Abstract
Introduction
During the last decades, the advent of flexible ureteroscopic lithotripsy has revolutionized the management of upper urinary tract stones. We designed a patented tip-bendable ureteral access sheath to facilitate stone clearance. Our current study reported our initial experience of 224 cases.
Materials and methods
The study is a descriptive, retrospective analysis. The initial 224 cases, operated consecutively by one surgeon during 16 months, were reviewed. The novel tip-bendable ureteral access sheath was applied in the procedure. Demographics, laboratory tests, and peri- and postoperative findings (operation duration, stone-free rate (SFR), utilization of flexible instruments and complications) were analyzed.
Resutls
The median age of the patients was 56 years and the mean stones size was 2.3 ± 1.3 cm. There were 63 cases of upper ureteral stone, 93cases of renal stone and 68 cases of ureteral-renal stones. The mean operative time was 69.2 ± 65.2 min. The immediate stone-free rate was 76.8% and the 1 month post-operative stone-free rate was 97.3%. Most cases(95.5%)were success in single session. Two patient experienced post-operative fever. There was no unplanned readmission. The frequency of post-operative complications was estimated at 0.89% (Clavien I).
Conclusion
Flexible ureteroscopic lithotripsy with tip-bendable ureteral access sheath is a safe and effective procedure, which can achieve excellent stone clearance.
Keywords: Lithotripsy, Ureteroscopy, Ureteral access sheath
Introduction
The urinary tract calculi are an important health problem with an incidence of 1–20% worldwide [1]. During the last decades, urologists are searching for the most efficient and minimally invasive surgical procedure for stone disintegration. Meanwhile, developments in endourological technologies make the retrograde intrarenal surgery (RIRS) more appealing for the majority of renal stones. It is recommended by the European Association of Urology (EAU) as the first recommended choice for renal stones ≤ 2 cm [2]. With the innovation in endourology, RIRS has been applied in some centers for more complex stones. Takazawa et al. [3] reported 100% stone free rate (SFR) handling RIRS for 2-4 cm renal stones. Riley et al. [4] showed a 90.9% success rate for stones averaging 3 cm in size. Naoya et al. [5] applied RIRS as a primary treatment for staghorn calculi, which could accomplish a final 48% SFR for patients with > 60 mm calculi.
However, the limited SFR, the necessity of multiple surgical sessions and the potentially life-threatening complications related to intra-renal pressure remain the major restrictions for such procedure [6], especially while managing larger kidney calculus. Intending to overcome the shortages of RIRS, we designed a patented ureter access sheath with features of suction and bendable-tip. The tip of the innovated ureteral access sheath (UAS) can reach the target calyx along with the flexible ureteroscope. Thus, it can facilitate dusts and fragments flushing. Applying the sheath extensively enhances the stone clearance while maintaining the intrarenal pressure. Herein, we summarized our initial experience of 224 cases as below.
Materials and methods
The medical files of 224 patients who were treated for ureteral or renal calculi during Oct 2021 and Nov 2022 in Xinchang County Hospital of Traditional Chinese Medicine and 1st Affiliated Hospital of Zhejiang University, School of Medicine, Zhejiang Province, China were retrospectively reviewed. All the patients were diagnosed with upper urinary tract calculi by preoperative imaging studies including CT scan. Patients with a congenital renal anomaly, previous urological surgery and refractory infection were excluded. Stone size and location were evaluated preoperatively by non-contrast CT scan. Stone size was measured in its largest diameter. When multiple stones presented, the sum of diameters was recorded as stone burden. Preoperative laboratory tests included routine CBC, urine analysis, urine culture, serum creatinine test, coagulation panel and basic metabolic panel including blood glucose test.
All procedures were performed under general or continuous epidural anesthesia by one single expert surgeon. Patients with positive urine cultures were treated with appropriate antibiotics preoperatively until thecultures turned to be negative. For others, broad-spectrum antibiotics were applied peri-operatively for prophylaxis. Most patients scheduled for RIRS were pre-stented 7–14 days prior to the RIRS surgery in outpatient surgery.
