HIGHLIGHTS
-
•
The impact of anti-Muslim discrimination on health, an understudied topic, was examined
-
•
Discrimination against Muslim Americans increased exponentially since the 9/11/2001 attacks.
-
•
Findings indicated that societal and interpersonal forms of anti-Muslim discrimination were associated with depressive symptoms.
-
•
No associations were observed with dietary patterns, tobacco use, or alcohol consumption.
-
•
Further research is needed to examine additional health implications of anti-Muslim discrimination.
Keywords: Depression, health risk behaviors, Muslim Americans, South Asian Americans, islamophobia
Abstract
Introduction
Anti-Muslim discrimination in the U.S. has increased exponentially since 2001, but the impact of anti-Muslim discrimination has yet to be fully examined because of limited data available on this topic and population. The objectives of this study were to (1) examine the association between perceived anti-Muslim discrimination and health risk behaviors, with depressive symptoms as a potential mediator, among South Asian Muslim Americans and (2) examine the association between other forms of perceived discrimination and health risk behaviors, with depressive symptoms as a potential mediator, among South Asian Muslim Americans.
Methods
Data were collected using an online survey, which was disseminated on subscriber e-mail lists for organizations that serve South Asian or Muslim communities. Participants were asked about perceived discrimination, depressive symptoms, diet, physical activity, tobacco use, and alcohol consumption. Data were analyzed using structural equation modeling in Mplus 8.
Results
Societal anti-Muslim discrimination had a positive association with depressive symptoms (0.19, p<0.05), as did interpersonal anti-Muslim discrimination (0.20, p<0.05) and other forms of discrimination (0.22, p<0.05). None of the discrimination scales were associated with dietary patterns, tobacco use, or alcohol consumption.
Conclusions
Study results demonstrated a link between discrimination and depressive symptoms. Further research is needed to examine associations with other adverse health outcomes and potential buffers against discrimination.
INTRODUCTION
South Asian Americans (SAAs), who can trace their ancestry to Bangladesh, India, Pakistan, Nepal, Maldives, and Sri Lanka, are one of the fastest growing subgroups of Asian Americans in the U.S.1 Epidemiologic data on this population indicate a heightened risk for chronic diseases, specifically Type 2 diabetes (23.3%) and hypertension (men: 25.7%, women: 24.3%).2,3 Risk factors for these chronic conditions include a genetic predisposition, higher rates of central obesity, tobacco use, alcohol consumption, low physical activity, and diet.4, 5, 6 Researchers have focused on these risk factors for Type 2 diabetes and hypertension among SAAs, but a gap remains in our knowledge of discrimination as a contributing factor. Discrimination is particularly salient to the lived experiences and health of SAAs because they are the second largest ethnic group of Muslim Americans (MAs), a religious minority that faces frequent interpersonal and structural forms of anti-Muslim discrimination.7,8 This study examined the associations between discrimination and depressive symptoms and health risk behaviors among South Asian MAs (SAMAs).
South Asian and Muslim American Experiences With Discrimination
There is a long history of discrimination directed toward South Asians (SAs) and MAs in the U.S. Given the overlapping identities and shared experiences with discrimination, this section will provide an overview of discrimination directed toward SAs and MAs. Examples include immigration laws from the 1800s restricting immigrants from Asian countries on the basis of country of origin and sex, denial of U.S. citizenship to SAs and Muslims, miscegenation laws that barred interracial marriages, workplace discrimination, and hate crimes against individuals and houses of worship.9, 10, 11 Visible markers of identity (i.e., wearing of religious garments) have been implicated in targeted verbal and physical attacks against SAAs of all ethnic and religious backgrounds, most notably Muslim women who wear headscarves and Sikh men who wear turbans.12, 13, 14 Anti-Muslim discrimination is an additional facet of discrimination experienced by SAAs, including bias incidents directed toward Muslims and non-Muslim SAs.8 As defined through an adaptation of a dictionary definition of Islamophobia, anti-Muslim discrimination refers to an irrational fear of, aversion to, or discrimination against Islam or people who practice Islam and people perceived as being Muslim.15,16
The stigmatization of Muslims as inherently violent people, people opposed to Western values, and backward people has contributed to an increase in anti-Muslim discrimination since 2001. The U.S. Equal Employment Opportunity Commission reported a 250% increase in discrimination claims from MAs in the months after the September 11 attacks.17 Employment discrimination against Muslim, Sikh, Middle Eastern, and SA communities continued in the years after September 11, leading the U.S. Equal Employment Opportunity Commission to create a specific code to track employment discrimination against these groups and file lawsuits on behalf of some complainants (approximately 90 lawsuits).17 Along with workplace discrimination motivated by anti-Muslim discrimination, the Federal Bureau of Investigation has documented increased hate crimes, defined as criminal acts motivated by religious-based bias against an individual, residence, school, or place of worship against Muslims and people perceived as Muslims in the period after September 11 (481 reported incidents in 2001 compared with 28 in 2000) and during the 2016 election (307 in 2016 compared with 154 in 2014).7,18,19 Other examples of anti-Muslim discrimination include bullying of Muslim students and government surveillance and profiling of Muslim communities.20, 21, 22, 23, 24, 25, 26, 27 The diversity of SAMAs as related to ethnicity, nativity, and SES has important implications for experiences with intersectional discrimination beyond anti-Muslim discrimination.12,28,29 This is reflected in gendered anti-Muslim attacks on visibly Muslim women who are perceived as easy targets and stereotyped as being oppressed and unintelligent and government surveillance and profiling of Muslim men who are perceived as violent and national security threats.30 These examples illustrate oppressive systems (e.g., sexism, anti-Muslim discrimination) shaping the experiences of people with overlapping social identities (gender and faith). Other salient identities include generational trauma (trauma from the partition of India among older SAMAs) and SES, such as education level, occupation, English proficiency, and household income, which shape access to resources and experiences with discrimination.31, 32, 33
Stress, Discrimination, and Health
Chronic stress, such as discrimination, can cause significant health consequences owing to the body's physiologic response and related behavioral changes. Exposure to stressful stimuli can activate the hypothalamic–pituitary–adrenocortical axis, resulting in the release of stress hormones and increased blood glucose levels.34,35 Elevated levels of stress have been associated with a range of adverse medical outcomes, including preterm birth, low birth weight, and cardiovascular disease.36, 37, 38 Behavioral problems may also arise from stress, including psychological distress, insomnia, over- or undereating, fatigue, headaches, and substance abuse such as increased consumption of alcohol and other drugs.39,40 Other relevant factors in the pathway between discrimination and poor health include mental health, specifically depression and anxiety.41 Symptoms of depression may include poor dietary habits, low physical activity, and increased tobacco use and alcohol consumption. The cumulative effects of stress-related symptoms and resulting behavioral changes may increase the risk of developing Type 2 diabetes and hypertension.42
Research on the health implications of discrimination has demonstrated that it is associated with poor mental health outcomes among SAs and MAs and with poor dietary habits among SAAs.20,43, 44, 45, 46 Other studies have indicated that anti-Muslim discrimination is associated with preterm birth, low birth weight, and low healthcare utilization.47, 48, 49 Despite increasing anti-Muslim discrimination in the past 20 years, the impact of this particular form of discrimination has yet to be fully examined because of limited data on this topic and population.50,51
Study Aims
On the basis of previous research establishing a connection between anti-Muslim discrimination and poor mental health (e.g., depression) among MAs, this cross-sectional study assessed the patterns of discrimination linked to health risk behaviors for Type 2 diabetes and hypertension among SAMAs.20,52 Using structural equation modeling, symptoms of depression were examined as a potential mediator in the study models, given the potential direct impact of discrimination on depressive symptoms and the indirect impact of discrimination through depressive symptoms on health risk behaviors. Specifically, symptoms of depression may include increased alcohol consumption and tobacco use, poor dietary habits, and low physical activity, which can be indirectly shaped by discrimination.53 The research aims of this study were to (1) examine the association between perceived anti-Muslim discrimination and health risk behaviors, with depressive symptoms as a potential mediator, and (2) examine the association between other forms of perceived discrimination and health risk behaviors, with depressive symptoms as a potential mediator.
