ciaa1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu E, Xie Y, Al-Aly Z. Risks and burdens of incident dyslipidaemia in long COVID: a cohort study. Lancet Diabetes Endocrinol. 2023;11:120–128. doi: 10.1016/S2213-8587(22)00355-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tan BKJ, et al. Prognosis and persistence of smell and taste dysfunction in patients with COVID-19: meta-analysis with parametric cure modelling of recovery curves. BMJ. 2022;378:e069503. doi: 10.1136/bmj-2021-069503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parker AM, et al. Addressing the post-acute sequelae of SARS-CoV-2 infection: a multidisciplinary model of care. Lancet Respir. Med. 2021;9:1328–1341. doi: 10.1016/S2213-2600(21)00385-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tran VT, Porcher R, Pane I, Ravaud P. Course of post COVID-19 disease symptoms over time in the ComPaRe long COVID prospective e-cohort. Nat. Commun. 2022;13:1812. doi: 10.1038/s41467-022-29513-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seessle J, et al. Persistent symptoms in adult patients 1 year after coronavirus disease 2019 (COVID-19): a prospective cohort study. Clin. Infect Dis. 2022;74:1191–1198. doi: 10.1093/cid/ciab611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Proal AD, VanElzakker MB. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 2021;12:698169. doi: 10.3389/fmicb.2021.698169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morrow AJ, et al. A multisystem, cardio-renal investigation of post-COVID-19 illness. Nat. Med. 2022;28:1303–1313. doi: 10.1038/s41591-022-01837-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu Q, et al. Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome. Gut. 2022;71:544–552. doi: 10.1136/gutjnl-2021-325989. [DOI] [PubMed] [Google Scholar]
- 23.Sherif ZA, et al. Pathogenic mechanisms of post-acute sequelae of SARS-CoV-2 infection (PASC) Elife. 2023;12:e86002. doi: 10.7554/eLife.86002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehandru S, Merad M. Pathological sequelae of long-haul COVID. Nat. Immunol. 2022;23:194–202. doi: 10.1038/s41590-021-01104-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osiaevi I, et al. Persistent capillary rarefication in long COVID syndrome. Angiogenesis. 2023;26:53–61. doi: 10.1007/s10456-022-09850-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davis HE, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;38:101019. doi: 10.1016/j.eclinm.2021.101019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang C, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang L, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med. 2022;10:863–876. doi: 10.1016/S2213-2600(22)00126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carvalho-Schneider C, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin. Microbiol. Infect. 2021;27:258–263. doi: 10.1016/j.cmi.2020.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moreno-Perez O, et al. Post-acute COVID-19 syndrome. Incidence and risk factors: a Mediterranean cohort study. J. Infect. 2021;82:378–383. doi: 10.1016/j.jinf.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Halpin SJ, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J. Med. Virol. 2021;93:1013–1022. doi: 10.1002/jmv.26368. [DOI] [PubMed] [Google Scholar]
- 32.Ballering AV, et al. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet. 2022;400:452–461. doi: 10.1016/S0140-6736(22)01214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arnold DT, et al. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax. 2021;76:399–401. doi: 10.1136/thoraxjnl-2020-216086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gunster C, et al. 6-month mortality and readmissions of hospitalized COVID-19 patients: a nationwide cohort study of 8,679 patients in Germany. PLoS One. 2021;16:e0255427. doi: 10.1371/journal.pone.0255427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chopra V, et al. Sixty-day outcomes among patients hospitalized with COVID-19. Ann. Intern. Med. 2021;174:576–578. doi: 10.7326/M20-5661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bull-Otterson L, et al. Post-COVID conditions among adult COVID-19 survivors aged 18-64 and ≥ 65 years - United States, March 2020-November 2021. MMWR Morbidity Mortality Wkly Rep. 2022;71:713–717. doi: 10.15585/mmwr.mm7121e1. [DOI] [Google Scholar]
- 37.Global Burden of Disease Long, C. C. et al. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. JAMA. 2022;328:1604–1615. doi: 10.1001/jama.2022.18931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Righi E, et al. Determinants of persistence of symptoms and impact on physical and mental wellbeing in long COVID: a prospective cohort study. J. Infect. 2022;84:566–572. doi: 10.1016/j.jinf.2022.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lam GY, et al. COVID-19 hospitalization is associated with pulmonary/diffusion abnormalities but not post-acute sequelae of COVID-19 severity. J. Intern. Med. 2022;291:694–697. doi: 10.1111/joim.13427. [DOI] [PubMed] [Google Scholar]
- 40.Menni C, et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study. Lancet. 2022;399:1618–1624. doi: 10.1016/S0140-6736(22)00327-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eyre DW, et al. Effect of COVID-19 vaccination on transmission of Alpha and Delta variants. N. Engl J. Med. 2022;386:744–756. doi: 10.1056/NEJMoa2116597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crook H, et al. Long COVID-mechanisms, risk factors, and management. BMJ. 2021;374:n1648. doi: 10.1136/bmj.n1648. [DOI] [PubMed] [Google Scholar]
- 43.Mizrahi B, et al. Long COVID outcomes at one year after mild SARS-CoV-2 infection: nationwide cohort study. BMJ. 2023;380:e072529. doi: 10.1136/bmj-2022-072529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fernandez-de-Las-Penas C, et al. Associated-onset symptoms and post-COVID-19 symptoms in hospitalized COVID-19 survivors infected with Wuhan, Alpha or Delta SARS-CoV-2 variant. Pathogens. 2022;11:725. doi: 10.3390/pathogens11070725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fernandez-de-Las-Penas C, et al. Long-COVID symptoms in individuals infected with different SARS-CoV-2 variants of concern: a systematic review of the literature. Viruses. 2022;14:2629. doi: 10.3390/v14122629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arjun MC, et al. Long COVID following Omicron wave in Eastern India-a retrospective cohort study. J. Med. Virol. 2023;95:e28214. doi: 10.1002/jmv.28214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Antonelli M, et al. Risk of long COVID associated with Delta versus Omicron variants of SARS-CoV-2. Lancet. 2022;399:2263–2264. doi: 10.1016/S0140-6736(22)00941-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Torjesen I. COVID-19: Omicron may be more transmissible than other variants and partly resistant to existing vaccines, scientists fear. BMJ. 2021;375:n2943. doi: 10.1136/bmj.n2943. [DOI] [PubMed] [Google Scholar]
