Abstract
Background
Cardiovascular disorders (CVDs) are the leading cause of death worldwide. This study aimed to evaluate the association between low-density lipoprotein (LDL) subfractions and cardiovascular disorders.
Methods
To ensure the rigor of the systematic review, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used. For this systematic review, a comprehensive search strategy was performed in important databases including PubMed, Scopus, Embase, International Statistical Institute (ISI) Web of Science, and google scholar from 2009 to February 2021. The following terms were used for systematic search: low-density lipoprotein, LDL, subfractions, subclasses, nuclear magnetic resonance, NMR, chromatography, high-pressure liquid, HPLC, cardiovascular disease, cerebrovascular, and peripheral vascular disease. Also, for evaluating the risk of bias, the Newcastle-Ottawa scale was employed.
Results
At the end of the search process, 33 articles were included in this study. The results of most of the evaluated studies revealed that a higher LDL particle number was consistently associated with increased risk for cardiovascular disease, independent of other lipid measurements. Also, small dense LDL was associated with an increased risk of CVDs. There was no association between LDL subfraction and CVDs in a small number of studies.
Conclusions
Overall, it seems that the evaluation of LDL subclasses can be used as a very suitable biomarker for the assessment and diagnosis of cardiovascular diseases. However, further studies are required to identify the mechanisms involved.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12872-023-03578-0.
Keywords: Low-density lipoprotein, Cholesterol, LDL subclasses, Small dense LDL, Cardiovascular Disease
Background
Cardiovascular disease is one of the leading causes of mortality in many countries [1]. Various factors, especially increased obesity, an inactive lifestyle, stress, and diseases such as diabetes and dyslipidemia have increased the risk of cardiovascular complications [2]. According to the Adult Treatment Panel III of the Expert Panel of the National Cholesterol Education Program recommendations, increased low-density lipoprotein (LDL) and reduction in high-density lipoprotein (HDL) levels are among the main risk factors for cardiovascular disease [3]. Various results from clinical trials as well as studies evaluating LDL genetic variants have indicated that treatment with statins and other therapies aimed at reducing LDL concentrations can prevent and reduce the risk of cardiovascular events [4–6]. Thus, LDL-lowering therapies are recommended by both European [7] and American guidelines [8] to prevent cardiovascular disease. Also, it has been reported in arteriographic investigations that any interventions to lower serum LDL and elevate HDL concentrations may reduce the rate of arteriographically defined disease progression [9–11].
Recognizing the role of LDL as a serious risk factor for cardiovascular disease, one of the questions that has arisen is whether the size of LDL particles and different subtypes of LDL plays the same role in the etiology of cardiovascular failure. It has been reported that some conditions such as metabolic syndrome, diabetes, familial combined hyperlipidemia, and hyperapobetalipoproteinemia (hyper-apoB) would elevate the concentration of small atherogenic LDL and lead to cardiovascular disease, as summarized in Fig. 1 [12, 13].
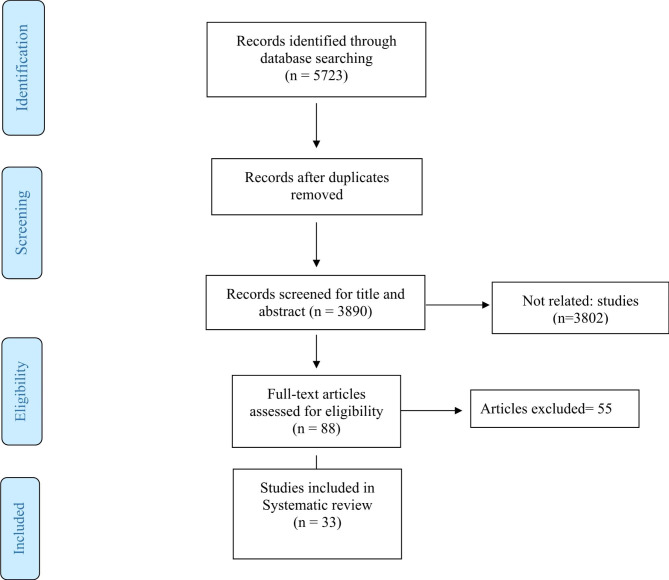
Fig. 1.
Flow chart of study selection
On the other hand, it has been shown that the effect of drug treatment such as statin therapy or Proprotein Convertase Subtilisin/Kexin type 9 (PCSK9) inhibitors was not the same in patients with high LDL levels, raising suspicion among researchers and physicians that differences in observed effects may be due to different concentrations of LDL subclasses [14–16]. Different terms are used to describe the characteristics and distribution of LDL particles such as LDL subclasses, subfraction and particle concentration, though all of these terms have almost the same meaning, and more attention has been paid to LDL subclasses since subclass separation techniques. Some studies have reported that small dense LDL (sdLDL) particles are at greater atherogenic risk than larger, less dense LDL, while some results are contradictory [17, 18]. Indeed, some studies have suggested that sdLDL are more taken up by macrophages and are at higher risk for oxidation. On the other hand, these particles easily penetrate into the subendothelial space and attach to the arterial wall, thus increasing the risk of atherosclerosis [19, 20]. A systematic review study conducted in 2009 by Stanley et al. [21] assessed the association between LDL subgroups and the incidence of cardiovascular Outcomes. However, the results of this study were contradictory and the authors of this article recommended that further studies be conducted to identify the mechanisms involved.
Due to the contradictory results and limitations mentioned in different studies, this updated systematic review study aimed to investigate the relationship between different LDL subclasses and the risk of cardiovascular disease.
