Abstract
Introduction:
The mainstay of endovascular treatment in peripheral arterial disease is digital subtraction angiography with an iodinated contrast. In patients with a known contrast allergy, the current most commonly used alternative is to perform carbon dioxide angiography. Operator experience and availability of carbon dioxide (CO2) angiography delivery systems are, however, limited. Intravascular ultrasound is now commonly used in combination with fluoroscopy in peripheral venous interventions and in coronary arterial disease and we propose that this also provides a safe and effective alternative option to guide endovascular intervention in patients with a known contrast allergy.
Case report:
We present a case describing the use of intravascular ultrasound and fluoroscopy to guide endovascular treatment of a critical left common iliac artery stenosis in a patient with known anaphylaxis to iodinated contrast.
Discussion:
Intravascular ultrasound is fast becoming the gold standard treatment option in peripheral venous interventions; however, the use in peripheral arterial disease is limited. We believe this is the first case that reports the use of predominantly intravascular ultrasound in endovascular peripheral arterial intervention with a contrast adjunct.
Conclusion:
We have demonstrated that intravascular ultrasound is a safe and effective alternative or adjunct to iodinated contrast for arterial angiography and stenting in the setting of patient contra-indications.
Keywords: Endovascular, ultrasound, peripheral arterial disease, IVUS, intravascular
A 67-year-old retired community nurse presented to the vascular surgery outpatient clinic with 1 year of gradual-onset left buttock claudication and reduced exercise tolerance. Her past medical history includes hypertension, for which she takes an angiotensin-converting enzyme (ACE) inhibitor, and she had a smoking history of 25 pack-years. Three years previously, she had an anaphylactic reaction to iodine contrast media when undergoing computed tomography (CT) for investigation of recurrent urinary tract infections. Ankle-Brachial Pressure Index (ABPI) was recorded as 0.57 in the outpatient clinic, and therefore the initial investigation was undertaken using ultrasound duplex scanning and magnetic resonance angiography (MRA). This demonstrated a critical stenosis of the left common iliac artery (Figure 1) with 45%–49% stenosis proximally 22 mm from the aortic bifurcation and up to 95% stenosis more distally with a peak systolic velocity of 229.3 cm/s. The vascular surgery team referred her to interventional radiology for potential endovascular treatment. Given the known iodine contrast allergy, conventional angiography was contraindicated, and therefore other potential techniques were discussed within a multidisciplinary team meeting. The decision to go ahead with the use of intravascular ultrasound (IVUS) was initiated following recent success at our institution with the use of IVUS in venous stenoses and venous stenting as well as very limited access to other techniques such as carbon dioxide (CO2) angiography.
Figure 1.
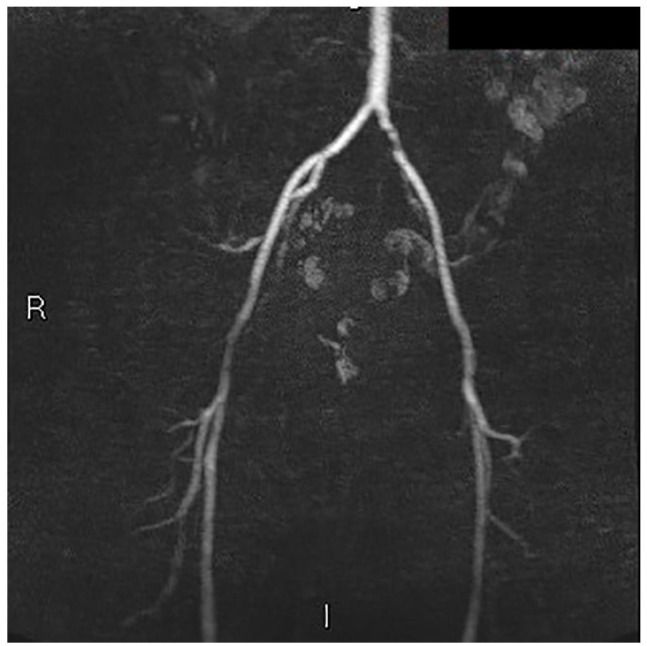
Magnetic resonance angiography demonstrating critical stenosis of the left common iliac artery.
The patient was admitted to hospital under the care of the vascular surgeons and attended the interventional radiology department. Following informed written consent, retrograde access to the left common femoral artery was gained under ultrasound guidance. A 45-cm 6-French vascular sheath was inserted over a stiff 0.035-inch guidewire before the iliac stenosis was crossed without any tactile resistance under fluoroscopy with a 0.035-inch Terumo hydrophilic guidewire and Cobra guide catheter. The catheter was then exchanged over an Amplatz stiff guide wire for the reconnaissance PV .018 IVUS catheter.
