Abstract
Background
Neurological disorders are still prevalent in HIV-infected people. We aimed to determine the prevalence of neurological disorders and identify their risk factors in HIV-infected persons in Taiwan.
Methods
We identified 30,101 HIV-infected people between 2002 and 2016 from the National Health Insurance Research Database in Taiwan, and analyzed the incidence of neurological disorders. We applied a retrospective, nested case–control study design. The individuals with (case group) and without (control group) a neurological disorder were then matched by age, sex and time. Factors associated with neurological disorders were analyzed using a conditional logistic regression model, and a nomogram was generated to estimate the risk of developing a neurological disorder.
Results
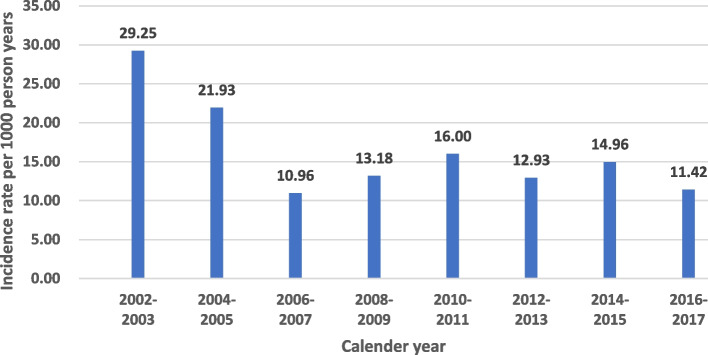
The incidence of neurological disorders was 13.67 per 1000 person-years. The incidence remained stable during the observation period despite the use of early treatment and more tolerable modern anti-retroviral therapy. The conditional logistic regression model identified nine clinical factors and comorbidities that were associated with neurological disorders, namely age, substance use, traumatic brain injury, psychiatric illness, HIV-associated opportunistic infections, frequency of emergency department visits, cART adherence, urbanization, and monthly income. These factors were used to establish the nomogram.
Conclusion
Neurological disorders are still prevalent in HIV-infected people in Taiwan. To efficiently identify those at risk, we established a nomogram with nine risk factors. This nomogram could prompt clinicians to initiate further evaluations and management of neurological disorders in this population.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12879-023-08761-4.
Keywords: HIV, Neurological disorders, National health insurance research database
Background
Due to the widespread use of combination antiretroviral therapy (cART), the life expectancy of individuals infected with human immunodeficiency virus (HIV) has improved and even approaches that of the general population [1]. However, a gap remains in comorbidity-free years between HIV-infected individuals and the general population [2]. In addition to comorbidities including cardiovascular diseases, cancers, diabetes, dyslipidemia and chronic renal diseases, which are prevalent in people living with HIV (PLWH)[3, 4], neuropsychiatric conditions are also common in PLWH [5]. The neurological complications of HIV are quite diverse, and in the early stages of infection can include meningitis, encephalitis and Bell's palsy. Late-stage symptoms include HIV-associated neurocognitive disorders, toxoplasma encephalitis, tuberculous meningitis, cryptococcal meningitis and neurosyphilis [6]. As with the other HIV-associated comorbidities, HIV-associated neurocognitive disorders are still prevalent in the modern cART era, with an overall prevalence rate of around 45% [7, 8]. These disorders can affect the quality of life and contribute to mortality in PLWH [9]. The pattern of HIV-associated neurocognitive disorders has changed in the recent two decades [10], and the prevalence may be underestimated due to a lack of awareness [11].
HIV also affects the central nervous system early in infection [12], and blood–brain barrier disruption has been demonstrated early in the course of primary HIV infection [13]. Thus, central nervous system infection caused by primary HIV infection or other pathogens (virus, bacteria, fungi) is also a common neurological complication in HIV-infected patients. However, there are limited data about neurological disorders in PLWH in the Asia–Pacific region [14, 15].
In Taiwan, cART has been provided free of charge since 1997. However, guidelines for the diagnosis and treatment of HIV/AIDS in Taiwan have recommended initiating cART according to different CD4 cell levels at different times: < 200 cells/mm3 in 2006, < 350 cells/mm3 in 2010, < 500 cells/mm3 in 2013, and "treat all" since 2016. Improvement in treatment coverage for PLWH was also implemented in other countries due to new scientific evidence around HIV treatment during this period of time [16]. Several studies have reported that CD4 nadir and CD4 count are predictors of HIV neurological disorders in the era of modern cART [17–19]. Thus, there may have been dynamic changes or even improvements in neurological disorders in PLWH in Taiwan during this time.
