Abstract
Adverse reactions in tattooed skin during magnetic resonance imaging (MRI) are rare but well known. Previous reports describe sudden burning pain in tattooed skin, sometimes accompanied by mild erythema and oedema when entering MRI scanners. The pathophysiology remains unclear, but simple direct thermal heating can be excluded. It has been hypothesized that MRI-triggered torque and traction create neural sensations from magnetic pigment particles. However, this case enlightens yet another possible mechanism. We present a 35-year-old woman experiencing reoccurring stinging sensations in three decorative black tattoos just seconds after the initiation of the MRI. Single-blind tests with handheld power magnets or a dummy could reproduce painful subjective feelings in her tattooed skin. Similar events were provoked during re-evaluation with MRI. Surprisingly, chemical analyses and electron microscopy of skin samples revealed carbon black as the colouring agent – no iron-based solids were detected. Our case demonstrates that MRI tattoo reactions are not limited to magnetic contaminants alone. More distinct subgroups of MRI-induced reactions may occur. We hypothesize that radiofrequency induction of surface currents in black carbon particles adjacent to sensory axons in the dermis may lead to neurosensations.
Keywords: Magnet, Iron oxide, Tattoo reaction, Permanent makeup, MRI safety
Introduction
Magnetic resonance imaging (MRI) is a frequently used diagnostic tool to evaluate soft tissue structures. It has the past decades evolved with more advanced imaging techniques, stronger static magnetic fields, and greater radiofrequency transmissions. MRI-induced adverse reactions in tattooed skin have been sporadically reported in the medical literature over the past 30 years [1]. Fast onset of intense burning, smarting, or stinging pain has been described, occasionally followed by transient erythema and oedema when patients enter the static magnetic field or abruptly after the start of scanning [1]. Due to the subjective overlap, the reactions have been misinterpreted as thermal burns, comparable to those caused by coiled wires and sensor leads [1]. MRI-tattoo interactions are exceptional in decorative body tattoos but more frequent in cosmetic tattoos despite the smaller tattooed area, such as permanent eyebrows or eyeliner tattoos. MR images may show pigment-related artefacts. Inks used for cosmetic tattooing are often based on iron oxide pigments which match the natural skin colour tones, while those used for decorative body tattooing are usually organic pigments and carbon black [2]. The many aspects of tattooing, tattoo inks, and tattoo complications were recently reviewed [3–5]. We present the case of a young woman with immediate stinging and fiery pain in her decorative tattoos right after the initiation of the MRI scanning. Uniquely, in this report, a panorama of new and advanced methods in experimental dermatology is applied to skin samples and the suspected culprit ink, including testing of magnetic properties. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. Supplemental materials include the CARE Checklist.
Case Presentation
Patient History
A 35-year-old woman in general good health, height 164 cm, and weight 69.5 kg was referred to the “Tattoo Clinic” at Bispebjerg University Hospital in Denmark to rule out whether future MRI examinations were contraindicated. She had suffered a painful MRI-related adverse reaction in her tattoo, interrupting the scan procedure.
In 2018, the patient was referred for an MRI of the cerebrum because of sudden transient hemiparesis of unknown aetiology. Three minutes after the start of scanning, the patient experienced a sense of painful traction and vibrating sensations from her left flank, where a large black tattoo was placed. The scanning, however, could be completed. After the scanning, no inflammatory cutaneous reaction was noted in or around the tattoo. In 2019, the patient was admitted for MRI because of lower back pain. Eighteen seconds after the start of the overview scan, painful traction and vibration struck the left shoulder, flank region, and dorsal foot directly in her old, black tattoos. The pain disappeared, within seconds, as the procedure stopped. Fearing thermal skin burn, the staff stopped the MRI procedure and referred her to the “Tattoo Clinic”. Both MRI procedures were made with 1.5-Tesla clinical scanners. The three reacting tattoos were all in black/greyish colours and located on the left dorsal foot, flank, and shoulder. All tattoos were made by the same professional artist in 2011, with the same ink stock product identified as “Lining Black” by Eternal Ink, USA. The pigment was carbon black, as specified by the labelled CI number. The flank tattoo was composed of a flower with meandering lines and decorative leaves covering almost the whole region (see Fig. 1). On the dorsal foot, she had a heart-shaped linear tattoo 5 cm in diameter and, on the shoulder, some fine line lettering. All tattoos had no palpable skin thickening, papules/nodules, and no discolouration or blowout of the pigment. Due to tattoo ageing and some wash out of the pigment over time, the colour density in tattoos was rather low. The patient had nine other tattoos made by various tattooists, primarily red, green, and blue colours. None of these tattoos reacted during MRI.