- 49.Tregoning JS, et al. Progress of the COVID-19 vaccine effort: viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat. Rev. Immunol. 2021;21:626–636. doi: 10.1038/s41577-021-00592-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grewal R, et al. Effectiveness of a fourth dose of COVID-19 mRNA vaccine against the omicron variant among long term care residents in Ontario, Canada: test negative design study. BMJ. 2022;378:e071502. doi: 10.1136/bmj-2022-071502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Perlis RH, et al. Prevalence and correlates of long COVID symptoms among US adults. JAMA Netw. Open. 2022;5:e2238804. doi: 10.1001/jamanetworkopen.2022.38804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ayoubkhani D, et al. Trajectory of long COVID symptoms after COVID-19 vaccination: community based cohort study. BMJ. 2022;377:e069676. doi: 10.1136/bmj-2021-069676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Azzolini E, et al. Association between BNT162b2 vaccination and long COVID after infections not requiring hospitalization in health care workers. JAMA. 2022;328:676–678. doi: 10.1001/jama.2022.11691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Taquet M, Dercon Q, Harrison PJ. Six-month sequelae of post-vaccination SARS-CoV-2 infection: a retrospective cohort study of 10,024 breakthrough infections. Brain Behav. Immun. 2022;103:154–162. doi: 10.1016/j.bbi.2022.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meza-Torres B, et al. Differences in clinical presentation with long COVID after community and hospital infection and associations with all-cause mortality: English sentinel network database study. JMIR Public Health Surveill. 2022;8:e37668. doi: 10.2196/37668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tsuchida T, et al. Relationship between changes in symptoms and antibody titers after a single vaccination in patients with long COVID. J. Med. Virol. 2022;94:3416–3420. doi: 10.1002/jmv.27689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bowe B, Xie Y, Al-Aly Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat. Med. 2022;28:2398–2405. doi: 10.1038/s41591-022-02051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nordstrom P, Ballin M, Nordstrom A. Risk of SARS-CoV-2 reinfection and COVID-19 hospitalisation in individuals with natural and hybrid immunity: a retrospective, total population cohort study in Sweden. Lancet Infect. Dis. 2022;22:781–790. doi: 10.1016/S1473-3099(22)00143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Al-Aly Z, Bowe B, Xie Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med. 2022;28:1461–1467. doi: 10.1038/s41591-022-01840-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023;21:133–146. doi: 10.1038/s41579-022-00846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Spudich S, Nath A. Nervous system consequences of COVID-19. Science. 2022;375:267–269. doi: 10.1126/science.abm2052. [DOI] [PubMed] [Google Scholar]
- 62.Almufarrij I, Munro KJ. One year on: an updated systematic review of SARS-CoV-2, COVID-19 and audio-vestibular symptoms. Int. J. Audiol. 2021;60:935–945. doi: 10.1080/14992027.2021.1896793. [DOI] [PubMed] [Google Scholar]
- 63.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kubota T, Kuroda N, Sone D. Neuropsychiatric aspects of long COVID: a comprehensive review. Psychiatry Clin. Neurosci. 2023;77:84–93. doi: 10.1111/pcn.13508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Park JW, Wang X, Xu RH. Revealing the mystery of persistent smell loss in long COVID patients. Int. J. Biol. Sci. 2022;18:4795–4808. doi: 10.7150/ijbs.73485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Blomberg B, et al. Long COVID in a prospective cohort of home-isolated patients. Nat. Med. 2021;27:1607–1613. doi: 10.1038/s41591-021-01433-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ceban F, et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav. Immun. 2022;101:93–135. doi: 10.1016/j.bbi.2021.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Montine TJ, Bukhari SA, White LR. Cognitive impairment in older adults and therapeutic strategies. Pharmacol. Rev. 2021;73:152–162. doi: 10.1124/pharmrev.120.000031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Taquet M, et al. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8:416–427. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kao J, Frankland PW. COVID fog demystified. Cell. 2022;185:2391–2393. doi: 10.1016/j.cell.2022.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Becker JH, et al. Assessment of cognitive function in patients after COVID-19 infection. JAMA Netw. Open. 2021;4:e2130645. doi: 10.1001/jamanetworkopen.2021.30645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Taquet M, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. 2022;9:815–827. doi: 10.1016/S2215-0366(22)00260-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhang BZ, et al. SARS-CoV-2 infects human neural progenitor cells and brain organoids. Cell Res. 2020;30:928–931. doi: 10.1038/s41422-020-0390-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rutkai I, et al. Neuropathology and virus in brain of SARS-CoV-2 infected non-human primates. Nat. Commun. 2022;13:1745. doi: 10.1038/s41467-022-29440-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Stein SR, et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature. 2022;612:758–763. doi: 10.1038/s41586-022-05542-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Charnley M, et al. Neurotoxic amyloidogenic peptides in the proteome of SARS-COV2: potential implications for neurological symptoms in COVID-19. Nat. Commun. 2022;13:3387. doi: 10.1038/s41467-022-30932-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Baig AM. Differential diagnosis and pathogenesis of the neurological signs and symptoms in COVID-19 and long-COVID syndrome. CNS Neurosci. Ther. 2022;28:1905–1907. doi: 10.1111/cns.13957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Douaud G, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022;604:697–707. doi: 10.1038/s41586-022-04569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Heine J, et al. Structural brain changes in patients with post-COVID fatigue: a prospective observational study. EClinicalMedicine. 2023;58:101874. doi: 10.1016/j.eclinm.2023.101874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fernandez-Castaneda A, et al. Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation. Cell. 2022;185:2452–2468.e2416. doi: 10.1016/j.cell.2022.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Venkataramani V, Winkler F. Cognitive deficits in long COVID-19. N. Engl. J. Med. 2022;387:1813–1815. doi: 10.1056/NEJMcibr2210069. [DOI] [PubMed] [Google Scholar]
- 82.Reiken S, et al. Alzheimer’s-like signaling in brains of COVID-19 patients. Alzheimers Dement. 2022;18:955–965. doi: 10.1002/alz.12558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Frere JJ, et al. SARS-CoV-2 infection in hamsters and humans results in lasting and unique systemic perturbations after recovery. Sci. Transl. Med. 2022;14:eabq3059. doi: 10.1126/scitranslmed.abq3059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Szewczykowski C, et al. Long COVID: association of functional autoantibodies against G-protein-coupled receptors with an impaired retinal microcirculation. Int. J. Mol. Sci. 2022;23:7209. doi: 10.3390/ijms23137209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fogarty H, et al. Persistent endotheliopathy in the pathogenesis of long COVID syndrome. J. Thromb. Haemost. 2021;19:2546–2553. doi: 10.1111/jth.15490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Oikonomou E, et al. Endothelial dysfunction in acute and long standing COVID-19: a prospective cohort study. Vascul. Pharmacol. 2022;144:106975. doi: 10.1016/j.vph.2022.106975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Choutka J, Jansari V, Hornig M, Iwasaki A. Unexplained post-acute infection syndromes. Nat. Med. 2022;28:911–923. doi: 10.1038/s41591-022-01810-6. [DOI] [PubMed] [Google Scholar]
- 88.Fukuda K, et al. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann. Intern. Med. 1994;121:953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- 89.Komaroff AL, Lipkin WI. Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute COVID-19 syndrome. Trends Mol. Med. 2021;27:895–906. doi: 10.1016/j.molmed.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Epstein L, Wong KK, Kallen AJ, Uyeki TM. Post-Ebola signs and symptoms in U.S. survivors. N. Engl. J. Med. 2015;373:2484–2486. doi: 10.1056/NEJMc1506576. [DOI] [PubMed] [Google Scholar]
- 91.Jones JF, et al. Evidence for active Epstein-Barr virus infection in patients with persistent, unexplained illnesses: elevated anti-early antigen antibodies. Ann. Intern. Med. 1985;102:1–7. doi: 10.7326/0003-4819-102-1-. [DOI] [PubMed] [Google Scholar]
- 92.Komaroff AL. Is human herpesvirus-6 a trigger for chronic fatigue syndrome? J. Clin. Virol. 2006;37:S39–S46. doi: 10.1016/S1386-6532(06)70010-5. [DOI] [PubMed] [Google Scholar]
