Abstract
Background
Autism spectrum disorder (ASD) is a neurodevelopmental disorder with deficits in social communication and interaction, restricted and repetitive patterns of behaviour, interests and activities. Autism spectrum disorder is associated with multiple comorbidities. As a result, caregivers of children with ASD experience increased levels of burden and poor quality of life. However, there is a paucity of information on the burden.
Aim
The study aimed to describe the sociodemographic profiles and determine the extent of the burden experienced by caregivers of children and adolescents with ASD.
Setting
The Child, Adolescent and Family Unit (CAFU) outpatient services at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH).
Methods
A quantitative, descriptive, cross-sectional study was done. Two self-administered questionnaires were used: a sociodemographic questionnaire and the 12-item Zarit Burden Interview questionnaire.
Results
The questionnaires were completed by 77 caregivers, of which the majority were female (n = 56 or 72.3%), mothers to children with ASD (n = 49 or 64.3%) and identified as Christian (p < 0.001). Most had completed secondary school or had a tertiary education (p = 0.003) and were employed (p < 0.001). Among the caregivers, 41.6% experienced mild to moderate burden, 33.8% experienced high burden and only 24.9% reported no to mild burden.
Conclusion
Caregivers of children and adolescents with a diagnosis of ASD are mostly mothers and experience mild to moderate levels of caregiver burden, suggesting the need for improved screening and psychosocial support programmes.
Contribution
This study highlights the burden experienced by primary caregivers of children with ASD and is one of the few comprehensive studies on this issue within the context of South Africa.
Keywords: autism spectrum disorders, caregiver burden, children, Zarit Burden Interview, South Africa
Introduction
Autism spectrum disorder (ASD) is a complex, heterogeneous, multifaceted neurodevelopmental disorder with onset during early childhood.1,2 It is characterised by significant and persistent deficits in social communication and social interaction, as well as restricted, repetitive patterns of behaviour, interests and activities.3
The Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM-5TM) divides the severity of ASD into three levels based on the degree of impairment in adaptive and cognitive functioning.3 Individuals with level 1 severity require some support, while individuals with level 2 need substantial support and those with level 3 need very substantial support.3
The global prevalence of ASD is increasing because of a better understanding of the disorder and the expansion of the diagnostic criteria.4 Elsabbagh et al.5 estimated that the mean global prevalence translated into 1 child out of 160 having ASD, while Franz et al.6 reported the prevalence to be between 1% and 2% of the global population. In Africa, studies on the prevalence of child and adolescent mental disorders have been conducted on small samples and are, therefore, poorly representative of the disease burden.5 Although prevalence studies in South Africa are limited, a survey by Pillay et al.7 in the Western Cape showed that the prevalence of ASD increased by 76.03% from 2012 to 2016, with an annual increase of 15.18%.
There is a high rate of medical and psychiatric comorbidities associated with ASD. Medical disorders include refractory epilepsy, sleep disorders and gastrointestinal disorders, whereas psychiatric disorders include intellectual disability, attention-deficit hyperactive disorder, motor disorders, behavioural problems, anxiety disorders and mood disorders.8,9,10,11,12,13,14,15,16,17,18 In addition, the complexity of the disorder, associated comorbidities and lifelong nature contribute to the burden experienced by caregivers.19
There are no definite protocols for treating ASD and its associated comorbidities.20 Pharmacological interventions are limited to treating comorbidities and lessening symptom severity, but they are ineffective in addressing the core symptoms of ASD.21
A well-informed caregiver is an essential part of managing a child with ASD. A caregiver is defined by Kent et al.22 as the person responsible for looking after someone who cannot function independently and requires assistance with activities of daily living. Caregivers are required to meet the needs of the child with ASD, manage challenging behaviour and follow through with professional recommendations from healthcare providers.23
Research on caregiver burden began receiving attention in the late 1970s, and in recent years, more research has been generated on caregivers looking after patients with medical and psychiatric disorders.24,25 However, research in children and adolescents primarily focuses on medical conditions, with research on psychiatric disorders and caregiver burden needing to be improved.26
Previous research on caregivers has reported on the comprehensive challenges experienced by caregivers, including negative impacts on their physical and emotional well-being, difficulties in relationships with other family members, work challenges and financial constraints because of loss of income.27 Primary caregivers face multiple challenges and experience impairments in their quality of life.23
Research has shown that biological mothers are usually the primary caregivers of children with ASD.28 It has been concluded that they often experience higher levels of burden than mothers of typically developing children.28 Caregivers of children with ASD have reported elevated fatigue levels and increased physical health complaints compared to caregivers of neurotypical and intellectually disabled children.29
Special attention has been given to the incidence of mental disorders in caregivers of children with ASD. Karst et al.30 reported a higher incidence rate of depression and anxiety among caregivers of children with developmental disabilities, including ASD. Lai et al.31 recognised that caregivers reported more depressive symptoms and that anxiety symptoms tend to fluctuate throughout the child’s development. Sharpley et al.32 concluded that challenging behavioural problems are associated with a higher prevalence of depression and anxiety. Paruk and Ramdhial33 conducted a study in South Africa that determined mothers were mostly the primary caregivers of children with psychiatric disorders and that they experienced high levels of burden and depressive and anxiety symptoms.
Challenges associated with behaviour and the stigmatisation of children with ASD often result in social isolation and decreased quality of life for caregivers.34 However, a more recent study by Ten Hoopen et al.28 did not find a significant decrease in health-related quality of life in primary caregivers of children with ASD. This finding was attributed to the measuring tools used and the sample characteristics of their study population.
Parents of children diagnosed with ASD reported lower marital satisfaction levels.35 The divorce rates among these families also appear to be nearly double compared to families with typically developing children, with younger parents at higher risk.36
Caregivers often incur financial burdens. As a result, they are more likely to experience a loss of income and ultimately less access to supportive resources, including appropriate school placements, specialised care facilities and social-emotional support.34
Identifying the specific areas of burden experienced by caregivers of children with ASD can help develop tailored support structures to meet their unique needs. By providing adequate support, caregivers can better manage the challenges associated with caring for a child with ASD and improve their quality of life.
