Summary
Coverage of migrant and refugee data is incomplete and of insufficient quality in European health information systems. This is not because we lack the knowledge or technology. Rather, it is due to various political factors at local, national and European levels, which hinder the implementation of existing knowledge and guidelines. This reflects the low political priority given to the topic, and also complex governance challenges associated with migration and displacement. We review recent evidence, guidelines, and policies to propose four approaches that will advance science, policy, and practice. First, we call for strategies that ensure that data is collected, analyzed and disseminated systematically. Second, we propose methods to safeguard privacy while combining data from multiple sources. Third, we set out how to enable survey methods that take account of the groups’ diversity. Fourth, we emphasize the need to engage migrants and refugees in decisions about their own health data. Based on these approaches, we propose a change management approach that narrows the gap between knowledge and action to create healthcare policies and practices that are truly inclusive of migrants and refugees. We thereby offer an agenda that will better serve public health needs, including those of migrants and refugees and advance equity in European health systems.
Funding
No specific funding received.
Keywords: Health information system, Health policy, Migration, Data linkage, Health monitoring surveys, Health equity
Introduction
Health systems have faced challenges in keeping up1 with the increasing global movement of people.2 Unfortunately, migrants and refugees have often been overlooked in discussions about health policies.3, 4, 5 The COVID-19 pandemic brought attention to deep inequalities, with migrants and refugees being particularly disadvantaged,6,7 emphasizing the need for detailed health data that considers the diversity within populations.8 However, only less than half of the countries in the WHO European Region were able to collect or properly analyze health data based on migratory or refugee status by 2019.5 The available data is often fragmented, incomplete, and of poor quality.5,9 This article aims to provide an overview of the current situation concerning health data for migrants and refugees in European health information systems (HIS) (see Search strategy and selection criteria). We discuss the need for including migrant and refugee health data in national HIS (see Definitions), identify significant gaps between knowledge and implementation, and suggest what actions should be prioritized.
Search strategy and selection criteria.
The references for this Health Policy paper were collected from various comprehensive reviews on the topic, including reports from the WHO Health Evidence Network (HEN) Series,5 WHO Technical Guidance on Collection and Integration of Data on Refugee and Migrant Health,9 reviews on health monitoring and data collection practices among migrants,10, 11, 12 and systematic reviews of COVID-19 impact in migrants.6,7 Key peer-reviewed scientific articles, reports, and policy documents were also consulted. The health needs of refugees and migrants were drawn from sources like the World Report on the Health of Refugees and Migrants,13 HEN Reports on variations in definitions of migrants and their access to health services,14 the European Commission report on newly arrived migrants and refugees in EU/EEA,15 and HEN Report on public health aspects of migrant health in the WHO European Region.16
Detailed search criteria can be found in the primary reports of the reviews this paper is based on. The selected reports focused on migrant and refugee health data in health information systems, while excluding papers related to one-off primary data collection exercises or ethnicity.5,9 Although understanding self-perceived or attributed ethnicity is crucial for addressing health inequalities due to racialization and racism, it can also contribute to “othering"17,18 of certain ethnicities, even those who are not migrants.19 So, using ethnicity as a sole marker for migration can perpetuate “othering” processes and racialize nationals. Therefore, the paper sought to avoid uncritically using ethnicity as an indicator of migration.
Additional searches were conducted in PubMed, Web of Science, and Google Scholar to identify papers on privacy-preserving data linkage. For further details on the search terms used, refer to Supplementary File S1.
Definitions.
The term “migrants and refugees” is used to refer to two legally distinct social categories, characterized by diverse backgrounds and reasons for migration, but with some shared health risk factors.
Migrants
There is no single definition of migrants. Generally, a migrant is someone who moves away from their usual place of residence, either within a country or to another country, temporarily or permanently, for various reasons.20,21 This includes labor migrants, international students, irregular migrants (without proper documentation), or circular migrants. Defining migrant categories can be complex, considering people move for diverse reasons and situations change over time. It is debated whether the term should include descendants of those who moved countries and, if so, to what extent (first, second, third generation, etc.). These categories are socially constructed and must be broken down into meaningful core indicators to monitor their health, considering their diverse backgrounds and intersecting factors.
Refugees
The term “refugee” has a clear legal definition according to the 1951 Geneva Convention and its protocol.22 It is often used as an umbrella term for displaced populations or people seeking international protection who haven't yet received official refugee status, like asylum seekers. It may also include those whose asylum applications were rejected and face difficult situations.5 To understand and monitor the health needs of diverse refugee populations, we must know their health and social rights (which vary between countries), and the context they are in, such as living in camps due to their legal status.
Health information system (HIS)
A Health Information System (HIS) is a crucial part of any health system. It includes all the activities and resources that gather, analyze, share, and use reliable and timely information about health factors, how well the health system is working, and the overall health status.23 It is like a system involving various people and factors that work together to produce and use health-related information.24 The HIS has four main functions: (i) collecting data, (ii) organizing and compiling data, (iii) analyzing and summarizing data, and (iv) sharing the data with those who need it.25 It can involve different sectors like interior affairs, labor, immigration, non-governmental organizations, or commercial sectors, all of which intersect with the healthcare system and might need information from different sources. The performance of a HIS is evaluated based on how easily accessible, reliable, and timely the data on health needs and determinants are for the entire population.
The structure of the report is as follows: We first discuss the arguments for and against disaggregating data by migratory status. We then propose four strategies to advance evidence, policy and practice. These comprise integrating migration related indicators into existing data collection systems, linking available data sources while respecting privacy, making better use of multilingual health surveys, and most importantly, ensuring participatory approaches so that migrants and refugees become a key partner in collecting and analyzing data, and disseminating evidence. We then proceed by considering political and structural barriers to high-quality data for diverse groups of migrants and refugees (see Definitions). We do so by comparing the current state of data collection with the potential offered by new approaches9 to highlight challenges in implementation. We find that, despite major international initiatives and global compacts (Panel 1), political factors such as lack of transparency and political will, and unclear responsibilities impede data collection, and we propose a policy agenda to bridge the gap between knowledge and action using a change management approach within the health system. This approach considers historical influences, anticipates resistance to change, and involves multiple actors who can contribute to advancing this agenda by improving cross-sectoral governance. Our main audience includes policy makers, scientists, and public health practitioners who can drive change in various sectors across European countries.
Panel 1: Selected global compacts and international initiatives promoting harmonized data on refugees and migrants.
Global compacts and international guidelines encourage countries to collect and standardize health data for refugees and migrants, even though they may not be legally binding. These frameworks can help countries integrate, harmonize, and organize health data based on the status of migrants in their national health information systems.
The Sustainable Development Goals (SDGs) have a target (17.8) that requires data to be broken down by migratory status. This target was supposed to be achieved by 2020, but it was not met.26 Out of 231 SDG indicators, 24 should be disaggregated by migratory status,27 and seven directly relate to migration.28 The European Commission also supports monitoring progress toward SDG 10 (reducing inequalities),29 and a New Pact on Migration and Asylum has been proposed to manage migration and cooperate with countries of origin, transit, and destination.30
The World Health Organization (WHO) has a Strategy and Action Plan for Refugee and Migrant Health in the WHO European Region.31 This plan ended in 202232 and a new regional action plan for 2023–2030 is being developed, which emphasizes strengthening health systems to be more inclusive for refugees and migrants. One of its pillars calls for collecting and sharing migration and health data for evidence-based responses to health challenges faced by refugees and migrants.33
The WHO Global Action Plan also recommends improving health information systems to ensure standardized and comparable records on migrant and refugee health are available at the global, regional, and country levels.34
The European Commission's Action Plan on Integration and Inclusion35 for 2021–2027 aims to modernize access to health and social services using digital tools to enhance the evidence base for policy development.
Although they might not be laws that countries must follow, global agreements and international guidelines suggest and expect countries to gather and organize health data about migrants in a systematic way. These frameworks can help countries combine, make consistent, and break down health data based on whether someone is a migrant or refugee in their own national health information systems.
Arguments for and against disaggregated health data
The need for detailed health data is crucial. Some have raised arguments against breaking down (i.e. disaggregating) health data based on whether someone is a migrant or a refugee. Some of these arguments are well-known. One perspective says that disaggregation could lead to discrimination against minority groups, and people often mention historical abuses36 as examples, like what happened during the Nazi, Stasi, and Soviet regimes.37 There are also legal arguments that say current data protection laws prevent breaking down data based on markers of migrant and refugee status.9 In Europe, for instance, the General Data Protection Regulation (GDPR)38 considers data about health, ethnicity, or nationality as sensitive information. Similar laws exist in other European countries. However, these laws do allow collecting and analyzing such data if there are valid reasons for doing so and appropriate safeguards are in place (Panel 2). Hence, existing data protection laws do not prohibit collecting and analyzing data on migrant and refugee health.9,39 Still, many health systems have not effectively incorporated migration status into their health information systems, despite the possibilities.
Panel 2: General Data Protection Law (GDPR) requirements for data on migrant and refugee health.
-
•
The GDPR is a strict data protection law applicable in EU and EEA countries, considered a gold standard for data management.
-
•
Migration health data is classified as sensitive data, encompassing information on race, ethnicity, political opinions, religion, and health, among others.
-
•
Collecting sensitive data is only permitted under specific conditions, such as explicit consent from the data subject or for health management, research, or cross-border health threats (Art. 9).
-
•
Standards for consent include that it must be freely given, specific, informed, intelligible, and easily accessible. Consent can be revoked (Art. 4 and Art. 7).
-
•
In projects involving multilingual and individuals in vulnerable situations characterized by power imbalances, providing understandable information while complying with GDPR's strict rules can be challenging.
-
•
Collection, processing, and storage of unconsented data are possible under strict circumstances if consent is unattainable. In such cases, objective anonymization must be ensured, and re-identification should be prevented. The societal and scientific benefits must outweigh the risks for the population or individuals involved.
Source: adapted from WHO Technical Guidance on Collection and integration of data on refugee and migrant health.9
There is a growing recognition of the importance of breaking down data by various personal characteristics to understand the social determinants of health.40 However, there is still sensitivity around data on ethnicity19 and migration status, partly due to widespread racism41,42 and concerns about potential discrimination.39 As a result, not much progress has been made in including migrants and refugees in health information systems for over a decade.1,5,12,43
From a public health perspective, it is essential to disaggregate health data to understand the specific health needs and challenges13,14 faced by diverse groups (see Definitions) of migrants and refugees.1,13,16 Otherwise, their unique needs might be overlooked, leading to inadequate responses10,44,45 and hiding inequalities and harmful policies.46,47 This creates a cycle where the lack of data leads to the lack of policies to improve data, perpetuating the problem.
