Abstract
Background: Studies are needed to evaluate medication-related problems (MRPs) to assess the effect of a pharmacist on managing medications postdischarge. Objective: To assess the ability of pharmacist-led medication review and reconciliation to reduce the number of MRPs found in transitional care medicine (TCM) visits, leading to medication optimization. Methods: This study involved a retrospective chart review of standard TCM procedure at a family/internal medicine clinic and a prospective, team-based TCM visit in the same clinic. Inclusion criteria included patients discharged from any hospital within our institution and seen in the clinic. The primary outcome was the difference in the proportion of MRPs found between the prospective and retrospective groups. Secondary outcomes included the number and specific type of MRPs found, classified by the Pharmaceutical Care Network Europe tool, and further subdivided by patient aware or unaware of MRP, only in the prospective group, as well as 30-day readmission rate. Results: Patients in the prospective group (n = 50) had an average age of 67.9 years versus 65.5 years in the retrospective group (n = 50). Four times as many patients in the prospective group were found to have MRPs than the retrospective group. The most common MRP was due to a patient-related factor, meaning the cause is related to a patient’s behavior. Patients were unaware of the MRP in a majority of these cases. Thirty-day readmission rate did not differ between the groups. Conclusion: Team-based TCM visits that included a pharmacist-led medication reconciliation uncovered more MRPs than patients who did not have a pharmacist perform a medication reconciliation.
Keywords: ambulatory care, drug-related problems, medication errors, medication safety, adherence
Introduction
Medication-related problems (MRPs) have been found to commonly occur during transitions of care, and 30-day readmission rates are nearly 20% in those who are discharged.1,2 An MRP is an event or circumstance involving drug therapy that actually or potentially interferes with desired health outcomes. Patients who are at higher risk for readmission include those with multiple comorbidities such as chronic heart failure (CHF), chronic obstructive pulmonary disorder (COPD), and other chronic diseases. 3 Pharmacists in ambulatory care play a key role in managing chronic diseases. Multiple studies have shown the benefit on hemoglobin A1c, blood pressure, and low-density lipoprotein cholesterol when managed with the help of a pharmacist. 4 Quality of prescribing and adherence improves in patients who receive pharmacist-run medication management. 5 Major targets for Centers of Medicare and Medicaid (CMS) and reimbursement include hospital 30-day readmission rates and patient adherence. 3 Hospital performance measured by CMS takes into account several major diagnoses, such as CHF and COPD. A hospital’s reimbursement is then calculated by taking these diagnoses and their current readmission rates into account. The better the readmission rates, the higher the reimbursement the hospital receives. Ambulatory care pharmacists support patients who are at high risk of readmission by managing their medications postdischarge. Several retrospective and prospective studies, described below, have been performed in this setting, with results showing a benefit in patients who participate in discharge follow-up with a pharmacist.
The investigators of the PATCH 6 (Pharmacist Ad-vancement of Transitions of Care to Home) trial examined the impact of the inpatient to outpatient transition of care (TCM [transitional care medicine]) process by implementing a face-to-face pharmacist visit in addition to a physician follow-up visit. The pharmacist visit focused on identifying MRPs. Forty-nine MRPs were identified in the group that had an additional pharmacist visit. Twenty-nine percent of MRPs discovered consisted of adherence or access issues. Other major MRPs found included inappropriate combination of drugs, no therapeutic monitoring, and too low or high of medication doses. The PATCH trial highlights the effectiveness of pharmacists identifying MRPs during TCM patient visits.
Investigators of another trial examining involvement of pharmacist follow-up after discharge by phone call showed similar results. 7 This retrospective chart review grouped patients into those reachable by phone and not reachable. Medication reconciliation was the primary focus of the postdischarge phone call with a primary outcome of any readmission or emergency department (ED) visit within 30 days. Patients in the pharmacist intervention group demonstrated a decreased rate (visits/patient) of readmission or ED visit (0.227 vs 0.519, P < .001).
