Abstract
Background and Objectives:
In Canada, competency-based medical education prepares family medicine (FM) graduates to provide a broad scope of practice (SoP). We compared the practice intentions of FM residents at the end of training with actual practice patterns of early career family physicians (FPs) for SoP activities reflective of comprehensive family medicine.
Methods:
We collected self-reported data from cross-sectional family medicine longitudinal surveys for exiting FM residents in 2015 and 2016 and from a separate cohort of FPs who were 3 years into practice in 2018 and 2019 from 15 programs. We measured outcomes from exiting FM residents intending to participate in SoP activities and FPs participating in 15 SoP domains of family medicine.
Results:
A total of 1,409 exiting FM residents (58.2% response rate) and 523 early career FPs (21% response rate) responded to the surveys. A high correlation existed between the percentage of exiting residents who intended to participate in each SoP activity and the percentage of FPs who participated in those activities (r 2=0.95). However, we found statistically significant declines in the percentage of FPs reporting involvement in the SoP activities compared to their reported practice intentions for 14 of the 15 domains. We saw the greatest declines in providing care in long-term care facilities, rural communities, emergency departments, intrapartum care, and care for Indigenous populations (P<.001).
Conclusions:
While SoP patterns are highly correlated with practice intentions, early-career FPs are less likely to provide care as intended for all SoP activities. Further research is needed on the factors influencing practice patterns in specific areas to determine how FP graduates can be supported to provide comprehensive care.
Keywords: family medicine, intentions, practice patterns, scope of practice
INTRODUCTION
In Canada, Triple C is a competency-based curriculum that prepares family medicine (FM) graduates to provide comprehensive care to patients. 1 The curriculum is designed to provide C omprehensive education and patient care focused on C ontinuity of education and patient care that is C entered in family medicine. 2 Graduates of FM residency programs can pursue further training by completing certificates of added competence in eight fields: addiction medicine, care of the elderly, enhanced surgical skills, emergency medicine, family practice anesthesia, obstetrical surgical skills, palliative care, and sport and exercise medicine. 3 Refer to Supplementary Material #1 for more information on Canada’s medical education system.
The College of Family Physicians of Canada (CFPC) defines comprehensive care as a type of care family physicians (FPs) provide (either on their own or with a team) to a defined population of patients across multiple domains. 4 Comprehensive care includes, but is not limited to, the following scope of practice (SoP) activities: care across the life cycle, intrapartum care, mental health care, chronic disease management, palliative care, office-based clinical procedures, in-hospital clinical procedures, emergency department (ED) care, home care, and care in long-term care (LTC) facilities. 4
Despite the aims of the Triple C curriculum, the practice of comprehensive care is declining in Canada. 5, 6, 7 For example, studies from Ontario and British Columbia have suggested that service volume, 8, 9, 10 working full-time, 11 and patient panel sizes 11 are decreasing. Furthermore, fewer physicians provide services at nonoffice-based locations (eg, hospitals, LTC facilities). 5, 12 The narrowing of SoP may contribute to system-wide workforce shortages, which have serious consequences for access to primary care for Canadians.
In the United States, one study showed that FM graduates’ intended SoP at the end of residency differed from the actual practice patterns of FPs. 13 The trends of high intention and declines in actual practice raise questions about whether similar declines are taking place in other jurisdictions worldwide. To date, no study has compared the intention of FM residents with their actual practice within the various SoP activities in Canada. Note that all residency programs in Canada are university affiliated, which is different from the United States. Assessing these trends is important because data can identify areas where FPs are not working despite having high intentions to practice in those areas. This evidence then can inform potential changes to the FM training program and facilitate the implementation of strategies to support future FPs in providing a broader SoP and improving access to care. Thus, this study aimed to compare the intention of FM residents at exit from the FM residency training program with their actual practice patterns at 3 years into practice for the various family medicine SoP activities.
METHODS
Study Design, Population, and Data Collection
We conducted a cross-sectional survey-based study of graduating and certified early career FPs. We collected and analyzed data for the project using the Family Medicine Longitudinal Survey (FMLS)—a pan-Canadian cross-sectional survey created by the CFPC to evaluate the Triple C curriculum. The FMLS is approved by the Human Research Ethics Board at each of the 17 Canadian faculties of medicine with family medicine departments. The University of Toronto Ethics Board reviewed this project, which was deemed exempt from the requirement for ethics approval because it is a quality improvement study.
