Abstract
Background:
World Health Organization has communicated that dementia as a public health priority in 2012. Behavioral and psychological symptoms of dementia are the main reason results in hospitalization of dementia patients. Horticulture is one of the favorite activity for many peoples to relax their minds.
Objectives:
To investigate psychological health benefits of horticulture intervention in dementia patients.
Methods:
The databases including Cochrane Library, ProQuest, PubMed, EMBASE, EBSCO, Web of Science, and Ovid Medline were searched up to August 2017.
Results:
Twenty-three articles for systematic review, whereas 8 articles were included in meta-analysis. Meta-analysis verified the beneficial effect of horticultural therapy (HT) on agitation level (standard mean difference: −0.59; P < .00001); increase time spent on activity engagement (mean differences [MD]: 45.10%, P < .00001); decrease time for doing nothing (MD: −29.36%, P = .02).
Conclusions:
Patients with dementia benefit from horticultural by alleviating their degrees of agitate behaviors, increasing time of engaging in activities and decrease time of doing nothing.
Keywords: BPSD, long-term care, psychological health, agitation, Cohen-Mansfield, agitation inventory, horticulture
Background
With the rapid aging of the world population, the impending dementia epidemic has triggered health policy responses. Dementia, a neurodegenerative disorder, is characterized by an inexorably progressive cognitive deterioration that diminishes self-care ability. However, the cognitive and daily functional impairments are not the main reasons for hospitalization. Behavioral and psychological symptoms of dementia (BPSD) are closely associated with adverse clinical outcomes in patients. 1 The associated psychiatric symptoms include hallucinations, delusions, restless behavior, and repetitious questioning, 2 which seriously reduce the quality of life of patients with dementia and of their families, resulting in a large burden of care.
In 2012, the World Health Organization designated dementia as a public health priority. 3 Current estimates of almost 60 million people globally who are living with dementia might double by 2030 and triple by 2050. 4 In 2015, the global economic burden of dementia was US$818 billion. 5 Levels of cognition and social impairment tend to vary widely and complicate the implementation of a standard care program for patients with dementia. 6,7 These factors make caregiving more difficult.
Abundant evidence demonstrates that nonpharmacological therapies (eg, music, reminiscence, and horticultural therapy [HT]) for BPSD are desirable because they may alleviate, without side effects, neuropsychiatric symptoms, such as agitation, physical aggression, and disruptive behavior. 8,9 However, because the benefits of reminiscence and music therapies are closely associated with patients’ past memories and experiences, plans sensitive to differences among patients with dementia warrant further study. In contrast to reminiscence and music therapies, HT is widely accepted for most patients with dementia because it invites them to watch, touch, and become close to the natural world. In addition, HT can be incorporated into the daily activities schedules of any care institute and easily woven into the living environments of patients to improve their emotional well-being. 10
The assimilation of HT into the daily lives of patients has been extremely effective at reducing agitated behavior, stabilizing emotions, and increasing social interaction among people with dementia. 11 Horticultural therapy can not only provide multisensory stimulation but also impart a sense of responsibility and achievement in patients with dementia. 11,12 Floriculture or garden clubs have become meaningful activities that provide beneficial opportunities to patients to care for fresh flowers and plants with their own hands. Engagement in physical activity while appreciating the floriculture and revival of plants provides an incentive for patients to join related courses and interact psychosocially with caregivers. 13
This systematic review and meta-analysis focused on various forms of garden activities, green care farms, green spaces, and therapeutic horticulture in facilities for long-term and dementia care to clarify how these activities affect the agitated behavior, cognitive functioning, activity engagement time, and inactivity status of patients with dementia.
Methods
Data Sources and Search Strategy
The methodology used here is in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. 14 In August 2017, the PubMed, ProQuest, Cochrane Library, Embase, Ovid MEDLINE, and Web of Science databases were systematically searched using the following keywords:” “horticul*,” “garden*,” “floricult*,” “arboricult*,” “olericult*,” “agricult*,” and “farm*” combined with “dement*,” “alzheimer*,” and “cogni*” (Supplemental File 1). The scope of the searches was constrained by the number of peer-reviewed publications in English language. Relevant reference lists for other potentially eligible studies (using a snowball procedure) were also included in this study (Supplemental File 2). All sources that were searched were later imported into EndNote X8, and the key information was extracted from the searched studies screened and reviewed by 2 authors to determine whether they were eligible for inclusion in this study (Supplemental File 3).
Inclusion and Exclusion Criteria
We included studies that (1) were randomized clinical trial (RCTs) or a prospective, retrospective, or longitudinal studies; (2) included participants were older adults with dementia or Alzheimer disease; (3) implemented interventions of interest (ie, gardening activities, a horticulture activity program, or the viewing of natural scenery through video); (4) measured agitation level, cognitive functioning, time spent engaged in an activity, and inactivity status as outcomes; and (5) were written in English. By contrast, reviews, letters to the editor, case reports, and case series were excluded.
