Abstract
Objective
The long‐term results of cervical disc arthroplasty (CDA) for noncontiguous cervical degenerative disc disease (CDDD) are still uncertain. Moreover, it is unclear whether CDA delays or avoids the degeneration of the intermediate segment (IS), leading to controversy in the field. Therefore, this study aimed to investigate the mid‐ to long‐term clinical and radiographic outcomes of CDA in treating noncontiguous CDDD and to explore whether the IS degenerated faster after CDA than other non‐surgically treated adjacent segments.
Methods
We retrospectively analyzed patients with noncontiguous CDDD who underwent CDA in our department between January 2008 and July 2018. The patients were divided into the CDA and hybrid surgery (HS) groups, and clinical and radiographic outcomes were evaluated at routine postoperative intervals. Clinical outcomes were assessed using the Japanese Orthopaedic Association (JOA), neck disability index (NDI), and visual analogue scale (VAS), while radiographic outcomes included cervical lordosis (CL), C2‐C7 range of motion (ROM), segmental ROM, and disc angle (DA) at the arthroplasty level. Complications were also evaluated.Pre‐ and postoperative values were compared using paired t‐tests or Wilcoxon rank‐sum tests. Independent Student t‐tests or Mann–Whitney U tests analyzed continuous data between CDA and HS groups, while chi‐square or Fisher exact tests assessed categorical data.
Results
Sixty‐four patients with noncontiguous CDDD, with 31 in the CDA group and 33 in the HS group, were evaluated. The mean follow‐up time was over 70 months. The most frequently involved levels were C4/5 and C5/6. Both groups showed significant improvements in JOA, NDI, and VAS values after surgery. Although CL was maintained, the CL in the CDA group was consistently lower than that in the HS group (p < 0.05). There was a significant decrease in C2‐C7 ROM (p < 0.05), but at the last follow‐up, the C2‐C7 ROM in the CDA group was greater than that in the HS group (p < 0.05). At the last follow‐up, 44.3% of arthroplasty levels had developed heterotopic ossification (HO), and 48.45% had developed anterior bone loss (ABL). In addition, adjacent segment degeneration (ASDeg) was observed in the IS (22.7%), superior adjacent segment (20.6%)and inferior adjacent segment (21.9%).
Conclusion
CDA or CDA combined with fusion are viable treatments for noncontiguous CDDD, with satisfactory outcomes after mid‐to‐long‐term follow‐up. ASDeg is similar in non‐surgical segments after 70 months of follow‐up. ROM of the IS issimilar to preoperative levels, indicating CDA does not increase the risk of IS degeneration.
Keywords: Adjacent segment degeneration, Cervical disc arthroplasty, Hybrid surgery, Intermediate segment, Noncontiguous cervical degenerative disc disease, Skip level
Noncontiguous cervical disc degenerative disease (CDDD) is a unique form of multilevel CDDD, characterized by segments with significant degeneration at both ends (C3/4, C5/6, C6/7) and an intermediate segment (C4/5) showing no apparent degeneration. The utilization of cervical disc arthroplasty with or without fusion is a potential effective approach for its treatment.
Introduction
Anterior cervical discectomy and fusion (ACDF) is a well‐established treatment for degenerative cervical pathology, characterized by radiculopathy or myelopathy, occurring at one or multiple levels. 1 However, as the number of fused segments increases, cervical mobility decreases, 2 leading to increased risk of pseudarthrosis formation 3 and the need for secondary surgery. 4 In cases of noncontiguous cervical degenerative disc disease (CDDD), long‐segment fusion surgery results in sacrificing the intermediate segment without disc degeneration. Even when a skipped ACDF is performed, treating only the index segments, the intermediate segment may still be exposed to extra mechanical stress, leading to disc degeneration or an accelerated development of it. Therefore, cervical fusion surgery may not be the optimal treatment strategy for noncontiguous CDDD.
After almost two decades of rapid development, cervical disc arthroplasty (CDA) has become an established alternative to ACDF for treating radiculopathy and myelopathy, with satisfactory long‐term clinical outcomes. 5 Clinical trials have shown noninferiority and potential superiority of CDA over ACDF for treating one‐level and contiguous two‐level CDDD, with 10‐year outcomes demonstrating successful results. 6 , 7 , 8 , 9 , 10 , 11 Due to its motion‐preservation capacity, CDA has been found to have superior patient outcomes for contiguous two‐level CDDD, and a reduced reoperation rate at the adjacent level due to adjacent segment disease (ASDis). 6 , 9 Although patients with noncontiguous CDDD were not considered the optimal candidates for CDA, previous studies have not regarded noncontiguous CDDD as an absolute contraindication for CDA. 12 , 13 Furthermore, some CDA clinical trials have included several patients with noncontiguous CDDD but have not analyzed the results separately.
Since there is a lack of sufficient evidence regarding the long‐term effectiveness of CDA in improving symptoms and function in patients with noncontiguous CDDD, the study aims to achieve the following objectives: (i) evaluating the long‐term clinical and radiographic outcomes in patients with noncontiguous CDDD; and (ii) investigating potential accelerated degeneration of the adjacent IS segment following CDA in comparison to non‐surgically treated segments.
Methods
Study Population
We conducted a retrospective review of patients who suffered from noncontiguous cervical disc degenerative disease (CDDD) at our hospital from January 2008 to July 2018. The study protocol was approved by the institutional ethics committee of West China Hospital of Sichuan University (2019 Review (No. 946)), and all enrolled patients provided informed consent. The inclusion criteria for patients were as follows: (i) between 18 to 65 years of age; (ii) symptomatic radiculopathy and/or myelopathy caused by cervical disc herniation or spondylosis at noncontiguous levels from C2‐T1; and (iii) followed up for at least 48 months. Patients were excluded if they had a history of previous (i) anterior cervical spine surgery; (ii) single or contiguous level DDD; and (iii) cervical deformity, trauma or tumor, or active systemic infection or infection at the operative level.
