Abstract
Objective
This study aimed to systematically evaluate the level of medical equipment alarm fatigue and its influencing factors among clinical nurses.
Methods
PubMed, Embase, CNKI, and Wanfang databases were systematically searched to identify articles on alarm fatigue of clinical nurses published before September 25, 2022. According to the evaluation criteria of prevalence studies recommended by JBI Evidence-Based Health Care Center, the quality of the literature meeting the inclusion criteria was evaluated, and Stata MP17 software was used for meta-analysis.
Results
A total of 14 cross-sectional studies were included, with a total sample of 2,848 nurses. The results showed that the alarm fatigue score of clinical nurses was 21.76 (95% CI [20.27, 23.25]). Subgroup analysis showed that the nurses who worked night shift and had lower professional title had higher alarm fatigue.
Conclusion
The alarm fatigue of clinical nurses was at a moderate level. To reduce the alarm fatigue level of clinical nurses, nursing managers should strengthen the alarm safety awareness of nurses, rationally arrange nurse manpower, carry out training to actively improve the alarm management ability of nurses, and optimize the alarm level and frequency of alarm equipment.
Keywords: nurse, alarm fatigue, systematic review
Relevance to Clinical Practice
Influencing factors of nurse alarm fatigue include alarm-setting factors, device factors, and clinical nurse factors.
It is suggested that nursing leaders adopt the alarm management guidelines for clinical training, so as to improve the alarm management ability of nurses and reduce the alarm fatigue of nurses.
Intervene the influencing factors of alarm fatigue and pay attention to the lasting effect.
A comprehensive consideration of staff, device, and technology can improve the security of alarm management and reduce the gap between guidelines or standards and practice.
Introduction
Medical equipment alarm fatigue refers to a phenomenon where medical personnel who are exposed to alarms from multiple medical equipment for a long time become less sensitive to these alarms, resulting in the potential for them to ignore critical equipment alarms. Alarm fatigue is often used to describe the impact of numerous alarms on nursing staff (Wilken et al., 2017). It refers to the desensitization and indifference of medical staff to numerous, repeated, or simultaneous alarm sounds, which is a major contributor to adverse alarm events, causing serious consequences for patients’ safety (Bach et al., 2018). In addition, attending to many alarms can lead to exhaustion in nursing (Casey et al., 2018). Medical equipment plays an indispensable role in patient care, and medical staff can be exposed to equipment alarms up to 1000 times during a single shift (Ruskin & Hueske-Kraus, 2015). It has been reported that 72%–99% of clinical alarms may be false alarms (Bach et al., 2018; Srinivasa et al., 2017). Excessive false and unactionable alarms desensitize nurses, which may result in them missing critical alarms (Sowan et al., 2015). Most hospitals have reported adverse events in patients related to medical device alarms (Casey et al., 2018). It is therefore necessary to improve alarm management strategies and measurement methods of alarm fatigue level (Lewandowska et al., 2020). The study of Lewandowska emphasized the negative impact of alarm fatigue and pointed out the importance of improving alarm management systems to reduce this burden (Lewandowska et al., 2020). Bach pointed out that although there is limited high-quality research on the effect of alarm management procedures on alarm fatigue, current evidence supports that improved alarm management procedures have a positive effect on alarm fatigue in nurses (Bach et al., 2018).
The issue of alarm fatigue as a potential risk to patient safety has received significant attention. Alarm fatigue can lead to burnout, which seriously affects the safety of patients (Ding et al., 2023; Storm & Chen, 2021). Although in 2003, the Joint Commission on Accreditation of Healthcare Organization (JCAHO) sought to improve the efficacy of alerts in relation to national patient safety goals, adverse events to alarms continue to occur, which resulted in the deaths of 80 patients and the permanent loss of function in 13 patients (Leigher, 2020). In 2014, alarm fatigue was recognized as a threat to patient safety and was included in the national alarm management patient safety target as a problem requiring improvement (Ruskin & Hueske-Kraus, 2015; Sendelbach & Funk, 2013). The China Hospital Association released the Patient Safety Goal (2019 Edition), which for the first time listed “strengthening the safety and alarm management of medical equipment” as one of the major goals of patient safety. Alarm fatigue has been recognized as a significant patient safety issue by multiple institutions (Scott et al., 2019).
So how to handle alarms correctly? Guidelines issued by the Emergency Care Research Institute (ECRI) refer to the concept of the life cycle of a clinical alarm, which refers to the process from the time an alarm is generated until the patient's condition is addressed and the alarm is eliminated. Clinical alarm life cycle includes four important parts: alarm generation, transmission, identification and response. ECRI believes that by mastering the life cycle of the alarm, the fault point can be identified in the alarm management and effective measures can be taken (ECRI, 2013). An implementation strategy to prevent nurse alarm fatigue incorporates guidelines from the American Association of Critical Care Nurses (AACN) for the management of ECG monitoring alarms, including daily electrode changes and appropriate skin preparation, eliminate inoperable and duplicate alarms and adjust default threshold alarms, educate and instruct registered nurses and custodial technicians to customize alerts, and reduce the overuse of continuous cardiac monitoring by implementing guidelines (AACN, 2018; Sandau et al., 2017; Turmell et al., 2017). The Practice Guide for Clinical Alarm Management of Multiparameter Monitors in China (2020 edition) recommends the use of the Subjective fatigue symptom Scale revised by the Japan Occupational Health Association to evaluate the alarm fatigue degree of nurses and suggests that hospitals may consider the use of Internet of Things technology signal filtering technology and advanced alarm generation algorithm artificial intelligence system to optimize the hospital alarm management system. By improving the specificity of the alarm, false alarms can be reduced effectively, thereby further preventing alarm fatigue (Yue, 2021). Therefore, it is very important to make clear the influencing factors of alarm fatigue and develop improvement strategies. In this study, meta-analysis was used to systematically evaluate alarm fatigue and its influencing factors among clinical nurses, which would provide a basis for improvement strategies. PROSPERO registration number CRD42023410993 has been obtained for this study.