Several clinical factors and comorbidities have been reported to contribute to cognitive impairment in PLWH, including advanced HIV disease [17], duration of HIV infection [20, 21], obesity and diabetes [22], increased age [23], and hepatitis C infection [23]. In addition, alcohol use, substance abuse, traumatic brain injury, sleep disorders and psychiatric illnesses may also predispose to cognitive disorders in PLWH [24].
In the present study, we aimed to determine the dynamic changes in neurological disorders from 2002 to 2017, and to identify risk factors for neurological disorders in HIV-infected persons even under different treatment strategies in Taiwan.
Methods
Study population and study design
This was a retrospective, population-based, nested case–control study using clinical data retrieved from the Taiwan National Health Insurance Research Database (NHIRD). Patients with a diagnosis of HIV infection during the period from 1 January 2002 to 31 December 2016 were identified in the NHIRD. HIV infection is a notifiable disease in Taiwan and the cost of copayments for medical services for patients with HIV infection can be waived, and this can help to ensure the accuracy of the diagnosis of these patients.
Data source
By using the incidence of neurological disorders in HIV patients as the outcome variable, we excluded individuals with missing age or sex data and neurological disorders before the diagnosis of HIV infection. To estimate the effects of potential covariates on the risk of neurological disorders, a nested case–control study design with age, sex and time matching was applied in this study (Fig. 1). The primary outcome was the incidence of a first diagnosis of a neurological disorder after a diagnosis of HIV. Neurological disorders included neurocognitive disorders and central nervous system infections. The covariates were dyslipidemia, hepatitis C infection, substance use, alcoholism, traumatic brain injury, sleep apnea, sexually transmitted diseases, diabetes mellitus, psychiatric illnesses and HIV-associated opportunistic infections. These covariates were defined as the diagnoses recorded once or more during inpatient care or twice or more during ambulatory care within 1 year before the index date. Demographic profile (including sex, birth date, urbanization and monthly income), frequency of emergency department (ED) visits, and cART adherence were also extracted as covariates. The frequency of ED visits was analyzed because a previous study showed that ED visits were primarily driven by disease severity in people with HIV infection [25]. Adherence to cART was calculated as the proportion of days covered by dividing the number of days of ART coverage during the measurement period by the length of the measurement period [26]. Urbanization level was classified into urban, suburban and rural categories based on five aspects: population density, percentage of residents who were agricultural workers, the number of physicians per 100,000 people, percentage of residents with college or higher education, and percentage of residents aged 65 years or older [27].
Fig. 1.
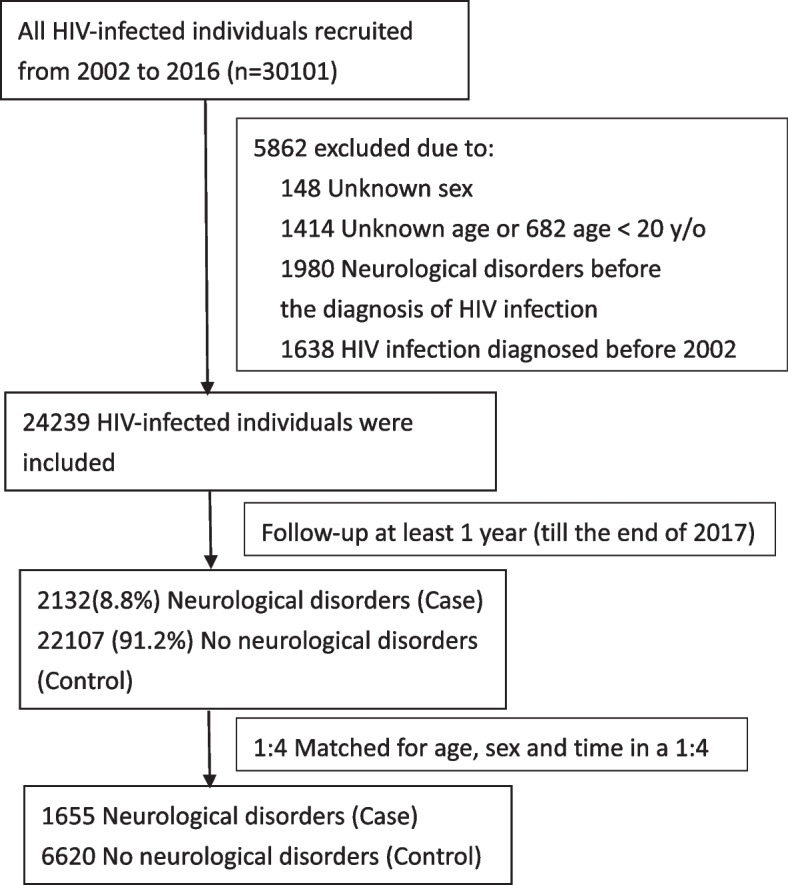
Flow chart of the HIV cohort for evaluating the risk of neurological disorders