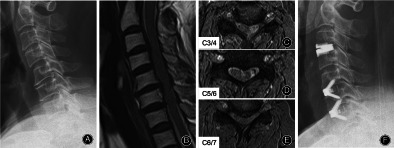
Based on the surgical methods used, patients were divided into two groups: the cervical disc arthroplasty (CDA) group and the hybrid surgery (HS) group, which involved a combination of CDA and anterior cervical discectomy and fusion (ACDF). In the HS group, ACDF was performed at the segment with radiographic signs of instability, bridging osteophytes, and severe facet degeneration (Fig. 1).
Fig. 1.
Special case. A 43‐year‐old patient suffered from weakness and pain in both upper limbs. Preoperative X‐rays (A) showed a significant loss of height at the C5/6, and CT scans (B) revealed osteophyte formation. MRI (C–F) demonstratedat disc protrusion C5/6 and C7/T1, leading to compression the spinal cord. The patient underwent C5/6 ACDF and C7/T1 CDA (G). Follow‐up evaluations at 3 months (H), 12 months (I), and 72 months (J–L) post‐surgery indicated no notable degeneration at the C6/7 level and preservation of mobility in the cervical spine.
Surgical Techniques
All surgical procedures were performed by the same experienced surgeon (HL). The anterior cervical spine surgery was performed as previously described, with a standard right‐sided anterior approach routinely used. 14 , 15 Thorough decompression was achieved by removing the disc material, cartilage, and osteophytes at the involved levels. A properly sized Prestige‐LP artificial disc (Medtronic SofamorDanek, Memphis, TN, USA) or Zero‐P implant (Synthes, Oberdorf, Switzerland) was then inserted into the well‐prepared intervertebral space based on the preoperative surgical plan. The placement of the prostheses was confirmed using C‐arm fluoroscopy. Subsequently, a drainage tube was inserted, and the wound was closed.
Data Collection
In this study, regular evaluations of clinical and radiographic outcomes were conducted at several time points: before surgery, at 3 and 12 months post‐surgery, and during the last follow‐up. X‐rays were performed at every follow‐up to maintain economic feasibility, while CT or MRI scans were performed if necessary. To evaluate clinical outcomes, self‐assessment questionnaires, including the Japanese Orthopaedic Association (JOA), neck disability index (NDI), and visual analogue scale (VAS), were utilized.
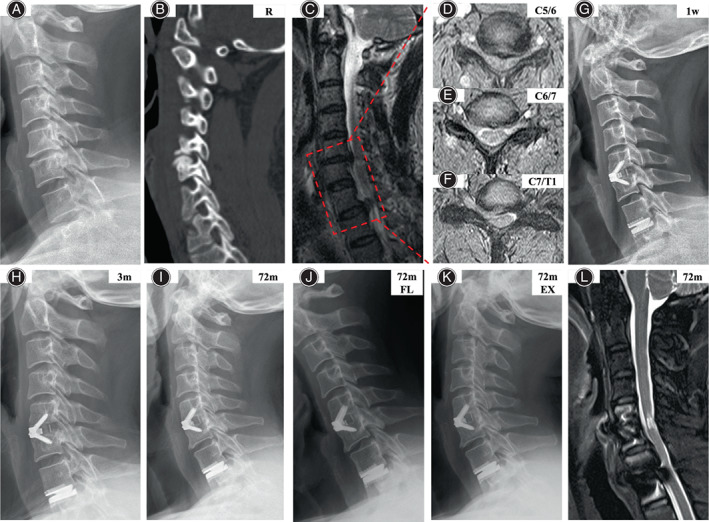
Radiographic parameters, including cervical lordosis (CL), C2‐C7 range of motion (ROM), segmental ROM at the arthroplasty level and non‐operated levels, disc angle (DA) at the operated levels, disc height (DH) at the arthroplasty levels, and fusion status, were measured in lateral neutral and extension‐flexion views. Cobb angles were used to measure C2‐C7 and segmental ROMs, which were defined as the difference between flexion and extension views. DH was measured as the vertical distance from the midpoint at the lower endplate of the cephalad vertebrae to the horizontal line of the anterior–posterior diameter of the upper endplate of the caudal vertebrae (Fig. 2).
Fig. 2.
Illustrations of disc height (DH) measurement before (A) and after surgery (B), and anterior bone loss (ABL) after CDA (C, D). DH was measured as the vertical distance from the midpoint of the lower endplate of the upper vertebrae to the horizontal line of the upper endplate of the lower vertebrae.The ABL was determined as the ratio of the change in anteroposterior (AP) endplate diameter at follow‐up compared to 1‐week postoperatively, relative to the initial 1‐week postoperative diameter. The formula was ABL% = (a − a′)/a × 100%. a, length of AP endplate at 1‐week postoperative; a′, length of APendplate at the follow‐up period.
During the follow‐up, data on complications and adverse events was also collected. Prosthesis subsidence was defined as a height loss of more than 2 mm in the anterior or posterior functional spinal unit (FSU), or a change of more than 5° between the horizontal line across the prosthesis and the posterior vertebral line when compared to the immediate postoperative value. 14 The occurrence of heterotopic ossification (HO) was graded according to the McAfee classification system 16 and was divided into low‐grade HO (0‐II) and high‐grade HO (III‐IV) based on impaired ROM criteria. 17 , 18 Anterior bone loss (ABL) was evaluated using Kieser's methods 14 , 19 (Figure 2). The adjacent segment degeneration (ASDeg) was semi‐quantitatively evaluated based on the overall degeneration of height loss (graded from 0 to 4), anterior osteophytes (graded from 0 to 3), and endplate sclerosis (graded from 0 to 2). Next, the three variables are summed to the overall degree of disc degeneration (ranging from 0 to 9;Table S1). 20
Statistical Analysis
The statistical analysis was conducted using SPSS v22.0 software (IBM SPSS Inc., Armonk, NY, USA). The results were reported as mean ± standard deviation (SD) and/or percentages as appropriate. The preoperative and postoperative values were compared using either the paired t‐test or Wilcoxon rank‐sum test. The independent Student t‐test or Mann–Whitney U test was employed for comparing contiguous data between the CDA and HS groups, as appropriate. For categorical data, a chi‐square test or Fisher exact test was used. The statistical significance was set at p < 0.05.