In this situation, debates about the health needs of migrants and refugees can be dominated by political ideologies and unsupported claims. Science can help take politics out of these debates by using evidence and effective communication that counters biased or ideological narratives48 about migrants and refugees, which often rely on unsubstantiated claims on (presumed) under-, over- or mis-use of services.49, 50, 51
While some people worry that collecting data on migration status might lead to discrimination, it is essential to recognize that not collecting this data can also be discriminatory. Everyone has the right to be counted, which is necessary for claiming economic, cultural, and social rights.52 The distinction between people in a nation as residents and citizens can create problems for migrants and refugees.53 This affects whether data is collected and available.5 The failure to collect data on migration status reinforces distinctions between people based on their citizenship and nationality,54 affecting access to healthcare and other rights for some migrants and refugees.5,14
Another aspect is the biopolitical dimension of not collecting migrant and refugee health data in national systems. Some argue53,55 that refugees are governed by states in a state of exception outside normal legal rules, providing only minimal support that reduces individuals to bare survival.56 Data collection may serve the interests of the state rather than the individuals, with a focus on immigration control and securitization,57 leading to restrictive practices like detention or encampment.58,59 This excludes them from political structures58 and limits their rights and agency.57 In contrast, if we collect their data and make their health needs visible, they can assert their rights and have their needs recognized.55,60
The role of a health system in the complex area of migration61 is closely tied to data justice,62,63 which seeks fairness in how people are represented and benefit from data collection. To achieve both integration and justice, health data must be collected for all population groups and properly broken down to support inclusive health policies. It is crucial to respect individual rights, encourage participation, and adhere to data protection laws to avoid stigmatization.
Strategies to advance evidence, policy and practice
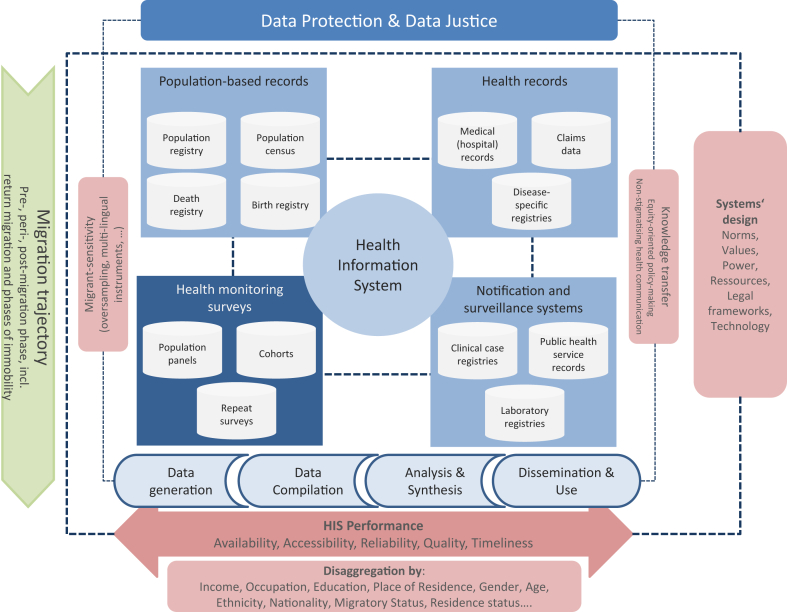
To improve evidence, policy, and practice, European health systems should make the most of data sources they already have and broaden their scope and coverage5,9,31 (Fig. 1). This involves utilizing yet unused data sources and adopting new methods to improve their systems.5,9 Since migration involves various stages and situations, no single data source can capture all the necessary information to track the health of migrants and refugees.9 Therefore, it is essential to consider diverse migration trajectories (Fig. 1) by looking at the different stages of their journey, like before they migrate, during the migration process, after they arrive, and if they return.64,65 It also involves considering times of immobility and looking at various sectors, situations, and countries they go through. To help countries achieving this goal, we present a conceptual framework (Fig. 1) that can be used to design their health information systems and maximize the utilization of both existing and new data sources. The system should effectively fulfil its essential functions (see Definitions) and perform well, considering the specific challenges of capturing the health of mobile populations with unique migration trajectories (Fig. 1). The specific elements and ingredients of such a HIS are explained in the subsequent paragraphs.
Fig. 1.
Conceptual Framework: Designing Health Information Systems sensitive for Migration Trajectories. Legend: This framework focuses on the design of health information systems, considering data sources, functions, and performance criteria intersecting with migration trajectories.
Source: Own illustration, adapted from and expanded based on HEN Report 66.5
Health systems and health information systems (HIS) are often limited by their focus on stable populations66 within individual countries,1,9 overlooking the complexities of migration67,68 and the need for sharing data across sectors9 and borders.69, 70, 71 To address this, data sources for HIS (Fig. 1) can be divided into population-based and institution-based categories,25 including emerging sources like big data72 and health data generated by patients73 through technology, such as electronic devices or health apps74 (Fig. 1).
HIS has essential functions, such as generating, disseminating, and using data to inform decisions. In the context of migration, these functions may involve various sectors, such as interior affairs, labor, immigration systems,44,75 and non-governmental or commercial sectors.9 The effectiveness of HIS is determined by the availability, accessibility, reliability, quality, and timeliness of data,25 along with the ability to capture diversity within societies (Fig. 1).
Implementing changes in HIS requires considering complex factors,76 including dependencies, norms, power relations, resources, legal frameworks, trust and technology (Fig. 1).5,43 The challenge is not always a lack of data; raw data is often available across sectors. The key is to develop processes to turn available data on refugees and migrants into accessible, high-quality information that allows reliable comparisons over time and across different places for monitoring health and making informed decisions. This requires addressing intangible factors of systems, such as values and trust (Fig. 1).
To improve the situation, we need action in both science and policy.5,9 This includes using innovative methods and technology in research, as well as advancing policies and practices based on evidence. By drawing on evidence syntheses5,10,12,13,44,77 and technical guidance from WHO,9,25 we highlight four key strategies to make progress in this matter (Panel 3).
Panel 3: Priority areas to improve European health information systems.
By implementing these strategies, we can strengthen the state of data collection, policies, and practices related to migrant and refugee health:
-
1.
Integrating refugee and migrant health data into national health information systems. This involves routinely collecting, analyzing, and sharing refugee and migrant health data while protecting data privacy.
-
2.
Developing and using innovative privacy-preserving data linkage strategies in fragmented health systems.
-
3.
Enhancing and systematically using diversity-sensitive data collection strategies, including multilingual health surveys and integrating qualitative data in health information systems.
-
4.
Engaging migrants and refugees in governance, data collection, analysis, and dissemination processes.
Sources: HEN report 665; WHO technical guidance on collection of refugee and migrant health data.9
HIS must integrate, routinely collect, analyze and disseminate refugee and migrant health data
Migrant and refugee data should be included in the national health information systems.9 To reflect the diverse health needs of migrants and refugees, their data should be collected, analyzed, and shared with their active involvement in system design at all levels of governance.
Besides technical challenges like language barriers and capturing information about people with different backgrounds (i.e. intersectionality), strong laws should be in place to protect health data from being used inappropriately (e.g., for immigration enforcement) while allowing access for researchers and practitioners. This way, powerful tools like data linkage (see below) can be used to identify health issues and solutions.
Given the complexity of defining migration status (see Definitions) and its dynamic nature, no single indicator can fully capture the diversity of migrants and refugees. However, it is important to have a set of core variables describing migratory status that can be used in health information systems9 (Panel 4), while considering national socio-political contexts.78 In the absence of standardized variables, migratory status can be derived from other parameters, such as name-based approaches79,80 or probability-based strategies using a combination of indicators.81, 82, 83
Panel 4: Core and recommended migration indicators.
The World Health Organization (WHO) Regional office for Europe has provided technical guidance on collecting data for refugees and migrants. They suggest a list of core and recommended variables to help national data systems break down health data based on migratory status. These variables were identified from existing recommendations, guidelines, and practices. The focus is on basic variables that, when combined, can help identify different migrant groups based on country priorities.
Core variables
-
1.
Country of birth
Identifies foreign-born individuals, allowing for easy international comparisons.
-
2.
Citizenship
Determines an individual's entitlements and obligations in social, legal, political, economic, and cultural aspects. Option to record multiple nationalities is recommended.
-
3.
Year and month of arrival in the host country
Helps to plan or evaluate integration programs and health interventions in relation to the duration of stay or phase of migration.
-
4.
Country of birth of both parents
Identifies nationals with a migratory background, such as children of migrants.
Recommended variables
-
1.
Reason for migration
Identifies subgroups of migrants with varying health needs, like forced displacement, labor migrants or family re-unification.
-
2.
Ever resided abroad
Considers emigration, return migration, or circular migratory patterns.
-
3.
Knowledge of host country’s language(s):
Important to access various services and actively engage with the society.
-
4.
Residence status:
May affect access and utilization of health services and be a health determinant due to uncertainties about legal status and differential entitlements to social determinants of health (housing, labor market, social services, education).
To ensure data can be linked and compared, it is crucial to collect the same core variables across different data collection systems. Introducing new variables at the European level is possible, but it is complex as comparable data must be available everywhere, and there are trade-offs involved. Additionally, interest in this issue might be low in places with little immigration.15
The evidence we gather should be used to guide daily practices and policy development, but we must acknowledge that evidence transfer is not value-free or completely neutral (Fig. 1). It should align with Sustainable Development Goals (SDGs) and the idea that health is a human right to promote equity-oriented policy making. Using non-stigmatizing language84 and effectively communicating evidence is essential, as is anticipating non-linear or unintended effects of scientific findings. To achieve this, we need ways, structures, and strategies to proactively share the findings of the HIS with policymakers, the media, and the general public. There is also a desire among individuals not to be permanently labelled as migrants or refugees, and any statistical definition and classification may diverge from, or even conflict with, individuals’ self-perceived identity. Participatory approaches and consideration of qualitative information (see below) may help to identify, avert or address such conflicts, not only related to data collection, but also during dissemination and communication of HIS results. While classification is essential for quantitative monitoring in public health, any system should avoid creating “permanent” labels or classifications that extend beyond the public health needs. This could lead to the classification of individuals and their offspring who may have never migrated themselves,9,78 resulting in Othering17,18 and discrimination.78
The classifications in a system depend on what public health information we want to gather,78 such as an individual's migratory status. For example, for hereditary diseases or specific health behaviors, individuals may be classified as migrants for multiple generations, while for travel-related exposure, the migratory status may only be relevant temporarily.9 Therefore, we propose core variables like country of birth, citizenship, date of arrival, residence status, and country of birth of parents in Panel 4 that can be combined to create indicators fit for purpose, instead of a singular migratory status indicator.