Methods
We used the PRISMA reporting guidelines to conduct this systematic review and meta-analysis (Page et al., 2021).
Literature and Strategy
We searched the English databases PubMed and EMBASE, the Chinese databases CNKI and Wanfang, and other relevant literatures on medical equipment alarm fatigue among clinical nurses and its influencing factors. Relevant articles published from the inception of the database to September 25, 2022, were retrieved. Regarding the search strategy, search terms were combined with subject words and free words, and truncated words were used to improve the recall ratio. The English search terms were “Clinical alarms” OR “Alarm fatigue” OR “Alarm fatigue*”; “Nurse” OR “Nurs*” OR “Nursing” OR “care” OR “caring.” Search strategies—PubMed as an example (Table 1):
Table 1.
Search Strategies—PubMed as an Example.
| ((((“Clinical Alarms"[Mesh]) OR (Alarm fatigue [Title/Abstract])) OR (Alarm fatigue*[Title/Abstract])) OR (Clinical alarms*[Title/Abstract])) AND ((((“Nurses"[Mesh]) OR (Nurs*[Title/Abstract])) OR (“Nursing"[Mesh])) OR (“Primary Health Care"[Mesh])) |
| #1 “ Clinical alarms” [MeSH] |
| #2 “Alarm fatigue” [Title/Abstract] |
| #3 “Alarm fatigue*” [Title/Abstract] |
| #4 # 1 OR #2 OR #3 |
| #5 “Nurse” [MeSH] |
| #6 “Nurs*” [Title/Abstract] |
| #7 “Health care” [Title/Abstract] |
| #8 # 5 OR #6 OR #7 |
| #9 # 4 AND #8 |
Inclusion and Exclusion Criteria for Literature
Inclusion criteria: studies involving clinical nurses, observational study describing alarm fatigue levels and related factors in clinical nurses, study tools including at least a clinical alarm fatigue-related scale for measurement, having a clear analysis of results, and the article that is in Chinese or English.
Exclusion criteria: literature reporting incomplete data or where data cannot be extracted, reviews and other secondary studies, interventional research, qualitative research, and studies where full text or repeated publication is not available.
Study Selection and Data Extraction
Literature selection and quality evaluation were conducted independently by two evidence-based trained researchers in strict accordance with inclusion and exclusion criteria. In case of disagreement, the evaluator discussed or consulted a third person for arbitration. Literature data were extracted by two researchers independently, including basic information of the study, sample size, influencing factors involved, outcome measurement data, and key elements of bias risk assessment.
Quality Assessment
The prevalence study quality assessment tool developed by the JBI Evidence-Based Health Care Centre in Australia (2016) was used. It consists of nine assessment items (Table 2), and the evaluator is required to make a judgment of “yes,” “no,” “unclear,” and “not applicable” for each evaluation item and to decide on whether to include, exclude, or obtain further information after group discussion. Literature quality evaluation was divided into A, B, and C grades. If all the nine evaluation criteria were satisfied, it is Grade A, indicating a low risk of bias. If six to eight criteria are met, it is Grade B, indicating a moderate risk of bias. If three to five criteria are met, it is the Class C, indicating a high risk of bias.
Table 2.
Quality Evaluation Results of the Included Literatures (n = 14).
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Level |
|---|---|---|---|---|---|---|---|---|---|---|
| Wang Jing | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Yin Xin | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Jiang Yifan | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Wang Donghua | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Liu Qiaohong | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Yang Jing | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Sun Jing | Y | Y | Y | Y | Y | Y | Y | N | Y | B |
| Wang Na | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Wang Qin | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Luo Lingling | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Yunxia Zhao | Y | Y | Y | Y | Y | Y | Y | N | Y | B |
| Neda Asadi | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Ok Min Ch | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
| Yu Jin Jeong | Y | Y | Y | Y | Y | Y | Y | Y | Y | A |
Note. 1. Was the sample frame appropriate to address the target population? 2. Was the sampling technique appropriate to address the target population? 3. Was the sample size adequate? 4. Were the study subjects and the setting described in detail? 5. Was the data analysis conducted with sufficient coverage of the identified sample? 6. Was the identification of the condition or phenomenon accurate? 7. Were objective, standard criteria used for measurement of the condition or phenomenon? 8. Was the timeframe for the condition or phenomenon appropriate? 9. Was the response rate adequate, and if not, were the characteristics of nonrespondents described?
“Y” indicates yes, “N” indicates no, “UN” indicates unclear, and “NA” indicates not applicable.