Diagnoses in the NHIRD are coded based on International Classification of Diseases, Ninth Edition (ICD-9) and Tenth Edition (ICD-10) codes. ICD-9 codes were used between 2002 and 2014, and ICD-10 codes were used between 2015 and 2017. The ICD-9 and ICD-10 codes for the outcomes and covariates are provided in the Supplementary Table 1. The end of the observation period was defined as the occurrence of a neurological disorder, the end of 2017, or withdrawal from the National Health Insurance program.
This study was conducted after approval by the Institutional Review Board (IRB) of the National Cheng Kung University Hospital (B-EX-109–026). Since personal identification information is encrypted before releasing the data to researchers, informed consent was able to be waived from the IRB of the institute.
Statistical analysis
Incidence rates were expressed per 1000 prospective person-years of observation from 2002 through 2017. Continuous variables were compared using the Student's t test, and categorical variables were compared using the chi-square test or Fisher's exact test. Variables significantly associated with the risk of neurological disorders in univariate conditional logistic regression analysis were then selected to construct the final multivariate logistic regression model. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC). A p value < 0.05 was considered to be statistically significant.
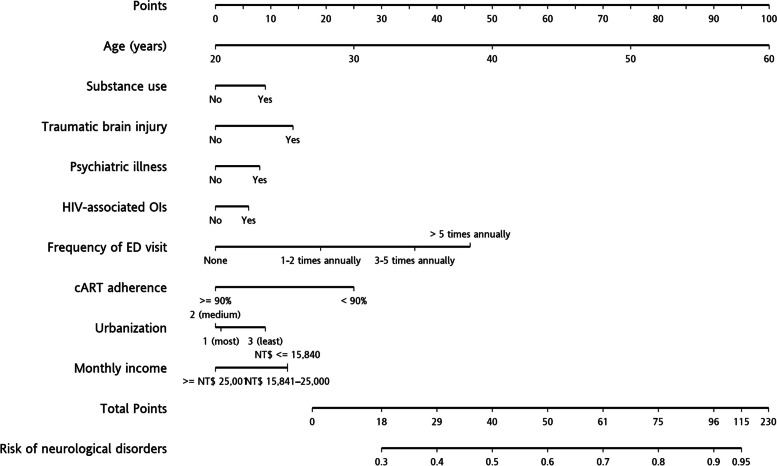
A nomogram is a two-dimensional diagram used to represent a mathematical function involving several predictors [28]. The variables significantly associated with the risk of neurological disorders in the multivariate logistic regression analysis were used to generate a nomogram.
Results
Demographic and clinical characteristics
A total of 30,101 HIV-infected people were identified from 2002 to 2016, of whom 24,239 were used for further matching. A total of 2132 (8.8%) individuals were diagnosed with neurological disorders during the follow-up period. Of the 2132 HIV-infected people with neurological disorders, 87.27% were male and the mean age (± standard deviation) at diagnosis was 38.5 ± 14.7 years. About 65.45% of individuals received cART therapy. Among these 2132 individuals, 1168 (54.8%) individuals have central nervous system infections, and 997 (46.8%) individuals have neurocognitive disorders. Half of the neurological disorders were identified before the initiation of cART. The proportion of central nervous system infections and neurocognitive disorders were quite similar before and after starting cART. The overall incidence of neurological disorders was 13.67 per 1000 person-years (Fig. 2). The incidence of central nervous system infections was 7.49 per 1000 person-years, and the incidence of neurocognitive disorders was 6.40 per 1000 person-years. The median time from the index date to a diagnosis of a neurological disorder was 3.6 years. The individuals with (case group) and without (control group) a neurological disorder were then matched by age, sex and time. The cases and controls were selected at a 1:4 ratio (Fig. 1). Table 1 shows the demographic and clinical characteristics of the case (n = 1655) and control (n = 6620) groups.