The studies described previously6,7 show promising results when examining the outcome of 30-day readmission; however, there are many factors that affect readmission. Lack of adherence is a major barrier to patient care and plays a large role in readmission rates. 8 The medications that have shown beneficial mortality data and reduced hospital admission rates are life-long; therefore, it is imperative that patients understand the necessity of adherence to medication regimens. Evaluators of adherence have found that the most common type of adherence issue involved patients taking medications inappropriately due to unawareness of the medication regimen. Other adherence problems include lack of knowledge about the medication and adverse reactions. These issues related to a medication regimen are classified as MRPs and can be the underlying cause of nonadherence. The purpose of this study is to assess the proportion of MRPs in patients receiving face-to-face pharmacist-led medication reconciliation.
Methods
The first phase of this study involved a retrospective electronic medical record (EMR) review of the standard TCM protocol, conducted on patients with scheduled TCM visits from July to September 2018. The second phase involved face-to-face visits with patients scheduled for a team-based TCM appointment from October 2018 until February 2019. This study was reviewed and approved by the institutional review board.
Standard TCM protocol at the Cleveland Clinic Foundation (CCF) involves several steps postdischarge. CCF consists of 1 quaternary care main campus with 11 regional hospitals throughout the city. This study was conducted at one of the regional hospitals, Hillcrest Hospital’s, Internal/Family Medicine clinic, located near the hospital. The TCM practice exists throughout the entire institution; however, each regional hospital and associated outpatient clinic run their own TCM practice. The standard TCM protocol begins with a call from a health care professional to the patient, within 48 hours of discharge, to perform a medication reconciliation. An internal readmission risk prioritization tool categorizes patients as high, medium, and low risk for readmission. Several of the variables that affect this readmission risk score are number of hospitalizations in previous 12 months, number of ED visits in past 6 months, history of COPD, or active anticoagulant order. Patients considered high risk for readmission are called by a care coordinator. Those deemed moderate risk are called by a pharmacist. The patient is asked about any concerns they may have about their medication regimen, new medications postdischarge, and which were held or discontinued. Adherence to the postdischarge medication regimen is assessed with the use of standardized questions and counseling is provided as deemed necessary. MRPs found during the phone call are documented in the patients EMR. All patients discharged from any CCF hospital are seen within 7 to 14 days of discharge. The TCM practice is a subclinic within Hillcrest’s outpatient, physician-run Family/Internal Medicine clinic, which services patients whose primary care physician (PCP) is located at this clinic. The clinic focuses mainly on chronic disease state management and has approximately 80 patient visits per day, and 1760 visits per month. Prior the implementation of this study, the pharmacist embedded within the clinic did not see patients in the TCM clinic on a daily basis. TCM appointments at Hillcrest’s clinic are scheduled for 20 minutes with the PCP, with the main focus of the appointment being the admission diagnosis. The PCP will also examine other pertinent medical problems during this appointment. A medical assistant or nurse performs the in-person medication reconciliation when the patient arrives to the clinic, and typically, does not document MRPs at this step. The motivation for this study arose from the lack of MRPs being identified and documented during the face-to-face TCM visits in the clinic.
The retrospective, control group consisted of patients who went through the standard TCM protocol. The prospective, treatment group included patients who underwent the same standard TCM protocol but had an additional 20-minute medication reconciliation appointment with a pharmacist, immediately prior to the PCP appointment. The pharmacist visit was conducted by a postgraduate year 1 pharmacy resident, who discussed all interventions with the clinical pharmacist embedded in the clinic. The additional medication reconciliation appointment allowed time for the pharmacist to delve deeper into the evaluation and analysis of all the patients’ medications, provide in-depth counseling, and resolve any discrepancies or problems with the PCP before their appointment. Prior to the scheduled face-to-face medication reconciliation visit, the pharmacist reviewed all aspects of the medication regimen plan. This included, but was not limited to, appropriate drug and dose selection, timing, drug interactions, and appropriateness of the medication therapy plan for each medical problem. At the time of the scheduled face-to-face visit, the pharmacists assessed adherence to the medication regimen and provided counseling to all patients on an individualized basis. Noted MRPs were reviewed with the PCP, who would implement the recommendation where appropriate. Recommendations were either deemed accepted or not. The pharmacist documented the appointment details, discussions with the PCP, and medication plan in the patient’s EMR.
Inclusion criteria for both the control and treatment groups consisted of patients, with any medical condition, discharged from any CCF hospital, and seen at Hillcrest’s Family Medicine/Internal medicine clinic. Patients with caregivers or those whose primary language was not English were included, as a translator was available. Exclusion criteria, in the treatment group only, consisted of patients not seen by the PCP and pharmacist on the same day.