The FMLS T1 survey captures FM residents’ practice intentions for a range of SoP activities, practice settings, and populations. The FMLS T2 survey incorporates similar questions as the T1 survey but focuses on exiting FM residents. The FMLS T3 survey examines practice patterns of FPs at 3 years into practice. See Supplementary Material #2 for all four surveys used in our study. The FMLS T1 was not used in this study because it focuses on FM residents who have just completed medical school and are entering into residency. Responses to statements about intention are evaluated using a 5-point Likert scale (“highly likely” to “very unlikely”). Actual practice patterns are assessed by asking respondents to select the domains that apply to their practice. The 15 domains of care included in this study are shown in Figure 1 and Table 1. The domains that best reflected the scope of FM residency training (a cross-section of different settings, spectrum, populations, and life cycles of patients) were included in the survey. 14*
Table 1. Aggregate Values for the Frequency, Corresponding Significance Level, and Magnitude of Effect for Intention (T2) and Practice (T3) of Cohorts 2015 and 2016*.
|
Domains/settings/populations |
T2, n (%) |
T3, n (%) |
χ2 |
P value |
Effect size, phi |
|
Care across the life cycle |
1,248 (96.1%) |
458 (88.4%) |
38.888 |
<.001 |
0.146335 |
|
Intrapartum care |
544 (43.9%) |
161 (31.1%) |
25.009 |
<.001 |
0.119307 |
|
Mental health care |
1,188 (94.5%) |
467 (90.0%) |
11.873 |
<.001 |
0.081763 |
|
Chronic disease management |
1,273 (97.4%) |
467 (90.2%) |
43.841 |
<.001 |
0.154992 |
|
Palliative/end-of-life care |
902 (79.9%) |
336 (64.9%) |
42.966 |
<.001 |
0.161516 |
|
Office-based clinical procedures |
1,164 (94.4%) |
410 (79.2%) |
93.396 |
<.001 |
0.230952 |
|
In-hospital clinical procedures |
569 (46.8%) |
194 (37.5%) |
12.863 |
<.001 |
0.08613 |
|
Practice setting: emergency departments |
620 (49.9%) |
175 (33.8%) |
38.250 |
<.001 |
0.147378 |
|
Practice setting: in hospital |
815 (72.5%) |
300 (57.8%) |
35.206 |
<.001 |
0.146383 |
|
Practice setting: care in the home |
581 (52.8%) |
221 (42.6%) |
14.781 |
<.001 |
0.095549 |
|
Practice setting: long-term care facilities |
544 (48.2%) |
145 (28.0%) |
59.496 |
<.001 |
0.190063 |
|
Marginalized, disadvantaged, and vulnerable populations |
724 (68.5%) |
333 (64.2%) |
2.960 |
.085 |
0.043339 |
|
Rural communities |
766 (67.7%) |
221 (42.7%) |
92.436 |
<.001 |
0.236689 |
|
Elderly populations |
1229 (95.1%) |
441 (85.0%) |
52.092 |
<.001 |
0.169553 |
|
Indigenous populations |
569 (55.1%) |
208 (40.2%) |
30.962 |
<.001 |
0.141336 |
*Results include responses of “highly likely” and “somewhat likely” (T2), and “Yes” (T3).
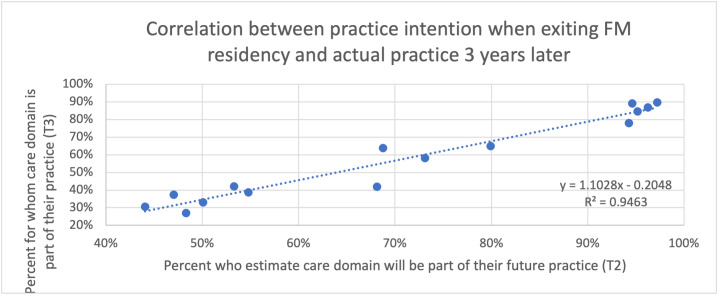
Figure 1 . Degree of Intention and Actual Practice of FPs by Domain Setting and Populations.
In 2015 and 2016, 15 of 17 programs were prepared to participate in the survey. To enable comparisons between the two cohorts, the same schools were included in the analysis for both years. FM residents who completed a residency in 2015 and 2016 (T2) and FPs who were 3 years into practice in 2018 and 2019 (T3) from 15 of the 17 residency programs in Canada were invited to participate. These two groups do not include the same responding individuals; thus, this is not a longitudinal cohort study. One program used incorrect language for the in-hospital clinical care question in a T2 survey, and the results from that question were excluded from analysis. The results are reported for the 15 programs that participated in all four surveys.