Results
Patient Demographics
A total of 64 patients were available for assessment after completing an average 70 months of follow‐up (range, 48–121 months). For further analysis, 31 patients were placed in the CDA group, with a mean age of 46.16 ± 6.48 years (range, 31–59 years) and a gender ratio of 16 males to 15 females. The remaining 33 patients were placed in the HS group, with a mean age of 48.97 ± 6.7 years (range, 33–65 years) and a gender ratio of 18 males to 15 females. The intermediate segment (IS) was predominantly distributed in the C4/5 (69%), followed by C5/6 (28%), and then C3/4 and C6/7 (3%). Fifty‐three cases skipped one segment and 11 cases skipped two segments. Detailed patient demographic information can be found in Table 1.
TABLE 1.
Demographic data of patients (mean ± SD).
| Variable | CDA | HS | Statistic | p value |
|---|---|---|---|---|
| No of patient | 31 | 33 | ‐ | ‐ |
| Age, yr | 46.16 ± 6.47 | 48.97 ± 6.70 | t = −1.703 | 0.094 a |
| Gender (M/F) | 16/15 | 18/15 | χ2 = 0.055 | 0.814 b |
| BMI, kg/m2 | 23.59 ± 3.11 | 24.05 ± 2.17 | t = −0.685 | 0.496 a |
| Diagnose | χ2 = 1.501 | 0.472 b | ||
| Radiculopathy | 15 | 16 | ||
| Myelopathy | 6 | 10 | ||
| Radiculomyelopathy | 10 | 7 | ||
| Level distribution | ‐ | 1.000 c | ||
| C3/4 | 1 | 0 | ||
| C4/5 | 26 | 26 | ||
| C5/6 | 10 | 11 | ||
| C6/7 | 0 | 1 | ||
| Follow‐up, mo | 71.35 ± 19.50 | 70.61 ± 18.85 | t = 0.156 | 0.881 a |
Independent t test.
chi‐square test.
Fisher exact test.
Clinical Outcomes
For all patients, there was a significant improvement in JOA, NDI, and VAS scores compared to preoperative values (p < 0.05). However, no significant difference was observed between the CDA and HS groups at any of the follow‐up time points (p > 0.05, see Table 2 for details).
TABLE 2.
Clinical outcomes between the two groups (mean ± SD).
| CDA group | HS group | Statistic | p value | |
|---|---|---|---|---|
| JOA | ||||
| Pre‐op | 8.77 ± 1.68 | 8.55 ± 1.46 | t = 0.581 | 0.563 |
| Post‐op | 16.10 ± 0.91 a | 16.09 ± 0.72 a | t = 0.029 | 0.977 |
| NDI | ||||
| Pre‐op | 29.74 ± 5.66 | 28.57 ± 5.89 | t = 0.807 | 0.423 |
| Post‐op | 7.87 ± 3.20 a | 9.00 ± 5.11 a | t = −1.052 | 0.297 |
| VAS | ||||
| Pre‐op | 5.81 ± 1.49 | 5.58 ± 1.66 | t = 0.584 | 0.562 |
| Post‐op | 1.23 ± 1.02 a | 1.36 ± 1.11 a | t = −0.515 | 0.609 |
Abbreviations: JOA, Japanese Orthopedic Association; NDI, neck disability index; Post‐op, postoperatively; Pre‐op, preoperatively; VAS, visual analogue scale.
p < 0.05 compared with preoperative values, independent t test.
Radiographic Outcomes
Cervical Lordosis and C2‐C7 ROM
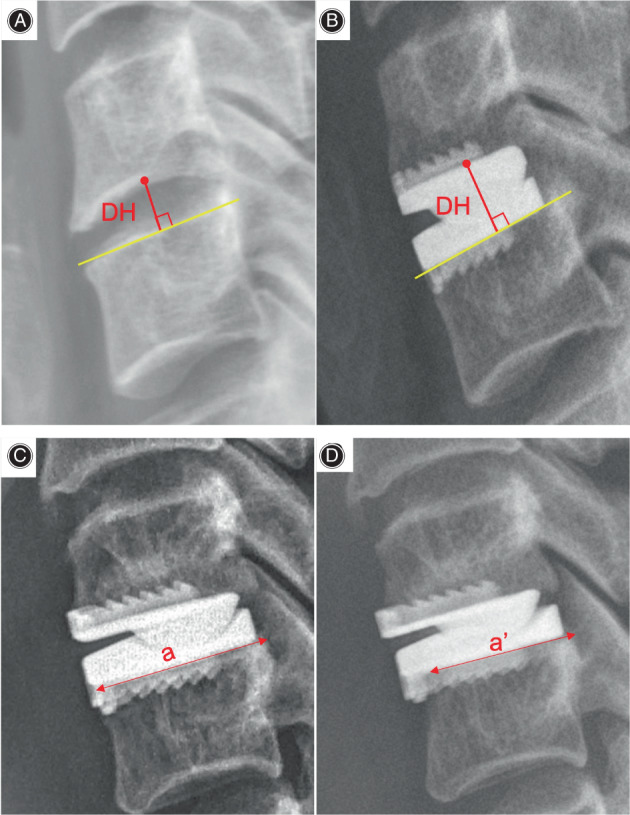
In the study population as a whole, the cervical lordosis (CL) increased significantly from 9.04° ± 7.78° before surgery to 11.57° ± 6.62° at the last follow‐up (p = 0.003, Figure 3). However, in the CDA group, the increase in CL was not statistically significant (p = 0.348). In contrast, the HS group had a preoperative CL of 9.53° ± 8.26°, which significantly increased to 13.69° ± 6.86° (p = 0.004). Despite similar preoperative CL values between the two groups, the CDA group had a significantly lower CL value than the HS group during the follow‐up (p < 0.05).
Fig. 3.
Cervical lordosis and C2‐C7 ROM were well preserved after CDA. *Compared the CDA group with the HS group, p < 0.05.