Fig. 1.
Clinical photos of reacting tattoos on the flank (a) and the foot (b).
Clinical Experiment with Blinded Exposure to Strong Handheld Magnets
The patient was tested single-blind with magnets applied to her tattoos versus normal skin of the same body region. In a random order, her skin was exposed to handheld magnets of varying Tesla (T) strength (0.0009T, 0.3T, 0.4T, 0.5T) or a plastic dummy. No objective skin lesions occurred, but subjective sensations of torque and traction in her tattooed skin were reported. Sensations intensified with the increasing strength of the magnet applied. At 0.5 T, a push-away motoric manoeuvre was observed due to painful discomfort in the flank tattoo. Similar sensations were felt in the dorsal foot tattoo. A feeling of warmth in the tattoos after magnet exposure was noted, but no significant thermal difference was measured using a handheld thermography camera. No sensations occurred when using the dummy or when testing normal skin.
A 3-mm punch-out biopsy of the flank tattoo was placed in a transparent container filled with sterile saline water. While floating and in a mobile state, the tissue sample was exposed to a 0.5 T magnet. No move or pull effect was observed, indicating no magnetism of the sample. Five 3-mm punch-out biopsies were prepared for regular histology, metal analysis by mass spectrometry (inductively coupled plasma mass spectrometry [ICP-MS]), mass spectrometry imaging (laser ablation-ICP-MS), Fe-57 Mössbauer spectroscopy of iron-containing compounds, X-ray powder diffraction (XRD), and transmission electron microscopy (TEM).
Confirmative Magnetic Resonance Imaging
The patient was placed in a Siemens Magnetom Verio 3T clinical MRI scanner to verify the clinical observations. At first, her flank region was positioned for 5 min in the ISO centre and thus only exposed to the static magnetic field. No objective or subjective symptoms occurred. Then, MRI of the vertebral column was initiated, copying the patient’s scanning in 2019. The protocol included a scouting scan with the following parameters: TE: 3.69 ms, TR: 7.8 ms, flip angle: 20°, voxels: 1.5 mm × 1.2 mm × 6 mm (slice thickness). Four scans of 18 s were completed, but within 10 s of each scanning, a stinging sensation occurred in the dorsal left foot and the flank. No cutaneous erythema or oedema was observed. The patient tolerated 10 min in the MRI field with no interruption.
Chemical Analysis of Skin Biopsies from Tattoos
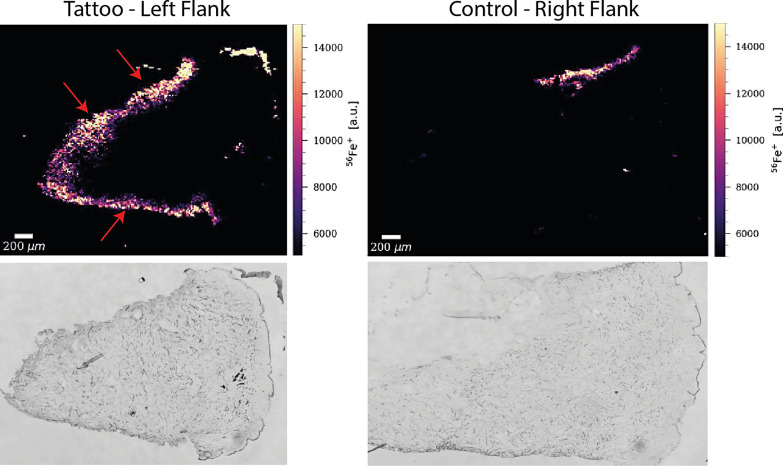
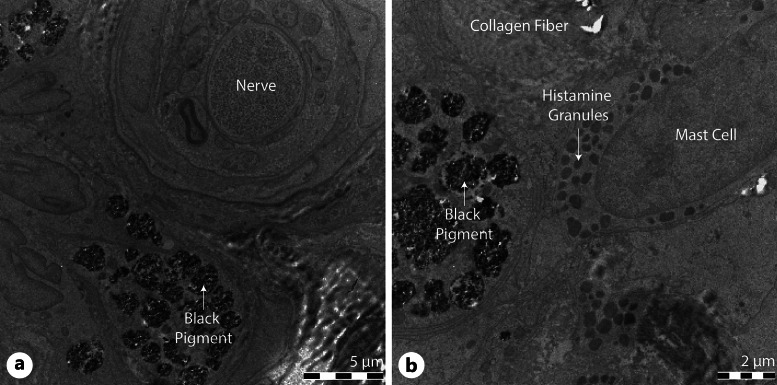