The FMLS T2 survey was administered to exiting FM residents by the 15 programs in person or by email. Data were collected between March and May of the graduating year. The FMLS T3 survey was administered to FPs by the CFPC via email. Participation in that survey was voluntary. Data were collected in the fall, 3 years into practice. The survey was available to participants until January of the following year. Participants could revise answers to initial responses. Consent was considered implied if participants chose to complete the survey. We retained data from partially completed surveys for analysis. We generated unique identifiers to prevent duplication of results.
Analysis
We analyzed data cross-sectionally at two points in time: at the exit from FM training and at 3 years into practice. To ensure accuracy of the results, the first and second authors reviewed the qualitative comments in the T3 surveys. Participants who indicated that they did not provide care in a particular domain were asked to provide a reason for why they did not choose to practice that domain. Options included, the domain is not an area of interest; obstacles outside of my control preventing me; I do not feel competent to provide care in this domain; I do not feel confident to provide care in this domain; I would include this domain in my practice if I had more training; I would include this domain in my practice if I had a mentor or someone to provide advice when needed; other. In cases where participants indicated that they had made an error or provided care in that domain, responses were recoded as providing care in the domain.
We calculated descriptive statistics for all survey questions. We dichotomized responses for the intention questions in T2 data to permit comparisons between T2 and T3 data. We combined “somewhat likely” and “highly likely,” as well as “somewhat unlikely” and “very unlikely.” We excluded survey responses with missing values. We used sensitivity analysis to confirm the elimination of the “neutral” response, which resulted in similar patterns as including it in the “somewhat likely” or “highly likely” category or randomly assigning it to either category. We applied the χ2 test of independence to determine whether practice intentions of exiting FM residents were independent of 3-year practice activities, settings, and populations. We set the level of significance at .05; we applied a Bonferroni correction to reduce the risk of type I error. We used the phi coefficient (ɸ) to examine the magnitude of observed changes. We weighted data by the residency program to account for differences in response rates. For descriptive purposes, we used Pearson correlation to examine the association between exiting FM residents’ practice intentions and the practice patterns of FPs 3 years into practice.
RESULTS
In the combined 2015 and 2016 cohorts, 1,409 of 2,420 exiting FM residents responded (58.2%) to the T2 surveys. In the combined 2018 and 2019 cohorts, 523 of 2,495 FPs responded (21%) to the corresponding T3 surveys. The demographic characteristics of T2 and T3 respondents are outlined in Table 2. See Supplementary Material #3 for age and jurisdictional distribution for T3 respondents. No modifications were made to the Triple C curriculum during the duration of the study.
Table 2. Demographic Characteristics of Participants in FMLS T2 and T3.
|
Demographic characteristics |
T2 (2015, 2016) N=1,417 |
T3 (2018, 2019) N=563 |
|
Age in years (mean) |
30.6 |
33.4 |
|
Sex (female) |
898 (64.9%) |
369 (66.5%) |
|
Married/common law |
825 (60.0%) |
443 (80%) |
|
Have/expecting children |
336 (24.3%) |
297 (53.9) |
|
Grew up in inner city/urban/suburban environment |
860 (60.8%) |
345 (61.5%) |
|
Grew up in small town/rural environment |
434 (30.7%) |
190 (33.8%) |
Abbreviations: FMLS, Family Medicine Longitudinal Survey
The proportions of graduating FM residents who reported intention to practice within the 15 care domains and actual practice among FPs 3 years later are shown in Table 1, along with P, phi, and χ2values. Approximately 80% or more of exiting residents reported that they were somewhat likely or highly likely to provide chronic disease management, care across the life cycle, mental health care, elderly, office-based clinical procedures, and palliative care. Fifty percent were somewhat likely or highly likely to provide care in the hospital; to marginalized, rural, and Indigenous communities; home care; and ED care. Less than 50% were somewhat likely or highly likely to provide LTC facility care, in-hospital clinical procedures, and intrapartum care.
In actual practice, 80% or more of early-career FPs reported providing chronic disease management, care across the life cycle, mental health care, and elderly care. More than 50% of FPs reported providing palliative care, care in the hospital, office-based clinical procedures, and care to a marginalized population. Less than 50% of FPs reported providing care to rural and Indigenous populations, in-home, ED, LTC, in-hospital clinical procedures, and intrapartum care.