Data Extraction and Quality Assessment
Title and abstract screening and data extraction (demographic data, designs, methods, procedures, intervention contents, and individual study effects) of the included studies were performed by 5 reviewers. In particular, the collected data pertained to methodology, gardening activity–related interventions, follow-up duration, and measurement of outcomes (eg, BPSD, cognitive functioning, inactivity status, and the time spent engaged in activity) were extracted. Behavioral and psychological symptoms of dementia measurements included those on agitation, aggression, delirium, screaming, wandering, and many noncognitive symptoms and behaviors of patients with dementia. The Cohen-Mansfield Agitation Inventory (CMAI), used here to assess agitation levels, measures 29 aggressive behaviors in patients with cognitive impairment and focuses only on agitated behaviors, such as inappropriate verbal, vocal, or motor activity.
Three review authors independently assessed the design of each study using the Joanna Briggs Institute (JBI) tool 15 to assess the methodological quality of the studies and determine the extent to which a study has addressed the possibility of bias in its design, conduct, and analysis.
Articles appraisals were assessed by grading their designs (namely RCT, cross-sectional, quasi-experimental, and cohort based) into 1 of 4 categories: 0 points, 1 point, unclear, and not applicable. 16 A study was considered high quality when it met more than half of the total score. Any disagreement in study selection was resolved through intensive discussion among reviewers.
Statistical Analysis
The control and experimental groups were designated to comprise those who received usual care and HT, respectively. Mean differences (MDs), standard mean differences (SMDs), and the corresponding 95% confidence intervals (CIs) were estimated. In this meta-analysis, the inverse variance was the weighting method used in both the fixed- and random-effects models, with the particularity that under the random-effects model, the heterogeneity variance was estimated using the DerSimonian and Laird method. 17 Finally, pooled-effect estimates were calculated.
The heterogeneity of the intervention effects between studies was assessed through the I 2 and Cochran Q tests; significance was set at I 2 > 50%, which indicated substantial heterogeneity. In cases of significant between-study heterogeneity, a random-effects model (DerSimonian and Laird method) was used. 18 Publication bias was examined using funnel plots, Begg test, and Egger regression asymmetry test. 19 Funnel plots (plots of effect estimates vs sample sizes) are useful to assess the validity of meta-analyses. The presence and absence of a symmetrical inverted funnel in the plot indicates the absence and presence of bias, respectively. If bias is absent, the plot resembles a symmetrical inverted funnel, and an asymmetrical one if bias is present. Begg test evaluates the correlation between the ranks of effect sizes. Egger regression of funnel plot asymmetry formally determines the association between estimated intervention effects and a measure of study size.
All statistical analyses were performed using Comprehensive Meta-Analysis (version 2.0; Biostat, Englewood, New Jersey) and RevMan (version 5.3; Cochrane’s Informatics & Knowledge Management Department, Copenhagen, Denmark: The Nordic Cochrane Centre).
Results
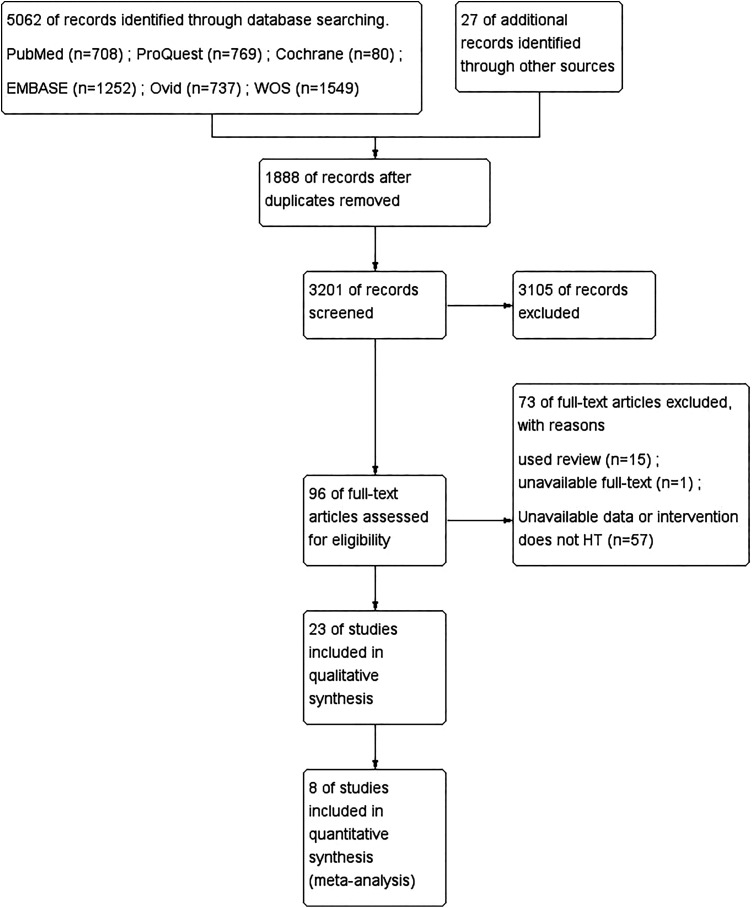
The study selection process flow is presented in Figure 1. The electronic database search retrieved 5062 records and 27 additional snowball records; 1888 were excluded for duplication, 3015 were irrelevant according to their title and abstract, and 69 were irrelevant according to the text; therefore, 23 full texts 9 -12,20 -38 were retrieved for review, and 8 of these were included in the meta-analysis.
Figure 1.
Flowchart of the study selection process. Electronic searches yielded 5062 records and 27 additional snowball records. Of those texts, 96 full texts were retrieved for closer examination. Twenty-three articles were included in the final review and 8 studies were included in the meta-analysis.
