Abstract
Purpose
Religious beliefs affect end-of-life practices in intensive care units (ICUs). Changes over time in end-of-life practices were not investigated regarding religions.
Methods
Twenty-two European ICUs (3 regions: Northern, Central, and Southern Europe) participated in both Ethicus-1 (years 1999–2000) and Ethicus-2 studies (years 2015–2016). Data of ICU patients who died or had limitations of life-sustaining therapy were analysed regarding changes in end-of-life practices and patient/physician religious affiliations. Frequencies, timing of decision-making, and religious affiliations of physicians/patients were compared using the same definitions.
Results
In total, 4592 adult ICU patients (n = 2807 Ethicus-1, n = 1785 Ethicus-2) were analysed. In both studies, patient and physician religious affiliations were mostly Catholic, Greek Orthodox, Jewish, Protestant, or unknown. Treating physicians (but not patients) commonly reported no religious affiliation (18%). Distribution of end-of-life practices with respect to religion and geographical regions were comparable between the two studies. Withholding [n = 1143 (40.7%) Ethicus-1 and n = 892 (50%) Ethicus-2] and withdrawing [n = 695 (24.8%) Ethicus-1 and n = 692 (38.8%) Ethicus-2] were most commonly decided. No significant changes in end-of-life practices were observed for any religion over 16 years. The number of end-of-life discussions with patients/ families/ physicians increased, while mortality and time until first decision decreased.
Conclusions
Changes in end-of-life practices observed over 16 years appear unrelated to religious affiliations of ICU patients or their treating physicians, but the effects of religiosity and/or culture could not be assessed. Shorter time until decision in the ICU and increased numbers of patient and family discussions may indicate increased awareness of the importance of end-of-life decision-making in the ICU.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00134-023-07228-z.
Keywords: End of life, Intensive care units, Religion, Withholding life-sustaining treatments, Withdrawing life-sustaining treatments, Active shortening of the dying process
Take-home message
| Religious beliefs and practices can influence end-of-life decision-making. However, changes in end-of-life practices observed over 16 years appear unrelated to religious affiliations of patients or their treating physicians. Shorter time until decision in intensive care units and increased numbers of discussions with patients and their families may indicate increased awareness of the importance of end-of-life decision-making in intensive care. |
Introduction
Religion and religious beliefs may affect end-of-life practices and decisions in intensive care units (ICUs) [1]. End-of-life decision-making was shown to change over time [2] and may vary according to geographical regions, contributing to major worldwide differences [3].
Many ICU physicians may not be aware of the potential role played by religious beliefs and regional/cultural values regarding end-of-life decision-making [4]. While improved ICU physician–patient communication may result in better understanding of the role of the patients’ religious beliefs, traditions, and culture, understanding patients’ wishes may lead to improved patient-centred care and respect for patient autonomy providing an improved basis for individual treatment goals in ICUs [5].
In the Ethicus-1 study (1999–2000), we observed significant differences associated with religious affiliations and regional variations regarding types of end-of-life practices (including withholding or withdrawing of life-sustaining therapy, shortening of the dying process, brain death, and cardio-pulmonary resuscitation), times to therapy limitation and death, and discussion of decisions with patient families [6].
There is a clear need for a better understanding of changes in religion and culture over time; however, such research is lacking. Nevertheless, with a more thorough understanding of changes over time in different regions, it would be possible to generate the evidence necessary to better understand and consider different aspects of end-of-life care [7]. The fact that such research may generally be difficult to perform and,e.g. patient religious affiliation often unknown in (e.g. unconscious) critically ill patients, it may also explain why several end-of-life studies worldwide have investigated the role of religion and/ or culture mainly via (self-reported) questionnaires [8, 9].
Few studies have investigated changes in end-of-life practices over time [3], and none have evaluated religion as a potential cause for practice changes. Therefore, using the same definitions as in Ethicus-1, the goal of this study was to investigate whether there was a change in the influence of religious affiliation of physicians and patients on end-of-life practices in 22 European ICUs over the course of 16 years. Since religion was previously shown to impact on whether doctors decide to withdraw or withhold life-sustaining treatments [10], we were particularly interested whether a change over time regarding “active” (i.e. withdrawing, WD and shortening of the dying process, SDP) vs. “passive” (i.e. withholding, WH) limitations has occurred.
Methods
The current study is a preplanned sub-investigation of the Ethicus-2 ICU end-of-life practices worldwide study [2]. Data from European ICUs participating in both Ethicus-1 [10] and Ethicus-2 [2] studies were analysed using the same methods. Patients were enrolled in Ethicus-2 during a self-selected 6-month observational period between September 1, 2015 and September 30, 2016. This study analysed the influence of religious affiliation of physicians and patients on end-of-life practices. Data from ICU patients of centres participating in both the Ethicus-1 and Ethicus-2 studies were analysed. Patients were followed up until ICU discharge, death, or 2 months from the first decision to limit treatment. These were selected from 22 European ICUs which participated in both Ethicus-1 and Ethicus-2 studies. Further details are given elsewhere [2].
Data recorded
Patient characteristics included age, gender, religious affiliations (patients and physicians), ICU admission diagnosis, chronic disorders, end-of-life categories, times of hospital and ICU admission, and discharge/ death. Institutional characteristics included ICU location (along three geographical regions), ICU size, and academic versus non-academic hospitals. Due to a technical problem with the Ethicus-2 website, physician religious affiliation was not available in the subgroups “cardio-pulmonary resuscitation” (CPR) and “brain death” (BD).