METHODS
Study Sample
Data were collected using an online survey developed on the Qualtrics platform. The study's recruitment strategy employed a convenience and snowball sampling approach to recruiting potential participants. The survey was disseminated on listservs and social media platforms for groups that serve SA or Muslim communities by the organization staff or the principal investigator. Participants were requested to forward the study invitation to their contacts. Questions were only available in English, and participation in the study was restricted to participants who self-identified as MA. Participants were offered the opportunity to enter a raffle for an iPad Air as an incentive, which was offered through a separate online form from the survey to ensure that participant responses were not linked to identifiable information required for the raffle.
A total of 347 MAs participated in the survey, and a subsample of SAMA participants was used for this study (n=173). Data were collected from May to July 2019.
Measures
General discrimination scale. The Everyday Discrimination Index (EDI) assesses perceived discriminatory treatment on the basis of a person's background. As described by William et al. in 1997, “The use of ‘perceived discrimination’ is not intended to dismiss or delegitimize the experiences of people who experience discrimination, but rather to reflect measurement challenges related to under- and overreporting of discriminatory incidents, and in some cases participants not knowing the motivation behind harsh or discriminatory actions.” The EDS begins by asking, In your day-to-day life, how often do any of the following things happen to you? Examples of instrument items include people act as if they're better than you and you're called names or insulted. The response scale for each item uses a 6-point Likert scale (range: almost everyday [5] to never [0]). After answering these items, participants selected the reason they felt they were treated in a discriminatory manner (e.g., ancestry, gender, religion). The average of index items was calculated because this approach is not affected by missing responses, unlike a total of item responses, which is influenced by missing responses.54 This scale has a Cronbach's alpha of 0.91 with Asian Americans.55 In this study, the EDI had a McDonald's omega estimate of 0.91, and principal component analysis indicated a 1-component model.
Perceived anti-Muslim discrimination. Anti-Muslim discrimination was assessed using 2 distinct scales: the Interpersonal Anti-Muslim Discrimination Index (IAMDI) and the Societal Anti-Muslim Discrimination Index (SAMDI).16 The IAMDI measures interpersonal incidents of anti-Muslim discrimination and begins by asking, We are interested in whether the following events ever happened to you, or you felt happened to you, because you are Muslim. Examples of instrument items include You have been physical attacked because you're Muslim and You are stopped for additional security screenings at the airport because you are Muslim. One scale item assesses intersectional discrimination as related to experiences with anti-Muslim discrimination and xenophobia (Someone tells you to ‘go back to your county’ or to ‘go back to where you came from’). Items are answered using a 6-point Likert scale (range: This event never happened to me [0] to This event happened and I was extremely upset).
The SAMDI assesses how Muslims are treated and perceived in the U.S. This begins by stating The following items are about how Muslims are treated and perceived in the U.S. Examples of index items include In the U.S., non-Muslims perceive Muslims as being dangerous and Muslim women who wear Islamic clothes are often harassed in public. One scale item addresses gendered anti-Muslim discrimination as directed toward Muslim women (In the U.S., non-Muslims perceive Muslim women as being oppressed). This index uses a 6-point Likert response scale (range: Strongly disagree [0] to Strongly agree [5]). Item responses were averaged, and each instrument was assessed individually. The McDonald's omega estimates of the anti-Muslim discrimination indexes in this study were 0.89 (SAMDI) and 0.75 (IAMDI). Principal component analysis for the indexes yielded 1-component models for both.
Health risk behaviors. A compilation of questions from the National Health Interview Survey, National Health and Nutrition Examination Survey, California Health Interview Survey, and Finnish Diabetes Risk Form were used to assess diet and physical activity.56, 57, 58 Respondents were asked how they would compare their exercise routine with those of others of their age (range: a lot more active [4] to a lot less active [0]) and how many days in the past 7 days they were active for at least 30 minutes. In relation to diet, respondents were asked to rate how healthy their diet is (range: excellent [4] to poor [0]) and how frequently they consume vegetables, fruit, fried foods, soda, and dessert weekly (range: 0 days to 7 days). Responses to questions regarding consumption of fruits and vegetables were averaged to create a healthy food variable and an unhealthy food variable created using the average of items regarding fried foods, soda, and dessert. The reliability of this combination of questions is unknown. The McDonald's omega estimate of the healthy food variable was low (0.62), as it was for the unhealthy food measure (0.56).
A total of 14 questions from the 2018 Centers for Disease Control and Prevention's National Health Interview Survey were used to assess current use of tobacco products.58 Culturally appropriate names for smokeless tobacco (e.g., paan, bidi, gutka, hookah) were added from a study on tobacco use among SAAs to capture the use of all forms of smokeless tobacco.6 Participants were asked how frequently (range: every day [4] to not at all [0]) they use each tobacco product and the highest response to these questions was selected as a measure of maximum tobacco use of any product. The tobacco use questions have a sensitivity ranging from 33.3% to 100% within SAAs.6
The first 2 questions from the 10-item self-reported Alcohol Use Disorders Identification Test were used to determine alcohol consumption patterns.59 Participants were asked how frequently they have an alcoholic drink (range: never [0] to 4 or more times a week [4]) and how many drinks they have in a typical sitting (range: 1 or 2 [0] to 10 or more [4]). Responses to these questions were used to calculate an estimate of monthly alcohol consumption.
Depressive symptoms scale. The 20-item Center for Epidemiologic Studies Depression Scale Revised (CESD-R) was used to assess depressive symptoms.60,61 Scale items include questions about common depressive symptoms (e.g., sadness, fatigue, agitation) (How often have you felt this way in the past week or so?). Each item is answered using a 5-point Likert scale (range: not at all or less than 1 day [0] to nearly everyday for 2 weeks [4]). The CESD-R has a Cronbach's alpha of 0.92 and was assessed as a factor in the analysis.62 Confirmatory factor analysis of the CESD-R in this study yielded poor fit indices (Root Mean Square Error of Approximation [RMSEA]=0.09, Comparative Fit Index [CFI]=0.79, Standardized Root Mean Square Residual [SRMR]=0.07), which may be due to the number of items in this scale. The CESD-R had a high-reliability estimate of 0.95 using the McDonald's omega estimate.
Covariates. Participants were asked close-ended questions regarding demographic traits: age, race/ethnicity, sex, education level, average household income, country of birth, nativity, years living in the U.S. for participants born outside of the U.S., health insurance status, and religious visibility as defined by the number of Islamic garments regularly worn in public (e.g., hijab, abaya, niqab, thobe). Participants had the option to skip any of the study questions (prefer not to answer or don't know/not sure), which were coded as missing.