The primary outcome was the comparison of the proportion of patients with at least one MRP found when a pharmacist performed a medication reconciliation in a team-based approach, versus a medication reconciliation performed by a non-pharmacist health care professional. The medication reconciliation involved comparing and verifying each drug listed in the EMR was the same as those the patient was taking. In the control group, MRPs were identified if documented in the patients’ EMR. This outcome was chosen to measure the efficacy of the work of the pharmacist in the TCM clinic. MRPs were described by a modified version of the validated Pharmaceutical Care Network Europe (PCNE) tool V 8.02. 8 This tool was chosen as it has been used in previous studies of this setting. We chose to further classify each type of patient-related MRP as aware or unaware, in the prospective group only, as the original tool does not allow for the understanding of the cause of the MRP. As an example, if a patient did not administer a medication correctly and was unaware of this issue, we classified this as patient-related cause, inappropriate administration, and patient unaware.
Secondary outcomes included the number and specific type of MRPs found, classified by the modified PCNE tool, and 30-day readmission rate. Baseline characteristics were collected for the control and treatment groups including age, gender, race, the number of medications at discharge, and the factors that are included in the internal readmission risk prioritization tool mentioned above.
We conducted a sample size calculation, setting our α level at 0.05, power at 80%, and a difference in the proportion of MRPs at 30% between the treatment and control groups. Previous literature that analyzes the difference in the proportions of MRPs in the TCM setting is limited; therefore, we chose 30% after consensus with the authors that this would represent a clinically significant difference. These parameters set a sample size of 49 patients in each group. Continuous variables were analyzed with an unpaired t test, and categorical variables were analyzed with a χ2 test.
Results
There were 50 patients included in the prospective and retrospective groups. Baseline demographics differed between the 2 groups in several categories (Table 1). The mean age of the patients in the prospective group was 68 years, whereas the mean age in the retrospective group was 65.5 years. Women and Caucasians comprised >50% of the prospective and retrospective groups. When comparing the presence of certain comorbidities, the prospective group included more patients with kidney issues (chronic kidney disease or acute kidney injury), COPD, and CHF. Reasons for admissions varied widely; however, the most common cause in both groups was chest pain, with 12% in the prospective group and 22% in the retrospective group (Table 1). Regarding the primary outcome, 36 (72%) patients in the prospective group had at least 1 MRP, versus 9 (18%) patients in the retrospective group, P < .001. Overall, we found 56 MRPs in the prospective group and 11 in the retrospective group (Table 2).
Table 1.
Baseline Demographics and Reason for Admission.
| Baseline Demographics | Prospective (n = 50) | Retrospective (n = 50) | P |
|---|---|---|---|
| Age (years, mean ± SD) | 67.9 ± 18.03 | 65.5 ± 16.46 | .489 |
| Gender | |||
| Female (n, %) | 29 (58) | 27 (54) | .689 |
| Race (n, %) | |||
| Caucasian | 29 (58) | 27 (54) | .689 |
| African American | 20 (40) | 22 (44) | .687 |
| Length of stay (days, mean ± SD) | 3.87 ± 4.85 | 4.16 ± 5.79 | .787 |
| Number of medications at discharge (includes maintenance and as needed; n, %) | |||
| ≤5 medications | 3 (6) | 5 (10) | .463 |
| 6-10 medications | 15 (30) | 13 (26) | .658 |
| >10 medications | 32 (64) | 32 (64) | 1 |
| Active anticoagulation order (n, %) | 18 (36) | 14 (28) | .637 |
| Number of total comorbidities (n, mean ± SD) | 8.02 ± 3.91 | 8.28 ± 3.5 | .727 |
| Presence of certain comorbidities (n, %) | |||
| Kidney (CKD or AKI) | 18 (36) | 10 (20) | .08 |
| COPD | 6 (12) | 4 (8) | .507 |
| DM | 16 (32) | 20 (40) | .407 |
| CHF | 7 (14) | 4 (8) | .340 |
| Previous admissions within 6 months (n, %) | 29 (58) | 28 (56) | .841 |
| Previous admissions within 12 months (n, %) | 22 (44) | 24 (48) | .69 |
| Reason for admission (n, %) | |||
| Cardiac | 15 (30) | 15 (30) | 1 |
| Chest pain | 6 (12) | 11 (22) | .185 |
| Infectious disease | 6 (12) | 14 (28) | .047 |
| Gastrointestinal | 2 (4) | 7 (14) | .082 |
| Psychology | 5 (10) | 0 (0) | .023 |
| Respiratory | 9 (18) | 2 (4) | .026 |
Abbreviations: CKD, chronic kidney disease; AKI, acute kidney injury; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; CHF, chronic heart failure.