Data linkage strategies are essential in fragmented health systems while preserving privacy
By using multiple indicators of migratory status (Panel 4) from various data sources (Fig. 1) and linking them to health-related indicators, we can gain comprehensive insights into migrant and refugee health. When we want to combine data from different records to get a more complete picture, we use a process called data-linkage. In the HEN Report 66, researchers found that data-linkage is a powerful tool to study a wide range of health outcomes, like suicide rates, mortality (death rates), maternal outcomes (pregnancy and childbirth-related outcomes), non-communicable diseases (like diabetes or heart disease), mental health, and infectious diseases.5 This tool can be used not only in countries with centralized health and information systems, but also in countries where health systems are more decentralized and fragmented (like Germany, Italy, Spain, and the Netherlands).5 There are different ways to do this85, 86, 87 depending on the type of information available and the level of accuracy and privacy needed (Panel 5).
Panel 5: Data linkage strategies and methods.
Exact linkage is used when we have unique identifiers (like an insurance number) that match exactly between different records.
Error-tolerant linkage is used when exact matches are not possible (or not wanted for privacy reasons), and it allows for more observations to be linked.
There are several types of error-tolerant linkage
Rule-based linkage: Rules are set to determine when identifiers must match completely or when a partial match is sufficient. A variant thereof is deterministic linkage, where identifiers or their transformations (like phonetic codes) are checked for an exact match. However, the decision rule may allow only a certain proportion of them to match to consider it a match between data pairs.
Distance-based linkage: Similarity of feature expressions of identifiers is computed using string metrics (e.g., counting changes needed to transform a string).
Probabilistic linkage: Probabilities are calculated to determine the likelihood of a match based on certain identifiers. It takes advantage of the fact that the match of some identifiers has more explanatory power regarding the relatedness of two observation units than the match of others.
Data can be linked using different types of identifiers
Direct identifiers: Unique characteristics like social security numbers or person-identifying data (e.g., name, date of birth, address, or policy number).
Indirect identifiers: Combinations of variables in different datasets that strongly suggest they correspond to the same person.
Encrypted identifiers: Personal data (e.g., last name, first name, and date of birth) is encrypted to preserve privacy. Bloom filters are one method for encrypted data linkage, allowing for error-tolerant linkage on encrypted data without revealing original information.
Bloom filters: are a data structure used for privacy when direct person identifiers cannot be used. They encrypt identifiers into unique patterns of zeros and ones using hash functions. This enables testing for presence in different datasets without revealing original information. They allow error-tolerant data linkage on encrypted data, preventing re-identification of individuals.
Sources: Derived and adapted from March et al.87
Privacy-preserving record linkage (PPRL) is a way to connect data from different sources without revealing personal information about individuals.85,86 It involves using encrypted IDs to link data, making it hard or impossible to identify specific people.88 This method is particularly important when dealing with data from international migration, where the same person might have records from different sources and there could be typographical errors in the data. To link this data effectively, error-tolerant record linkage methods are used.89 Scandinavian countries use a unique ID for linking data across various sources, but this approach is not feasible or deliberately avoided in fragmented systems to avoid centralization of sensitive data. In some countries, such linkage is legally prohibited and considered “red lines” by data protection officers due to historical reasons. In such cases, error-tolerant record linkage with so called Bloom filters (Panel 5) is more suitable.90,91
PPRL can provide valuable insights by linking pre-migration data with post-migration health data75,81,92,93 or connecting health data with information about the post-migratory context.94, 95, 96, 97 This helps understand the migration journey and related health needs.5 For instance, it can be useful in ensuring continuity of care and vaccination coverage during the migration process.93,98 PPRL can also be helpful in emergencies like the COVID-19 pandemic by leveraging important data,99 or by linking routine data (e.g. from laboratories) with primary data from surveys.5,100
PPRL can be applied to data with or without consent (Panel 2). Health data is usually collected with consent, but administrative data related to migration may not be collected for health purposes, and its use in health information systems could be considered unconsented. More research is needed to determine the acceptability and best strategies for using unconsented data101 in migration health monitoring and research. PPRL faces technical and practical challenges even with consent,5 especially in decentralized health and immigration systems. Additionally, ethical concerns arise62 regarding the potential misuse of data for non-health purposes, such as immigration enforcement.9,44
While PPRL is valuable, it is not a perfect solution. In some cases, even with consent, pseudonymized datasets might still be used to identify individuals. To address this, decentralized, federated analysis methods102, 103, 104, 105 can be used to ensure individual-level analysis without linking data across different sources (see below under Political and structural barriers). These methods are increasingly being used in general health systems, but yet rarely used in the context of migrant and refugee health.9,106,107 The proposed European Health Data Space108 by the European Commission aims to provide a secure environment for accessing and processing health data at national and EU levels, supporting healthcare delivery, research, innovation, and policymaking.
Health monitoring surveys must be sensitive to diversity and multilingual groups
Diversity-sensitive, multilingual health monitoring surveys are an important tool to gather information (primary data) about the health of migrants and refugees.5,9 Data from registries and routine administrative and health sources have limitations because they often lack self-reported health measures. Health monitoring surveys (Fig. 1), which include migrants and refugees and are conducted regularly, can provide additional information on their health.9,77,109,110 During the COVID-19 pandemic, repeat surveys with data on migratory status or conducted in multiple languages were particularly helpful in understanding infection risk and vaccination status among migrants and refugees.111,112 These surveys can also help monitor socio-economic inequalities in self-reported health over time,113 study the health effects of changes in subjective social status due to migration,114,115 and identify health factors related to post-migration situations like housing and employment.116,117 Surveys by NGOs and integration of qualitative data can improve understanding of social determinants of health among migrants.118 Qualitative information can also help to capture more information on living and working conditions. It can also capture self-reported identities, and explore potential conflicts between statistical migrant categories and individuals’ self-expressed group-identity. Such information is also relevant during emergencies: in response to the war in Ukraine, IOM conducted face-to-face surveys at border crossing points, assessing needs and intentions of migrants.119 WHO also produced a health needs assessment for refugees, aiding decision-making in the refugee response.120
However, such surveys are still rare. Out of 242 data sources on migrant and refugee health in the WHO European Region, only 31 (12.8%) were health monitoring surveys.5 Many surveys use only one language and exclude certain groups, like migrants in precarious work or refugees in camps5,77 or humanitarian emergencies.121 National health monitoring surveys in Europe often use multi-lingual surveys to ensure cross-cultural comparability between countries with different languages.122 However, with the increasing diversity in European societies,12 a paradigm shift is needed for surveys to become diversity-sensitive (Fig. 1). This means capturing the health status of the population by conducting surveys in multiple languages within countries while ensuring comparability of response scales.122, 123, 124 Harmonized approaches should be used across countries, e.g. through multi-national EU initiatives such as the European Health Interview Survey (EHIS). Oversampling and innovative sampling5,9 and recruitment methods125 can improve response rates.77,125, 126, 127 Digital technologies, like videos and audio materials in different languages, along with online interpreting services, can help with informed consent and increase trust and response rates.
In precarious settings like refugee camps or undocumented migrant clinics, setting-based sampling approaches can be used to collect data using a combination of different strategies, ranging from probabilistic128 to non-probabilistic and participatory ones.129 The main challenge is not to run a one-off data collection, but to implement these approaches systematically and structurally within the health information systems, ensuring funding, structures, and legal aspects are in place to protect the rights and benefit the migrant and refugee groups being studied.
Participatory approaches to designing HIS must include migrants and refugees
Participatory approaches involve working closely with all stakeholders, including migrants and refugees, to create knowledge together and make decisions collectively.130 These methods can overcome barriers like language, cultural differences, and power imbalances, ensuring broad stakeholder involvement. Good governance of health information systems (HIS) stresses the importance of participatory approaches with broad stakeholder involvement, based on transparency, accountability, and fairness.131 This builds trust among migrants and refugees in the data collection, security, and use, aligning with data protection laws like GDPR (Panel 2) and the idea of data justice.62 Refugees and migrants face challenges in trusting authorities collecting their data, due to perceived132 and real misuse133 of data, both in countries of origin and destination. This mistrust depends on factors including lack of awareness, language barriers, lack of involvement of refugee and migrant communities in HIS processes such as data collection and dissemination, and on weak data protection laws.9,132,133 Solutions to address this mistrust include awareness raising on the public health need for collecting refugee and migrant health data and how the data is protected in languages refugees and migrants can understand, multilingual surveys, training of staff in cultural competency, better data protection and participatory approaches facilitating involvement of refugees and migrants in HIS processes.9,39,134
Participatory approaches to data collection with migrants and refugees can include designing health surveys together, using peer researchers who speak multiple languages to distribute surveys,135 and working with community partners in focus groups to understand how to collect sensitive data in HIS.136 Such approaches will also help to identify discrepancies between self-perceived identities and statistical categories used in HIS and understand health or social aspects arising from such tensions. However, to implement and sustain these approaches, enough resources from the government and funders are required,137 and national policies should support migrant and refugee involvement in health decision-making at a societal level.130
Political and structural barriers
The main challenge in obtaining high-quality and timely data on migrant and refugee health in European health systems is not because we lack knowledge, methods, or technology. The main problem is that the existing recommendations and guidelines for data collection5,9,11,78,131 are not being implemented effectively into the health information systems at both European and national levels. This lack of implementation is a result of a lack of political priority given to health information systems in general, and to migrant and refugee health topics in particular (beyond a health-security approach48). It also involves the political determination of the data collection process. This issue is further complicated because migration health falls under the responsibility of various ministries, including health, interior, labor, and foreign affairs, which also plays a significant role in hindering implementation.
Challenges to implementation must be recognised
There are several reasons why existing guidelines are not being implemented effectively. Some of these factors include a lack of digitalization in refugee camps, inadequate frameworks to prevent misuse of data for non-health purposes, neglect of migrants and refugees in national public health plans, and financial limitations and trade-offs that overlook the complexity of population health (e.g., prioritizing health monitoring for citizens over non-nationals). Moreover, dedicated structures within public health authorities focusing on refugee and migrant health are often lacking, limiting progress in this area.