Study Characteristics and Quality
Twenty-three studies recruited elderly people with dementia. Eighteen studies were from Western countries: 9 from the United States, 2 from Canada, 2 from the United Kingdom, 2 from the Netherlands, 1 from Sweden, and 2 from Australia. Five studies were from East Asian countries: 1 from Japan, 3 from South Korea, and 1 from Taiwan. These studies varied in design and included 2 RCTs and 3 cohort studies, in addition to observational studies (that had pretests, midtests, or posttests) and comparative studies. Of the 23 studies, 8 and 14 studies had high and moderate JBI qualities, respectively, whereas 1 had a low JBI quality (Table 1).
Table 1.
Study Characteristics of Horticulture Interventions.a
| Author (Publication Year; Country) | Characteristic (Facility, Patients, Age) | Study Design | Duration of Follow-up | Intervention | Participants | Outcomes | Quality |
|---|---|---|---|---|---|---|---|
| Monney and Nicell (1992; Canada) | Special care units Alzheimer’s disease Mean age 83 |
Comparative, observational study | 4 month | Exterior space Garden |
25-31 | Violence (%): ↓, All incidents (%): ↓ | low |
| Mather et al (1997; Canada) | Care center Alzheimer’s disease Mean age 83 |
Comparative, observational study with pretest, midtest, posttest | 6 month | Walled garden | 10 | Disruptive behavior (%): NS | High |
| Jarrott et al (2002; United States) | Not clear Dementia Mean age 79 |
Comparative, observational study | 10-week | HT activities—3 time each week over a 10-week period. Activities lasted 30 to 45 min per session. |
9 | Time engagement (%): ↑, Doing nothing (%): ↓ | High |
| Cox et al (2004; Australia) | Care center (Rice Village) Alzheimer’s disease Mean age non |
pretest, posttest design | non | Multisensory Environments Living room Garden Snoezelen room |
24 | Snoezelen room was calming and appeared to be relaxing | High |
| Gigliotti et al (2004; United States) | Care institutional Dementia Mean age 83 |
Comparative study with pretest, posttest | 9-week | HT activities in 30 minutes, 3 times per week over 9 weeks in groups both indoors and outdoors three types of HT activities: cooking, crafts, and planting |
14 | Time engagement (%): NS, Doing nothing (%): ↓, Affect was more positive during HT than traditional activities. |
Medium |
| Gigliotti and Jarrott (2005; United States) | Veterus administration Dementia Mean age 80 |
Comparative study with pretest, posttest | 9-week | HT activities were facilitated half an hour per week over 9 weeks in addition to ordinary ADS activities | 48 | Time engagement (%): ↑, Doing nothing (%): ↓ Affect was more positive during HT than traditional activities. |
Medium |
| Detweiler et al (2008; United States) | Dementia facility Dementia Mean age 80.7 |
pretest, posttest design | 1 year | Open wander garden with free and direct access from the dementia unit | 34 | CMAI score: ↓, PRNs medications: ↓ Staff and family members felt that intervention improved mood and quality of life of the dementia residents. |
Medium |
| Lee and Kim (2008; Korea) | Nursing home Mild or severe dementia patients Mean age not clear |
pretest, posttest design (3 times measured) | 5-week | Indoor garden activities (4 weeks): dropwort and bean sprout | 23 | Sleep patterns: WASO: ↓, nap: ↓, TST: NS, NST: ↑ and NSE: ↑ CMAI scores: ↓, Cognition (HDS-R): ↑ |
Medium |
| Park et al (2008; Japan) | S-group home dementia patients Mean age 81.3 |
pretest, posttest design (3 times measured) | 8 or 9-month (Unclear) |
Horticulture activity program mixed individual activity and group activity was offered for a total of 20 sessions | 16 | ADL: ↑, Desire to participate: ↑, Facial expression: ↑, Cooperation levels: ↑ | Medium |
|
Thelander et al (2008; Sweden) |
Nursing home Moderate to serious dementia patients Mean age 86.8 |
pretest, posttest design | 6-week | The activities used were gardening activities (ie watering, weeding, raking, and planting), walks, and social activities. Every intervention session lasted between 40 and 70 min. | 8 | Cognitive capacity (MMSE): NS | Medium |
| Detweiler et al (2009; United States) | Dementia unit Dementia Mean age 80.5 |
Comparative study with pretest, posttest | 1 year | Open wander garden | 28 | The mean monthly fall severity score declined. The most significant changes in scheduled psychiatric medications were reductions in scheduled antipsychotics and an increase in residents requiring no antipsychotics. |
Medium |
| Jarrott and Gigliotti (2010; United States) | 5 Nursing home & 3 ADS Dementia Mean age 80.09 |
Comparative study with a cluster randomization | 6-week | Horticultural therapy-based programming was implemented twice weekly at 4 treatment sites for 6 weeks | 75 in HT group | Measure of engagement: Active (AE), Passive (PE), Self (SE), Other (OE) were found significant difference in 4 of the 5 engagement categories. Only Non (NE) was not. Apparent Affect Rating Scale (AARS): 3 affective coding categories, including pleasure: NS, anxiety: NS, interest: NS. |