Table 2.
Results.
| Results | Prospective (n = 50) | Retrospective (n = 50) |
|---|---|---|
| Primary outcome results (n, %) a | 36 (72%) | 9 (18%) |
| Secondary outcome results | ||
| Number of MRPs found (n) | 56 | 11 |
| 30-day readmission after TCM appointments (n) b | 9 | 11 |
| Number of medications after TCM appointments (n, %) | ||
| ≤5 medications | 4 (8%) | 9 (18%) |
| 6-10 medications | 18 (36%) | 12 (24%) |
| >10 medications | 28 (56%) | 29 (58%) |
Abbreviations: MRP, medication-related problem; TCM, transitional care management.
P < .001.
P = .065.
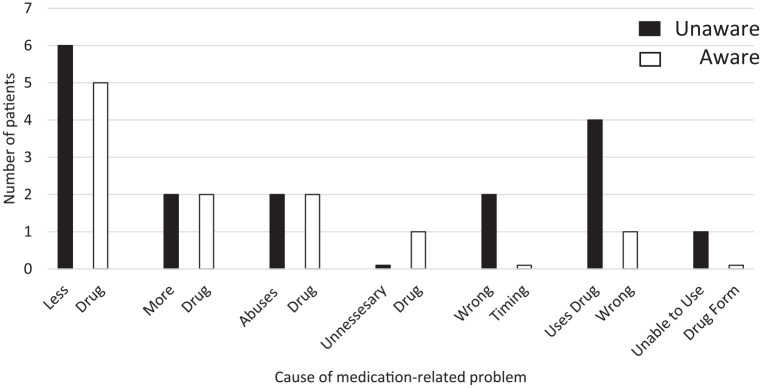
MRPs were identified in 6 of the 8 primary domains, as classified by a modified PCNE tool (Table 3). The most common primary domain was patient-related cause with 28 MRPs in the prospective group and 7 in the retrospective group. Using or taking less drug than prescribed or none at all was prevalent in 11 patients in the prospective group, and 5 in the retrospective group. Six of these 11 patients were unaware of this MRP, whereas 5 were aware that they were incorrectly using a prescribed medication (Figure 1). Another common MRP within the patient-related domain was patient administers/uses drug in a wrong way, and was generally related to inappropriate inhaler technique. Prior to their TCM appointment, 4 of these patients were not on appropriate statin therapy. After the TCM appointments, 3 patients were prescribed an appropriate statin regimen. Additionally, 6 patients had no or inappropriate outcome monitoring that was discussed with the PCP and subsequently resolved.
Table 3.
Medication-Related Problems (MRP).
| Primary Domain and MRP Cause | Prospective (n = 50) | Retrospective (n = 50) |
|---|---|---|
| 1. Drug selection (n) | 9 | 1 |
| 1.1. Inappropriate drug according to guidelines/formulary | 2 | 1 |
| 1.3. No indication for drug | 1 | 0 |
| 1.5. Inappropriate duplication of therapeutic group/active ingredient | 1 | 0 |
| 1.6. No drug treatment in spite of existing indication | 5 | 0 |
| 3. Dose selection (n) | 6 | 0 |
| 3.1. Drug dose too low | 1 | 0 |
| 3.2. Drug dose too high | 2 | 0 |
| 3.4. Dosage regimen too frequent | 3 | 0 |
| 4. Treatment duration (n) | 1 | 0 |
| 4.2. Duration of treatment too long | 1 | 0 |
| 5. Dispensing (n) | 1 | 0 |
| 5.2. Necessary information not provided | 1 | 0 |
| 7. Patient related (n) | 28 | 7 |
| 7.1. Patient uses/takes less drug than prescribed or does not take drug at all | 11 | 5 |
| 7.2. Patient uses/takes more drug than prescribed | 4 | 0 |
| 7.3. Patient abuses drug (unregulated overuse) | 4 | 1 |
| 7.4. Patient uses unnecessary drug | 1 | 0 |
| 7.7. Inappropriate timing or dosing intervals | 2 | 0 |
| 7.8. Patient administers/uses the drug in a wrong way | 5 | 1 |
| 7.9. Patient unable to use drug/form as directed | 1 | 0 |
| 8. Other (n) | 11 | 3 |
| 8.1. No or inappropriate outcome monitoring (including therapeutic drug monitoring) | 6 | 0 |
| 8.2. Other cause | 5 | 3 |
Figure 1.