Considered as a whole population, the C2‐C7 range of motion (ROM) decreased significantly from 47.94° ± 12.01° at admission to 41.89° ± 9.08° at the last follow‐up (p < 0.001). In the CDA group, there was a trend towards a modest decrease in the C2‐C7 ROM, but it was not statistically significant (p = 0.115). In contrast, in the HS group, the C2‐C7 ROM at the last follow‐up decreased dramatically and significantly when compared to the baseline (p < 0.001).
Radiographic Changes at the Arthroplasty Levels
Considered as a whole, there was a small decrease in disc angle (DA) from 2.01° ± 2.00° preoperatively to 1.95° ± 2.37° at the last follow‐up (p = 0.852, Figure 4). Regardless of the arthroplasty levels in the CDA or HS group, a similar DA was observed before and after surgery, and no significant difference was observed between the two groups (p > 0.05). In contrast, at the fusion levels in the HS group, the DA significantly improved after surgery and was well maintained through the follow‐up period (p = 0.016).
Fig. 4.
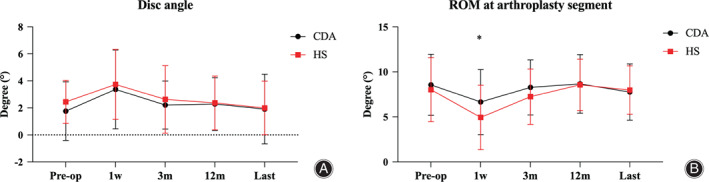
Disc angle and ROM at the arthroplasty segment were well preserved during the follow‐up period, and no significant differences were found between the CDA and HS group. *Compared the CDA group with the HS group, p < 0.05.
Similar to the change in the whole cervical spine, the segmental ROM at the arthroplasty levels decreased from 8.36° ± 3.44° preoperatively to 7.79° ± 2.95°, but no statistical significance was found (p = 0.143). Regardless of the location of the arthroplasty levels, the segmental ROM at the last follow‐up slightly decreased when compared to preoperative values (p > 0.05). Similarly, the corresponding segmental ROM in the HS group also slightly decreased (p = 0.970). Furthermore, at only 1 week after surgery, the ROM at the arthroplasty levels in the CDA group was significantly larger than that in the HS group (p = 0.027).
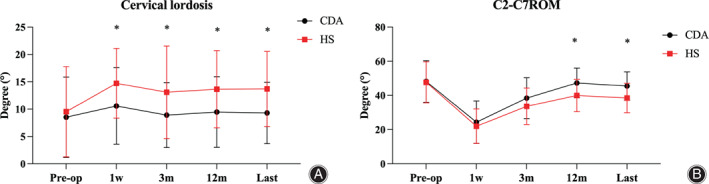
ROM at the Non‐operated Levels
Intermediate Segment
Overall, the ROM at the index segment (IS) increased from 9.58° ± 3.00° preoperatively to 10.19° ± 3.15° at the last follow‐up (p = 0.042, Figure 5). In the CDA group, the ROM at the IS increased to 10.93° ± 3.52° at the 3‐month follow‐up (p = 0.044), and then gradually returned to a level similar to the preoperative value, at 9.96° ± 3.13° (p = 0.987). In contrast, the ROM at the IS in the HS group gradually increased to 10.42° ± 3.18° at the last follow‐up (p = 0.007). Although the ROM at the IS in the CDA group was smaller than that in the HS group at 12 months after the operation and at the last follow‐up, the difference was not statistically significant (p > 0.05).
Fig. 5.
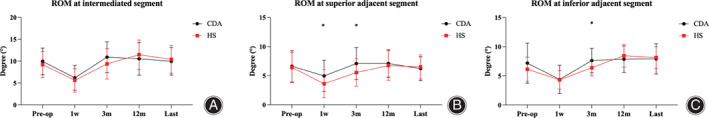
ROM of non‐surgical segments remained stable or slightly increased after CDA. Intermediate segment (A), superior adjacent segment (B), inferior adjacent segment (C). *Compared the CDA group with the HS group, p < 0.05.
Superior Adjacent Segment
Overall, the ROM at the superior adjacent segment slightly decreased from 6.56° ± 2.65° before surgery to 6.36° ± 2.03° at the last follow‐up, but this change was not statistically significant (p = 0.557). This trend was consistent regardless of whether patients were in the CDA group or HS group, as the ROM at the superior adjacent segment at the last follow‐up was not significantly different from the preoperative value (p > 0.05). However, when comparing between the two groups, significant differences in the ROM of the superior adjacent segment were only found at 1 week and 3 months follow‐up (p < 0.05).
Inferior Adjacent Segment
The overall result showed a significant increase in ROM at the inferior adjacent segment from 6.65° ± 2.86° preoperatively to 8.02° ± 2.23° at the last follow‐up (p < 0.001). However, in the CDA group, although there was a decrease in ROM at the inferior adjacent segment, there was no significant difference between the preoperative and postoperative values (p = 0.05). In contrast, the corresponding segmental ROM in the HS group significantly increased from 6.13° ± 2.07° preoperatively to 8.14° ± 1.84° at the last follow‐up (p < 0.001). Significant differences in ROM at the inferior adjacent segment were observed at 3‐month follow‐up between the two groups.
Complications
One case of prosthesis subsidence was reported in the CDA group. The incidence of HO was 44.3%, with 26 segments in the CDA group and 17 replacement segments in the HS group developing HO (Table 3). However, there was no significant difference in the rate of HO between the two groups (p > 0.05). The overall incidence of ABL (Table 4) was 48.45%, with ABL occurring in 50.0% of arthroplasty levels in the CDA group and 45.7% in the HS group, but this difference was not statistically significant (p > 0.05). Among all the operated levels, ASDeg (Table 5) occurred in 22.7% of the IS, 20.6% of the superior adjacent segment, and 21.9% of the inferior adjacent segment. In the CDA group, ASDeg at the IS occurred in 18.9% of cases, which was lower than in the HS group (26.3%), but the difference was not statistically significant. Additionally, irrespective of the group, there was no statistically significant difference in ASDeg among non‐operated levels.
TABLE 3.