In the literature, caregiver burden is measured by well-defined tools, with the Zarit Burden Interview (ZBI) questionnaire being one of them.37 The ZBI has been used in multiple international research studies over a wide range of sociodemographic profiles.38,39 However, while South African researchers have used the ZBI questionnaire to determine caregiver burden among caregivers of orphaned children in rural South Africa, there has yet to be any known research on its use in the psychiatric caregiving population in South Africa.40
There is a paucity of research in South Africa measuring caregiver burden in child and adolescent psychiatry. Nonetheless, because of the unique challenges of caring for a child with ASD, it is essential to research this population to better understand the extent of the burden and develop appropriate support structures.
Aim
The study aimed to describe the sociodemographic profiles and to determine the extent of caregiver burden among caregivers of children and adolescents diagnosed with ASD at the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) in South Africa.
Research method and design
Study design and setting
A quantitative, descriptive, cross-sectional study was conducted. The participants were asked to complete a self-administered sociodemographic questionnaire and the 12-item ZBI questionnaire.24
The sociodemographic questionnaire comprised questions on the following variables: age, gender, marital status, religion, the highest level of education, employment status, monthly income or disability grant and the relationship between the caregiver and the patient with ASD.
The ZBI questionnaire is a standardised questionnaire validated for research use in the caregiving population by Seng et al.41 Previous research has identified that the 12-item short-form version was suitable for screening for caregiver burden, demonstrated good psychometric properties and was validated in cross-sectional and longitudinal studies.37 The 12-item version consists of two domains, personal and role strain and is measured on a five-point Likert scale. The range of summed scores is between 0 and 48, with a total score of 0–10 representing no to mild burden, 11 to 20 representing mild to moderate burden and above 20 representing high burden.42
The study was conducted at the Child, Adolescent and Family Unit (CAFU) at CMJAH from October 2021 to February 2022. The unit provides outpatient services and is part of the Division of Child and Adolescent Psychiatry at the Department of Psychiatry, University of Witwatersrand Medical School.
Study population
All consenting caregivers older than 18 years of age looking after a child or adolescent diagnosed with ASD attending the unit at CMJAH were included in the study.
Participants of all genders, ethnicities, religions and sociodemographic backgrounds were included. Participants unable to complete the questionnaires because of a language barrier were provided with a translator after obtaining consent. Caregivers declining to participate were excluded from the study and only participants who completed both questionnaires were included in the data analysis.
The sample size was determined by assessing z-scores of expected frequencies per question in the ZBI questionnaire. Statistical significance could be expected with a minimum sample of 70, assuming a large effect size.
Data collection
The consenting caregivers completed the questionnaires in a private room. Where assistance with completing the questionnaires was required, the researcher or the allocated case manager aided. The complete questionnaires were placed in a sealed box.
Data analysis
Categorical data scores were analysed using Pearson’s chi-square tests for sociodemographic variables and the multiple responses for each ZBI question. Continuous variables (e.g. age) were summarised as mean (SD). In addition, Likert plots were generated for various responses to the ZBI question. All tests were two-tailed probability values and statistical significance was accepted when α ≤ 0.05.
Ethical considerations
Permission for this study was granted by the Human Research Ethics Committee (Medical) of the University of the Witwatersrand (no. M210841).
Written informed consent was obtained for every participant in the study. Each participant was allocated a study number and no identifying data was used.
A distress protocol with available resources and contact information was provided to all participants.
Results
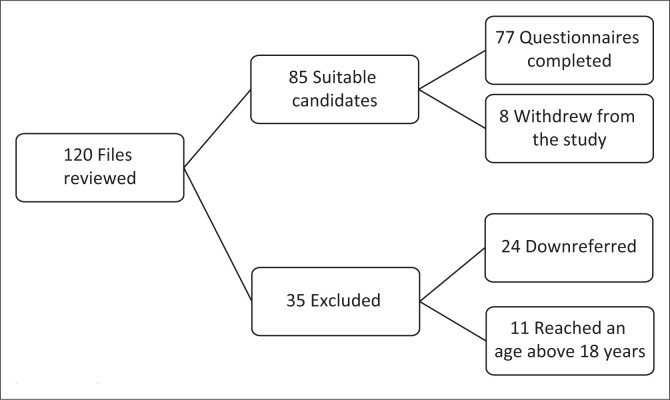
The clinical records of 120 patients with a primary diagnosis of ASD were reviewed (Figure 1). Thirty-five patients were excluded from the study, with 24 being down-referred to community clinics and 11 being transferred to adult psychiatric services after reaching the age of 18 years. The questionnaires were administered to 85 participants, of which 8 did not complete the questionnaires. Only 77 were included in the final data analysis.
FIGURE 1.
Flowchart outlining participant selection.
The sociodemographic characteristics
Table 1 presents the sociodemographic characteristics of the participants. Most caregivers were female (n = 56 or 72.73%), while only 21 (27.27%) were male. The mean age of the participants was 44.4 (SD ± 8.9) years. The females were younger with a mean age of 43.6 years and males were slightly older with a mean age of 47.2 years.
TABLE 1.