Fig. 2.
Incidence rate (per 1000 person-years) of neurological disorders among HIV-infected persons in Taiwan from 2002–2017
Table 1.
Demographic and clinical characteristics of the neurological disorders and control subjects used to identify possible risk factors in HIV-infected persons
| Control subjects (N = 6620) | Patients with neurological disorders (N = 1655) | |
|---|---|---|
| Variables | n (%) | n (%) |
| Duration of HIV infection (years) | ||
| Median (IQR) | 3.62 (1.23, 6.69) | 3.63 (1.21, 6.70) |
| Sex | ||
| Male | 6472 (97.76) | 1618 (97.76) |
| Female | 148 (2.24) | 37 (2.24) |
| Age (years) | ||
| Mean ± SD | 32.9 ± 7.2 | 33.0 ± 7.2 |
| Comorbidities (2 year before index date) | ||
| Dyslipidemia | 134 (2.02) | 33 (1.99) |
| Hepatitis C infection | 180 (2.72) | 88 (5.32) |
| Substance use | 418 (6.31) | 195 (11.78) |
| Alcoholism | 35 (0.53) | 32 (1.93) |
| Traumatic brain injury | 59(0.89) | 34 (2.05) |
| Sleep apnea | 11 (0.17) | 4 (0.24) |
| Sexually transmitted disease | 1319 (19.92) | 268 (16.19) |
| Diabetes mellitus | 86 (1.30) | 32 (1.93) |
| Psychiatric illness | 784 (11.84) | 316 (19.09) |
| HIV-associated OIs | 519 (7.84) | 170 (10.27) |
| Frequency of ED visits | ||
| None | 3404 (51.42) | 510 (30.82) |
| 1–2 times annually | 2671 (40.35) | 794 (47.98) |
| 3–5 times annually | 473 (7.15) | 279 (16.86) |
| >5 times annually | 72 (1.09) | 72 (4.35) |
| cART adherence | ||
| <90% PDC | 6514 (98.40) | 1640 (99.09) |
| ≥ 90% PDC | 106 (1.60) | 15 (0.91) |
| Urbanization | ||
| Urban | 2027 (30.62) | 395 (23.87) |
| Suburban | 1461 (22.07) | 306 (18.49) |
| Rural | 3132 (47.31) | 954 (57.64) |
| Monthly income | ||
| NT$≤ 15,840 | 2958 (44.68) | 879 (53.11) |
| NT$ 15,841–25,000 | 1888 (28.52) | 513 (31.00) |
| ≥ NT$ 25,001 | 1774 (26.80) | 263 (15.89) |
HIV Human immunodeficiency virus, IQR Interquartile range, SD Standard deviation, OIs Opportunistic infections, ED Emergency department, PDC Proportion of days covered, NT$ New Taiwan dollar
Factors associated with neurological disorders in the HIV-infected persons
Risk factors included in conditional logistic regression analysis were age at HIV diagnosis, dyslipidemia, hepatitis C infection, substance use, alcoholism, traumatic brain injury, sleep apnea, sexually transmitted diseases, diabetes mellitus, psychiatric illnesses, HIV-associated opportunistic infections, frequency of ED visits, cART adherence, urbanization level and monthly income. Odds ratios, adjusted odds ratios and their corresponding upper and lower 95% confidence intervals are presented in Table 2. In the univariate analysis, older age, hepatitis C infection, substance use, alcoholism, traumatic brain injury, sexually transmitted diseases, psychiatric illnesses, HIV-associated opportunistic infections, frequency of ED visits, cART adherence, urbanization and monthly income were associated with neurological disorders. Dyslipidemia, sleep apnea and diabetes were not associated with neurological disorders. In the multivariate analysis, hepatitis C infection, alcoholism and sexually transmitted diseases were no longer significant. Due to concerns about confounding by age, we then performed subgroup analyses of only younger subjects (arbitrarily defined as less than 40 years of age) and only older subjects (40 years or older). The results are shown in Table 3.
