Abstract
Background:
Children with sickle cell anemia (SCA) have substantial medical needs and more unmet basic needs than children with other medical conditions. Despite a recent focus on social determinants of health (SDoH), there remains an incomplete understanding of the processes linking SDoH and disease management, particularly for youth with SCA. This study elucidated these processes and identified ways to mitigate deleterious effects of adverse SDoH on SCA management.
Methods:
Parents/primary caregivers (N=27) of children with SCA (≤12 years old) participated in semi-structured interviews regarding SCA management and SDoH and completed quantitative measures of basic needs. Qualitative data were systematically coded and analyzed using applied thematic analysis. Quantitative data were presented descriptively.
Results:
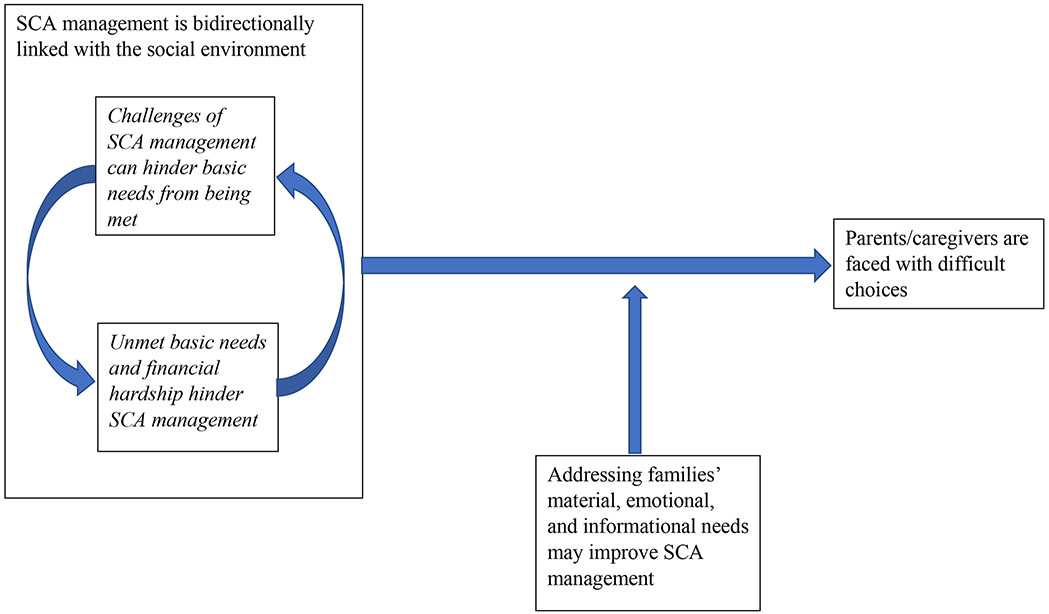
Three qualitative themes were identified. First, SCA management is bidirectionally linked with the social environment, whereby challenges of SCA management can hinder basic needs from being met, and unmet basic needs and financial hardship hinder SCA management. Second, due to limited resources, parents/caregivers are faced with difficult choices between prioritizing basic needs versus SCA management. Third, addressing material, emotional, and informational needs may improve SCA management. Quantitatively, 73% of families endorsed ≥1 basic need, including food insecurity (42%), housing instability (62%) and/or energy insecurity (20%).
Conclusion:
Despite documented associations, there remains a poor understanding of the processes linking SDoH and health. Findings underscore how day-to-day conditions undermine the management of SCA treatments, symptoms, and complications, limiting treatment effectiveness. Understanding these processes may inform family-centered, health equity interventions and policies to improve living conditions, disease management, and health outcomes.
Keywords: pediatric, sickle cell disease, social determinants of health, basic needs, family
Introduction
Sickle cell disease (SCD) is a chronic inherited disorder characterized by repeated episodes of pain crises and chronic organ dysfunction predominantly affecting individuals of African descent,1 including ~100,000 individuals in the United States (US)2. SCD leads to life expectancy 20-30 years less than the general population, with more notable decreases for those with sickle cell anemia (SCA), a more severe form of SCD.1,3,4 Families of children with SCD must manage varied, unpredictable care requirements spanning treatment administration (hydroxyurea, prophylactic penicillin, and sometimes hematopoietic stem cell transplant), symptom management (e.g., preventing and/or responding to pain crises), and ongoing surveillance to limit the development or progression of serious SCD complications.1 The significant responsibility of SCD management is stressful to parents,5 and parental stress and distress are associated with more frequent and intense pain episodes and complications, lower quality of life, worse functional disability, and higher healthcare utilization in children with SCD.6-8
Families’ experiences of SCD may be influenced by the social environment – the physical surroundings, social relationships, and cultural milieus within which people function and interact.9 Compared to other chronic diseases, individuals with SCD have less access to comprehensive and preventative care and more treatment barriers.4,10 They are more likely to be publicly-insured, which is associated with lower access to high-quality healthcare and poorer outcomes in the US.4,11 Medication barriers include under-prescription by physicians, difficulty obtaining refills, the need for follow-up monitoring visits, high deductibles, denied pre-authorization requests, and fears about side effects.4,12,13 Opioids are first-line treatments14 but are associated with stigmatization, denied treatment, and drug-seeking presumptions by providers.4,15-17 These systemic barriers contribute to estimates that less than one-quarter of individuals with SCD receive standard-of-care treatment.18,19
Due to the disproportionate prevalence of SCD among Black individuals, the chronic burden of managing and coping with SCD is amplified by the historical and enduring context of structural, interpersonal, and internalized racism within the US.20,21 In addition to lower access to high-quality healthcare, Black children are more likely to experience poverty, unsafe neighborhoods, poorer schools, and unmet basic needs.22 Together, these sociocultural and structural factors comprise social determinants of health (SDoH) – the circumstances in which children are born, live, and age.23 SDoH may have a greater influence on health than medical care, accounting for up to 80% of health outcomes.24-26 A recent scoping review of SDoH and SCD (N=59 studies, 68% in the US, 51% pediatric) documents associations between SDoH and SCD but highlights significant knowledge gaps regarding the specificity and nature of these associations.27
The confluence of high medical needs and adverse SDoH, including racism, may amplify the burden of SCD on families. Despite a surge of interest in SDoH,27 there remains an incomplete understanding of the processes through which SDoH influence disease management and outcomes. The current study is grounded in two frameworks. The Pediatric Self-Management Framework emphasizes the behavioral aspects of managing pediatric illness (e.g., adherence to medical recommendations) and acknowledges the family’s central role.28 The World Health Organization (WHO) Framework for Action on SDoH highlights intermediary determinants of health including material circumstances (e.g., living and working conditions), behaviors, and psychosocial factors.29,30 Specifically, this qualitative study focused on children with SCA and aimed to clarify (a) the processes through which pediatric SCA disease management and SDoH interact, (b) how parents/caregivers manage these simultaneous demands, and (c) ways to mitigate the deleterious effects of adverse SDoH on SCA management. A better understanding of the processes linking SCA and SDoH will inform policies and interventions to address SDoH and promote SCA management.