Definitions
The same definitions for ICU patient populations, end-of-life categories, geographical regions, religions, ethical and legal considerations, and data collection were used in both the Ethicus-1 and Ethicus-2 studies [2, 10]. End-of-life categories were defined prospectively as CPR, BD, WH or WD of life-sustaining treatment, and active SDP [2]. The 22 ICUs were grouped into three geographical regions: Northern (Denmark, Ireland, The Netherlands, and the United Kingdom, UK), and Central (Belgium, Czech Republic, Germany, and Switzerland) and Southern (Greece, Israel, Italy, Portugal, Spain, and Turkey) Europe.
Ethics
No interventions or treatments were given, withheld, or withdrawn from patients as part of this observational study. Countries, centres, and study data were coded to ensure confidentiality and to allow clinicians to report end-of-life practices of (potential) questionable legality. Ethics Committees approval or waivers were obtained from all participating centres.
Statistical analyses
Data were described by frequencies and percentages, or median and interquartile ranges (IQR), as appropriate. Cohen's kappa coefficients were calculated for the agreement between the physician's and patient's religion. Regression analyses using a generalised estimating equations (GEE) model to describe the populations of patients were developed with robust standard errors and exchangeable working correlation structure accounting for the ICU clinic factor. End-of-life practices were grouped into two categories, either WD (including SDP) or WH life-sustaining treatments (SDP insufficient to stand as a category by itself due to limited case numbers). The dependent variable was hence defined as WD (any limitation) versus WH, while reporting odds for WD. These were estimated from the GEE model for the considered independent variables and corresponding p values testing the null hypothesis assuming odds ratio equal to 1, meaning no observable difference in response to each of the considered variables across the population.
All life-sustaining treatment limitations were included in the models to describe the associations between the treatment limitation event, and factors describing the patient’s ICU region, religious affiliation, and study (Ethicus-1 or Ethicus-2). Several confounders were included in the definition of the models, accounting for the effects of patient age, sex, acute diagnosis, and chronic disorder. Separate models were developed to describe the effects on end-of-life practices from either the religious affiliations of patients or treating physicians. Two additional linear mixed models (LMMs) with ICU site as random factor were implemented to describe the association of a patient’s and (separately) physician’s religious affiliations with the time until the first limitation decision. Further model details are available in the online supplement to this article [11–14].
Results
Our models indicate that large changes in end-of-life practices over 16 years (from Ethicus-1 to Ethicus-2) cannot be observed with respect to any particular religious affiliation. While some of the confidence intervals are too wide to suggest that religion did not play a role in the decision-making of treating physicians, significant changes in end-of-life practice are mostly associated with broader changes within end-of-life practices. The number of end-of-life discussions with patients, families, and physicians increased, while mortality and time until the first end-of-life decision decreased across both physician and patient religious affiliation groups.
Patient demographics and end-of-life decisions
A total of 4592 ICU patients (39% females overall) were included in this study comparing end-of-life practices from 22 European ICUs between Ethicus-1 (E1) and Ethicus-2 (E2). The distribution of 2807 Ethicus-1 and Ethicus-2 patient religious affiliations mostly consisted in Catholic (37.2% E1, 23.5% E2), Greek Orthodox (12.2% E1, 5.7% E2), Jewish (8.7% E1, 4% E2), Protestant (7.1% E1, 11.8% E2), Muslim (3.6% E1, 3.4% E2), none (3.2% E1, 5.2% E2), and unknown (25.7% E1, 44.7% E2) religious affiliations. Withholding (n = 1143 from E1 and n = 892 from E2; 40.7% and 50% of the total end-of-life decisions, respectively) and withdrawing (n = 695 from E1 and n = 692 from E2; 24.8% and 38.8% of the total end-of-life decisions, respectively) were recorded as the most common end-of-life practices. Detailed patient demographics of the E1 and E2 studies are given in combination with end-of-life decision categories in supplementary Table S1, while further demographics details are given elsewhere [2, 10]. Patient religious affiliations per country are provided in supplementary Table S15.
Physician religious affiliations and regional variability
The geographical distribution of included patients across Central, Northern, and Southern Europe remained similar across the two studies (supplementary Table S13). The GEE model odds of withholding life-sustaining treatments among all patients who had limitations of life-sustaining therapy was higher in the Southern European ICUs compared to Central European ICUs (supplementary Tables S2 and S3, p = 0.044 and p = 0.032, respectively).
Physician religious affiliations and end-of-life decisions
Treating physicians’ (that established end-of-life decisions) religious affiliations included from Ethicus-1 and Ethicus-2 were predominantly Catholic (40.7% E1, 37.5% E2), Jewish (15.8% E1, 4.9% E2), Protestant (13.3% E1, 9.9% E2), Greek Orthodox (9.2% E1, 7.1% E2), and without religious affiliation (17.9% E1, 16.2% E2). The distributions of treating physician religious affiliations are comparable between studies, and given for the different end-of-life categories in Table 1. The most notable difference is the fivefold larger percentage of no religious affiliation among physicians when compared to patients. Treating physician’s religious affiliations per country are provided in supplementary Table S16.
Table 1.