Sociodemographic characteristics of the caregivers in a study population at the Charlotte Maxeke Johannesburg Academic Hospital.
| Demographics | Count | % | p |
|---|---|---|---|
| Age (n = 77) | |||
| Mean age | 44.4 | - | - |
| Mean age of males | 47.2 | - | - |
| Mean age of females | 43.6 | - | - |
| Gender (n = 77) | - | - | < 0.001 |
| Male | 21 | 27.27 | - |
| Female | 56 | 72.73 | - |
| Other | 0 | 0.00 | - |
| Marital status (n = 76) | - | - | < 0.001 |
| Single | 34 | 44.74 | - |
| Married | 30 | 39.47 | - |
| Divorced | 4 | 5.26 | - |
| Separated | 2 | 2.63 | - |
| Widowed | 6 | 7.89 | - |
| Religion (n = 77) | - | - | < 0.001 |
| Christian | 65 | 84.42 | - |
| Muslim | 3 | 3.90 | - |
| Hindu | 0 | 0.00 | - |
| Jewish | 2 | 2.60 | - |
| Spiritual | 3 | 3.90 | - |
| African traditional beliefs | 2 | 2.60 | - |
| Other (specify) | 2 | 2.60 | - |
| Highest level of education (n = 76) | - | - | < 0.001 |
| Primary school | 4 | 5.26 | - |
| Secondary school | 37 | 48.68 | - |
| Tertiary education | 27 | 35.53 | - |
| College | 8 | 10.53 | - |
| Employment (n = 77) | - | - | 0.003 |
| Full time employed | 35 | 45.45 | - |
| Part-time employed | 12 | 15.58 | - |
| Unemployed | 30 | 38.96 | - |
| Income (n = 77) | - | - | < 0.001 |
| Disability grant | 12 | 15.58 | - |
| R0 – R3000 | 23 | 29.87 | - |
| R3000 – R6000 | 13 | 16.88 | - |
| R6000 – R9000 | 4 | 5.19 | - |
| R9000 – R12 000 | 4 | 5.19 | - |
| R12 000 – R15 000 | 3 | 3.90 | - |
| Above R15 000 | 18 | 23.38 | - |
| Other (specify) | 0 | 0.00 | - |
| Relationship to the patient (n = 76) | - | - | < 0.001 |
| Mother | 49 | 64.47 | - |
| Father | 16 | 21.05 | - |
| Grandmother | 6 | 7.89 | - |
| Grandfather | 1 | 1.32 | - |
| Aunt | 0 | 0.00 | - |
| Uncle | 0 | 0.00 | - |
| Sibling | 0 | 0.00 | - |
| Foster parent | 0 | 0.00 | - |
| Other (specify) | 4 | 5.26 | - |
Note: Sample sizes vary because of missing data.
In this sample, most caregivers were single (n = 34 or 44.74%), while more than one-third were married (39.47% or n = 30). Of the remaining caregivers, 7.89% (n = 6) were widowed, 5.26% (n = 4) were divorced and 2.63% (n = 2) were separated.
Most caregivers identified as Christian (84.42% or n = 65), while two (2.6%) identified as Jehovah’s Witnesses. A small percentage identified as Muslim or followed spiritual beliefs (3.9% or n = 3, respectively) and Jewish or African traditional beliefs (2.6% or n = 2 each).
Most caregivers (48.68% or n = 37) completed secondary education, while 46.06% (n = 35) completed tertiary education. On the other hand, very few caregivers (5.26%, n = 4) did not study further than primary school.
Out of all the caregivers, 61.03% (n = 47) were employed. Of those employed, 45.45% (n = 35) worked full time and 15.58% (n = 12) worked part time. Meanwhile, over one-third (38.9% or n = 30) were unemployed.
Approximately one-third of caregivers (29.87% or n = 23) received a monthly income of R3000 or less, with 15.58% (n = 12) solely relying on a child disability grant. An income between R6000 to R15 000 was reported by 31.16% (n = 24) and only 23.38% (n = 18) received a monthly income greater than R15 000.
Mothers comprised the majority of caregivers (64.47% or n = 49) for children and adolescents with ASD, while fathers accounted for only 21.05% (n = 16) of primary caregivers. In seven cases (9.21%), grandparents were identified as primary caregivers. Only 5.26% (n = 4) of the caregivers were not biological relatives of the children or adolescents, with 3 being formally employed full-time help and one being a stepfather to the child with ASD. Siblings, aunts, uncles and foster parents were not identified as caregivers in this sample population.
The Zarit Burden Interview characteristics
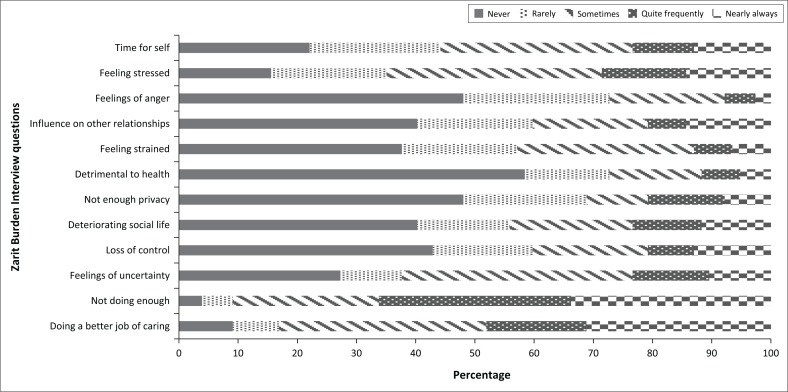
The findings are summarised in Table 2 and Figure 2.
TABLE 2.