Methods
This analysis is part of a larger study examining the implementation of an SDoH intervention within pediatric hematology settings.31 Current study participants were recruited from control sites and therefore did not receive SDoH screening/referral beyond the standard of care. Findings are presented according to the Standards for Reporting Qualitative Research.32
Participants & Recruitment
Parents/caregivers were recruited from two urban hematology departments within children’s hospitals in the Northeast US. Inclusion criteria included being ages ≥18 years, speaking English fluently, and identifying as the parent/primary caregiver of a child with SCA (HbSS or HbS-beta zero) aged 0-12 years who was prescribed daily penicillin or hydroxyurea. Both clinics prescribe hydroxyurea for all children with SCA as disease-modifying therapy, rather than waiting for symptoms to develop. There were no exclusion criteria.
During routine clinic visits, clinic or research staff approached families and shared fliers to guide conversations inviting participation. Parents/caregivers provided consent for clinic staff to share contact information with researchers, who reached out via telephone or text to provide study details, ascertain eligibility, and schedule data collection. Consistent with purposive sampling, participant sociodemographics were periodically reviewed, and subsequent outreach targeted families with characteristics under-represented in the sample to ensure breadth across child age and gender. Data collection continued until thematic saturation was reached (i.e., additional interviews did not yield unique information).33
Quantitative Measures
Unmet basic needs were measured using items from the Children’s HealthWatch survey34 (Table 1), a validated questionnaire that has been widely-used among racially- and ethnically-diverse individuals. Four items from the Children’s HealthWatch assessed energy insecurity, including risk of utility shut-off. The two-item Hunger Vital Sign35 assessed risk for food insecurity. Three items from the Housing Stability Vital Sign36 assessed risk for displacement and homelessness. Across all three basic needs measures, a positive endorsement of any item(s) indicates risk.
TABLE 1.
Items and outcomes regarding basic needs
| Basic Needs Measures & Items* | Endorsement of Risk Item (n; %) |
Meets Risk Criteria (n; %) |
|---|---|---|
| Hunger Vital Sign35 | ||
| Within the past 12 months, we worried whether our food would run out before we got money to buy more.** | 11 (42.3%) | 11 (42.3%) |
| Within the past 12 months, the food we bought just didn’t last and we didn’t have money to get more.** | 7 (26.9%) | |
| Housing Stability Vital Sign36 | ||
| During the past 12 months, was there a time when you were not able to pay the mortgage or rent on time? | 13 (50.0%) | 16 (61.5%) |
| In the past 12 months, how many places has the child lived? (3+ residences = positive for risk item) | 3 (11.5%) | |
| Do you and [child’s name] currently have a steady place to sleep at night? (no = positive for risk item) | 0% | |
| Energy Security34 | ||
| During the winter, were there any days that your home was not heated because the bills were not paid? | 1 (3.8%) | 5 (19.2%) |
| During the summer, were there any days that your home was not cooled because the bills were not paid? | 1 (3.8%) | |
| Over the past year, did the water company shut off the water in the house because the bills were not paid? | 4 (15.4%) | |
| Over the past year, did the electric company shut off the elecricity in the house because the bills were not paid? | 4 (15.4%) | |
| Combined Risk | ||
| Meets criteria for ≥1 risk area(s) | 19 (73.1%) | |
| Meets criteria for ≥2 risk areas | 11 (42.3%) | |
| Meets criteria for 3 risk areas | 2 (7.7%) | |
Responses of “yes” were coded as positive endorsement of the risk item, unless otherwise indicated
Responses of “often true” and “sometimes true” were coded as positive endorsement of the risk item; responses of “never true” and “don’t know” were coded as non-endorsement of the risk item
A background survey captured sociodemographic and SCA-related information including age, gender, race/ethnicity, insurance, education, and health concerns.
Qualitative Interviews
A semi-structured interview guide (Appendix) began with broad questions to characterize participants’ social environment including family, work, and neighborhood. Participants were asked to reflect on how aspects of their social environment affected and were affected by SCA management. The interview also included questions about SCA presentation, treatments, treatment barriers, and ways to mitigate these barriers. Throughout data collection, preliminary and emerging findings were periodically summarized to inform whether saturation was reached in primary research questions33 and to highlight remaining unanswered questions. Qualitative interview guides were iteratively updated to de-emphasize questions corresponding to saturated themes and emphasize questions regarding unsaturated themes.
Data Collection
Data were collected between March 2020 and January 2021. After obtaining informed consent, semi-structured interviews were conducted by two doctoral trainees (AB, JE) and one psychologist (CA). Interviews lasted ~75-minutes and occurred via Zoom. Interviews were audio-recorded and transcribed verbatim; two participants declined audio-recording. Quantitative surveys were administered via REDCap. Participants were compensated $50. The study was approved by the Boston Children’s Hospital Institutional Review Board.