Statistical Analysis
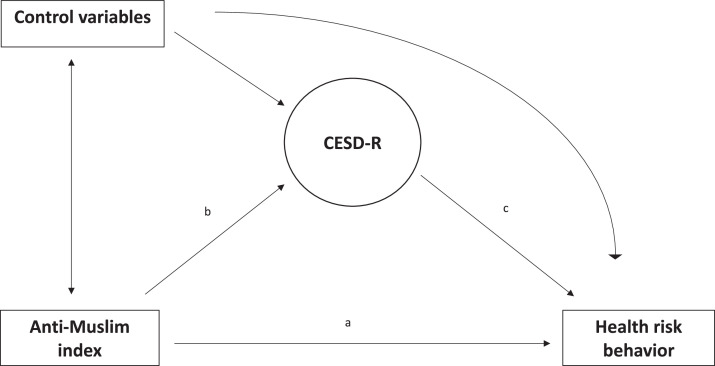
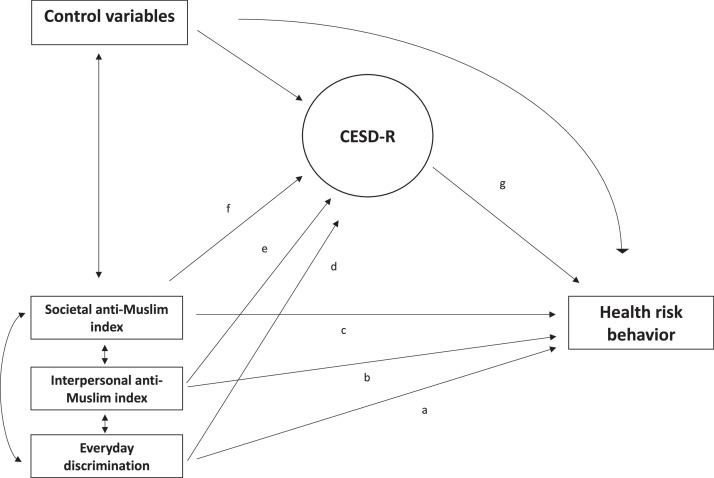
First, descriptive statistics were used to assess the sociodemographic characteristics of participants. Second, principal component analysis was used to examine index measures, and McDonald's omega estimate was used to determine the reliability of indexes. Finally, structural equation modeling was used to assess the association between anti-Muslim discrimination and health risk behaviors, with depressive symptoms as a potential mediator (Figure 1). The anti-Muslim indexes were included in the model separately and then simultaneously with the EDI (Figure 2).
Figure 1.
Study Model 1.
CESD-R, Center for Epidemiologic Studies Depression Scale Revised.
Figure 2.
Study Model 2.
CESD-R, Center for Epidemiologic Studies Depression Scale Revised.
Direct and mediated pathways were examined simultaneously in the path analysis. Health risk behaviors were assessed separately by type (physical activity, diet, tobacco use, alcohol consumption). Covariate variables included sociodemographic questions. Model fit was assessed using the following fit indices and thresholds: RMSEA (≤0.06), SRMR (≤0.08), and CFI (≥0.95).63 Missing data were included and accounted for using full information maximum likelihood. The Mplus MLR analysis option was used for all models because this form of maximum likelihood is robust to non-normality. Data were analyzed using SAS University, JASP 10.2, and Mplus 8.
Ethics
The University of Maryland, College Park's IRB approved this study on March 3, 2019. Consent was obtained using an electronic document on the first page of the online survey, which detailed the study objectives, potential risks and benefits of participation, and the contact information for the principal investigator; the University of Maryland, College Park's IRB; and telephone numbers for obtaining free, confidential counseling in case participants felt upset recollecting discriminatory encounters while answering survey questions.
RESULTS
Sample Demographics and Health Risk Behaviors
Demographic information of participants is detailed in Table 1. Most participants were aged 18–24 (27.8%) and 25–34 (38.2%) years and female (64.7%), most had some form of health insurance (89.6%), and most held a bachelor's degree or higher (85%).
Table 1.
Sample Demographics (n=173)
| Characteristic | n | % |
|---|---|---|
| Age, years | ||
| 18–24 | 48 | 27.8 |
| 25–34 | 66 | 38.2 |
| 35–44 | 36 | 20.8 |
| 45–54 | 11 | 6.4 |
| 55–64 | 5 | 2.9 |
| ≥65 | 7 | 4.1 |
| Prefer not to answer | 0 | 0 |
| Sex | ||
| Male | 60 | 34.7 |
| Female | 112 | 64.7 |
| Intersex | 0 | 0 |
| Other | 1 | 0.6 |
| Prefer not to answer | 0 | 0 |
| Education | ||
| Less than high school | 1 | 0.6 |
| High school/GED | 6 | 3.5 |
| Trade/technical/vocational | 0 | 0 |
| Some college | 13 | 7.5 |
| Associate degree | 6 | 3.5 |
| Bachelor's degree | 50 | 28.9 |
| Some postgraduate work | 12 | 6.9 |
| Master's degree | 54 | 31.2 |
| Professional or doctoral degree | 31 | 17.9 |
| Prefer not to answer | 0 | 0 |
| Household income ($) | ||
| <25,000 | 13 | 7.5 |
| 25,000<50,000 | 17 | 9.8 |
| 50,000<75,000 | 31 | 17.9 |
| 75,000<100,000 | 22 | 12.7 |
| 100,000<125,000 | 17 | 9.8 |
| 125,000<150,000 | 14 | 8.1 |
| ≥150,000 | 42 | 24.3 |
| Prefer not to answer | 17 | 9.8 |
| Health insurance | ||
| Yes | 155 | 89.6 |
| No | 14 | 8.1 |
| Prefer not to answer | 4 | 2.3 |
| Country of birth | ||
| The U.S. | 83 | 48 |
| Outside of the U.S. | 89 | 51.4 |
| Prefer not to answer | 1 | .6 |
| Years living in the U.S. (non–U.S.-born participants) (n=89), year | ||
| <1 | 1 | 1.1 |
| 1–3 | 6 | 6.7 |
| 4–6 | 7 | 7.8 |
| 7–9 | 6 | 6.7 |
| ≥10 | 70 | 77.8 |
| Prefer not to answer | 0 | 0 |
| Number of Islamic garments worn | ||
| 0 | 90 | 52 |
| 1 | 61 | 35.3 |
| 2 | 11 | 6.4 |
| 3 | 2 | 1.2 |
| 4 | 3 | 1.7 |
| 5 | 0 | 0 |
| 6 | 1 | .6 |
| 7 | 0 | 0 |
| 8 | 0 | 0 |
| Prefer not to answer | 5 | 2.9 |
Responses to diet, physical activity, tobacco use, and alcohol consumption are presented in Table 2. There was a range of responses to a question asking about physical activity in comparison with responses from other people of their age. The average consumption of healthy food was higher than that of unhealthy food. The prevalence of tobacco use and alcohol consumption was low in the sample.
Table 2.