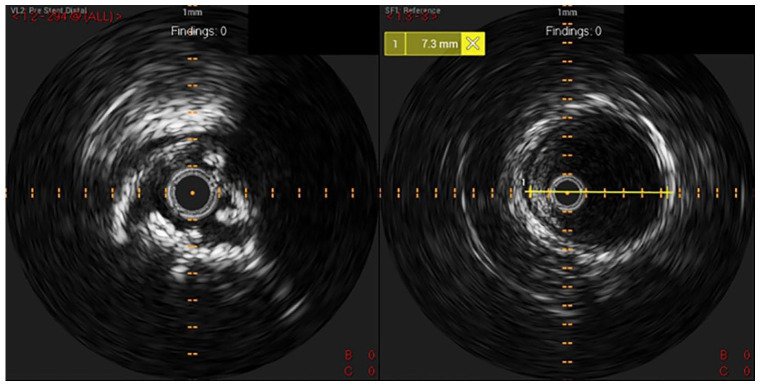
The common iliac artery stenosis was then assessed using a combination of fluoroscopic images and the IVUS, mapping the stenosis and bookmarking the point at which the IVUS marker reached the proximal and distal ends of the stenosis (Figure 2). Using the IVUS, the calcified plaque on the arterial walls could be clearly visualised and the tight stenosis in the cross section can be uniquely demonstrated. Using the IVUS images, the diameter of the normal disease-free common iliac artery was measured to confirm the stent diameter required (Figure 2). Prior ultrasound duplex had demonstrated that the internal iliac artery in this patient was already occluded, and therefore the stent could be safely extended past its origin into the disease-free external iliac artery; however, the internal iliac origin can also be visualised on the IVUS.
Figure 2.
Intravascular ultrasound images demonstrating the critical common iliac artery stenosis and the normal common iliac artery where luminal diameter can be measured as shown.
An 8 × 57-mm balloon-mounted stent (Bentley BeSmooth) was deployed. We elected to deploy a balloon-mounted system because from previous operator experience, placement is more controlled and precise during deployment. Before advancing the stent, the lesion was crossed with the 6-French vascular sheath to minimise the risk of stent displacement. After retraction of the sheath, the stent was deployed under fluoroscopy at the prior marked position.
Following deployment, the IVUS catheter was used again to re-image the iliac artery and assess the stent position and patency. This confirmed good stent apposition (see Figure 3). For further confirmation and visualisation, a single-hand injection run of digital subtraction angiography (DSA) was captured using a Gadolinium-based contrast with a total volume of 6 mL (the maximum volume which could be utilised using a dose calculation of 0.3 mL/kg or 20 mL). This clearly confirmed a very good result from the iliac stent deployment (Figure 4). The puncture site was closed using a 6-French vascular closure device (Angio-Seal; Terumo Medical Corporation). There were no immediate complications and the patient remained as an inpatient overnight for monitoring. On subsequent outpatient follow-up, the patient’s ABPI measurement had improved to 0.87 on the left side and there had been a significant improvement in claudication symptoms with the patient able to walk approximately 5 times further than previously.
Figure 3.
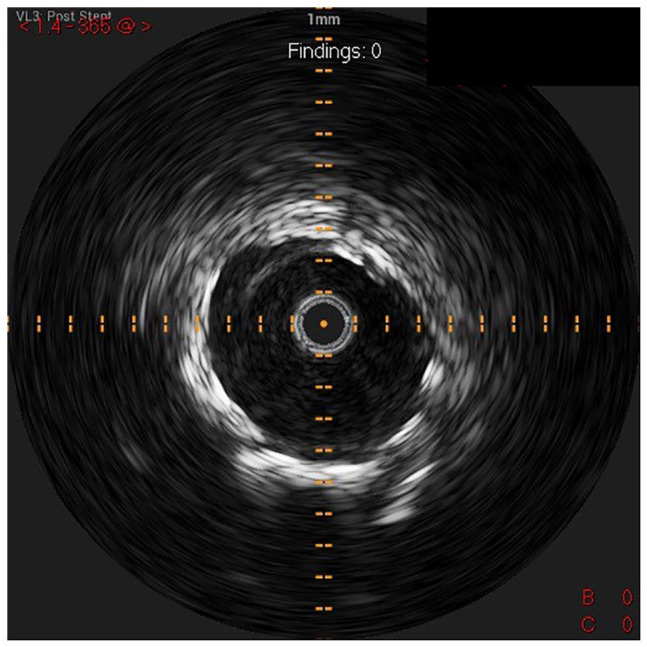
In-stent IVUS imaging at the site of previous stenosis showing successful deployment and stent apposition.
Figure 4.