Data Analysis
Qualitative interviews were transcribed verbatim, except for two non-recorded interviews for which detailed notes were taken. Transcripts or interview notes were deidentified, checked for accuracy, and entered into NVivo 12.37 A detailed coding structure was developed both deductively (based on a priori research questions and guiding frameworks) and inductively (to incorporate emerging findings). The coding structure included the name and operational definition for each code, including exceptions and examples. Eight transcripts were coded as a group to increase the clarity and specificity of the coding structure, foster its consistent application across coders (AB, JE, CA), and incorporate codes to capture emerging findings. The coding structure was considered final once no new codes were added or revised. All transcripts were (re)coded using the final coding structure. Twenty-three percent of transcripts were double-coded to confirm acceptable inter-coder concordance (i.e., the number of concordant codes divided by total number of codes in each transcript).38 Discrepancies were discussed by the analysis team (AB, JE, CA, KL) until consensus was reached.
Consistent with the aim of understanding the processes linking SDoH and SCA management, qualitative data were analyzed using applied thematic analysis,39 which involves initial familiarization with the data, systematic coding (i.e., assigning concise labels to chunks of text), and developing, refining, and defining semantic and latent themes.
Descriptive statistics (means, standard deviations, and/or frequencies) were calculated for quantitative data using SPSS.
Positionality Statement
The research team includes doctoral-level researchers, clinicians, and trainees across clinical psychology, medicine, and public health. Professional expertise spans pediatric SCD, health equity, SDoH, and family-centered care. Approximately one-half of the team has clinical experience caring for children with SCD. No authors have lived experience of SCD, though several authors have immediate family members with serious pediatric medical conditions. Authors identify as Black, white, and Asian; cis-gender male and female; and LGBTQ and heterosexual. Authors involved in qualitative interviewing and analysis had no prior relationship with participants.
Results
The sample was predominantly Black, female, and publicly-insured (Table 2). Seventy-three percent of participants reported at least one unmet basic need, including food insecurity (42%), housing instability (62%) and energy insecurity (20%; Table 1). Three qualitative themes were identified (Figure 1). To illustrate representative patterns in the data, exemplar quotes appear in Tables 3-5.
TABLE 2.
Participant Characteristics (N = 27*)
| Caregiver | Child | |
|---|---|---|
| Age, years, mean (SD) | 35.7 (8.1) | 5.6 (4.2) |
| Gender, n (%) | ||
| Female | 23 (88.5) | 12 (46.2) |
| Male | 3 (11.5) | 14 (53.8) |
| Country of birth, n (%) | ||
| USA | 15 (57.7) | 23 (88.5) |
| Other | 10 (38.5) | 3 (11.5) |
| Not reported | 1 (3.8) | 0 |
| Race, n (%) | ||
| Black/African American (including Haitian) ** | 24 (92.3) | 24 (92.3) |
| Not listed | 1 (3.8) | 1 (3.8) |
| More than one race | 1 (3.8) | 1 (3.8) |
| Ethnicity, n (%) | ||
| Hispanic/Latinx | 1 (3.8) | 1 (3.8) |
| Health Insurance, n (%)¥ *** | ||
| Public | 15 (57.7) | 19 (73.1) |
| Private | 9 (34.6) | 6 (23.1) |
| None | 2 (7.7) | 1 (3.8) |
| Medical Diagnoses, n (%)¥ | ||
| Asthma | 3 (11.5) | 2 (7.7) |
| Sickle cell disease | 1 (3.8) | 26 (100) |
| Cardiac | 1 (3.8) | 0 |
| Endocrinologic | 2 (7.7) | 0 |
| Hematologic | 0 | 1 (3.8) |
| Neurologic | 1 (3.8) | 1 (3.8) |
| Orthopedic | 1 (3.8) | 0 |
| Psychiatric | 2 (7.7) | 1 (3.8) |
| Attentional | 0 | 2 (7.7) |
| Caregiver type, n (%) | N/A | |
| Mother | 22 (84.6) | |
| Father | 3 (7.7) | |
| Grandmother | 1 (43.8) | |
| Marital status, n (%)¥ | N/A | |
| Single | 14 (53.8) | |
| Married | 8 (30.8) | |
| Separated or Divorced | 3 (11.5) | |
| Highest year of school completed, n (%)¥ | N/A | |
| High school graduate or GED | 2 (7.7) | |
| Vocational, trade, or business school program | 4 (15.4) | |
| Some college credit, but no degree | 6 (23.1) | |
| Associate’s degree | 4 (15.4) | |
| Bachelor’s degree | 7 (26.9) | |
| Master’s degree | 2 (7.7) |
One participant was a second caregiver for the same child and therefore did not contribute unique background data
One respondent specified their race as “Haitian” when given the “write-in” option
One family was double insured
Health insurance, medical diagnoses, marital status, and school completed collected for 25 participants (one participant left some background questions blank)
FIGURE 1.
Thematic Map of Findings
TABLE 3.
