Abstract
This review provides a systematic overview of the state of knowledge to date of psychosocial risk factors with a focus on anxiety, depressiveness, and (lack of) social support among involuntarily childless women and men prior to assisted reproduction. The databases PubMed, PubPsych, PsycINFO-Ebsco, and Web of Science were searched for relevant publications in English or German, and finally a total of 20 publications were included in the systematic review. Of these, 18 studies focused on depressiveness, 15 studies focused on anxiety, and 9 studies focused on social support. Half of the studies included both men and women, while the other half included only women. Due to the large heterogeneity of the study results as well as limitations, no clear conclusions can be drawn regarding a difference between the risk profiles of men and women with an unfulfilled desire to have children. However, it has been shown that infertile couples or women experience higher levels of stress in the form of depressiveness and anxiety compared to fertile participants. Furthermore, it was found that social support, regardless of gender difference, within the couple and from family and friends may be associated with a lower risk for depressiveness and anxiety.
Keywords: infertility, anxiety, depressiveness, social support, assisted reproductive technology (ART)
Introduction
Infertility is thought to affect between 48 million couples and 186 million individuals of reproductive age worldwide 1 2 . The stigma of infertility can cause great psychological pressure on patients and severely affect their quality of life 3 . Reviews have shown that the unfulfilled desire to have children can affect marital and sexual relationships in addition to psychological well-being and quality of life 4 5 6 . However, from a psychological perspective, other papers report an extensive depathologization of infertile couples 7 8 . On the one hand, research shows that women with an unfulfilled desire to have children are more likely than men to suffer from depression and infertility-related stress 9 10 . On the other hand, there is a view that the assumption that women suffer more from infertility than their partners is influenced by outdated gender stereotypes 11 . The role of the man, but also of the couple as a dyad, has become more of a focus of infertility research in recent years 12 . The coping strategies of both partners are interrelated in infertility-related problems, and unfavorable strategies of one partner may increase the other’s risk for depressiveness and anxiety 13 .
In vitro fertilization was introduced in 1978 and represents a significant source of hope for patients with an unfulfilled desire to have children and thus a major factor influencing the psychological risk profile of patients 14 . According to the ESHRE guideline 13 , during an IVF/ICSI cycle, patients’ emotional stress levels fluctuate with peaks during oocyte collection, embryo transfer, and especially during the waiting period before the pregnancy test. In addition, one to two in ten women experience (transiently) clinically significant levels of depressive symptoms when treatment is unsuccessful. It is also emphasized that before the start of IVF treatment, patients are not more depressed than the general population 13 . Thus, it is necessary to differentiate between the influence of the sole diagnosis of infertility on the one hand and the influence of intensive fertility treatment in the form of assisted reproductive therapy (ART) on psychological stability on the other. Psychological findings on couples before ART tends to be underrepresented in the literature. Therefore, the AWMF guideline “Psychosomatic Diagnosis and Therapy in Fertility Disorders” comes to the following conclusion regarding psychological abnormalities (such as increased depressiveness and anxiety): “A generalization of these findings on couples not in treatment is only limited (see AWMF-LL 015–085)” 8 , p. 761). The aim of this systematic review is to provide an overview of the psychological characteristics of women and men with an unfulfilled desire to have children prior to ART, giving particular attention to the psychological risk factors of anxiety, depression, and lack of social support.
Methods
Literature inclusion and exclusion criteria
A comprehensive search was performed in the electronic databases PubMed, PubPsych, PsycINFO-Ebsco, and Web of Science for publications published in English and German before 2022. The articles were exported on 22 August 2022. The publications focused on the effect of infertility or the unfulfilled desire to have children on anxiety, depression, and social support. The search keywords were: infertil* AND anxiety AND depression AND social support.
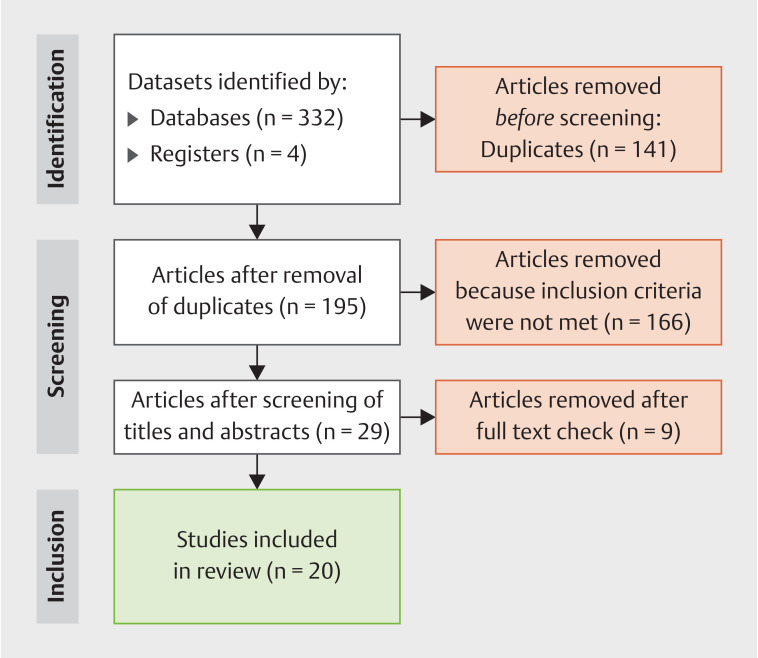
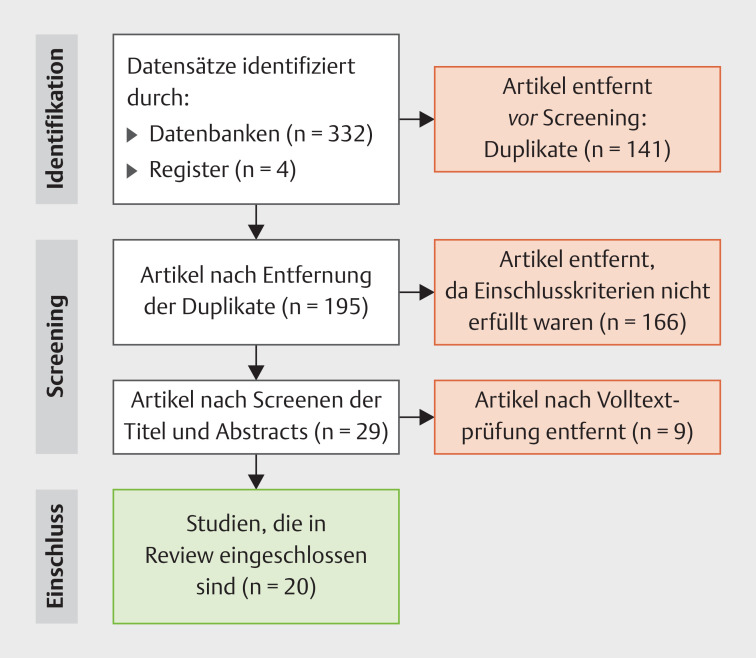
A total of 332 publications were found, plus relevant articles from the author search (n = 4). Fig. 1 illustrates the search process for identifying the relevant literature. Publications were added to the search results if they
Fig. 1.
