The optimal strategy to manage hypoxaemic respiratory failure associated with COVID-19 remains uncertain. Potentially overwhelming demand on critical care resources requires strategies to reduce progression to invasive ventilation. Awake prone positioning has been proposed, 1 with evidence that it is associated with improved oxygenation in selected patients.2–5 The aim of this study is to report our experience using APP and its impact on respiratory physiology in COVID-19.
Methods
A retrospective observational cohort study was conducted between 1 April 2020 and 20 May 2020. An APP protocol was established for adult patients with COVID-19, requiring an inspired fractional concentration of oxygen (FiO2) ≥ 0.28 to maintain peripheral oxygen saturations (SpO2) 92–96%, in line with national guidelines. 1 Patients requiring immediate intubation, with cardiovascular instability, altered consciousness or other factors rendering APP unsafe were excluded. Patients were required to independently self-prone and free to cease at any stage. APP was commenced in the Emergency Department or wards, aiming for at least 30 min initially, with immediate supervision. Observations, including FiO2, SpO2 and respiratory rate (RR), were recorded at baseline (pre-proning), 5 and 30 min post-proning. If tolerated and beneficial, APP was encouraged for up to 4 h, twice a day. Patients who were for escalation were transferred to critical care for ongoing APP. Those limited to ward-based therapy continued APP in designated wards supervised by the attending teams. No patients received concurrent continuous positive airway pressure.
Data were extracted from the electronic medical record. SpO2/FiO2 ratio was calculated for the first APP session. Where arterial blood gas (ABG) data were available for subsequent sessions, arterial partial pressure of oxygen (PaO2)/FiO2 ratio and shunt fraction were calculated, assuming pulmonary end-capillary oxygen saturation 100% for ventilated lung units and central venous oxygen saturation 70%. Statistical analysis was performed using R (version 4.0.0, www.r-project.org). Wilcoxon signed-rank tests were used for paired comparisons, Friedman test with Bonferroni correction for >2 sequential comparisons and Mann–Whitney–Wilcoxon tests for unpaired data. All tests were two-sided. p < 0.05 was considered significant.
Results
Seventeen patients with COVID-19 received APP and were included; four for ward-based care and 13 admitted to critical care, one of whom had subsequent limitations. Fifteen (88.2%) were male, age was 63.0 [55.0–69.0] years, BMI 26.1 [24.4–28.1] kg/m2. Time from hospital admission to first APP was 94.8 [19.8–145.0] hours and the duration of initial APP trial was 55.0 [30.0–116.3] minutes. APP was performed for three [1–3] days with the total duration of 9.2 [5.2–17.6] hours over five [2.8–10.0] sessions. Twelve patients (70.6%) laid both prone and laterally and five (29.4%) laid prone only. APP was well tolerated; only one patient declined APP beyond their initial session. All patients had bilateral infiltrates on chest radiograph, elevated RR 22.0 [19.8–27.3] breaths/min and were hypoxic at baseline (SpO2/FiO2 156.7, [123.8–232.5]).
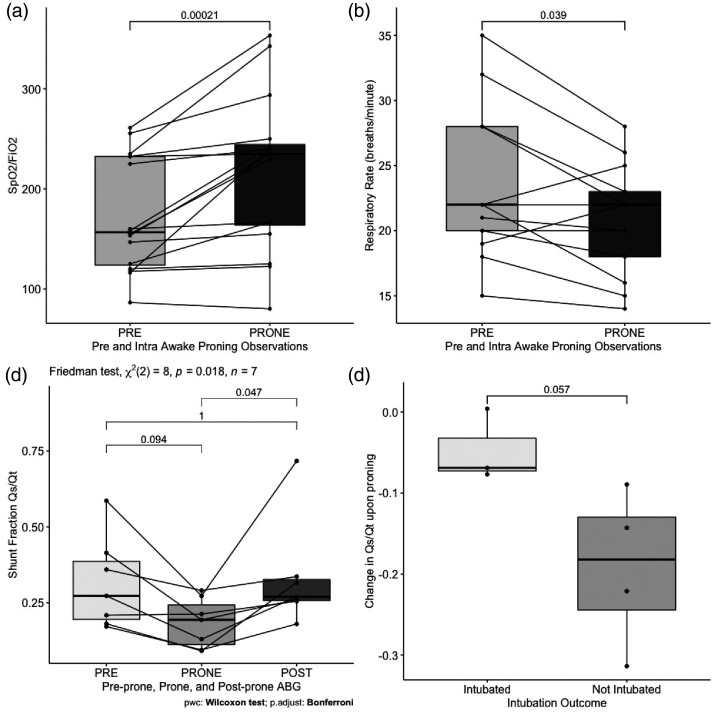
Following APP, SpO2/FiO2 increased (+27.8 [6.3–82.3]; p < 0.001) (Figure 1(a)) and RR decreased (−2 breaths/min, [−6–0]; p = 0.039) (Figure 1(b)). In the subgroup with ABG data, PaO2/FiO2 increased (+9.8 kPa [2.2–13.1]; p = 0.016, p.adj = 0.047) and shunt fraction decreased (−8.9% [−18.2 – −7.3]; p = 0.031, p.adj = 0.094). Following supination, both PaO2/FiO2 (−3.0 kPa [−3.3– −1.6]; p = 0.016, p.adj = 0.047)) and shunt (+8.6% [5.6–18.3]; p = 0.016, p.adj = 0.047) reverted to pre-APP levels (Figure 1(c)). The decrease in shunt was 6.9% [7.3–3.2] in those subsequently intubated versus 18.2% [24.4–13.0] in those not requiring intubation (p = 0.057) (Figure 1(d)). Time from first APP to intubation was 32.3 [8.7–90.9] hours; two patients required emergency intubation. Critical care length of stay was four [3.5–6.5] days in unintubated and 26 [20–65] days in intubated patients, with ventilation for 20 [19–61] days. Overall hospital mortality was 35.3% (6/17); 25.0% (3/12) in those without limitations of therapy.