Counts and percentages of end-of-life decision categories (SDP, WD and WH) are reported for each of the studies and religious affiliation of treating physicians
| Religious affiliation | SDP | WD | WH | Total | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ethicus-1 | Ethicus-2 | Ethicus-1 | Ethicus-2 | Ethicus-1 | Ethicus-2 | Ethicus-1 | Ethicus-2 | |||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| Catholic | 64 | 8.2 | 10 | 1.7 | 371 | 47.6 | 282 | 47 | 345 | 44.2 | 308 | 51.3 | 780 | 40.7 | 600 | 37.5 |
| Greek Orthodox | 0 | 0 | 0 | 0 | 38 | 21.5 | 21 | 18.4 | 139 | 78.5 | 93 | 81.6 | 177 | 9.2 | 114 | 7.1 |
| Muslim | 0 | 0 | 0 | 0 | 8 | 36.4 | 19 | 26.8 | 14 | 63.6 | 52 | 73.2 | 22 | 1.2 | 71 | 4.4 |
| Jewish | 0 | 0 | 0 | 0 | 54 | 17.8 | 0 | 0 | 249 | 82.2 | 78 | 100 | 303 | 15.8 | 78 | 4.9 |
| None | 14 | 4.1 | 6 | 2.3 | 126 | 36.6 | 116 | 44.8 | 204 | 59.3 | 137 | 52.9 | 344 | 17.9 | 259 | 16.2 |
| Other | 0 | 0 | 1 | 1 | 11 | 35.5 | 47 | 46.5 | 20 | 64.5 | 53 | 52.5 | 31 | 1.6 | 101 | 6.3 |
| Protestant | 2 | 0.8 | 0 | 0 | 83 | 32.6 | 80 | 50.6 | 170 | 66.7 | 78 | 49.4 | 255 | 13.3 | 158 | 9.9 |
| Unknown | 0 | 0 | 0 | 0 | 3 | 60 | 127 | 57.7 | 2 | 40 | 93 | 42.3 | 5 | 0.3 | 220 | 13.7 |
| Missing | 0 | 0 | 0 | 0 | 1 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0.1 | 0 | 0 |
| Total | 80 | 4.2 | 17 | 1.1 | 695 | 36.2 | 692 | 43.2 | 1143 | 59.59 | 892 | 55.72 | 1918 | 100 | 1601 | 100 |
Percentages are computed separately for the Ethicus-1 and Ethicus-2 studies and show the distribution of end-of-life decision categories within religions. The “Total” row shows the overall distribution of end-of-life decision categories in each of the studies, and the “Total” columns show the distribution of treating physician’s religion in each of the studies. SDP shortening of dying process, WD withdrawing, WH withholding
Catholic, Protestant, or physicians without religious affiliations commonly performed withholding or withdrawing, whereas withholding, but not withdrawing, was performed by Jewish physicians in the Ethicus-2 study. Overall, withholding and withdrawing life-sustaining treatments were the most common decisions taken. Shortening of the dying process was rare (2.9% of limitations in Ethicus-1 and 1% in Ethicus-2) and decreasing, and mostly performed by Catholic physicians or physicians without religious affiliation (supplementary Figure S1).
The observed agreement between physician and patient religious affiliations in Ethicus-2 (total Cohen’s kappa 0.32, supplementary Table S12) was fair to moderate for withdrawing (Cohen’s kappa 0.27) and withholding (Cohen’s kappa 0.34) of the final end-of-life practice, similarly to Ethicus-1, while patient numbers in shortening of the dying process are considered too low to be meaningfully interpreted.
Information availability
Information of patient wishes asked and/or received at any time and information on discussions with family by end-of-life category is reported for the Ethicus-1 and Ethicus-2 studies (Tables 2, 3). Over 16 years, the overall availability of information of decisions discussed with family members increased (n = 1268/2807, 45.2% vs. n = 1147/1785, 64.3%). Although unknown/missing information is widely present across the Ethicus-1 data, discussions between treating physicians and patient families increased across all religious affiliations but Greek Orthodox. Descriptive statistics are presented in supplementary Figure S2. Overall consideration of patient’s wishes also increased from Ethicus-1 to Ethicus-2, by about 27% (n = 570/2807, 20.3% vs. n = 840/1785, 47.1%), most notably across the most common end-of-life decisions (WH and WD), as presented in supplementary Figure S3.
Table 2.
Counts (number and per column percentages within answer category: no/yes/missing) of Ethicus-1 and Ethicus-2 discussed wishes with patients with respect to final end-of-life decision categories (BD, CPR, SDP, WD and WH) and physician religious affiliations
| EOL | Ethicus-1 | Ethicus-2 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | Missing | Total | No | Yes | Missing | Total | |||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| BD | 95 | 5.7 | 18 | 3.2 | 148 | 26.2 | 261 | 9.3 | 41 | 5.1 | 18 | 2.1 | 15 | 10.6 | 74 | 4.2 |
| CPR | 242 | 14.5 | 18 | 3.2 | 368 | 65.3 | 628 | 22.4 | 74 | 9.2 | 12 | 1.4 | 24 | 17 | 110 | 6.2 |
| SDP | 44 | 2.6 | 34 | 6 | 2 | 0.4 | 80 | 2.9 | 12 | 1.5 | 5 | 0.6 | 0 | 0 | 17 | 1 |
| WD | 474 | 28.3 | 195 | 34.2 | 26 | 4.6 | 695 | 24.8 | 304 | 37.8 | 350 | 41.7 | 38 | 27 | 692 | 38.8 |
| WH | 818 | 48.9 | 305 | 53.5 | 20 | 3.6 | 1143 | 40.7 | 373 | 46.4 | 455 | 54.2 | 64 | 45.4 | 892 | 50 |
| Total | 1673 | 59.6 | 570 | 20.3 | 564 | 20.1 | 2807 | 100 | 804 | 45 | 840 | 47.1 | 141 | 7.9 | 1785 | 100 |
Frequencies of brain death and cardio-pulmonary resuscitation events are additionally reported. Cases of missing discussions include patient’s unresponsiveness and limited understanding or feasibility. “Yes” and “No” indicate the number of end-of-life decisions where a discussion occurred or did not occur, respectively. “Total” row shows the overall distribution of answer categories within each study. “Total” column shows the distribution of end-of-life decision categories. BD brain death, CPR cardiopulmonary resuscitation, EOL end-of-life, SDP active shortening of dying process, WD withdrawing, WH withholding
Table 3.