high |
| 54 in TA group | |||||||
| Kang et al (2010; South Korea) | Senior welfare center Mild dementia Age range 65-79 |
quasi-experimental | 9-week | art and horticultural therapies in this intervention 3-hour sessions twice per week for 9 weeks | 20 in the experimental group | Significant differences were found post intervention between the 2 groups including, Cognition function (MMSE): ↑, Depression (GDS): ↓, Mental-emotional health: ↑ | high |
| 18 in control group | |||||||
| Murphy et al (2010; United States) | Dementia facility Dementia Mean age 80.71 |
pretest, posttest design | 1 year | Open wander garden | 34 | Agitation levels (CMAI): ↓, wander garden visits by month: ↑ | Medium |
| de Brunin et al (2012; Netherland) | Day care Dementia Mean age 77.7; 83.4 |
Observational cohort study | 6 month 1 year |
Green care farms (GCFs) | 47 | Medication use: NS, ADL: NS, IADL: NS | Medium |
| Regular day care facilities (RDCFs) | 41 | ||||||
| Edwards et al (2013; Australian) | Dementia-specific unit Alzheimer’s disease Age range: 79–90 |
pretest, posttest design | 3 month | Garden | 10 | QoI: ↑, CMAI: ↓, Depression (CSDD): ↓ | Medium |
| Hewitt et al (2013; UK) | Hospital Alzheimer’s disease Mean age 58.6 |
pretest, posttest design | 1 year | Structured Gardening program | 12 | QoI: ↑, Cognition function (MMSE): NS | Medium |
| Goto et al (2014; United States) | Nursing home Alzheimer’s disease Mean age 88 |
prospective | 1-month | A multimedia room and an interior garden | 18 | Behavioral assessment Assessment of pulse rate |
Medium |
| Chung et al (2016; United States) | Long-term nursing facility Dementia Mean age 61; 83 |
Qualitative study | 6 week | Media presentation on natural scenes | 23 | Agitation related of Behavior: NS | high |
| Hall et al (2016; UK) | Long-term care home Dementia Mean age 84.8 (range: 61-96) |
Mixed methods | 10 week | Horticultural activities | 14 | Well-being Neutral Ill-being |
Medium |
| Kim et al (2016; Korea) | Seongdong-gu center Alzheimer’s disease Mean age 78.48 |
Randomized control study | 6 month | Multidomain cognitive stimulation | 32 | Cognition function (MMSE): ↑, Qol: NS, Depression (GDS): ↓ | Medium |
| control | 21 | ||||||
| de Boer et al (2017; Netherland) | Nursing homes Dementia unclear |
Longitudinal observation study | 6 month | Green care farms | 5 | activate: ↑, social interaction: ↑ (compare with traditional nursing homes) | high |
| Traditional nursing homes | 4 | ||||||
| Regular small-scale living facilities | 9 | ||||||
| de Boer et al (2017; Netherland) | Nursing homes Dementia Mean age 83.8 |
Cross-sectional design | non | Green care farms | 34 | Qol: ↑, NPI: NS, CMAI: NS, Depression (CSDD): NS, (compare with traditional nursing homes) | high |
| Traditional nursing homes | 29 | ||||||
| Regular small-scale living facilities | 52 | ||||||
| Hsu et al (2017; Taiwan) | Veteran Home Dementia Mean age 86.4 |
Retrospective pretest, posttest design |
6 month | Multiple intervention | 141 | Cognition function (MMSE): NS, Depression (CSDD): ↓, ADL: ↑, IADL: NS, NPI: ↓, CMAI: ↓, NPI caregiver’s burden: ↓, | high |
Abbreviations: ADL, activities of daily living; ADS, adult day service; BMI, body mass index; CMAI, Cohen-Mansfield Agitation Inventory; HDS, Hasegawa Dementia Scale; HT, horticulture therapy; MMSE, Mini-Mental State Examination; NPI, neuropsychiatric inventory; NS, nonsignificant; NST, Nocturnal sleep; NSE, Nocturnal sleep efficacy; PRN, pro re nata; TA; traditional activities;TST, total sleep time; WASO, wake up after sleep onset.
a Dementia-related behavior disturbance was assessed with the Cohen-Mansfield Agitation Inventory (CMAI).
Eight studies met the inclusion criteria for meta-analysis, and 552 participants were recruited across all studies. Studies emphasized on the behavioral categories of agitation and engagement. Of the interventions, 2 studies had audiovisual presentations of natural scenes, 1 had a structured gardening program, 5 had combinations of gardening with other activities, and 17 had only garden activities.
Effect of HT on Behavior
Patients with dementia who received HT interventions had significantly lower levels of agitation than those who did not. Behavioral issues were assessed by 5 studies, with 237 participants in the post-HT intervention and 233 in the control groups. The pooled results of CMAI scores were significantly lower after HT intervention with an SMD of −0.59 (95% CI: −0.77 to −0.40, P < .00001, I 2 = 0%; Figure 2) indicating that patients who joined HT programs experienced decreased BPSD.
Figure 2.
Forest plot of CMAI scores (A) and subgroup of CMAI scores (B). CMAI scores were significantly lower after HT intervention (A); no significant differences were observed between the Western and East Asian subgroups (B). CMAI indicates Cohen-Mansfield Agitation Inventory; HT, horticultural therapy.