RIRS was performed in the dorsal lithotomy position. After D-J stent retrieval, a 0.035-inch guidewire was introduced into the upper urinary tract. Ureteroscopic inspection was performed. If ureter stone presented, it was fragmented and flushed back to the renal pelvis. A 12/14F tip-bendable UAS (Elephant II, Zhejiang YiGao Medical Technology Co. Ltd, Hangzhou, China) was inserted over the guidewire. A 9.9 F digital flexible ureteroscope (URF-V, Olympus) was advanced along with the UAS into the renal pelvis or the targeted calyces. For the cases with stones in the lower calyx, basket was applied for stone relocation when the infundibulopelvic angle (IPA) was steep. Stones were fragmented with 200 μm holmium laser fibers (Raykeen Laser Technology Limited Corporation, Shanghai, China) under specific energy setting of 1-1.5 J and a rate of 15–20 Hz.
All patients were evaluated on postoperative days 1 by CT to assess stone-free status. For those failed to gain stone-free status, an additional CT was required on postoperative day 30 as further evaluation. Stone-free was defined as the absence of any stones or residual fragments ≤ 2 mm under non-contrast CT [5]. The operative time was counted from the beginning of lithotripsy to the end of the surgery. Complications were evaluated to the Clavien classification.
All statistical analyses were performed using a standard software package (Stata, version. 11.0, StataCorp). Descriptive analysis was performed to evaluate distribution patterns of patients’ demographics, stone characteristics, and operation data. Operation time was recorded as mean ± standard deviation (SD) and examined using a Kruskai-Wallis H Test. Categorical variables were expressed as percentages. Chi-square or Fisher’s exact Test was used to compare the pairs of categorical variables. The analysis considered significant when P < 0.05.
Results
Demographics and preoperative data are shown in Table 1. Overall, ages of the patients ranged from 19 to 68 years old with a median age of 56 years old. There were 93 patients with renal calculi only and 63 cases with ureteral calculi only. The other 68 cases were diagnosed with concomitant renal and ureteral calculi. In the patients with renal calculi, there were 96 cases with lower calyx involved. Most patients were pre-stented to ensure the accurate placement of UAS. There were 10 patients required planned multiple surgical sessions because of massive stone burden. For these patients with multiple surgical sessions, the operative time for each session were amounted. The mean operative time was 69.2 ± 65.2 min. Immediate stone clearance was achieved in 172 (76.8%) cases. The SFR on postoperative day 30 was 97.3%. The overall complication rate in the study group was extremely lower. Post-operative fever (Clavien Ia) occurred in 2 patient and it was successfully managed by potent antibiotics.
Table 1.
Peri-operative data of 224 cases
| Peri-operative parameters | Value |
|---|---|
| Stone size (cm) | 2.2 ± 1.3 |
| Hounsfield Unit Value | 1019 ± 328 |
| Stone Distribution | |
| Renal Stone Only | 93 |
| Ureteral Stone Only | 63 |
| Renal and Ureteral Stone | 68 |
| Lower calyx involved | 96 |
| Pre-stented | 220 |
| Operation time(min) | 69.2 ± 65.2 |
| Use of basket(%) | 32.6 |
| Complications | |
| Clavien grade I | 2 |
| Clavien grade II-IV | 0 |
| Stone-free rates | |
| Immediate | 76.8% |
| 30 days postoperative | 97.3% |
The data was further stratified by stone burden, stone location and Hounsfield unit values (Table 2). We identified that SFR dramatically dropped when the stone size increased. For the patients with stone size ≤ 3 cm, the surgical duration and SFR was excellent. However, in the subgroup with stone size > 3 cm, the operation time prolonged (157.5 ± 108.1 min) and the final SFR decreased to 84.2%. Ten cases (26.3%) even required additional surgical session. The localization of stone did not significantly affect the final SFR. However, cases with lower calyx involvement consume more operation time. More baskets were applied in these cases. Totally, basket was utilized in 73 (32.6%) cases in our case series for stone relocation prior to laser lithotripsy and fragments extraction. In the subgroup with lower calyx stone, half cases needed basket for assistance. The Hounsfield unit values failed to present any significant effect on SFR. However, stone with Hounsfield unit > 1200 consumed more surgical time and would need additional surgical session more frequently.
Table 2.