Statistical Analysis
StataMP17 software was used for data analysis. First, clinical heterogeneity among the included studies was assessed. The fixed-effects model is used if there is no heterogeneity (P > 0.1, I2 < 50%), and the random-effects model is used if there is high heterogeneity (P ≤ 0.1, I2 ≥ 50%). Subgroup analysis was used to explore the sources of heterogeneity, such as educational background and professional title, which were basically the same classification criteria in the included literature. P ≤ 0.001 was considered statistically significant. Continuous variable data were mean difference (MD) or standardized mean difference (SMD) due to different measurement tools. 95% CI was calculated in all effects analysis.
Results
Overview of the Included Studies
A total of 1,246 relevant literatures were retrieved, including 272 from PubMed, 839 from Embase, 68 from CNKI, and 67 from Wanfang. After screening (Figure 1), 14 cross-sectional studies were finally included, including 10 Chinese and 4 English literatures, with a total sample size of 2,848 nurses. See Table 4 for the basic characteristics of the included studies and Table 2 for the results of bias risk assessment.
Figure 1.
Literature screening flow chart.
Table 4.
Basic information of the 14 included literatures.
| Author | year | country | Study population | Sample size | Research type | Sampling method | Research tool | Alarm fatigue score | Influencing factor |
|---|---|---|---|---|---|---|---|---|---|
| Wang Jing | 2017 | China | ICU | 118 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 19.88 ± 3.72 | Different educational background, departments, scheduling, alarm parameter setting frequency; high false alarm rate and inadequate system training |
| Yin Xin | 2018 | China | ICU nurses | 622 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 19.50 ± 6.40 | Years of work, professional title |
| Jiang Yifan | 2022 | China | Anesthesiology nurse | 241 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 20.19 ± 7.33 | Major, night duty |
| Wang Donghua | 2018 | China | ICU nurses | 326 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 17.04 ± 5.97 | Nursing work environment; job title, night shift situation, frequency of setting alarm parameters, health status, attitude toward nursing work |
| Liu Qiaohong | 2022 | China | ICU nurses | 225 | Descriptive study | Cluster sampling method | Alarm fatigue questionnaire | 22.32 ± 2.83 | Age, working years, working with illness, job title, shift, no habit of setting medical equipment alarm, medical equipment management factors |
| Yang Jing | 2021 | China | ICU nurses | 164 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 20.25 ± 6.09 | Scheduling and false alarm rate |
| Sun Jing | 2018 | China | Emergency department nurse | 351 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 21.05 ± 10.00 | Working years |
| Wang Na | 2018 | China | ICU nurses | 123 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 18.88 ± 3.68 | Educational background, professional title, department, working years, night shift, management factors of medical equipment alarm, and obstacles perceived by nurses |
| Wang Qin | 2018 | China | Hemodialysis room nurse | 80 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 25.01 ± 2.38 | Gender, education, working years, annual number of training, setting parameter frequency |
| Luo Lingling | 2022 | China | ICU nurses | 160 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 23.82 ± 6.75 | Working life, manpower, material resources, the basis of high-quality nursing services |
| Yunxia Zhao | 2021 | China | ICU nurses | 215 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 24.63 ± 8.99 | Job title, working years, educational background |
| Neda Asadi | 2022 | Iran | ICU nurses | 140 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 19.08 ± 6.26 | Training, education, gender |
| Ok Min Cho | 2016 | Korea | ICU nurses | 35 | Descriptive study | Observation method | Alarm fatigue questionnaire | 24.3 ± 4.0 | High false alarm rate |
| Yu Jin Jeong | 2021 | Korea | ICU nurses | 48 | Descriptive study | Convenience sampling | Alarm fatigue questionnaire | 28.97 ± 4.01 | High false alarm rate |
Risk of Bias Assessment
In the 14 cross-sectional studies included in this study, the inclusion and exclusion criteria of the study population were clearly defined in the literature, which was consistent with the purpose of this study. All studies used standard measurement tools with good reliability and validity, reported outcome indicators, and used appropriate statistical methods. Generally, 12 papers included in the study were Grade A, and the rest were Grade B.
Meta-Analysis Results of Alarm Fatigue of Clinical Nurses
Primary Outcomes
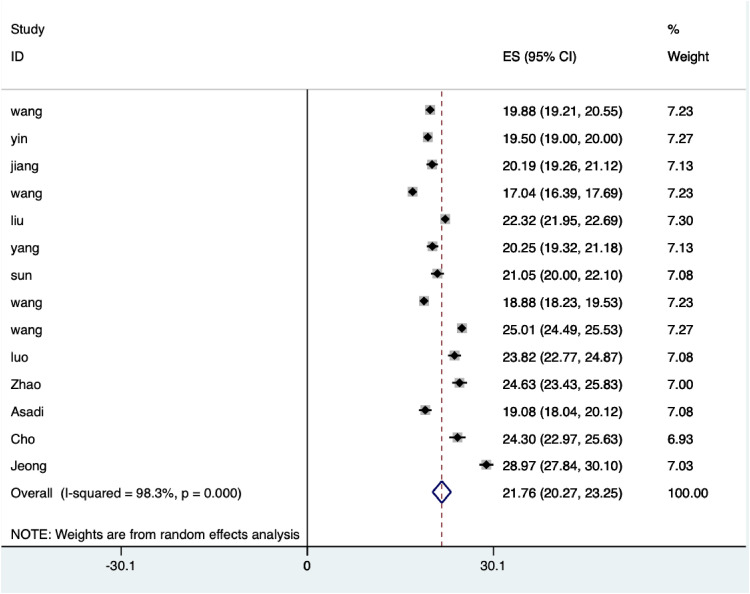
Alarm fatigue levels in clinical nurses were reported in the 14 included studies. All studies used the clinical alarm fatigue scale as the evaluation tool, with one study using the Japanese version of the scale. All 14 papers were included in the meta-analysis, which may have certain limitations. The results of random-effects model meta-analysis showed that the alarm fatigue score of clinical nurses was 21.76 (95% CI [20.27, 23.25]), as shown in Figure 2.