Change management approaches are needed
To successfully implement the existing knowledge, methods, and technologies, a change management approach is necessary. This approach involves understanding the national and organizational context, considering the different actors and forces involved (including resistance to change), having a clear agenda and idea of the changes needed, focusing on the process of change (e.g., top-down or from within organizations), and defining the desired outcomes.138 Effective leadership138 and action-oriented efforts139 across various sectors are essential to transform HIS and effectively address the health needs of a mobile world. To enhance HIS regarding migrants and refugees, it is crucial to tailor interventions to the specific contexts, settings and variations among European countries. This requires considering factors like national policies, local conditions, institutional structures, political climates, and cultural differences. Establishing local coalitions that bridge cross-sectoral divides (see below) is crucial in achieving this objective.
Politics cannot be ignored
One important explanation for failure to share migrant data is politics influence data governance. In some cases, public health authorities collect migrant data but do not publicize or share it with the health community in a timely manner for political reasons.140 There may be undue influence or interference by local or national authorities in data collection, compromising transparency and accountability.140, 141, 142 Additionally, varying levels of governance (national, sub-national, local) may have different perspectives on the significance of migrant and refugee health data. Addressing these political challenges is essential for improving data systems and promoting fairness and transparency in data collection processes. Examples from Greece (Panel 6), Türkiye (Panel 7) and Germany (Panel 8) show how political context can impact data collection, handling and (non-)availability.
Panel 6: Availability and access to migration health data inGreece.
Context and type of data
Greece is a major entry point for migrants and refugees in Europe.143,144 However, there is no comprehensive and transparent migration health information system in the country. The COVID-19 pandemic has exposed this data gap and vulnerability in public health preparedness.145 Until early 2022, the Greek Ministry of Defense and the International Organization for Migration (IOM) were responsible for reporting data on new arrivals and refugees in specific facilities.146,147 In March 2022, this responsibility was transferred to the Greek Ministry of Migration and Asylum. However, this transition led to the loss of crucial data,144,146 such as age, sex, and ethnicity distribution of refugees in reception sites, which are essential for public health planning and response.
Political intersections
There is an epidemiological surveillance system in place for refugee/migrant reception sites, reporting on medical conditions.148 During the pandemic, COVID-19 data was included in the reports, but it disappeared from the surveillance reports later on.149 This happened around the time when independent scientific reports suggested a higher incidence rate of COVID-19 among refugees/asylum seekers in these facilities compared to the general population.150 Surprisingly, national authorities in Greece have barely recorded or reported data on COVID-19 hospitalizations, deaths, and vaccine uptake among migrants and refugees, despite the calls from the scientific and public health community.140
Consequences for HIS/health of refugees and migrants
The lack of routine data on demographics, morbidity, and mortality among migrant and refugee populations in Greece poses serious challenges for public health interventions. It leaves policymakers and healthcare providers with limited information to address the health needs of these vulnerable groups effectively. This situation demands urgent attention and action to establish a comprehensive migration health information system that can support evidence-based and accountable public health policies and interventions.
Panel 7: Availability and access to migration health data in Türkiye.
Context and type of data
In Türkiye, health data has become a political issue over the last two decades, especially after the health transformation project aimed to improve healthcare infrastructure, including the integrated health information system (HIS).151 One result of this development is a national health record system called e-pulse, which allows citizens to access their personal health information, medical records, and prescriptions. However, epidemiological data collected from various health facilities through the HIS is only available to higher-level government policy makers and not easily accessible to independent researchers.
Political intersections
Health-related data in Türkiye are collected through three main channels: the integrated HIS, nationally representative surveys such as demographic and health surveys (DHS), and independent research by researchers or NGOs. Access to data from the health system is subject to authorization from the Ministry of Health (MoH), and independent researchers often face challenges in obtaining data, even for important public health issues like the COVID-19 pandemic. While some papers based on health records have been published,152,153 independent researchers often face difficulties in obtaining COVID-19-related data,154,155 including vaccination information, which limits our understanding of the true burden of the pandemic and its impact on vulnerable groups, including migrants.
Consequences for HIS/health of refugees and migrants
Nationally representative surveys conducted by the government with university collaboration can provide some information, but there have been instances of missed opportunities, such as skipping to include non-Syrian migrants in Türkiye in a recent DHS report.156 The COVID-19 pandemic has also been a missed opportunity for the HIS to prove its usefulness in research, as data sharing and access have been restricted, leaving the true burden of the pandemic among vulnerable groups, including migrants, largely unknown.
Panel 8: Availability of migration health data in refugee camps in Germany.
Context and type of data
In 2015, over a million refugees migrated to Europe, with many arriving in Germany. However, the lack of functional electronic health record systems in reception centers and refugee camps posed challenges.70,157 This deficit made it difficult to plan for health-related matters, as crucial information like chronic disease prevalence and the number of pregnant women was not easily accessible for policy decisions.157 To tackle this problem, the German Ministry of Health initiated scientific initiatives to improve data collection, including surveys and electronic health records (EHR).158 In 2017, an academic project successfully developed and implemented a digital monitoring tool. This tool enabled real-time analysis of more than 60 health indicators, based on routine health care encounters in the centers and camps, while safeguarding refugee privacy and data protection through federated analysis techniques.107
Political intersections
The nationwide rollout of the innovative technology in Germany faced significant challenges due to its decentralized system with 16 federal states, each having its own Ministry of Health and Ministry of Interior Affairs overseeing reception centers. Until 2020, only three states adopted the system in 18 reception centers. In some states, health authorities discontinued its use due to changes in mandates or the Ministry of Interior handing over responsibilities to commercial providers who did not use standardized EHR. Different levels of governance had varied views on the need for data systems in these settings, leading to reluctance or lack of support. In one state, a change in government resulted in the technology losing support, despite local interest in implementing it. In another state, authorities decided they were not responsible for data collection or providing a system for it. Some states did not respond or actively follow the calls to introduce such systems from the Federal Ministry of Health.
Consequences for HIS/health of refugees and migrants
Fragmented governance and differing views among state-level and regional authorities hindered the adoption of the system. During the COVID-19 pandemic, the limited use of the monitoring system in refugee centers made it challenging to identify health needs. The lack of clear responsibilities and mandates for health information systems in refugee settings resulted in them being inaccessible “black boxes” during the pandemic. Despite the tool being available for six years, it is currently only used in 30 centers across two states.
Greece lacks a comprehensive and transparent migration health information system, which has become more evident during the COVID-19 pandemic. The transition of data reporting responsibilities led to the loss of crucial data, and the absence of routine data on migrant and refugee health poses significant challenges for public health interventions (Panel 6). In Türkiye, health data has become a political issue, and access to health-related data is limited for independent researchers, particularly for important public health issues like the COVID-19 pandemic. This lack of transparency and limited data access hinders our understanding of the health needs of vulnerable groups, including migrants (Panel 7). In Germany, the lack of functional electronic health record systems in reception centers and refugee camps in Germany posed challenges for health planning and policy decisions in 2015. While an innovative digital monitoring tool was developed and implemented successfully,107 its nationwide rollout faced challenges due to decentralized governance and varying levels of support among different authorities. This case shows that crises can drive technology development, but technology alone cannot overcome the political challenges in health information systems (Panel 8).
Public health specialists aiming to bring about positive change within health information systems should be aware of these tensions and political dynamic and work together with government, academia, and civil society to shift power balances in a way that aligns with the functions and principles of health information systems governance (transparency, accountability, and fairness) and ensures data collection serves the health needs of migrants and refugees.
Another important issue is the scattered nature of data on migrants (especially data related to their health). This is because healthcare services for these groups are provided by various organizations, such as NGOs, international organizations, charities, and national public health authorities. These organizations collect data in a haphazard and ad-hoc manner, leading to limited and disconnected information in separate systems.5 To solve this problem of fragmented migrant and refugee health data, their healthcare needs to be integrated into national healthcare strategies and systems. Strengthening migrant health monitoring requires addressing the political aspects of data collection and bridging cross-sectoral divides.
Cross-sectoral governance is essential
Health is a crucial requisite for ensuring safe and humane migration, but the health sector is not often involved in decision-making processes related to migration. The examples from Greece (Panel 6), Türkiye (Panel 7) and Germany (Panel 8) illustrate the poor inter-sectoral coordination that impact the (non-)availability of data, despite varying country contexts. Most decisions are made by ministries dealing with immigration control, foreign policy, and labor migration, with health authorities’ engagement usually ushered during health emergencies or for border-health management. Migration health and human mobility are not fully integrated into national health care strategies, priority setting or health care financing. As a consequence, health systems lack systematic inclusion of migration data.
To meaningfully improve the collection of migration health data, inter-sectoral coordination is needed. Some countries have successfully ushered such coordination across government ministries, including collaboration with academia and migrant communities themselves.159 There is a need to systematically map and analyze existing data to make the most of the available information. Migration health data exists not only within health systems but also in other sectors44 like labor migration, immigration, border management, detention centers, pre-migration health assessment clinics, resettlement services, and health insurance providers. The newly established EU Atlas of Migration160 showcases harmonized and validated migration data by country. However, many migration data sources remain unmapped, unanalyzed, and disconnected from health information systems.
In general, information silos and the lack of data integration and interoperability within different societal sectors, including different parts of the healthcare system, pose a broader challenge not exclusive to migration or health. Health systems face difficulties in these areas overall. Therefore, finding solutions to enhance health information systems for migrant and refugee data may also benefit other sectors and aspects of the HIS for the general population.
The challenges mentioned earlier, related to information silos, also impact the sharing of health data for healthcare purposes within and between organizations of the same country but also across countries. The healthcare provided to refugees and certain migrant groups is often fragmented, delivered by a diverse range of organizations, including humanitarian, commercial, public, volunteer, and governmental entities. Sharing data is vital for the effective operation of health information systems (HIS), but faces many barriers, including lack of technology, legal issues, data protection, or issues related to organizational cultures and trust (e.g. of NGOs in authorities or vice versa). However, these issues are not confined to migrants and go beyond the scope of this paper, even though they are increasingly important in today's mobile world, where people move across borders and countries, but also among different organizations within countries. This calls for solutions that enable both privacy and continuity of care.
An agenda for moving policy forward
Strengthening health information systems (HIS) to better serve the health needs of refugees and migrants presents challenges and opportunities for European countries. They must rebuild after the COVID-19 pandemic, tackle the economic and political consequences of the Russian invasion of Ukraine, and confront extreme climatic events. Prioritizing investment in HIS becomes challenging but is still necessary. Crises will continue,161 and as the pandemic revealed, high quality HIS are vital to navigate uncertainties at individual, organizational, and societal levels.162 This investment will not only benefit refugees and migrants but also the entire population, supporting evidence-informed policies and practices that leave no-one behind.