Zarit Burden Interview questionnaire.
| Question: How often do you feel … | Never |
Rarely |
Sometimes |
Quite frequently |
Nearly always |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |
| … that because of the time you spend with your relative that you don’t have enough time for yourself? | 17 | 22.08 | 17 | 22.08 | 25 | 32.47 | 8 | 10.9 | 10 | 12.99 |
| … stressed between caring for your relative and trying to meet other responsibilities (work or family)? | 12 | 15.58 | 15 | 19.48 | 28 | 36.36 | 11 | 14.29 | 11 | 14.29 |
| … angry when you are around your relative? | 37 | 48.05 | 19 | 24.68 | 15 | 19.48 | 4 | 5.19 | 2 | 2.60 |
| … that your relative currently affects your relationship with family members or friends negatively? | 31 | 40.26 | 15 | 19.48 | 15 | 19.48 | 5 | 6.49 | 11 | 14.29 |
| … strained when you are around your relative? | 29 | 37.66 | 15 | 19.48 | 23 | 29.87 | 5 | 6.49 | 5 | 6.49 |
| … that your health has suffered because of your involvement with your relative? | 45 | 58.44 | 11 | 14.29 | 12 | 15.58 | 5 | 6.49 | 4 | 5.19 |
| … that you don’t have as much privacy as you would like because of your relative? | 37 | 48.05 | 16 | 20.78 | 8 | 10.39 | 10 | 12.99 | 6 | 7.79 |
| … that your social life has suffered because you are caring for your relative? | 31 | 40.26 | 12 | 15.58 | 16 | 20.78 | 9 | 11.69 | 9 | 11.69 |
| … that you have lost control of your life since your relative’s illness? | 33 | 42.86 | 13 | 16.88 | 15 | 19.48 | 6 | 7.79 | 10 | 12.99 |
| … uncertain about what to do about your relative? | 21 | 27.27 | 8 | 10.39 | 30 | 38.96 | 10 | 12.99 | 8 | 10.39 |
| … you should be doing more for your relative? | 3 | 3.90 | 4 | 5.19 | 19 | 24.68 | 25 | 32.47 | 26 | 33.77 |
| … you could do a better job in caring for your relative? | 7 | 9.09 | 6 | 7.79 | 27 | 35.06 | 13 | 16.88 | 24 | 31.17 |
FIGURE 2.
Likert plots of the responses to a Zarit Burden Interview questionnaire by caregivers of children with autism spectrum disorder at the Charlotte Maxeke Johannesburg Academic Hospital.
Of the caregivers in this sample, 25 (32.47%) reported feeling that they sometimes did not have enough time for themselves because of their caregiving responsibilities. However, only 10 (12.99%) reported experiencing these feelings nearly always.
Of all the caregivers, 36.36% (n = 28) reported experiencing frequent stress while caring for a child with ASD and trying to meet the demands of work and family responsibilities. Among the remaining caregivers, 14.29% (n = 11) selected ‘quite frequently’ and ‘nearly always’ as their stress levels.
Feelings of anger towards the child with ASD were uncommon, with 48.05% (n = 37) reporting ‘never’ feeling this way. In addition, 40.26% (n = 31) felt that caring for the child or adolescent did not negatively affect their other relationships. Only five (6.49%) participants reported feeling ‘quite frequently’ or ‘nearly always’ strained by their caregiving roles.
Most caregivers (n = 45 or 58.44%) did not report a decline in their physical health. Additionally, 37 participants (48.05%) did not feel that their privacy had been affected by caring for a child with ASD. Only 9 participants (11.69%) reported a significant negative impact on their social lives because of their caregiving role, while 31 (40.26%) reported ‘never’ feeling this way.
Although most participants (n = 48 or 62.34%) experienced uncertainty about their role as a caregiver and what to do for the child with ASD under their care, the majority (n = 33 or 42.86%) did not feel they had lost control of their own lives.
The study found that caregivers felt a strong sense of responsibility to do more for the child with ASD and to improve their caregiving performance. These findings were statistically significant, with a p-value of less than < 0.001.
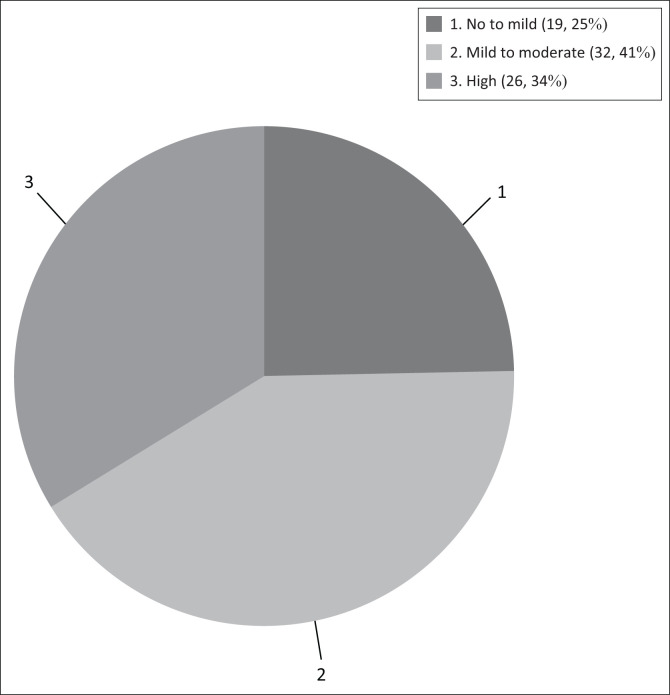
Burden prevalence
The burden prevalence results are presented in Figure 3, with each participant receiving an individual score. The majority of participants (n = 32 or 41.56%) experienced mild to moderate burden, while 26 (33.77%) reported high levels of burden. Less than one-quarter of participants (n = 19 or 24.68%) experienced no to mild burden. It is worth noting that the distribution of the scores was not found to be significantly different from chance (p = 0.19).
FIGURE 3.
Burden prevalence.
Of the male participants, 38.09% (n = 8) experienced no to mild burden, 47.62% (n = 10) experienced mild to moderate burden and 14.29% (n = 3) experienced high levels of burden. The majority of female participants also experienced mild to moderate burden (n = 27 or 48.21%). Only 10.71% (n = 6) of females experienced no to mild burden and 41.07% (n = 23) reported high levels of burden.
Discussion
Autism spectrum disorder is a complex neurodevelopmental disorder associated with challenging behaviour.1 Therefore, taking care of a child with ASD can be strenuous and caregivers often face multiple difficulties that subject them to higher stress levels.
Sociodemographic characteristics
Different sociodemographic characteristics can contribute to the level of burden that caregivers experience.