Exemplar Quotes for Theme 1: SCA Management is Bidirectionally Linked with the Social Environment
| Theme Description | Exemplar Quotes | |
|---|---|---|
| Challenges of SCD management can hinder basic needs from being met |
|
I think I was spending about – traveling from [Southeast Massachusetts] to Boston – $250-something a month. I'm not kidding. It was horrible. And that was taking away from the amount of food I could buy. That was taking away from the stuff that we needed on a day-to-day basis, 'cause children get hurt all the time so you always gotta keep your first aid kit, stuff like that. It was taking away from a lot of stuff and it was taking away from me being able to pay off my credit. And like, you know, it was horrible. We didn't get a car until a week after her second pain crisis… before that, we didn't have a car, and it was really hard to go into the ER as many times as we had to because we didn't have a car. So, it was really expensive you know, with the taxis and the Ubers. And as much as my Mom wanted to bring us, my Mom lives in [town in MA] and works everyday so it's like, and we don't have anybody else who we can rely on…. [Currently], she's had like two or three appointments in one week, and we have to pay parking every time that we have to go. And although it may not seem like a lot… that's money that we have to – that we usually don't have that we have to find. Even with my insurance, I have to put aside an equivalent of $200 every month for just medications. And that's just for Hydroxyurea. Out of pocket deductible is $10,000 this year alone, that's already been paid. And I'm just like, "What the hell?"… And then there's still bills coming in from [hospital]. I'm like, "How? I have insurance?" So the bills actually, in all honestly, they get paid when they can… At first, [child]'s medicine was not covered by insurance, because it’s a compound medicine - we had issues with that, so I was having to pay out of pocket.…I rather get his medicine than pay my rent here.… if [child] has a crisis, I'm out of commission. 'Cause everything stops. That's my income. Now, that money that I'm budgeting – could be going to a light bill, or it could be going to this or that. Then it's like, "Well, I missed this work 'cause [child] was sick. Now I have to make up for it. How am I gonna pay this bill?" |
| Unmet basic needs and financial hardship hinder SCD management |
|
Kids in a hospital - it does take toll on the family, especially when the parents have to be in and out of the hospital a lot of times, and either to work – especially with a single parent – or has other kids… You're thinking about how to survive. And, how to survive, like, you know, financially. So, it's not like – you're not giving that child 100% that you should, because you're thinking about how you gonna come up with payments, you know, for bills. Hospital bills, for your other children, a place to live, how to pay your, your other bills. You know, if that child is not getting that attention that she's supposed to – you know, as a parent that you're supposed to be giving… It's like you've got, like, competing things almost. You get overwhelmed, you get tired. Yeah, it’s bad. When she is sick and does have to stay in the hospital, [I have] to leave her to go to work. Um, I always call out the first day, but she always had to stay three days. So, the next two days I would definitely have to leave her to go to work. So leaving her in the hospital by herself… Being able to say, "oh I can't [go to work], I'm not going to work for three days,” – I can't do that. One day I didn't have, um, penicillin and then my car, the car that I have was broke down all night and [I was] not able to go get the medicine. And then they didn't do delivery. Then I keep him without penicillin for about three to four days. After that, he got fever. And then I was – I feel bad. I feel really, really bad. The goal would be to have the bone marrow transplant with a sibling match, but you need the in-house services in order to, kind of, properly care, um, for [him] - I need the in-house services. I need the adequate housing. So, I need all those resources we talked about, in order to be safe for him to go to the transplant. And so he can't have the transplant until that happens. If you had to deal with trying to figure out how your family's going to eat – you know, staying on top of their medicine regimen or, um, making sure you're at doctor appointments probably wouldn't be priority anymore. When you're happy and you're balanced and you're not stressed out and you don't feel like you have a billion things that you just can't manage – you're open to a lot more things. Especially if they say that we're having a class on education on sickle cell, you're gonna show up. Because you wanna learn, because your mind space can absorb it, because you're not stressed out about the ten million things you have to do. And if your child had an additional appointment, it's not like, "Oh gosh, I had another appointment." It's more like, "Okay, let's go." Because it doesn't feel like an additional burden. Because other things in your life have been taken care of. Because you're not feeling the burnout. And it's the burnout that is hindering people. You can only do so much when you're burnt out, and sometimes you can't do a single thing. |
TABLE 5.
Exemplar Quotes for Theme 3: Addressing families’ material, emotional, and informational needs may improve SCD management
| Theme Description | Exemplar Quotes |
|---|---|
|
A financial burden on top of raising a sick kid, it's stressful. It's very stressful. So I feel like if some parents had help in those areas, whether it's help with the housing, help with the utilities or bills, or help with finding a job. If we could improve those three areas, I feel like parents would have more time on how to run their household and what helps their child thrive. [It would be important to help families with] housing, most importantly. Transportation, that's a key thing. Mental and emotional well-being, because being a parent of a child that has sickle cells disease, your mental can go haywire. You will stress yourself out with so much worry and so much, "Am I doing this right? Am I doing that?" It's a lot of stress, because I was constantly worried about my son passing away on me. That was my biggest worry. Something's gonna happen, he's gonna die, it's going to be totally my fault, because I don't know what I'm doing. You've gotta get yourself to that calm place, and sometimes you need a little extra help to keep you there… And of course, if they can send you off to a food pantry or something like that if you don't have enough food, like that's very helpful… Some people are too proud to do that type of stuff, but sometimes you need that stuff… [accepting help] makes you a better parent, it makes you a stronger parent. It's a pride thing… It's hard for me to say, like, "I need help” or “I need support…” Maybe ask people what they need. Maybe doing it on a survey, or some sort of electronic or paper, ‘cause maybe people will… feel more comfortable answering that way instead of speaking with someone. I think sometimes people are embarrassed. if it's something that they need, they may be reluctant to say it to someone. As a parent, you're already stressed and trying to provide for the kids. And then you, now you have to provide for a child who is sick, who needs a lot more of your time and attention. So to have a program that is helping you with basically necessities of life, like rent and food and those kind of things, kinda take the weight off your shoulders just a little bit. It then gives you more wiggle room to then be able to be better parents for your kid that's sick. |
SCA management is bidirectionally linked with the social environment
Challenges of SCA management can hinder basic needs from being met
Parents/caregivers emphasized how their responsibility for managing time-consuming, unpredictable aspects of SCA affects employment and finances. They described missing work for routine clinic visits and unplanned emergency department visits and hospitalizations, especially those stemming from pain crises, which affect work attendance, productivity, and compensation. Financial effects are amplified for single parents and for those with hourly jobs or self-employment who do not get paid when they miss work. Repeated SCA-related work disruptions can lead to termination, further exacerbating financial instability.