New technologies offer many opportunities and will be crucial if we are to enhance coverage of migrant and refugee health data by HIS. They aid data collection (using data gathering devices, online interpretation, audio and video recording of consent, digital health records), data analysis (linkage, encryption, federated analysis systems), and data dissemination (dashboards, visualizations for policy and community use). However, the challenges in making data available are not primarily due to technological limitations.
If we are to bridge the gap between knowledge and action and advance policy and practice, we need collaborative efforts at multiple levels. Inter-ministerial and intersectoral working groups at the EU/EEA, national, and local levels should fully involve civil-society organizations and refugees and migrants. This would help to mainstream migration within health governance and vice versa,163 fostering transformational change tailored to each country's context and health system.
Enhancing data systems requires a comprehensive strategy that promotes the appropriate use of migrant and refugee health data while preventing misuse. It is essential to understand the complexities involved and find incentives and sanctions to encourage equitable and innovative applications. Data protection legislation should be seen as a means to promote inclusive policies, not as a barrier. Building trust is crucial in this process to ensure the successful implementation of these strategies and protect human rights while avoiding othering17,18 of migrants and refugees and ensuring they are the ones benefitting most from improved data and health information. This is especially crucial because how public health systems group individuals can sometimes conflict with how these individuals see themselves, a concern that goes beyond legal labels and where they come from. The decision of individuals to share health related information, take part in surveys, or use digital tools, also depends on and influences how they see themselves. This should be kept in mind and migrants and refugees should be a major partner when creating plans and actions to enhance data systems despite the challenges it entails.
National public strategies must address the health needs of migrants and refugees, but this must be supported by effective monitoring systems that collect sufficiently granular data to track progress among all population groups. The EU and WHO, along with specialized agencies like IOM, ECDC, UNICEF, and UNHCR, can support the exchange of good practices and harmonize data collection at national and international levels. This involves creating knowledge sharing platforms, conducting workshops, and offering support on data linkage and secure data environments. A thorough inventory of existing data sources and practices can help identify gaps5,9 and promote consolidation, avoiding duplication of efforts. It would help to identify intervention points - technological, legal, or organizational - to consolidate and improve the fragmented approaches that exist. This should be complemented by measures to integrate core variables into all functional data collection systems. These activities will require training programs and there are obvious economies of scale to be achieved by international collaboration. Leapfrogging, or adopting advanced technologies and practices will to achieve this progress more rapidly.
Overall, investing in HIS for refugee and migrant health is vital for addressing health challenges in diverse populations, supporting evidence-based policies. International collaboration to develop strategic approaches will pave the way for effective data-driven policies and practices that benefit both migrants and the general population.
Contributors
KB conceived and conceptualized the report, developed the methodology, performed the investigation, curated data, performed literature searches, wrote the original and final draft, led reviews & editing, performed visualization, and led the project administration. MM and SJ substantially contributed to conceptualization and writing (review & editing), methodology and writing (review & editing). NAM, JB, IC, TIG, AH, JJ, DK, JK, IK, EK, LL, IM, AM, JS and KW contributed to writing (review & editing). Technical input was provided by JB, JK, and AM. TIG, AH, IK, EK, LL, IM and KW substantially contributed to the literature search. IK and EK contributed substantially to data curation (country case studies).
All authors had full access to all data in the study and had final responsibility for the decision to submit for publication.
Use of AI or AI-assisted technologies
A first version of the manuscript was written and submitted without the use of AI technology. AI technology based on language models (ChatGPT) was then used to improve readability and language, and to simplify the text for better accessibility for a non-expert audience (based on the requests of editors and reviewers). The technology was applied with human oversight and control, and authors carefully reviewed, checked and edited the AI-generated text for accuracy, originality and integrity. The AI technology was not used to replace researcher tasks such as producing scientific insights, analyzing and interpreting data, or drawing scientific conclusions. Authors take full responsibility for the content of the publication.
Declaration of interests
All authors declare no competing interest.
Acknowledgements
We thank Niklas Nutsch (Bielefeld University) for his support in literature searches on data linkage and Jan Oppenberg (Bielefeld University) for technical support.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanepe.2023.100744.
Appendix A. Supplementary data
References
- 1.Abubakar I., Aldridge R.W., Devakumar D., et al. The UCL-Lancet commission on migration and health: the health of a world on the move. Lancet. 2018;392(10164):2606–2654. doi: 10.1016/S0140-6736(18)32114-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.IOM . World migration report 2022. International Organization for Migration; Geneva: 2022. [Google Scholar]
- 3.Knipper M., Bozorgmehr K., Offe J., Orcutt M. Germany's new global health strategy: leaving migrants behind. Lancet. 2021;397(10268):20–21. doi: 10.1016/S0140-6736(20)32546-0. [DOI] [PubMed] [Google Scholar]
- 4.Kluge H.H.P., Jakab Z., Bartovic J., D'Anna V., Severoni S. Refugee and migrant health in the COVID-19 response. Lancet. 2020;395(10232):1237–1239. doi: 10.1016/S0140-6736(20)30791-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bozorgmehr K., Biddle L., Rohleder S., Puthoopparambil S., Jahn R. WHO Regional Office for Europe; Copenhagen: 2019. What is the evidence on availability and integration of refugee and migrant health data in health information systems in the WHO European Region? Health Evidence Network (HEN) Synthesis Report 66. [PubMed] [Google Scholar]
- 6.Hayward S.E., Deal A., Cheng C., et al. Clinical outcomes and risk factors for COVID-19 among migrant populations in high-income countries: a systematic review. J Migr Health. 2021;3 doi: 10.1016/j.jmh.2021.100041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hintermeier M., Gencer H., Kajikhina K., et al. SARS-CoV-2 among migrants and forcibly displaced populations: a rapid systematic review. J Migr Health. 2021;4 doi: 10.1016/j.jmh.2021.100056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKee M. Drawing light from the pandemic: a new strategy for health and sustainable development. 2021. https://eurohealthobservatory.who.int/publications/m/drawing-light-from-the-pandemic-a-new-strategy-for-health-and-sustainable-development [DOI] [PMC free article] [PubMed]
- 9.WHO . Collection and integration of data on refugee and migrant health in the WHO European Region: technical guidance. World Health Organization Regional Office for Europe; Copenhagen: 2020. [Google Scholar]
- 10.Chiesa V., Chiarenza A., Mosca D., Rechel B. Health records for migrants and refugees: a systematic review. Health Policy. 2019;123(9):888–900. doi: 10.1016/j.healthpol.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 11.Mladovsky P., Ingleby D., Rechel B. Good practices in migrant health: the European experience. Clin Med. 2012;12(3):248–252. doi: 10.7861/clinmedicine.12-3-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rechel B., Mladovsky P., Ingleby D., Mackenbach J.P., McKee M. Migration and health in an increasingly diverse Europe. Lancet. 2013;381(9873):1235–1245. doi: 10.1016/S0140-6736(12)62086-8. [DOI] [PubMed] [Google Scholar]
- 13.WHO . World Health Organization; Geneva: 2022. World report on the health of refugees and migrants. [Google Scholar]
- 14.Hannigan A., O’Donnell P., O’Keeffe M., MacFarlane A. World Health Organization Regional Office for Europe; Copenhagen: 2016. How do variations in definitions of “migrant” and their application influence the access of migrants to health care services? Health Evidence Network Synthesis Report 46. [PubMed] [Google Scholar]
- 15.European Commission, Consumers Health Agriculture, Food Executive Agency . Report on the health status of newly arrived migrants and refugees in EU/EEA. European Commission; Brussel: 2020. [Google Scholar]
- 16.Bradby H., Humphris R., Newall D., Phillimore J. Health evidence Network synthesis report 44. World Health Organization Regional Office for Europe; Copenhagen: 2015. Public health aspects of migrant health: a review of the evidence on health status for refugees and asylum seekers in the European Region. [PubMed] [Google Scholar]
- 17.Grove N.J., Zwi A.B. Our health and theirs: forced migration, othering, and public health. Soc Sci Med. 2006;62(8):1931–1942. doi: 10.1016/j.socscimed.2005.08.061. [DOI] [PubMed] [Google Scholar]
- 18.Brons L.L. Othering, an analysis. Transcience. 2015;6(1):69–90. [Google Scholar]
- 19.Routen A., Akbari A., Banerjee A., et al. Strategies to record and use ethnicity information in routine health data. Nat Med. 2022;28(7):1338–1342. doi: 10.1038/s41591-022-01842-y. [DOI] [PubMed] [Google Scholar]
- 20.IOM . International Organization for Migration; Geneva: 2019. International migration law: glossary on migration. [Google Scholar]
- 21.UN Statistics Division . United Nations Department of Economic and Social Affairs Statistics Division; New York: 1998. Recommendations on statistics of international migration, revision 1. [Google Scholar]
- 22.UNHCR . Convention and protocol relating to the status of refugees. United Nations High Commissioner for Refugees; Geneva: 2010. [PubMed] [Google Scholar]
- 23.WHO . World Health Organization; Geneva: 2007. Everybody's business: strengthening health systems to improve health outcomes: WHO's framework for action. [Google Scholar]
- 24.MEASURE Evaluation Defining health information systems. 2020. https://www.measureevaluation.org/his-strengthening-resource-center/his-definitions.html
- 25.Health Metrics Network . World Health Organization; Geneva: 2012. Framework and standards for country health information systems. [Google Scholar]