Diet, Physical Activity, Tobacco Use, Alcohol Consumption, Discrimination, and CESD-R
| Measure | n or value |
|---|---|
| Exercise comparison | n=140 |
| A lot more active | 16 |
| A little more active | 29 |
| About as active | 37 |
| A little less active | 32 |
| A lot less active | 26 |
| Prefer not to answer | 0 |
| Physical activity in the past 7 days | n=140 |
| 7 | 13 |
| 6 | 5 |
| 5 | 20 |
| 4 | 15 |
| 3 | 27 |
| 2 | 18 |
| 1 | 11 |
| 0 | 23 |
| Prefer not to answer | 8 |
| Cigarettes | n=120 |
| Every day | 4 |
| Most days | 0 |
| Some days | 0 |
| Rarely | 2 |
| Not at all | 113 |
| Prefer not to answer | 1 |
| E-cigarettes | n=140 |
| Every day | 0 |
| Most days | 0 |
| Some days | 1 |
| Rarely | 5 |
| Not at all | 133 |
| Prefer not to answer | 1 |
| Cigars | n=140 |
| Every day | 0 |
| Most days | 0 |
| Some days | 0 |
| Rarely | 2 |
| Not at all | 136 |
| Prefer not to answer | 2 |
| Pipes | n=140 |
| Every day | 0 |
| Most days | 0 |
| Some days | 5 |
| Rarely | 9 |
| Not at all | 124 |
| Prefer not to answer | 2 |
| Smokeless | n=140 |
| Every day | 0 |
| Most days | 0 |
| Some days | 0 |
| Rarely | 1 |
| Not at all | 137 |
| Prefer not to answer | 2 |
| Self-rating of diet | n=140 |
| Excellent | 11 |
| Very good | 24 |
| Good | 60 |
| Fair | 37 |
| Poor | 7 |
| Prefer not to answer | 1 |
| Healthy food consumption in the past 7 days | |
| Range | 0–14 |
| Median | 10 |
| Mean | 9.18 |
| Unhealthy food consumption in the past 7 days | |
| Range | 0–21 |
| Median | 5 |
| Mean | 5.79 |
| Maximum use of any tobacco product | n=139 |
| Every day | 4 |
| Most days | 0 |
| Some days | 5 |
| Rarely | 9 |
| Not at all | 121 |
| Frequency of alcohol consumption | n=140 |
| ≥4 times a week | 2 |
| 2–3 times a week | 6 |
| 2–4 times a month | 8 |
| Monthly or less | 10 |
| Never | 113 |
| Prefer not to answer | 1 |
| Number of drinks consumed | n=140 |
| ≥10 | 0 |
| 7, 8, or 9 | 0 |
| 5 or 6 | 2 |
| 3 or 4 | 7 |
| 1 or 2 | 16 |
| 0 | 113 |
| Prefer not to answer | 2 |
| Monthly alcohol consumption | |
| Range | 0–99 |
| Median | 0 |
| Mean | 2.48 |
| Everyday discrimination | |
| Range | 0–45 |
| Median | 10 |
| Mean | 10.59 |
| Interpersonal anti-Muslim discrimination | |
| Range | 0–36 |
| Median | 9 |
| Mean | 9.95 |
| Societal anti-Muslim discrimination | |
| Range | 0–95 |
| Median | 61 |
| Mean | 54.74 |
| CESD-R | |
| Range | 0–80 |
| Median | 4 |
| Mean | 9.81 |
CESD-R, Center for Epidemiologic Studies Depression Scale Revised.
Perceived Anti-Muslim Discrimination and Health
Each anti-Muslim index was assessed individually with the health outcomes of interest. The first models examined the associations among interpersonal anti-Muslim discrimination, depressive symptoms, and health risk behaviors (Table 3 and Figure 1). Interpersonal anti-Muslim discrimination was positively associated with depressive symptoms (range of estimates=0.18–0.20, p<0.05), which was seen across all 7 models. Discrimination was not associated with physical activity, dietary patterns, tobacco use, or alcohol consumption. Discrimination had a positive, direct association with rating of diet (0.29, p<0.05) but had a negative mediated relation through CESD-R (−0.50, p<0.01).
Table 3.
Unstandardized (Standardized) Direct and Indirect Estimates of Interpersonal Anti-Muslim Discrimination (n=173)
| Dependent variables | CESD-Rb | Through CESD-Rc | RMSEA | CFI | SRMR |
|---|---|---|---|---|---|
| Exercise comparisona | |||||
| 0.15 (0.09) | 0.19 (0.28)* | −0.24 (−0.1) | 0.05 | 0.89 | 0.07 |
| Physical activity in the past 7 daysa | |||||
| 0.48 (0.17) | 0.18 (0.27)* | −0.09 (−0.02) | 0.05 | 0.88 | 0.07 |
| Self-rating of dieta | |||||
| 0.29 (0.22)* | 0.19 (0.27)* | −0.50 (−0.27)** | 0.05 | 0.87 | 0.07 |
| Healthy food consumption in the past 7 daysa | |||||
| −0.14 (−0.06) | 0.20 (0.29)* | −0.46 (−0.14) | 0.05 | 0.88 | 0.08 |
| Unhealthy food consumption in the past 7 daysa | |||||
| −0.15 (−0.09) | 0.19 (0.28)* | 0.46 (0.19) | 0.05 | 0.88 | 0.07 |
| Maximum use of tobacco producta | |||||
| −0.07 (−0.07) | 0.20 (0.30)** | −0.06 (−0.04) | 0.05 | 0.87 | 0.06 |
| Monthly alcohol consumptiona | |||||
| 1.42 (0.09) | 0.18 (0.27)* | −1.39 (−0.06) | 0.05 | 0.87 | 0.07 |
Note: Boldfaces indicate statistical significance (*p<0.05 and **p<0.01).
This table is the model depicted in Figure 1. Modification suggestions were employed to improve the overall fit of the model, specifically in regard to items in the CESD-R scale that are related to each other. These modification indices were implemented one by one and used for all study models.
See model path a in Figure 1.
See model path b in Figure 1.
See model path c in Figure 1.
CESD-R, Center for Epidemiologic Studies Depression Scale Revised; CFI, comparative fit index; RMSEA, root mean square error of approximation; SRMR, standardized root mean square residual.
Next, associations among societal anti-Muslim discrimination, depressive symptoms, and health risk behaviors were examined (Table 4 and Figure 2). Similar to the interpersonal anti-Muslim discrimination model results, societal forms of anti-Muslim discrimination were positively associated with depressive symptoms (range of estimates=0.17–0.19, p<0.05). Societal anti-Muslim discrimination was not associated with physical activity, diet, tobacco use, or alcohol consumption.
Table 4.
Unstandardized (Standardized) Direct and Indirect Estimates of Societal Anti-Muslim Discrimination (n=173)
| Dependent variables | CESD-Rb | Through CESD-Rc | RMSEA | CFI | SRMR |
|---|---|---|---|---|---|
| Exercise comparisona | |||||
| −0.23 (−0.12) | 0.17 (0.22) | −0.12 (−0.05) | 0.05 | 0.88 | 0.06 |
| Physical activity in the past 7 daysa | |||||
| −0.39 (−0.12) | 0.17 (0.22) | 0.27 (0.06) | 0.05 | 0.87 | 0.07 |
| Self-rating of dieta | |||||
| −0.08 (−0.05) | 0.17 (0.22) | −0.37 (−0.20) | 0.05 | 0.87 | 0.06 |
| Healthy food consumption in the past 7 daysa | |||||
| −0.34 (−0.13) | 0.18 (.22) | −0.44 (−0.13) | 0.05 | 0.87 | 0.08 |
| Unhealthy food consumption in the past 7 daysa | |||||
| 0.000 (0.000) | 0.17 (0.22) | 0.40 (0.17) | 0.05 | 0.87 | 0.07 |
| Maximum use of tobacco producta | |||||
| −0.004 (−0.003) | 0.19 (0.24) | 0.12 (−0.08) | 0.05 | 0.87 | 0.06 |
| Monthly alcohol consumptiona | |||||
| 1.80 (0.10) | 0.17 (0.21) | −1.66 (−0.08) | 0.05 | 0.86 | 0.07 |
Note: Boldfaces indicate statistical significance (p<0.05).
This table is related to Figure 1.
See model path a in Figure 1.
See model path b in Figure 1.
See model path c in Figure 1.
CESD-R, Center for Epidemiologic Studies Depression Scale Revised; CFI, comparative fit index; RMSEA, root mean square error of approximation; SRMR, standardized root mean square residual.