Figure 1.
Effect of awake prone positioning (APP) on physiological parameters. (a) Peripheral oxygen saturations (SpO2, %)/Inspired fractional concentration of oxygen (FiO2) ratio in paired data pre- and intra-APP trial (n = 16). p = 0.00021; two-sided Wilcoxon signed-rank test. (b) Respiratory rate (breaths/minute) in paired data pre- and intra-APP trial (n = 13). p = 0.039; two-sided Wilcoxon signed-rank test. (c) Calculated shunt fraction in paired data pre-, intra- and post-APP trial (n = 7). Pre-prone (PRE) to prone (PRONE) p = 0.031, p.adj = 0.094 and prone (PRONE) to supine (POST) p = 0.016, p.adj = 0.047; Friedman test (p) with Bonferroni correction (p.adj). (d) Unpaired data showing the change in calculated shunt fraction upon proning by intubation status (n = 7), p = 0.057; Mann–Whitney–Wilcoxon test.
FiO2: inspired fractional concentration of oxygen; Qs: pulmonary physiologic shunt (mL/min); Qt: cardiac output (mL/min); SpO2: peripheral oxygen saturations.
Discussion
These data demonstrate that APP is a feasible, tolerable and effective technique to improve acute respiratory physiology in hypoxaemic patients with COVID-19, including those for ward-based care only. Implementation was straightforward and the technique is potentially transferable to low resource settings. Whilst our ABG data represents a subgroup, it indicates that improvement in oxygenation is non-sustained. The relationship between improvement in shunt and requirement for intubation is interesting but inconclusive, due to small sample and potential confounding. Notably, 45% of patients who were for escalation failed APP, requiring intubation; therefore we recommend that, where appropriate, APP occurs in areas where prompt intubation is deliverable. If APP avoids intubation there is potential to significantly reduce demand for ventilators. However, potential benefits must be balanced against risks associated with delayed intubation. 6 In conclusion, our study shows that APP is feasible and can achieve improvements in gas exchange. The effects on intubation rate and outcome of these transient changes in oxygenation warrant prospective trials.
Ethics approval
Research Ethics Committee approval was granted (20/HRA/1871).
Availability of data and material
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
This study was devised by GG and NK. Data were collected by NK and AC and analysed by NK. AC, AG, SD and GG devised the APP protocol. The article was drafted by NK, GG and LC. All authors reviewed the article and contributed to the final draft.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Nicola L Kelly https://orcid.org/0000-0003-0368-0016 Alexandra Curtis https://orcid.org/0000-0002-9526-2059
References
- 1.Bamford P, Bentley A, Dean J, et al. ICS guidance for prone positioning of the conscious COVID patient 2020, https://emcrit.org/wp-content/uploads/2020/04/2020-04-12-Guidance-for-conscious-proning.pdf (accessed 17 September 2020).
- 2.Caputo ND, Strayer RJ, Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ED’s experience during the COVID-19 pandemic. Acad Emerg Med 2020; 27: 375–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sartini C, Tresoldi M, Scarpellini P, et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA. Epub ahead of print 15 May 2020. DOI: 10.1001/jama.2020.7861. [DOI] [PMC free article] [PubMed]
- 4.Elharrar X, Trigui Y, Dols A-M, et al. Use of Prone Positioning in Nonintubated Patients With COVID-19 and Hypoxemic Acute Respiratory Failure. JAMA. Epub ahead of print 2020. DOI: 10.1001/jama.2020.8255. [DOI] [PMC free article] [PubMed]
- 5.Coppo A, Bellani G, Winterton D, et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med 2020; 8(8): 765–774. DOI:10.1016/S2213-2600(20)30268-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med 2020; 46: 1099–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.