Beyond lost wages, parents/caregivers described “crushing” costs associated with gaps in insurance coverage including out-of-pocket expenses for non-covered medications, deductibles, co-insurance, and co-pays. Similarly, parents/caregivers estimated that parking and transportation costs to/from healthcare facilities could exceed $250 per month. Additional SCA-related costs include ensuring adequate nutrition and hydration, finding accessible housing, or paying for parking to decrease children’s exposure to extreme hot or cold temperatures. SCA-related financial burden was emphasized across participants’ income, education, and employment levels, with many parents/caregivers reporting ongoing struggles with debt, collections, and credit.
Parents/caregivers described tough day-to-day choices about how to obtain and use their limited resources. Financial strain that is precipitated or exacerbated by SCA management may require families to choose between medical care and basic needs, such as buying food, paying rent or utility bills, or filing immigration paperwork. Beyond finances, families face additional incompatibilities between medical and basic needs. For example, remaining with their child during inpatient hospitalizations violates homeless shelter rules requiring people to return each night. Together, prioritizing medical care can threaten food, energy, and housing security.
Unmet basic needs and financial hardship hinder SCA management
Unmet basic needs and associated stressors can limit parents’/caregivers’ abilities to manage SCA treatment consistently and effectively and reduce SCA-related sequelae. Regarding financial strain, the high cost of appointments (transportation, co-pays, lost wages, etc.) can lead families to forego routine appointments and lab work to save money and/or time, and instead adopt more reactive approaches to seeking care when SCA-related problems arise. Gaps in insurance coverage can stop families from administering necessary medications. Inconsistent access to reliable transportation can lead to missing appointments and not (re)filling prescriptions. Without consistent electricity/energy, families cannot refrigerate medications such as hydroxyurea or control temperature through heating or cooling, thereby triggering or exacerbating pain crises. Without adequate housing, children may be denied bone marrow transplants due to the inability to accommodate post-transplant in-home services. Finally, high psychological stress and burden from managing SCA while attending to the family’s basic needs can lower adherence to recommended medications, healthcare visits, and lab work. These challenges are compounded for parents/caregivers who are undocumented, have limited English proficiency, or have limited social support. Although parents/caregivers generally discussed challenges associated with unmet basic needs, the opposite also was articulated: more-resourced participants explained how having resources and feeling stable allowed them to prevent and respond to their child’s medical needs more effectively.
Parents/caregivers are faced with difficult choices
Parents/caregivers described actively constructing their social environments to accommodate SCA management, necessitating difficult decisions about housing, neighborhoods, schools, and employment. When seeking housing, parents/caregivers carefully consider advantages and disadvantages of various living situations. Many participants, particularly those without access to a dependable car, emphasized the benefits of proximity to hospitals and/or specialty pharmacies to ensure that emergent medical needs are addressed without relying on time-consuming, often-unreliable public transportation. Parents/caregivers explained that quicker response to medical needs led to better SCA outcomes. This proximity became more salient when families were less comfortable using public transportation during COVID-19. However, the benefits of living near the hospital were offset by undesirable aspects of the surrounding neighborhoods, including safety concerns, less space, and limited power over property owners to address unsafe living conditions (e.g., mold, poor air quality, predatory neighbors). Families who chose suburban housing described being further from the hospital but also having lower cost of living and better schools, including school nurses to oversee 504 plans. Although cost of living was salient across study sites, Boston-based parents/caregivers emphasized their desire to move out of Massachusetts due to the high cost of living but stayed because of perceived better healthcare quality.
Parents/caregivers described a similar decision-making process regarding employment. They prioritized flexible work schedules, remote work options, and supportive bosses, which together could enable stable employment despite repeatedly missing work for planned or unplanned medical situations. However, these favorable work conditions were often unattainable. Parents/caregivers described tension between needing time off versus not wanting to be perceived as uncommitted or unreliable. They described a general lack of understanding from employers regarding the severity and unpredictability of SCA and feared losing their jobs. Few parents/caregivers had the option of flexible hours, and SCA-related work disruptions precluded them from establishing trust or demonstrating reliability for employers to even consider flexible hours. Although self-employed parents/caregivers had more flexibility to set their hours and miss work when necessary, this flexibility was offset by lost wages when not working. The net result was that many parents/caregivers needed to choose between providing optimal medical care versus maintaining steady employment and financial stability.
Although the importance of centering SCA when choosing housing and employment was broadly represented across participants, many families lacked the resources to make choices consistent with their preferences. Across different housing and employment situations, participants described active, ongoing efforts to reduce negative impacts of the family’s living situation on SCA management or outcomes. For many families, this means prioritizing medical needs over other basic needs.
Addressing families’ material, emotional, and informational needs may improve SCA management
Although balancing SCA management with other responsibilities would remain challenging, parents/caregivers noted how support meeting basic needs and managing associated stress would allow them to better attend to and follow SCA-related recommendations. They emphasized the primary importance of mitigating financial concerns, including those stemming from medical costs and lost wages, and also requested help meeting needs related to housing, transportation, energy, food, clothes, holiday gifts, insurance, school (e.g., information and skills to advocate for accommodations), and emotional wellbeing. They acknowledged the importance of screening for basic needs to individualize service recommendations and emphasized the essential need to follow up by connecting families with resources.
Parents/caregivers described the current process for requesting services, resources, and/or supports as complex, time-consuming, and drawn-out. They requested assistance to understand what services exist, connect with emotional and practical supports, and navigate barriers to service receipt, such as falling outside income eligibility ranges or lacking immigration documentation. They suggested that social workers are well-positioned to provide emotional and practical support. Parents/caregivers emphasized the interpersonal aspects of SDoH disclosure and expressed reluctance to request or receive assistance. Barriers include pride, desire for privacy, and variable levels of trust in healthcare providers. They highlighted the importance of positive, trusting relationships with the healthcare team to lessen perceptions of being judged and increase their likelihood of requesting and accepting assistance to address adverse SDoH.