PRISMA flow chart (Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-analyses: The PRISMA Statement. PLoS Med 2009; 6(7): e1000097. doi: 10.1371/journal.pmed.1000097 ).
had been published in peer-reviewed journals;
presented original results (i.e., no reviews);
included infertile couples with an unfulfilled desire to have children, men and/or women;
used validated measurement methods;
included couples who had not yet begun the assisted reproduction treatment process.
Because the emotional stress of couples undergoing ART may vary, publications that focused on reproductive medicine treatment or on in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI) were excluded 15 16 17 . Based on this, those studies were excluded in which it was clear that half or more of the participants were on or after ART.
After excluding duplicates, 195 publications remained. Titles and abstracts were screened for inclusion criteria. Publications that did not address infertility (n = 41) or the psychological aspects prior to starting infertility treatment (n = 35) were excluded, as were publications that focused on cancer (n = 3), COVID (n = 5), effects of psychotherapeutic therapies (n = 28), questionnaire validation (n = 7), medical diagnoses such as endometriosis or polycystic ovary syndrome (PCOS) (n = 14), or outcome variables other than depression, anxiety, and lack of social support (n = 5). In addition, publications that were not written in English or German were excluded (n = 7), as well as reviews and meta-analyses (n = 19), and non-peer-reviewed publications (n = 2). A total of 166 publications were discarded, while 29 publications remained. Two reviewers (CLT and TW) independently conducted the review of the 29 studies using the full texts, and nine publications were subsequently excluded. The nine excluded studies were publications on the psychological aspects after or during ART. In 12 studies, it was unclear whether patients were undergoing intensive fertility treatment at the time of data collection. However, because their results did not differ significantly from the eight studies that clearly did not address ART, these 12 studies were included in the systematic review. Ultimately, 20 quantitative studies were included in the review.
Quality assessment
The quality of the studies was assessed using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Guideline 18 . This checklist includes a maximum score of 22 points covering the areas of title, abstract, introduction, methods, results, and discussion of a publication. One point corresponds to one item, provided that the criteria apply. 18 of the 22 items are applicable to all study designs and four items are specific to cross-sectional, case-control, and cohort studies. If the total study score was ≥ 17, the quality of the study was rated as high, with a score between 11 and 16 as moderate, and at ≤ 10 points as a low-quality study. No low-quality study could be found, while 17 of the 20 studies were rated as moderate-quality, and three studies were rated as high-quality ( Table 1 ).
Table 1 Variables and methodological quality of studies.
| Reference | Depression | Anxiety | Social support | Quality assessment | |
| Quality of evidence | Score | ||||
| Aldemir et al. (2015) 19 | ☑ | ☑ | ☑ | Moderate | 14 |
| Al-Homaidan (2011) 20 | ☑ | Moderate | 16 | ||
| Alhassan et al. (2014) 21 | ☑ | Moderate | 14 | ||
| Baghiani Moghadam et al. (2011) 22 | ☑ | ☑ | Moderate | 12 | |
| Batool and de Visser (2014) 23 | ☑ | ☑ | ☑ | Moderate | 13 |
| Berg and Wilson (1990) 24 | ☑ | ☑ | Moderate | 14 | |
| Connolly et al. (1992) 25 | ☑ | ☑ | ☑ | Moderate | 15 |
| Dadhwal et al. (2022) 26 | ☑ | ☑ | Moderate | 15 | |
| Giannouli and Stoyanova (2018) 27 | ☑ | ☑ | ☑ | Moderate | 12 |
| Karlidere et al. (2007) 28 | ☑ | ☑ | ☑ | High | 17 |
| Kiesswetter et al. (2020) 29 | ☑ | Moderate | 13 | ||
| Mao et al. (2022) 30 | ☑ | Moderate | 16 | ||
| Matsubayashi et al. (2001) 31 | ☑ | ☑ | Moderate | 14 | |
| Matsubayashi et al. (2004) 32 | ☑ | ☑ | ☑ | Moderate | 13 |
| Noorbala et al. (2009) 33 | ☑ | ☑ | Moderate | 14 | |
| Pinar and Zeyneloglu (2012) 34 | ☑ | ☑ | Moderate | 15 | |
| Sadiq et al. (2022) 35 | ☑ | ☑ | Moderate | 16 | |
| Shafierizi et al. (2022) 36 | ☑ | ☑ | ☑ | High | 19 |
| Vo et al. (2019) 37 | ☑ | High | 20 | ||
| Wischmann et al. (2001) 38 | ☑ | ☑ | Moderate | 14 | |
Results
Characteristics of the selected studies
All 20 selected studies were published in peer-reviewed journals. These included 15 cross-sectional studies, four case-control studies, and one cohort study. The studies include a heterogeneous patient population with 5226 participants from 15 different countries. These included six studies in Europe (Bulgaria, Germany, Greece, Italy, and the United Kingdom [UK]), nine studies in the Middle East (Iran, Pakistan, Saudi Arabia, Turkey), five in East Asia (China, India, Japan, Vietnam), one study in Africa (Ghana), and one study in North America (United States). Two publications focused on the comparison of infertile women between two countries (Bulgaria and Greece, UK and Pakistan).
The publications all addressed the psychological aspects of depressiveness, anxiety, and (lack of) social support in the unfulfilled desire to have children. Among these, 18 studies addressed depressiveness, 15 studies addressed anxiety, and nine studies addressed social support. Fifteen publications elaborated on more than one of the psychological factors. Ten studies included both women and men, ten studies included only infertile women, and no study addressed infertile men alone.