- 26.Roser M.O.-O.E., Ritchie H., Mispy J. Sustainable Development Goal 17: revitalize the global partnership for sustainable development. 2021. https://sdg-tracker.org/global-partnerships
- 27.UN Statistics Division . 2020. SDG indicators: global indicator framework for the sustainable development goals and targets of the 2030 agenda for sustainable development.https://unstats.un.org/sdgs/indicators/indicators-list/ [Google Scholar]
- 28.UN Statistics Division . Report of the UN expert group meeting on improving migration data in the context of the 2030 Agenda. United Nations Statistis Division; New York: 2017. Improving migration data in the context of the 2030 Agenda. [Google Scholar]
- 29.European Commission . REPORT from the commission to the European parliament, the council, the European economic and social committee and the committee of the Regions: EU voluntary review on progress in the implementation of the 2030 agenda for sustainable development. European Commission; Brussels: 2023. [Google Scholar]
- 30.European Commission . Communication from the commission to the European parliament, the council, the European economic and social committee and the committee of the Regions on a new Pact on migration and asylum. European Commission; Brussels: 2020. [Google Scholar]
- 31.WHO . Regional Committee for Europe 66th Session, 12–15 September 2016. WHO Regional Office for Europe; Copenhagen: 2016. Strategy and action plan for refugee and migrant health in the WHO European Region. [Google Scholar]
- 32.WHO . Refugee and migrant health in the WHO European region: final progress report. WHO Regional Committee for Europe; Tel Aviv: 2022. [Google Scholar]
- 33.WHO . Report on the high-level meeting on health and migration: 17–18 March 2022, Istanbul. WHO Regional Office for Europe; Copenhagen: 2022. [Google Scholar]
- 34.WHO . Promoting the health of refugees and migrants: draft global action plan, 2019–2023. World Health Organization; Geneva: 2019. [Google Scholar]
- 35.European Commission . Communication from the commission to the European parliament, the council, the European economic and social committee and the committee of the Regions action plan on integration and inclusion 2021-2027. European Commission; Brussels: 2020. [Google Scholar]
- 36.Labisch A. The Sonal construction of Illness Illness and medical knowledge in past and present. Franz Steiner; Stuttgart: 1992. The social construction of health. From early modern times to the beginnings of the industrialization; pp. 85–101. [PubMed] [Google Scholar]
- 37.Hoofnagle C.J., Van Der Sloot B., Borgesius F.Z. The European Union general data protection regulation: what it is and what it means. Inform Commun Technol Law. 2019;28(1):65–98. [Google Scholar]
- 38.European Union Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) (Text with EEA relevance) 2016. https://eur-lex.europa.eu/eli/reg/2016/679/oj
- 39.European Commission Directorate-General for Justice Consumers. Farkas L. Publications Office; Brussels: 2020. Analysis and comparative review of equality data collection practices in the European Union : data collection in the field of ethnicity. [Google Scholar]
- 40.Solar O., Irwin A. World Health Organization; Geneva: 2010. A conceptual framework for action on the social determinants of health. [Google Scholar]
- 41.Falkenbach M., Heiss R. Springer; 2021. Populist radical right and health. [Google Scholar]
- 42.Bozorgmehr K., Kühne S., Biddle L. Local political climate and spill-over effects on refugee and migrant health: a conceptual framework and call to advance the evidence. BMJ Global Health. 2023;8(3) doi: 10.1136/bmjgh-2022-011472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.WHO . Progress report on implementation of the strategy and action plan for refugee and migrant health in the WHO European Region. WHO Regional Office for Europe; Copenhagen: 2020. [Google Scholar]
- 44.Zenner D., Wickramage K., Bozorgmehr K., et al. In: Migration in west and North Africa and across the mediterranean: trends, risks, development and governance. IOM, editor. International Organization for Migration - Global Migration Data Analysis Centre; Brussels: 2020. Health information management in the context of forced migration in Europe; pp. 245–260. [Google Scholar]
- 45.Rechel B., Mladovsky P., Deville W. Monitoring migrant health in Europe: a narrative review of data collection practices. Health policy. 2012;105:10–16. doi: 10.1016/j.healthpol.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 46.Juárez S.P., Honkaniemi H., Dunlavy A.C., et al. Effects of non-health-targeted policies on migrant health: a systematic review and meta-analysis. Lancet Glob Health. 2019;7(4):e420–e435. doi: 10.1016/S2214-109X(18)30560-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Biddle L., Hintermeier M., Costa D., Wasko Z., Bozorgmehr K. Context, health and migration: a systematic review of natural experiments. eClinicalMedicine. 2023;64:102206. doi: 10.1016/j.eclinm.2023.102206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Voss M., Wahedi K., Bozorgmehr K. In: Health policy and systems responses to forced migration. Bozorgmehr K., Roberts B., Razum O., Biddle L., editors. Springer International Publishing; Cham: 2020. Health security in the context of forced migration; pp. 119–139. [Google Scholar]
- 49.Gottlieb N., Trummer U., Davidovitch N., et al. Economic arguments in migrant health policymaking: proposing a research agenda. Glob Health. 2020;16(1):113. doi: 10.1186/s12992-020-00642-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Trummer U., Krasnik A. Migrant health: the economic argument. Eur J Publ Health. 2017;27(4):590–591. doi: 10.1093/eurpub/ckx087. [DOI] [PubMed] [Google Scholar]
- 51.Bozorgmehr K., Razum O. Effect of restricting access to health care on health expenditures among asylum-seekers and refugees: a quasi-experimental study in Germany, 1994-2013. PLoS One. 2015;10(7) doi: 10.1371/journal.pone.0131483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Correa-Velez I., Gifford M. When the right to be counted doesn't count: the politics and challenges of researching the health of asylum seekers. Crit Publ Health. 2007;17(3):273–281. [Google Scholar]
- 53.Owens P. Reclaiming ‘bare life’?: against Agamben on refugees. Int Relat. 2009;23(4):567–582. [Google Scholar]
- 54.Ooms G., Keygnaert I., Hammonds R. The right to health: from citizen's right to human right (and back) Public Health. 2019;172:99–104. doi: 10.1016/j.puhe.2019.01.019. [DOI] [PubMed] [Google Scholar]
- 55.Owens P. Refugees in international relations. 2011. Beyond “bare life”: refugees and the “right to have rights”; pp. 133–150. [Google Scholar]
- 56.Agamben G. Suhrkamp Verlag; 2012. Homo sacer: Die souveräne Macht und das nackte Leben. [Google Scholar]
- 57.Kaurin D. Center for International Governance Innovation; Waterloo: 2019. Data protection and digital agency for refugees. [Google Scholar]
- 58.Ajana B. Asylum, identity management and biometric control. J Refug Stud. 2013;26(4):576–595. [Google Scholar]
- 59.Weiler G., Bartovic J., Ebbesen B.B., Gottardo C., Puthoopparambil S.J. Improving health in immigration detention and promoting alternatives to detention. Lancet. 2022;399(10338):1849–1850. doi: 10.1016/S0140-6736(22)00742-5. [DOI] [PubMed] [Google Scholar]
- 60.Bozorgmehr K., Wenner J., Razum O. Restricted access to health care for asylum-seekers: applying a human rights lens to the argument of resource constraints. Eur J Public Health. 2017;27(4):592–593. doi: 10.1093/eurpub/ckx086. [DOI] [PubMed] [Google Scholar]
- 61.Bozorgmehr K., Jahn R. Adverse health effects of restrictive migration policies: building the evidence base to change practice. Lancet Glob Health. 2019;7(4):e386–e387. doi: 10.1016/S2214-109X(19)30042-7. [DOI] [PubMed] [Google Scholar]
- 62.Taylor L. What is data justice? The case for connecting digital rights and freedoms globally. Big Data Soc. 2017;4(2) [Google Scholar]
- 63.Shaw J., Sekalala S. Health data justice: building new norms for health data governance. NPJ Digit Med. 2023;6(1):30. doi: 10.1038/s41746-023-00780-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zimmerman C., Kiss L., Hossain M. Migration and health: a framework for 21st century policy-making. PLoS Med. 2011;8(5) doi: 10.1371/journal.pmed.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schapendonk J., van Liempt I., Schwarz I., Steel G. Re-routing migration geographies: migrants, trajectories and mobility regimes. Geoforum. 2020;116:211–216. [Google Scholar]
- 66.Biddle L., Wahedi K., Bozorgmehr K. Comparable worth of life for all? Conducting and disseminating health economic evaluations for refugees in Germany. Glob Health. 2022;18(1):48. doi: 10.1186/s12992-022-00845-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pannetier J., Ravalihasy A., Lydié N., Lert F., du Loû A.D. Prevalence and circumstances of forced sex and post-migration HIV acquisition in sub-Saharan African migrant women in France: an analysis of the ANRS-PARCOURS retrospective population-based study. Lancet Public Health. 2018;3(1):e16–e23. doi: 10.1016/S2468-2667(17)30211-6. [DOI] [PubMed] [Google Scholar]
- 68.Nöstlinger C., Cosaert T., Landeghem E.V., et al. HIV among migrants in precarious circumstances in the EU and European Economic Area. Lancet HIV. 2022;9(6):e428–e437. doi: 10.1016/S2352-3018(22)00032-7. [DOI] [PubMed] [Google Scholar]
- 69.Dara M., Colombani P., Petrova-Benedict R., Centis R., Zellweger J.P., Sandgren A. Minimum package for cross-border TB control and care in the WHO European region: a Wolfheze consensus statement. Eur Respir J. 2012;40:1081–1090. doi: 10.1183/09031936.00053012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bozorgmehr K., Samuilova M., Petrova-Benedict R., Girardi E., Piselli P., Kentikelenis A. Infectious disease health services for refugees and asylum seekers during a time of crisis: a scoping study of six European Union countries. Health Policy. 2019;123(9):882–887. doi: 10.1016/j.healthpol.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 71.Piselli P., Samuilova M., Bozorgmehr K., et al. Infectious-disease screening and vaccination for refugees and asylum seekers entering Europe in 2015–16: a scoping study of six European union countries. J Refug Stud. 2019;32(Special_Issue_1):i92–i104. doi: 10.1016/j.healthpol.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 72.Mooney S.J., Pejaver V. Big data in public health: terminology, machine learning, and privacy. Annu Rev Publ Health. 2018;39(1):95–112. doi: 10.1146/annurev-publhealth-040617-014208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sayeed R., Gottlieb D., Mandl K.D. SMART markers: collecting patient-generated health data as a standardized property of health information technology. NPJ Digit Med. 2020;3:9. doi: 10.1038/s41746-020-0218-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Boston D., Cohen D., Stine J., et al. Agency of Healthcare Research and Quality; Rockville: 2021. Integrating patient-generated health data into electronic health records in ambulatory care settings: a practical guide. [Google Scholar]