Discussion
Despite documented associations between SDoH and health, there remains a poor understanding of the processes through which SDoH affect health outcomes. To address this gap, the current study found that parents’/caregivers’ abilities to effectively manage SCA both affects and is affected by the social environment. Specifically, SCA management can hinder basic needs from being met, and unmet basic needs interfere with SCA management. With limited resources, these competing demands require parents/caregivers to confront difficult choices between basic versus medical needs. Addressing material, emotional, and informational needs may improve SCA management.
Consistent with the WHO Framework for Action on SDoH,29,30 the current study showed how intermediary determinants of health (material circumstances such as living and working conditions) relate to behavioral and psychosocial factors. Findings also align with the Pediatric Self-Management Framework,28 which emphasizes families’ management of chronic illnesses, with important implications for adherence to treatments that can reduce morbidity and increase life expectancy. A review and meta-analysis of 49 studies revealed wide variation in adherence rates in pediatric SCD, depending on the specific medication and measurement method (e.g., subjective adherence was higher than objective measures).40 Regarding correlates of SCD treatment non-adherence, they found moderate effect sizes for medication barriers (e.g., forgetting, caregiver too busy, medication ran out), and smaller effects across most demographic characteristics, psychosocial factors (e.g., parental coping), and disease knowledge.40 Current findings complement previous research40 by exploring how treatment barriers limit adherence.
Regarding treatment, hydroxyurea is associated with better health outcomes and fewer hospitalizations,41 but current findings reveal increased burdens with its use including missed work and transportation costs to attend monitoring visits, need for specialty pharmacies (hydroxyurea is a chemotherapeutic agent), and increased co-pays. Thus, families face trade-offs between these predictable hydroxyurea-related burdens versus unpredictable, painful, and costly pain crises.
Although links between SDoH and illness management are likely applicable across pediatric conditions, these associations may be compounded by systemic racism affecting individuals with SCD in the US, including cycles of poverty that disproportionately affect Black individuals.42 A recent qualitative analysis from the current project elucidated parent/caregivers’ and healthcare staffs’ perceptions of how aspects of the healthcare system (e.g., racism toward Black individuals, providers’ inadequate SCD knowledge, SCD stigma) contribute to challenging interpersonal interactions with healthcare providers and lead to race- and SCD-based discrimination.21 These race-based inequities reflect a broader discounting of SCD in research and clinical initiatives.1 For example, research funding for cystic fibrosis was 10 times greater than that for SCD in 2020, despite SCD having a prevalence >3 times larger.43 Healthcare indicators are similarly concerning; many individuals with SCD lack access to comprehensive and/or preventative care4 or physicians with specialized SCD knowledge,4,10 and only one-quarter receive standard-of-care hydroxyurea treatment.18,19 Together, the confluence of adverse SDoH, high SCD-related costs, and longstanding racism highlights the exceptional burden faced by individuals with SCD.
To disrupt cycles of inequity, screening for and addressing adverse SDoH are recommended by numerous professional societies, including the American Academy of Pediatrics.44,45 Recommendations include direct, high-involvement strategies (e.g., social workers helping families access services) and indirect, low-involvement strategies (e.g., providing resource sheets).46 One example of an indirect, low-involvement strategy is WE CARE, an SDoH screening-and-referral system associated with increased referrals and resources to address adverse SDoH within pediatric primary care.47,48 A recent quality-improvement initiative examined the feasibility of implementing WE CARE in pediatric hematology clinics within a public safety-net hospital.49 Of 156 screens completed (58% of those eligible), 66% included ≥1 unmet need, and 80% were referred for community resources. Similarly, parents/caregivers in the current study indicated that screening and intervening regarding adverse SDoH may mitigate the detrimental effects of unmet basic needs and financial instability on health outcomes. However, they emphasized that screening should be done with sensitivity to privacy, pride, and trust, and only if referrals/resources are available.
The effectiveness of strategies to mitigate SDoH may be limited without larger, systems-level changes. For example, reduced race- or disease-based discrimination may improve healthcare experiences and outcomes. Inequities also may be reduced via improved SCD training, especially for emergency department providers who are often the first point of contact. The Emergency Department Sickle Cell Care Coalition50 created a point-of-care tool to guide sickle cell treatment (https://www.acep.org/patient-care/sickle-cell/). To support children within their immediate environments, hospital-based SDoH programs and school partnerships could be expanded and delivered more equitably and empathically.51 Finally, creation of a national surveillance system to inform healthcare resource allocation and research gaps may improve access to care (e.g., via coordinated care models).4
Several methodological considerations are noteworthy. We enrolled children with SCA exclusively, so generalizability to other forms of SCD remains unknown. The sample came from two urban hospitals in New England, and 73% endorsed ≥1 unmet basic need(s). Processes linking SDoH and SCD may differ globally or for rural families in the US who face different barriers to care. As the sample was English-speaking, barriers may be even more pronounced for those with limited English proficiency. Developmentally, findings relate to parents’/caregivers’ management of children’s SCD; interrelationships between SDoH and SCD during adolescence and adulthood remain unexamined. Finally, data collection after COVID-19 onset may have increased the salience of treatment barriers and difficult choices between disease management and basic needs.
In conclusion, findings underscore how day-to-day conditions and financial hardship can undermine the management of SCA treatments, symptoms, and complications, thereby limiting treatment effectiveness. Understanding these processes may inform the development of family-centered, health equity interventions and policies to improve living conditions, disease management, and health outcomes.
TABLE 4.