Patient-related and medication-related problems classified as unaware or aware.
There was no significant difference in 30-day readmission after TCM appointment; 9 patients in the prospective group versus 11 in the retrospective group (P = .065; Table 3).
The number of medications at discharge and after TCM appointments differed between the prospective and retrospective groups. Over 50% of patients in both groups had over 10 medications at discharge. The prospective group had an 8% decrease in the number of patients with more than 10 medications, whereas the retrospective group had a 6% decrease (Table 2). Last, 47 (76%) recommendations were implemented from a total of 62.
Discussion
This study showed that when a pharmacist performed a medication reconciliation as part of a team-based TCM appointment, the pharmacist uncovered more MRPs. The patient-related domain made up the majority of MRPs found, and the most common cause within the patient-related domain was a patient using or taking less drug than prescribed, or not taking the drug at all. Several of these MRPs were results of a patient’s lack of education about the medication. As an example, one patient discontinued her proton pump inhibitor without understanding that her recent gastrointestinal bleed was the reason she was started on it. After providing the necessary information about the medication and discussing the case with the PCP, the patient restarted the medication. Furthermore, this study demonstrated that pharmacists discovered MRPs which could have otherwise gone unnoticed, but that were resolved on the same day of the postdischarge appointment. Changes to the number of medications postdischarge in the prospective group can be attributed to the pharmacist discontinuing unnecessary medications from the patient’s regimen, resulting in safer, optimized drug utilization.
These findings support similar data published in other studies that examine causes of MRPs. The PATCH trial 6 found 13 patients who did not take a prescribed medication, and 3 patients who deliberately underused or underadministered a medication. Although the PATCH trial did not assess a patient’s awareness of the MRP, these results suggest that patients are generally using less drug than prescribed. Our trial supports a similar finding.
Patients in our study were split fairly evenly with regard to being aware or unaware of several MRPs. This pattern was seen when patients used less drug than prescribed, more drug than prescribed, and when there was unregulated overuse of a drug. Regardless of the patient-specific reason for the MRP and the patient’s awareness of the MRP, the pharmacist provided education about the prescribed medication to ensure that any lack of knowledge about the prescribed medication was addressed. The investigators of Revisiting Project Re-Engineered Discharge (RED) divided MRPs into groupings similar to aware and unaware. Overall, there were 23 unaware errors and only 5 errors the patients were aware of, which differs greatly from the results in our study. This difference could be due to the fact that Project RED was a telephone-based pharmacist intervention design versus in-person intervention. When speaking with a patient over the phone, nonverbal cues are lost, which can make it difficult to truly understand a patient’s understanding of a medication. Without knowing the specific medications involved, it is difficult to discern the precise reason for this variance.
The number of recommendations accepted in our study of 76% is lower than other published acceptance rates. 6 Several recommendations were given for future laboratory tests and appointments and therefore not acted upon on the day of the appointment, which potentially lowered our acceptance rate. Data regarding the follow-up of these future recommendations were not collected.
Variations in the data between the prospective and retrospective groups can be explained by several factors. The differences in the reasons for admission between the prospective and retrospective groups could be a result of the time of year in which the data were collected. The proportion of Caucasian females seen in this study are a reflection of the surrounding area’s demographics.