Method
Search strategy
To ensure the rigor of this systemic review, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used [22]. For this systematic review, a comprehensive search strategy was employed in important databases including PubMed, Scopus, Embase, International Statistical Institute (ISI) Web of Science, and google scholar from 2009 to February 2021. In order not to miss an article, manual searching was performed. For systematic search, the following search strategy was used: (“Low-density lipoprotein” OR Cholesterol, LDL OR LDL OR lipoprotein) AND (particle size.mp. OR subfractions OR subclasses OR “Nuclear Magnetic Resonance” OR Biomolecular/ OR exp Magnetic Resonance Spectroscopy/ OR “nuclear magnetic resonance” OR NMR OR “magnetic resonance spectroscopy” OR Chromatography OR “High-Pressure Liquid” OR HPLC OR ultracentrifugation.mp OR centrifugation.mp OR Electrophoresis) AND (“cardiovascular disease” OR cerebrovascular OR peripheral vascular disease OR Cardiovascular OR Cardio* OR Atherosclerosis).
Criteria for selecting articles
Table 1 summarizes the population, interventions, comparators, and outcomes (PICOS) criteria for eligibility of studies. Articles were included in this study if they met the following criteria: prospective, longitudinal, and cross-sectional design which evaluated the association between LDL subfractions and cardiovascular disease, participation of at least 10 people in the study, serum (or plasma) samples must have been obtained before determination of outcomes, evaluation of specific clinical outcome such as minimum lumen diameter.
Table 1.
PICOS criteria for inclusion and exclusion of studies
| Parameter | |
|---|---|
| Population | Participants with abnormal levels of LDL subfraction |
| Exposure (or Intervention) | For studies that examined the association between serum LDL subfraction concentration and the risk of cardiovascular diseases, exposure is " LDL subfraction” |
| Comparators | Subjects with normal levels of LDL subfraction |
| Outcome | Risk of cardiovascular diseases |
The results of a systematic search for initial screening were entered into the EndNote software. After eliminating duplicate studies, the two authors independently evaluated the titles and abstracts of the articles. In the second stage, the researchers evaluated the full text of the remaining articles and the studies that met the necessary criteria were included in the final analysis. Also, studies with low methodological quality were detected. Data such as authors, country of study, method of assessing LDL levels, cardiovascular disease, etc. were extracted.
Risk of bias assessment
For evaluating the risk of bias, the Newcastle-Ottawa scale was used [23]. NOS was developed to evaluate the quality of nonrandomized studies, including cross-sectional, case-control, and cohort studies. This assessment allowed a total score of up to 9 points. The NOS for cohort studies was divided into three groups: selection of cohort (4 points), comparability of cohort (2 points), and assessment of outcome (3 points). The quality of the study was considered high or moderate if the sum score was ≥ 8 points or between 5 and 7 points, respectively.
Results
Characteristics of the included studies
In total, after searching the mentioned databases, 5723 studies entered the Endnote 20 software and after removing duplicate articles, 3890 articles remained for initial screening. Following the initial screening, 88 studies were chosen to evaluate the full text of these articles, and among them, finally, 33 articles were included in this study (Table 2). The flow chart of study selection has been presented in Fig. 1.
Table 2.
Characteristics of the included studies
| First Author | Type of study | Subjects | LDL subclass type | Evaluation Method | Main results | Total quality score |
|---|---|---|---|---|---|---|
|
Pallarés (2021) |
Cross-Sectional | Adults | LDL-Ps, L-LDL-P, M-LDL-P, S-LDL-P | NMR spectroscopy | higher CVDs rate and systolic blood pressure were significantly associated with abnormalities in the number of S-LDL-P | 8 |
|
Antonio (2021) |
Case-Control | women without CVD | LDL-P | NMR spectroscopy |
LDL-related variables were the most strongly associated with atherosclerosis |
9 |
|
Duan (2020) |
Cross-Sectional | hospitalized patients with Acute ischemic stroke | LDL-1, LDL-2, LDL-3, LDL-4, LDL-5 to 7 | polyacrylamide gel electrophoresis technique | LDL-3 and LDL-4 levels, were significantly positively correlated with AIS | 9 |
| Rodríguez (2019) | Cross-Sectional | middle- aged US- White and Japanese men | Small LDL- P, Large LDL- P, | NMR spectroscopy | total LDL- P and small LDL- P were significantly associated with coronary heart disease | 8 |
|
Kidawa (2019) |
Cross-Sectional | patients with Acute Coronary Syndromes (ACS) | LDL 1-LDL 5, IDLA | NMR spectroscopy | Patients with multi-vessel CADs disease had higher levels of LDL3 subfraction and IDL-C and a lower proportion of IDLA | 7 |
| Notarnicola (2018) | Prospective Cohort | cardiovascular diseases | Small LDL-C, Large LDL-C | NMR spectroscopy | Higher small LDL concentration was associated with higher CVDs mortality | 7 |
|
Llauradó (2019) |
Case-Control | participants with T1DM | Small LDL-C, Large LDL-C | NMR spectroscopy | Higher small LDL concentration was associated CVDs risk factors. | 8 |
|
Chang (2019) |
Cross-Sectional | Rheumatoid Arthritis Patients | LDL 1-LDL 5 | fast-protein liquid chromatography | Plasma L5 levels were significantly higher in patients with subclinical atherosclerosis | 9 |
|
Aneni (2019) |
Cross-Sectional | High-Risk Individuals | LDL-VS, LDL-S, LDL-M, LDL-La | gas-phase differential electrical mobility | Higher concentrations of large LDL were seen among those with no coronary artery calcification. small and medium LDL particles were seen among those with coronary artery calcification | 9 |