The results of the systematic review are listed in the following tables: The correlation between infertility and depressiveness ( Table 2 ), anxiety ( Table 3 ), and social support ( Table 4 ).
Table 2 Summary of involuntary childlessness and depressiveness.
| Reference | Design | Sample size | Instrument | Findings |
| BDI = Beck Depression Inventory; CES-D = Center for Epidemiologic Studies Depression Scale; DASS = Depression, Anxiety, Stress Scale; GHQ-28 = General Health Questionnaire; HADS = Hospital Anxiety and Depression Scale; HDRS = Hamilton Depression Rating Scale; PHQ-9 = Patient Health Questionnaire; SCL-90-R = Symptom Check List (revised) | ||||
| Aldemir et al. (2015) 19 (Turkey) | Cross-section | 66 infertile couples | HADS | There was no clinical depression detectable in the participants. No significant differences were found between the two genders. |
| Al-Homaidan (2011) 20 (Saudi Arabia) | Case-control | 91 infertile women, 94 fertile women |
BDI | 53.8% of infertile women and 37.2% of fertile women experienced depression. The mean BDI score was higher in infertile women than in fertile women. Infertile women suffered significantly more frequently from severe depression than fertile women. |
| Alhassan et al. (2014) 21 (Ghana) | Cross-section | 100 infertile women | BDI | 62.0% of women had some form of depression, including 40% with a mild form and 22% with a moderate form of depression. No woman had severe depression. |
| Baghiani Moghadam et al. (2011) 22 (Iran) | Cross-section | 150 infertile couples | GHQ-28 | Women showed higher depression scores than men. No threshold for pathological significance was given for the individual subscales. |
| Batool and de Visser (2014) 23 (UK and Pakistan) | Cross-section | 312 infertile women (UK [n = 148], Pakistan [n = 164]) | GHQ-28 | Although no significant differences in overall outcomes were demonstrated, Pakistani women showed higher depression scores than British women. There were no thresholds for pathological significance. |
| Berg and Wilson (1990) 24 (USA) | Cross-section | 104 infertile couples | SCL-90-R | A psychiatric disorder was identified in 44% of men and 52% of women according to the SCL-90-R instrument. No difference between men and women could be shown. Women were above the 84th percentile (borderline range) in depression. |
| Connolly et al. (1992) 25 (UK) | Cohort | 130 infertile couples | BDI | Depression scores remained low in the couples over the 7-month period. A significant difference was found between the two sexes (women had higher BDI scores than men). There was no threshold for pathological significance. |
| Dadhwal et al. (2022) 26 (India) | Cross-section | 150 infertile women | HDRS | 58% of women had depression, including 35.6% with moderate to severe depression. 24% of women had both depression and anxiety according to HDRS and HAM-A. On average, the women had mild depression. |
| Giannouli and Stoyanova (2018) 27 (Bulgaria and Greece) | Cross-section | 148 infertile women (Bulgaria [n = 74], Greece [n = 74]) | CES-D | No difference could be demonstrated between the two countries, Bulgaria and Greece (CES_D: Greek: M = 24.4; Bulgarian: M = 21.8). |
| Karlidere et al. (2007) 28 (Turkey) | Cross-section | 103 infertile couples | BDI | No clinical depression could be detected. The depression scores of women were higher than those of men in all groups except the male infertility group. Female symptoms were lowest when the cause was unknown and highest when the cause was female only. |
| Matsubayashi et al. (2001) 31 (Japan) | Case-control | 101 infertile women, 81 pregnant women |
HADS | The depression scores of infertile women were significantly higher than those of pregnant women. 38.6% of infertile women were above the threshold of the HADS scale, compared to 16.0% of pregnant women. |
| Matsubayashi et al. (2004) 32 (Japan) | Cross-section | 101 infertile women | HADS, “in-house” questionnaire | Depressiveness correlated significantly with a lack of support from the husband and feelings of stress. The prevalence of depressiveness in this sample was previously published by Matsubayashi et al. (2001) 31 . |
| Noorbala et al. (2009) 33 (Iran) | Case-control | 150 infertile women, 150 fertile women |
SCL-90-R | 44% of infertile women and 28.7% of fertile women had a psychiatric disorder. Both infertile and fertile women had the highest mean scores for depression, with the scores of infertile women being higher than those of fertile women. |
| Pinar and Zeyneloglu (2012) 34 (Turkey) | Case-control | 160 infertile participants, 160 fertile participants | BDI | Infertile participants had higher BDI scores than fertile participants. 35% of the infertile group showed no symptoms of depression, while 25% had a “mild” level of symptoms and 40% had a “moderate” level of depressive symptoms. Infertile women had higher depression scores than men. |
| Sadiq et al. (2022) 35 (Pakistan) | Cross-section | 115 infertile women | DASS | Self-compassion was negatively associated with psychological distress (depression, anxiety, and stress). Marital quality was a significant predictor of depression and stress. Self-compassion significantly influenced the relationship between marital quality and psychological distress (depression and stress). No thresholds for pathological significance were determined on the DASS scale. |
| Shafierizi et al. (2022) 36 (Iran) | Cross-section | 162 infertile participants (122 women, 40 men) | BDI-II | Women had higher mean scores than men. Overall, 40.7% of participants exhibited depression. |
| Vo et al. (2019) 37 (Vietnam) | Cross-section | 401 infertile women | PHQ-9 | A prevalence of depressiveness of 12.2% was demonstrated. The mean score of the PHQ-9 scale was 3.04 (SD = 3.75). |
| Wischmann et al. (2001) 38 (Germany) | Cross-section | 564 infertile couples | SCL-90-R | Women showed slightly higher depression scores compared to the norm. No notable differences were found in men compared to the comparison group. There were no thresholds for pathological significance on the SCL-90-R scale. |
Table 3 Summary of involuntary childlessness and anxiety.