- 75.Wickramage K., Mosca D. Can migration health assessments become a mechanism for global public health good? Int J Environ Res Publ Health. 2014;11(10):9954–9963. doi: 10.3390/ijerph111009954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sheikh K., Gilson L., Agyepong I.A., Hanson K., Ssengooba F., Bennett S. Building the field of health policy and systems research: framing the questions. PLoS Med. 2011;8(8) doi: 10.1371/journal.pmed.1001073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Biddle L., Bozorgmehr K., Jahn R. Oxford University Press; 2021. Health information systems and migrant health in Europe. [Google Scholar]
- 78.Kajikhina K., Koschollek C., Sarma N., et al. Recommendations for collecting and analysing migration-related determinants in public health research. J Health Monit. 2023;8(1):55–77. doi: 10.25646/11144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Spallek J., Spix C., Zeeb H., Kaatsch P., Razum O. Cancer patterns among children of Turkish descent in Germany: a study at the German Childhood Cancer Registry. BMC Publ Health. 2008;8(1):152. doi: 10.1186/1471-2458-8-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Razum O., Zeeb H., Beck K., Becher H., Ziegler H., Stegmaier C. Combining a name algorithm with a capture–recapture method to retrieve cases of Turkish descent from a German population-based cancer registry. Eur J Cancer. 2000;36(18):2380–2384. doi: 10.1016/s0959-8049(00)00333-6. [DOI] [PubMed] [Google Scholar]
- 81.Burns R., Pathak N., Campos-Matos I., et al. Million Migrants study of healthcare and mortality outcomes in non-EU migrants and refugees to England: analysis protocol for a linked population-based cohort study of 1.5 million migrants. Wellcome Open Res. 2019;4:4. doi: 10.12688/wellcomeopenres.15007.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pathak N., Zhang C.X., Boukari Y., et al. Development and validation of a primary care electronic health record phenotype to study migration and health in the UK. Int J Environ Res Publ Health. 2021;18(24) doi: 10.3390/ijerph182413304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhang C.X., Boukari Y., Pathak N., et al. Migrants’ primary care utilisation before and during the COVID-19 pandemic in England: an interrupted time series analysis. Lancet Reg Health Eur. 2022;20 doi: 10.1016/j.lanepe.2022.100455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bilgic L., Sarma N., Loer A.M., et al. [A guideline on discrimination-sensitive language in research on migration and health] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2022;65(12):1316–1323. doi: 10.1007/s00103-022-03620-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Vatsalan D., Karapiperis D., Verykios V.S. In: Encyclopedia of big data technologies. Sakr S., Zomaya A., editors. Springer International Publishing; Cham: 2018. Privacy-preserving record linkage; pp. 1–8. [Google Scholar]
- 86.Vatsalan D., Christen P., Verykios V.S. A taxonomy of privacy-preserving record linkage techniques. Inform Syst. 2013;38(6):946–969. [Google Scholar]
- 87.March S., Antoni M., Kieschke J., et al. Quo vadis data linkage in Germany? An initial inventory. Gesundheitswesen. 2018;80(3):20–31. doi: 10.1055/s-0043-125070. [DOI] [PubMed] [Google Scholar]
- 88.Christen P., Ranbaduge T., Schnell R. Methods and techniques for practical privacy-preserving information sharing. Springer; Cham: 2020. Linking sensitive data. [Google Scholar]
- 89.March S., Andrich S., Drepper J., et al. Good practice data linkage (GPD): a translation of the German version. Int J Environ Res Public Health. 2020;17(21):7852. doi: 10.3390/ijerph17217852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schnell R., Bachteler T., Reiher J. Privacy-preserving record linkage using Bloom filters. BMC Med Inform Decis Mak. 2009;9(1):41. doi: 10.1186/1472-6947-9-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Schnell R., Borgs C. Protecting record linkage identifiers using a language model for patient names. Stud Health Technol Inform. 2018;253:91–95. GMDS. [PubMed] [Google Scholar]
- 92.Aldridge R.W., Zenner D., White P.J., et al. Tuberculosis in migrants moving from high-incidence to low-incidence countries: a population-based cohort study of 519 955 migrants screened before entry to England, Wales, and Northern Ireland. Lancet. 2016;388(10059):2510–2518. doi: 10.1016/S0140-6736(16)31008-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Deal A., Hayward S.E., Crawshaw A.F., et al. Immunisation status of UK-bound refugees between January, 2018, and October, 2019: a retrospective, population-based cross-sectional study. Lancet Public Health. 2022;7(7):e606–e615. doi: 10.1016/S2468-2667(22)00089-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hamad R., Öztürk B., Foverskov E., et al. Association of neighborhood disadvantage with cardiovascular risk factors and events among refugees in Denmark. JAMA Netw Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.14196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.White J.S., Hamad R., Li X., et al. Long-term effects of neighbourhood deprivation on diabetes risk: quasi-experimental evidence from a refugee dispersal policy in Sweden. Lancet Diabetes Endocrinol. 2016;4(6):517–524. doi: 10.1016/S2213-8587(16)30009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Foverskov E., White J.S., Norredam M., et al. Neighbourhood socioeconomic disadvantage and psychiatric disorders among refugees: a population-based, quasi-experimental study in Denmark. Soc Psychiatr Psychiatr Epidemiol. 2022;58(5):711–721. doi: 10.1007/s00127-022-02300-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Reiss K., Berger U., Winkler V., Voigtländer S., Becher H., Razum O. Assessing the effect of regional deprivation on mortality avoiding compositional bias: a natural experiment. J Epidemiol Commun Health. 2013;67(3):213–218. doi: 10.1136/jech-2012-201336. [DOI] [PubMed] [Google Scholar]
- 98.Crawshaw A.F., Pareek M., Were J., et al. Infectious disease testing of UK-bound refugees: a population-based, cross-sectional study. BMC Med. 2018;16(1):143. doi: 10.1186/s12916-018-1125-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Burns R., Campos-Matos I., Harron K., Aldridge R.W. COVID-19 vaccination uptake for half a million non-EU migrants and refugees in England: a linked retrospective population-based cohort study. Lancet. 2022;400:S5. doi: 10.1016/S0140-6736(22)02215-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.van der Klis F.R., Mollema L., Berbers G.A., de Melker H.E., Coutinho R.A. Second national serum bank for population-based seroprevalence studies in the Netherlands. Neth J Med. 2009;67(7):301–308. [PubMed] [Google Scholar]
- 101.Harron K. Administrative Data Research Network (ADRN); Essex: 2016. An introduction to data linkage. [Google Scholar]
- 102.Zerka F., Barakat S., Walsh S., et al. Systematic review of privacy-preserving distributed machine learning from federated databases in health care. JCO Clin Cancer Inform. 2020;4:184–200. doi: 10.1200/CCI.19.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Appenzeller A., Bartholomäus S., Breitschwerdt R., et al. 2021 IEEE/ACS 18th international Conference on computer systems and applications (AICCSA); 2021 30 Nov.-3 Dec. 2021. 2021. Towards distributed healthcare systems – virtual data pooling between cancer registries as backbone of care and research; pp. 1–8. [Google Scholar]
- 104.Aminifar A., Shokri M., Rabbi F., Pun V.K.I., Lamo Y. Extremely randomized trees with privacy preservation for distributed structured health data. IEEE Access. 2022;10:6010–6027. [Google Scholar]
- 105.Kristoffersen E.S., Bjorvatn B., Halvorsen P.A., et al. The Norwegian PraksisNett: a nationwide practice-based research network with a novel IT infrastructure. Scand J Primary Health Care. 2022;40(2):217–226. doi: 10.1080/02813432.2022.2073966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Erdmann S., Biddle L., Kieser M., Bozorgmehr K. Using independent cross-sectional survey data to predict post-migration health trajectories among refugees by estimating transition probabilities and their variances. Biom J. 2022;64(5):964–983. doi: 10.1002/bimj.202100045. [DOI] [PubMed] [Google Scholar]
- 107.Jahn R., Rohleder S., Qreini M., et al. Health monitoring of refugees in reception centres for asylum seekers: decentralized surveillance network for the analysis of routine medical data. J Health Monit. 2021;6(1):30–52. doi: 10.25646/7865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.European Commission European health data Space. https://health.ec.europa.eu/ehealth-digital-health-and-care/european-health-data-space_en
- 109.Biddle L., Menold N., Bentner M., et al. Health monitoring among asylum seekers and refugees: a state-wide, cross-sectional, population-based study in Germany. Emerg Themes Epidemiol. 2019;16:3. doi: 10.1186/s12982-019-0085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Santos-Hövener C., Schumann M., Schmich P., Gößwald A., Rommel A., Ziese T. Improving the information base regarding the health of people with a migration background. Project description and initial findings from IMIRA. J Health Monit. 2019;4(1):46–57. doi: 10.25646/5874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Koschollek C., Kajikhina K., El Bcheraoui C., Wieler L.H., Michalski N., Hövener C. Public Health; 2023. SARS-CoV-2 infections in migrant populations in Germany: results from the COVID-19 Snapshot Monitoring Survey. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bug M., Blume M., Kajikhina K., et al. COVID-19 vaccination status among people with selected citizenships: results of the study GEDA Fokus. J Health Monit. 2023;8(1):34. doi: 10.25646/11142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wulkotte E., Bozorgmehr K. Trends and changes in socio-economic inequality in self-rated health among migrants and non-migrants: repeated cross-sectional analysis of national survey data in Germany, 1995-2017. Int J Environ Res Publ Health. 2022;19(14) doi: 10.3390/ijerph19148304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bauer J.M., Brand T., Zeeb H. Pre-migration socioeconomic status and post-migration health satisfaction among Syrian refugees in Germany: a cross-sectional analysis. PLoS Med. 2020;17(3) doi: 10.1371/journal.pmed.1003093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Costa D., Biddle L., Mühling C., Bozorgmehr K. Subjective social status mobility and mental health of asylum seekers and refugees: population-based, cross-sectional study in a German federal state. J Mig Health. 2020;1–2 doi: 10.1016/j.jmh.2020.100020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ambrosetti E., Dietrich H., Kosyakova Y., Patzina A. The impact of pre- and postarrival mechanisms on self-rated health and life satisfaction among refugees in Germany. Front Sociol. 2021;6 doi: 10.3389/fsoc.2021.693518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.ONS . Office for National Statistics; London: 2023. Visa holders entering the UK under the Ukraine humanitarian schemes, outcomes survey: 27 february to 13 March 2023. [Google Scholar]