Stratified peri-operative data
| n | Operation time(min) | Immediate SFR | SFR 30 days postoperative | multiple sessions | No. of basket(%) | |
|---|---|---|---|---|---|---|
| Stone size | ||||||
| <2 cm | 125 | 40.1 ± 22.4 | 84.8% | 100.0% | 0 | 31(24.8)* |
| 2-3 cm | 61 | 73.7 ± 28.9* | 77.0% | 100.0% | 0 | 28(45.9) |
| >3 cm | 38 | 157.5 ± 108.1* | 50.0%* | 84.2%* | 10* | 14(36.8) |
| Lower calyx involved | ||||||
| No | 90 | 48.0 ± 42.7 | 88.9% | 97.8% | 2 | 6(6.7) |
| Yes | 134 | 83.3 ± 73.5* | 68.6%* | 97.0% | 8 | 67(50.0) * |
| Hounsfield Unit Value | ||||||
| ≤1200Hu | 146 | 58.9 ± 49.8 | 80.8% | 98.6% | 3 | 48(32.9) |
| >1200Hu | 78 | 88.3 ± 84.0* | 69.2% | 96.1% | 7* | 25(32.0) |
*P < 0.05
Discussion
Recently, the improvement in flexible endoscopes, the accessories, and laser technology have made RIRS one of the most popular surgical choices in the management of upper urinary calculi [7, 8]. Thulium fiber laser (TFL), disposable flexible ureteroscope and suctioning UAS are considered as 3 game changers for RIRS [7]. Unfortunately, RIRS is restricted by several drawbacks. First, unlike PCNL, RIRS can not clear the fragments immediately. The requirement of multiple surgical sessions and unexpected re-admission are the main concerns. Even more, RIRS might cause the formation of steinstrasse while managing larger stone, which may require a series of surgical interventions [9]. The removal of small, asympatomatic kidney stones during surgery resulted in fewer subsequent emergency department visits, surgeries and stone regrowth in randomized controlled trial [10]. Second, the prolonged operation time and the rising intrarenal pressure would lead to reflux, and subsequently increase the risk of hemorrhage and infection [11]. One of the most important innovations to overcome these drawbacks is the application of UAS [7]. UAS allows multiple entrance of ureteroscope and facilitates active removal of the stone fragments during the procedure. However, with conventional UAS, the back-flow mainly depends on scope-sheath ratio [12] and the baskets should be used for fragments retrieval frequently.
To improve initial SFR of RIRS, several strategies have been introduced to optimize the procedure. Bryniarski et al. [13] introduced the method by modifying the position of the patient to relocate lower pole stones. Multescu et al. [14] recommended that fragmented the stone to the extractable fragments was the optimal lithotripsy method for stones larger than 1 cm because the dust may hinder visualization of the clear operative field and the difficulty of differentiating a small fragmented stone in the midst of dust. Currently, the vacuum assisted UAS greatly improved the efficiency. It is able to aspirate the tiny fragments during lithotripsy simultaneously. Zeng et al. [15] revealed that suction UAS could improve stone clearance, optimize visual field and reduce stone retropulsion. Chen et al. [16] introduced a novel method to aspirate the fragments directly by suction UAS combined with artificial saline circulation, which could reduce the use of baskets and thus decrease the operation time and medical costs.
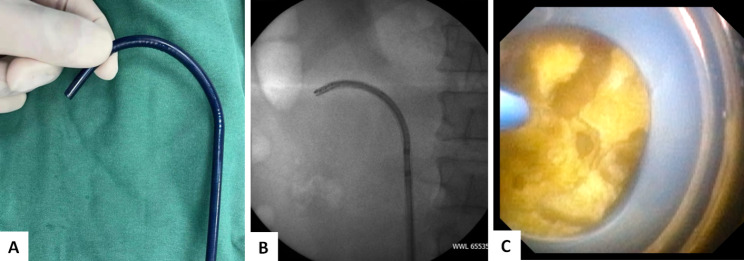
However, the conventional suction UAS usually cannot pass through the ureteropelvic junction (UPJ) and get close to the stone. So the aspiration effect will be weakened and the efficiency of fragments clearance is limited. The application of our tip-bendable UAS can overcome the shortcoming from the conventional suction UAS. The proximal 10 cm tip of our novel UAS is bendable. It can cross over the UPJ and be passively navigated to the targeted renal calyx or stone surface (Fig. 1). The oblique suction-evacuation channel can provide continuous aspiration effect towards specific calyx or fragments, thus made the fragments being washed out by the vortex flow much more efficiently while maintaining a clear operative vision (Fig. 2). It can efficiently remove fragments, which can achieve an ideal stone free rate of 97.3% in our case series. The tip-bendable UAS is compatible to regular vacuum system. It is easy to be manipulated and the learning curve is steeper.