The differences between intention versus practice rates are statistically significant for 14 of the 15 domains of care (Figure 1). On average, we noted an overall decline of 20.9% between intended and actual practice rates (Figure 2). The largest percentage of declines were for practice in LTC facilities, rural communities, and emergency departments. Care for marginalized populations was the only domain for which the difference in intention versus practice rates was not statistically significant.
Figure 2 . Degree of Intention and Actual Practice of FPs by Domain Setting and Populations.
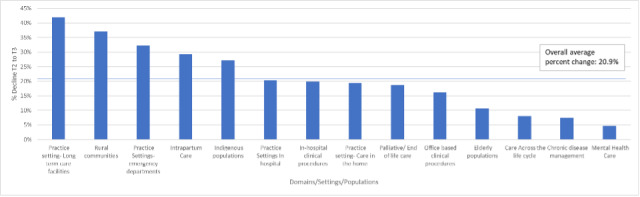
Despite the across-the-board declines, we found a high degree of correlation (r 2=0.95; Figure 3) between intended practice and actual practice. The areas with the highest practice intentions (ie, chronic disease management, care across the life cycle, elderly populations, mental health care, and office-based clinical procedures) were the most common areas of practice for early career FPs. In contrast, the areas with lower practice intentions (ie, intrapartum care, practice in LTC facilities, in-hospital clinical procedures, and work in the ED) were the least common areas of practice.
Figure 3 . Correlation Between Practice Intention When Exiting FM Residency and Actual Practice 3 Years Later.
DISCUSSION
Our study shows a high degree of correlation between exiting FM residents’ future practice intentions at the end of training and the observed SoP of early career FPs 3 years later. The top five intended domains of practice for exiting residents are the most common areas of practice for early career FPs: chronic disease management, care across the life cycle, elderly populations, mental health care, and office-based clinical procedures. Similarly, the areas that exiting residents are least likely to see as part of their future practice are, generally, the least likely to be part of early career FP’s practice: intrapartum care, practice in LTC facilities, in-hospital clinical procedures, and work in the ED. These findings suggest that the expressed practice intentions of exiting FM residents provide a relatively accurate picture of what future FPs will do in practice. This, then, is potentially compelling information for planning future health care services and informing strategies for the FM curriculum and opportunities for improvement. The most significant declines between intention and actual practice were in providing intrapartum care; care in LTC facilities, EDs, and rural communities; and care for Indigenous populations.
The intention of exiting FM residents to provide a broader SoP compared to actual practice aligns with trends in the United States, 13 in which substantial differences have been found between intention and actual practice in prenatal care, inpatient care, nursing home care, home visits, and women’s health procedures. 13 The results on the actual practice patterns of FPs align with Canadian studies that show declines in the delivery of comprehensive care. 5, 6, 7These patterns suggest that FPs are not providing the full breadth of services they are trained to provide as part of the Triple C curriculum. This reality exacerbates the existing problem of access to primary care in Canada. 15 In addition, this finding has implications for physician resource planning because current approaches to estimating FP supply mainly focus on the numbers of FPs and do not account for the SoP of those FPs. Thus, future health and human resource modeling needs to be based on data that include the SoP activities of FPs.
This study cannot explain the observed declines between intention and practice in intrapartum care, care in LTC and ED, and in-hospital clinical procedures. However, the underlying causes are likely due to various multifaceted factors. 16, 17 For example, health system factors, such as hospital privileging, 18 can impede practice related to ED, hospital inpatient, and intrapartum care. 18, 19 Current health policies and the insufficient spread of interprofessional teams could be barriers to FPs providing a broad scope of services. 20 Educational factors, such as insufficient experiential learning, may influence practice patterns. Early career FPs have reported not feeling competent or confident to provide care in intrapartum, hospital, and emergency care. 19, 21 Time constraints and transportation logistics can influence an FP’s ability to routinely work in multiple settings, such as rural and inner-city communities, hospitals, LTC facilities, and patients’ homes. 19, 21 Practice location also may influence the populations that can be served in practice (ie, Indigenous populations). Due to on-call services, lifestyle, 18 family obligations, and parenthood can influence decisions about intrapartum, hospital, and ED care. 19 Other reasons for the differences between intention and actual practice could be high aspirational goals or fear of reporting the lack of intent to deliver comprehensive care activities at the end of FM training. 13
To support FM graduates with intentions to provide a broader SoP, further research is needed to examine the factors influencing intention and actual patterns for intrapartum care, in-hospital clinical procedures, care in LTC facilities, and EDs. A better understanding of these factors can help to identify the barriers that need to be addressed to permit FM graduates with intentions to provide comprehensive care to provide a broader SoP to Canadians and to enable the effective use of health and human resources in Canada.