Counts (number and per column percentages within answer category: no/yes/missing) of Ethicus-1 and Ethicus-2 discussions with the patient’s family regarding end-of-life decision categories with respect to physician religious affiliations
| Physician religious affiliation | Ethicus-1 | Ethicus-2 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | Missing | Total | No | Yes | Missing | Total | |||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| Catholic | 247 | 37 | 535 | 42.2 | 284 | 32.6 | 1066 | 38 | 157 | 34.5 | 443 | 38.6 | 0 | 0 | 600 | 33.6 |
| Greek Orthodox | 122 | 18.3 | 55 | 4.3 | 171 | 19.6 | 348 | 12.4 | 92 | 20.2 | 22 | 1.9 | 0 | 0 | 114 | 6.4 |
| Muslim | 18 | 2.7 | 4 | 0.3 | 13 | 1.5 | 35 | 1.3 | 31 | 6.8 | 40 | 3.5 | 0 | 0 | 71 | 4 |
| Jewish | 115 | 17.2 | 189 | 14.9 | 81 | 9.3 | 385 | 13.7 | 10 | 2.2 | 68 | 5.9 | 0 | 0 | 78 | 4.4 |
| None | 101 | 15.1 | 256 | 20.2 | 248 | 28.5 | 605 | 21.6 | 55 | 12.1 | 204 | 17.8 | 0 | 0 | 259 | 14.5 |
| Other | 11 | 1.7 | 20 | 1.6 | 18 | 2.1 | 49 | 1.8 | 23 | 5.1 | 78 | 6.8 | 0 | 0 | 101 | 5.7 |
| Protestant | 53 | 7.9 | 204 | 16.1 | 38 | 4.4 | 295 | 10.5 | 21 | 4.6 | 137 | 11.9 | 0 | 0 | 158 | 8.9 |
| Unknown | 1 | 0.2 | 4 | 0.3 | 5 | 0.6 | 10 | 0.4 | 65 | 14.3 | 155 | 13.5 | 0 | 0 | 220 | 12.3 |
| Missing | 0 | 0 | 1 | 0.1 | 13 | 1.5 | 14 | 0.5 | 1 | 0.2 | 0 | 0 | 183 | 100 | 184 | 10.3 |
| Total | 668 | 23.8 | 1268 | 45.2 | 871 | 31 | 2807 | 100 | 455 | 25.5 | 1147 | 64.3 | 183 | 10.3 | 1785 | 100 |
“Yes” and “No” indicate the number of end-of-life decisions where a discussion occurred or did not occur, respectively. “Total” row shows the overall distribution of answer categories within each study. “Total” column shows the distribution of end-of-life decision categories
Patient outcomes and multivariable analyses
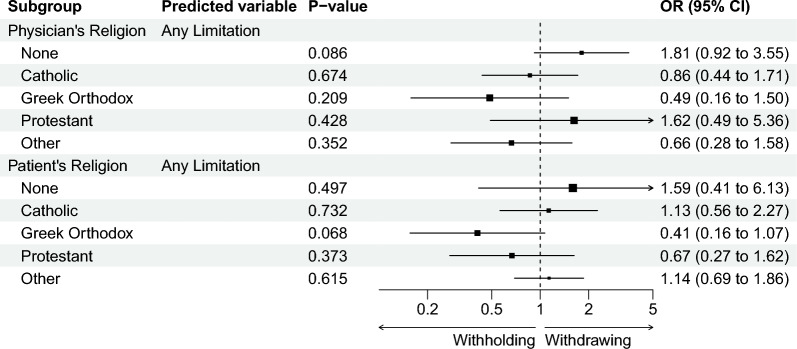
Multivariable analyses of time until limitation and time until mortality were performed using LMM and GEE to determine whether differences in end-of-life practices emerged in response to the different religious affiliations of patient and treating physicians. Time until death was estimated in patients that died as no survival analysis technique was applied. Differences in end-of-life practices within religious affiliations were further tested to assess changes over the course of 16 years (Fig. 1, supplementary Tables S5–S7).. A summary visualisation of the GEE model built to compare WH and WD changes in odds ratio between Ethicus-1 and Ethicus-2 is provided in Fig. 1, while the full model results are provided in supplementary Tables S2–S5. Percentages of WD, WH, and SDP per physician religious affiliation are indicated in supplementary Figure S1, and discussed further below.
Fig. 1.
Forest plot from the general estimating equation (GEE) model estimates showing the changes in odds ratios (OR) from Ethicus-1 to Ethicus-2 in the odds of life-sustaining treatment withdrawal (including shortening of the dying process) with respect to different physician and patient religious affiliations. P values indicate the statistical significance of change for each religion factor when compared to the model’s intercept. Confidence intervals (CI) at 95% from the estimate indicate lower and upper limits of the changes. The size of squares positioned at fold-change estimates are proportional to the size of the corresponding standard errors. Changes in odds ratios for physician and patient religious affiliations are estimated from separate models. The fold-change estimates are based on the models in Tables S2, S4. Estimates for changes in odds ratios for Jewish religious affiliation are not provided as no withdrawing was recorded in Ethicus-2
Changes in the odds of withholding versus withdrawing life-sustaining treatment over the time period under investigation from Ethicus-1 to Ethicus-2 were not found to be statistically significant (all p > 0.05) with respect to any patient or physician religious affiliation (Fig. 1, supplementary Tables S3, S5). Additional models specifically accounting for the interactions between study and religion factors (supplementary Tables S2, S4) further confirmed these observations.