Table 2.
Crude and adjusted odds ratios of neurological disorders in HIV-infected persons
| Variables | Crude OR (95% CI) | p-value | aAdjusted OR (95% CI) | p-value |
|---|---|---|---|---|
| Age (years) | 1.11 (1.05–1.17) | <0.001* | 1.10 (1.04–1.16) | <0.001* |
| Comorbidities (2 year before index date) | ||||
| Dyslipidemia | 0.98 (0.66–1.46) | 0.936 | ||
| Hepatitis C infection | 2.01 (1.55–2.61) | < 0.001* | 1.27 (0.95–1.69) | 0.103 |
| Substance use | 2.06 (1.71–2.48) | <0.001* | 1.35 (1.10–1.67) | 0.005* |
| Alcoholism | 3.71 (2.29–6.02) | < 0.001* | 1.26 (0.74–2.16) | 0.398 |
| Traumatic brain injury | 2.36 (1.54–3.63) | < 0.001* | 1.69 (1.06–2.70) | 0.026* |
| Sleep apnea | 1.46 (0.46–4.57) | 0.521 | ||
| Sexually transmitted disease | 0.77 (0.67–0.89) | 0.001* | 0.88 (0.76–1.03) | 0.117 |
| Diabetes mellitus | 1.50 (1.00–2.26) | 0.053 | 1.12 (0.72–1.73) | 0.621 |
| Psychiatric illness | 1.76 (1.52–2.03) | <0.001* | 1.34 (1.15–1.57) | <0.001* |
| HIV-associated OIs | 1.35 (1.13–1.63) | 0.001* | 1.25 (1.03–1.52) | 0.026* |
| Frequency of ED visits | ||||
| None | Ref. | |||
| 1–2 times annually | 2.18 (1.92–2.48) | <0.001* | 2.12 (1.86–2.41) | <0.001* |
| 3–5 times annually | 4.44 (3.69–5.34) | <0.001* | 4.03 (3.34–4.87) | <0.001* |
| >5 times annually | 7.67 (5.38–10.92) | <0.001* | 5.90 (4.09–8.52) | <0.001* |
| cART adherence (in observation period) | ||||
| <90% | Ref. | Ref. | ||
| ≥90% | 0.48 (0.26–0.88) | 0.018* | 0.37 (0.20–0.71) | 0.003* |
| Urbanization | ||||
| Urban | Ref. | Ref. | ||
| Suburban | 1.07 (0.91–1.26) | 0.415 | 0.95 (0.80–1.12) | 0.524 |
| Rural | 1.61 (1.41–1.84) | <0.001* | 1.31 (1.13–1.51) | <0.001* |
| Monthly income | ||||
| NT$ ≤ 15,840 | Ref. | Ref. | ||
| NT$ 15,841–25,000 | 0.91 (0.80–1.03) | 0.117 | 0.98 (0.86–1.12) | 0.807 |
| ≥ NT$ 25,001 | 0.48 (0.41–0.56) | <0.001* | 0.61 (0.52–0.72) | <0.001* |
OR Odds ratio, CI Confidence interval, ED Emergency department, cART Combination antiretroviral therapy, NT$ New Taiwan dollar
*p-value ≤ 0.05
aAdjusted for age, hepatitis C infection, substance use, alcoholism, traumatic brain injury, sexually transmitted disease, psychiatric illness, HIV-associated OIs, frequency of ED visit, cART adherence, urbanization and monthly income
Table 3.