| Žitňanová (2019) | Case-Control |
patients with acute ischemic stroke |
LDL 1-LDL 5 | electrophoresis |
sdLDL was significantly higher in patients after acute ischemic stroke |
7 |
|
Schulte (2018) |
Cross-Sectional | Patients with Chronic inflammatory diseases | lbLDL-C, sdLDL-C | gas-phase differential electrical mobility | The sdLDL/LDL ratio was higher in patients with cardiovascular risk factors. | 8 |
|
Chu (2018) |
Cross-Sectional | patients with coronary artery disease | L1-L5 | liquid chromatography | Plasma L5 levels were significantly higher in patients with coronary artery disease | 6 |
|
Aday (2018) |
Prospective Cohort | women ≥ 45 years old free of cardiovascular disease | Small LDL-C, Large LDL-C | NMR spectroscopy | sdLDL-C particle concentration, but not LDL-C, were associated with peripheral artery disease (PAD) | 7 |
|
Siarnik (2017) |
Cross-Sectional | Patients with acute ischemic stroke | IDL1, IDL2,IDL3, LDL1, LDL2, LDL3-7 | Lipoprint LDL System | LDL1 was significantly associated with acute ischemic stroke | 8 |
|
Shiffman (2017) |
Case-Control | Adult participants | small LDL subfraction (LDL-VS), large LDL subfraction | ion mobility | LDL-VS was associated with CVDs | 6 |
| Pokharel et al. (2017) | Cross-Sectional | Patients with Myocardial Infarction | pattern A consisted of a preponderance of large, buoyant LDL subclass, while pattern B consisted mainly of small, dense LDL subclass | ultracentrifugation | when LDL pattern B was compared with LDL pattern A, there was significant 60% relative reduction in CV mortality. | 9 |
| Lawler et al. (2017) | Cross-Sectional | Individuals With Low Low-Density LipoproteinCholesterol | total LDL-p, small and large LDL-p, intermediate density lipoprotein [IDL-p] | NMR spectroscopy | Smaller LDL size was a marker of increased risk, but this was no longer significant after additionally adjusting for LDL-p | 9 |
| Gluba‑Brzózka (2017) | Case-Control | end‑stage renal disease (ESRD) patients | LDL1-LDL7 | Lipoprint LDL System | There wasn’t significant association between LDL subclasses and cardiovascular abnormalities. | 8 |
| Shen et al. (2016) | Case-Control | ischemic stroke patients | L5 | NMR spectroscopy | levels of plasma L5 were significantly higher in acute ischemic stroke patients than in controls | 6 |
| Steffen et al. (2015) | Cross-Sectional | Adult participants | total LDL particles (LDL-P) | NMR spectroscopy | There was a significant association between LDL-P and CHD events | 7 |
| Vishnu et al. (2014) | Cross-Sectional | middle-aged men | Large LDL-P, Small LDL-P, Total HDL-P | NMR spectroscopy | arterial stiffness had a significant positive association with small LDL-P and significantly inversely associated with large LDL-P and LDL size. | 8 |
| Nishikura (2014) | Cross-Sectional | Patients with Coronary Artery Disease | sdLDL-C, Large LDL-C | gradient gel electrophoresis | Those who experienced cardio-vascular events had higher levels of sdLDL-C, sdLDL-C/LDL-C, and LDL-C/high-density lipoprotein cholesterol (HDL-C) ratios | 7 |
|
Jug et al. (2014) |
Cross-Sectional | Patient at Intermediate Cardiovascular Risk | Small LDL-C, Large LDL-C | NMR spectroscopy | LDL pattern B (predominance of small dense particles) emerged as an independent predictor of coronary calcium | 6 |
| Gerber et al. (2013) | Prospective Cohort | Patients with (pre)diabete | sdLDL-C | gradient gel electrophoresis | Higher concentration of sdLDL-C was associated with intima media thickness | 8 |
| Cure et al. (2013) | Case-Control | Patients with ischemic stroke | Small LDL-C, Large LDL-C | NMR spectroscopy | The mean LDL particle size was smaller in patients with stroke than in the controls | 7 |
| Okumura et al. (2013) | Cross-Sectional | Patients with Endothelial Dysfunction | sdLDL-C | HPLC | small LDL cholesterol emerged as an independent determinant of Endothelial Dysfunction among lipoprotein subfractions | 8 |
| Lakshmy et al. (2012) | Cross-Sectional | young Indian industrial population | sdLDL-C | polyacrylamide gel electrophoresis technique | small dense LDL was associated with cardiovascular risk factors | 6 |
| Hirayama et al. (2012) | Cross-Sectional | adult | Small LDL- C | NMR spectroscopy | Small LDL- C is a emerging risk factor for cardiovascular disorder | 5 |
| Prado et al. (2012) | Cross-Sectional | asymptomatic adults at intermediate risk of cardiovascular disease | Large-pattern LDL(Pattern A) was defined as 23.0–20.6 nm, and small-pattern LDL (Pattern B) was defined as 20.5–18.0 nm. | NMR spectroscopy | small-pattern LDL (Pattern B) was an independent predictor of coronary artery calcification | 7 |
| Zeljkovic et al. (2012) | Cross-Sectional | Patients with acute ischemic stroke | LDL I-IV | gradient gel electrophoresis | AIS patients had significantly more LDL III and IVb, but less LDL I and II particles. | 8 |
| Chung et al. (2010) | Case-Control | Patients with rheumatoid arthritis | Small LDL-C, Large LDL-C | NMR spectroscopy | There wasn’t any significant association between small LDL level with coronary artery calcification (CAC) | 7 |
| Rizzo et al. (2009) | Prospective Cohort | subjects with the metabolic syndrome | sdLDL-C, Large LDL-C | gradient gel electrophoresis | small, dense LDL was a predictor of CVDs | 8 |
| Mora et al. (2009) | Prospective Cohort | Healthy women | Small LDL-C, Large LDL-C | NMR spectroscopy | CVDs risk prediction associated with LDL subclass profiles evaluated by NMR | 9 |
From those articles included, based on the design of studies, 20 studies had cross-sectional, 5 prospective cohort design, and 8 studies had a case-control design.