Patients in the subgroup meta-analysis were further divided by whether they were from a Western or East Asian country. The subgroup meta-analysis indicated that HT reduced their CMAI scores, but no difference was observed between the patients of the 2 country subgroups who received HT, with an SMD of −0.63 (95% CI: −0.97 to −0.29, P < .00001) versus −0.57 (95% CI: −0.79 to −0.35, P < .00001). However, no heterogeneity was observed in both the Western (I 2 = 0%) and East Asian subgroups (I 2 = 0%). Subgroup difference results also demonstrated no heterogeneity (I 2 = 0%). This subgroup meta-analysis demonstrated that the patients who received HT interventions had increased behavioral and psychological stability.
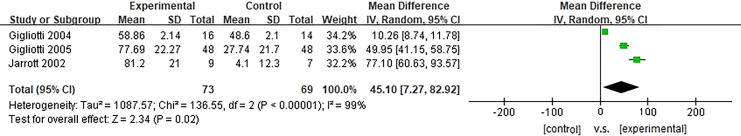
Effect of HT on Activity Engagement
Patients with dementia who received HT interventions spent significantly more time engaged in activity. Three studies investigated the effects of HT on enhanced engagement in activity; 73 and 69 participants were in the experiment and control groups, respectively. The pooled results revealed that activity engagement time in the HT group was much greater than that in the control group, with an MD of 45.10% during HT (95% CI: 7.27-82.92, P = .02, I 2 = 99%; Figure 3).
Figure 3.
Forest plot of time spent engaged in activity. Patients with dementia who received HT interventions spent significantly more time engaged in activity. HT indicates horticultural therapy.
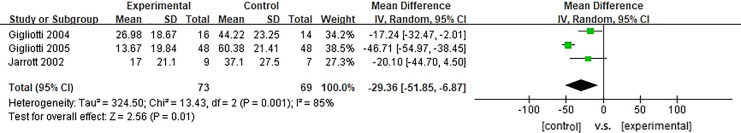
Effect of HT on Inactivity Status
Based on the assessments of 3 studies with 73 and 69 participants in the experimental and control groups, respectively, HT interventions had significant effects on the inactivity status of patients. The pooled results revealed that patient inactivity status was significantly lower in the control group, with an MD of −29.36% during HT (95% CI: −51.85 to −6.87, P = .01; Figure 4). All results indicated that some inherent heterogeneity in these studies (I 2 = 85%).
Figure 4.
Forest plot of inactive status. HT intervention had significant effects on the inactivity status of patients. HT indicates horticultural therapy.
Publication Bias
First, funnel plots, Begg test, and Egger test were employed to evaluate the publication bias in the agitation meta-analysis. Egger test indicated the presence of bias (P = .09), whereas Begg test indicated no substantial publication bias (P = .014). Second, for the activity engagement outcome, Egger test and Begg test revealed no publication bias (P = .19 and .60, respectively). Finally, the inactivity status outcome also demonstrated no publication bias (Egger test: P = .31, Begg test: P = .60). The funnel plots of the results are presented in Supplementary Figures.
Discussion
Studies on HT interventions have reported that HT reduced accident frequency, alleviated agitation levels, and improved well-being, among other positive effects associated with HT. 8,22,33 Kamioka et al suggested that HT was an effective treatment for psychological and behavioral disorders. 39 However, further confirmation of the effects of HT on BPSD is required. Through meta-analysis, this study combined published results to evaluate the effectiveness of HT in patient behavior and activity engagement.
For patients with dementia, a critical aspect is not only “what they need” but “what they want”; Mapes et al observed that 82.2% of patients with dementia agreed that being in a natural environment, such as with flowers, trees, leaves, and other plants, helped them relax, feel joyful, and relieve emotional tension. 22,23,40,41 The results of the current study demonstrated that HT interventions reduced CMAI scores. Horticultural therapy is related to a general scene or outdoor activity that provides a connection to the past experiences of the patients and arouses their interest in life. 10,26,36 Dementia symptoms, such as memory loss, lack of attention, and impaired visual perception, might cause patients with dementia to be psychologically stressed and experience confusion, anxiety, or anger. Emotional stability and social interaction are critical factors that better the lives of patients with dementia.
A study has found that unfamiliar environments cause anxiety. 42 Cohen-Mansfield reported that nursing home residents exhibited inappropriate behavior, possibly because they experienced sensory deprivation, boredom, and loneliness. 43 Therefore, providing a welcoming environment to patients with dementia and their caregivers is a major aspect of their care. Because caregiver burden is significantly associated with BPSD severity in patients, 44 the alleviation of BPSD is a pressing concern that not only mitigates undesirable behavior but also improves patients’ quality of life. 7 Notably, personalized improvements in care quality is key to stabilizing patient conditions. This study indicated that HT activities alleviate negative emotions in patients with dementia, which not only alleviate the difficulties faced by patients and their caregivers but also increase their quality of life.