- 93.Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11:37. doi: 10.1186/1471-2377-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Salit IE. Sporadic postinfectious neuromyasthenia. CMAJ. 1985;133:659–663. [PMC free article] [PubMed] [Google Scholar]
- 95.Wong TL, Weitzer DJ. Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)-a systemic review and comparison of clinical presentation and symptomatology. Medicina. 2021;57:418. doi: 10.3390/medicina57050418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Twomey R, et al. Chronic fatigue and postexertional malaise in people living with long COVID: an observational study. Phys. Ther. 2022;102:pzac005. doi: 10.1093/ptj/pzac005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sorg AL, et al. Association of SARS-CoV-2 seropositivity with myalgic encephalomyelitis and/or chronic fatigue syndrome among children and adolescents in Germany. JAMA Netw. Open. 2022;5:e2233454. doi: 10.1001/jamanetworkopen.2022.33454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Fluge O, Tronstad KJ, Mella O. Pathomechanisms and possible interventions in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) J. Clin. Invest. 2021;131:e150377. doi: 10.1172/JCI150377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hu Z, Li S, Song X. Cytokine storm with rapidly elevated interleukin-6 indicates sudden death in patients with critical COVID-19. Cytokine Growth Factor Rev. 2021;58:30–31. doi: 10.1016/j.cytogfr.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lv Y, et al. Bioinformatics and systems biology approach to identify the pathogenetic link of long COVID and myalgic encephalomyelitis/chronic fatigue syndrome. Front. Immunol. 2022;13:952987. doi: 10.3389/fimmu.2022.952987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Haffke M, et al. Endothelial dysfunction and altered endothelial biomarkers in patients with post-COVID-19 syndrome and chronic fatigue syndrome (ME/CFS) J. Transl. Med. 2022;20:138. doi: 10.1186/s12967-022-03346-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Diaz-Resendiz KJG, et al. Loss of mitochondrial membrane potential (DeltaPsi(m)) in leucocytes as post-COVID-19 sequelae. J. Leukoc. Biol. 2022;112:23–29. doi: 10.1002/JLB.3MA0322-279RRR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Guntur VP, et al. Signatures of mitochondrial dysfunction and impaired fatty acid metabolism in plasma of patients with post-acute sequelae of COVID-19 (PASC) Metabolites. 2022;12:1026. doi: 10.3390/metabo12111026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Vogl T, et al. Systemic antibody responses against human microbiota flagellins are overrepresented in chronic fatigue syndrome patients. Sci. Adv. 2022;8:eabq2422. doi: 10.1126/sciadv.abq2422. [DOI] [PubMed] [Google Scholar]
- 105.Bragee B, et al. Signs of intracranial hypertension, hypermobility, and craniocervical obstructions in patients with myalgic encephalomyelitis/chronic fatigue syndrome. Front. Neurol. 2020;11:828. doi: 10.3389/fneur.2020.00828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hoad A, Spickett G, Elliott J, Newton J. Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome. QJM. 2008;101:961–965. doi: 10.1093/qjmed/hcn123. [DOI] [PubMed] [Google Scholar]
- 107.Weinstock LB, et al. Mast cell activation symptoms are prevalent in long-COVID. Int. J. Infect. Dis. 2021;112:217–226. doi: 10.1016/j.ijid.2021.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lund LC, et al. Post-acute effects of SARS-CoV-2 infection in individuals not requiring hospital admission: a Danish population-based cohort study. Lancet Infect. Dis. 2021;21:1373–1382. doi: 10.1016/S1473-3099(21)00211-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sudre CH, et al. Attributes and predictors of long COVID. Nat. Med. 2021;27:626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022;28:583–590. doi: 10.1038/s41591-022-01689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Fedorowski A, Sutton R. Autonomic dysfunction and postural orthostatic tachycardia syndrome in post-acute COVID-19 syndrome. Nat. Rev. Cardiol. 2023;20:281–282. doi: 10.1038/s41569-023-00842-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Aikawa T, Takagi H, Ishikawa K, Kuno T. Myocardial injury characterized by elevated cardiac troponin and in-hospital mortality of COVID-19: an insight from a meta-analysis. J. Med. Virol. 2021;93:51–55. doi: 10.1002/jmv.26108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Raman B, Bluemke DA, Luscher TF, Neubauer S. Long COVID: post-acute sequelae of COVID-19 with a cardiovascular focus. Eur. Heart J. 2022;43:1157–1172. doi: 10.1093/eurheartj/ehac031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pellegrini D, et al. Microthrombi as a major cause of cardiac injury in COVID-19: a pathologic study. Circulation. 2021;143:1031–1042. doi: 10.1161/CIRCULATIONAHA.120.051828. [DOI] [PubMed] [Google Scholar]
- 115.Chen L, et al. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc. Res. 2020;116:1097–1100. doi: 10.1093/cvr/cvaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Khan AO, et al. Preferential uptake of SARS-CoV-2 by pericytes potentiates vascular damage and permeability in an organoid model of the microvasculature. Cardiovasc. Res. 2022;118:3085–3096. doi: 10.1093/cvr/cvac097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gaebler C, et al. Evolution of antibody immunity to SARS-CoV-2. Nature. 2021;591:639–644. doi: 10.1038/s41586-021-03207-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tejerina F, et al. Post-COVID-19 syndrome. SARS-CoV-2 RNA detection in plasma, stool, and urine in patients with persistent symptoms after COVID-19. BMC Infect. Dis. 2022;22:211. doi: 10.1186/s12879-022-07153-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ceulemans LJ, et al. Persistence of SARS-CoV-2 RNA in lung tissue after mild COVID-19. Lancet Respir. Med. 2021;9:e78–e79. doi: 10.1016/S2213-2600(21)00240-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Su Y, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022;185:881–895.e820. doi: 10.1016/j.cell.2022.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wang EY, et al. Diverse functional autoantibodies in patients with COVID-19. Nature. 2021;595:283–288. doi: 10.1038/s41586-021-03631-y. [DOI] [PubMed] [Google Scholar]
- 122.Carfi A, Bernabei R, Landi F, Gemelli Against C-P-ACSG. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Takakura K, Suka M, Kajihara M, Koido S. Clinical features, therapeutic outcomes, and recovery period of long COVID. J. Med. Virol. 2023;95:e28316. doi: 10.1002/jmv.28316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Skinner JP, Moran LV. Persistent effects of COVID-19 in patients hospitalized during the first wave of the pandemic: the impact of persistent fatigue on quality of life in a cross-sectional study. J. Med. Virol. 2023;95:e28491. doi: 10.1002/jmv.28491. [DOI] [PubMed] [Google Scholar]
- 125.Ackermann M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N. Engl. J. Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cho JL, et al. Quantitative chest CT assessment of small airways disease in post-acute SARS-CoV-2 infection. Radiology. 2022;304:185–192. doi: 10.1148/radiol.212170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.McElvaney OJ, et al. Characterization of the inflammatory response to severe COVID-19 illness. Am. J. Respir. Crit. Care Med. 2020;202:812–821. doi: 10.1164/rccm.202005-1583OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Vijayakumar B, et al. Immuno-proteomic profiling reveals aberrant immune cell regulation in the airways of individuals with ongoing post-COVID-19 respiratory disease. Immunity. 2022;55:542–556.e545. doi: 10.1016/j.immuni.2022.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Littlefield KM, et al. SARS-CoV-2-specific T cells associate with inflammation and reduced lung function in pulmonary post-acute sequalae of SARS-CoV-2. PLoS Pathog. 2022;18:e1010359. doi: 10.1371/journal.ppat.1010359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594:259–264. doi: 10.1038/s41586-021-03553-9. [DOI] [PubMed] [Google Scholar]