For evaluating LDL subclasses, 17 studies had employed NMR spectroscopy, 8 studies gel electrophoresis, one study HPLC, two studies liquid chromatography, one study electrical mobility, and four studies the ion mobility ultracentrifugation and lipoprint system.
Based on the Newcastle–Ottawa checklist, regarding the score of methodological quality, all included studies except six [4, 24–28] had high quality (more than 7 scores) (Table 3).
Table 3.
Quality assessment of included studies
| First author | Selection | Comparability | Outcome | Total |
|---|---|---|---|---|
| Pallarés | 4 | 1 | 3 | 8 |
| Antonio | 4 | 2 | 3 | 9 |
| Duan | 4 | 2 | 3 | 9 |
| Rodríguez | 3 | 2 | 3 | 8 |
| Kidawa | 3 | 1 | 3 | 7 |
| Notarnicola | 4 | 1 | 2 | 7 |
| Llauradó | 4 | 2 | 2 | 8 |
| Chang | 4 | 2 | 3 | 9 |
| Aneni | 4 | 2 | 3 | 9 |
| Žitňanová | 3 | 2 | 2 | 7 |
| Schulte | 3 | 2 | 3 | 8 |
| Chu | 3 | 1 | 2 | 6 |
| Aday | 4 | 2 | 2 | 8 |
| Siarnik | 3 | 2 | 2 | 7 |
| Shiffman | 3 | 2 | 1 | 6 |
| Pokharel | 4 | 2 | 3 | 9 |
| Lawler | 4 | 2 | 3 | 9 |
| Gluba‑Brzózka | 4 | 2 | 2 | 8 |
| Shen | 3 | 2 | 1 | 6 |
| Steffen | 4 | 2 | 1 | 7 |
| Vishnu | 4 | 2 | 2 | 8 |
| Nishikura | 4 | 2 | 1 | 7 |
| Jug | 3 | 1 | 2 | 6 |
| Gerber | 4 | 2 | 2 | 8 |
| Cure | 3 | 2 | 2 | 7 |
| Okumura | 4 | 2 | 2 | 8 |
| Lakshmy | 3 | 2 | 1 | 6 |
| Hirayama | 3 | 1 | 1 | 5 |
| Prado | 3 | 2 | 2 | 7 |
| Zeljkovic | 4 | 2 | 2 | 8 |
| Chung | 4 | 2 | 1 | 7 |
| Rizzo | 4 | 2 | 2 | 8 |
| Mora | 4 | 2 | 3 | 9 |
NMR-measured LDL subfractions
Among the studied studies, 17 studies had utilized the NMR method to evaluate LDL subfraction. Pallarés et al. [29] in a cross-sectional study conducted on 400 participants, reported that subjects with higher concentrations of small LDL particle size had a higher chance of developing cardiovascular disease. Also, Notarnicola et al. [30] showed that higher concentrations of sdLDL would increase the risk of mortality in patients with CVDs. In line with the two studies mentioned, other studies reported similar results [24, 25, 31–34]. Further, some studies have specifically examined the association between LDL subtypes and the incidence of various cardiovascular diseases. Cure et al. in a case-control study among patients with ischemic stroke reported that the level of sd‑LDL was 8.2 ± 7.8 mg/dL in the stroke group, which was significantly higher than the control group. However, the concentration of total LDL and large particles of LDL did not differ significantly between the two groups [35]. Also, Zeljkovic et al. in a cross-sectional study evaluated the concentration of various LDL subfractions among 100 patients with acute ischemic stroke and found that acute ischemic stroke (AIS) patients had significantly more LDL III and IV, but fewer LDL I and II particles [36].
LDL subfractions and coronary artery calcification (CAC)
Aneni et al. in a study conducted among 182 high cardiometabolic risk participants evaluated the association between LDL subfraction and risk of CAC. The result of this study revealed that subjects with higher concentrations of small/medium LDL subfractions had a higher risk for CAC odds compared to the participants with large LDL subfractions [37]. Prado et al. in a cross-sectional study evaluated the association between LDL subfractions and CAC among the 284 adults at intermediate risk of cardiovascular disease. They reported that the risk of CAC was 3.7 times higher in people with higher tertile of LDL particle (LDL-P) number [38]. Also, Jug et al. showed that serum concentration of small dense LDL lipoprotein was an independent predictor of CAC among the 410 patients at intermediate cardiovascular risk [26]. However, contrary to the results of the three studies mentioned, Chung et al. in a case-control study among 139 patients with rheumatoid arthritis concluded that there was no significant association between small LDL concentration and CAC [39].
LDL subfractions and stroke risk as well as atherosclerosis
Antonio et al. in a case-control study among 112 women with type 1 diabetes reported that patients with higher LDL particle (LDL-P) had a higher risk for atherosclerosis. Also, participants with higher concentrations of small LDL showed a higher risk for atherosclerosis and stroke [40]. Further, Duan et al. in a study on 566 patients with AIS reported that patients with AIS had a significantly higher concentration of LDL-3, LDL-4, and LDL-5 subclasses as well as lower concentration of LDL1 compared to the non-AIS participants [41]. A similar finding was observed in Chang et al. study [42]. In addition, Žitňanová et al. in a cross-sectional study which evaluated the association between LDL subfraction and AIS outcome, found that the serum concentration of anti-atherogenic large LDL1 subfractions was significantly lower in patients with AIS, and in contrast, they have a higher concentration of LDL3 and LDL5, which atherogenic properties [43].