Multiple research studies in Europe and Africa revealed that mothers are generally the primary caregivers of their children with ASD.33,43 The current study supported previous findings, with 72.7% of the caregivers being female, of which 64.5% were mothers of the children with ASD. An additional finding was that one-fifth of caregivers were fathers to the children with ASD. However, there is a paucity of data on single fathers caring for children with ASD. It has been identified that the roles and experiences of fathers as primary caregivers are often overlooked.44
A review article by Lai et al.31 concluded that caregivers of children with ASD mostly fall within the middle-aged group. The current study also showed that most caregivers were middle-aged, with female caregivers slightly younger than males.
A South African study done in 2017 reported that most children with ASD grew up in a two-parent household.45 However, our study found that most caregivers were single (never married, divorced, separated or widowed), with only 39.5% being married. This finding could reflect the general South African household, where 42% of children are raised by their mothers only.46
A multinational study done in the United Kingdom, the United States, Canada and Australia looked at the influence of spirituality and religion on caregivers of ASD. The study identified that most caregivers (61%) were of the Christian religion.47 The current research supported this finding. However, the conclusion that most caregivers were Christian is in keeping with the religious affiliation of the general population in South Africa and might not be a significant study finding.48
Past research showed that most caregivers have at least completed secondary education.39,49 The current study showed similar results, with most caregivers having an education level of high school and above. A higher level of education can contribute to caregivers’ acquired knowledge of their child’s condition and the availability of supportive resources leading to better management and quality of life for the child. This could be explained by the assumption that educated caregivers are more likely to be employed and have access to specialised care.
Previous publications showed that caregivers of children with ASD were often unemployed.39,49 However, a Green50 study identified that employment could be a protective factor when caring for a child with ASD. In this study, most participants were either full-time or part-time employed. However, over one-third of the participants were unemployed. This finding could reflect the current economic climate in South Africa, where there is a higher unemployment rate compared to other countries.51
Research in South Africa identified that the costs of special education, medication, therapeutic interventions and special dietary requirements for children with ASD are high.52 Twelve caregivers relied exclusively on a child disability grant and 23 received between no income and R3000 per month. However, research done by Geldenhuys concluded that the current amount received from a monthly disability grant is insufficient to meet all the child’s demands.52 This can put additional strain on caregivers.
Zarit Burden Interview questionnaire characteristics
This study used the ZBI questionnaire to determine the extent of the caregiver burden.
Caregivers of children with ASD are at risk of developing psychiatric disorders, including depression and anxiety.53 Research done by Lai et al.31 compared parents of children with ASD to those of neurotypically developed children and found that parents of children with ASD experienced remarkably more difficulties regarding psychological well-being and coping. From this research, it is also evident that the personal well-being of caregivers suffered because of the role they were fulfilling. Caregivers reported feeling stressed about caring for the child with ASD and meeting all their responsibilities at home and work.
Functioning as a caregiver can lead to feelings of isolation, specifically related to the stigmatisation of the child with ASD and can contribute to interpersonal relationship strain.54 Caregivers in this study population were less likely to report that their relationships and social lives suffered severely. However, more than one-third did experience these feelings.
There is a paucity of research on the privacy of caregivers and how it is affected by the role they are fulfilling. However, despite the lack of research on this subject, the current study found that caregivers did not perceive their privacy to be impacted by their caregiving role.
The previous literature identified that physical health complaints and symptoms of fatigue were prominent features in caregivers.28,55 These symptoms were more pronounced when associated with depressive symptoms.28,55 In this study, caregivers did not feel that their physical health had been affected. A possible explanation could be that caregivers underreported these symptoms.
Most caregivers in this study felt that they still had enough time for themselves, had not lost control over their own lives and that they did not feel strained when they were around the child with ASD. This contrasts with a study by Ten Hoopen et al.28 which identified that more than half of the participating caregivers had difficulties combining their caregiving role with daily activities.
Behavioural problems in children with ASD can lead to anger and frustration.56 However, an interesting finding in this study was that most caregivers did not report feelings of anger but instead reported feeling that they could do more for the child with ASD.
Previous research reported that caregivers felt guilty for not spending all their free time with the child diagnosed with ASD and that they were not doing enough for them.54 This study agreed with previous publications and confirmed that caregivers felt uncertain about the child with ASD and, at the same time, reported that they could do a better job of taking care of the child.
Burden prevalence characteristics
Caregiver burden is frequently reported in the literature.
Consistent with prior research regarding caregiver burden in the context of ASD, most caregivers in this study encountered levels of burden ranging from mild to moderate.28,57 An intriguing discovery from the study was that a significant portion of both male and female participants indicated experiencing mild to moderate levels of burden. Notably, there exists a lack of research directly comparing the caregiving burden between men and women who care for children with ASD.
Previous research has identified possible protective factors against high levels of burden. Pandey et al.39 reported that higher levels of education were associated with lower levels of burden, and Mumtaz et al.58 further identified that non-working caregivers scored higher on the ZBI questionnaire. Unemployed caregivers could be subjected to social isolation and experience economic burdens because of the loss of income.59 Possible protective factors against high burden levels in this study population could have been that most participants were educated, employed and received an income.
An additional protective factor could have been that most participants were religious. However, the full spectrum of the influence of religion on caregiver burden in South Africa still needs to be explored in future research.
Limitations
To the author’s knowledge, this is one of the few studies conducted in South Africa on the caregiver burden in caregivers of children with ASD. Although it contributes to the understanding of the caregiver burden, several limitations must be acknowledged:
This cross-sectional descriptive study and correlations between variables could not be drawn because of the limited sample size. Further research harnessing a larger sample size would be beneficial.
The study’s cross-sectional nature precludes understanding the temporal sequence of factors that increase the caregiver burden.
The study does not show any causal relationship between the demographic characteristics and the extent of the caregiver burden. Therefore risk and protective factors among the demographics could not be established with certainty.