Fig. 1.
The proximal 10 cm tip of the novel UAS is bendable (A). The UAS can be passively deflected and navigated into the targeted calyx (B) or the stone surface (C)
Fig. 2.
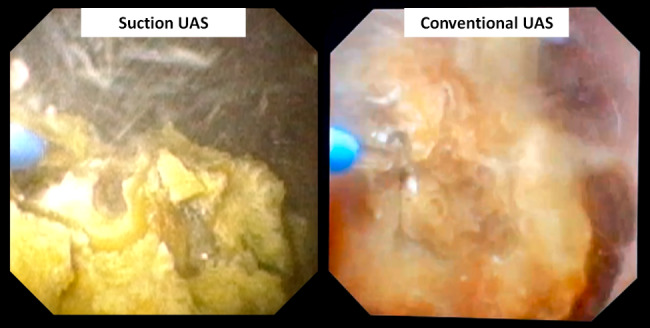
The tip-bendable suction UAS can provide better surgical vision while comparing with the conventional UAS
In our current case series, we also identified the following features. First, stone size does matter a lot. Benefiting from the direct suction effect of tip-bendable UAS, the potential for SFR can approach those of percutaneous surgery for small to moderate-sized stone. In our current study, for patients with stone size ≤ 3 cm, both surgical duration and SFR were comparable with PCNL as reported in the literatures [17, 18]. However, the enlarged stone size deteriorates the SFR and consumes more operative time. For larger stone (> 3 cm), the final SRF is dramatically reduced to 84.2% and operative time is significantly prolonged. Larger stone will also bring extra surgical session for the patients. However, since it can maintain low intra-renal pressure during the whole procedure, which made the RIRS a safe approach for stone with larger size. In all of our cases, only two patients suffered from fever.
Second, the maximal deflection of the tip-bendable UAS is limit and depends on flexibility of ureteroscope. It cannot reach the inferior calyx when the IPA is sharp. In such cases, accessing the lower pole to treat the stone in situ becomes difficult. So, when inferior calyx stone presented, baskets should be applied for stone relocation or fragments retrieval. In the subgroup with lower calyx stone, the basket was used much more frequently.
Third, the effect of stone density was also assessed. Hounsfield density used to be an important parameter to predict the outcome of RIRS [19]. In our study, we assigned 1200 Hu as a specific threshold to stratify the hardness into two categories. However, there were no significant differences in operative time, SRF and basket usage between the two categories. Possibly, because our laser setting is effective enough to handle all types of stones. As we have noticed, for stone with Hounsfield density > 1200 Hu, more fragments would be produced. We should withdrawal the scope much more frequently to facilitate fragments aspiration during the procedure, which pose the scope to the risk of damage and lower the efficiency. Two strategies may further optimize the procedure. Laser with efficient dusting property, such as TFL, will generate smaller particles and obtain higher stone clearance [20, 21]. Smaller caliber endoscopes will bring an ideal scope-sheath ratio allows larger fragments to be aspirated out without scope withdraw, thus enhance the stone clearance [22].
Our current study also had several limitations. The study was in retrospective observational design. Since it was our initial clinical experience, the sample size was still small. So, our study was insufficient to validate the superiority of current technique over conventional techniques. Larger-scale prospective comparative study should be conducted to confirm our hypothesis. Besides, most cases in our study were pre-stented to facilitate the UAS insertion. Smaller caliber UAS cooperated with novel endoscopes may overcome the drawback.
Conclusion
Our present study showed that RIRS with tip-bendable UAS was promising in the management of upper urinary tract stones. It is safe and effective. Prospective randomized trials would be required to further delineate the superiority over conventional RIRS and PCNL.
Acknowledgements
None.
Authors’ contributions
H.L., L.L. and Y.L. performed the surgery. H.L. and Y.L. wrote the main manuscript text. L.L. conducted the follow-up. Y.Y., X.X., Z.L. and J.S. collected the data and finished the statistical analysis. B.S. designed the study and provided figures. All authors reviewed the manuscript.