Figure 2.
Forest plot of alarm fatigue score.
Meta-Analysis of Influencing Factors of Alarm Fatigue in Clinical Nurses
Meta-analysis was performed on three or more studies with the same assessment tools and influencing factors. The results showed that night shift and having a professional title had significant heterogeneity among the included literatures (p ≤ .001), and random-effects model was used. Meta-analysis results showed that night shift and different professional titles were the main influencing factors of alarm fatigue among clinical nurses, as shown in Table 3.
Table 3.
Subgroup-Analysis of Influencing Factors of Nurses’ Alarm Fatigue.
| Subgroup analysis | Inclusion study | Number | Heterogeneity test | Effect model | Alarm fatigue score Combined effect value (95% CI) |
||
|---|---|---|---|---|---|---|---|
| I2 (95%) | p | ||||||
| Night shift | Yes | 3 (Wang, 2017; Wang, 2018c; Yang, 2021) | 356 | 95.7 | p ≤ .001 | Random | 21.07 (18.78, 23.37) |
| No | 3 (Wang, 2017; Wang, 2018c; Yang, 2021) | 49 | 90.1 | p ≤ .001 | Random | 19.89 (16.26, 23.51) | |
| Professional title | Nurse | 3 (Wang, 2018a; Wang, 2018c; Yin, 2018) | 405 | 93.2 | p ≤ .001 | Random | 19.50 (16.56, 22.44) |
| Nurse practitioner | 3 (Wang, 2018a; Wang, 2018c; Yin, 2018) | 511 | 98.0 | p ≤ .001 | Random | 20.02 (16.89, 23.16) | |
| Supervisor nurse | 3 (Wang, 2018a; Wang, 2018c; Yin, 2018) | 139 | 95.2 | p ≤ .001 | Random | 18.40 (14.61, 22.18) | |
| Deputy chief nurse and above | 3 (Wang, 2018a; Wang, 2018c; Yin, 2018) | 16 | 74.9 | p ≤ .001 | Random | 15.43 (11.52, 19.35) | |
Influencing Factors of Alarm Fatigue Among Clinical Nurses
Factors Related to Clinical Nurses
Five studies showed that nurses with low education had higher alarm fatigue (Asadi et al., 2022; Wang, 2017; Wang, 2018b; Wang, 2018c; Zhao et al., 2021). The alarm fatigue score of nurses with bachelor's degree or above was lower than that of nurses with junior college degree. The group with higher education level has a better ability to accept new knowledge and new skills. However, in Asadi's study, nurses with doctoral degrees had a higher degree of alarm fatigue, which may be related to the fact that doctors devote more energy to scientific research and participate less in clinical work, making them more prone to alarm fatigue when faced with more clinical alarms. Six studies have shown that night shift is an influencing factor of alarm fatigue (Jiang, 2022; Liu, 2022; Wang, 2017; Wang, 2018a; Wang, 2018c; Yang, 2021). Most studies indicated that the alarm fatigue score of shift nurses was higher than that of nonshift nurses, and shift nurses responsible for patient observation and nursing plan implementation had longer alarm exposure time and a higher frequency. However, Yang Jing concluded that the alarm fatigue of nurses in dayshift was significantly higher than that of nightshift nurses (Yang, 2021). This could be due to the longer working hours in day shift and shorter working hours in night shift of nurses included in the study (Table 4).
Seven studies have shown that working years is an influencing factor of nurse alarm fatigue (Liu, 2022; Luo, 2022; Sun, 2018; Wang, 2018b; Wang, 2018c; Yin, 2018; Zhao et al., 2021). Low working years is an independent risk factor for alarm fatigue of nurses. Nurses lack clinical alarm management experience and usually do not have the ability to deal with the alarms of monitoring instruments quickly and accurately. Excessive psychological pressure makes them more prone to alarm fatigue. However, Wang et al. pointed out in their study that nurses with longer working years tend to have higher alarm fatigue due to their long-term exposure to frequent medical alarms (Wang, 2018b). As a result, they choose to delay or refuse to deal with alarms of routine medical equipment that do not endanger patients’ lives.
Five studies have shown that having a professional title is an influencing factor of nurse alarm fatigue (Liu, 2022; Wang, 2018a; Wang, 2018c; Yin, 2018; Zhao et al., 2021). Two studies showed that alarm fatigue was higher among female nurses, which may be related to the differences in psychology between men and women (Asadi et al., 2022; Wang, 2018c). Men are known to have stronger endurance and willpower and are less affected by external interference. Three studies showed that insufficient training was associated with higher alarm fatigue (Asadi et al., 2022; Wang, 2017; Wang, 2018c). Nurses who rarely attended training each year had higher alarm fatigue scores than those who attended training occasionally and often. Nurses with insufficient alarm knowledge cannot recognize or fully understand all alarms and are prone to alarm fatigue.
