Abstract
How to cite this article: Dada T, Chauhan N. Optimizing Glaucoma Care: A Holistic Approach. J Curr Glaucoma Pract 2023;17(3):111–112.
Managing a glaucoma patient is like entering into a lifelong partnership with a fellow human being. The treating doctor is dealing with not only ocular disease but various mental and physical health issues that impact the overall quality of life of the patient, in addition to integrating the patient into a new family and social dynamic as vision-related quality of life gets hampered. There are also several unforeseen circumstances that may arise, like what we saw during the coronavirus disease 2019 pandemic, where many patients lost access to healthcare and economic constraints caused by job cuts which pushed patients into a situation where they could not afford topical medical therapy. It is time to expand the role of a glaucoma surgeon beyond prescribing drops and performing lasers/surgery such that they can positively impact the lives of glaucoma patients and their families.
Glaucoma is the leading cause of irreversible blindness worldwide.1 It's been noted that blindness is considered to be one of the most feared medical conditions, and adults who lose visual function are 90% more likely to experience depression than people whose visual function is not compromised.2 Giving the patient a diagnosis of glaucoma incites immediate anxiety with fearful and negative emotions. “Am i going blind?” is a question often the glaucoma patients ask us with great apprehension about the future. They need to be spoken to with care and compassion and made to understand the disease and its holistic management in a manner that instills hope for the future.
Furthermore, as a patient follows up and notices the progression of disease with advancing visual field defects (this may happen even with adequate intraocular pressure (IOP) control, which becomes even more frustrating for both the patient and the treating doctor) and age-related deterioration, this creates a condition of chronic stress (allostatic overload) which increases the risk of other life-threatening diseases such as cardiovascular disease, diabetes, obesity, arthritis, and cancer and increases the risk of mortality. Chronic stress leads to an increase in endogenous cortisol, which has the potential to raise IOP and worsen optic neuropathy, while at the same time, high cortisol levels are detrimental to the hippocampal neurons and are implicated in cognitive decline and neurodegenerative disease. This can create a vicious cycle and lead to further deterioration of the disease. An increase in stress can also lead to a rise in catecholamines, which can compromise optic disc perfusion.3,4 Increasing evidence from human to animal studies has shown that glaucoma shares some common neurodegenerative pathways with Alzheimer's disease and other tauopathies, such as chronic traumatic encephalopathy and frontotemporal dementia.5 Alleviating chronic stress and reducing allostatic load and other strategies to target neurodegeneration can be additional goals in the management of glaucoma patients, which are often overlooked in routine clinical care.
Holistic glaucoma management would entail a focus on all the mechanisms that are implicated in apoptosis of retinal ganglion cells (RGC), including barotrauma,6,7 autonomic dysfunctions with sympathetic overactivity leading to vasoconstriction and ischemia/hypoxia,8 reductions in neurotrophic factors like brain-derived neurotrophic factor,9 increase in inflammatory mediators like transforming growth factor-β,10 increased cortisol levels,11 mitochondrial and nitric oxide pathway dysfunction, and age-related neurodegeneration which leads to progressive loss of RGC. Health education regarding the disease, appropriate use and application of eye drops, associated systemic disease and drug interaction with glaucoma medications, dietary and lifestyle modifications, vitamin supplements, physical exercise, breathing techniques for relaxation, yoga (without head down postures), and meditation, eligibility for driving and risk of motor vehicle accidents, cessation of smoking, etc., should be imparted to all glaucoma patients. Appropriate referral to physicians for the detection and management of systemic disease on a regular basis is essential, and rehabilitation of visually impaired patients with assistive devices is required. The importance of family screening (especially for siblings) should be discussed with the patient, and appropriate annual appointments should be fixed for family members.
In addition, psychological counseling of the patient and the family, along with an assessment of the caregiver burden, is essential, especially when dealing with visually impaired/blind glaucoma patients.
With glaucoma patients, we are not just treating the disease at one point of interaction but are following up with them for the rest of their lives. How we can support them in this long journey is the goal of effective management. Assessing their existing support group, evaluating their financial burden, and titrating therapy accordingly with generic/branded medications or low-cost microinvasive glaucoma surgery or even a primary trabeculectomy where medications are not available/affordable is essential. Providing them with access to the required psychological, social, and financial support is vital to any glaucoma management strategy.
In a recent study at a tertiary care center, it was seen that 58.11% of glaucoma patients were noncompliant due to the unavailability of drugs in a government pharmacy or the incapability of the patient to afford drugs from a private pharmacy.12
With many glaucoma patients becoming severely impaired visually, they are dependent on their caregivers. They are responsible for the physical, mental, and emotional well-being of the patient. It's been seen that caring for a person dependent on them can be a precipitating factor for depression in caregivers.13 The burden carried by them and the negative feelings harbored can affect the quality of care provided by them.14 While we speak to our patients on follow-up, we recommend spending a few minutes talking to the caregiver and assessing their mental well-being. Creating social support groups for the caregivers encouraging patients to involve themselves in social activities with friends and families outside of their household can positively impact their health,15 suggesting healthy mind-body practices to them can aid in elevating their as well as the patient's quality of life.