Funding
This work was supported by Zhejiang Medicine and Health Program (2018KY853).
Data Availability
The original data in the current study was available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This retrospective study was approved by the Ethics Committee of Xinchang County Hospital of Traditional Chinese Medicine and the 1st Affiliated Hospital of Zhejiang University, School of Medicine. The study was conducted in compliance with the principles of the Declaration of Helsinki. All procedures followed applicable guidelines and regulations. Informed written consent was also obtained from the patients in this study.
Consent for publication
Not applicable.
Competing interests
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhang L, Zhang X, Pu Y, Zhang Y, Fan J. Global, Regional, and National Burden of Urolithiasis from 1990 to 2019: a systematic analysis for the global burden of Disease Study 2019. Clin Epidemiol. 2022;14:971–83. doi: 10.2147/CLEP.S370591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.EAU Guidelines. Edn. presented at the EAU Annual Congress Milan 2023. ISBN 978-94-92671-19-6.
- 3.Takazawa R, Kitayama S, Tsujii T. Successful outcome of flexible ureteroscopy with holmium laser lithotripsy for renal stones 2 cm or greater. Int J Urol. 2012;19(3):264–7. doi: 10.1111/j.1442-2042.2011.02931.x. [DOI] [PubMed] [Google Scholar]
- 4.Riley JM, Stearman L, Troxel S. Retrograde Ureteroscopy for renal stones larger than 2.5 cm. J Endourol. 2009;23(9):1395–8. doi: 10.1089/end.2009.0391. [DOI] [PubMed] [Google Scholar]
- 5.Niwa N, Matsumoto K, Ohigashi T, et al. Clinical outcomes of Retrograde Intrarenal Surgery as a primary treatment for Staghorn Calculi: a single-center experience. Clin Med Insights: Urol. 2019;12. 10.1177/1179561119854772.
- 6.Corrales M, Sierra A, Doizi S, Traxer O. Risk of Sepsis in Retrograde Intrarenal Surgery: a systematic review of the literature. Eur Urol Open Sci. 2022;44:84–91. doi: 10.1016/j.euros.2022.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Coninck V, Somani B, Sener ET, Emiliani E, Corrales M, Juliebø-Jones P, Pietropaolo A, Mykoniatis I, Zeeshan Hameed BM, Esperto F, Proietti S, Traxer O, Keller EX. Ureteral Access sheaths and its use in the future: a Comprehensive Update based on a literature review. J Clin Med. 2022;11(17):5128. doi: 10.3390/jcm11175128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Traxer O, Corrales M. Managing Urolithiasis with Thulium Fiber laser: updated real-life Results-A systematic review. J Clin Med. 2021;10(15):3390. doi: 10.3390/jcm10153390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Birowo P, Rasyid N, Atmoko W, Sutojo B. Case Report: an occurrence of steinstrasse in retrograde intra renal Surgery (RIRS) for large staghorn kidney stone: a difficult experience in managing surgical outcomes. F1000Res. 2020;9:184. doi: 10.12688/f1000research.22448.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sorensen MD, Harper JD, Borofsky MS, Hameed TA, Smoot KJ, Burke BH, Levchak BJ, Williams JC, Jr, Bailey MR, Liu Z, Lingeman JE. Removal of small, asymptomatic kidney stones and incidence of Relapse. N Engl J Med. 2022;387(6):506–13. doi: 10.1056/NEJMoa2204253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sugihara T, Yasunaga H, Horiguchi H, Nishimatsu H, Kume H, Ohe K, Matsuda S, Fushimi K, Homma Y. A nomogram predicting severe adverse events after ureteroscopic lithotripsy: 12 372 patients in a Japanese national series. BJU Int. 2013;111(3):459–66. doi: 10.1111/j.1464-410X.2012.11594.x. [DOI] [PubMed] [Google Scholar]