The model fit was moderate overall, with the RMESA being within the acceptable range (<0.06) for all models, most SRMR estimates within the ideal threshold <0.08, and CFI falling short of the accepted value (>0.95) across all models. The poor CFI estimates were most likely due to low correlations among the study variables because the CFI fit index is a comparison between the study model and null model where paths are nonsignificant, and weak study model correlations contribute to poor fit on this particular estimate.64
Other Forms of Discrimination and Health
In the final analysis, models were run using all 3 discrimination scales (EDI, IAMDI, and SAMDI) as independent variables to examine their associations with depressive symptoms and health risk behaviors (Table 5). The EDI had a positive association with depressive symptoms (range of estimates=0.20–0.22, p<0.05), but neither of the anti-Muslim indexes had significant paths with depressive symptoms. Societal anti-Muslim discrimination was related to reduced physical activity in comparison with the physical activity of other people of the participants’ ages (−0.42, p<0.05), but paths were nonsignificant for EDI and interpersonal anti-Muslim discrimination.
Table 5.
Unstandardized (Standardized) Direct and Indirect Estimates of Discrimination Indexes (n=173)
| Discrimination scales | Dependent variables | CESD-R | Through CESD-Rg | RMSEA | CFI | SRMR |
|---|---|---|---|---|---|---|
| Exercise comparison | ||||||
| — | — | −0.25 (−0.10) | 0.05 | 0.87 | 0.06 | |
| Everydaya | 0.16 (0.11) | 0.21d(0.37)* | — | — | — | — |
| Interpersonalb | 0.22 (0.13) | 0.02e (0.03) | — | — | — | — |
| Societalc | −0.42 (−0.21)* | 0.04f (0.06) | — | — | — | — |
| Physical activity in the past 7 days | ||||||
| — | — | −0.24 (−0.05) | 0.05 | 0.86 | 0.07 | |
| Everydaya | 0.70 (0.28)* | 0.20d(0.35)* | — | — | — | — |
| Interpersonalb | 0.39 (0.13) | 0.02e (0.03) | — | — | — | — |
| Societalc | −0.94 (−0.28)** | 0.04f (0.05) | — | — | — | — |
| Self-rating of diet | ||||||
| — | — | −0.50 (−0.27)** | 0.05 | 0.86 | 0.07 | |
| Everydaya | 0.10 (0.09) | 0.21d(0.36)* | — | — | — | — |
| Interpersonalb | 0.36 (0.28)* | 0.02e (0.03) | — | — | — | — |
| Societalc | −0.32 (−0.21)* | 0.04f (0.05) | — | — | — | — |
| Healthy food consumption in the past 7 days | ||||||
| — | — | −0.55 (−0.17) | 0.05 | 0.86 | 0.08 | |
| Everydaya | 0.39 (0.21) | 0.21d(0.37)* | — | — | — | — |
| Interpersonalb | −0.19 (−0.08) | 0.02e (0.03) | — | — | — | — |
| Societalc | −0.44 (−0.17) | 0.05f (0.06) | — | — | — | — |
| Unhealthy food consumption in the past 7 days | ||||||
| — | — | 0.55 (0.23) | 0.05 | 0.86 | 0.07 | |
| Everydaya | −0.24 (−0.17) | 0.22d(0.38)* | — | — | — | — |
| Interpersonalb | −0.05 (−0.03) | 0.02e (0.03) | — | — | — | — |
| Societalc | 0.13 (0.07) | 0.04f (0.06) | — | — | — | — |
| Max use of tobacco product | ||||||
| — | — | −0.02 (−0.01) | 0.05 | 0.86 | 0.06 | |
| Everydaya | −0.07 (−0.08) | 0.21d(0.37)* | — | — | — | —- |
| Interpersonalb | −0.02 (−0.02) | 0.02e (0.04) | — | — | — | — |
| Societalc | 0.02 (0.02) | 0.05f (0.06) | — | — | — | — |
| Monthly alcohol consumption | ||||||
| — | — | −2.40 (−0.11) | 0.05 | 0.85 | 0.07 | |
| Everydaya | 2.64 (0.21) | 0.20d(0.36)* | — | — | — | — |
| Interpersonalb | −0.49 (−0.03) | 0.02e (0.03) | — | — | — | — |
| Societalc | 0.67 (0.04) | 0.04f (0.05) | — | — | — | — |
Note: Boldfaces indicate statistical significance (*p<0.05 and **p<0.01).
This table is the model depicted in Figure 2.
See model path a in Figure 2.
See model path b in Figure 2.
See model path c in Figure 2.
See model path d in Figure 2.
See model path e in Figure 2.
See model path f in Figure 2.
See model path g in Figure 2.
CESD-R, Center for Epidemiologic Studies Depression Scale Revised; CFI, comparative fit index; RMSEA, root mean square error of approximation; SRMR, standardized root mean square residual.
EDI was associated with physical activity (0.70, p<0.05), whereas exposure to societal anti-Muslim discrimination was negatively associated with physical activity (−0.94, p<0.05). Exposure to interpersonal anti-Muslim discrimination had a direct positive association with rating of diet (0.36, p<0.05), but societal anti-Muslim discrimination was negatively associated with rating of diet (−0.32, p<0.05). Discriminatory incidents had a negative-mediated pathway through depressive symptoms on the rating of diet (−0.50, p<0.05). None of the discrimination scales were associated with dietary patterns, tobacco use, or alcohol consumption. The fit indices of models were moderate overall. The RMSEA estimates were within the excellent range, SRMR values were acceptable for most of the models, and CFI estimates were low as expected given low model variable correlations.
DISCUSSION
The study findings yielded mixed results in terms of the associations between discrimination and health outcomes. Exposure to interpersonal and societal forms of anti-Muslim discrimination was associated with depressive symptoms, which has been confirmed in prior studies on SAs and MAs.20,46 Interpersonal anti-Muslim discrimination was associated with rating of diet. However, interpersonal discrimination was not associated with dietary patterns, and this association was partially mediated by depressive symptoms; therefore, this atypical association may be due to other factors beyond the scope of this study. Neither form of anti-Muslim discrimination was associated with dietary patterns, tobacco use, or alcohol consumption. These nonsignificant results may be due to the extremely low prevalence of these health risk behaviors in the sample and insufficient power to detect significant associations. Prior research has indicated generational differences in tobacco use among SAs, and because this sample was primarily younger, this may explain the low prevalence of tobacco use.65 Underreporting may be a factor as well owing to religious prohibitions against consumption of alcohol.
In models assessing other forms of discrimination, the inclusion of 3 distinct discrimination scales resulted in interesting findings. The EDI was associated with depressive symptoms, but significant associations were not seen with either anti-Muslim discrimination index. Structural differences between the scales may explain varying relations in the model paths because the EDI first asks about experiences with mistreatment and then the primary reason why the participants felt that they were mistreated. This 2-step approach allows participants to think of mistreatment generally without a specific impetus behind incidents, which may reflect an indirect measure of perceived intersectional discrimination.66 Given that the sum of intersectional discrimination will have a greater impact than a specific form of discrimination, these results were expected.28 This finding may reflect the overlapping social identities of SAMAs (e.g., immigration status, ethnicity, socioeconomic level) and resulting experiences with intersectional discrimination.
Other notable results from the models include societal anti-Muslim discrimination being associated with a decline in physical activity in comparison with those of others of the same age as the participant and physical activity in the past 7 days, which partially confirms that discrimination is associated with health risk behaviors. The lack of significant associations between interpersonal anti-Muslim discrimination and physical activity may be explained by the pervasiveness of societal anti-Muslim discrimination at all levels of American society and, as a result, its greater impact on Muslims. Conversely, the EDI was associated with physical activity in the past 7 days. The positive association between the EDI and physical activity is unexpected and may be explained by the moderating effects of beneficial coping mechanisms.
The negative associations between depressive symptoms and diet and discrimination and diet were expected on the basis of the literature regarding harmful coping mechanisms arising from discrimination.39,67 However, the positive association between interpersonal discrimination and rating of diet was unusual and not supported by past studies. It should be noted that none of the discrimination scales were associated with dietary patterns; therefore, the significant associations between discrimination and rating of diet should be interpreted with caution.