- 131.Meringer H, Mehandru S. Gastrointestinal post-acute COVID-19 syndrome. Nat. Rev. Gastroenterol. Hepatol. 2022;19:345–346. doi: 10.1038/s41575-022-00611-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Marasco G, et al. Post COVID-19 irritable bowel syndrome. Gut. 2023;72:484–492. doi: 10.1136/gutjnl-2022-328483. [DOI] [Google Scholar]
- 133.Fernandez-de-Las-Penas C, et al. Exploring the recovery curve for gastrointestinal symptoms from the acute COVID-19 phase to long-term post-COVID: the LONG-COVID-EXP-CM multicenter study. J. Med. Virol. 2022;94:2925–2927. doi: 10.1002/jmv.27727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Blackett JW, Wainberg M, Elkind MSV, Freedberg DE. Potential long coronavirus disease 2019 gastrointestinal symptoms 6 months after coronavirus infection are associated with mental health symptoms. Gastroenterology. 2022;162:648–650.e642. doi: 10.1053/j.gastro.2021.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Joukar F, et al. Persistence of SARS-CoV-2 RNA in the nasopharyngeal, blood, urine, and stool samples of patients with COVID-19: a hospital-based longitudinal study. Virol. J. 2021;18:134. doi: 10.1186/s12985-021-01599-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Swank Z, et al. Persistent circulating severe acute respiratory syndrome coronavirus 2 spike is associated with post-acute coronavirus disease 2019 sequelae. Clin. Infect. Dis. 2023;76:e487–e490. doi: 10.1093/cid/ciac722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zollner A, et al. Postacute COVID-19 is characterized by gut viral antigen persistence in inflammatory bowel diseases. Gastroenterology. 2022;163:495–506 e498. doi: 10.1053/j.gastro.2022.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Weersma RK, Zhernakova A, Fu J. Interaction between drugs and the gut microbiome. Gut. 2020;69:1510–1519. doi: 10.1136/gutjnl-2019-320204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wang B, et al. Alterations in microbiota of patients with COVID-19: potential mechanisms and therapeutic interventions. Signal Transduct Target Ther. 2022;7:143. doi: 10.1038/s41392-022-00986-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yeoh YK, et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut. 2021;70:698–706. doi: 10.1136/gutjnl-2020-323020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Liu Q, et al. Multi-kingdom gut microbiota analyses define COVID-19 severity and post-acute COVID-19 syndrome. Nat. Commun. 2022;13:6806. doi: 10.1038/s41467-022-34535-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Vestad B, et al. Respiratory dysfunction three months after severe COVID-19 is associated with gut microbiota alterations. J. Intern. Med. 2022;291:801–812. doi: 10.1111/joim.13458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zanoli L, et al. Vascular dysfunction of COVID-19 is partially reverted in the long-term. Circ. Res. 2022;130:1276–1285. doi: 10.1161/CIRCRESAHA.121.320460. [DOI] [PubMed] [Google Scholar]
- 144.Pretorius E, et al. Persistent clotting protein pathology in long COVID/post-acute sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc. Diabetol. 2021;20:172. doi: 10.1186/s12933-021-01359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lee MH, et al. Neurovascular injury with complement activation and inflammation in COVID-19. Brain. 2022;145:2555–2568. doi: 10.1093/brain/awac151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Katsoularis I, et al. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after COVID-19: nationwide self-controlled cases series and matched cohort study. BMJ. 2022;377:e069590. doi: 10.1136/bmj-2021-069590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Petersen EL, et al. Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: the Hamburg city health study COVID programme. Eur. Heart J. 2022;43:1124–1137. doi: 10.1093/eurheartj/ehab914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Dennis A, et al. Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: a prospective, community-based study. BMJ Open. 2021;11:e048391. doi: 10.1136/bmjopen-2020-048391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wang Y, et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J. Hepatol. 2020;73:807–816. doi: 10.1016/j.jhep.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Nayar M, et al. SARS-CoV-2 infection is associated with an increased risk of idiopathic acute pancreatitis but not pancreatic exocrine insufficiency or diabetes: long-term results of the COVIDPAN study. Gut. 2022;71:1444–1447. doi: 10.1136/gutjnl-2021-326218. [DOI] [PubMed] [Google Scholar]
- 151.Liu F, et al. ACE2 expression in pancreas may cause pancreatic damage after SARS-CoV-2 infection. Clin. Gastroenterol. Hepatol. 2020;18:2128–2130.e2122. doi: 10.1016/j.cgh.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Xie Y, Al-Aly Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 2022;10:311–321. doi: 10.1016/S2213-8587(22)00044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Enghard P, et al. Long-term effects of COVID-19 on kidney function. Lancet. 2021;397:1806–1807. doi: 10.1016/S0140-6736(21)00880-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Yende S, Parikh CR. Long COVID and kidney disease. Nat. Rev. Nephrol. 2021;17:792–793. doi: 10.1038/s41581-021-00487-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Phelan N, Behan LA, Owens L. The impact of the COVID-19 pandemic on women’s reproductive health. Front. Endocrinol. 2021;12:642755. doi: 10.3389/fendo.2021.642755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Khan SM, et al. SARS-CoV-2 infection and subsequent changes in the menstrual cycle among participants in the Arizona CoVHORT study. Am. J. Obstet. Gynecol. 2022;226:270–273. doi: 10.1016/j.ajog.2021.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ding T, et al. Analysis of ovarian injury associated with COVID-19 disease in reproductive-aged women in Wuhan, China: an observational study. Front. Med. 2021;8:635255. doi: 10.3389/fmed.2021.635255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Herrero Y, et al. SARS-CoV-2 infection negatively affects ovarian function in ART patients. Biochim. Biophys. Acta Mol. Basis Dis. 2022;1868:166295. doi: 10.1016/j.bbadis.2021.166295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Madendag IC, Madendag Y, Ozdemir AT. COVID-19 disease does not cause ovarian injury in women of reproductive age: an observational before-and-after COVID-19 study. Reprod. Biomed. Online. 2022;45:153–158. doi: 10.1016/j.rbmo.2022.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.He Y, et al. Effect of COVID-19 on male reproductive system - a systematic review. Front. Endocrinol. 2021;12:677701. doi: 10.3389/fendo.2021.677701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mannur S, Jabeen T, Khader MA, Rao LSS. Post-COVID-19-associated decline in long-term male fertility and embryo quality during assisted reproductive technology. QJM. 2021;114:328–330. doi: 10.1093/qjmed/hcab019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Long COVID includes breathing and reproductive problems and has a range of risk factors. Nat Med. 28, 1554–1555, (2022). [DOI] [PMC free article] [PubMed]
- 163.Kresch E, et al. COVID-19 endothelial dysfunction can cause erectile dysfunction: histopathological, immunohistochemical, and ultrastructural study of the human penis. World J. Mens Health. 2021;39:466–469. doi: 10.5534/wjmh.210055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Thomas N, et al. The underlying sex differences in neuroendocrine adaptations relevant to myalgic encephalomyelitis chronic fatigue syndrome. Front. Neuroendocrinol. 2022;66:100995. doi: 10.1016/j.yfrne.2022.100995. [DOI] [PubMed] [Google Scholar]