Limitations
This study had some limitations. It focused on the 2-year core FM residency program and did not examine exiting residents in extended training programs offering certificates of added competence. The results were based on aggregate-level data of T2 and T3 responses, without matched data. In addition, both cohorts had lower response rates for the FMLS T3. The differences in the response rates reflect the timing and approach to survey distribution because exiting residents responding to the T2 survey received their survey from program leadership while still in residency whereas the T3 survey was distributed by the CFPC at a time when graduates were in practice. Health policy factors that may have impacted the availability of physician time to complete the survey may have included the lack of access to team-based care or remuneration models. Our data, however, also showed consistency in the results for both cohorts.
A small number of FM programs did not participate in all four surveys. In addition, due to the use of incorrect language in the exit survey, the results from one program were excluded from two questions in the survey at the end of residency for both cohorts. Comparing participants and nonparticipants by practice type was not possible for this study. The sample may not represent the physician practice because participants were largely female and had variable representation across jurisdictions. Furthermore, this paper reports only on domains of practice, not the percentage of specific domains in a practice. Finally, the findings presented are based on self-report and are subject to social desirability bias. Although self-reported data have their limitations, there is no other way of capturing the intrapsychic concepts about a topic, such as intentions, other than through subjective reporting.
CONCLUSION
The intention to provide a broader SoP is greater than the actual practice of early-career FPs in Canada.This finding has implications for health and human resources planning. Further research is needed on factors that explain the differences between intention and practice patterns. This research should help guide the development of FM training to better prepare FPs for practice and the implementation of health system interventions to enable a broader SoP. Together, these interventions could improve access to equitable and comprehensive primary care services for all Canadians.
Footnote
*While FMLS questionnaires are designed to capture the breadth of family practice, survey methodologies are limited with respect to the amount of detailed information they can gather. For example, questionnaires ask about chronic disease management but do not gather details about specific chronic diseases. Similarly, questionnaires ask about mental health care but do not ask about specific therapeutic techniques, such as cognitive behavioral therapy and psychotherapy.
Financial Support
Funding for the study was from the College of Family Physicians of Canada.
Conflict Disclosure
Steve Slade (Director of Research) is employed by the CFPC. Alixandra Holtby was the Evaluation and Research Analytics Project Lead for the CFPC at the time of the study. Monica Aggarwal, PhD, was partially compensated for her time on this project through the CFPC and the University of Toronto.
Acknowledgments
The authors acknowledge the 17 university-based family medicine residency programs that participated in evaluating the Triple C Competency-Based Curriculum through the Family Medicine Longitudinal Survey. We want to thank Dragan Kljujic and Lorelei Nardi from the CFPC Education Evaluation and Research Unit (EERU) for their contribution. We want to acknowledge the College of Family Physicians of Canada for sponsoring the study.
References
- 1. Standards of accreditation for residency programs in family medicine. The College of Family Physicians of Canada. 2020. https://www.cfpc.ca/CFPC/media/Resources/Accreditation/2020701-RB-V2-0-ENG.pdf https://www.cfpc.ca/CFPC/media/Resources/Accreditation/2020701-RB-V2-0-ENG.pdf
- 2.Triple C competency-based curriculum. The College of Family Physicians of Canada. 2023. https://www.cfpc.ca/en/education-professional-development/educational-frameworks-and-reference-guides/triple-c-competency-based-curriculum https://www.cfpc.ca/en/education-professional-development/educational-frameworks-and-reference-guides/triple-c-competency-based-curriculum
- 3.Certificates of added competence in family medicine. The College of Family Physicians of Canada. 2023. https://www.cfpc.ca/en/education-professional-development/examinations-and-certification/certificates-of-added-competence-in-family-medicin https://www.cfpc.ca/en/education-professional-development/examinations-and-certification/certificates-of-added-competence-in-family-medicin