Alarm-Setting Factors
Five studies showed that alarm parameter setting frequency is related to alarm fatigue (Liu, 2022; Wang, 2017; Wang, 2018a; Wang, 2018b; Zhao et al., 2021). The study showed that nurses who “always set alarm parameters” had lower alarm fatigue than other nurses. Nurses routinely set alarm parameters according to the patient's condition and age at the end of the shift and can timely modify inappropriate alarm parameters to reduce invalid alarm.
Device Factors
Six studies showed that a high false alarm rate easily leads to higher alarm fatigue (Cho et al., 2016; Jeong & Kim, 2023; Wang, 2017; Wang, 2018b; Yang, 2021; Yin, 2018). The highest score in the study survey was “frequent false alarms led to a decrease in my attention and response speed to the alarm prompts of the monitor.” Approximately 91% of nurses felt the noise of the alarm interfered with their work, resulting in alarm fatigue.
Discussion
Summary and Interpretation of Findings
Clinical Nurse Factors
Nurses’ lack of awareness of alarm management and alarm fatigue lead to patient safety problems (Petersen & Costanzo, 2017). At present, the use of medical equipment in hospitals is increasing exponentially, and alarm is inevitable. Therefore, it is crucial to provide effective and continuous education and training on clinical alarm management for nurses and to improve their awareness of alarm fatigue (Nyarko et al., 2022). However, alarm management is complicated, with a variety of alarm settings, alarm signal priorities, and alarm upgrade algorithms. Nurses are the main users of medical alarms, and they work in a complex environment with many alarms. The adverse events related to alarms are common. As the main operators of these systems, clinical nurses need to receive adequate training to properly set and respond to device alarms (Johnson et al., 2017; Yue et al., 2017). Sowan's survey results showed that 50% of nurses clearly expressed the need for more training in cardiac monitoring instruments to properly manage alarms (Sowan et al., 2016). Bi's training of monitoring and alarm management based on the theory of planned behavior effectively reduces the alarm fatigue of nurses in the intensive care unit (Bi et al., 2020). Nyarko pointed out that educational intervention is conducive to reducing the total number of alarms and false reports and can effectively control the alarm fatigue of nurses (Nyarko et al., 2022). Therefore, it is necessary to carry out training for different nurse groups to reduce alarm fatigue.
Device Factors
Numerous false alarms and alarm-generating devices can easily lead to alarm fatigue, and most alarms lack clinical relevance (Simpson & Lyndon, 2019). Medical equipment sends alarm signals that do not need priority treatment for low-priority events (Johnson et al., 2017), and frequent monitor alarms often distract nurses’ attention. False alarms due to faulty ECG leads, oximeter probes, or motion interference probes can also seriously cause alarm fatigue. In Alsaad's study, a total of 8,336 alarms were recorded during 4 weeks of monitoring instrument data collection, of which only 333 (4%) were actually actionable alarms (Alsaad, 2017). Kern-Goldberger pointed out that excessive monitoring can increase the risk of alarm fatigue, which could have a negative impact on nursing effect and lead to clinical nurses not being able to observe abnormal vital signs in time (Kern-Goldberger et al., 2022). Simpson pointed out that monitoring-only patients who need to be monitored and physiological indicators determined according to patients’ conditions can reduce alarm burden and thus improve alarm fatigue (Simpson & Lyndon, 2019). Various problems in the design and practical use of patient monitoring systems can also lead to alarm fatigue (Kobayashi et al., 2017). Multidisciplinary teams should facilitate informatics research to alleviate alarm fatigue. Alarm fatigue due to low-priority alerts can be reduced by extending alert delays, changing to visual alerts, or even considering eliminating alerts altogether (Cvach et al., 2013). A study describing the effect of implementing a nurse-driven, evidence-based, patient-customized monitoring package CEASE showed that reducing the number of monitoring alarms improved nurses’ perception of alarm fatigue (Lewis & Oster, 2019). The specific meaning of this monitoring package CEASE is Communication, Electrodes (daily change), Appropriateness (assessment), and Setup alarm, an acronym for setting alarm parameters (patient customization), and education (Ongoing).
Alarm-Setting Factors
Alarm fatigue can lead to delayed or nonresponse to alarms related to patient safety, resulting in low job satisfaction and adverse nursing safety events, among which the reasons for alarm fatigue include the increase in alarm-related workload (Shanmugham et al., 2018). Frequent false alarms lead to reduced attention to or response to alarms, which is the primary obstacle to effective alarm management (Casey et al., 2018). Approximately 90% of nurses felt that inoperable alarms were frequent, disrupting patient care, and that trust in alarms was reduced, prompting nurses to sometimes disable the alarms. In Chromik's study, for both patients and healthcare workers, excessive alarms can cause stress, lead to distractions at work, and disrupt circadian rhythms (Chromik et al., 2022). Shanmugham showed that modifying alarm threshold based on patients’ conditions had a positive impact on the accurate handling of alarms and nurses’ overall satisfaction (Shanmugham et al., 2018). However, clinical data are needed to guide practical decisions, such as when the setting of low oxygen saturation alarm limits and alarm delays can ensure patient safety and minimize alarm fatigue (Johnson et al., 2017). Alarm fatigue is a multidisciplinary problem requiring a multidisciplinary approach, and the solutions involve various aspects, such as reducing false alarms, setting alarm priorities, and alarm presentation content (Chromik et al., 2022). Scott et al. pointed out in their study on the correlation between alarm fatigue and alarm fatigue generated by mechanical ventilation equipment that patients may be desensitized to alarm sound due to alarm fatigue and ignore alarms that alert about patient injury (Scott et al., 2019). However, in Micah Seifert's quality improvement project on alarm management, through the management of problematic physiological alarms, the alarm fatigue of nurses did not decrease despite the reduction in alarm frequency (Seifert et al., 2021).