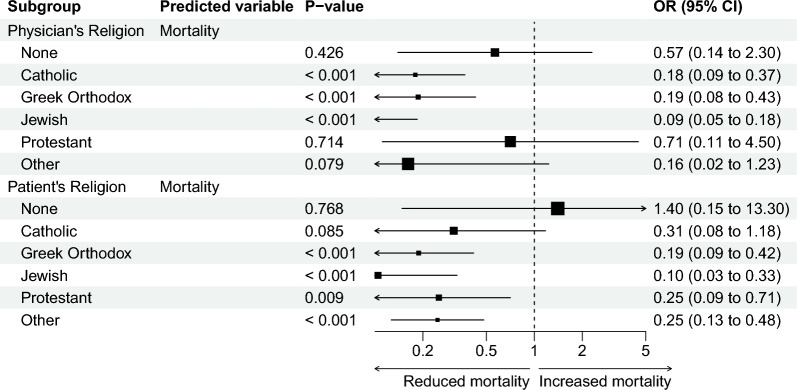
Mortality
Significant declines in patient mortality between the Ethicus-1 and Ethicus-2 studies were observed across Catholic, Greek Orthodox, and Jewish physician religious affiliations. The corresponding GEE model for mortality frequency, and the time until mortality model (LLM estimates) within patients that died are shown in Figs. 2 and 3, and further detailed in supplementary Tables S6–S9. With respect to patient religious affiliations, a significant decline in mortality was observed in Greek Orthodox, Jewish, Protestant, and other religions. It seems reasonable to suggest that such declines are supported by increased frequencies of withholding therapy in Ethicus-2 when compared to Ethicus-1 across almost all religions. The multivariable time models predict a significant decrease by 53% in the time period between limitation and patient death when patients were treated by physicians with no religious affiliation. Conversely, the time period significantly increased by 154% and 99% in patients treated by Greek Orthodox physicians and physicians with other (unspecified) religious affiliations, respectively.
Fig. 2.
Forest plot from the general estimating equation (GEE) model estimates showing the changes in odds ratios (OR) from Ethicus-1 to Ethicus-2 in the odds of patient mortality with respect to different physician and patient religious affiliations. P values indicate the statistical significance of change for each religion factor when compared to the model’s intercept. Confidence intervals (CI) at 95% from the estimate indicate lower and upper limits of the changes. The size of squares positioned at fold-change estimates are proportional to the size of the corresponding standard errors. Changes in odds ratios for physician and patient religious affiliations are estimated from separate models. The fold-change estimates are based on the models in Tables S6–S7
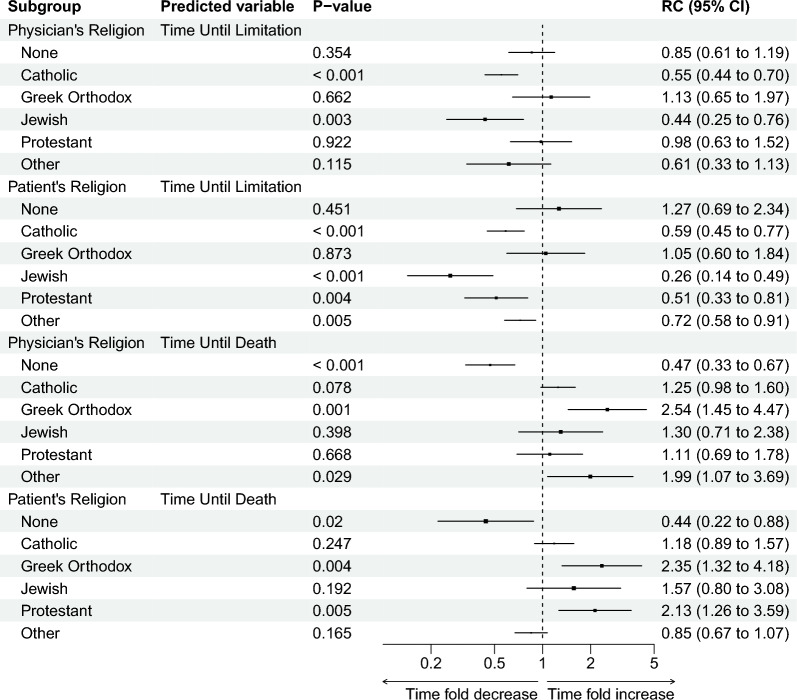
Fig. 3.
Forest plot with relative changes (RC) from the LMM estimates from Ethicus-1 to Ethicus-2 of time until first limitation and time until death with respect to physician and patient religious affiliations. P values indicate the statistical significance of change for each religion factor when compared to the model’s intercept. Confidence intervals (CI) at 95% from the estimate indicate lower and upper limits of the relative changes. The size of squares positioned at relative change estimates are proportional to the size of the corresponding standard errors. Relative changes for physician and patient religious affiliations are estimated from separate models. The relative change estimates are based on the models in Tables S8–S11
Religion and time until end-of-life decision
Among all patients who had limitations of life-sustaining therapy, time from ICU admission to first end-of-life decision decreased between studies from a median of 4.16 days (IQR 1.0–12.5) to 2.07 days (IQR 0.3–7.5). The time until limitation was significantly reduced from Ethicus-1 to Ethicus-2 when Catholic and Jewish physicians made end-of-life decisions (− 45% and − 56% respectively, Fig. 3 and supplementary Table S10), and when patients were Catholic, Jewish, Protestant, or with other non-specified religious affiliations (− 41%, − 74%, − 49%, and − 28% respectively, Fig. 3 and supplementary Table S11).