Routine histology of the tattooed skin showed a normal epidermis. The tattoo pigment extended halfway down the dermis with no signs of inflammation. An iron test by staining was negative, with no deposition of hemosiderin. ICP-MS found no significant difference in metals between tattooed and normal skin (see Table 1). Mass spectroscopy imaging (Fig. 2) showed metals only in the incision margins of the tissue samples, indicating metal contamination from the biopsy punch itself. Neither Mössbauer spectroscopy nor XRD could detect iron oxides. TEM showed no iron oxide crystals but only pigment clusters identical to carbon black particles (Fig. 3). Interestingly, aggregates of black pigment were found neighbouring peripheral nerves (Fig. 3a). Most of the pigment was located intracellularly, engulfed by macrophages, or interlaced with collagen fibres in the dermis layer, often accompanied by mast cells filled with histamine granules (Fig. 3b).
Table 1.
Element contents (mg/kg) in two samples of black inks manufactured by Eternal Ink, USA (product: Lining Black) and metals in tattooed skin (punch biopsy, flank left side, tattoo reacting on MRI) and normal skin from the same anatomical region, contralateral side
| Cr | Mg | Fe | Ni | Cu | Zn | Pb | Cd | |
|---|---|---|---|---|---|---|---|---|
| Tattoo ink, 2011 | 120 | 60 | 10,000 | 10 | 8 | I.D. | I.D. | I.D. |
| Tattoo ink, 2021 | 10 | I.D. | 850 | I.D. | I.D. | I.D. | I.D. | I.D. |
| Tattooed skin | I.D. | I.D. | 45 | 55 | I.D. | 10 | I.D. | I.D. |
| Normal skin | I.D. | I.D. | 95 | 75 | 30 | 10 | I.D. | I.D. |
Analysis performed by ICP-MS.
I.D., not detected.
Fig. 2.
Laser ablation-ICP-MS, punch biopsies, and cross-sectional imaging with the visualization of iron (Fe) distribution in the punches (epidermal surface to the right); left column: from the tattoo; right column: reference normal skin from the contralateral side. Red arrows indicate iron contamination of the tissue along the cutting line originating from the punch. Figures below show unstained tissue sections of the biopsy cores.
Fig. 3.
TEM of flank tattoo. a Black tattoo pigment clustered close to a peripheral nerve, with the axon seen in the centre of the nerve. Scale bar, 5 a.m. b Black tattoo pigment located close to a mast cell with densely packed granules in the cytoplasm. Scale bar, 2 μm.
Chemical Analysis of Tattoo Pigment
A sample of Eternal Ink “Lining Black” was found in stock in the Tattoo Clinic since 2011 and, according to the patient, identical to the ink applied (likely to be the same batch from the same supplier). In reference, a newly acquired batch (2021) of the same brand was available. From the labelling, the ink was composed of organic pigment, distilled water, alcohol, and witch hazel; colour index number 77266, e.g., carbon black. Before chemical analysis, droplets of each ink were placed in Petri dishes and tested for magnetic behaviour. No metal ball for stirring was found in the bottles. The 2011-ink product could be dragged freely around while moving a solid neodymium magnet underneath the dish, demonstrating the magnetic activity of the ink product assumed to be used for the original tattoo. No response was induced on the 2021-ink.