Limitations of the Study
Due to language limitations, only Chinese and English articles were included in this study, and all of them were cross-sectional studies, which poses an inevitable risk of bias. The influencing factors involved in this study were many but inconsistent, and the common influencing factors included in the study were few; therefore, it was not possible to conduct a meta-analysis on the influencing factors of a single study. In addition, a convenience sampling method was used in most of the included studies, which may have sampling errors. This conclusion needs to be verified using multicenter and large-sample studies.
Conclusion
To sum up, this study systematically evaluated the influencing factors of alarm fatigue in clinical nurses and found that there was a moderate level of alarm fatigue among clinical nurses. The results also showed that night shift, different professional titles, high false alarm rate, and excessive monitoring alarm were risk factors for alarm fatigue in clinical nurses. To reduce nurse alarm fatigue, managers need to develop reasonable intervention strategies to improve the alarm frequency and alarm level of various equipment and rationally organize nurse work shift.
An important part of the alarm management strategy is to educate nurses about alarm and pay attention to the assessment of alarm fatigue. Therefore, the next step will be to investigate the knowledge, attitude, and behavior of nurses about alarm fatigue from commonly used monitoring devices, in order to provide a basis for targeted intervention strategies.
Acknowledgments
First of all, I would like to express my gratitude to all those who helped me during the writing of this thesis. I gratefully acknowledge the help of my supervisor, who has offered me valuable suggestions in the academic studies. Second, I am also deeply indebted to all the authors in this study; with their help and teamwork, we finished this paper perfectly. Last, I should finally like to express my gratitude to my beloved family who have always been helping me and supporting without a word of plaint.
How does this paper contribute to the wider global clinical community?: • Alarm fatigue can lead to serious adverse nursing events and harm patient safety. The research on the influencing factors of alarm fatigue can provide the basis for further intervention.
• Current studies on alarm fatigue focus on nurses in intensive care unit, but alarm fatigue does not only occur in this group. We systematically reviewed the status quo and influencing factors of alarm fatigue in nurse groups, including anesthesia nurses and emergency nurses.
• More high-quality studies are needed to confirm whether avoiding these influencing factors can reduce alarm fatigue in nurses.
Author contributions: C.S.: conceptualization, methodology, data curation, writing—original draft, writing—review and editing, and project administration. Z.H.: conceptualization, methodology, resources, writing—review, and editing. W.S.: methodology, and data curation. J.R.: methodology and data curation. Z.H.: writing—reviewing and supervision. Z.H.: writing—reviewing and supervision. Z.H.: writing—reviewing. W.J.: writing—review and proof checking.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Medical Education Research project of Henan Province (Wjlx2020385).
ORCID iD: Chen Shaoru https://orcid.org/0000-0001-8445-6598
References
- AACN. (2018). Managing alarms in acute care across the life span: Electrocardiography and pulse oximetry. Critical Care Nurse, 38(2), e16–e20. 10.4037/ccn2018468 [DOI] [PubMed] [Google Scholar]
- Alsaad A. A. (2017). A multidisciplinary approach to reducing alarm fatigue and cost through appropriate use of cardiac telemetry. Postgraduate Medical Journal, 93(1101), 430–435. 10.1136/postgradmedj-2016-134764 [DOI] [PubMed] [Google Scholar]
- Asadi N., Salmani F., Asgari N., Salmani M. (2022). Alarm fatigue and moral distress in ICU nurses in COVID-19 pandemic. BMC Nursing, 21(1), 125. 10.1186/s12912-022-00909-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bach T. A., Berglund L.-M., Turk E. (2018). Managing alarm systems for quality and safety in the hospital setting. BMJ Open Quality, 7(3), e000202. 10.1136/bmjoq-2017-000202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi J., Yin X., Li H., Gao R., Zhang Q., Zhong T., Li Z. (2020). Effects of monitor alarm management training on nurses’ alarm fatigue: A randomised controlled trial. Journal of Clinical Nursing, 29(21–22), 4203–4216. 10.1111/jocn.15452 [DOI] [PubMed] [Google Scholar]
- Casey S., Avalos G., Dowling M. (2018). Critical care nurses’ knowledge of alarm fatigue and practices towards alarms: A multicentre study. Intensive & Critical Care Nursing, 48, 36–41. 10.1016/j.iccn.2018.05.004 [DOI] [PubMed] [Google Scholar]