- 165.Harlow BL, et al. Reproductive correlates of chronic fatigue syndrome. Am. J. Med. 1998;105:94S–99S. doi: 10.1016/S0002-9343(98)00173-9. [DOI] [PubMed] [Google Scholar]
- 166.Korszun A, et al. Follicular phase hypothalamic-pituitary-gonadal axis function in women with fibromyalgia and chronic fatigue syndrome. J. Rheumatol. 2000;27:1526–1530. [PubMed] [Google Scholar]
- 167.Soares MN, et al. Skeletal muscle alterations in patients with acute COVID-19 and post-acute sequelae of COVID-19. J. Cachexia Sarcopenia Muscle. 2022;13:11–22. doi: 10.1002/jcsm.12896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Gobbi M, et al. Skeletal muscle mass, sarcopenia and rehabilitation outcomes in post-acute COVID-19 patients. J. Clin. Med. 2021;10:5623. doi: 10.3390/jcm10235623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Zhang H, et al. Data-driven identification of post-acute SARS-CoV-2 infection subphenotypes. Nat. Med. 2023;29:226–235. doi: 10.1038/s41591-022-02116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Silva CC, et al. Muscle dysfunction in the long coronavirus disease 2019 syndrome: pathogenesis and clinical approach. Rev. Med. Virol. 2022;32:e2355. doi: 10.1002/rmv.2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Martone AM, et al. Sarcopenia as potential biological substrate of long COVID-19 syndrome: prevalence, clinical features, and risk factors. J. Cachexia Sarcopenia Muscle. 2022;13:1974–1982. doi: 10.1002/jcsm.12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Wahlgren C, et al. Rehabilitation needs following COVID-19: five-month post-discharge clinical follow-up of individuals with concerning self-reported symptoms. EClinicalMedicine. 2022;43:101219. doi: 10.1016/j.eclinm.2021.101219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Karaarslan F, Guneri FD, Kardes S. Long COVID: rheumatologic/musculoskeletal symptoms in hospitalized COVID-19 survivors at 3 and 6 months. Clin. Rheumatol. 2022;41:289–296. doi: 10.1007/s10067-021-05942-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Munblit D, et al. A core outcome set for post-COVID-19 condition in adults for use in clinical practice and research: an international Delphi consensus study. Lancet Respir. Med. 2022;10:715–724. doi: 10.1016/S2213-2600(22)00169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Disser NP, et al. Musculoskeletal consequences of COVID-19. J. Bone Joint Surg. Am. 2020;102:1197–1204. doi: 10.2106/JBJS.20.00847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Aschman T, et al. Association between SARS-CoV-2 infection and immune-mediated myopathy in patients who have died. JAMA Neurol. 2021;78:948–960. doi: 10.1001/jamaneurol.2021.2004. [DOI] [PubMed] [Google Scholar]
- 177.Suh J, et al. Skeletal muscle and peripheral nerve histopathology in COVID-19. Neurology. 2021;97:e849–e858. doi: 10.1212/WNL.0000000000012344. [DOI] [PubMed] [Google Scholar]
- 178.Hooper JE, et al. Muscle biopsy findings in a case of SARS-CoV-2-associated muscle injury. J. Neuropathol. Exp. Neurol. 2021;80:377–378. doi: 10.1093/jnen/nlaa155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Han H, et al. Profiling serum cytokines in COVID-19 patients reveals IL-6 and IL-10 are disease severity predictors. Emerg. Microbes Infect. 2020;9:1123–1130. doi: 10.1080/22221751.2020.1770129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Ong SWX, et al. Persistent symptoms and association with inflammatory cytokine signatures in recovered coronavirus disease 2019 patients. Open Forum. Infect. Dis. 2021;8:ofab156. doi: 10.1093/ofid/ofab156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Di Girolamo FG, et al. Skeletal muscle in hypoxia and inflammation: insights on the COVID-19 pandemic. Front. Nutr. 2022;9:865402. doi: 10.3389/fnut.2022.865402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Khoja O, et al. Clinical characteristics and mechanisms of musculoskeletal pain in long COVID. J. Pain Res. 2022;15:1729–1748. doi: 10.2147/JPR.S365026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Herridge MS, et al. Functional disability 5 years after acute respiratory distress syndrome. N. Engl. J. Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 184.Paneroni M, et al. Muscle strength and physical performance in patients without previous disabilities recovering from COVID-19 pneumonia. Am. J. Phys. Med. Rehabil. 2021;100:105–109. doi: 10.1097/PHM.0000000000001641. [DOI] [PubMed] [Google Scholar]
- 185.Van Aerde N, et al. Intensive care unit acquired muscle weakness in COVID-19 patients. Intensive Care Med. 2020;46:2083–2085. doi: 10.1007/s00134-020-06244-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Wang X, et al. A mitofusin 2/HIF1alpha axis sets a maturation checkpoint in regenerating skeletal muscle. J. Clin. Invest. 2022;132:e161638. doi: 10.1172/JCI161638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Merad M, Blish CA, Sallusto F, Iwasaki A. The immunology and immunopathology of COVID-19. Science. 2022;375:1122–1127. doi: 10.1126/science.abm8108. [DOI] [PubMed] [Google Scholar]
- 188.Schultheiss C, et al. Liquid biomarkers of macrophage dysregulation and circulating spike protein illustrate the biological heterogeneity in patients with post-acute sequelae of COVID-19. J. Med. Virol. 2023;95:e28364. doi: 10.1002/jmv.28364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Ruffieux H, et al. A patient-centric modeling framework captures recovery from SARS-CoV-2 infection. Nat. Immunol. 2023;24:349–358. doi: 10.1038/s41590-022-01380-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Dotan A, David P, Arnheim D, Shoenfeld Y. The autonomic aspects of the post-COVID19 syndrome. Autoimmun. Rev. 2022;21:103071. doi: 10.1016/j.autrev.2022.103071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Hallmann E, et al. IgG autoantibodies against ACE2 in SARS-CoV-2 infected patients. J. Med. Virol. 2023;95:e28273. doi: 10.1002/jmv.28273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Son K, et al. Circulating anti-nuclear autoantibodies in COVID-19 survivors predict long COVID symptoms. Eur. Respir. J. 2023;61:2200970. doi: 10.1183/13993003.00970-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Ryan FJ, et al. Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection. BMC Med. 2022;20:26. doi: 10.1186/s12916-021-02228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Peluso MJ, et al. Markers of immune activation and inflammation in individuals with postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection. J. Infect. Dis. 2021;224:1839–1848. doi: 10.1093/infdis/jiab490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Phetsouphanh C, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat. Immunol. 2022;23:210–216. doi: 10.1038/s41590-021-01113-x. [DOI] [PubMed] [Google Scholar]
- 196.Thompson RC, et al. Molecular states during acute COVID-19 reveal distinct etiologies of long-term sequelae. Nat. Med. 2023;29:236–246. doi: 10.1038/s41591-022-02107-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Scott NA, et al. Monocyte migration profiles define disease severity in acute COVID-19 and unique features of long COVID. Eur. Respir. J. 2023;61:2202226. doi: 10.1183/13993003.02226-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Sneller MC, et al. A longitudinal study of COVID-19 sequelae and immunity: baseline findings. Ann. Intern. Med. 2022;175:969–979. doi: 10.7326/M21-4905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Fietsam AC, Bryant AD, Rudroff T. Fatigue and perceived fatigability, not objective fatigability, are prevalent in people with post-COVID-19. Exp. Brain Res. 2023;241:211–219. doi: 10.1007/s00221-022-06518-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Kachaner A, et al. Somatic symptom disorder in patients with post-COVID-19 neurological symptoms: a preliminary report from the somatic study (somatic symptom disorder triggered by COVID-19) J. Neurol. Neurosurg. Psychiatry. 2022;93:1174–1180. doi: 10.1136/jnnp-2021-327899. [DOI] [PubMed] [Google Scholar]