The study looked only at caregivers of children attending CMJAH and excluded caregivers of children with ASD attending community clinics, NGOs and the private sector.
The study did not look at community (non-clinical) samples of caregivers. Therefore the results cannot be applied to all caregivers of children with ASD.
The study did not measure the impact of the level of function and severity of symptoms in children with ASD on the caregiver burden.
In cases where translation was used, the accuracy of information collected could only be partially ascertained.
Conclusion
Autism spectrum disorder is a complex neurodevelopmental condition with many comorbidities. Taking care of a child with this disorder has a significant impact on the caregiver’s life. This is one of the few studies done in South Africa on caregiver burden in caregivers of children with ASD.
In this study, most of the caregivers were single mothers of the Christian faith. Most of the caregivers were educated and had part-time or full-time jobs. Despite most of the caregivers reporting that looking after a child with ASD was stressful, the minority reported that their social life and personal relationships were negatively affected.
Most of the caregivers did not report fatigue and ill physical health. Despite the difficult task of looking after a child with ASD, most caregivers did not report insufficient time for themselves. Caregivers in this study did not experience anger towards the child with ASD. Most experienced mild to moderate burden and felt guilty for not spending enough time with the child in their care.
Identifiable protective factors could be education, employment and religion, but more studies are needed to confirm the above findings.
Recommendations
Despite its limitations, this study suggests clinical implications for assessing the caregivers’ burden among caregivers of children with ASD.
Improved knowledge about the caregiver burden might inspire the development of more culturally sensitive screening tools for the South African population. In addition, the awareness that caregivers experience stress and guilt might encourage the development of support groups in tertiary and community settings.
Developing programmes aimed at improving caregivers’ understanding of their burden, risk factors and protective factors can lead to a better quality of life for them. Additionally, educating the community and other healthcare providers about the challenges faced by caregivers of children with ASD can increase awareness and support for this population.
And finally, future research is needed to assess the prevalence of mental health disorders among caregivers, given the significant stress and burden they experience.
Acknowledgements
The following contributions are gratefully acknowledged: all the caregivers who participated in this study, the staff at CAFU at the CMJAH and the University of Witwatersrand.
Competing interests
The authors have declared that no competing interest exists.
Authors’ contributions
All authors, K.v.N., V.S. and C.S. contributed to the research design. All authors conceptualised and developed the initial draft, collected and analysed the data and interpreted the results. All authors critically reviewed, revised and approved the final draft.
Funding information
The research was funded by the research investigator. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
The data supporting the study’s findings are available from the corresponding author, K van Niekerk, upon reasonable request.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
Footnotes
Research Project Registration:
Project Number: M210637 MED21-06-021
How to cite this article: Van Niekerk K, Stancheva V, Smith C. Caregiver burden among caregivers of children with autism spectrum disorder. S Afr J Psychiat. 2023;29(0), a2079. https://doi.org/10.4102/sajpsychiatry.v29i0.2079
References
- 1.Pope K, Doll J, Kyvelidou A, et al. Clinician, caregiver and patient perspectives of the continuum of care for autism. J Interprof Educ Pract. 2020;9:100335. 10.1016/j.xjep.2020.100335 [DOI] [Google Scholar]
- 2.Freitag CM. Early signs and early intervention. Key Issues Ment Health. 2015;180:135–150. 10.1159/000363613 [DOI] [Google Scholar]
- 3.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 4.Rutter M. Aetiology of autism: Findings and questions. J Intellect Disabil Res. 2005;49(4):231–238. 10.1111/j.1365-2788.2005.00676.x [DOI] [PubMed] [Google Scholar]
- 5.Elsabbagh M, Divan G, Koh Y, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res. 2012;5(3):160–179. 10.1002/AUR.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franz L, Adewumi K, Chambers N, et al. Providing early detection and early intervention for autism spectrum disorder in South Africa: Stakeholder perspectives from the Western Cape province. J Child Adolesc Ment Health. 2018;30(3):149–165. 10.2989/17280583.2018.1525386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pillay S, Duncan M, De Vries PJ. Autism in the Western Cape province of South Africa: Rates, socio-demographics, disability and educational characteristics in one million school children. Autism. 2021;25(4):1076–1089. 10.1177/1362361320978042 [DOI] [PubMed] [Google Scholar]
- 8.Tuchman R, Rapin I. Epilepsy in autism. Lancet Neurol. 2002;1(6):352–358. 10.1016/S1474-4422(02)00160-6 [DOI] [PubMed] [Google Scholar]
- 9.Klukowski M, Wasilewska J, Lebensztejn D. Sleep and gastrointestinal disturbances in autism spectrum disorder in children. Dev Period Med. 2015;19:157–161. [PubMed] [Google Scholar]
- 10.Buie T, Fuchs GJ, Furuta GT, et al. Recommendations for evaluation and treatment of common gastrointestinal problems in children with ASD. Pediatrics. 2010;125(suppl. 1):S19–S29. 10.1542/PEDS.2009-1878D [DOI] [PubMed] [Google Scholar]