However, some patients with dementia with comorbid affective disorders or unpredictable behavioral disturbances 7 tend to engage in fewer or no activities. Stabilizing patient emotions and encouraging their involvement in activities is a main challenge. The pooled results of this study revealed that HT can entice patients to spend more time active. Hartig et al reported that patients benefit from multiple forms of contact with nature in the form of decreased stress and increased physical and social engagement. 45 Furthermore, nature is an excellent resting environment that focuses attention and produces a restorative effect. 46 Dahlkvist et al suggested a significantly positive relationship between garden visits and self-perceived health. 47 Furthermore, participation in activities is considered a crucial component of some therapeutic programs. According to Park et al, HT provides forms of activity that improve the physical and cognitive functions of patients and enable interpersonal communication and social interaction. 26
The results of this systematic review revealed that 4 studies focused on adapting HT interventions to improve cognitive function. Horticultural therapy includes sensory stimulation, which may spark memories and arouse reminiscence. However, with regard to improvements in cognitive function and depressive symptoms, HT may not have a significant effect on reminiscence therapy. The meta-analysis results pooled from the literature revealed no conclusive evidence that HT results in significant improvements in patients’ cognitive function. However, in some groups, HT may help patients recall memories, such as their experiences at work or in life. The effect of HT on these group of patients may be similar to that of reminiscence therapy. However, with regard to cognitive improvements, the combined effects of HT and reminiscence therapy warrant further investigation.
Horticultural therapy is not only suitable for patients with dementia but also popular in the general population. Most studies have focused on the building of specialized gardens or green places for patients with dementia. These sites, in addition to their original function, can serve as sightseeing attractions for the general public as well as patients with autism or other psychological illnesses. Patients with dementia can interact with visitors and participate in the design, creation, monitoring, and maintenance of the gardens. Ample evidence indicates that social activities help patients with dementia maintain their cognitive function. Tending to a garden can not only help patients with dementia increase their social network but also enhance their creativity, self-esteem, and sense of ownership. Horticultural therapy can provide other benefits to patients with dementia.
Conclusions
The results of this meta-analysis indicated the effects of sensory gardens and HT programs on improvements in agitation levels and the time spent in activity and inactivity. Furthermore, HT is a widely accepted method that can contribute to the enrichment and emotional stability of patients with dementia. From this perspective, HT is a suitable, stimulating, and productive activity for dementia care programs. All studies in the systematic review that used HT in caring for patients with dementia had a decreased score on the CMAI; these results can encourage administrators in care facilities to use HT to care for patients with dementia.
Study Limitations
The study had several limitations. First, no relevant RCTs could be extracted. However, to provide more credible evidence, this study summarized the existing published data. Second, across most articles, the definition of HT is unclear and inconsistent. For instance, HT might be considered to involve only activities related to nature scenes. Moreover, therapeutic landscape studies on garden activities, green care farms, green spaces, and topics on therapeutic horticulture were not covered in this meta-analysis. Third, heterogeneity is across the studies in this meta-analysis was unavoidable because of subjective differences between the participants, executors, and people involved with the institutions and intervention programs. Finally, the currently available cognitive function data were insufficient for a complete meta-analysis. Although 7 studies could be used with regard to cognitive function,1, 9,10,25,28,33,37 only 2 reported on Mini-Mental State Examination data that could be used in the meta-analysis. Further investigation is required to corroborate the credibility of the currently-scant results on the effects of cognitive function in HT.
Despite these limitations, the current meta-analysis presents promising benefits of HT in patients with dementia. More rigorously designed studies, such as RCTs or cluster RCTs, are required to confirm the effects of HT in patients with dementia.
Supplemental Material
Supplemental Material, Suppl._1_Search_strategies for Horticultural Therapy in Patients With Dementia: A Systematic Review and Meta-Analysis by Li-Chin Lu, Shao-Huan Lan, Yen-Ping Hsieh, Yea-Yin Yen, Jong-Chen Chen and Shou-Jen Lan in American Journal of Alzheimer's Disease & Other Dementias
Supplemental Material, Suppl._2_Search_strategy_Table for Horticultural Therapy in Patients With Dementia: A Systematic Review and Meta-Analysis by Li-Chin Lu, Shao-Huan Lan, Yen-Ping Hsieh, Yea-Yin Yen, Jong-Chen Chen and Shou-Jen Lan in American Journal of Alzheimer's Disease & Other Dementias