| Reference | Design | Sample size | Instrument | Findings |
| BAI = Beck Anxiety Inventory; DASS = Depression, Anxiety, Stress Scale; GHQ-28 = General Health Questionnaire; HADS = Hospital Anxiety and Depression Scale; HAM-A = Hamilton Anxiety Inventory; SCL-90-R = Symptom Check List (revised), STAI = State-Trait Anxiety Inventory | ||||
| Aldemir et al. (2015) 19 (Turkey) | Cross-section | 66 infertile couples | HADS | The couples’ anxiety scores were within the normal range, with females showing higher anxiety scores compared to males. |
| Baghiani Moghadam et al. (2011) 22 (Iran) | Cross-section | 150 infertile couples | GHQ-28 | Women showed higher anxiety scores than men. No threshold for pathological significance was given for the individual subscales. |
| Batool and de Visser (2014) 23 (UK and Pakistan) | Cross-section | 312 infertile women (UK [n = 148], Pakistan [n = 164]) |
GHQ-28 | Although there were no significant differences in overall General Health Questionnaire (GHQ) scores, British women reported more anxiety than Pakistani women. There were no thresholds for pathological significance. |
| Berg and Wilson (1990) 24 (USA) | Cross-section | 104 infertile couples | SCL-90-R | There were 44% of men and 52% of women identified with a psychiatric disorder according to the SCL-90-R evaluation. With regard to anxiety, no difference was found between men and women. |
| Connolly et al. (1992) 25 (UK) | Longitudinal section | 260 infertile couples | STAI | In both men and women, anxiety scores decreased within the 7–9 months. In men, a correlation of higher anxiety scores and a diagnosis of a male problem was found. For women, “tangible support” was associated with lower anxiety scores. No threshold for pathological significance was given. |
| Dadhwal et al. (2022) 26 (India) | Cross-section | 150 infertile women | HAM-A | 24% of women exhibited anxiety according to HAM-A, of which 52.77% were in the mild category. 24% of women exhibited both depression and anxiety. The group mean anxiety score was below the cut-off for clinical relevance. |
| Giannouli and Stoyanova (2018) 27 (Bulgaria and Greece) | Cross-section | 148 infertile women (Bulgaria [n = 74], Greece [n = 74]) | STAI | No difference could be found between both countries Bulgaria and Greece (STAI: Greek: M = 48.8; Bulgarian: M = 47.6). The study results were not considered in relation to the given thresholds for pathological significance of the scales. |
| Karlidere et al. (2007) 28 (Turkey) | Cross-section | 103 infertile couples | STAI | State anxiety scores were in the normal range for all participants. For trait anxiety, high scores were found in both females and males. |
| Matsubayashi et al. (2001) 31 (Japan) | Case-control | 101 infertile women, 81 pregnant women |
HADS | The anxiety HADS scores of the infertile women were significantly higher than those of the pregnant women. 38.6% of infertile women were above the threshold of the HADS scale, compared to 16.0% of pregnant women. |
| Matsubayashi et al. (2004) 32 (Japan) | Cross-section | 101 infertile women | HADS, “in-house” questionnaire | Anxiety and depressiveness correlated significantly with a lack of support from the husband and feelings of stress. The prevalence of anxiety in this sample was previously published by Matsubayashi et al. (2001) 31 . |
| Noorbala et al. (2009) 33 (Iran) | Case-control | 150 infertile women, 150 fertile women |
SCL-90-R | In the anxiety subscale, there was no difference between infertile and fertile women. Infertile and fertile women had the lowest mean scores for phobic anxiety. Here, infertile women scored significantly higher than fertile women. |
| Pinar and Zeyneloglu (2012) 34 (Turkey) | Case-control | 160 infertile participants, 160 fertile participants | BAI | Involuntarily childless participants showed higher anxiety scores than fertile participants. In the infertile group, 62.5% suffered from “mild” anxiety, 25% from “moderate” anxiety, and 12.5% from “severe” anxiety. Infertile women had higher anxiety scores than men. |
| Sadiq et al. (2022) 35 (Pakistan) | Cross-section | 115 infertile women | DASS | Self-compassion was negatively associated with psychological distress (depression, anxiety, and stress). Marital quality was not a significant predictor of anxiety. No thresholds for pathological significance were determined on the DASS scale. |
| Shafierizi et al. (2022) 36 (Iran) | Cross-section | 122 infertile women, 40 infertile men |
STAI | Women showed a higher level of trait anxiety compared to men. No significant difference was identified in state anxiety. The overall prevalence of anxiety was 45.7%. |
| Wischmann et al. (2001) 38 (Germany) | Cross-section | 564 infertile couples | SCL-90-R | Compared to the norm, women showed slightly higher anxiety scores. No differences were found among men. There were no thresholds for pathological significance on the SCL-90-R scale. |
Table 4 Summary of involuntary childlessness and social support.
| Reference | Design | Sample size | Instrument | Findings |
| Berlin Social Support Scale (ARS = Actual Received Support; PAS = Perceived Available Support), ISEL = Interpersonal Support Evaluation List; MSPSS = Multidimensional Scale of Perceived Social Support; PFS = Procidano and Heller’s Perceived Family Support; PPS = Perceived Peer Support; PSS = Perceived Social Support; SSQ = Social Support Questionnaire; SSRS = Social Support Rating Scale | ||||
| Aldemir et al. (2015) 19 (Turkey) | Cross-section | 66 infertile couples | MSPSS | No difference was found between the two genders in perceived social support. When couples’ social support scores increased, anxiety and depression scores decreased. |
| Batool and de Visser (2014) 23 (UK and Pakistan) | Cross-section | 312 infertile women (UK [n = 148], Pakistan [n = 164]) |
Berlin Social Support Scale (PAS, ARS) | British women reported higher Actual Received Support (ARS) scores than Pakistani women. Higher ARS scores were associated with higher GHQ scores in both groups. Higher Perceived Available Support (PAS) scores were associated with higher GHQ scores for Pakistani scores. There were no thresholds for pathological significance. |
| Connolly et al. (1992) 25 (UK) | Longitudinal section | 260 infertile couples | ISEL | For women, tangible support (subscale of ISEL) was associated with lower anxiety scores. There was no threshold for pathological significance. |
| Giannouli and Stoyanova (2018) 27 (Bulgaria and Greece) | Cross-section | 148 infertile women (Bulgaria [n = 74], Greece [n = 74]) | MSPSS | Greek women perceived less social support from their environment (from family, friends, and significant others) than Bulgarian women. The study results were not considered in relation to the given thresholds for pathological significance of the scales. |
| Karlidere et al. (2007) 28 (Turkey) | Cross-section | 103 infertile couples | PFS, PPS | Compared with their husbands, women perceived more social support from their families, regardless of whether they or their husbands were the cause of the infertility. In the area of peer support, equal scores were found for the two genders. |
| Kiesswetter et al. (2020) 29 (Italy) | Cross-section | 228 infertile couples | SSQ | Women had higher scores than men on the total social support scale score and on 4 of the 5 subscales (Emotional Support, Practical Support, Social Inclusion, Person of Trust). There was no threshold for pathological significance. |
| Mao et al. (2022) 30 (China) | Cross-section | 57 infertile women, 3 infertile men |
SSRS | The use of social support was an influencing factor of coping style (confrontation, avoidance, yielding). There was no threshold for pathological significance on the SSRS scale. |
| Matsubayashi et al. (2004) 31 (Japan) | Cross-section | 101 infertile women | HADS, “in-house” questionnaire | Anxiety and depression scores correlated significantly with a lack of support from the husband. No threshold for pathological significance was given. |
| Shafierizi et al. (2022) 36 (Iran) | Cross-section | 122 infertile women, 40 infertile men |
PSS | No significant differences were found between men and women in the total score and the 4 of 5 subscales of social support. However, for social support from the family, women scored higher than men. |
Involuntary childlessness and depressiveness
Of the 18 publications that dealt with the risk factor of depressiveness, eight studies examined both men and women. These included six studies that explicitly included only infertile couples and two studies that had an unequal number of men and women and thus did not focus solely on the couple. Among these two publications was also a study comparing infertile patients with fertile patients. Ten studies included only women, and among these ten studies, three studies compared infertile women with fertile women. In addition, two publications dealt with the comparison of infertile women between two countries (Bulgaria and Greece, UK and Pakistan).