- 11.Jang J, Matson JL, Williams LW, et al. Rates of comorbid symptoms in children with ASD, ADHD, and comorbid ASD and ADHD. Res Dev Disabil. 2013;34(8):2369–2378. 10.1016/J.RIDD.2013.04.021 [DOI] [PubMed] [Google Scholar]
- 12.Stahlberg O, Nilsson T, Lundström S, et al. Autism spectrum disorders and coexisting mental health problems. Key Issues Ment Health. 2015;180:5–19. 10.1159/000363561 [DOI] [Google Scholar]
- 13.Fournier KA, Hass CJ, Naik SK, et al. Motor coordination in autism spectrum disorders: A synthesis and meta-analysis. J Autism Dev Disord. 2010;40:1227–1240. 10.1007/s10803-010-0981-3 [DOI] [PubMed] [Google Scholar]
- 14.Blatter S, Bliem HR, Juen BH, et al. We are empowering people with Autism. The effect of an integrated daily structure as well as improved communication on the lives of people with Autism. Open J Soc Sci. 2014;2(8):7–14. 10.4236/JSS.2014.28002 [DOI] [Google Scholar]
- 15.Van Steensel FJA, Bögels SM, Perrin S. Anxiety Disorders in children and adolescents with autistic spectrum disorders: A meta-analysis. Clin Child Fam Psychol Rev. 2011;14:302–317. 10.1007/s10567-011-0097-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matson JL, Williams LW. Depression and mood disorders among persons with autism spectrum disorders. Res Dev Disabil. 2014;35(9):2003–2007. 10.1016/J.RIDD.2014.04.020 [DOI] [PubMed] [Google Scholar]
- 17.Cohen D, Casanova MF, Frye RE, et al. Editorial: Comorbidity and autism spectrum disorder editorial on the research topic comorbidity and autism spectrum disorder. Front Psychiatry. 2020;11:617395. 10.3389/fpsyt.2020.617395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rossignol DA, Frye RE. Melatonin in autism spectrum disorders: A systematic review and meta-analysis. Dev Med Child Neurol. 2011;53(9):783–792. 10.1111/J.1469-8749.2011.03980.X [DOI] [PubMed] [Google Scholar]
- 19.Kuhaneck HM, Watling R. Occupational therapy: Meeting the needs of families of people with autism spectrum disorder. Am J Occup Ther. 2015;69(5):6905170010p1–6905170010p5. 10.5014/AJOT.2015.019562 [DOI] [PubMed] [Google Scholar]
- 20.Drockton M. Exploring autism and the caregiver burden relationship. Honors Research Projects [homepage on the Internet]. Akron: Williams Honors College; 2017. [cited n.d.]. Available from: https://ideaexchange.uakron.edu/honors_research_projects/505 [Google Scholar]
- 21.Pallanti S, Bencini L, Cantisani A, et al. Psychotropic treatment of Autism. Key Issues Ment Health. 2015;180:151–165. 10.1159/000363614 [DOI] [Google Scholar]
- 22.Kent EE, Rowland JH, Northouse L, et al. Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer. 2016;122(13):1987–1995. 10.1002/CNCR.29939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bruder MB. Family-centered early intervention: Clarifying our values for the new millennium. Topics Early Child Spec Educ 2016;20(2):105–115. 10.1177/027112140002000206 [DOI] [Google Scholar]
- 24.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20(6):649–655. 10.1093/GERONT/20.6.649 [DOI] [PubMed] [Google Scholar]
- 25.Hoffmann RL, Mitchell AM. Caregiver burden: Historical development. Nurs Forum (Auckl). 1998;33(4):5–12. 10.1111/J.1744-6198.1998.TB00223.X [DOI] [PubMed] [Google Scholar]
- 26.Angold A, Farmer EMZ, Costello EJ, et al. Perceived parental burden and service use for child and adolescent psychiatric disorders. Am J Public Health. 2011;88(1):75–80. 10.2105/AJPH.88.1.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sherman CW, Burgio LD, Kowalkowski JD. Assessment of dementia family caregivers. In: Lichtenberg PA, editor. Handbook of assessment in clinical gerontology. 2nd ed. Boston: Academic Press, 2008; p. 243–271. [Google Scholar]
- 28.Ten Hoopen LW, De Nijs PFA, Duvekot J, et al. Children with an autism spectrum disorder and their caregivers: Capturing health-related and care-related quality of life. J Autism Dev Disord 2020;50:263–277. 10.1007/s10803-019-04249-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mugno D, Ruta L, D’Arrigo VG, et al. Impairment of quality of life in parents of children and adolescents with pervasive developmental disorder. Health Qual Life Outcomes. 2007;5:1–9. 10.1186/1477-7525-5-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karst JS, Van Hecke AV. Parent and family impact of autism spectrum disorders: A review and proposed model for intervention evaluation. Clin Child Fam Psychol Rev. 2012;15:247–277. 10.1007/s10567-012-0119-6 [DOI] [PubMed] [Google Scholar]
- 31.Lai WW, Goh TJ, Oei TPS, et al. Coping and well-being in parents of children with autism spectrum disorders (ASD). J Autism Dev Disord. 2015;45:2582–2593. 10.1007/S10803-015-2430-9 [DOI] [PubMed] [Google Scholar]
- 32.Sharpley CF, Bitsika V, Efremidis B. Influence of gender, parental health, and perceived expertise of assistance upon stress, anxiety, and depression among parents of children with autism. J Intellect Dev Disabil 2009;22(1):19–28. 10.1080/13668259700033261 [DOI] [Google Scholar]
- 33.Paruk S, Ramdhial M. Prevalence of caregiver burden, depressive and anxiety symptoms in caregivers of children with psychiatric disorders in Durban, South Africa. S Afr J Psychiatry. 2018;24:9685. 10.4102/sajpsychiatry.v24i0.1314 [DOI] [Google Scholar]
- 34.Cohen SA, Cook S, Kelley L, et al. Psychosocial factors of caregiver burden in child caregivers: Results from the new national study of caregiving. Health Qual Life Outcomes. 2015;13:120. 10.1186/s12955-015-0317-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saini M, Stoddart KP, Gibson M, et al. Couple relationships among parents of children and adolescents with autism spectrum disorder: Findings from a scoping review of the literature. Res Autism Spectr Disord. 2015;17:142–157. 10.1016/J.RASD.2015.06.014 [DOI] [Google Scholar]