This study advances our understanding of the health implications of anti-Muslim discrimination by focusing on a particular ethnic group of MAs and examining health risk behaviors and mental health outcomes. Findings from this study confirm those of previous results establishing a link between anti-Muslim discrimination and poor mental health.20,68 Although paths between discrimination and health risk behaviors were nonsignificant, these results do not preclude an association between anti-Muslim discrimination and poor health because future studies may establish a link. It is important to note that the study sample has high SES in terms of education levels, household income, and health insurance and is relatively young. These factors may mitigate potential health risk behaviors arising from discrimination because of knowledge regarding healthy coping mechanisms, access to supportive resources (e.g., health care, including behavioral health services and social networks), and the ability to understand and navigate stressful situations. Cardiovascular risk is high among SAs, so there is the possibility that despite access to resources and healthy behaviors, SAs may still experience poor health outcomes.
Limitations
This is one of the few studies to examine the associations between anti-Muslim discrimination and health risk behaviors among SAMAs and serves as an important first step in assessing the health implications of anti-Muslim discrimination. Given the diversity of MAs, it is critical that researchers focus on a specific group of Muslims (by race/ethnicity, gender, nativity) in recognition of the varying health concerns and experiences with discrimination. The use of scales specifically for measuring anti-Muslim discrimination is a strength of this study because it provides a direct examination of anti-Muslim discrimination and how this particular form of bias can be harmful.
Limitations of this study include the use of an online survey to collect data and the survey only being offered in English, which restricts participation to English-proficient participants with Internet access. This has significant implications for the experiences reflected among study participants because SAMAs with limited English proficiency and Internet access may have varying experiences with discrimination, navigating healthcare systems, and specific health needs. Another limitation is that although poor diet, low physical activity, tobacco use, and alcohol consumption can be symptoms of depression, these health risk behaviors can occur on their own. Furthermore, the use of self-reported data and recruitment of a convenience sample contributed to bias in the data and a nonrepresentative sample of SAMAs. Given the challenges of recruiting a random, representative sample of a minority population that makes up only 1.1% of the total U.S. population and the absence of religious affiliation questions in national health surveys, research on MAs may be restricted to convenience samples for the time being.8 Finally, there is a significant amount of within-group diversity among SAMAs. The heterogeneity of SAMAs is seen in varying socioeconomic levels and health outcomes.4,69, 70, 71, 72 The challenges of achieving a sufficient sample size for 1 subethnic population led to the aggregate sampling strategy for this study.50
CONCLUSIONS
Increasing available data on MAs and corresponding disaggregated data on ethnic groups (e.g., SAs, African, and Arab Americans) are crucial for furthering our understanding of anti-Muslim discrimination. National health data sets rarely ask participants about their religious affiliation. The inclusion of a religious identity question in national health surveys would not only facilitate research on MAs but will also facilitate studies on religious-based discrimination in general because Muslims and other minority groups (e.g., Jewish and Sikh Americans) are facing an increase in hate crimes.19,73
The case for adding this question is tied to the need for expanding our conceptualization of health disparity populations, which, as defined by the National Institute on Minority Health and Health Disparities, includes racial/ethnic minorities, underserved rural populations, socioeconomically disadvantaged populations, sexual and gender minorities, and populations characterized by ≥2 of these descriptors.74 Given the increase in hate crimes against Muslims, Jews, and Sikhs and the established link between discrimination and poor health, it is imperative that religious minority groups be added to the list of health disparity populations to solicit the resources needed to understand health disparities among religious minorities.
Considerations for future studies on anti-Muslim discrimination include examining other psychosocial outcomes (e.g., anxiety, anger) and health risk behaviors associated with discrimination and continuing to examine other health outcomes (e.g., preterm birth, hypertension, anxiety) that may arise from anti-Muslim discrimination. Other factors to consider include intersectional discrimination given the overlapping social identities of MAs and resulting experiences with multiple systems of oppression (e.g., sexism, racism, xenophobia, anti-Muslim discrimination).24
Another important area of further inquiry is potential buffers to discrimination, which is an overlooked gap in much of the literature. Long-term solutions to addressing discrimination, such as policies to support and protect minority communities, will take time to implement. In the meantime, it is vital that interventions to counter the harmful impacts of discrimination be enacted. To design effective interventions, potential buffers to discrimination must be identified and assessed, such as social support, identity formation, and mental health services. Considering the various environments where bias incidents take place (e.g., schools, workplaces, neighborhoods), interventions should be developed and tested for a variety of locations. Drawing attention to the impact of anti-Muslim discrimination on MAs is critical, as is offering solutions to mitigate the harmful impacts of anti-Muslim discrimination.
Despite the known linkages between discrimination and health, our understanding of the health implications of anti-Muslim discrimination is limited. MAs have dealt with anti-Muslim discrimination for decades without any substantial support or understanding of their experiences. The time for improving our knowledge of the health implications of anti-Muslim discrimination and designing and implementing interventions to support MAs is long overdue. Combating bigotry is a long-term objective requiring a significant investment of time and resources, and the public health field can contribute to these initiatives through research drawing attention to the harmful impacts of discrimination and evaluating the efficacy of interventions to support stigmatized communities.
CRediT authorship contribution statement
Naheed Ahmed: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Funding acquisition. Nadia S. Islam: Writing – review & editing.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Gregory R. Hancock for his guidance on the statistical analysis. We are grateful for the assistance of community- and faith-based organizations in disseminating the survey among their members. Finally, we extend our sincere gratitude and appreciation to the participants for their time and participation in this study.
This study was funded by a grant from the University of Maryland Graduate School (College Park, MD). NI’s time is partially supported by the NIH; National Institute of Diabetes and Digestive and Kidney Diseases (grants R01DK110048-01A1; R18DK110740 and P30DK111022R01DK11048); National Institute on Minority Health and Health Disparities (grant U54MD000538); National Heart, Lung, and Blood Institute (grant 1UG3HL151310); National Center for Advancing Translational Science (grant UL1TR001445); and Centers for Disease Control and Prevention (grant U48DP001904). The views expressed are those of the authors and do not necessarily represent the official position of the funding organizations.
Declaration of interest: None.