Exemplar Quotes for Theme 2: Parents/Caregivers are Faced with Difficult Choices
| Theme Description | Exemplar Quotes |
|---|---|
|
It's like a bondage when I'm stuck having to play the case manager, the advocate, the nurse, the doctor, the mother, the administrator. You know what I mean?… The amount of time and care it has taken me for [son with sickle cell]- where would I have the time to work? And that's just him. That's not even considering his sister and his brother, which makes it a whole other level, because what employer is gonna take you calling out almost every other day? If we look at his admissions and the frequency of his illness, and how much I've been called upon to medicate him around the clock on my own, without any support or VNA help, where would I be able to do that with an employer? So my unemployment is necessary to care for him… [but] it adds to my stress. I can't afford to have a job, because who's gonna care for the kids and do all the things I'm called upon to do for them? Especially when they're sick. The challenge is we wanted to be close enough to the hospital because of, uh, emergencies and whatnot. And, um, so being close to the hospital is important… Because then, if [son with sickle cell] is having a crisis, or his sister's having a crisis, or they have a fever, then I need to be able to jump at a drop of a hat and, um, grab all three to get to the hospital. Especially if it's something more critical like a fever, or a really bad pain crisis, because time is of the essence when they're having pain and when they have fevers. How quickly their pain is responded to appropriately makes all the difference in the world in terms of the length of stay in the hospital. So if they're delayed or they're not managed adequately with the pain, um, it escalates really quickly. A lot of the time, especially in the low economy bracket, parentshave tosacrifice whether they're going to pay their heat bill or their rent. I've literally seen it done a couple of times, not with my household but with other people's household, where they had to choose, am I going to pay these two [medical] bills or am I going to pay for rent? If something else has to go unpaid to make sure that his medication is obtained, or you know, there's food in the house - that something else just has to go unpaid, unfortunately. He comes first. So I have to make sure, whatever I need to do, I, I will get it done to make sure that he's provided for. |
Acknowledgements
The authors would like to thank the participating families and the outstanding team of research assistants who contributed to the completion of this work. This work was funded by the National Heart, Lung, and Blood Institute (R01 HL141774; PIs: Garg & Kavanagh).
Abbreviations
- SDoH
Social Determinants of Health
- SCA
Sickle Cell Anemia
- SCD
Sickle Cell Disease
- US
United States
- WHO
World Health Organization
APPENDIX. Semi-structured interview topics & example interview questions
| Topic | Example Interview Questions |
|---|---|
| Social Context |
|
| |
| |
| |
| SCD Description, Treatment, & Barriers |
|
| |
| |
| |
| |
| Making Connections between Social Context and SCD Management |
|
| |
| |
| |
| |
| |
| Addressing Barriers to SCD Management |
|
Footnotes
Conflict of Interest Statement
None of the authors have conflicts of interest to disclose.
References
- 1.Kavanagh PL, Fasipe TA, Wun T. Sickle cell disease: A review. JAMA. 2022;328(1):57–68. [DOI] [PubMed] [Google Scholar]
- 2.National Academies of Sciences, Engineering, and Medicine. Addressing sickle cell disease: A strategic plan and blueprint for action. National Academies Press; 2020. [PubMed] [Google Scholar]
- 3.Hamideh D, Alvarez O. Sickle cell disease related mortality in the United States (1999–2009). Pediatr Blood Cancer. 2013;60(9):1482–1486. [DOI] [PubMed] [Google Scholar]
- 4.Lee L, Smith-Whitley K, Banks S, Puckrein G. Reducing health care disparities in sickle cell disease: A review. Public Health Rep. 2019;134(6):599–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cousino MK, Hazen RA. Parenting stress among caregivers of children with chronic illness: A systematic review. J Pediatr Psychol. 2013;38(8):809–828. [DOI] [PubMed] [Google Scholar]
- 6.Barakat LP, Patterson CA, Weinberger BS, Simon K, Gonzalez ER, Dampier C. A prospective study of the role of coping and family functioning in health outcomes for adolescents with sickle cell disease. J Pediatr Hematol Oncol. 2007;29(11):752–760. [DOI] [PubMed] [Google Scholar]
- 7.Logan DE, Radcliffe J, Smith-Whitley K. Parent factors and adolescent sickle cell disease: Associations with patterns of health service use. J Pediatr Psychol. 2002;27(5):475–484. [DOI] [PubMed] [Google Scholar]
- 8.Sil S, Woodward KE, Johnson YL, Dampier C, Cohen LL. Parental psychosocial distress in pediatric sickle cell disease and chronic pain. J Pediatr Psychol. 2021;46(5):557–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casper M. A definition of “social environment”. Am J Public Health. 2001;91(3):465–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCavit TL, Lin H, Zhang S, Ahn C, Quinn CT, Flores G. Hospital volume, hospital teaching status, patient socioeconomic status, and outcomes in patients hospitalized with sickle cell disease. Am J Hematol. 2011;86(4):377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robinson MR, Daniel LC, O’Hara EA, Szabo MM, Barakat LP. Insurance status as a sociodemographic risk factor for functional outcomes and health-related quality of life among youth with sickle cell disease. J Pediatr Hematol Oncol. 2014;36(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brandow AM, Panepinto JA. Hydroxyurea use in sickle cell disease: The battle with low prescription rates, poor patient compliance and fears of toxicities. Expert Rev Hematol. 2010;3(3):255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Department of Health and Human Services. National Heart, Lung and Blood Institute. Evidence-based Management of Sickle Cell Disease—Expert Panel Report, 2014. 2018. [Google Scholar]
- 14.Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: Summary of the 2014 evidence-based report by expert panel members. JAMA. 2014;312(10):1033–1048. [DOI] [PubMed] [Google Scholar]
- 15.Freiermuth CE, Haywood C Jr, Silva S, et al. Attitudes towards patients with sickle cell disease in a multi-center sample of emergency department providers. Adv Emerg Nurs J. 2014;36(4):335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pack-Mabien A, Labbe E, Herbert D, Haynes J Jr. Nurses' attitudes and practices in sickle cell pain management. Appl Nurs Res. 2001;14(4):187–192. [DOI] [PubMed] [Google Scholar]
- 17.Labbé E, Herbert D, Haynes J. Physicians’ attitude and practices in sickle cell disease pain management. J Palliat Care. 2005;21(4):246–251. [PubMed] [Google Scholar]
- 18.Reeves SL, Tribble AC, Madden B, Freed GL, Dombkowski KJ. Antibiotic prophylaxis for children with sickle cell anemia. Pediatrics. 2018;141(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stettler N, McKiernan CM, Adejoro OO, Walczak NB. Proportion of adults with sickle cell anemia and pain crises receiving hydroxyurea. JAMA. 2015;313(16):1671–1672. [DOI] [PubMed] [Google Scholar]
- 20.Nelson SC, Hackman HW. Race matters: Perceptions of race and racism in a sickle cell center. Pediatr Blood Cancer. 2013;60(3):451–454. [DOI] [PubMed] [Google Scholar]
- 21.Blakey AO, Lavarin C, Brochier A, et al. Effects of experienced discrimination in pediatric sickle cell disease: Caregiver and provider perspectives. J Racial Ethn Health Disparities. 2022:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gee GC, Ford CL. Structural racism and health inequities: Old issues, new Directions1. Du Bois review: social science research on race. 2011;8(1):115–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1. Accessed February 27, 2023.