- 118.Fu L., Lindenmeyer A., Phillimore J., Lessard-Phillips L. Vulnerable migrants’ access to healthcare in the early stages of the COVID-19 pandemic in the UK. Public Health. 2022;203:36–42. doi: 10.1016/j.puhe.2021.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.IOM Slovakia Data collection on mobility, needs and intentions of displaced populations due to war in Ukraine. 2022. https://www.iom.sk/en/activities/iom-response-ukraine/data-collection.html
- 120.WHO . WHO Regional Office for Europe; Copenhagen: 2023. WHO’s response to the Ukraine crisis: annual report, 2022. [Google Scholar]
- 121.Kumar B.N., James R., Hargreaves S., et al. Meeting the health needs of displaced people fleeing Ukraine: drawing on existing technical guidance and evidence. Lancet Reg Health Eur. 2022;17 doi: 10.1016/j.lanepe.2022.100403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Leitgöb H., Seddig D., Asparouhov T., et al. Measurement invariance in the social sciences: historical development, methodological challenges, state of the art, and future perspectives. Soc Sci Res. 2023;110 doi: 10.1016/j.ssresearch.2022.102805. [DOI] [PubMed] [Google Scholar]
- 123.Menold N., Biddle L., von Hermanni H., Kadel J., Bozorgmehr K. Ensuring cross-cultural data comparability by means of anchoring vignettes in heterogeneous refugee samples. BMC Med Res Methodol. 2023;23(1):213. doi: 10.1186/s12874-023-02015-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kadel J., Menold N., von Hermanni H. PH-LENS Working Paper Series. Universität Bielefeld; Bielefeld: 2022. Measurement Invariance of central social science and health constructs among Syrian, Iraq and Afghan refugee groups in Germany; p. 4. [Google Scholar]
- 125.Biddle L., Hintermeier M., Mohsenpour A., Sand M., Bozorgmehr K. Monitoring the health and healthcare provision for refugees in collective accommodation centres: results of the population-based survey RESPOND. J Health Monit. 2021;6(1):7–29. doi: 10.25646/7863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Georges D., Buber-Ennser I., Rengs B., Kohlenberger J., Doblhammer G. Health determinants among refugees in Austria and Germany: a propensity-matched comparative study for Syrian, Afghan, and Iraqi refugees. PLoS One. 2021;16(4) doi: 10.1371/journal.pone.0250821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kohlenberger J., Buber-Ennser I., Rengs B., Al Zalak Z. A social survey on refugees in and around Vienna in fall 2015: methodological approach and field observations. Refug Surv Q. 2017;36(4):90–109. [Google Scholar]
- 128.Chung R.Y.-N., Liao T.F., Fong E. Data collection for migrant live-in domestic workers: a three-stage cluster sampling method. Am Behav Sci. 2020;64(6):709–721. [Google Scholar]
- 129.Goodson L., Grzymala-Kazlowska A. Researching migration in a superdiverse society: challenges, methods, concerns and promises. Sociol Res Online. 2017;22(1):15–27. [Google Scholar]
- 130.MacFarlane A., Ogoro M., de Freitas C., Niranjan V., Severoni S., Waagensen E. Migrants’ involvement in health policy, service development and research in the WHO European Region: a narrative review of policy and practice. Trop Med Int Health. 2021;26(10):1164–1176. doi: 10.1111/tmi.13643. [DOI] [PubMed] [Google Scholar]
- 131.WHO . World Health Organization Regional Office for Europe; Copenhagen: 2021. Guidance for health information system governance. [Google Scholar]
- 132.Nkulu Kalengayi F.K., Hurtig A.-K., Ahlm C., Krantz I. Fear of deportation may limit legal immigrants’ access to HIV/AIDS-related care: a survey of Swedish language school students in Northern Sweden. J Immigr Minority Health. 2012;14:39–47. doi: 10.1007/s10903-011-9509-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Papageorgiou V., Wharton-Smith A., Campos-Matos I., Ward H. Patient data-sharing for immigration enforcement: a qualitative study of healthcare providers in England. BMJ Open. 2020;10(2) doi: 10.1136/bmjopen-2019-033202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Castaneda A., Rask S., Härkänen T., et al. Finnish Yearbook of Population Research; 2018. Enhancing survey participation among foreign-born populations: experiences from the Finnish migrant health and wellbeing study (Maamu) [Google Scholar]
- 135.Müllerschön J., Koschollek C., Santos-Hövener C., Kuehne A., Müller-Nordhorn J., Bremer V. Impact of health insurance status among migrants from sub-Saharan Africa on access to health care and HIV testing in Germany: a participatory cross-sectional survey. BMC Int Health Hum Right. 2019;19(1):1–13. doi: 10.1186/s12914-019-0189-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Roura M., LeMaster J.W., Hannigan A., et al. ‘If relevant, yes; if not, no’: general practitioner (GP) users and GP perceptions about asking ethnicity questions in Irish general practice: a qualitative analysis using normalization process theory. PLoS One. 2021;16(5) doi: 10.1371/journal.pone.0251192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.MacFarlane A., Puthoopparambil S.J., Waagensen E., et al. Framework for refugee and migrant health research in the WHO European Region. Trop Med Int Health. 2023;28(2):90–97. doi: 10.1111/tmi.13845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kuipers B.S., Higgs M., Kickert W., Tummers L., Grandia J., Van Der Voet J. The management of change in public organizations: a literature review. Publ Adm. 2014;92(1):1–20. [Google Scholar]
- 139.Burnes B. Kurt lewin and the planned approach to change: a Re-appraisal. J Manag Stud. 2004;41(6):977–1002. [Google Scholar]
- 140.Kondilis E., Papamichail D., Gallo V., Benos A. COVID-19 data gaps and lack of transparency undermine pandemic response. J Public Health. 2021;43(2):e307–e308. doi: 10.1093/pubmed/fdab016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pala K. COVID-19: case and death notification problems in Turkey. Turk Thorac J. 2020;21(3):213–214. doi: 10.5152/TurkThoracJ.2020.20744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Bozorgmehr K. Power of and power over COVID-19 response guidelines. Lancet. 2020;396(10260) doi: 10.1016/S0140-6736(20)32081-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Greek Ministry of Migration and Asylum . Updated situation: unaccompanied minors in Greece, March 2023. Hellenic Republic, Ministry of Migration and Asylum; Athens: 2023. [Google Scholar]
- 144.Greek Ministry of Migraton and Asylum . Hellenic Republic, Ministry of Migration and Asylum; Athens: 2023. Information note on the process of reception, asylum and integration: March 2023. [Google Scholar]
- 145.Kondilis E., Puchner K., Veizis A., Papatheodorou C., Benos A. Covid-19 and refugees, asylum seekers, and migrants in Greece. BMJ. 2020;369 doi: 10.1136/bmj.m2168. [DOI] [PubMed] [Google Scholar]
- 146.IOM . IOM Greece; Athens: 2022. Supporting the Greek Authorities in managing the national reception system for asylum seekers and vulnerable migrants (SMS) [Google Scholar]
- 147.Greek Ministry of National Defence . Hellenic Republic, Ministry of National Defence; Athens: 2021. Press release: EU co-funded actions of the Grrek Military Force in response to the migration - refugee crisis. [Google Scholar]
- 148.Hellenic National Public Health Organisation . National Public Health Organisation; Athens: 2023. Epidemiological surveillance in points of care for refugees/migrants. Weekly report: week 17/2023. [Google Scholar]
- 149.Hellenic National Public Health Organization . 2021. Epidemiological surveillance in points of care for refugees/migrants. Weekly report: week 1/2021. Athens: National Public Health Organisation. [Google Scholar]
- 150.Kondilis E., Papamichail D., McCann S., et al. The impact of the COVID-19 pandemic on refugees and asylum seekers in Greece: a retrospective analysis of national surveillance data from 2020. eClinicalMedicine. 2021;37 doi: 10.1016/j.eclinm.2021.100958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ministry of Health of the Republic of Turkey Sağlıkta dönüşüm programı (health transformation programme) 2003. https://extranet.who.int/mindbank/item/3885
- 152.Atun R., Aydin S., Chakraborty S., et al. Universal health coverage in Turkey: enhancement of equity. Lancet. 2013;382(9886):65–99. doi: 10.1016/S0140-6736(13)61051-X. [DOI] [PubMed] [Google Scholar]
- 153.Hone T., Gurol-Urganci I., Millett C., Başara B., Akdağ R., Atun R. Effect of primary health care reforms in Turkey on health service utilization and user satisfaction. Health Policy Plan. 2017;32(1):57–67. doi: 10.1093/heapol/czw098. [DOI] [PubMed] [Google Scholar]
- 154.Bayram H., Köktürk N., Elbek O., Kılınç O., Sayıner A., Dağlı E. Interference in scientific research on COVID-19 in Turkey. Lancet. 2020;396(10249):463–464. doi: 10.1016/S0140-6736(20)31691-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Aykaç N., Etiler N. COVID-19 mortality in Istanbul in association with air pollution and socioeconomic status: an ecological study. Environ Sci Pollut Res Int. 2022;29(9):13700–13708. doi: 10.1007/s11356-021-16624-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hacettepe University Institute of Population Studies . Hacettepe University Institute of Population Studies, T.R. Presidency of Turkey Directorate of Strategy and Budget and TÜBİTAK; Ankara: 2019. 2018 Turkey demographic and health survey. [Google Scholar]
- 157.Bozorgmehr K., Noest S., Thaiss H.M., Razum O. [Health care provisions for asylum-seekers : a nationwide survey of public health authorities in Germany] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2016;59(5):545–555. doi: 10.1007/s00103-016-2329-4. [DOI] [PubMed] [Google Scholar]
- 158.Bozorgmehr K., Hövener C. Monitoring refugee health: integrative approaches using surveys and routine data. J Health Monit. 2021;6(1):3–6. doi: 10.25646/7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.IOM . International Organization for Migration; Geneva: 2017. Migration Health Research to advance evidence based policy and practice in Sri Lanka. [Google Scholar]
- 160.Scapolo F., Tarchi D., Alvarez Alvarez M., et al. Publications Office of the European Union; Luxembourg: 2023. Atlas of migration - 2022. [Google Scholar]
- 161.Bozorgmehr K., Saint V., Kaasch A., Stuckler D., Kentikelenis A. COVID and the convergence of three crises in Europe. Lancet Public Health. 2020;5(5):e247–e248. doi: 10.1016/S2468-2667(20)30078-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Bozorgmehr K., Zick A., Hecker T. Resilience of health systems: understanding uncertainty uses, intersecting crises and cross-level interactions: comment on “Government actions and their relation to resilience in healthcare during the COVID-19 pandemic in New South Wales, Australia and Ontario, Canada”. Int J Health Policy Manag. 2022;11(9):1956–1959. doi: 10.34172/ijhpm.2022.7279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wickramage K., Annunziata G. Advancing health in migration governance, and migration in health governance. Lancet. 2018;392(10164):2528–2530. doi: 10.1016/S0140-6736(18)32855-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.