Mössbauer spectroscopy of the old and new ink samples revealed, exclusively for the 2011 batch, traces of maghemite (γ-Fe2O3) and minute amounts of magnetite (Fe3O4). ICP-MS showed a high concentration of iron in the 2011-ink sample contrasting with little iron in the 2021 batch, indicating iron oxide content in the old carbon black-dominated ink (see Table 1). Maghemite and magnetite in the old ink were considered processing/industrial contaminants due to their low concentration, but at a level that could explain the observed positive drag test of ink droplets in Petri dishes when exposed to powerful magnets. The structure of the dermis medium is entirely different from the Petri dish, e.g., packed with collagen fibres and mechanically robust with little space for free movement of particles.
Discussion
This is, to our knowledge, the 18th case report of MRI-induced tattoo reactions since the first report of burning pain and swelling in a dark blue permanent eyeliner in 1987 [6]. Sensory reactions in the tattoos were reproduced on re-examination with an MRI clinical scanner and single-blinded exposure to powerful handheld magnets or a dummy. In cosmetic tattoos, reports are associated with iron oxide pigments and metallic contaminants. Unexpectedly, in our case, no significant traces of metals or magnetic ingredients were detected in the skin samples, confirmed by different methods for metal analysis referenced to normal skin. Tattoos undergo ageing with washout of pigment, contaminants, and substances over time. More soluble substances are expected to be relatively short-lived in any tattoo. However, the ink sample from 2011 contained traces of maghemite and magnetite, which might explain the magnetic properties of the ink product when exposed to a strong magnet in the laboratory.
The age of the tattoo is a variable determining the severity of sensory events on MRI. Previously reported events occurred within a mean of 2.4 years after tattooing [1]. The pain with no objective skin symptoms that our patient experienced is likely to be dose-dependent and influenced by pigment washout from the tattoo over time. Black pigment in the ink bottle and the skin gradually undergoes agglomeration and aggregation, forming larger otherwise shaped clusters likely to have new properties such as altered electrical load, polarity, and conductivity [7]. Over time, the pigment density in a tattoo decreases due to macrophage scavenging, local chemical breakdown, and distribution to regional lymph nodes or the blood.
It has been assumed but not substantiated that MRI causes thermal heating directly in the tattooed skin with burning pain, erythema, and oedema [1, 8]. But no measurable increase in temperature after MRI can be confirmed in neither ex vivo nor in vivo experimental models [8, 9]. In our patient, no temperature increase in the tattooed skin after MRI was measured. The reaction is clearly non-thermal.
The sensation of burn is processed in the sensory cortex and communicated to the brain from the skin via unmyelinated dermal c-fibres [10]. A burn sensation subjectively can be triggered by non-thermal stimuli such as chemical etching, mechanical tissue traction, peripheral nerve damage, and even hypothermia or temperature shifts. Magnetic field gradients may induce electrical currents in the body, causing peripheral nerve stimulation with regional distribution and pain [11]. Repetitive transcranial magnetic stimulation is introduced in the management of treatment-resistant depression and other psychiatric disorders to supplement or replace electroconvulsive therapy [12]. In tattoos, the microanatomical closeness between tattoo pigment and the axon is the expected prerequisite for an MRI, pigment, and axon interaction to be possible. Figure 3a shows a TEM image of the tissue sample from the flank tattoo of our patient. Clusters of black tattoo pigment are found bordering a peripheral nerve fibre. This is an original finding, which to our knowledge no other studies have observed. Pigment particles neighbouring nerves may activate the axon through an electrical stimulus triggered by MRI. Carbon crystallized or layered as graphite is diamagnetic and an electrical conductor widely used in the industry. The carbon black raw material used in tattoo inks is amorphous if purity is high, but physical alterations happen over time.
Tattooed skin is known to have a lower threshold of pain. The neurosensory reaction of tattoos with severe, sometimes invalidating pain, despite no objective change of the tattoo or no identified external trigger, is a distinct type of tattoo complication [13, 14]. Allergic reactions to red pigment often have a surprisingly high level of pain and discomfort disproportionate to the size of the affected tattoo [13].