REFERENCES
- 1.Budiman A, Ruiz NG. Key facts about Asian Americans, a diverse and growing population. Pew Res Center. 2017 https://www.pewresearch.org/short-reads/2021/04/29/key-facts-about-asian-americans/ [Google Scholar]
- 2.Cheng YJ, Kanaya AM, Araneta MRG, et al. Prevalence of diabetes by race and ethnicity in the United States, 2011–2016. J Am Med Assoc. 2019;322(24):2389–2398. doi: 10.1001/jama.2019.19365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao B, Jose PO, Pu J, et al. Racial/ethnic differences in hypertension prevalence, treatment, and control for outpatients in northern California 2010–2012. Am J Hypertens. 2015;28(5):631–639. doi: 10.1093/ajh/hpu189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gujral UP, Pradeepa R, Weber MB, Narayan KMV, Mohan V. Type 2 diabetes in South Asians: similarities and differences with white Caucasian and other populations. Ann N Y Acad Sci. 2013;1281(1):51–63. doi: 10.1111/j.1749-6632.2012.06838.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iwamoto D, Takamatsu S, Castellanos J. Binge drinking and alcohol-related problems among U.S.-born Asian Americans. Cult Divers Ethn Minor Psychol. 2012;18(3):219–227. doi: 10.1037/a0028422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manderski MTB, Steinberg MB, Rahi KN, Banerjee SC, Delnevo CD. Surveillance of tobacco use among South Asians in the US: are we underestimating prevalence? J Community Health. 2016;41(6):1140–1145. doi: 10.1007/s10900-016-0226-2. 2016/12// [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kishi K. Anti-Muslim assaults reach 9/11-era levels, FBI data show. Pew Res Center. 2016 https://www.pewresearch.org/short-reads/2016/11/21/anti-muslim-assaults-reach-911-era-levels-fbi-data-show/ [Google Scholar]
- 8.Mohamed B. A new estimate of U.S. Muslim population. Pew Res Center. 2018 https://www.pewresearch.org/short-reads/2016/01/06/a-new-estimate-of-the-u-s-muslim-population/ [Google Scholar]
- 9.Joshi KY. The racialization of Hinduism, Islam, and Sikhism in the united states. Equity Excell Educ. 2006;39(3):211–226. doi: 10.1080/10665680600790327. [DOI] [Google Scholar]
- 10.Ngai MM. The architecture of race in American immigration law: A reexamination of the Immigration Act of 1924. J Am Hist. 1999;86(1):67–92. doi: 10.2307/2567407. [DOI] [Google Scholar]
- 11.Sohoni D. Unsuitable suitors: anti-miscegenation laws, naturalization laws, and the construction of Asian identities. Law Soc Rev. 2007;41(3):587–618. doi: 10.1111/j.1540-5893.2007.00315.x. [DOI] [Google Scholar]
- 12.Ahluwalia MKMK, Pellettiere L. Sikh men post-9/11: misidentification, discrimination, and coping. Asian Am J Psychol. 2010;1(4):303–314. doi: 10.1037/a0022156. [DOI] [Google Scholar]
- 13.Ghumman S, Jackson L. The downside of religious attire: the Muslim headscarf and expectations of obtaining employment. J Organiz Behav. 2010;31(1):4–23. doi: 10.1002/job.601. [DOI] [Google Scholar]
- 14.Ghumman S, Ryan AM. Not welcome here: discrimination towards women who wear the Muslim headscarf. Hum Relat. 2013;66(5):671–698. doi: 10.1177/0018726712469540. [DOI] [Google Scholar]
- 15.Merriam-Webster. Definition of Islamophobia Merriam-Webster; 2009. https://www.merriam-webster.com/dictionary/Islamophobia. 2009. Accessed November 15, 2018.
- 16.Ahmed N. Measurement of perceived interpersonal and societal anti-Muslim discrimination in the United States. Assessment. 2021;28(2):668–681. doi: 10.1177/1073191120973388. [DOI] [PubMed] [Google Scholar]
- 17.EEOC . U.S. Equal Employment Opportunity Commission; 2023. What you should know about the EEOC and religious and national origin discrimination involving the Muslim, Sikh, Arab, Middle Eastern and South Asian communities.https://www.eeoc.gov/wysk/what-you-should-know-about-eeoc-and-religious-and-national-origin-discrimination-involving Accessed November 15, 2018. [Google Scholar]
- 18.Disha I, Cavendish JC, King RD. Historical events and spaces of hate: hate crimes against Arabs and Muslims in post-9/11 America. Soc Probl. 2011;58(1):21–46. doi: 10.1525/sp.2011.58.1.21. [DOI] [Google Scholar]
- 19.FBI . 2016. 2016 Hate Crime Statistics Released. [Google Scholar]
- 20.Amer MM, Bagasra A. Psychological research with Muslim Americans in the age of Islamophobia: trends, challenges, and recommendations. Am Psychol. 2013;68(3):134–144. doi: 10.1037/a0032167. [DOI] [PubMed] [Google Scholar]
- 21.Bhattarai N, Charlton J, Rudisill C, Gulliford MC. PS28 impact of number and type of comorbidity on depression prevalence and health care costs. Population-based cohort study. J Epidemiol Community Health. 2012;66(suppl 1):A49.2–A4A49. doi: 10.1136/jech-2012-201753.127. [DOI] [Google Scholar]
- 22.Lajevardi N, Oskooii KAR. Old-fashioned racism, contemporary Islamophobia, and the isolation of Muslim Americans in the age of trump. J Race Ethnicity Politics. 2018;3(1):112–152. doi: 10.1017/rep.2017.37. [DOI] [Google Scholar]
- 23.Nadal KL, Griffin KE, Hamit S, Leon J, Tobio M, Rivera DP. Subtle and overt forms of Islamophobia: microaggressions toward Muslim Americans. J Muslim Ment Health. 2012;6(2):15–37. doi: 10.3998/jmmh.10381607.0006.203. [DOI] [Google Scholar]
- 24.Ahmed N, Quinn SC, Limaye RJ, Khan S. From interpersonal violence to institutionalized discrimination: documenting and assessing the impact of Islamophobia on Muslim American. J Muslim Ment Health. 2021;15(2) doi: 10.3998/jmmh.119. [DOI] [Google Scholar]
- 25.Alimahomed-Wilson S. When the FBI knocks: Racialized State surveillance of Muslims. Crit Sociol. 2019;45(6):871–887. doi: 10.1177/0896920517750742. [DOI] [Google Scholar]
- 26.Newburgh Four: poor, black, and jailed under FBI ‘entrapment’ tactics, The Guardian, 2011, New City: York. Accessed November 15, 2018.
- 27.U.S. Department of Justice. Office of the Inspector General . 2008. A review of the FBI's use of national security letters: assessment of corrective actions and examination of NSL usage in 2006; pp. 1–157. [Google Scholar]
- 28.Crenshaw K. Demarginalizing the intersection of Race and sex: a black feminist critique of antidiscrimination doctrine. Univ Chic Leg Forum. 1989 http://chicagounbound.uchicago.edu/uclfhttp://chicagounbound.uchicago.edu/uclf/vol1989/iss1/8 [Google Scholar]
- 29.Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev. 1991;43(6):1241. doi: 10.2307/1229039. [DOI] [Google Scholar]
- 30.Center Stage HJ . In: Islamophobia in America: the Anatomy of Intolerance. Ernst C, editor. Palgrave MacMillan; 2013. Gendered Islamophobia and Muslim women; pp. 107–144. [Google Scholar]
- 31.Ross CE, Wu C-l. The links between education and health. Am Sociol Rev. 1995;60(5):719–745. doi: 10.2307/2096319. [DOI] [Google Scholar]
- 32.Saydah SH, Imperatore G, Beckles GL. Socioeconomic status and mortality: contribution of health care access and psychological distress among U.S. adults with diagnosed diabetes. Diabetes Care. 2013;36(1):49–55. doi: 10.2337/dc11-1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82(6):816–820. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berger M, Sarnyai Z. “More than skin deep”: stress neurobiology and mental health consequences of racial discrimination. Stress. 2015;18(1):1–10. doi: 10.3109/10253890.2014.989204. [DOI] [PubMed] [Google Scholar]
- 35.Wells S, Tremblay PF, Flynn A, et al. Associations of hair cortisol concentration with self-reported measures of stress and mental health-related factors in a pooled database of diverse community samples. Stress. 2014;17(4):334–342. doi: 10.3109/10253890.2014.930432. [DOI] [PubMed] [Google Scholar]
- 36.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92(4):615–623. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schneiderman N, Ironson G, Siegel SD. Stress and health: psychological, behavioral, and biological determinants. Annu Rev Clin Psychol. 2005;1:607–628. doi: 10.1146/annurev.clinpsy.1.102803.144141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Curr Dir Psychol Sci. 2004;13(5):206–209. doi: 10.1111/j.0963-7214.2004.00309.x. [DOI] [Google Scholar]