Adjusted odds ratios of neurological disorders in HIV-infected persons, stratification by age
| Variables | 20 ≤ Age < 40 | Age ≥ 40 | ||
|---|---|---|---|---|
| Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
| Comorbidities (2 year before index date) | ||||
| HCV infection | 1.34 (0.95–1.88) | 0.094 | 1.12 (0.64–1.97) | 0.696 |
| Substance use | 1.45 (1.13–1.86) | 0.003* | 1.01 (0.66–1.54) | 0.963 |
| Alcoholism | 1.23 (0.66–2.29) | 0.524 | 1.45 (0.48–4.40) | 0.516 |
| Traumatic brain injury | 1.42 (0.83–2.42) | 0.200 | 2.76 (0.98–7.78) | 0.055 |
| Sexually transmitted disease | 0.87 (0.73–1.03) | 0.097 | 0.93 (0.60–1.45) | 0.760 |
| Diabetes mellitus | 0.98 (0.52–1.84) | 0.952 | 1.24 (0.64–2.40) | 0.522 |
| Psychiatric illness | 1.23 (1.03–1.48) | 0.024* | 1.78 (1.27–2.51) | 0.001* |
| HIV-associated OIs | 1.37 (1.10–1.72) | 0.005* | 0.95 (0.62–1.45) | 0.806 |
| Frequency of ED visits | ||||
| None | Ref. | Ref. | ||
| 1–2 times annually | 2.18 (1.88–2.53) | <0.001* | 1.89 (1.39–2.56) | <0.001* |
| 3–5 times annually | 4.22 (3.41–5.22) | <0.001* | 3.19 (2.06–4.93) | <0.001* |
| > 5 times annually | 5.36 (3.58–8.01) | <0.001* | 14.20 (4.74–42.54) | <0.001* |
| cART adherence (in observation period) | ||||
| <90% | Ref. | Ref. | ||
| ≥90% | 0.41 (0.21–0.81) | 0.011* | 0.16 (0.02–1.34) | 0.091 |
| Urbanization | ||||
| Urban | Ref. | Ref. | ||
| Suburban | 0.97 (0.80–1.17) | 0.737 | 0.98 (0.64–1.50) | 0.930 |
| Rural | 1.29 (1.10–1.52) | 0.002* | 1.54 (1.07–2.23) | 0.021* |
| Monthly income | ||||
| NT$≤15,840 | Ref. | Ref. | ||
| NT$ 15,841–25,000 | 0.95 (0.82–1.10) | 0.481 | 1.12 (0.83–1.52) | 0.467 |
| ≥ NT$ 25,001 | 0.60 (0.50–0.73) | <0.001* | 0.67 (0.45–0.99) | 0.044* |
OR Odds ratio, CI Confidence interval, ED Emergency department, cART Combination antiretroviral therapy, NT$ New Taiwan dollar
*p-value ≤ 0.05
Nomogram
According to the multivariate analysis results, a nomogram was generated to estimate the risk of developing a neurological disorder as shown in Fig. 3. By summing the risk score for each factor as shown in the nomogram, the risk of developing a neurological disorder for each individual can be assessed.
Fig. 3.
Nomogram for predicting the development of neurological disorders in HIV-infected persons
Discussion
In this retrospective nested case–control study, we found several risk factors for neurological disorders in HIV-infected people and then developed a simple risk scoring system to identify those at risk. To the best of our knowledge, this scoring system is the first to be specifically designed for identifying neurological disorders in people infected with HIV. Several clinical factors and comorbidities have been reported to be associated with neurological disorders in HIV-infected people, including the frequency of ED visits [29], cART adherence [30, 31], advanced HIV disease [17], duration of HIV infection [20, 21], and older age [23]. Comorbidities including obesity, diabetes [22], hepatitis C infection [23], alcohol use, substance abuse, traumatic brain injury, sleep disorders and psychiatric illnesses [24] have also been associated with neurological disorders in HIV-infected people. The large number of factors which can contribute to the development of neurological disorders in this population makes it more complex to predict. Through the proposed nomogram with some basic clinical information, clinicians can identify those at risk and initiate further screening for comorbidities, drug compliance education, or even cognitive function evaluations. This nomogram may serve as a screening tool for identifying risk populations.
Educational attainment [32], tobacco use [33], and cART regimen [34, 35] can also influence neurocognitive function. Since educational attainment is closely related to the level of income [36, 37] and monthly income could be extracted from the NHIRD, we used monthly income as a covariate instead of educational attainment as data on educational attainment are not available in the NHIRD. However, more research is needed to evaluate whether adding more parameters (clinical factors and/or biomarkers) could better predict the development of neurological complications in HIV-infected people.