An intracellular tattoo pigment in mast cells loaded with histamine granules is illustrated in Figure 3b. Quivering pigment particles might provoke mast cells to degranulate and elicit local erythema and oedema, seen as a wheal-and-flare reaction. Such a mechanism is not realistic in our case since no triple response and no special itching occurred. No case of MRI-induced itching or wheal and flare has been noted in the literature. Acute and chronic urticaria independent of external stimuli is a known adverse event from tattooing, however, a separate entity [14]. MRI-induced release of reactive oxygen species is plausible since reactive oxygen species can cause sudden, severe pain with or without associated inflammation; erythropoietic protoporphyria and other conditions with abnormal sun sensitivity demonstrate this.
The tattoo ink sample from 2011 contained only small amounts of iron oxides, maghemite, and magnetite, contrasting the convincingly strong magnetic draw effect of the ink exposed to a powerful magnet when studied in a Petri dish. It is likely that maghemite, if present in the original tattoo, was eliminated from the tattoo within a few years. Observed draw effects on the 2011 ink may be caused by magnetic iron contamination or carbon black crystallization in the direction of graphite that may result in upcoming electrical properties as the typically amorphous raw material undergoes physical changes. The same change over time might happen with the black pigment inside the skin and explain our case's unusual reaction in black tattoos. A recent study investigating commonly used cosmetic inks formulated with iron oxide pigments identified magnetite as the responsible ingredient behind the magnetic properties and MRI responsiveness of these inks (data under publication). In nature, the rock mineral maghemite is formed by topotactic oxidation from magnetite, known as maghemitization. This oxidation is often incomplete, resulting in the coexistence of magnetite and maghemite [15]. These contaminants may be challenging to avoid in iron oxide pigments used in tattoo ink production.
In conclusion, this unique case report of MRI-induced neurosensory reactions in decorative black tattoos demonstrates that MRI reactions are not limited to cosmetic tattoos, iron oxide pigments, or their magnetic contaminants. The pain with sudden onset and no associated inflammatory response is hypothesized to be due to peripheral nerve stimulation through radiofrequency induction of surface currents in carbon black particles located close to sensory axons of the dermis. This might be slightly enhanced by alteration of the originally amorphous structure of the carbon black pigment in the direction of layered or crystallized graphite. The latter process is suggested by the images, but its mechanism is unclear. MRI-induced painful reactions in black tattoos made with carbon black pigment can be categorized as a unique clinical type under neurosensitive tattoo reactions. The decision to discontinue an MRI should be assessed on a case-by-case basis weighed by the diagnostic value of the scanning, as reported events are ranging from mild sensations to severe burning pain without any permanent damage to the skin [1].
Statement of Ethics
Written informed consent was obtained from the patient to publish this case report with clinical photos. Ethical approval is not required for this study in accordance with local or national guidelines.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors received no financial support for this article's research, authorship, and publication.
Author Contributions
Kasper Køhler Alsing: contribution in conception, patient consultations, work design, data analysis and interpretation, the primary writer of the manuscript, journal submission, and publication. Ole Olsen: chemical analysis with ICP-MS, drafting the work, revision, and intellectual content. Christian Bender Koch: chemical and mineralogical analysis by Mössbauer spectroscopy and XRD, drafting the work, revision, and intellectual content. Rasmus Hvass Hansen: MRI scanning and advice, drafting the work, revision, and intellectual content. Daniel Pergament Persson: preparation of tissue samples and analysis with LA-ICP-MS, drafting the work, revision, and intellectual content. Klaus Qvortrup: professional assistance with TEM, selection of TEM images and interpretation, drafting the work, revision, and intellectual content. Jørgen Serup: study concept, work design, patient consultations and drafting, revision and conclusion of the work, and the intellectual content.
Funding Statement
The authors received no financial support for this article's research, authorship, and publication.
Data Availability Statement
All relevant data generated or analysed during this study are included in this article. Further enquiries for supplementary material, such as Mössbauer spectrums, can be directed to the corresponding author.