The survey instruments were very heterogeneous. The following questionnaires were used to assess the participants’ level of depression: Beck Depression Inventory 20 21 25 28 34 , Beck Depression Inventory-II 36 , Center for Epidemiologic Studies Depression Scale 27 , Depression Anxiety Stress Scale 35 , General Health Questionnaire 28 23 22 , Hospital Anxiety and Depression Scale 19 31 32 ,Hamilton Depression Rating Scale 26 , Patient Health Questionnaire 9 37 , Symptom Check List 90-R 24 33 38 , and an “in-house” questionnaire 32 .
In two Turkish publications that looked at both men and women, no clinically relevant depression was found in the couples 19 28 . In another Turkish study that compared infertile participants with fertile participants, 25% of participants were found to have mild levels of depressive symptoms and 40% had moderate levels 34 . Here, the infertile group had higher depression scores compared to the fertile participants. When depression scores were compared between the two sexes, four studies showed higher scores for women compared to men 28 22 34 36 . In contrast, again no differences between women and men were found in three studies 19 24 25 . When comparing women and men, respectively, with a representative sample, slightly higher scores for depression were found in women compared to the norm, whereas no differences were detected in men 38 .
In the studies that included only women, different prevalences of depressiveness were noted. The study from Ghana was able to identify 62.0% of women with a mild to moderate form of depression 21 . According to the results of the Indian cross-sectional study, 58% of infertile women were identified with depression, including 35.6% with a moderate to severe form of depression 26 . The Iranian study identified 40.7% of participants with depression 36 . In contrast, in the Vietnamese study, the prevalence of depression was 12.2% 37 . The 2001 Japanese study comparing infertile women with pregnant women showed that 38.6% of infertile women were above the cut-off score of the HADS depression scale, compared with 16.0% of pregnant women 31 . The studies from Saudi Arabia and Iran also showed that infertile women have higher depression scores compared to fertile women 20 33 . The study, which examined cross-country differences between infertile Bulgarian and Greek women, did not find differences in depression scores between infertile women from Bulgaria and Greece 27 . Infertile Pakistani women were found to have higher scores on the depression subscale compared to infertile British women 23 . The importance of marital quality in relation to depressiveness among infertile women is demonstrated by two studies from Japan and Pakistan. The research results showed, on the one hand, that low marital quality is a significant predictor of depression and stress and, on the other hand, that depressiveness correlates with a lack of support from the husband and feelings of stress 32 35 .
Involuntary childlessness and anxiety
Among the 15 publications that addressed infertility and anxiety, eight studies addressed both women and men and seven studies addressed only infertile women. The survey instruments used were as follows: Beck Anxiety Inventory 34 , Depression Anxiety Stress Scale 35 , General Health Questionnaire 28 23 22 , Hospital Anxiety and Depression Scale 19 31 32 , Hamilton Anxiety Inventory, 26 , Symptom Check List 90 (revised) 24 33 38 , and State-Trait Anxiety Inventory 25 27 36 39 .
In the British longitudinal study, a decrease in anxiety scores within 7–9 months was found in both men and women 25 . In three studies, women had higher scores for anxiety compared to men 19 22 34 , and trait anxiety in the Iranian study 36 . For trait anxiety, another study from Turkey demonstrated high scores in both genders 28 . It was highlighted in both Turkish studies that despite the gender difference, the overall and state anxiety scores were not in the pathological range 19 28 . This was also shown in the study from India, in which the group mean of infertile women was below the threshold for clinical relevance 26 . The German study found no difference in anxiety scores for infertile males compared to the norm, while females had slightly higher scores compared to the norm 38 . In the American study, which also examined men and women, no difference was found between the sexes 24 . This was also shown in the study by Shafierizi et al. (2022) for state anxiety. Here, however, 45.7% of participants showed increased anxiety. When infertile participants were compared with fertile participants, a Turkish study found higher anxiety scores in the infertile group 34 . The Iranian and Japanese study comparing infertile women with fertile women also demonstrated this difference 31 33 . According to the results of the study from Pakistan, marital quality was not a significant predictor of anxiety 35 , whereas results from the Japanese study showed that a lack of support from the husband correlated significantly with anxiety in the wife 32 . The comparative country studies did not find any relevant differences between infertile British and Pakistani women or between Bulgarian and Greek women 23 27 .
Involuntary childlessness and social support
The construct “social support” is generally defined as helpful interaction with others (e.g., partnership, family, friendships) in coping with a problem. Usually, a distinction is made between emotional support (e.g., comfort), instrumental support (e.g., practical help), and informational support (e.g., guidance). What is measured is mostly the subjectively perceived support (not the actual received support). Of the nine publications, three studies included only infertile women and six included both women and men in terms of social support. The nine studies used the Berlin Social Support Scale 23 , an in-house questionnaire 32 , Interpersonal Support Evaluation List 25 , Multidimensional Scale of Perceived Social Support 19 27 , Procidano and Heller’s Perceived Family Support and Perceived Peer Support 36 , Social Support Questionnaire 29 , and Social Support Rating 30 .