- 41.Hodge DR, Zidan T, Husain A. Depression among Muslims in the United States: examining the role of discrimination and spirituality as risk and protective factors. Soc Work. 2016;61(1):45–52. doi: 10.1093/sw/swv055. : Table 1. [DOI] [PubMed] [Google Scholar]
- 42.Detka J, Kurek A, Basta-Kaim A, Kubera M, Lasoń W, Budziszewska B. Neuroendocrine link between stress, depression and diabetes. Pharmacol Rep. 2013;65(6):1591–1600. doi: 10.1016/s1734-1140(13)71520-2. [DOI] [PubMed] [Google Scholar]
- 43.Nadimpalli SB, Dulin-Keita A, Salas C, Kanaya AM, Kandula NR. Associations between discrimination and cardiovascular health among Asian Indians in the United States. J Immigr Minor Health. 2016;18(6):1284–1291. doi: 10.1007/s10903-016-0413-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nadimpalli S, Keita A, Wang J, et al. Are experiences of discrimination related to poorer dietary intakes among South Asians in the MASALA study? J Nutr Educ Behav. 2017;49(10):872–876.e1. doi: 10.1016/j.jneb.2017.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nadimpalli SB, Cleland CM, Hutchinson MK, Islam N, Barnes LL, Van Devanter N. The association between discrimination and the health of Sikh Asian Indians. Health Psychol. 2016;35(4):351–355. doi: 10.1037/hea0000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nadimpalli SB, Kanaya AM, McDade TW, Kandula NR. Self-reported discrimination and mental health among Asian indians: cultural beliefs and coping style as moderators. Asian Am J Psychol. 2016;7(3):185–194. doi: 10.1037/aap0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lauderdale DS. Birth outcomes for Arabic-named women in California before and after September 11. Demography. 2006;43(1):185–201. doi: 10.1353/dem.2006.0008. [DOI] [PubMed] [Google Scholar]
- 48.Samari G, Catalano R, Alcalá HE, Gemmill A. The Muslim Ban and preterm birth: analysis of U.S. vital statistics data from 2009 to 2018. Soc Sci Med. 2020;265 doi: 10.1016/j.socscimed.2020.113544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Samuels EA, Orr L, White EB, et al. Health care utilization before and after the “Muslim Ban” executive order among people born in Muslim-majority countries and living in the US. JAMA Netw Open. 2021;4(7) doi: 10.1001/jamanetworkopen.2021.18216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shah NS, Kandula NR. Addressing Asian American misrepresentation and underrepresentation in research. Ethn Dis. 2020;30(3):513–516. doi: 10.18865/ed.30.3.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Samari G, Alcalá HE, Sharif MZ. Islamophobia, health, and public health: A systematic literature review. Am J Public Health. 2018;108(6):e1–e9. doi: 10.2105/AJPH.2018.304402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abu-Ras W, Ahmed S, Arfken CL. Alcohol use among U.S. Muslim College students: risk and protective factors. J Ethn Subst Abuse. 2010;9(3):206–220. doi: 10.1080/15332640.2010.500921. [DOI] [PubMed] [Google Scholar]
- 53.Ahmed N, De Silva D, Kanaya AM, Kandula NR. Psychological symptoms as mediators in the association between discrimination and health among South Asian Americans. J Asian Health. 2022;2(1) [PMC free article] [PubMed] [Google Scholar]
- 54.Pett MA, Lackey NR, Sullivan JJ. Sage Publications; Thousand Oaks, CA: 2003. Making sense of factor analysis : the use of factor analysis for instrument development in health care research. p. 348–348. [Google Scholar]
- 55.Gee GC, Spencer M, Chen J, Yip T, Takeuchi DT. The association between self-reported racial discrimination and 12-month DSM-IV mental disorders among Asian Americans nationwide. Soc Sci Med. 2007;64(10):1984–1996. doi: 10.1016/j.socscimed.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.UCLA Center for Health Research . UCLA Center for Health Research; Los Angeles, CA: 2018. California Health Interview Survey: sample design. [Google Scholar]
- 57.Zhang L, Zhang Z, Zhang Y, Hu G, Chen L. Evaluation of Finnish diabetes risk score in screening undiagnosed diabetes and prediabetes among U.S. adults by gender and race: NHANES 1999–2010. PLoS One. 2014;9(5):e97865. doi: 10.1371/journal.pone.0097865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta, GA: 2018. National Health Interview Survey. [Google Scholar]
- 59.World Health Organization . World Health Organization; Geneva, Switzerland: 2001. AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. [Google Scholar]
- 60.Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A. In: The use of pshychological testing for treatment planning and outcomes assessment: instruments for adults. Maruish ME, editor. Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 2004. Center for Epidemiologic Studies Depression Scale: Review and Revision (CESD and CESD-R) pp. 366–377. [Google Scholar]
- 61.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 62.Van Dam NT, Earleywine M. Validation of the Center for Epidemiologic Studies Depression Scale—revised (CESD-R): pragmatic depression assessment in the general population. Psychiatry Res. 2011;186(1):128–132. doi: 10.1016/j.psychres.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 63.Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 64.Hooper D, Coughlan J, Mullen MR. Structural equation modelling: guidelines for determining model fit. Electron J Bus Res Methods. 2008;6(1):53–60. [Google Scholar]
- 65.Hrywna M, Jane Lewis M, Mukherjea A, Banerjee SC, Steinberg MB, Delnevo CD. Awareness and use of South Asian tobacco products among South Asians in New Jersey. J Community Health. 2016;41(6):1122–1129. doi: 10.1007/s10900-016-0208-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Harnois CE, Bastos JL, Shariff-Marco S. Intersectionality, contextual specificity, and everyday discrimination: assessing the difficulty associated with identifying a main reason for discrimination among racial/ethnic minority respondents. Sociol Methods Res. 2022;51(3):983–1013. doi: 10.1177/0049124120914929. [DOI] [Google Scholar]
- 67.Druss BG. Chair RC, walker ER. Mental Disorders and Medical Comorbidity. http://www.integration.samhsa.gov/workforce/mental_disorders_and_medical_comorbidity.pdf. 2011. Accessed November 15, 2018. [PubMed]
- 68.Abu-Ras WM, Suarez ZE. Muslim men and women's perception of discrimination, hate crimes, and PTSD symptoms post 9/11. Traumatology. 2009;11(3):48–63. doi: 10.1177/1534765609342281. September. [DOI] [Google Scholar]
- 69.Gujral UP, Narayan KMV, Kandula NR, Liu K, Kanaya AM. Incidence of diabetes and prediabetes and predictors of glycemic change among South Asians in the USA: the MASALA study. BMJ Open Diabetes Res Care. 2020;8(1) doi: 10.1136/bmjdrc-2019-001063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gujral UP, Narayan KMV, Pradeepa RG, et al. Comparing Type 2 diabetes, prediabetes, and their associated risk factors in Asian indians in India and in the U.S.: the CARRS and MASALA studies. Diabetes Care. 2015;38(7):1312–1318. doi: 10.2337/dc15-0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gupta R, Guptha S, Sharma KK, Gupta A, Deedwania P. Regional variations in cardiovascular risk factors in India: India heart watch. World J Cardiol. 2012;4(4):112–120. doi: 10.4330/wjc.v4.i4.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pew research C. The Rise of Asian Americans. http://www.pewsocialtrends.org/2012/06/19/the-rise-of-asian-americans/. 2013. Accessed on November 15, 2018.
- 73.Tessler H, Choi M, Kao G. The anxiety of being Asian American: hate crimes and negative biases during the COVID-19 pandemic. Am J Crim Justice. 2020;45(4):636–646. doi: 10.1007/s12103-020-09541-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The National Institute on Minority Health and Health Disparities research framework. Am J Public Health. 2019;109(suppl 1):S16–S20. doi: 10.2105/AJPH.2018.304883. [DOI] [PMC free article] [PubMed] [Google Scholar]