- Cho O. M., Kim H., Lee Y. W., Cho I. (2016). Clinical alarms in intensive care units: Perceived obstacles of alarm management and alarm fatigue in nurses. Healthcare Informatics Research, 22(1), 46–53. 10.4258/hir.2016.22.1.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chromik J., Klopfenstein S. A. I., Pfitzner B., Sinno Z.-C., Arnrich B., Balzer F., Poncette A.-S. (2022). Computational approaches to alleviate alarm fatigue in intensive care medicine: A systematic literature review. Frontiers in Digital Health, 4, 843747. 10.3389/fdgth.2022.843747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cvach M. M., Biggs M., Rothwell K. J., Charles-Hudson C. (2013). Daily electrode change and effect on cardiac monitor alarms: An evidence-based practice approach. Journal of Nursing Care Quality, 28(3), 265–271. 10.1097/NCQ.0b013e31827993bc [DOI] [PubMed] [Google Scholar]
- Ding S., Huang X., Sun R., Yang L., Yang X., Li X., Wang X. (2023). The relationship between alarm fatigue and burnout among critical care nurses: A cross-sectional study. Nursing in Critical Care. 10.1111/nicc.12899 [DOI] [PubMed] [Google Scholar]
- ECRI. (2013). The life cycle of an alarm. A conceptual model understanding clinical alarms hazards. Health Devices, 42(9), 294–300. PMID: 24187709 [PubMed] [Google Scholar]
- Jeong Y. J., Kim H. (2023). Critical care nurses’ perceptions and practices towards clinical alarms. Nursing in Critical Care, 28(1), 101–108. 10.1111/nicc.12751 [DOI] [PubMed] [Google Scholar]
- Jiang y. (2022). Investigation of medical equipment alarm fatigue of nurses in anesthesiology department and its influencing factors. Journal of Nursing, 37(9), 62–64. 10.3780/j.issn.1001-4152.2022.09.062 [DOI] [Google Scholar]
- Johnson K. R., Hagadorn J. I., Sink D. W. (2017). Alarm safety and alarm fatigue. Clinics in Perinatology, 44(3), 713–728. 10.1016/j.clp.2017.05.005 [DOI] [PubMed] [Google Scholar]
- Kern-Goldberger A. R., Hamm R. F., Raghuraman N., Srinivas S. K. (2022). Reducing alarm fatigue in maternal monitoring on labor and delivery: A commentary on deimplementation in obstetrics. American Journal of Perinatology. 10.1055/a-1785-9175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi L., Gosbee J. W., Merck D. L. (2017). Development and application of a clinical microsystem simulation methodology for human factors-based research of alarm fatigue. HERD, 10(4), 91–104. 10.1177/1937586716673829 [DOI] [PubMed] [Google Scholar]
- Leigher D. (2020). Skin preparation and electrode replacement to reduce alarm fatigue in a community hospital intensive care unit. American Journal of Critical Care: An Official Publication, American Association of Critical-Care Nurses, 29(5), 390–395. 10.4037/ajcc2020120 [DOI] [PubMed] [Google Scholar]
- Lewandowska K., Weisbrot M., Cieloszyk A., Mędrzycka-Dąbrowska W., Krupa S., Ozga D. (2020). Impact of alarm fatigue on the work of nurses in an intensive care environment-A systematic review. International Journal of Environmental Research and Public Health, 17(22), 8409. 10.3390/ijerph17228409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis C. L., Oster C. A. (2019). Research outcomes of implementing CEASE: An innovative, nurse-driven, evidence-based, patient-customized monitoring bundle to decrease alarm fatigue in the intensive care unit/step-down unit. Dimensions of Critical Care Nursing: DCCN, 38(3), 160–173. 10.1097/DCC.0000000000000357 [DOI] [PubMed] [Google Scholar]
- Liu q. (2022). Construction of alarm fatigue risk prediction model for nurses in pediatric ICU. Chinese Journal of Modern Nursing, 28(22), 3016–3021. 10.3760/cma.j.cn115682-20211006-04507 [DOI] [Google Scholar]
- Luo l. (2022). Study on the status quo and influencing factors of alarm fatigue in ICU nurses. General Nursing, 20(16), 2166–2170. 10.12104/j.issn.1674-4748.2022.16.002 [DOI] [Google Scholar]
- Nyarko B. A., Nie H., Yin Z., Chai X., Yue L. (2022). The effect of educational interventions in managing nurses’ alarm fatigue: An integrative review. Journal of Clinical Nursing. 10.1111/jocn.16479 [DOI] [PubMed] [Google Scholar]
- Page M. J., McKenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., Moher D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clinical Research Ed.), 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen E. M., Costanzo C. L. (2017). Assessment of clinical alarms influencing nurses’ perceptions of alarm fatigue. Dimensions of Critical Care Nursing: DCCN, 36(1), 36–44. 10.1097/DCC.0000000000000220 [DOI] [PubMed] [Google Scholar]
- Ruskin K. J., Hueske-Kraus D. (2015). Alarm fatigue: Impacts on patient safety. Current Opinion in Anaesthesiology, 28(6), 685–690. 10.1097/ACO.0000000000000260 [DOI] [PubMed] [Google Scholar]
- Sandau K. E., Funk M., Auerbach A., Barsness G. W., Blum K., Cvach M., & American Heart Association Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Council on Cardiovascular Disease in the Young. (2017). Update to practice standards for electrocardiographic mnitoring in hospital settings: A scientific statement from the American Heart Association. Circulation, 136(19), e273–e344. 10.1161/CIR.0000000000000527 [DOI] [PubMed] [Google Scholar]
- Scott J. B., De Vaux L., Dills C., Strickland S. L. (2019). Mechanical ventilation alarms and alarm fatigue. Respiratory Care, 64(10), 1308–1313. 10.4187/respcare.06878 [DOI] [PubMed] [Google Scholar]