Two studies found higher levels of social support from the family in women than in men 28 36 . This difference was also shown by the Italian study in the areas of emotional and practical support, social inclusion, and “Person of Trust” support 29 . However, results from the two Turkish and Iranian studies showed that the two genders did not differ in all areas of their perceived social support. For example, no differences between women and men were detectable in the total scales of social support 19 28 36 . It was also found that in women or couples, tangible social support from the environment was associated with low anxiety and depression scores 19 25 32 . The Chinese study showed the influence of social support in infertile women and men on their respective coping styles 30 . In the comparative country studies, Greek women were found to have lower perceived social support compared to infertile women from Bulgaria 27 . British women showed higher scores compared to Pakistani women on the “Actual Received Support” scale 23 .
Discussion
The aim of this review, which comprised a total of 20 studies, was to provide an overview of the psychological aspects of women and men with an unfulfilled desire to have children prior to assisted reproduction in terms of depression, anxiety, and social support.
For depressiveness, it was not found overall that women are more depressed compared to men. Since an equal number of studies each found a difference or no difference between the two genders, no clear conclusion can be drawn. It can be seen that the data are very heterogeneous. However, when comparing infertile couples and women, each with a representative sample, a difference in depression scores was shown in the corresponding studies. The very wide range of depressive prevalences is striking. While some studies found no pathological significance in couples (0%), prevalences of depression in other studies of infertile women ranged from 12 to 62%. As Kiani et al. (2021) describe in their work, the different prevalences of depression among infertile women worldwide can be explained by, among other things, different income levels between countries 40 . Here, while 44.3% of infertile women in low or middle-income countries were identified with depression, only 28% of infertile women from high-income countries showed depression. Using the Human Development Index (HDI) to measure human development, which comprises the three dimensions of “long and healthy life”, “knowledge”, and “adequate standard of living”, the different countries can be compared 41 . Thus, the HDI also reflects, in part, differences in the quality and availability of national health care systems (which, in the context of the question posed in this review, relates particularly to the financially as well as logistically low-threshold availability of professional infertility-specific diagnostics). By classifying the survey countries into the respective “human development” groups, orientation can be provided with regard to factors such as social development, health status of the population, and level of education. The survey countries in our studies that had high prevalences of depression were in the middle (Ghana and India) and high (Vietnam and Iran) “Human Development” group according to the 2022 index. The two Turkish studies, for which no clinical relevance was demonstrated, could be classified in the group with a very high HDI. The comparative country studies also support the assumption that the differences in psychological stress among infertile women and men can be explained by differences regarding cultural, social, and economic factors. It must additionally be taken into account when interpreting the prevalences that the different studies used different survey instruments. The results of Fisher and Hammarberg’s (2012) review found, in comparison, that both fertile and infertile men have as great a desire for parenthood as their female partners do 42 . This showed no clinically significant mental health problems in men compared with the general population.
Anxiety related to involuntary childlessness also showed mixed results in terms of gender difference. While several studies showed a difference between anxiety scores in women and men, others showed no significant difference. In a majority of studies, higher anxiety scores were demonstrated in infertile couples or women compared to fertile participants. It can be assumed that women who have just received a diagnosis of infertility are anxious about the reproductive medical treatment that may follow. Infertile women face treatment-specific problems, feelings of failure, and also fear of operations compared to fertile women. It was found that women who felt better informed about infertility treatment had lower anxiety and depression scores 34 .
Likewise, in the area of social support in infertility, an equal number of studies found a difference or no difference between men and women. A review by Cousineau and Domar (2007) concludes that men suffer silently to support their wives 43 . The importance of high social support among infertile women and men was demonstrated in several studies in our review by associated low levels of depression and anxiety. Infertile women, on the other hand, experience social isolation in very pronatalist cultures due to the stigma of childlessness and usually receive less support from their husbands or family and friends 3 . Regardless of the gender difference, good social support from the partner is negatively associated with the risk for depressiveness or anxiety in the sense of “buffering” 44 .
In comparison to the results of this review, the systematic review by Luk and Loke (2015) shows that couples with infertility are impaired in the areas of life of psychological well-being, marital relations, sexual relations, and quality of life. It has been highlighted that involuntary childlessness has a negative impact on the psychological well-being of couples. That infertility is a more stressful experience for women than for men is inferred by Greil et al. (1997) with the help of their review. This is inconsistent with our results because no clear conclusion can be made about the gender difference with regard to psychological stress due to the heterogeneity of the study results. It can be surmised that over the past few decades, the defined roles of the genders have changed. This assumption is also held by Edelmann and Connolly, who argue that the claim that women react more negatively to infertility than their partners is shaped by outdated gender stereotypes 11 . On the other hand, the results can be explained by the fact that men now answer less in line with social desirability compared to the last decade.
Limitations and Strengths of this Review
With these findings, the results discussed here, which come from a total of 15 different countries, should be viewed with caution. As a further limitation of this review, it must be mentioned that due to the many different survey instruments used, a direct comparability of the study results is very limited. In addition, only publications in English or German could be included. The majority of the included studies were cross-sectional, so no conclusion can be drawn about the causality of psychological factors. Because cut-off scores of the questionnaires used were not presented in all included studies, the pathological relevance of the discussed results cannot be understood from each study. It must also be mentioned that, depending on the study, both pregnant women and postpartum women were used to compare the infertile participants with a fertile group. Due to various external influences (including hormonal), the groups may be subject to different emotional stresses that are not comparable. Furthermore, the number of publications found is comparatively low because [and] and not [or] was used in the search string. In this systematic review, no exclusion criterion was set in relation to the time of publication of the studies. However, the data collection of all studies took place after the introduction of IVF in 1978. In addition, it must be mentioned that in the included studies it is often assumed that only heterosexual couples are meant under the definition of couple. The significance of the psychosocial aspects of the unfulfilled desire to have children in same-sex couples or other sexual identities or in individuals is therefore only transferable to a limited extent.