The incidence of neurological disorders in HIV-infected persons was stable from 2006 to 2017 (13.67 per 1000 person-years) even though early treatment and even a "treat all" policy was applied during this period and more tolerable modern cART was used. This finding is consistent with previous studies in which neurological complications were still prevalent in HIV-infected persons due to it being neuroinvasive, neurotropic and neurovirulent [38, 39]. Thus, neurological manifestations are an important concern among people with HIV infection.
In the subgroup analyses of only younger subjects and only older subjects, substance use was significantly associated with neurological disorders in the younger subjects(adjusted HR = 1.45, p = 0.003), but not in the older subjects(adjusted HR = 1.01, p = 0.963). This may be because substance use is typically higher in adolescents and young adults, and the neurological complications of substance use can occur in both acute and early HIV infection [40]. This should raise awareness of neurological disorders in young HIV-infected people with substance use disorders.
The key strength of this study is the application of a nationwide database to identify predictors of neurological disorders. The high coverage, easy accessibility, and low copayments result in high adherence of beneficiaries to the National Health Insurance program, which minimizes potential selection and information biases.
Some limitations should also be addressed. First, some risk factors for neurological disorders such as low CD4 cell count, high blood viral load, low educational attainment, tobacco use and cART regimen are not included in the NHIRD and could not be incorporated into the scoring system. Both CD4 cell count and blood viral load are important predictors of outcomes in HIV-infected persons [17, 41]. In addition, we used HIV-associated opportunistic infections as a proxy for advanced HIV status. Second, the diagnosis of neurological disorders and comorbidities depended on claims data from the NHIRD, and physicians who cared for these patients were not neurologists, which may have led to underestimation of the proportion of neurological disorders. Third, cART adherence was calculated by the proportion of days covered, and the actual adherence rate may have been lower, especially in those with neurological disorders [42, 43].
In conclusion, neurological disorders are still prevalent in HIV-infected persons. To efficiently identify those at risk, we established a nomogram with nine risk factors. This nomogram could prompt clinicians to initiate further evaluations and management of neurological disorders.
Supplementary Information
Additional file 1: Supplementary Table 1. ICD-9 and ICD 10 codes used for neurological disorders and covariates.
Acknowledgements
We are grateful to all research assistants for providing the statistical consulting services from the Biostatistics Consulting Center, Clinical Medicine Research Center, National Cheng Kung University Hospital.
Abbreviations
- cART
Combination antiretroviral therapy
- ED
Emergency department
- HIV
Human immunodeficiency virus
- ICD-9/10
International Classification of Diseases, Ninth/Tenth Edition
- NHIRD
National Health Insurance Research Database
- PLWH
People living with HIV
Authors’ contributions
YWW, SJL, HCT and SHL conceived the study and designed the protocol. YWW, CHH and SHL performed the data management and analyses. YWW drafted the paper. SJL and HCT revised the manuscript. SHL provided critical revisions and supervised the paper. All authors contributed to and approved the final paper.
Funding
This work was supported by Kaohsiung Veterans General Hospital (KSVGH110-D08-1 to YWW) and Veterans Affairs Council, Republic of China (VAC112-001).
Availability of data and materials
The de-linked datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. The data are not publicly available because the use of the National Health Insurance Research Database is limited to research purposes only.
Declarations
Ethics approval and consent to participate
This study was conducted after approval by the Institutional Review Board (IRB) of the National Cheng Kung University Hospital (B-EX-109–026). Since personal identification information is encrypted before releasing the data to researchers, informed consent was able to be waived from the Institutional Review Board (IRB) of the National Cheng Kung University Hospital (B-EX-109–026). And all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Antiretroviral Therapy Cohort C Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV. 2017;4(8):e349–e356. doi: 10.1016/S2352-3018(17)30066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Increased overall life expectancy but not comorbidityfree years for people with HIV. https://www.croiconference.org/wp-content/uploads/sites/2/resources/2020/program-information/croi2020-program-and-information-guide.pdf .