Heterotopic ossification developed in the CDA and HS groups.
| CDA group (n = 64) | ||||||
|---|---|---|---|---|---|---|
| Upper arthroplasty segment | Lower arthroplasty segment | total | HS group (n = 35) | Statistic | p value a | |
| HO (%) | 12 (19.3%) | 14 (22.6%) | 26 (41.9%) | 17 (48.6%) | χ2 = 0.399 | 0.528 b |
| High‐grade HO (%) | 4 (6.5%) | 5 (8.0%) | 9 (14.5%) | 4 (11.4%) | 0.765 c | |
Abbreviation: HO, heterotopic ossification.
Compared with all the arthroplasty segment in the CDA group.
chi‐square test.
Fisher exact test.
TABLE 4.
Degree of anterior bone loss in the two groups.
| Degree of ABL | ||||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | Total | |
| CDA | 31 (50.0%) | 13 (21.0%) | 12 (19.4%) | 6 (9.7%) | 0 | 31 |
| HS | 19 (54.3%) | 8 (22.9%) | 6 (17.1%) | 2 (5.7%) | 0 | 16 |
| Total | 50 (51.5%) | 21 (21.6%) | 18 (18.5) | 8 (8.2%) | 0 | 97 |
Abbreviation: ABL, anterior bone loss.
TABLE 5.
Comparison of the adjacent segment degeneration between the CDA and HS groups.
| CDA | HS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 | Statistic | p value | |
| Preoperative | ||||||||||
| Upper adjacent segment | 27 | 3 | 0 | 0 | 29 | 4 | 0 | 0 | 1.000 a | |
| Intermediate segment | 32 | 5 | 0 | 0 | 30 | 8 | 0 | 0 | χ2 = 0.744 | 0.389 b |
| Lower adjacent segment | 28 | 3 | 0 | 0 | 31 | 2 | 0 | 0 | 0.667 a | |
| Last follow‐up | ||||||||||
| Upper adjacent segment | 22 | 8 | 0 | 0 | 23 | 8 | 2 | 0 | χ2 = 0.551 | 0.458 b |
| Intermediate segment | 28 | 6 | 3 | 0 | 25 | 9 | 3 | 1 | χ2 = 0.585 | 0.444 b |
| Lower adjacent segment | 22 | 4 | 4 | 0 | 25 | 6 | 1 | 0 | χ2 = 0.544 | 0.461 b |
Fisher exact test,
chi‐square test.
Discussion
In this present study, our objective is to assess the enduring clinical and radiographic results in patients with noncontiguous CDDD, while also exploring potential escalated degeneration in adjacent segments following CDA. Our findings revealed an ASDeg occurrence rate of 18.9% at the IS after CDA, which was consistent with the incidence of ASDeg in all non‐surgical segments. Notably, although the ASDeg incidence in the IS reached 25.8% after HS, statistical significance between the CDA and HS groups was not observed.
CDA: Potential Surgical Management for Noncontiguous CDDD
The practice of anterior cervical fusion surgery for treating contiguous or noncontiguous CDDD has been established since the 1950s, demonstrating successful decompression and favorable outcomes. Nonetheless, complications such as nonunion, 21 hardwire failure, 22 ASDis 23 and secondary surgery 4 have been associated with long‐segment fusions. If long‐segment fusion is performed for noncontiguous CDDD, at least three levels would need to be sacrificed, making this surgical strategy not recommended. Researchers have discovered that contiguous‐level degeneration is more common than skip lesions in patients with multiple levels of disc degeneration. This suggests that there is a higher probability of subsequent degeneration occurring at adjacent levels. 24 Theoretically, performing ACDF solely at the index levels may cause exaggerated biomechanical changes on the adjacent levels, particularly the IS. In fact, studies have shown that skip‐level ACDF can increase the IS mobility by 35%, 25 which ultimately changes its biomechanical environment and may lead to ASDis in the long‐term postoperative follow‐up, ultimately requiring a reoperation. 26 Previous studies have reported a range of 6.25%–43.75% for the incidence of ASDeg at the IS after skip‐level fusion surgery, but the relatively short follow‐up period may explain the lower incidence. 27 , 28 , 29 Interestingly, about 20% of Klippel–Feil patients have congenital noncontiguous fusion, 30 and these patients have a significantly larger range of motion and higher degeneration rate at the non‐fusion segment when compared to the normal population. 31 Given these factors that promote degeneration of the IS after skip‐level ACDF, some surgeons have started using CDA to treat noncontiguous CDDD.
CDA Presents Biomechanical Advantages
It is pertinent to note a range of findings that contribute to the understanding of the biomechanical implications and long‐term outcomes of CDA for noncontiguous CDDD. Biomechanical studies have confirmed that two‐level CDA did not affect the stability of the cervical spine or the ROM of adjacent segments. 32 , 33 Additionally, our previous finite element analysis (FEA) demonstrated that skip‐level CDA can preserve segmental ROM and maintain the disc pressure and facet joint force of the IS similar to the intact C2‐C7 cervical spine model under hybrid control test protocol. 26 , 34 These biomechanical findings suggest that CDA does not cause hypermobility or additional strain on the IS, and may even retard degeneration in theory. In the present study, we found that the incidence of ASDeg at the IS after CDA was 18.9%, which is higher than the incidence reported for ACDF in the literature. This difference could be attributed to longer follow‐up time and differences in ASDeg evaluation criteria. Furthermore, compared to the 2‐year results (14.3%), the incidence of ASDeg at the IS slightly increased. 35 It is important to note that disc degeneration and aging are closely related, and we cannot determine whether the new radiographic changes were caused by arthroplasty surgery or natural progression of disc degeneration. Unlike prior studies, the current study documented the incidence of ASDeg in all non‐surgical segments, and the results suggest that the degeneration of the IS was not accelerated compared to other non‐surgical segments after CDA.