Discussion
End-of-life practices changed considerably over 16 years in the participating European ICUs. In this preplanned sub-study of a large multinational observational study [2], we observed that the distribution of physician religious affiliations did not substantially change over time, or across geographical regions. Nevertheless, substantial changes in end-of-life practices are highlighted by significantly reduced patient mortality and time until end-of-life decisions, supported by an increased awareness of patient-centred ICU practice through more frequent contemplation of patient wishes and communication with their families. Differences in withholding versus withdrawing life-sustaining treatments over 16 years of practice appear likely not a result of changes in practices within specific religious affiliations.
However, although large changes in practices with respect to religion can be excluded, a few wide confidence intervals cannot completely exclude religion’s role in specific cases of end-of-life decision-making. As an example, withdrawing over withholding treatment was increasingly performed by Protestant physicians and physicians without religious affiliation, whereas Jewish physicians did not withdraw life-sustaining treatments at all in the Ethicus-2 study.
In the Ethicus-1 study, we concluded that a certain practice change might have occurred when Jewish physicians worked in environments where withdrawal was part of the routine decisions taken [5]. However, we have no explanation for this observation and why this practice change seems to have “disappeared”. Further, over the 16-year observational interval, we noted a significant reduction in the time until an end-of-life decision occurred. In general, the availability of information on patient wishes increased over time, and more often, end-of-life practices were established after previous discussions with family.
Previous studies indicate that religion and culture affect end-of-life practices in the ICU [5, 15, 16]. In the current study, we noted both an expedited process (time until decision) and more involvement by patients and families in end-of-life decision-making. Although the reasons for this are not clear due to the observational nature of the investigation, the most likely explanation is that since the mid-1980s, the former paternalistic model has given way to a model that places more value on efforts to respect patient autonomy and to include patients’ families in shared decision-making [17]. We found that these changes were not based on changes in religious views, which matches the Ethicatt study results, where it was seen that physicians´ religious affiliation versus those without any affiliation had no influence on their view on patient autonomy [4].
Strengths and limitations
This is the first large multinational study to assess the impact of different religions on changes in end-of-life practices over time. Additionally, the same definitions for end-of-life practices were used to ensure comparability between the two Ethicus studies [2, 10]. The observational nature of the study may thus reflect a reality of the time of investigation in the selected ICUs [8, 9]. While physician religious affiliations were noted from the physicians performing the actual end-of-life practices, data confidentiality allowed clinicians to report their religion in a protected environment, including reporting of practices of questionable legality in some regions, such as shortening of the dying process. Still, underreporting of practices for fear of legal consequences cannot be excluded with certainty.
Our descriptive analysis also has a number of limitations. First, data from only about 60% (i.e. 22 out of 37) of ICUs participating in Ethicus-1 was available (some were closed, some were clinically not comparable anymore, and some were unable/ abstained from participation). Further, despite that some religions appear mainly represented in specific countries (like Judaism in Israel, Greek Orthodox in Greece, etc.) (supplementary Tables S15, S16), detailed statistical “per-country” analyses were refrained from in the light of the complexity of country/regions, culture, religious affiliations, religion-related influence on ethical aspects, and the varying frequencies of respective religions within these multiple countries. Second, patients were followed up until ICU discharge, death, or 2 months from the first decision to limit treatment (limited observational period). Third, both Ethicus studies included patients who died or had limitations of life-sustaining treatments. Conversely, although interesting, data on patients that did not die or did not have limitations of life-sustaining treatments are unavailable, preventing e.g. additional statistical comparisons of a “no limitation survivor group” versus a “limitation group” (independently of survival status). Fourth, data on physician religious affiliations for CPR and BD were not available for technical reasons, which prevented performing of additional statistical subgroup analyses [e.g. on patients who died without having a limitation (i.e. failed CPR and BD subgroups) vs. patients with WH/WD/SDP]. Fifth, distributions of physician and patient religious affiliations appear unbalanced, with the Catholic group greatly over-represented. However, this over-representation is present in both the Ethicus-1 and Ethicus-2 data, making overall comparison of the two time periods valid. Sixth, over-representation and unknown/ missing records of specific end-of-life practices from particular religious affiliations may challenge the assumption of statistical models presented in this observational study. Seventh, patient religious affiliations were unknown in a considerable number of cases. Despite study team efforts, that information was often unknown (not missing) and could not be retrieved in e.g. unconscious, critically ill patients. Nevertheless, as most decisions were made by physicians, the unknown data for patient religious affiliation may be regarded not that relevant as it would be for potential unknown data regarding physician religious affiliation. Further, although certainly of particular interest, “strength” of religious beliefs (religiosity) and/or “weight” of the religion in the culture of patients and families was not analysed in the present comparison study. Although this might be regarded particularly difficult to assess, this aspect should be explored in subsequent investigations. Nevertheless, based on the currently available medical literature and the results of the Ethicus-1 study, religion plays an important factor on whether doctors decide to withdraw or withhold life-sustaining treatments. This is why in the Ethicus-2 study, we deliberately decided to choose a dependent variable of “active” (i.e. WD & SDP) vs. “passive” (i.e. WH) limitations in the statistical analyses. The focal point in the current analysis was to compare the evolution over time (16 years) using the exact same definitions in Ethicus-1/Ethicus-2 in the pre-defined end-of-life categories, including the aspect whether the physician decision was “active” vs. “passive”.