- 4. Capturing learner trends from the Triple C competency-based curriculum 2015 to 2021: results of the T2 (exit) Family Medicine Longitudinal Survey, aggregate findings across family medicine residency programs. The College of Family Physicians of Canada. 2022. https://www.cfpc.ca/CFPC/media/Resources/Research/Capturing-Learner-Trends-Results-of-the-T2.pdf https://www.cfpc.ca/CFPC/media/Resources/Research/Capturing-Learner-Trends-Results-of-the-T2.pdf
- 5.Chan B T. The declining comprehensiveness of primary care. CMAJ. 2002;166(4):429–434. [PMC free article] [PubMed] [Google Scholar]
- 6.Freeman T R, Boisvert L, Wong E, Wetmore S, Maddocks H. Comprehensive practice: normative definition across 3 generations of alumni from a single family practice program. Can Fam Physician. 1985;64(10):750–759. [PMC free article] [PubMed] [Google Scholar]
- 7.Lavergne M R, Peterson S, Mckendry R, Sivananthan S, Mcgrail K. Full-service family practice in British Columbia: policy interventions and trends in practice. Healthc Policy. 1991;9(4):32–47. [PMC free article] [PubMed] [Google Scholar]
- 8.Hedden L, Barer M L, Cardiff K, Mcgrail K M, Law M R, Bourgeault I L. The implications of the feminization of the primary care physician workforce on service supply: a systematic review. Hum Resour Health. 2014;12(1):32–32. doi: 10.1186/1478-4491-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hedden L, Barer M L, Mcgrail K, Law M, Bourgeault I L. In British Columbia, the supply of primary care physicians grew, but their rate of clinical activity declined. Health Aff (Millwood) 2017;36:904–905. doi: 10.1377/hlthaff.2017.0014. [DOI] [PubMed] [Google Scholar]
- 10.Sarma S, Thind A, Chu M-K. Do new cohorts of family physicians work less compared to their older predecessors? The evidence from Canada. Soc Sci Med. 2011;72(12):2049–2058. doi: 10.1016/j.socscimed.2011.03.047. [DOI] [PubMed] [Google Scholar]
- 11.Hedden L, Banihosseini S, Strydom N, Mccracken R. Modern work patterns of “classic” versus millennial family doctors and their effect on workforce planning for community-based primary care: a cross-sectional survey. Hum Resour Health. 2020;18(1):67. doi: 10.1186/s12960-020-00508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hedden L, Lavergne M R, Mcgrail K M. Trends in providing out-of-office, urgent after-hours, and on-call care in British Columbia. Ann Fam Med. 2019;17(2):116–124. doi: 10.1370/afm.2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coutinho A J, Cochrane A, Stelter K, Phillips R L, Peterson L E. Comparison of intended scope of practice for family medicine residents with reported scope of practice among practicing family physicians. JAMA. 2015;314(22):2364–2372. doi: 10.1001/jama.2015.13734. [DOI] [PubMed] [Google Scholar]
- 14.Tannenbaum D, Kerr J, Konkin J. The scope of training for family medicine residency: report of the working group on postgraduate curriculum review. Triple C Competency-based Curriculum Report. 2011:15–18. [Google Scholar]
- 15.Canadian Community Health Survey. Statistics Canada. 2020. https://www150.statcan.gc.ca/n1/daily-quotidien/210908/dq210908b-eng.htm https://www150.statcan.gc.ca/n1/daily-quotidien/210908/dq210908b-eng.htm
- 16.Reitz R, Horst K, Davenport M, Klemmetsen S, Clark M. Factors influencing family physician scope of practice: a grounded theory study. Fam Med. 2018;50(4):269–274. doi: 10.22454/FamMed.2018.602663. [DOI] [PubMed] [Google Scholar]
- 17.Russell A, Fromewick J, Macdonald B. Drivers of scope of practice in family medicine: a conceptual model. Ann Fam Med. 2021;19(3):217–223. doi: 10.1370/afm.2669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barreto T W, Eden A R, Petterson S, Bazemore A W, Peterson L E. Intention versus reality: family medicine residency graduates’ intention to practice obstetrics. J Am Board Fam Med. 2017;30(4):405–406. doi: 10.3122/jabfm.2017.04.170120. [DOI] [PubMed] [Google Scholar]
- 19.Aggarwal M, Holtby A, Oandasan I. Factors that influence practice choices of early-career family physicians: an outcomes of training project evidence summary. College of Family Physicians of Canada. 2022. https://www.cfpc.ca/en/factors-that-influence-practice-choices-of-early-career-family-physicians https://www.cfpc.ca/en/factors-that-influence-practice-choices-of-early-career-family-physicians
- 20.Aggarwal M, Hutchison B, Canadian Foundation for Healthcare Improvement Toward a primary care strategy for Canada . 2012
- 21.Jewell K, Newton C, Dharamsi S. Length of family medicine training and readiness for independent practice: residents’ perspectives at one Canadian university. UBC Med J. 2015;6(2) [Google Scholar]