- 201.Horn M, et al. Persistent physical symptoms after COVID-19 infection and the risk of somatic symptom disorder. J. Psychosom. Res. 2023;166:111172. doi: 10.1016/j.jpsychores.2023.111172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Matta J, et al. Association of self-reported COVID-19 infection and SARS-CoV-2 serology test results with persistent physical symptoms among French adults during the COVID-19 pandemic. JAMA Intern. Med. 2022;182:19–25. doi: 10.1001/jamainternmed.2021.6454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Fleischer M, et al. Post-COVID-19 syndrome is rarely associated with damage of the nervous system: findings from a prospective observational cohort study in 171 patients. Neurol. Ther. 2022;11:1637–1657. doi: 10.1007/s40120-022-00395-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Hawke LD, et al. Interventions for mental health, cognition, and psychological wellbeing in long COVID: a systematic review of registered trials. Psychol. Med. 2022;52:2426–2440. doi: 10.1017/S0033291722002203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Magnusdottir I, et al. Acute COVID-19 severity and mental health morbidity trajectories in patient populations of six nations: an observational study. Lancet Public Health. 2022;7:e406–e416. doi: 10.1016/S2468-2667(22)00042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Tenforde MW, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network - United States, March-June 2020. MMWR Morb. Mortal Wkly Rep. 2020;69:993–998. doi: 10.15585/mmwr.mm6930e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Saunders C, Sperling S, Bendstrup E. A new paradigm is needed to explain long COVID. Lancet Respir. Med. 2023;11:e12–e13. doi: 10.1016/S2213-2600(22)00501-X. [DOI] [PubMed] [Google Scholar]
- 208.Mazza MG, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Yang CP, et al. Long COVID and long chain fatty acids (LCFAs): psychoneuroimmunity implication of omega-3 LCFAs in delayed consequences of COVID-19. Brain Behav. Immun. 2022;103:19–27. doi: 10.1016/j.bbi.2022.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Malik P, et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-a systematic review and meta-analysis. J. Med. Virol. 2022;94:253–262. doi: 10.1002/jmv.27309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Lemogne C, Gouraud C, Pitron V, Ranque B. Why the hypothesis of psychological mechanisms in long COVID is worth considering. J. Psychosom. Res. 2023;165:111135. doi: 10.1016/j.jpsychores.2022.111135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Byrne EA. Understanding long COVID: nosology, social attitudes and stigma. Brain Behav. Immun. 2022;99:17–24. doi: 10.1016/j.bbi.2021.09.012. [DOI] [PubMed] [Google Scholar]
- 213.Fava GA, Cosci F, Sonino N. Current psychosomatic practice. Psychother. Psychosom. 2017;86:13–30. doi: 10.1159/000448856. [DOI] [PubMed] [Google Scholar]
- 214.Pantelic M, et al. The prevalence of stigma in a UK community survey of people with lived experience of long COVID. Lancet. 2022;400:S84. doi: 10.1016/S0140-6736(22)02294-2. [DOI] [Google Scholar]
- 215.Satterfield BA, Bhatt DL, Gersh BJ. Cardiac involvement in the long-term implications of COVID-19. Nat. Rev. Cardiol. 2022;19:332–341. doi: 10.1038/s41569-021-00631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Blanco JR, et al. Pulmonary long-term consequences of COVID-19 infections after hospital discharge. Clin. Microbiol. Infect. 2021;27:892–896. doi: 10.1016/j.cmi.2021.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Bungenberg J, et al. Long COVID-19: objectifying most self-reported neurological symptoms. Ann. Clin. Transl. Neurol. 2022;9:141–154. doi: 10.1002/acn3.51496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Guedj E, et al. (18)F-FDG brain PET hypometabolism in patients with long COVID. Eur. J. Nucl. Med. Mol. Imaging. 2021;48:2823–2833. doi: 10.1007/s00259-021-05215-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Dressing A, et al. Neuropsychologic profiles and cerebral glucose metabolism in neurocognitive long COVID syndrome. J. Nucl. Med. 2022;63:1058–1063. doi: 10.2967/jnumed.121.262677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Giannos P, Prokopidis K. Gut dysbiosis and long COVID-19: feeling gutted. J. Med. Virol. 2022;94:2917–2918. doi: 10.1002/jmv.27684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Su Q, et al. Faecal microbiome-based machine learning for multi-class disease diagnosis. Nat. Commun. 2022;13:6818. doi: 10.1038/s41467-022-34405-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Haran JP, et al. Inflammation-type dysbiosis of the oral microbiome associates with the duration of COVID-19 symptoms and long COVID. JCI Insight. 2021;6:e152346. doi: 10.1172/jci.insight.152346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Bizjak DA, et al. Kynurenine serves as useful biomarker in acute, long- and post-COVID-19 diagnostics. Front. Immunol. 2022;13:1004545. doi: 10.3389/fimmu.2022.1004545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Guasp M, et al. CSF biomarkers in COVID-19 associated encephalopathy and encephalitis predict long-term outcome. Front. Immunol. 2022;13:866153. doi: 10.3389/fimmu.2022.866153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Hanson BA, et al. Plasma biomarkers of neuropathogenesis in hospitalized patients with COVID-19 and those with postacute sequelae of SARS-CoV-2 infection. Neurol. Neuroimmunol. Neuroinflamm. 2022;9:e1151. doi: 10.1212/NXI.0000000000001151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Mandal S, et al. ‘Long-COVID’: a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. 2021;76:396–398. doi: 10.1136/thoraxjnl-2020-215818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Mazza MG, et al. Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: effect of inflammatory biomarkers at three-month follow-up. Brain Behav. Immun. 2021;94:138–147. doi: 10.1016/j.bbi.2021.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Patel MA, et al. Elevated vascular transformation blood biomarkers in long-COVID indicate angiogenesis as a key pathophysiological mechanism. Mol Med. 2022;28:122. doi: 10.1186/s10020-022-00548-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Peluso MJ, et al. SARS-CoV-2 and mitochondrial proteins in neural-derived exosomes of COVID-19. Ann. Neurol. 2022;91:772–781. doi: 10.1002/ana.26350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Queiroz MAF, et al. Cytokine profiles associated with acute COVID-19 and long COVID-19 syndrome. Front. Cell Infect. Microbiol. 2022;12:922422. doi: 10.3389/fcimb.2022.922422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Sun B, et al. Characterization and biomarker analyses of post-COVID-19 complications and neurological manifestations. Cells. 2021;10:386. doi: 10.3390/cells10020386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Yong SJ, et al. Inflammatory and vascular biomarkers in post-COVID-19 syndrome: a systematic review and meta-analysis of over 20 biomarkers. Rev. Med. Virol. 2023;33:e2424. doi: 10.1002/rmv.2424. [DOI] [PubMed] [Google Scholar]
- 233.Esteller M. Non-coding RNAs in human disease. Nat. Rev. Genet. 2011;12:861–874. doi: 10.1038/nrg3074. [DOI] [PubMed] [Google Scholar]
- 234.Zhao Q, et al. Identification of a SARS-CoV-2 virus-encoded small non-coding RNA in association with the neurological disorders in COVID-19 patients. Signal Transduct. Target Ther. 2022;7:107. doi: 10.1038/s41392-022-00969-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Donyavi T, et al. Acute and post-acute phase of COVID-19: analyzing expression patterns of miRNA-29a-3p, 146a-3p, 155-5p, and let-7b-3p in PBMC. Int. Immunopharmacol. 2021;97:107641. doi: 10.1016/j.intimp.2021.107641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.NICE. COVID-19 rapid guideline: managing the long-term effects of COVID-19, https://www.ncbi.nlm.nih.gov/books/NBK567261/ (2020). [PubMed]