Supplemental Material, Suppl._3_Funnel_plot_of_CMAI for Horticultural Therapy in Patients With Dementia: A Systematic Review and Meta-Analysis by Li-Chin Lu, Shao-Huan Lan, Yen-Ping Hsieh, Yea-Yin Yen, Jong-Chen Chen and Shou-Jen Lan in American Journal of Alzheimer's Disease & Other Dementias
Acknowledgments
This manuscript was edited by Wallace Academic Editing.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Shou-Jen Lan  https://orcid.org/0000-0002-8395-2052
https://orcid.org/0000-0002-8395-2052
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Fabrigoule C, Letenneur L, Dartigues JF, Zarrouk M, Commenges D, Barberger-Gateau P. Social and leisure activities and risk of dementia: a prospective longitudinal study. J Am Geriatr Soc. 1995;43(5):485–490. [DOI] [PubMed] [Google Scholar]
- 2. Prince M, Guerchet M, Prina M. The Epidemiology and Impact of Dementia—Current State and Future Trends. WHO Thematic Briefing. WHO; 2015. https://www.who.int/mental_health/neurology/dementia/dementia_thematicbrief_epidemiology.pdf [Google Scholar]
- 3. World Health Organization and Alzheimer’s Disease International. Dementia: A Public Health Priority. World Health Organization and Alzheimer’s Disease International. 2012. https://www.who.int/mental_health/publications/dementia_report_2012/en/ [Google Scholar]
- 4. World Alzheimer’s Report 2009. London, Alzheimer’s Disease International; 2009. [Google Scholar]
- 5. Wimo A, Guerchet M, Ali GC, et al. The worldwide costs of dementia 2015 and comparisons with 2010. Alzheimers Dement. 2017;13(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Morgan DG, Stewart NJ. The Importance of the social environment in dementia care. West J Nurs Res. 1997;19:740–761. [Google Scholar]
- 7. Woodhead EL, Zarit SH, Braungart ER, Rovine MR, Femia EE. Behavioral and psychological symptoms of dementia: the effects of physical activity at adult day service centers. Am J Alzheimers Dis Other Demen. 2005;20(3):171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gonzalez MT, Kirkevold M. Benefits of sensory garden and horticultural activities in dementia care: a modified scoping review. J Clin Nurs. 2014;23(19-20):2698–2715. [DOI] [PubMed] [Google Scholar]
- 9. Hsu TJ, Tsai HT, Hwang AC, Chen LY, Chen LK. Predictors of non-pharmacological intervention effect on cognitive function and behavioral and psychological symptoms of older people with dementia. Geriatr Gerontol Int. 2017;17(suppl 1):28–35. [DOI] [PubMed] [Google Scholar]
- 10. Kang HY, Bae YS, Kim EH, Lee KS, Chae MJ, Ju RA. An integrated dementia intervention for Korean older adults. J Psychosoc Nurs Ment Health Serv. 2010;48(12):42–50. [DOI] [PubMed] [Google Scholar]
- 11. Gigliotti CM, Jarrott SE. Effects of horticulture therapy on engagement and affect. CJA/RCV. 2005;24(4):367–77. [Google Scholar]
- 12. Jarrott SE, Kwack HR, Relf D. An observational assessment of a dementia-specific horticultural therapy program. Horttechnology. 2002;12(3):403–410. [Google Scholar]
- 13. McGuire DL. Implementing horticultural therapy into a geriatric long-term care facility. Activ Adapt Aging. 1997;22(1-2):61–80. [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269, W64. [DOI] [PubMed] [Google Scholar]
- 15. Peters M, Godfrey C, McInerney P, Soares C, Hanan K, Parker D. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology For JBI Scoping Reviews. Adelaide, SA Australia: The Joanna Briggs Institute; 2015. [Google Scholar]
- 16. Adams V, Mathisen B, Baines S, Lazarus C, Callister R. A systematic review and meta-analysis of measurements of tongue and hand strength and endurance using the Iowa Oral Performance Instrument (IOPI). Dysphagia. 2013;28(3):350–369. [DOI] [PubMed] [Google Scholar]
- 17. DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28(2):105–114. [DOI] [PubMed] [Google Scholar]
- 18. Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 19. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mooney P, Nicell PL. The importance of exterior environment for Alzheimer residents: effective care and risk management. Healthc Manage Forum. 1992;5(2):23–29. [DOI] [PubMed] [Google Scholar]
- 21. Mather JA, Nemecek D, Oliver K. The effect of a walled garden on behavior of individuals with Alzheimer’s. Am J Alzheimers Dis. 1997;12(6):252–257. [Google Scholar]
- 22. Cox H, Burns I, Savage S. Multisensory environments for leisure: promoting well-being in nursing home residents with dementia. J Gerontol Nurs. 2004;30(2):37–45. [DOI] [PubMed] [Google Scholar]
- 23. Gigliotti CM, Jarrott SE, Yorgason J. Harvesting health: effects of three types of horticultural therapy activities for persons with dementia. Dementia. 2004;3(2):161–180. [Google Scholar]
- 24. Detweiler MB, Murphy PF, Myers LC, Kim KY. Does a wander garden influence inappropriate behaviors in dementia residents. Am J Alzheimers Dis Other Demen. 2008;23(1):31–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lee Y, Kim S. Effects of indoor gardening on sleep, agitation, and cognition in dementia patients—A pilot study. Int J Geriatr Psychiatry. 2008;23(5):485–489. [DOI] [PubMed] [Google Scholar]
- 26. Park SY, Yamane K, Yamaki Y, Takahashi S. Effects of horticulture activities on activities of daily living to participation and cooperation in cases of dementia. Acta Hortic. 2008;775(775):41–46. [Google Scholar]