Discussion
The present study has been a systematic review evaluating the association between LDL subclasses and cardiovascular disease. The results of the study revealed that participants with higher concentrations of small dense LDL were at a higher risk for CVDs. Additionally, we found that subjects with CVDs or those at risk for CVDs had higher concentrations of atherogenic LDL subclasses, such as LDL3 and LDL5.
In numerous countries, cardiovascular disease has emerged as a primary cause for mortality. Several articles have put different etiologies and theories for CVDs, among which a significant one is the rise in LDL levels, comprising seven subclasses (LDL-1 to LDL-7) [44]. The studies conducted so far on how LDL subclasses are linked to the development of different cardiovascular diseases have produced inconsistent findings [45, 46]. As the importance of evaluating LDL subclasses to predict cardiovascular disease has expanded, various methods have been developed to evaluate them [47]. For evaluating LDL subclasses, 17 studies had used NMR spectroscopy, 8 studies gel electrophoresis, one study HPLC, two studies liquid chromatography, one study electrical mobility, and four studies the ion mobility ultracentrifugation and lipoprint system. Most of the studies included in this systematic review had utilized the NMR spectroscopy method. NMR evaluates the number of LDL particles by applying a particular formula to measure the area and identifying the signal from the combined quantity of terminal methyl groups of the lipid present within the particle. Nonetheless, certain studies have employed the ultracentrifugation technique to assess LDL subgroups, where the separation of LDL subgroups is based on their density [48].
Although dyslipidemia is recognized as a traditional risk factor for cardiovascular disease, many patients with a history of acute vascular events have normal LDL levels. Concurrently,
Some people without any clinical or laboratory signs of CVDs exhibited higher concentrations of LDL-cholesterol [49, 50]. These findings promoted researchers to investigate and identify atherogenic and non-atherogenic subclasses of lipoproteins profiles. Some of the studies revealed that an atherogenic profile, characterized by elevated concentrations of VLDL, IDL1–3, small HDL, and especially by high levels of small dense LDL (LDL3–7) subfractions, can increase the risk of atherogenesis and CVDs. Meanwhile, the anti-atherogenic profile of lipoprotein subclasses, which includes a higher level of subtypes such as LDL1-2, large HDL, intermediate HDL and by only trace concentrations of LDL3–7 subfractions, has been identified by improving the body’s defenses against cardiovascular disease [51–53].
Despite numerous clinical and in vitro investigations, the precise mechanism behind the atherogenic effects of certain LDL subclasses remains uncertain. One proposed mechanism is that small, high-density LDL particles have a weaker binding affinity to hepatic LDL receptors, thus prolonging their clearance process [54]. Other researchers have suggested that elevated concentrations of small, dense LDL particles would increase their binding to intimal proteoglycans [55]. Additionally, LDL subclasses with smaller particles and higher density are more susceptible to oxidation, which leads to the formation of macrophage-derived foam cells, the hallmark of atherosclerotic plaques [56]. Furthermore, some studies have linked specific LDL subclasses to endothelial dysfunction [57].
The significance of examining lipoprotein subclasses has become so great that some associations that deal with cardiovascular diseases have included this field in their recommendations. While the American Heart Association still issues guidelines for treating CVD patients based on LDL levels, certain European associations, such as the European Society of Cardiology, suggest recommendations based on the level of LDL subclasses, such as sdLDL [58]. Evaluation of LDL subclasses can be used as a useful biomarker to identify people at risk for cardiovascular disease and to provide early preventive recommendations including diet and exercise [59].
The present review has been an updated systematic review, which evaluated observational studies evaluating the association between LDL subclasses and CVDs risk factors, incidence, and outcome. It has assessed results from 33 studies with a total of 12,320 subjects, providing substantial statistical power. Also, most of the studies had employed the same method to measure LDL subclasses, which is a standard method, though the evaluation method was different in some studies.
According to our knowledge, the present study has been the first systematic study examining the relationship between LDL subclasses and cardiovascular diseases. The current study had many strengths, including the systematic and comprehensive search across various databases, accurate and complete screening process, evaluation of methodological quality of studies with standard tools, and comprehensive review of all subclasses of LDL. Several limitations warrant discussion. One of the most important limitations of this study was the impossibility of meta-analysis due to the high heterogeneity of the studied outcomes. Also, the participants included in the studies in terms of health status or type of disease was a wide range, which can affect the accuracy of the results. Also, the consequences evaluated in different studies were adjusted for different confounding variables, which in turn can affect the accuracy of the results.
Conclusions
In conclusion, the assessment of LDL subclasses can be a useful biomarker for the evaluation and diagnosis of cardiovascular diseases. The results of this systematic review suggest that higher concentrations of small dense LDL particles are associated with increased risk for cardiovascular disease. However, further studies are needed to identify the mechanisms involved and to determine the clinical utility of measuring LDL subfractions in the management of cardiovascular disease.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- CAC
Coronary artery calcification
- CVDs
Cardiovascular disorders
- LDL
Low-Density Lipoprotein
- HDL
High-Density Lipoprotein
- PICOS
Population,interventions,comparators and outcomes
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- ISI
International Statistical Institute
- AIS
Acute Ischemic Stroke
- HPLC
High-performance liquid chromatography
- NMR
Nuclear magnetic resonance spectroscopy
- NOS
Newcastle-Ottawa scale
- sdLDL
Small dense LDL
- PCSK9
Proprotein Convertase Subtilisin/Kexin type 9
Author contributions
ACh and MH conceived of the presented idea and developed the theory and performed the computations. MT and MH were encouraged to investigate and supervised the findings of this work. All authors discussed the results and contributed to the final manuscript. ACh wrote the manuscript with support from MT and MH.