CDA with ACDF: Suitable Option for Noncontiguous CDDD
We also focus on the findings that shed light on the efficacy and biomechanical implications of hybrid surgery (HS) in the context of noncontiguous CDDD. HS is a combination of CDA and ACDF, which can be performed on the index segment based on the extent of degeneration. For instance, a segment with soft protrusions may be treated with CDA, while a segment with osteophytes and severe degeneration may require ACDF. In recent years, various clinical studies have shown that HS can yield satisfactory outcomes while preserving some level of mobility in the cervical spine for continuous two‐ or multi‐level CDDD. 15 , 36 , 37 Due to the skipped lesion, HS is considered to be a suitable option for noncontiguous CDDD, as there is a lower likelihood of the CDA level and ACDF level affecting each other. Biomechanical studies have confirmed that the increase in ROM at adjacent segments after HS is lower than that observed with 2‐level ACDF, indicating that HS has a less detrimental biomechanical effect on adjacent segments. 38 Additionally, our FEA study revealed that the contributions to motion and force of the non‐surgical levels were evenly distributed, suggesting that the adjacent segments did not experience additional biomechanical stress. 26 Thus, ASDeg was expected to occur with the same likelihood on each non‐surgical segment. However, in our current study, the incidence of ASDeg at the intermediated segment was 25.8% after HS, which was similar to the superior adjacent segment (24.2%) but higher than the inferior adjacent segment (18.2%). This may be attributed to the fact that the inferior adjacent segment included several C7/T1 levels, which have a smaller range of physiological motion and a lower risk of degeneration. 39 , 40 , 41 On the contrary, despite the higher incidence of ASDeg at the IS in patients who underwent HS compared to those who underwent CDA, the lack of statistical significance between the two groups may be due to the small sample size. Furthermore, it is worth noting that the HS group maintained better cervical lordosis, a critical factor in the development of ASDeg, which could also explain the similar incidence of ASDeg between the two groups. Notably, the ROM of the non‐surgical segments increased by 1°‐2° at the last follow‐up compared to preoperative values in the HS group, which may increase the risk of ASDeg during a longer follow‐up.
Main Complication after CDA
HO and ABL were the main complications after CDA, 14 , 42 and were currently considered two stages of bone remodeling following CDA surgery. 43 In the present study, the incidence of HO, high‐grade HO, and ABL at the arthroplasty levels did not differ significantly between the CDA and HS groups at the last follow‐up. Moreover, the incidence of HO and ABL was consistent with previous studies on 1‐level or contiguous 2‐level CDA. Ganbat et al. 44 predicted that the formation of HO may be related to the redistribution of vertebral strain energy after artificial cervical disc prosthesis implantation. Lee et al. 45 conducted a cadaveric study and found no statistically significant difference in segmental ROM of arthroplasty segments between pure CDA and HS. Based on these findings, we suggest that surgical levels after non‐contiguous CDA or HS are relatively independent, and device‐related complications at one surgical level do not affect the other.
Limitation and Strengths
The current study has several limitations that should be acknowledged. First, it was a retrospective study with a small sample size due to the low incidence of noncontiguous CDDD, and the follow‐up time of over 4 years may not have been sufficient to determine whether CDA can delay the degeneration of the IS. Second, the patients included in the study had high heterogeneity, with different IS distribution and number, and patients who underwent 3‐level HS may have had different baseline levels compared to those who underwent 2‐level HS. Third, the study did not include patients who underwent skip‐level ACDF for comparative analysis, as there were not enough such patients in our research center. Fourth, we have extensively used the Zero‐P system during ACDF procedures for cervical spondylosis since 2008 in our department, with very few patients undergoing the plate‐cage system. As a result, we only included patients who underwent Zero‐P ACDF in the current study. Finally, PACS and Canvas software used to measure disc height and endplate diameter on X‐ray films, despite being standardized, may have had measurement inaccuracies that could have been improved.
This study also possesses several strengths. First, this study represents the first long‐term follow‐up report on CDA for noncontiguous multi‐segment CDDD. It provides insights into the extended outcomes of intervening non‐surgical segments and offers valuable guidance for the formulation of surgical strategies. Second, this study simultaneously examines the implementation of personalized CDA surgical strategies within the context of hybrid replacement and fusion procedures. This expanded exploration of surgical approaches for patients with noncontiguous CDDD offers additional choices and clinical evidence for treatment planning. Third, for the first time, this study compares the differences in radiographic changes between the IS and other adjacent non‐surgical segments, observing a similar extent of degeneration among the non‐surgical segments.
Conclusion
CDA or CDA combined with ACDF to treat noncontiguous CDDD can achieve satisfactory mid‐to‐long‐term clinical and radiographic outcomes, and might be considered as safe and effective surgical strategies for noncontiguous CDDD. Among non‐surgical segments, ASDeg incidence was similar after 70 months, and the segmental ROM at the IS was similar to that before surgery, indicating CDA theoretically did not increase the risk of degeneration of the IS. However, HS may slightly increase ROM at the non‐surgical segments, which may increase the risk of ASDeg during longer‐term follow‐up.
Author Contributions
TKW, BYW and HL contributed to the design of the study. TKW drafted the manuscript with the help from JBH. JBH and KKH helped in the statistical analyses. Statistical analyses were discussed with TKW, XR and HL. TKW, CD and BYW contributed to the revision. All authors have read and approved the final manuscript.
Conflict of Interest Statement
All authors declare that they have no conflict of interest.
Ethical Statement
The study protocol was approved by the institutional ethics committee of West China Hospital of Sichuan University (2019 Review (No. 946)), and all enrolled patients provided informed consent.
Supporting information
Table S1. Scoring system for adjacent disc degeneration (20).
Acknowledgments
This study was supported by the Foundation of Science and Technology Department of Sichuan Province (2023NSFSC1741), the Foundation Health Commission of Sichuan Province (21PJ039), the Cadre Health Research Project of Sichuan Province (ZH2023‐105) and 1.3.5 project for Postdoctoral Foundation of West China Hospital of Sichuan University (2023HXBH080).
Ting‐kui Wu and Jun‐bo He are contributed to the work equally and should be regarded as co‐first authors.
Contributor Information
Bei‐yu Wang, Email: dove-baker@163.com.
Hao Liu, Email: dr.liuhao6304@hotmail.com.