Among patients with an end-of-life decision, the type of decisions did not change significantly with respect to religious affiliations, while some of the confidence intervals are too wide to suggest that religion did not play a role in the decision-making processes of treating physicians. Nevertheless, the models indicate that for some religions a large change in end-of-life practice due to religious affiliation can be excluded.
Another interesting observation might be that more patients survived after withholding life-sustaining therapies on the ICU. Limitations occurred earlier, likely to respect patients' wishes and to avoid invasive therapies that might prolong a “dying process”, and/or to avoid poor quality of life. Although certainly speculative, questions might remain whether some additional patients would survive if therapy was continued. Further, and importantly, decreased time until limitations might reflect increased attention to patient wishes and discussions with families. Overall, it seems tempting to speculate that the fact that religious affiliations did not affect end-of-life decisions over a 16-year time period might reflect increased awareness on the importance of patient-centred care and rapidly evolving intensive care medicine [17], while religious beliefs and traditions do not seem to be associated with changes in end-of-life practices over time [18].
Conclusions
In the present observational study, we observed significant changes in end-of-life practices over 16 years in European ICUs, which appear not primarily driven by religious affiliations of ICU patients or their treating physicians. Importantly, although a general substantial impact of religion on the noted changes in end-of-life practices appears unlikely, more granular data on “strength” of religious beliefs (religiosity) and/or “weight” of the religion in the culture was not available and the observed confidence intervals do formally not allow to entirely dismiss any impact of religion in specific instances. Moreover, a reduced time until decision-making and increased numbers of patient and family discussions was noted, which may indicate increased awareness of the importance of end-of-life decision-making in today’s ICUs.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The study team is indebted to all participating ICU physicians, nurses, study nurses, and technicians for their dedicated help and support to Ethicus-2.
The ETHICUS-2 study group: Scientific Coordinating Center (Israel)—C. L. Sprung (Coordinator), R. Bernstein (Administrator), A. Avidan (Internet webmaster and Database manager). Steering Committee—Charles L. Sprung (Chair), Matthew Anstey, Alexander Avidan, Elie Azoulay, Julie Benbenishty, Du Bin, Deborah Cook, Randy Curtis, Charles Feldman, Christiane Hartog, Gavin Joynt, Motoshi Kainuma, Mitchell Levy, RK Mani, Andrej Michalsen, Bara Ricou, Marcio Soares, Robert Truog. Investigators of the ETHICUS comparison study (centre coordinators underlined) and affiliation: Belgium: D. Ledoux, University of Liège, Liège; C. Ingels, University Hospital Gasthuisberg, Leuven. Czech Republic: D. Nalos, Aro Masarykova Nemonice; Usti nad Labem. Denmark: J. Gjedsted, Arhus University Hospital, Arhus. Germany: C. Hartog, Jena University Hospital, Jena. Greece: S. Zakynthinos, Evangelismos Hospital, Athens; C. Mathas, Agia Olga Hospital of Nea Ionia, Athens; G Nakos, B. Koulouras, G. Papathanakos, University Hospital of Ioannina, Ioannina. Ireland: O. Miskolci, Mater Hospital, University College; Dublin. Israel: C. L. Sprung, A. Avidan, V. de la Guardia, A. Farran, V. Van Heerden, Hadassah Medical Center, Hebrew University of Jerusalem, Faculty of Medicine, Jerusalem; M. Klein, Soroka Hospital, Beer-Sheva; P. Levin, Shaarei Zedek Medical Center, Jerusalem. Italy: A. Palo, Policlinico San Matteo, Pavia. Netherlands: A. Girbes, VU Hospital, Amsterdam. Portugal: P. Maia, Hospital Geral Santo Antonio, Porto; L. Bento, Hospital de S. Jose, Lisboa. Spain: J.M.G. Garcia, Hospital Gregorio Maradon, Madrid; A. Vidal Tegedor, Hospital General de Castello, Castello. Switzerland: B. Ricou, Hôpital Cantonal Universitaire de Genève, Geneva; S. Marsch, Kantonsspital Basel, Basel; J.C. Schefold, Inselspital, University of Bern, Bern. Turkey: F. Esen, University of Istanbul, Istanbul. United Kingdom. D. Brealey, University College London, London.
Author contributions
CS and AA developed the research strategy and steered Ethicus-1 and Ethicus-2 together with the scientific steering board. LR co-drafted the article and performed data analyses. JCS co-drafted the article and recruited patients, and LR and JCS coordinated the input of all authors. AG, LR, MP, and PM performed all statistical/ data analyses and LR produced all figures. All authors contributed to the data interpretation and co-drafted the article for important intellectual content. All authors read and approved the final version of the manuscript.
Funding
Open access funding provided by University of Bern.
Data availability
The datasets generated or analyzed during the current study are available from the corresponding author (after approval by the study steering team) on reasonable non-commercial request.
Declarations
Conflicts of interest
JCS declares that the Dept. of Intensive Care Medicine, Inselspital, Bern, has received research or other grants from (full departmental disclosure): Orion Pharma, Abbott Nutrition International, B. Braun Medical AG, CSEM AG, Edwards Lifesciences Services GmbH, Kenta Biotech Ltd, Maquet Critical Care AB, Omnicare Clinical Research AG, Nestle, Pierre Fabre Pharma AG, Pfizer, Bard Medica S.A., Abbott AG, Anandic Medical Systems, Pan Gas AG Healthcare, Bracco, Hamilton Medical AG, Fresenius Kabi, Getinge Group Maquet AG, Dräger AG, Teleflex Medical GmbH, Glaxo Smith Kline, Merck Sharp and Dohme AG, Eli Lilly and Company, Baxter, Astellas, Astra Zeneca, CSL Behring, Novartis, Covidien, Nycomed, Phagenesis, and Cytel outside the submitted work. The money was paid into departmental funds. No personal financial gain applies. The other authors declare no conflict of interest.