In conclusion, the management of glaucoma patients should move forward from just medical/laser/surgical therapies to lower IOP and establish a lifetime management system to optimize the quality of life of glaucoma patients with an enhanced focus on systemic health, lifestyle interventions, psychological and social support networks and matching medical care with available financial resources along with the involvement of the caregiver looking after these patients. We should strive to make our patients thrive and flourish and live happily even with a sight-threatening disease, and that should be the matrix for our measurement of a successful outcome.
The four pillars of glaucoma management are summarized in Figure 1.
Fig. 1.
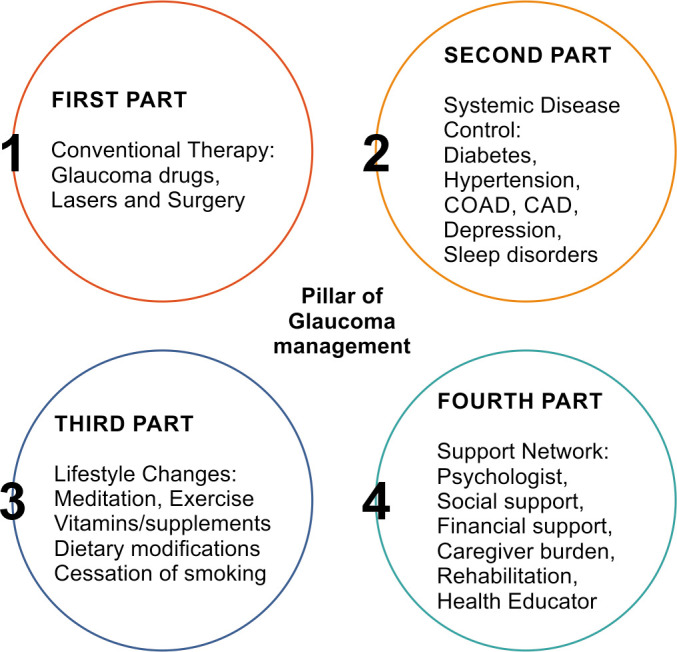
Pillars of glaucoma management
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Resnikoff S, Pascolini D, Etya’ ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82(11):844–851. 15640920 [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang X, Bullard KM, Cotch MF, et al. Association between depression and functional vision loss in persons 20 years of age or older in the United States, NHANES 2005-2008. JAMA Ophthalmol. 2013;131(5):573–581. doi: 10.1001/jamaophthalmol.2013.2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKlveen JM, Myers B, Flak JN, et al. Role of prefrontal cortex glucocorticoid receptors in stress and emotion. Biol Psychiatry. 2013;74(9):672–679. doi: 10.1016/j.biopsych.2013.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lupien SJ, McEwen BS, Gunnar MR, et al. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10(6):434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- 5.Chan JW, Chan NCY, Sadun AA. Glaucoma as neurodegeneration in the brain. Eye Brain. 2021;13:21–28. doi: 10.2147/EB.S293765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burgoyne CF, Downs JC, Bellezza AJ, et al. The optic nerve head as a biomechanical structure: a new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog Retin Eye Res. 2005;24(1):39–73. doi: 10.1016/j.preteyeres.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Fechtner RD, Weinreb RN. Mechanisms of optic nerve damage in primary open angle glaucoma. Surv Ophthalmol. 1994;39(1):23–42. doi: 10.1016/s0039-6257(05)80042-6. [DOI] [PubMed] [Google Scholar]
- 8.Pasquale LR. Vascular and autonomic dysregulation in primary open-angle glaucoma. Curr Opin Ophthalmol. 2016;27(2):94–101. doi: 10.1097/ICU.0000000000000245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson EC, Guo Y, Cepurna WO, et al. Neurotrophin roles in retinal ganglion cell survival: lessons from rat glaucoma models. Exp Eye Res. 2009;88(4):808–815. doi: 10.1016/j.exer.2009.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu H, Chen M, Forrester JV. Para-inflammation in the aging retina. Prog Retin Eye Res. 2009;28(5):348–368. doi: 10.1016/j.preteyeres.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz B, McCarty G, Rosner B. Increased plasma free cortisol in ocular hypertension and open angle glaucoma. Arch Ophthalmol. 1987;105(8):1060–1065. doi: 10.1001/archopht.1987.01060080062029. [DOI] [PubMed] [Google Scholar]
- 12.Usgaonkar UPS, Naik R, Shetty A. The economic burden of glaucoma on patients. Indian J Ophthalmol. 2023;71(2):560–566. doi: 10.4103/ijo.IJO_1676_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dada T, Aggarwal A, Bali SJ, et al. Caregiver burden assessment in primary congenital glaucoma. Eur J Ophthalmol. 2013;23(3):324–328. doi: 10.5301/ejo.5000238. [DOI] [PubMed] [Google Scholar]
- 14.Chow MY, Morrow AM, Cooper Robbins SC, et al. Condition-specific quality of life questionnaires for caregivers of children with pediatric conditions: a systematic review. Qual Life Res. 2013;22(8):2183–2200. doi: 10.1007/s11136-012-0343-z. [DOI] [PubMed] [Google Scholar]
- 15.Jin S, Trope GE, Buys YM, et al. Reduced social participation among seniors with self-reported visual impairment and glaucoma. PLoS One. 2019;14(7):e0218540. doi: 10.1371/journal.pone.0218540. [DOI] [PMC free article] [PubMed] [Google Scholar]