References
- 1. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long‐term follow‐up of one hundred and twenty‐two patients. J Bone Joint Surg Am. 1993;75(9):1298–1307. [DOI] [PubMed] [Google Scholar]
- 2. Wu XD, Wang XW, Yuan W, Liu Y, Tsai N, Peng YC, et al. The effect of multilevel anterior cervical fusion on neck motion. Eur Spine J. 2012;21(7):1368–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Epstein NE. A review of complication rates for anterior cervical Diskectomy and fusion (ACDF). Surg Neurol Int. 2019;10:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Laratta JL, Reddy HP, Bratcher KR, McGraw KE, Carreon LY, Owens RK 2nd. Outcomes and revision rates following multilevel anterior cervical discectomy and fusion. J Spine Surg. 2018;4(3):496–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang QL, Tu ZM, Hu P, Kontos F, Li YW, Li L, et al. Long‐term results comparing cervical disc arthroplasty to anterior cervical discectomy and fusion: a systematic review and meta‐analysis of randomized controlled trials. Orthop Surg. 2020;12(1):16–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gornet MF, Lanman TH, Burkus JK, Dryer RF, McConnell JR, Hodges SD, et al. Two‐level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10‐year outcomes of a prospective, randomized investigational device exemption clinical trial. J Neurosurg Spine. 2019;1‐11:508–518. [DOI] [PubMed] [Google Scholar]
- 7. Gornet MF, Burkus JK, Shaffrey ME, Schranck FW, Copay AG. Cervical disc arthroplasty: 10‐year outcomes of the prestige LP cervical disc at a single level. J Neurosurg Spine. 2019;31(3):317–325. [DOI] [PubMed] [Google Scholar]
- 8. Ghobrial GM, Lavelle WF, Florman JE, Riew KD, Levi AD. Symptomatic adjacent level disease requiring surgery: analysis of 10‐year results from a prospective, randomized, clinical trial comparing cervical disc arthroplasty to anterior cervical fusion. Neurosurgery. 2019;84(2):347–354. [DOI] [PubMed] [Google Scholar]
- 9. Kim K, Hoffman G, Bae H, Redmond A, Hisey M, Nunley P, et al. Ten‐year outcomes of 1‐ and 2‐level cervical disc arthroplasty from the Mobi‐C investigational device exemption clinical trial. Neurosurgery. 2021;88(3):497–505. [DOI] [PubMed] [Google Scholar]
- 10. Nunley PD, Hisey M, Smith M, Stone MB. Cervical disc arthroplasty vs anterior cervical discectomy and fusion at 10 years: results from a prospective, randomized clinical trial at 3 sites. Int J Spine Surg. 2023;17(2):230–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fransen P, Noriega D, Chatzisotiriou A, Pointillart V. Cervical disc arthroplasty with the Baguera C prosthesis: clinical and radiological results of a 10‐year follow‐up study. Eur Spine J. 2023. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 12. Leven D, Meaike J, Radcliff K, Qureshi S. Cervical disc replacement surgery: indications, technique, and technical pearls. Curr Rev Musculoskelet Med. 2017;10(2):160–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fehlings MG, Arvin B. Surgical management of cervical degenerative disease: the evidence related to indications, impact, and outcome. J Neurosurg Spine. 2009;11(2):97–100. [DOI] [PubMed] [Google Scholar]
- 14. Wu TK, Liu H, Wang BY, He JB, Ding C, Rong X, et al. Incidence of bone loss after prestige‐LP cervical disc arthroplasty: a single‐center retrospective study of 396 cases. Spine J. 2020;20(8):1219–1228. [DOI] [PubMed] [Google Scholar]
- 15. Wu TK, Meng Y, Wang BY, Hong Y, Rong X, Ding C, et al. Is the behavior of disc replacement adjacent to fusion affected by the location of the fused level in hybrid surgery? Spine J. 2018;18(12):2171–2180. [DOI] [PubMed] [Google Scholar]
- 16. McAfee PC, Cunningham BW, Devine J, Williams E, Yu‐Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech. 2003;16(4):384–389. [DOI] [PubMed] [Google Scholar]
- 17. Yang MMH, Ryu WHA, Casha S, DuPlessis S, Jacobs WB, Hurlbert RJ. Heterotopic ossification and radiographic adjacent‐segment disease after cervical disc arthroplasty. J Neurosurg Spine. 2019;1–10:660–669. [DOI] [PubMed] [Google Scholar]
- 18. Zeng C, Tian W, Liu B, Fan M. The assessment of paravertebral ossification progression after cervical disc arthroplasty based on CT images: a long‐term follow‐up. Orthop Surg. 2020;12(6):1760–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kieser DC, Cawley DT, Fujishiro T, Tavolaro C, Mazas S, Boissiere L, et al. Anterior bone loss in cervical disc arthroplasty. Asian Spine J. 2019;13(1):13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Walraevens J, Liu B, Meersschaert J, Demaerel P, Delye H, Depreitere B, et al. Qualitative and quantitative assessment of degeneration of cervical intervertebral discs and facet joints. Eur Spine J. 2009;18(3):358–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee DH, Park S, Seok SY, Cho JH, Hwang CJ, Kim IH, et al. Fate of pseudarthrosis detected two years after anterior cervical discectomy and fusion: results of a minimum five‐year follow‐up. Spine J. 2023;S1529‐9430(23)03286‐2. [DOI] [PubMed] [Google Scholar]
- 22. Lowery GL, McDonough RF. The significance of hardware failure in anterior cervical plate fixation. Patients with 2‐to 7‐year follow‐up. Spine. 1998;23(2):181–186. discussion 6‐7. [DOI] [PubMed] [Google Scholar]
- 23. Kwok WCH, Wong CYY, Law JHW, Tsang VWT, Tong LWL, Samartzis D, et al. Risk factors for adjacent segment disease following anterior cervical discectomy and fusion with plate fixation: a systematic review and meta‐analysis. J Bone Jt Surg Am. 2022;104(21):1915–1945. [DOI] [PubMed] [Google Scholar]