- 24.Magnan S. Social determinants of health 101 for health care: Five plus five. NAM perspectives. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hood CM, Gennuso KP, Swain GR, Catlin BB. County health rankings: Relationships between determinant factors and health outcomes. Am J Prev Med. 2016;50(2):129–135. [DOI] [PubMed] [Google Scholar]
- 26.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff. 2002;21(2):78–93. [DOI] [PubMed] [Google Scholar]
- 27.Khan H, Krull M, Hankins JS, Wang WC, Porter JS. Sickle cell disease and social determinants of health: A scoping review. Pediatr Blood Cancer. 2023;70(2):e30089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Modi AC, Pai AL, Hommel KA, et al. Pediatric self-management: A framework for research, practice, and policy. Pediatrics. 2012;129(2):e473–e485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Solar O, Irwin A. A conceptual framework for action on the social determinants of health. 2010. [Google Scholar]
- 30.Commission on Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health: Final report of the commission on social determinants of health. World Health Organization; 2008. [Google Scholar]
- 31.Loo S, Brochier A, Wexler MG, et al. Addressing unmet basic needs for children with sickle cell disease in the united states: Clinic and staff perspectives. BMC Health Serv Res. 2021;21(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. [DOI] [PubMed] [Google Scholar]
- 33.Morse JM. The significance of saturation. Qual Health Res. 1995;5(2)147–149. [Google Scholar]
- 34.Frank DA, Casey PH, Black MM, et al. Cumulative hardship and wellness of low-income, young children: Multisite surveillance study. Pediatrics. 2010;125(5):e1115–e1123. [DOI] [PubMed] [Google Scholar]
- 35.Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–e32. [DOI] [PubMed] [Google Scholar]
- 36.Sandel M, Sheward R, Ettinger de Cuba S, et al. Unstable housing and caregiver and child health in renter families. Pediatrics. 2018;141(2). [DOI] [PubMed] [Google Scholar]
- 37.QSR International Pty Ltd. NVivo qualitative data analysis software, Version 12. 2018. [Google Scholar]
- 38.Morse JM, Barrett M, Mayan M, Olson K, Spiers J. Verification strategies for establishing reliability and validity in qualitative research. Int J Qual Methods. 2002;1(2):13–22. [Google Scholar]
- 39.Guest G, MacQueen KM, Namey EE. Applied thematic analysis. Sage Publications; 2011. [Google Scholar]
- 40.Loiselle K, Lee JL, Szulczewski L, Drake S, Crosby LE, Pai AL. Systematic and meta-analytic review: Medication adherence among pediatric patients with sickle cell disease. J Pediatr Psychol. 2016;41(4):406–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization. Adherence to long-term therapies: Evidence for action. World Health Organization; 2003. [Google Scholar]
- 42.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: Evidence and interventions. Lancet. 2017;389(10077):1453–1463. [DOI] [PubMed] [Google Scholar]
- 43.Farooq F, Mogayzel PJ, Lanzkron S, Haywood C, Strouse JJ. Comparison of US federal and foundation funding of research for sickle cell disease and cystic fibrosis and factors associated with research productivity. JAMA Netw Open. 2020;3(3):e201737. [DOI] [PubMed] [Google Scholar]
- 44.Gitterman BA, Flanagan PJ, Cotton WH, et al. Poverty and child health in the United States. Pediatrics. 2016;137(4). [DOI] [PubMed] [Google Scholar]
- 45.Daniel H, Bornstein SS, Kane GC, Health and Public Policy Committee of the American College of Physicians. Addressing social determinants to improve patient care and promote health equity: An American College of Physicians position paper. Ann Intern Med. 2018;168(8):577–578. [DOI] [PubMed] [Google Scholar]
- 46.Beck AF, Tschudy MM, Coker TR, et al. Determinants of health and pediatric primary care practices. Pediatrics. 2016;137(3). [DOI] [PubMed] [Google Scholar]
- 47.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: A cluster RCT. Pediatrics. 2015;135(2):e296–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the management of family psychosocial problems at low-income children's well-child care visits: The WE CARE project. Pediatrics. 2007;120(3):547–558. [DOI] [PubMed] [Google Scholar]
- 49.Power-Hays A, Li S, Mensah A, Sobota A. Universal screening for social determinants of health in pediatric sickle cell disease: A quality-improvement initiative. Pediatr Blood Cancer. 2020;67(1):e28006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kavanagh PL, Hirshon JM. EDSC3: Working to improve emergency department care of individuals with sickle cell disease. Ann Emerg Med. 2020;76(3):S80–S82. [DOI] [PubMed] [Google Scholar]
- 51.Daly BP, Litke S, Kiely J, et al. Effectively supporting youth with chronic illness in schools: External partnerships and training recommendations. Pediatr Clin North Am. 2022;69(4):695–707. [DOI] [PubMed] [Google Scholar]