Funding
Not applicable.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wilkins E, Wilson L, Wickramasinghe K, Bhatnagar P, Leal J, Luengo-Fernandez R. Europeancardiovasculardiseasestatistics2017.2017.
- 2.Thayer JF, Yamamoto SS, Brosschot JF. The relationship of autonomic imbalance, heart rate variability and Cardiovascular Disease risk factors. Int J Cardiol. 2010;141(2):122–31. doi: 10.1016/j.ijcard.2009.09.543. [DOI] [PubMed] [Google Scholar]
- 3.Cleeman J, Grundy S, Becker D, Clark L. Expert panel on detection, evaluation and treatment of high blood cholesterol in adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP III) JAMA. 2001;285(19):2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Shiffman D, Louie JZ, Caulfield MP, Nilsson PM, Devlin JJ, Melander O. LDL subfractions are associated with incident Cardiovascular Disease in the Malmö Prevention Project Study. Atherosclerosis. 2017;263:287–92. doi: 10.1016/j.atherosclerosis.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK. Plasma HDL cholesterol and risk of Myocardial Infarction: a mendelian randomisation study. The Lancet. 2012;380(9841):572–80. doi: 10.1016/S0140-6736(12)60312-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hedayati M, Daneshpour MS, Zarkesh M, Yeganeh MZ, Sheikholeslami S, Faam B. etal.Biochemical assessment: findings from 20 years of the Tehran lipid and glucose study.Int J Endocrinol Metabolism.2018;16(4 Suppl). [DOI] [PMC free article] [PubMed]
- 7.Binno S. 2016EuropeanGuidelinesoncardiovasculardiseasepreventioninclinicalpractice–WebAddenda.2016.
- 8.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. J Am Coll Cardiol. 2014;63(25 Part B):2889–934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Investigators M. Effect of simvastatin on coronary atheroma: the Multicentre Anti-atheroma Study (MAAS) The Lancet. 1994;344(8923):633–8. doi: 10.1016/S0140-6736(94)92082-6. [DOI] [PubMed] [Google Scholar]
- 10.Rosenson RS, Otvos JD, Freedman DS. Relations of lipoprotein subclass levels and low-density lipoprotein size to progression of coronary artery Disease in the Pravastatin limitation of Atherosclerosis in the coronary arteries (PLAC-I) trial. Am J Cardiol. 2002;90(2):89–94. doi: 10.1016/S0002-9149(02)02427-X. [DOI] [PubMed] [Google Scholar]
- 11.Hedayati M, Daneshpour M. Evaluation of HDL-C determination methods. Iran J Endocrinol Metabolism. 2005;7(4):365–73. [Google Scholar]
- 12.Sniderman AD. How, when, and why to use apolipoprotein B in clinical practice. Am J Cardiol. 2002;90(8):48–54. doi: 10.1016/S0002-9149(02)02633-4. [DOI] [PubMed] [Google Scholar]
- 13.Kwiterovich PO., Jr Clinical relevance of the biochemical, metabolic, and genetic factors that influence low-density lipoprotein heterogeneity. Am J Cardiol. 2002;90(8):30–47. doi: 10.1016/S0002-9149(02)02749-2. [DOI] [PubMed] [Google Scholar]
- 14.Dadu RT, Ballantyne CM. Lipid lowering with PCSK9 inhibitors. Nat Reviews Cardiol. 2014;11(10):563. doi: 10.1038/nrcardio.2014.84. [DOI] [PubMed] [Google Scholar]
- 15.Navarese EP, Kołodziejczak M, Schulze V, Gurbel PA, Tantry U, Lin Y. Effects of proprotein convertase subtilisin/kexin type 9 antibodies in adults with hypercholesterolemia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(1):40–51. doi: 10.7326/M14-2957. [DOI] [PubMed] [Google Scholar]
- 16.Kazi DS, Moran AE, Coxson PG, Penko J, Ollendorf DA, Pearson SD. Cost-effectiveness of PCSK9 inhibitor therapy in patients with heterozygous familial hypercholesterolemia or atherosclerotic Cardiovascular Disease. JAMA. 2016;316(7):743–53. doi: 10.1001/jama.2016.11004. [DOI] [PubMed] [Google Scholar]
- 17.Wang TJ, Gona P, Larson MG, Tofler GH, Levy D, Newton-Cheh C. Multiple biomarkers for the prediction of first major cardiovascular events and death. N Engl J Med. 2006;355(25):2631–9. doi: 10.1056/NEJMoa055373. [DOI] [PubMed] [Google Scholar]
- 18.Ware JH. The limitations of risk factors as prognostic tools. N engl J med. 2006;355(25):2615–7. doi: 10.1056/NEJMp068249. [DOI] [PubMed] [Google Scholar]
- 19.Krauss RM. Dense low density lipoproteins and coronary artery Disease. Am J Cardiol. 1995;75(6):53B–7B. doi: 10.1016/0002-9149(95)80012-H. [DOI] [PubMed] [Google Scholar]
- 20.Krauss RM. Dietary and genetic effects on low-density lipoprotein heterogeneity. Annu Rev Nutr. 2001;21(1):283–95. doi: 10.1146/annurev.nutr.21.1.283. [DOI] [PubMed] [Google Scholar]
- 21.Ip S, Lichtenstein AH, Chung M, Lau J, Balk EM. Systematic review: association of low-density lipoprotein subfractions with cardiovascular outcomes. Ann Intern Med. 2009;150(7):474–84. doi: 10.7326/0003-4819-150-7-200904070-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 23.Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2011. [Google Scholar]