- Seifert M., Tola D. H., Thompson J., McGugan L., Smallheer B. (2021). Effect of bundle set interventions on physiologic alarms and alarm fatigue in an intensive care unit: A quality improvement project. Intensive & Critical Care Nursing, 67, 103098. 10.1016/j.iccn.2021.103098 [DOI] [PubMed] [Google Scholar]
- Sendelbach S., Funk M. (2013). Alarm fatigue: A patient safety concern. AACN Advanced Critical Care, 24(4), 378–386. quiz 387–388. 10.1097/NCI.0b013e3182a903f9 [DOI] [PubMed] [Google Scholar]
- Shanmugham M., Strawderman L., Babski-Reeves K., Bian L. (2018). Alarm-related workload in default and modified alarm settings and the relationship between alarm workload, alarm response rate, and care provider experience: Quantification and comparison study. JMIR Human Factors, 5(4), e11704. 10.2196/11704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson K. R., Lyndon A. (2019). False alarms and overmonitoring: Major factors in alarm fatigue among labor nurses. Journal of Nursing Care Quality, 34(1), 66–72. 10.1097/NCQ.0000000000000335 [DOI] [PubMed] [Google Scholar]
- Sowan A. K., Gomez T. M., Tarriela A. F., Reed C. C., Paper B. M. (2016). Changes in default alarm settings and standard in-service are insufficient to improve alarm fatigue in an intensive care unit: A pilot project. JMIR Human Factors, 3(1), e1. 10.2196/humanfactors.5098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowan A. K., Tarriela A. F., Gomez T. M., Reed C. C., Rapp K. M. (2015). Nurses’ perceptions and practices toward clinical alarms in a transplant cardiac intensive care unit: Exploring key issues leading to alarm fatigue. JMIR Human Factors, 2(1), e3. 10.2196/humanfactors.4196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasa E., Mankoo J., Kerr C. (2017). An evidence-based approach to reducing cardiac telemetry alarm fatigue. Worldviews on Evidence-Based Nursing, 14(4), 265–273. 10.1111/wvn.12200 [DOI] [PubMed] [Google Scholar]
- Storm J., Chen H.-C. (2021). The relationships among alarm fatigue, compassion fatigue, burnout and compassion satisfaction in critical care and step-down nurses. Journal of Clinical Nursing, 30(3–4), 443–453. 10.1111/jocn.15555 [DOI] [PubMed] [Google Scholar]
- Sun j. (2018). Investigation of emergency nurses’ fatigue degree and its influencing factors in medical equipment alarm. Electronic Journal of Practical Clinical Nursing, 3(42), 158–159. 10.3969/j.issn.2096-2479.2018.42.135 [DOI] [Google Scholar]
- Turmell J. W., Coke L., Catinella R., Hosford T., Majeski A. (2017). Alarm fatigue: Use of an evidence-based alarm management strategy. Journal of Nursing Care Quality, 32(1), 47–54. 10.1097/NCQ.0000000000000223 [DOI] [PubMed] [Google Scholar]
- Wang j. (2017). Study on the degree of medical equipment alarm fatigue and its influencing factors in ICU nurses. Chinese Journal of Nursing, 52(2), 211–215. 10.3761/j.issn.0254-1769.2017.02.019 [DOI] [Google Scholar]
- Wang d. (2018a). Investigation on the status quo and influencing factors of medical equipment alarm fatigue in ICU nurses. Journal of Nursing, 33(13), 19–21. 10.3870/j.issn.1001-4152.2018.13.019 [DOI] [Google Scholar]
- Wang n. (2018b). Current situation and influencing factors of medical equipment alarm fatigue of nurses in intensive care unit. Modern Clinical Nursing, 17(12), 11–16. 10.1155/2021/9994303 [DOI] [Google Scholar]
- Wang q. (2018c). Current situation and influencing factors of medical equipment alarm fatigue of nurses in hemodialysis room. International Journal of Nursing, 37(22), 3051–3054. 10.1155/2021/9994303 [DOI] [Google Scholar]
- Wilken M., Hüske-Kraus D., Klausen A., Koch C., Schlauch W., Röhrig R. (2017). Alarm fatigue: Causes and effects. Studies in Health Technology and Informatics, 243, 107–111. [PubMed] [Google Scholar]
- Yang j. (2021). Medical equipment alarm fatigue status and influencing factors of 164 nurses in intensive care unit. General Nursing, 19(1), 133–135. 10.12104/j.issn.1674-4748.2021.01.041 [DOI] [Google Scholar]
- Yin x. (2018). Investigation on clinical alarm cognition and alarm fatigue among nurses in intensive care unit. Nursing Management in China, 18(2), 260–264. 10.3969/j.issn.1672-1756.2018.02.025 [DOI] [Google Scholar]
- Yue l. (2021). The practice guide for clinical alert management of multi-parameter monitors (2020 edition). Nursing Management in China, 21(05), 758–765. (CNKI). 10.3969/j.issn.1672-1756.2021.05.025 [DOI] [Google Scholar]
- Yue L., Plummer V., Cross W. (2017). The effectiveness of nurse education and training for clinical alarm response and management: A systematic review. Journal of Clinical Nursing, 26(17–18), 2511–2526. 10.1111/jocn.13605 [DOI] [PubMed] [Google Scholar]
- Zhao Y., Wan M., Liu H., Ma M. (2021). The current situation and influencing factors of the alarm fatigue of Nurses’ medical equipment in the intensive care unit based on intelligent medical care. Journal of Healthcare Engineering, 2021, 9994303. 10.1155/2021/9994303 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]