Summary
A total of 20 studies were included in the systematic review, of which 18 focused on depressiveness and 15 on anxiety, while nine addressed the social support aspect. Both women and men were studied in half of the studies, while the other half included only women. Due to the large heterogeneity of the study results in the areas of depressiveness, anxiety, and social support, and considering the limitations, it is currently not possible to draw clearly provable conclusions about a difference between psychological risks of men versus women with an unfulfilled desire to have children. However, it could be shown that infertile couples or women compared to fertile participants experience an overall higher emotional stress in the form of depressiveness and anxiety, which can only be partially “buffered” by protective factors such as good social support.
Accordingly, future interventions and research focusses should emphasize strengthening social relationships. It is important to promote the education of family and friends in order to strengthen the sympathy from this group and thus (somewhat) reduce the psychosocial stress of infertile women and men. This can be achieved, on the one hand, by education in the context of fertility treatment or in the media context, and, on the other hand, by involving both partners in the course of treatment.
Further studies of depression, anxiety, and social support should be conducted to provide a more comprehensive picture of the impact of infertility on couples. In addition to cross-sectional studies, longitudinal studies should be performed at different times of ART. Here, it is necessary, among other things, to clearly identify the time of data collection during the course of assisted reproductive therapy (ART) to ensure comparability of study results. In addition, uniform measurement tools and larger samples should be used for better comparison.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References/Literatur
- 1.Mascarenhas MN, Flaxman SR, Boerma T et al. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9:e1001356. doi: 10.1371/journal.pmed.1001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boivin J, Bunting L, Collins JA et al. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506–1512. doi: 10.1093/humrep/dem046. [DOI] [PubMed] [Google Scholar]
- 3.Xie Y, Ren Y, Niu C et al. The impact of stigma on mental health and quality of life of infertile women: A systematic review. Front Psychol. 2023;13:1.093459E6. doi: 10.3389/fpsyg.2022.1093459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luk BH, Loke AY. The Impact of Infertility on the Psychological Well-Being, Marital Relationships, Sexual Relationships, and Quality of Life of Couples: A Systematic Review. J Sex Marital Ther. 2015;41:610–625. doi: 10.1080/0092623X.2014.958789. [DOI] [PubMed] [Google Scholar]
- 5.Chachamovich JR, Chachamovich E, Ezer H et al. Investigating quality of life and health-related quality of life in infertility: a systematic review. J Psychosom Obstet Gynaecol. 2010;31:101–110. doi: 10.3109/0167482x.2010.481337. [DOI] [PubMed] [Google Scholar]
- 6.Greil AL. Infertility and psychological distress: a critical review of the literature. Soc Sci Med. 1997;45:1679–1704. doi: 10.1016/s0277-9536(97)00102-0. [DOI] [PubMed] [Google Scholar]
- 7.Greil AL, Slauson-Blevins K, McQuillan J. The experience of infertility: a review of recent literature. Sociol Health Illn. 2010;32:140–162. doi: 10.1111/j.1467-9566.2009.01213.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wischmann T, Borkenhagen A, David M et al. Psychosomatically Oriented Diagnostics and Therapy for Fertility Disorders. Guideline of the DGPFG (S2k-Level, AWMF Registry Number 016/003, December 2019) Geburtshilfe Frauenheilkd. 2021;81:749–768. doi: 10.1055/a-1341-9664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson BD, Sejbaek CS, Pirritano M et al. Are severe depressive symptoms associated with infertility-related distress in individuals and their partners? Hum Reprod. 2014;29:76–82. doi: 10.1093/humrep/det412. [DOI] [PubMed] [Google Scholar]
- 10.Donarelli Z, Lo Coco G, Gullo S et al. Are attachment dimensions associated with infertility-related stress in couples undergoing their first IVF treatment? A study on the individual and cross-partner effect. Hum Reprod. 2012;27:3215–3225. doi: 10.1093/humrep/des307. [DOI] [PubMed] [Google Scholar]
- 11.Edelmann RJ, Connolly KJ. Gender differences in response to infertility and infertility investigations: Real or illusory. Br J Health Psychol. 2000;5:365–375. [Google Scholar]
- 12.Quinlivan J, Rowe H, Wischmann T et al. Setting the global research agenda in psychosocial aspects of women’s health – outcomes from ISPOG world conference at The Hague. J Psychosom Obstet Gynaecol. 2020;41:1–4. doi: 10.1080/0167482X.2020.1695872. [DOI] [PubMed] [Google Scholar]
- 13.Gameiro S, Boivin J, Dancet E et al. ESHRE guideline: routine psychosocial care in infertility and medically assisted reproduction-a guide for fertility staff. Hum Reprod. 2015;30:2476–2485. doi: 10.1093/humrep/dev177. [DOI] [PubMed] [Google Scholar]
- 14.Eskew AM, Jungheim ES. A History of Developments to Improve in vitro Fertilization. Mo Med. 2017;114:156–159. [PMC free article] [PubMed] [Google Scholar]
- 15.Quant HS, Zapantis A, Nihsen M et al. Reproductive implications of psychological distress for couples undergoing IVF. J Assist Reprod Genet. 2013;30:1451–1458. doi: 10.1007/s10815-013-0098-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agostini F, Monti F, Paterlini M et al. Effect of the previous reproductive outcomes in subfertile women after in vitro fertilization (IVF) and/or intracytoplasmic sperm injection (ICSI) treatments on perinatal anxious and depressive symptomatology. J Psychosom Obstet Gynaecol. 2018;39:29–37. doi: 10.1080/0167482x.2017.1286474. [DOI] [PubMed] [Google Scholar]