- 12.Fang L, Xie G, Zheng Z, Liu W, Zhu J, Huang T, Lu Y, Cheng Y. The effect of ratio of endoscope-sheath diameter on intrapelvic pressure during flexible ureteroscopic lasertripsy. J Endourol. 2019;33(2):132–9. doi: 10.1089/end.2018.0774. [DOI] [PubMed] [Google Scholar]
- 13.Bryniarski P, Paradysz A, Zyczkowski M, Kupilas A, Nowakowski K, Bogacki R. A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal Surgery in the management of renal stones more than 2 cm in diameter. J Endourol. 2012;26(1):52–7. doi: 10.1089/end.2011.0235. [DOI] [PubMed] [Google Scholar]
- 14.Mulţescu R, Geavlete B, Georgescu D, Geavlete P, Chiuţu L. Holmium laser intrarenal lithotripsy in pyelocaliceal lithiasis treatment: to dust or to extractable fragments? Chirurgia (Bucur). 2014 Jan-Feb;109(1):95–8. [PubMed]
- 15.Zeng G, Wang D, Zhang T, Wan SP. Modified Access Sheath for continuous Flow Ureteroscopic lithotripsy: a preliminary Report of a Novel Concept and technique. J Endourol. 2016;30(9):992–6. doi: 10.1089/end.2016.0411. [DOI] [PubMed] [Google Scholar]
- 16.Chen HQ, Chen ZY, Zeng F, Li Y, Yang ZQ, He C, He Y. Comparative study of the treatment of 20–30 mm renal stones with miniaturized percutaneous nephrolithotomy and flexible ureterorenoscopy in obese patients. World J Urol. 2018;36(8):1309–14. doi: 10.1007/s00345-018-2258-y. [DOI] [PubMed] [Google Scholar]
- 17.Zhao Z, Sun H, Zeng T, Deng T, Liu Y, Zeng G. An easy risk stratification to recommend the optimal patients with 2–3 cm kidney stones to receive retrograde intrarenal Surgery or mini-percutaneous nephrolithotomy. Urolithiasis. 2020;48(2):167–73. doi: 10.1007/s00240-019-01134-0. [DOI] [PubMed] [Google Scholar]
- 18.Wang C, Wang S, Wang X, Lu J. External validation of the R.I.R.S. scoring system to predict stone-free rate after retrograde intrarenal Surgery. BMC Urol. 2021;21(1):33. doi: 10.1186/s12894-021-00801-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keat WOL, Somani BK, Pietropaolo A, Chew BH, Chai CA, Inoue T, Ragoori D, Biligere S, Galosi AB, Pavia MP, Milanese G, Ahn T, More S, Sarica K, Traxer O, Teoh JY, Gauhar V, Castellani D. Do Hounsfield units have any significance in predicting intra- and postoperative outcomes in retrograde intrarenal Surgery using Holmium and Thulium fiber laser? Results from the FLEXible ureteroscopy outcomes Registry (FLEXOR). World J Urol. 2023 Mar;16. 10.1007/s00345-023-04362-7. [DOI] [PubMed]
- 20.Jiang P, Peta A, Brevik A, Arada RB, Ayad M, Afyouni AS, Limfueco L, Nguyen N, Palma A, Patel RM, Landman J, Clayman RV. Ex vivo Renal Stone Dusting: impact of laser modality, Ureteral Access Sheath, and suction on Total Stone Clearance. J Endourol. 2022;36(4):499–507. doi: 10.1089/end.2021.0544. [DOI] [PubMed] [Google Scholar]
- 21.Jiang P, Okhunov Z, Afyouni AS, Ali S, Hosseini Sharifi SH, Bhatt R, Brevik A, Ayad M, Larson K, Osann K, Patel RM, Landman J, Clayman RV. Comparison of Superpulse Thulium Fiber Laser vs Holmium laser for ablation of renal calculi in an in vivo Porcine Model. J Endourol. 2023;37(3):335–40. doi: 10.1089/end.2022.0445. [DOI] [PubMed] [Google Scholar]
- 22.Gauhar V, Traxer O, Castellani D, Ragoori D, Heng CT, Chew BH, Somani BK, Bin Hamri S. A feasibility study on clinical utility, Efficacy and limitations of 2 types of flexible and navigable suction Ureteral Access sheaths in Retrograde Intrarenal Surgery for Renal stones. Urol 2023;14:S0090-4295(23)00479-X. 10.1016/j.urology.2023.05.032. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original data in the current study was available from the corresponding author on reasonable request.