- 24.Hirayama S, Miida T. Small dense LDL: an emerging risk factor for Cardiovascular Disease. Clin Chim Acta. 2012;414:215–24. doi: 10.1016/j.cca.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 25.Lakshmy R, Dorairaj P, Tarik M, Gupta R, Reddy KS. LDL particle heterogeneity, and its association with other established cardiovascular risk factors in a young Indian industrial population. Heart Asia. 2012;4(1):141–5. doi: 10.1136/heartasia-2012-010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jug B, Papazian J, Lee R, Budoff MJ. Association of lipoprotein subfractions and coronary artery calcium in patient at intermediate cardiovascular risk. Am J Cardiol. 2013;111(2):213–8. doi: 10.1016/j.amjcard.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shen MY, Chen FY, Hsu JF, Fu RH, Chang CM, Chang CT. Plasma L5 levels are elevated in ischemic Stroke patients and enhance platelet aggregation. Blood. 2016;127(10):1336–45. doi: 10.1182/blood-2015-05-646117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chu CS, Chan HC, Tsai MH, Stancel N, Lee HC, Cheng KH. Range of L5 LDL levels in healthy adults and L5’s predictive power in patients with hyperlipidemia or coronary artery Disease. Sci Rep. 2018;8(1):11866. doi: 10.1038/s41598-018-30243-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pallarés-Carratalá V, Quesada JA, Orozco-Beltrán D, Amigó-Grau N, Lopez-Pineda A, Fernández Giménez A. Analysis of LDL and HDL size and number by nuclear magnetic resonance in a healthy working population: the LipoLab Study. Int J Clin Pract. 2021;75(1):e13610. doi: 10.1111/ijcp.13610. [DOI] [PubMed] [Google Scholar]
- 30.Notarnicola M, Tutino VDEN, et al. Integrated Small dense low-density Lipoprotein Profile in Cardiovascular Disease and Cancer: a longitudinal study. Anticancer Res. 2019;39(11):6035–9. doi: 10.21873/anticanres.13809. [DOI] [PubMed] [Google Scholar]
- 31.Llauradó G, Amigó N, Cano A, Ballesta S, Albert L, Mazarico I. etal.Specific nuclear magnetic resonance lipoprotein subclass profiles and central arterial stiffness in type 1 Diabetes Mellitus: a Case Control Study.J Clin Med.2019;8(11). [DOI] [PMC free article] [PubMed]
- 32.Steffen BT, Guan W, Remaley AT, Paramsothy P, Heckbert SR, McClelland RL. etal.Utility of lipoprotein particle measures for assessing coronary Heart Disease risk post-AHA/ACC guidelines: the multi-ethnic study of Atherosclerosis. Arteriosclerosis, Thrombosis, and vascular biology.2015;35(2):448. [DOI] [PMC free article] [PubMed]
- 33.Rizzo M, Pernice V, Frasheri A, Di Lorenzo G, Rini GB, Spinas GA. Small, dense low-density lipoproteins (LDL) are predictors of cardio- and cerebro-vascular events in subjects with the metabolic syndrome. Clin Endocrinol (Oxf) 2009;70(6):870–5. doi: 10.1111/j.1365-2265.2008.03407.x. [DOI] [PubMed] [Google Scholar]
- 34.Mora S, Otvos JD, Rifai N, Rosenson RS, Buring JE, Ridker PM. Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident Cardiovascular Disease in women. Circulation. 2009;119(7):931–9. doi: 10.1161/CIRCULATIONAHA.108.816181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cure MC, Tufekci A, Cure E, Kirbas S, Ogullar S, Kirbas A. Low-density lipoprotein subfraction, carotid artery intima-media thickness, nitric oxide, and Tumor necrosis factor alpha are associated with newly diagnosed ischemic Stroke. Ann Indian Acad Neurol. 2013;16(4):498–503. doi: 10.4103/0972-2327.120438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zeljkovic A, Vekic J, Spasojevic-Kalimanovska V, Jelic-Ivanovic Z, Bogavac-Stanojevic N, Gulan B. LDL and HDL subclasses in acute ischemic Stroke: prediction of risk and short-term mortality. Atherosclerosis. 2010;210(2):548–54. doi: 10.1016/j.atherosclerosis.2009.11.040. [DOI] [PubMed] [Google Scholar]
- 37.Aneni EC, Osondu CU, De La Cruz J, Martin SS, Blaha MJ, Younus A. Lipoprotein Sub-fractions by Ion-Mobility Analysis and Its Association with subclinical coronary Atherosclerosis in high-risk individuals. J Atheroscler Thromb. 2019;26(1):50–63. doi: 10.5551/jat.40741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prado KB, Shugg S, Backstrand JR. Low-density lipoprotein particle number predicts coronary artery calcification in asymptomatic adults at intermediate risk of Cardiovascular Disease. J Clin Lipidol. 2011;5(5):408–13. doi: 10.1016/j.jacl.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 39.Chung CP, Oeser A, Raggi P, Sokka T, Pincus T, Solus JF. Lipoprotein subclasses determined by nuclear magnetic resonance spectroscopy and coronary Atherosclerosis in patients with rheumatoid arthritis. J Rheumatol. 2010;37(8):1633–8. doi: 10.3899/jrheum.090639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Amor AJ, Vinagre I, Valverde M, Urquizu X, Meler E, López E. etal.Nuclear magnetic resonance lipoproteins are associated with carotid Atherosclerosis in type 1 Diabetes and pre-eclampsia.Diab/Metab Res Rev.2020:e3362. [DOI] [PubMed]