- 237.Chee YJ, et al. Clinical trials on the pharmacological treatment of long COVID: a systematic review. J. Med. Virol. 2023;95:e28289. doi: 10.1002/jmv.28289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Yelin D, et al. ESCMID rapid guidelines for assessment and management of long COVID. Clin. Microbiol. Infect. 2022;28:955–972. doi: 10.1016/j.cmi.2022.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Vanfleteren L, Spruit MA, Wouters EFM, Franssen FME. Management of chronic obstructive pulmonary disease beyond the lungs. Lancet Respir. Med. 2016;4:911–924. doi: 10.1016/S2213-2600(16)00097-7. [DOI] [PubMed] [Google Scholar]
- 240.Nopp S, et al. Outpatient pulmonary rehabilitation in patients with long COVID improves exercise capacity, functional status, dyspnea, fatigue, and quality of life. Respiration. 2022;101:593–601. doi: 10.1159/000522118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.McNarry MA, et al. Inspiratory muscle training enhances recovery post-COVID-19: a randomised controlled trial. Eur. Respir. J. 2022;60:2103101. doi: 10.1183/13993003.03101-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Philip KEJ, et al. An online breathing and wellbeing programme (ENO Breathe) for people with persistent symptoms following COVID-19: a parallel-group, single-blind, randomised controlled trial. Lancet Respir. Med. 2022;10:851–862. doi: 10.1016/S2213-2600(22)00125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Shi L, et al. Human mesenchymal stem cells treatment for severe COVID-19: 1-year follow-up results of a randomized, double-blind, placebo-controlled trial. EBioMedicine. 2022;75:103789. doi: 10.1016/j.ebiom.2021.103789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Besnier F, et al. Cardiopulmonary rehabilitation in long-COVID-19 Patients with persistent breathlessness and fatigue: the COVID-Rehab study. Int. J. Environ. Res. Public Health. 2022;19:4133. doi: 10.3390/ijerph19074133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Grandi E, Ripplinger CM. Antiarrhythmic mechanisms of beta blocker therapy. Pharmacol. Res. 2019;146:104274. doi: 10.1016/j.phrs.2019.104274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Fedorowski A. Postural orthostatic tachycardia syndrome: clinical presentation, aetiology and management. J. Intern. Med. 2019;285:352–366. doi: 10.1111/joim.12852. [DOI] [PubMed] [Google Scholar]
- 247.NICE. Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management, https://www.ncbi.nlm.nih.gov/books/NBK579533/ (2021).
- 248.Cash A, Kaufman DL. Oxaloacetate treatment for mental and physical fatigue in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and long-COVID fatigue patients: a non-randomized controlled clinical trial. J. Transl. Med. 2022;20:295. doi: 10.1186/s12967-022-03488-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Robbins T, et al. Hyperbaric oxygen therapy for the treatment of long COVID: early evaluation of a highly promising intervention. Clin. Med. 2021;21:e629–e632. doi: 10.7861/clinmed.2021-0462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Tirelli U, et al. Fatigue in post-acute sequelae of SARS-CoV2 (PASC) treated with oxygen-ozone autohemotherapy - preliminary results on 100 patients. Eur. Rev. Med. Pharmacol. Sci. 2021;25:5871–5875. doi: 10.26355/eurrev_202109_26809. [DOI] [PubMed] [Google Scholar]
- 251.Blackett JW, et al. Decreased gut microbiome tryptophan metabolism and serotonergic signaling in patients with persistent mental health and gastrointestinal symptoms after COVID-19. Clin. Transl. Gastroenterol. 2022;13:e00524. doi: 10.14309/ctg.0000000000000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Zhang L, et al. Gut microbiota-derived synbiotic formula (SIM01) as a novel adjuvant therapy for COVID-19: an open-label pilot study. J. Gastroenterol. Hepatol. 2022;37:823–831. doi: 10.1111/jgh.15796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Trimarco V, et al. Endothelial dysfunction in long-COVID: new insights from the nationwide multicenter LINCOLN study. Pharmacol. Res. 2022;185:106486. doi: 10.1016/j.phrs.2022.106486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Izzo R, et al. Combining L-Arginine with vitamin C improves long-COVID symptoms: the LINCOLN survey. Pharmacol. Res. 2022;183:106360. doi: 10.1016/j.phrs.2022.106360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Pitt B, et al. Repurposing low-dose naltrexone for the prevention and treatment of immunothrombosis in COVID-19. Eur. Heart J. Cardiovasc. Pharmacother. 2022;8:402–405. doi: 10.1093/ehjcvp/pvac014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Weiler CR, et al. AAAAI mast cell disorders committee work group report: mast cell activation syndrome (MCAS) diagnosis and management. J. Allergy Clin. Immunol. 2019;144:883–896. doi: 10.1016/j.jaci.2019.08.023. [DOI] [PubMed] [Google Scholar]
- 257.Noda Y, et al. Real world research on transcranial magnetic stimulation treatment strategies for neuropsychiatric symptoms with long-COVID in Japan. Asian J. Psychiatr. 2023;81:103438. doi: 10.1016/j.ajp.2022.103438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Vaira LA, et al. Efficacy of corticosteroid therapy in the treatment of long-lasting olfactory disorders in COVID-19 patients. Rhinology. 2021;59:21–25. doi: 10.4193/Rhin20.515. [DOI] [PubMed] [Google Scholar]
- 259.De Luca P, et al. Effect of ultra-micronized palmitoylethanolamide and luteolin on olfaction and memory in patients with long COVID: results of a longitudinal study. Cells. 2022;11:2552. doi: 10.3390/cells11162552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Shanthanna H, Nelson AM, Kissoon N, Narouze S. The COVID-19 pandemic and its consequences for chronic pain: a narrative review. Anaesthesia. 2022;77:1039–1050. doi: 10.1111/anae.15801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Korompoki E, et al. Epidemiology and organ specific sequelae of post-acute COVID19: a narrative review. J. Infect. 2021;83:1–16. doi: 10.1016/j.jinf.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Fancourt D, Steptoe A, Bu F. Psychological consequences of long COVID: comparing trajectories of depressive and anxiety symptoms before and after contracting SARS-CoV-2 between matched long- and short-COVID groups. Br. J. Psychiatry. 2023;222:74–81. doi: 10.1192/bjp.2022.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Kharaeva Z, et al. Fermented Carica papaya and Morinda citrifolia as perspective food supplements for the treatment of post-COVID symptoms: randomized placebo-controlled clinical laboratory study. Nutrients. 2022;14:2203. doi: 10.3390/nu14112203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Motti ML, et al. The role of nutrients in prevention, treatment and post-coronavirus disease-2019 (COVID-19) Nutrients. 2022;14:1000. doi: 10.3390/nu14051000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Suran M. VA finds nirmatrelvir associated with lower risk of long COVID. JAMA. 2022;328:2386. doi: 10.1001/jama.2022.20051. [DOI] [PubMed] [Google Scholar]
- 266.Oronsky B, et al. A review of persistent post-COVID syndrome (PPCS) Clin. Rev. Allergy Immunol. 2023;64:66–74. doi: 10.1007/s12016-021-08848-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Hammond J, et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with COVID-19. N. Engl. J. Med. 2022;386:1397–1408. doi: 10.1056/NEJMoa2118542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Bi WL, et al. Artificial intelligence in cancer imaging: clinical challenges and applications. CA Cancer J. Clin. 2019;69:127–157. doi: 10.3322/caac.21552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Liang H, et al. Evaluation and accurate diagnoses of pediatric diseases using artificial intelligence. Nat. Med. 2019;25:433–438. doi: 10.1038/s41591-018-0335-9. [DOI] [PubMed] [Google Scholar]