- 17.Moura-Ramos M, Gameiro S, Canavarro MC et al. Does infertility history affect the emotional adjustment of couples undergoing assisted reproduction? The mediating role of the importance of parenthood. Br J Health Psychol. 2016;21:302–317. doi: 10.1111/bjhp.12169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.von Elm E, Altman DG, Egger M et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 19.Aldemir S, Eser A, Ozturk Turhan N et al. Relation of anxiety and depressive symptoms with perceived social support according to gender within infertile couples. Dusunen Adam. 2015;28:328–336. doi: 10.5350/DAJPN2015280404. [DOI] [Google Scholar]
- 20.Al-Homaidan HT. Depression among Women with Primary Infertility attending an Infertility Clinic in Riyadh, Kingdom of Saudi Arabia: Rate, Severity, and Contributing Factors. Int J Health Sci (Qassim) 2011;5:108–115. [PMC free article] [PubMed] [Google Scholar]
- 21.Alhassan A, Ziblim AR, Muntaka S. A survey on depression among infertile women in Ghana. BMC Womens Health. 2014;14:42. doi: 10.1186/1472-6874-14-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baghiani Moghadam MH, Aminian AH, Abdoli AM et al. Evaluation of the general health of the infertile couples. Iran J Reprod Med. 2011;9:309–314. [PMC free article] [PubMed] [Google Scholar]
- 23.Batool SS, de Visser RO. Psychosocial and contextual determinants of health among infertile women: a cross-cultural study. Psychol Health Med. 2014;19:673–679. doi: 10.1080/13548506.2014.880492. [DOI] [PubMed] [Google Scholar]
- 24.Berg BJ, Wilson JF. Psychiatric morbidity in the infertile population: a reconceptualization. Fertil Steril. 1990;53:654–661. [PubMed] [Google Scholar]
- 25.Connolly KJ, Edelmann RJ, Cooke ID et al. The impact of infertility on psychological functioning. J Psychosom Res. 1992;36:459–468. doi: 10.1016/0022-3999(92)90006-n. [DOI] [PubMed] [Google Scholar]
- 26.Dadhwal V, Choudhary V, Perumal V et al. Depression, anxiety, quality of life and coping in women with infertility: A cross-sectional study from India. Int J Gynaecol Obstet. 2022;158:671–678. doi: 10.1002/ijgo.14084. [DOI] [PubMed] [Google Scholar]
- 27.Giannouli V, Stoyanova S. Exploring emotional aspects of infertility in women from two countries. Psychiatriki. 2018;29:34–41. doi: 10.22365/jpsych.2018.291.34. [DOI] [PubMed] [Google Scholar]
- 28.Karlidere T, Bozkurt A, Yetkin S et al. [Is there gender difference in infertile couples with no axis one psychiatric disorder in context of emotional symptoms, social support and sexual function?] Turk Psikiyatri Derg. 2007;18:311–322. [PubMed] [Google Scholar]
- 29.Kiesswetter M, Marsoner H, Luehwink A et al. Impairments in life satisfaction in infertility: Associations with perceived stress, affectivity, partnership quality, social support and the desire to have a child. Behav Med. 2020;46:130–141. doi: 10.1080/08964289.2018.1564897. [DOI] [PubMed] [Google Scholar]
- 30.Mao J, Guo HP, Wang J et al. Analysis of Related Factors of Coping Styles in Infertile Patients in Central China. Patient Prefer Adherence. 2022;16:1605–1612. doi: 10.2147/ppa.S364345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Matsubayashi H, Hosaka T, Izumi S et al. Emotional distress of infertile women in Japan. Hum Reprod. 2001;16:966–969. doi: 10.1093/humrep/16.5.966. [DOI] [PubMed] [Google Scholar]
- 32.Matsubayashi H, Hosaka T, Izumi S et al. Increased depression and anxiety in infertile Japanese women resulting from lack of husband’s support and feelings of stress. Gen Hosp Psychiatry. 2004;26:398–404. doi: 10.1016/j.genhosppsych.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 33.Noorbala AA, Ramezanzadeh F, Abedinia N et al. Psychiatric disorders among infertile and fertile women. Soc Psychiatry Psychiatr Epidemiol. 2009;44:587–591. doi: 10.1007/s00127-008-0467-1. [DOI] [PubMed] [Google Scholar]
- 34.Pinar G, Zeyneloglu HB. Quality of life, anxiety and depression in Turkish women prior to receiving assisted reproductive techniques. Int J Fertil Steril. 2012;6:1–12. [PMC free article] [PubMed] [Google Scholar]
- 35.Sadiq U, Rana F, Munir M. Marital Quality, Self-compassion and Psychological Distress in Women with Primary Infertility. Sex Disabil. 2022;40:167–177. doi: 10.1007/s11195-021-09708-w. [DOI] [Google Scholar]
- 36.Shafierizi S, Faramarzi M, Esmaelzadeh S et al. Does infertility develop posttraumatic growth or anxiety/depressive symptoms? Roles of personality traits, resilience, and social support. Perspect Psychiatr Care. 2022;58:2017–2028. doi: 10.1111/ppc.13023. [DOI] [PubMed] [Google Scholar]
- 37.Vo TM, Tran QTT, Le CV et al. Depression and associated factors among infertile women at Tu Du hospital, Vietnam: a cross-sectional study. Int J Womens Health. 2019;11:343–351. doi: 10.2147/ijwh.S205231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wischmann T, Stammer H, Scherg H et al. Psychosocial characteristics of infertile couples: a study by the ‘Heidelberg Fertility Consultation Service’. Hum Reprod. 2001;16:1753–1761. doi: 10.1093/humrep/16.8.1753. [DOI] [PubMed] [Google Scholar]
- 39.Karlidere T, Bozkurt A, Ozmenler KN et al. The influence of emotional distress on the outcome of in-vitro fertilization (IVF) and/or intracytoplasmic sperm injection (ICSI) treatment among infertile Turkish women. Isr J Psychiatry Relat Sci. 2008;45:55–64. [PubMed] [Google Scholar]
- 40.Kiani Z, Simbar M, Hajian S et al. The prevalence of depression symptoms among infertile women: a systematic review and meta-analysis. Fertil Res Pract. 2021;7:6. doi: 10.1186/s40738-021-00098-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.UNDP . New York: UNDP (United Nations Development Programme); 2022. Human Development Report 2021/2022. [Google Scholar]
- 42.Fisher JR, Hammarberg K. Psychological and social aspects of infertility in men: an overview of the evidence and implications for psychologically informed clinical care and future research. Asian J Androl. 2012;14:121–129. doi: 10.1038/aja.2011.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cousineau TM, Domar AD. Psychological impact of infertility. Best Pract Res Clin Obstet Gynaecol. 2007;21:293–308. doi: 10.1016/j.bpobgyn.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 44.Thanscheidt CL, Pätsch P, Rösner S et al. Psychological Aspects of Infertility – Results from an Actor–Partner Interdependence Analysis. Geburtshilfe Frauenheilkd. 2023;83:843–849. doi: 10.1055/a-2041-2831. [DOI] [PMC free article] [PubMed] [Google Scholar]