- 27. Detweiler MB, Murphy PF, Kim KY, Myers LC, Ashai A. Scheduled medications and falls in dementia patients utilizing a wander garden. Am J Alzheimers Dis Other Demen. 2009;24(4):322–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thelander VB, Wahlin T-BR, Olofsson L, Heikkilä K, Sonde L. Gardening activities for nursing home residents with dementia. Adv Physiother. 2009;10(1):53–56. [Google Scholar]
- 29. Ford Murphy P, Miyazaki Y, Detweiler MB, Kim KY. Longitudinal analysis of differential effects on agitation of a therapeutic wander garden for dementia patients based on ambulation ability. Dementia. 2010;9(3):355–373. [Google Scholar]
- 30. Jarrott SE, Gigliotti CM. Comparing responses to horticultural-based and traditional activities in dementia care programs. Am J Alzheimers Dis Other Demen. 2010;25(8):657–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. de Bruin S, Oosting S, Tobi H, Enders-Slegers MJ, van der Zijpp A, Schols J. Comparing day care at green care farms and at regular day care facilities with regard to their effects on functional performance of community-dwelling older people with dementia. Dementia. 2012;11(4):503–519. [Google Scholar]
- 32. Edwards CA, McDonnell C, Merl H. An evaluation of a therapeutic garden’s influence on the quality of life of aged care residents with dementia. Dementia (London). 2013;12(4):494–510. [DOI] [PubMed] [Google Scholar]
- 33. Hewitt P, Watts C, Hussey J, et al. Does a structured gardening programme improve well-being in young-onset dementia? A preliminary study. Br J Occup Ther. 2013;76(8):355–361. [Google Scholar]
- 34. Goto S, Kamal N, Puzio H, Kobylarz F, Herrup K. Differential responses of individuals with late-stage dementia to two novel environments: a multimedia room and an interior garden. J Alzheimers Dis. 2014;42(3):985–998. [DOI] [PubMed] [Google Scholar]
- 35. Chung J, Choi SI, Kim J. Experience of media presentations for the alleviation of agitation and emotional distress among dementia patients in a long-term nursing facility. Dementia (London). 2016;15(5):1021–1033. [DOI] [PubMed] [Google Scholar]
- 36. Hall J, Mitchell G, Webber C, et al. Effect of horticultural therapy on wellbeing among dementia day care programme participants: a mixed-methods study (Innovative Practice). Dementia (London). 2018;17(5):611–620. [DOI] [PubMed] [Google Scholar]
- 37. Kim HJ, Yang Y, Oh JG, et al. Effectiveness of a community-based multidomain cognitive intervention program in patients with Alzheimer’s disease. Geriatr Gerontol Int. 2016;16(2):191–199. [DOI] [PubMed] [Google Scholar]
- 38. de Boer B, Hamers JP, Zwakhalen SM, Tan FE, Beerens HC, Verbeek H. Green care farms as innovative nursing homes, promoting activities and social interaction for people with dementia. J Am Med Dir Assoc. 2017;18(1):40–46. [DOI] [PubMed] [Google Scholar]
- 39. Kamioka H, Tsutani K, Yamada M, et al. Effectiveness of horticultural therapy: a systematic review of randomized controlled trials. Complement Ther Med. 2014;22(5):930–943. [DOI] [PubMed] [Google Scholar]
- 40. Kam MC, Siu AM. Evaluation of a horticultural activity programme for persons with psychiatric illness. Hong Kong J Occup Ther. 2010;20(2):80–86. [Google Scholar]
- 41. Mapes N, Hine R. Research Project: Living With Dementia and Connecting With Nature–Looking Back and Stepping Forwards. Chelmsford, England: Dementia Adventure; 2011. [Google Scholar]
- 42. Schreiner AS, Yamamoto E, Shiotani H. Agitated behavior in elderly nursing home residents with dementia in Japan. J Gerontol B Psychol Sci Soc Sci. 2000;55:P180–P186. [DOI] [PubMed] [Google Scholar]
- 43. Cohen-Mansfield J. Nonpharmacologic interventions for inappropriate behaviors in dementia: a review, summary, and critique. Am J Geriatr Psychiatry. 2001;9(4):361–381. [PubMed] [Google Scholar]
- 44. Tanji H, Ootsuki M, Matsui T, et al. Dementia caregivers’ burdens and use of public services. Geriatr Gerontol Int. 2005;5(2):94–98. [Google Scholar]
- 45. Hartig T, Mitchell R, de Vries S, Frumkin H. Nature and health. Annu Rev Public Health. 2014;35:207–228. [DOI] [PubMed] [Google Scholar]
- 46. Kaplan R, Kaplan S. The Experience of Nature: A Psychological Perspective. Cambridge, England: CUP Archive; 1989. [Google Scholar]
- 47. Dahlkvist E, Hartig T, Nilsson A, et al. Garden greenery and the health of older people in residential care facilities: a multi-level cross-sectional study. J Adv Nurs. 2016;72(9):2065–2076. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Suppl._1_Search_strategies for Horticultural Therapy in Patients With Dementia: A Systematic Review and Meta-Analysis by Li-Chin Lu, Shao-Huan Lan, Yen-Ping Hsieh, Yea-Yin Yen, Jong-Chen Chen and Shou-Jen Lan in American Journal of Alzheimer's Disease & Other Dementias
Supplemental Material, Suppl._2_Search_strategy_Table for Horticultural Therapy in Patients With Dementia: A Systematic Review and Meta-Analysis by Li-Chin Lu, Shao-Huan Lan, Yen-Ping Hsieh, Yea-Yin Yen, Jong-Chen Chen and Shou-Jen Lan in American Journal of Alzheimer's Disease & Other Dementias
Supplemental Material, Suppl._3_Funnel_plot_of_CMAI for Horticultural Therapy in Patients With Dementia: A Systematic Review and Meta-Analysis by Li-Chin Lu, Shao-Huan Lan, Yen-Ping Hsieh, Yea-Yin Yen, Jong-Chen Chen and Shou-Jen Lan in American Journal of Alzheimer's Disease & Other Dementias