Footnotes
The members of the ETHICUS II Study Group are listed in Acknowledgements.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Joerg C. Schefold and Livio Ruzzante shared first authorship.
Contributor Information
Joerg C. Schefold, Email: joerg.schefold@insel.ch
Livio Ruzzante, Email: livio.ruzzante@gmail.com.
the ETHICUS II Study Group:
C. Sprung, R. Bernstein, A. Avidan, Charles L. Sprung, Matthew Anstey, Alexander Avidan, Elie Azoulay, Julie Benbenishty, Du Bin, Deborah Cook, Randy Curtis, Charles Feldman, Christiane Hartog, Gavin Joynt, Motoshi Kainuma, Mitchell Levy, R. K. Mani, Andrej Michalsen, Bara Ricou, Marcio Soares, Robert Truog, D. Ledoux, C. Ingels, D. Nalos, J. Gjedsted, C. Hartog, S. Zakynthinos, C. Mathas, G. Nakos, B. Koulouras, G. Papathanakos, O. Miskolci, C. L. Sprung, A. Avidan, V. de la Guardia, A. Farran, V. Van Heerden, M. Klein, P. Levin, A. Palo, A. Girbes, P. Maia, L. Bento, J. M. G. Garcia, A. Vidal Tegedor, B. Ricou, S. Marsch, J. C. Schefold, F. Esen, and D. Brealey
References
- 1.Sprung CL, et al. The influence of geography, religion, religiosity and institutional factors on worldwide end-of-life care for the critically ill: the WELPICUS study. J Palliat Care. 2021 doi: 10.1177/08258597211002308. [DOI] [PubMed] [Google Scholar]
- 2.Sprung CL, et al. Changes in end-of-life practices in European intensive care units from 1999 to 2016. JAMA. 2019;322(17):1692–1704. doi: 10.1001/jama.2019.14608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Avidan A, et al. Variations in end-of-life practices in intensive care units worldwide (Ethicus-2): a prospective observational study. Lancet Respir Med. 2021;9(10):1101–1110. doi: 10.1016/S2213-2600(21)00261-7. [DOI] [PubMed] [Google Scholar]
- 4.Bülow HH, et al. Are religion and religiosity important to end-of-life decisions and patient autonomy in the ICU? The Ethicatt study. Intensive Care Med. 2012;38(7):1126–1133. doi: 10.1007/s00134-012-2554-8. [DOI] [PubMed] [Google Scholar]
- 5.Lautrette A, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356(5):469–478. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 6.Sprung CL, et al. The importance of religious affiliation and culture on end-of-life decisions in European intensive care units. Intensive Care Med. 2007;33(10):1732–1739. doi: 10.1007/s00134-007-0693-0. [DOI] [PubMed] [Google Scholar]
- 7.Blank RH. End-of-life decision making across cultures. J Law Med Ethics. 2011;39(2):201–214. doi: 10.1111/j.1748-720X.2011.00589.x. [DOI] [PubMed] [Google Scholar]
- 8.Phua J, et al. Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med. 2015;175(3):363–371. doi: 10.1001/jamainternmed.2014.7386. [DOI] [PubMed] [Google Scholar]
- 9.Meñaca A, et al. End-of-life care across Southern Europe: a critical review of cultural similarities and differences between Italy, Spain and Portugal. Crit Rev Oncol Hematol. 2012;82(3):387–401. doi: 10.1016/j.critrevonc.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Sprung CL, et al. End-of-life practices in European intensive care units the Ethicus study. JAMA. 2003;290(6):790–797. doi: 10.1001/jama.290.6.790. [DOI] [PubMed] [Google Scholar]
- 11.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- 12.Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest package: tests in linear mixed effects models. J Stat Softw. 2017;82:1–26. doi: 10.18637/jss.v082.i13. [DOI] [Google Scholar]
- 13.Højsgaard S, Halekoh U, Yan J. The R package geepack for generalized estimating equations. J Stat Softw. 2006;15:1–11. doi: 10.18637/jss.v015.i02. [DOI] [Google Scholar]
- 14.Dayimu A (2022) ‘Forestploter: Create Flexible Forest Plot’. [Online]. https://CRAN.R-project.org/package=forestploter. Accessed 4 Nov 2022
- 15.Schweda M, Schicktanz S, Raz A, Silvers A. Beyond cultural stereotyping: views on end-of-life decision making among religious and secular persons in the USA, Germany, and Israel. BMC Med Ethics. 2017;18(1):13. doi: 10.1186/s12910-017-0170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El Jawiche R, Hallit S, Tarabey L, Abou-Mrad F. Withholding and withdrawal of life-sustaining treatments in intensive care units in Lebanon: a cross-sectional survey of intensivists and interviews of professional societies, legal and religious leaders. BMC Med Ethics. 2020;21(1):80. doi: 10.1186/s12910-020-00525-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kilbride MK, Joffe S. The new age of patient autonomy: implications for the patient-physician relationship. JAMA. 2018;320(19):1973–1974. doi: 10.1001/jama.2018.14382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bülow HH, et al. The world’s major religions’ points of view on end-of-life decisions in the intensive care unit. Intensive Care Med. 2008;34(3):423–430. doi: 10.1007/s00134-007-0973-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated or analyzed during the current study are available from the corresponding author (after approval by the study steering team) on reasonable non-commercial request.