- 41.Duan R, Xue W, Wang K, Yin N, Hao H, Chu H. Estimation of the LDL subclasses in ischemic Stroke as a risk factor in a Chinese population. BMC Neurol. 2020;20(1):414. doi: 10.1186/s12883-020-01989-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chang CY, Chen CH, Chen YM, Hsieh TY, Li JP, Shen MY. etal.Association between negatively charged low-density lipoprotein L5 and subclinical Atherosclerosis in rheumatoid arthritis patients.J Clin Med.2019;8(2). [DOI] [PMC free article] [PubMed]
- 43.Žitňanová I, Šiarnik P, Füllöp M, Oravec S, Penesová A, Ďuračková Z. Gender differences in LDL-and HDL-cholesterol subfractions in patients after the acute ischemic Stroke and their association with oxidative stress markers. J Clin Biochem Nutr. 2018;63(2):144–8. doi: 10.3164/jcbn.17-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. The Lancet. 2019;394(10204):1145–58. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwon SW, Yoon S-J, Kang TS, Kwon HM, Kim J-H, Rhee J. Significance of small dense low-density lipoprotein as a risk factor for coronary artery Disease and acute coronary syndrome. Yonsei Med J. 2006;47(3):405. doi: 10.3349/ymj.2006.47.3.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Superko HR, Gadesam RR. Is it LDL particle size or number that correlates with risk for Cardiovascular Disease? Curr Atheroscler Rep. 2008;10(5):377–85. doi: 10.1007/s11883-008-0059-2. [DOI] [PubMed] [Google Scholar]
- 47.Chung M, Lichtenstein AH, Ip S, Lau J, Balk EM. Comparability of methods for LDL subfraction determination: a systematic review. Atherosclerosis. 2009;205(2):342–8. doi: 10.1016/j.atherosclerosis.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 48.Witte D, Taskinen MR, Perttunen-Nio H, van Tol A, Livingstone S, Colhoun H. Study of agreement between LDL size as measured by nuclear magnetic resonance and gradient gel electrophoresis. J Lipid Res. 2004;45(6):1069–76. doi: 10.1194/jlr.M300395-JLR200. [DOI] [PubMed] [Google Scholar]
- 49.Oravec S, Gruber K, Dostal E, Mikl J. Hyper-betalipoproteinemia LDL 1, 2: a newly identified nonatherogenic hypercholesterolemia in a group of hypercholesterolemic subjects. Neuroendocrinol Lett. 2011;32(3):322–7. [PubMed] [Google Scholar]
- 50.Oravec S, Dukát A, Gavorník P, Lovásová Z, Gruber K. Atherogenic normolipidemia-a new phenomenon in the lipoprotein profile of clinically healthy subjects. Neuroendocrinol Lett. 2011;32(3):317–21. [PubMed] [Google Scholar]
- 51.Berneis KK, Krauss RM. Metabolic origins and clinical significance of LDL heterogeneity. J Lipid Res. 2002;43(9):1363–79. doi: 10.1194/jlr.R200004-JLR200. [DOI] [PubMed] [Google Scholar]
- 52.Asztalos BF, Cupples LA, Demissie S, Horvath KV, Cox CE, Batista MC. etal.High-density lipoprotein subpopulation profile and coronary Heart Disease prevalence in male participants of the Framingham offspring study. Arteriosclerosis, Thrombosis, and vascular biology.2004;24(11):2181–7. [DOI] [PubMed]
- 53.Oravec S, Dukat A, Gavornik P, Caprnda M, Kucera M, Ocadlik I. Contribution of the atherogenic lipoprotein profile to the development of arterial Hypertension. Bratisl Lek Listy. 2011;112(1):4–7. [PubMed] [Google Scholar]
- 54.Nigon F, Lesnik P, Rouis M, Chapman MJ. Discrete subspecies of human low density lipoproteins are heterogeneous in their interaction with the cellular LDL receptor. J Lipid Res. 1991;32(11):1741–53. doi: 10.1016/S0022-2275(20)41629-3. [DOI] [PubMed] [Google Scholar]
- 55.Maaninka K, Nguyen SD, Mäyränpää MI, Plihtari R, Rajamäki K, Lindsberg PJ. Human mast cell Neutral proteases generate modified LDL particles with increased proteoglycan binding. Atherosclerosis. 2018;275:390–9. doi: 10.1016/j.atherosclerosis.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 56.Gerber PA, Nikolic D, Rizzo M. Small, dense LDL: an update. Curr Opin Cardiol. 2017;32(4):454–9. doi: 10.1097/HCO.0000000000000410. [DOI] [PubMed] [Google Scholar]
- 57.Atiq F, van de Wouw J, Sorop O, Heinonen I, de Maat MP, Merkus D. etal.Endothelial dysfunction, Atherosclerosis, and increase of Von Willebrand factor and factor VIII: a Randomized Controlled Trial in Swine.Thromb Haemost.2021. [DOI] [PubMed]
- 58.Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) Eur Heart J. 2020;41(1):111–88. doi: 10.1093/eurheartj/ehz455. [DOI] [PubMed] [Google Scholar]
- 59.Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes E. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular Disease: meta-analysis of individual data from 27 randomised trials. Lancet (London England) 2012;380(9841):581–90. doi: 10.1016/S0140-6736(12)60367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.