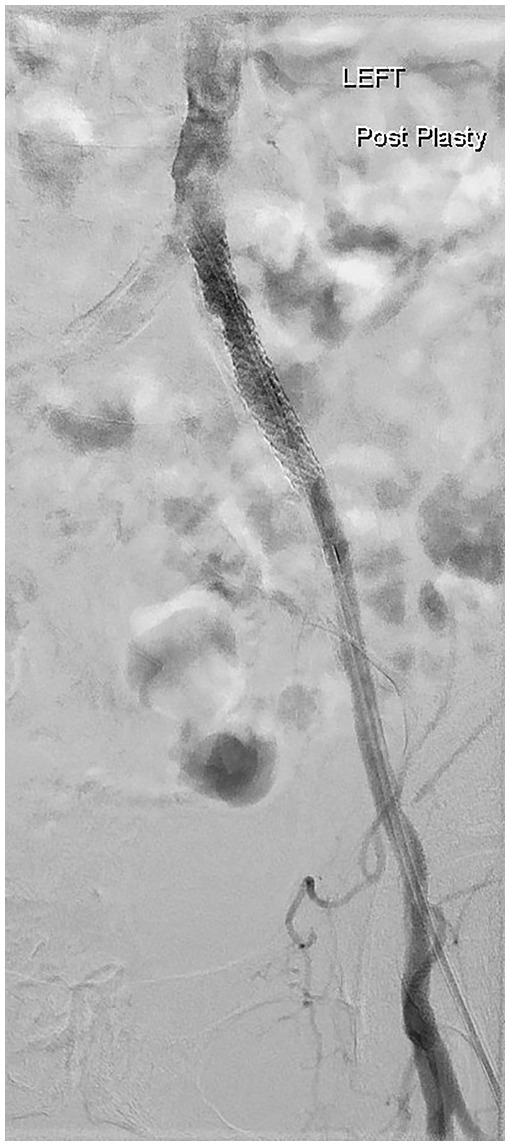
Post stent deployment digital subtraction angiography using a Gadolinium-based contrast, confirming procedural success and stent patency.
Discussion
IVUS has already been introduced as an adjunct to standard DSA in percutaneous arterial, venous and coronary interventions. The advantages of IVUS include offering detailed three-dimensional intraluminal imaging of blood vessels, accurate location and mapping of stenoses, detailing precise plaque characteristics and assessing for stent expansion post intervention. 1 The combination of IVUS and digital subtraction venography is quickly becoming the gold standard in endovascular treatment for multiple venous conditions, including iliac vein compression syndrome (May-Thurner) and mechanical thrombectomy for deep venous thrombosis, as well as showing promise as a useful adjunct in peripheral arterial intervention. 2 There have been reported cases of the sole use of IVUS for venoplasty and coronary artery intervention in cases of known patient contrast allergy.3,4 However, to our knowledge, there are no previous case reports of the use of IVUS for peripheral arterial disease without iodinated contrast.
Conclusion
In conclusion, we have demonstrated that IVUS is a safe and effective alternative or adjunct to iodinated contrast for arterial angiography and stenting in the setting of patient contra-indications, providing both the diagnostic information required to assess a stenosis and accurate siting for stent deployment.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Permission from patient(s) or subject(s) obtained in writing for publishing their case report: Yes
Permission obtained in writing from patient or any person whose photo is included for publishing their photographs and images: Yes
Confirm that you are aware that permission from a previous publisher for reproducing any previously published material will be required should your article be accepted for publication and that you will be responsible for obtaining that permission: Yes
Guarantor: C.F. is the guarantor of this article.
Contributors: C.F. wrote the first version of the manuscript. K.L. conceived project and reviewed and edited the manuscript and approved the final version of the manuscript.
ORCID iD: Charles Fee  https://orcid.org/0000-0002-0045-8498
https://orcid.org/0000-0002-0045-8498
References
- 1. Darmoch F, Chadi Alrais M, Al-Khadra Y, et al. Intravascular ultrasound imaging-guided versus coronary angiography-guided percutaneous coronary intervention: a systematic review and meta-analysis. J Am Heart Assoc 2020; 9: e013678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Loffroy R, Falvo N, Galland C, et al. Intravascular ultrasound in the endovascular treatment of patients with peripheral arterial disease: current role and future perspectives. Front Cardiovasc Med 2020; 7: 551861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang X, Yu C, Chen G, et al. Iliac vein stenting guided by intravascular ultrasound without iodinated contrast medium. Vasa 2021; 50: 68–73. [DOI] [PubMed] [Google Scholar]
- 4. Okura H, Nezuo S, Yoshida K. Successful stent implantation guided by intravascular ultrasound and a Doppler guidewire without contrast injection in a patient with allergy to iodinated contrast media. J Invasive Cardiol 2011; 23: 297–299. [PubMed] [Google Scholar]