There are several limitations that should be mentioned to properly understand the results of our study. First, there was an inherent bias toward the primary outcome. The pharmacist who reviewed the patient’s medical record prior to the TCM appointment identified MRPs prior to meeting with the patient. However, as pharmacists, it is our duty to seek out potential or actual MRPs and address them. Therefore, it is not surprising that more MRPs were found with the involvement of a pharmacist. Due to time constraints placed on the timeframe for this study, a prospective comparison of the identification of MRPs by a non-pharmacist in the control group could not be performed. Additionally, previous literature 9 has demonstrated that structured patient interviews identify additional MRPs. Employing these methods would have helped limit the amount of bias seen in our study. Furthermore, the MRPs in the retrospective group were identified through a retrospective EMR review. MRPs could only be identified if noted in the EMR during the TCM appointment. This could have potentially limited the number of MRPs found in the retrospective group.
Second, due to the wide variation in reasons for admission between the prospective and retrospective group, limited comparisons can be drawn from these data.
Third, a modified version of the PCNE tool was used, which classified 9% of the prospective MRPs as “other cause,” suggesting that the PCNE tool may not be the most exhaustive MRP tool available. Basger and colleagues 10 performed a literature review on MRP classification systems and concluded that there was no consensus on the preference or structure of the classification system. Future studies are needed to evaluate the best MRP classification system available.
Last, our readmission rates were low, which could be attributed to the fact that only CCF hospital or ED admissions could be captured. In the greater Cleveland area, there are only 2 health systems with major hospitals; consequently, patients tend to receive care in only one of the health systems. Nevertheless, if a patient was readmitted to a hospital outside of the CCF, the data were not able to be seen.
Conclusion
This study supports the role of pharmacists within the transitions of care setting and validates the need for pharmacist review of patient’s medications postdischarge. Medication reconciliations performed postdischarge led to the discovery and resolution of patient-related MRPs, as well as safer and more appropriate use of medications. Follow-up studies that examine patient-specific factors that cause MRPs could allow for proactive identification and resolution prior to discharge.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Bianca Mayzel  https://orcid.org/0000-0002-4685-7451
https://orcid.org/0000-0002-4685-7451
References
- 1. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161-167. doi: 10.7326/0003-4819-138-3-200302040-00007 [DOI] [PubMed] [Google Scholar]
- 2. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418-1428. doi: 10.1056/NEJMsa0803563 [DOI] [PubMed] [Google Scholar]
- 3. Centers for Medicare and Medicaid Services. Readmissions Reduction Program (HRRP). https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed August 7, 2018.
- 4. Jacobs M, Sherry PS, Taylor LM, Amato M, Tataronis GR, Cushing G. Pharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) study. J Am Pharm Assoc (2003). 2012;52:613-621. doi: 10.1331/JAPhA.2012.10183 [DOI] [PubMed] [Google Scholar]
- 5. Perlroth D, Marrufo G, Montesinos A. Medication therapy management in chronically ill populations: final report. http://innovation.cms.gov/Files/reports/MTM_Final_Report.pdf. Published August 2013. Accessed August 7, 2018.
- 6. Trang J, Martinez A, Aslam S, Duong MT. Pharmacist Advancement of Transitions of Care to Home (PATCH) Service. Hosp Pharm. 2015;50:994-1002. doi: 10.1310/hpj5011-994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sanchez GM, Douglass MA, Mancuso MA. Revisiting project Re-Engineered Discharge (RED): the impact of a pharmacist telephone intervention on hospital readmission rates. Pharmacotherapy. 2015;35:805-812. doi: 10.1002/phar.1630 [DOI] [PubMed] [Google Scholar]
- 8. Pharmaceutical Care Network Europe. PCNE classification for drug-related problems V 8.02. https://www.pcne.org/working-groups/2/drug-related-problem-classification. Accessed October 25, 2018.
- 9. Stämpfli D, Boeni F, Gerber A, Bättig VAD, Hersberger KE, Lampert ML. Contribution of patient interviews as part of a comprehensive approach to the identification of drug-related problems on geriatric wards. Drugs Aging. 2018;35:665-675. doi: 10.1007/s40266-018-0557-z [DOI] [PubMed] [Google Scholar]
- 10. Basger BJ, Moles RJ, Chen TF. Application of drug-related problem (DRP) classification systems: a review of the literature. Eur J Clin Pharmacol. 2014;70:799-815. doi: 10.1007/s00228-014-1686-x [DOI] [PubMed] [Google Scholar]