- 36.Hartley SL, Barker ET, Seltzer MM, et al. The relative risk and timing of divorce in families of children with an autism spectrum disorder. J Fam Psychol. 2010;24(4):449–457. 10.1037/A0019847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bédard M, William Molloy D, Squire L, et al. The Zarit Burden Interview: A new short version and screening version. Gerontologist. 2001;41(5):652–657. 10.1093/geront/41.5.652 [DOI] [PubMed] [Google Scholar]
- 38.Bianchi M, Flesch LD, Da Costa Alves EV, et al. Zarit Burden Interview psychometric indicators applied in older people caregivers of other elderly. Rev Lat Am Enfermagem. 2016;24:e2835. 10.1590/1518-8345.1379.2835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pandey S, Sharma C. Perceived burden in caregivers of children with autism spectrum disorder in Kathmandu Valley. J Nepal Health Res Counc. 2018;16(2):184–189. 10.3126/jnhrc.v16i2.20308 [DOI] [PubMed] [Google Scholar]
- 40.Kidman R, Thurman TR. Caregiver burden among adults caring for orphaned children in rural South Africa. Vulnerable Child Youth Stud. 2014;9(3):234. 10.1080/17450128.2013.871379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Seng BK, Luo N, Ng WY, et al. Validity and reliability of the Zarit Burden Interview in assessing caregiving burden. Ann Acad Med Singapore. 2010;39:758–763. 10.47102/annals-acadmedsg.V39N10p758 [DOI] [PubMed] [Google Scholar]
- 42.Gratão ACM, Brigola AG, Ottaviani AC, et al. Brief version of Zarit Burden Interview (ZBI) for burden assessment in older caregivers. Dementia e Neuropsychologia. 2019;13(1):122–129. 10.1590/1980-57642018DN13-010015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jones L, Totsika V, Hastings RP, et al. Gender differences when parenting children with autism spectrum disorders: A multilevel modeling approach. J Autism Dev Disord. 2013;43:2090–2098. 10.1007/s10803-012-1756-9 [DOI] [PubMed] [Google Scholar]
- 44.Frye L. Fathers’ experience with autism spectrum disorder: Nursing implications. J Pediatr Health Care 2016;30(5):453–463. 10.1016/J.PEDHC.2015.10.012 [DOI] [PubMed] [Google Scholar]
- 45.Schlebusch L, Dada S, Samuels AE. Family quality of life of South African families raising children with autism spectrum disorder. J Autism Dev Disord. 2017;47:1966–1977. 10.1007/s10803-017-3102-8 [DOI] [PubMed] [Google Scholar]
- 46.Families and parents are key to well-being of children [homepage on the Internet]. Statistics South Africa; n.d.. [cited 2023 Jan 19]. Available from: https://www.statssa.gov.za/?p=14388 [Google Scholar]
- 47.Pandya SP. Spirituality to build resilience in primary caregiver parents of children with autism spectrum disorders: A cross-country experiment. Int J Dev Disabil. 2018;64(1):53. 10.1080/20473869.2016.1222722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schoeman WJ. South African religious demography: The 2013 general household survey. HTS Teologiese Studies/Theological Studies 2017;73(2):a3837. 10.4102/HTS.V73I2.3837 [DOI] [Google Scholar]
- 49.Fithriyah I, Carrasco ME. Caregiver burden and psychosocial factors in mothers with autism spectrum disorder children. Biomol Health Sci J. 2021;4(2):103. 10.20473/BHSJ.V4I2.28875 [DOI] [Google Scholar]
- 50.Green SE. “We’re tired, not sad”: Benefits and burdens of mothering a child with a disability. Soc Sci Med. 2007;64(1):150–163. 10.1016/J.SOCSCIMED.2006.08.025 [DOI] [PubMed] [Google Scholar]
- 51.South Africa – Unemployment rate 2021 [homepage on the Internet]. Statista; n.d.. [cited 2023 Jan 19]. Available from: https://www.statista.com/statistics/370516/unemployment-rate-in-south-africa/ [Google Scholar]
- 52.Geldenhuys A. The financial and psychological cost of raising a child with Autism Spectrum Disorder: A qualitative study [homepage on the Internet]. Durban: The University of KwaZulu-Natal ResearchSpace; 2019. [cited n.d.]. Available from: https://researchspace.ukzn.ac.za/handle/10413/21232 [Google Scholar]
- 53.Fewster DL, Uys C, Govender P. Interventions for primary caregivers of children with autism spectrum disorder: a cross-sectional study of current practices of stakeholders in South Africa. S Afr J Occup Ther. 2020;50:41–48. 10.17159/2310-3833/2020/VOL50NO1A7 [DOI] [Google Scholar]
- 54.Kuhlthau K, Payakachat N, Delahaye J, et al. Quality of life for parents of children with autism spectrum disorders. Res Autism Spectr Disord 2014;8:1339–50. 10.1016/J.RASD.2014.07.002 [DOI] [Google Scholar]
- 55.Masefield SC, Prady SL, Sheldon TA, et al. The caregiver health effects of caring for young children with developmental disabilities: A Meta-analysis. Matern Child Health J 2020;24:561–74. 10.1007/s10995-020-02896-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bradshaw J, Gillespie S, McCracken C, et al. Predictors of caregiver strain for parents of children with Autism Spectrum Disorder. J Autism Dev Disord 2021;51(1):3039–3049. 10.1007/s10803-020-04625-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Phetrasuwan S, Shandor Miles M. Parenting stress in mothers of children with autism spectrum disorders. J Specialists Pediatr Nurs. 2009;14(3):157–165. 10.1111/J.1744-6155.2009.00188.X [DOI] [PubMed] [Google Scholar]
- 58.Mumtaz N, Fatima T, Saqulain G. Perception of burden and stress among mothers of autistic children in Pakistani cultural background. Iran Rehabil J. 2022;20(1):43–52. 10.32598/IRJ.20.1.1335.5 [DOI] [Google Scholar]
- 59.Maciej Serda, Becker FG, Cleary M, et al. Assessing caregiver burden and its correlation to quality of life of mother with autism spectrum disorder in Surabaya Indonesia. Uniwersytet Śląski. 2020;7:3367–3373. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the study’s findings are available from the corresponding author, K van Niekerk, upon reasonable request.