- 24. Lin Q, Zhou X, Wang X, Cao P, Tsai N, Yuan W. A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy. Eur Spine J. 2012;21(3):474–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Finn MA, Samuelson MM, Bishop F, Bachus KN, Brodke DS. Two‐level noncontiguous versus three‐level anterior cervical discectomy and fusion: a biomechanical comparison. Spine. 2011;36(6):448–453. [DOI] [PubMed] [Google Scholar]
- 26. Wu TK, Meng Y, Liu H, Wang BY, Hong Y, Rong X, et al. Biomechanical effects on the intermediate segment of noncontiguous hybrid surgery with cervical disc arthroplasty and anterior cervical discectomy and fusion: a finite element analysis. Spine J. 2019;19(7):1254–1263. [DOI] [PubMed] [Google Scholar]
- 27. Shi S, Zheng S, Li XF, Yang LL, Liu ZD, Yuan W. Comparison of a stand‐alone anchored spacer versus plate‐cage construct in the treatment of two noncontiguous levels of cervical spondylosis: a preliminary investigation. World Neurosurg. 2016;89:285–292. [DOI] [PubMed] [Google Scholar]
- 28. Wang HR, Li XL, Dong J, Yuan FL, Zhou J. Skip‐level anterior cervical discectomy and fusion with self‐locking stand‐alone PEEK cages for the treatment of 2 noncontiguous levels of cervical spondylosis. J Spinal Disord Tech. 2013;26(7):E286–E292. [DOI] [PubMed] [Google Scholar]
- 29. Bisson EF, Samuelson MM, Apfelbaum RI. Intermediate segment degeneration after noncontiguous anterior cervical fusion. Acta Neurochir. 2011;153(1):123–127. discussion 8. [DOI] [PubMed] [Google Scholar]
- 30. Nouri A, Patel K, Evans H, Saleh M, Kotter MRN, Heary RF, et al. Demographics, presentation and symptoms of patients with Klippel‐Feil syndrome: analysis of a global patient‐reported registry. Eur Spine J. 2019;28(10):2257–2265. [DOI] [PubMed] [Google Scholar]
- 31. Pizzutillo PD, Woods M, Nicholson L, MacEwen GD. Risk factors in Klippel‐Feil syndrome. Spine. 1994;19(18):2110–2116. [DOI] [PubMed] [Google Scholar]
- 32. Phillips FM, Tzermiadianos MN, Voronov LI, Havey RM, Carandang G, Dooris A, et al. Effect of two‐level total disc replacement on cervical spine kinematics. Spine. 2009;34(22):E794–E799. [DOI] [PubMed] [Google Scholar]
- 33. Barrey C, Campana S, Persohn S, Perrin G, Skalli W. Cervical disc prosthesis versus arthrodesis using one‐level, hybrid and two‐level constructs: an in vitro investigation. Eur Spine J. 2012;21(3):432–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wu TK, Meng Y, Wang BY, Rong X, Hong Y, Ding C, et al. Biomechanics following skip‐level cervical disc arthroplasty versus skip‐level cervical discectomy and fusion: a finite element‐based study. BMC Musculoskelet Disord. 2019;20(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wu TK, Wang BY, Deng MD, Hong Y, Rong X, Chen H, et al. A comparison of anterior cervical discectomy and fusion combined with cervical disc arthroplasty and cervical disc arthroplasty for the treatment of skip‐level cervical degenerative disc disease: a retrospective study. Medicine. 2017;96(41):e8112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Xiong Y, Xu L, Yu X, Yang Y, Zhao D, Hu Z, et al. Comparison of 6‐year follow‐up result of hybrid surgery and anterior cervical discectomy and fusion for the treatment of contiguous two‐segment cervical degenerative disc diseases. Spine. 2018;43(20):1418–1425. [DOI] [PubMed] [Google Scholar]
- 37. Scott‐Young M, McEntee L, Rathbone E, Hing W, Nielsen D. Clinical outcomes of cervical hybrid reconstructions: a prospective study. Int J Spine Surg. 2020;14(s2):S57–S66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gandhi AA, Kode S, DeVries NA, Grosland NM, Smucker JD, Fredericks DC. Biomechanical analysis of cervical disc replacement and fusion using single level, two level, and hybrid constructs. Spine. 2015;40(20):1578–1585. [DOI] [PubMed] [Google Scholar]
- 39. Zhou C, Wang H, Wang C, Tsai TY, Yu Y, Ostergaard P, et al. Intervertebral range of motion characteristics of normal cervical spinal segments (C0‐T1) during in vivo neck motions. J Biomech. 2020;98:109418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Anderst WJ, Donaldson WF 3rd, Lee JY, Kang JD. Three‐dimensional intervertebral kinematics in the healthy young adult cervical spine during dynamic functional loading. J Biomech. 2015;48(7):1286–1293. [DOI] [PubMed] [Google Scholar]
- 41. Okada E, Matsumoto M, Ichihara D, Chiba K, Toyama Y, Fujiwara H, et al. Aging of the cervical spine in healthy volunteers: a 10‐year longitudinal magnetic resonance imaging study. Spine. 2009;34(7):706–712. [DOI] [PubMed] [Google Scholar]
- 42. Virk S, Phillips F, Khan S, Qureshi S. A cross‐sectional analysis of 1347 complications for cervical disc replacements from medical device reports maintained by the United States Food and Drug Administration. Spine J. 2020;21:265–272. [DOI] [PubMed] [Google Scholar]
- 43. He J, Liu H, Wu T, Ding C, Huang K, Hong Y, et al. Association between anterior bone loss and anterior heterotopic ossification in hybrid surgery. BMC Musculoskelet Disord. 2020;21(1):664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ganbat D, Kim YH, Kim K, Jin YJ, Park WM. Effect of mechanical loading on heterotopic ossification in cervical total disc replacement: a three‐dimensional finite element analysis. Biomech Model Mechanobiol. 2016;15(5):1191–1199. [DOI] [PubMed] [Google Scholar]
- 45. Lee SB, Cho KS, Kim JY, Yoo DS, Lee TG, Huh PW. Hybrid surgery of multilevel cervical degenerative disc disease: review of literature and clinical results. J Korean Neurosurg Soc. 2012;52(5):452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Scoring system for adjacent disc degeneration (20).