- 270.Wang C, et al. Development and validation of an abnormality-derived deep-learning diagnostic system for major respiratory diseases. npj Digit Med. 2022;5:124. doi: 10.1038/s41746-022-00648-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Zhang K, et al. Clinically applicable AI system for accurate diagnosis, quantitative measurements, and prognosis of COVID-19 pneumonia using computed tomography. Cell. 2020;181:1423–1433.e1411. doi: 10.1016/j.cell.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Wang G, et al. A deep-learning pipeline for the diagnosis and discrimination of viral, non-viral and COVID-19 pneumonia from chest X-ray images. Nat. Biomed. Eng. 2021;5:509–521. doi: 10.1038/s41551-021-00704-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Qi E, et al. Investigation of liquid biopsy analytes in peripheral blood of individuals after SARS-CoV-2 infection. EBioMedicine. 2023;90:104519. doi: 10.1016/j.ebiom.2023.104519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Sonnweber T, et al. Investigating phenotypes of pulmonary COVID-19 recovery: a longitudinal observational prospective multicenter trial. Elife. 2022;11:e72500. doi: 10.7554/eLife.72500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Pfaff ER, et al. Identifying who has long COVID in the USA: a machine learning approach using N3C data. Lancet Digit Health. 2022;4:e532–e541. doi: 10.1016/S2589-7500(22)00048-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Hultstrom M, et al. Dehydration is associated with production of organic osmolytes and predicts physical long-term symptoms after COVID-19: a multicenter cohort study. Crit. Care. 2022;26:322. doi: 10.1186/s13054-022-04203-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Reese JT, et al. Generalisable long COVID subtypes: findings from the NIH N3C and RECOVER programmes. EBioMedicine. 2023;87:104413. doi: 10.1016/j.ebiom.2022.104413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Hughes SE, et al. Development and validation of the symptom burden questionnaire for long COVID (SBQ-LC): rasch analysis. BMJ. 2022;377:e070230. doi: 10.1136/bmj-2022-070230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Tran VT, et al. Development and validation of the long coronavirus disease (COVID) symptom and impact tools: a set of patient-reported instruments constructed from patients’ lived experience. Clin. Infect Dis. 2022;74:278–287. doi: 10.1093/cid/ciab352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Sivan M, et al. The modified COVID-19 Yorkshire rehabilitation scale (C19-YRSm) patient-reported outcome measure for long COVID or post-COVID-19 syndrome. J. Med. Virol. 2022;94:4253–4264. doi: 10.1002/jmv.27878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Bocchino M, et al. Chest CT-based assessment of 1-year outcomes after moderate COVID-19 pneumonia. Radiology. 2022;305:479–485. doi: 10.1148/radiol.220019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Han X, et al. Six-month follow-up chest CT findings after severe COVID-19 pneumonia. Radiology. 2021;299:E177–E186. doi: 10.1148/radiol.2021203153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Lerum TV, et al. Dyspnoea, lung function and CT findings 3 months after hospital admission for COVID-19. Eur. Respir. J. 2021;57:2003448. doi: 10.1183/13993003.03448-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Luger AK, et al. Chest CT of lung injury 1 year after COVID-19 pneumonia: the CovILD study. Radiology. 2022;304:462–470. doi: 10.1148/radiol.211670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Solomon JJ, et al. CT of post-acute lung complications of COVID-19. Radiology. 2021;301:E383–E395. doi: 10.1148/radiol.2021211396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Li D, et al. Healthy outcomes of patients with COVID-19 two years after the infection: a prospective cohort study. Emerg. Microbes Infect. 2022;11:2680–2688. doi: 10.1080/22221751.2022.2133639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Vijayakumar B, et al. CT lung abnormalities after COVID-19 at 3 months and 1 year after hospital discharge. Radiology. 2022;303:444–454. doi: 10.1148/radiol.2021211746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Lipkova J, et al. Artificial intelligence for multimodal data integration in oncology. Cancer Cell. 2022;40:1095–1110. doi: 10.1016/j.ccell.2022.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Shao J, et al. Predicting gene mutation status via artificial intelligence technologies based on multimodal integration (MMI) to advance precision oncology. Semin. Cancer Biol. 2023;91:1–15. doi: 10.1016/j.semcancer.2023.02.006. [DOI] [PubMed] [Google Scholar]
- 290.Boehm KM, et al. Harnessing multimodal data integration to advance precision oncology. Nat. Rev. Cancer. 2022;22:114–126. doi: 10.1038/s41568-021-00408-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Cauchemez S, Bosetti P. A reconstruction of early cryptic COVID spread. Nature. 2021;600:40–41. doi: 10.1038/d41586-021-02989-3. [DOI] [PubMed] [Google Scholar]
- 292.Kucirka LM, et al. Variation in false-negative rate of reverse transcriptase polymerase chain reaction-based SARS-CoV-2 tests by time since exposure. Ann. Intern. Med. 2020;173:262–267. doi: 10.7326/M20-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Dos Santos PG, et al. When to test for COVID-19 using real-time reverse transcriptase polymerase chain reaction: a systematic review. Int. J. Infect. Dis. 2022;123:58–69. doi: 10.1016/j.ijid.2022.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Davido B, et al. Predictors of nonseroconversion after SARS-CoV-2 infection. Emerg. Infect. Dis. 2022;28:492–493. doi: 10.3201/eid2802.211971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Van Elslande J, et al. Longitudinal follow-up of IgG anti-nucleocapsid antibodies in SARS-CoV-2 infected patients up to eight months after infection. J. Clin. Virol. 2021;136:104765. doi: 10.1016/j.jcv.2021.104765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Toh ZQ, et al. Comparison of seroconversion in children and adults with mild COVID-19. JAMA Netw. Open. 2022;5:e221313. doi: 10.1001/jamanetworkopen.2022.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Deeks JJ, et al. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst. Rev. 2020;6:CD013652. doi: 10.1002/14651858.CD013652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Peterson TM, et al. Coverage of CFS within U.S. medical schools. Univers. J. Public Health. 2013;1:177–179. doi: 10.13189/ujph.2013.010404. [DOI] [Google Scholar]
- 299.Shaw BH, et al. The face of postural tachycardia syndrome - insights from a large cross-sectional online community-based survey. J. Intern. Med. 2019;286:438–448. doi: 10.1111/joim.12895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Brigham E, et al. The Johns Hopkins Post-Acute COVID-19 Team (PACT): a multidisciplinary, collaborative, ambulatory framework supporting COVID-19 survivors. Am. J. Med. 2021;134:462–467.e461. doi: 10.1016/j.amjmed.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Adeloye D, et al. The long-term sequelae of COVID-19: an international consensus on research priorities for patients with pre-existing and new-onset airways disease. Lancet Respir. Med. 2021;9:1467–1478. doi: 10.1016/S2213-2600(21)00286-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Aiyegbusi OL, et al. Symptoms, complications and management of long COVID: a review. J. R. Soc. Med. 2021;114:428–442. doi: 10.1177/01410768211032850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Yong SJ, Liu S. Proposed subtypes of post-COVID-19 syndrome (or long-COVID) and their respective potential therapies. Rev. Med. Virol. 2022;32:e2315. doi: 10.1002/rmv.2315. [DOI] [PubMed] [Google Scholar]
- 304.He ST, et al. Long COVID: the latest manifestations, mechanisms, and potential therapeutic interventions. MedComm. 2022;3:e196. doi: 10.1002/mco2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]