Supplementary Material
References
- 1. Alsing KK, Johannesen HH, Hansen RH, Serup J. Tattoo complications and magnetic resonance imaging: a comprehensive review of the literature. Acta Radiol. 2020;61(12):1695–700. 10.1177/0284185120910427. [DOI] [PubMed] [Google Scholar]
- 2. Dirks M. Manufacturing of safe tattoo inks and suited pigments binding agents. 1st ed. In: Serup J, Kluger N, Bäumler W, editors. Tattooed skin and health. Basel: Karger; 2015. p. 118–27. [Google Scholar]
- 3. Serup J, Bäumler W. Diagnosis and therapy of tattoo complications: with atlas of illustrative cases. 1st ed. Basel: Karger; 2017. [Google Scholar]
- 4. Serup J, Kluger N, Bäumler W. Tattooed skin and health. 1st ed.Basel: Karger; 2015. [Google Scholar]
- 5. Laux P, Tralau T, Tentschert J, Blume A, Dahouk S, Bäumler W, et al. A medical-toxicological view of tattooing. Lancet. 2016;387(10016):395–402. 10.1016/S0140-6736(15)60215-X. [DOI] [PubMed] [Google Scholar]
- 6. Jackson JG, Acker JD. Permanent eyeliner and MR imaging. AJR Am J Roentgenol. 1987;149(5):1080. 10.2214/ajr.149.5.1080-a. [DOI] [PubMed] [Google Scholar]
- 7. Hutton Carlsen K, Larsen G, Serup J. Tattoo pigment agglomerates measured in skin biopsies by computerised light microscopy: study of 161 patients with adverse reactions in black and red tattoos. Skin Res Technol. 2020;26(2):284–91. 10.1111/srt.12798. [DOI] [PubMed] [Google Scholar]
- 8. Alsing KK, Johannesen HH, Hvass Hansen R, Dirks M, Olsen O, Serup J. MR scanning, tattoo inks, and risk of thermal burn: an experimental study of iron oxide and organic pigments: effect on temperature and magnetic behavior referenced to chemical analysis. Skin Res Technol. 2018;24(2):278–84. 10.1111/srt.12426. [DOI] [PubMed] [Google Scholar]
- 9. Tomita S, Miyawaki T. Multifaceted Evaluation of Ultra-high-field 9.4-T Magnetic resonance imaging after inorganic tattoos: an animal study. JMA J. 2019 Sep;2(2):155–63. 10.31662/jmaj.2019-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ständer S, Schneider SW, Weishaupt C, Luger TA, Misery L. Putative neuronal mechanisms of sensitive skin. Exp Dermatol. 2009;18(5):417–23. 10.1111/j.1600-0625.2009.00861.x. [DOI] [PubMed] [Google Scholar]
- 11. Kihlberg J, Hansson B, Hall A, Tisell A, Lundberg P. Magnetic resonance imaging incidents are severely underreported: a finding in a multicentre interview survey. Eur Radiol. 2022 Jan 1;32(1):477–88. 10.1007/s00330-021-08160-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Senova S, Cotovio G, Pascual-Leone A, Oliveira-Maia AJ. Durability of antidepressant response to repetitive transcranial magnetic stimulation: systematic review and meta-analysis. Brain Stimul. 2019 Jan 1;12(1):119–28. 10.1016/j.brs.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 13. Serup J, Carlsen KH, Sepehri M. Tattoo complaints and complications: diagnosis and clinical spectrum. 1st ed. In: Serup J, Kluger N, Bäumler W, editors. Tattooed skin and health. Basel: Karger; 2015. p. 48–60. [DOI] [PubMed] [Google Scholar]
- 14. Serup J, Sepehri M, Hutton Carlsen K. Classification of tattoo complications in a hospital material of 493 adverse events. Dermatology. 2016;232(6):668–78. 10.1159/000452148. [DOI] [PubMed] [Google Scholar]
- 15. Gehring AU, Fischer H, Louvel M, Kunze K, Weidler PG. High temperature stability of natural maghemite: a magnetic and spectroscopic study. Geophys J Int. 2009 Dec;179(3):1361–71. 10.1111/j.1365-246x.2009.04348.x. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data generated or analysed during this study are included in this article. Further enquiries for supplementary material, such as Mössbauer spectrums, can be directed to the corresponding author.