- 3.Pourcher V, Gourmelen J, Bureau I, Bouee S. Comorbidities in people living with HIV: an epidemiologic and economic analysis using a claims database in France. PLoS One. 2020;15(12):e0243529. doi: 10.1371/journal.pone.0243529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roomaney RA, van Wyk B, Pillay-van Wyk V: Aging with HIV: Increased Risk of HIV Comorbidities in Older Adults. Int J Environ Res Public Health 2022, 19(4). [DOI] [PMC free article] [PubMed]
- 5.Owe-Larsson B, Sall L, Salamon E, Allgulander C. HIV infection and psychiatric illness. Afr J Psychiatry (Johannesbg) 2009;12(2):115–128. doi: 10.4314/ajpsy.v12i2.43729. [DOI] [PubMed] [Google Scholar]
- 6.Thakur KT, Boubour A, Saylor D, Das M, Bearden DR, Birbeck GL. Global HIV neurology: a comprehensive review. AIDS. 2019;33(2):163–184. doi: 10.1097/QAD.0000000000001796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y, Liu M, Lu Q, Farrell M, Lappin JM, Shi J, Lu L, Bao Y. Global prevalence and burden of HIV-associated neurocognitive disorder: a meta-analysis. Neurology. 2020;95(19):e2610–e2621. doi: 10.1212/WNL.0000000000010752. [DOI] [PubMed] [Google Scholar]
- 8.Wei J, Hou J, Su B, Jiang T, Guo C, Wang W, Zhang Y, Chang B, Wu H, Zhang T. The prevalence of frascati-criteria-based HIV-Associated Neurocognitive Disorder (HAND) in HIV-Infected Adults: a systematic review and meta-analysis. Front Neurol. 2020;11:581346. doi: 10.3389/fneur.2020.581346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banerjee N, McIntosh RC, Ironson G. Impaired neurocognitive performance and mortality in HIV: assessing the prognostic value of the HIV-dementia scale. AIDS Behav. 2019;23(12):3482–3492. doi: 10.1007/s10461-019-02423-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heaton RK, Franklin DR, Ellis RJ, McCutchan JA, Letendre SL, Leblanc S, Corkran SH, Duarte NA, Clifford DB, Woods SP, et al. HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. J Neurovirol. 2011;17(1):3–16. doi: 10.1007/s13365-010-0006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ian E, Gwen CL, Soo CT, Melissa C, Chun-Kai H, Eosu K, Hyo-Youl K, Asad K, Scott L, Chung-Ki LP, et al. The burden of HIV-associated neurocognitive disorder (HAND) in the Asia-Pacific region and recommendations for screening. Asian J Psychiatr. 2016;22:182–189. doi: 10.1016/j.ajp.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 12.Valcour V, Chalermchai T, Sailasuta N, Marovich M, Lerdlum S, Suttichom D, Suwanwela NC, Jagodzinski L, Michael N, Spudich S, et al. Central nervous system viral invasion and inflammation during acute HIV infection. J Infect Dis. 2012;206(2):275–282. doi: 10.1093/infdis/jis326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rahimy E, Li FY, Hagberg L, Fuchs D, Robertson K, Meyerhoff DJ, Zetterberg H, Price RW, Gisslen M, Spudich S. Blood-Brain Barrier Disruption Is Initiated During Primary HIV Infection and Not Rapidly Altered by Antiretroviral Therapy. J Infect Dis. 2017;215(7):1132–1140. doi: 10.1093/infdis/jix013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan FCC, Chan P, Chan I, Chan A, Tang THC, Lam W, Fong WC, Lee MP, Li P, Chan GHF. Cognitive screening in treatment-naive HIV-infected individuals in Hong Kong - a single center study. BMC Infect Dis. 2019;19(1):156. doi: 10.1186/s12879-019-3784-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cysique LA, Letendre SL, Ake C, Jin H, Franklin DR, Gupta S, Shi C, Yu X, Wu Z, Abramson IS, et al. Incidence and nature of cognitive decline over 1 year among HIV-infected former plasma donors in China. AIDS. 2010;24(7):983–990. doi: 10.1097/QAD.0b013e32833336c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta S, Williams B, Montaner J. Realizing the potential of treatment as prevention: global ART policy and treatment coverage. Curr HIV/AIDS Rep. 2014;11(4):479–486. doi: 10.1007/s11904-014-0230-z. [DOI] [PubMed] [Google Scholar]
- 17.Ellis RJ, Badiee J, Vaida F, Letendre S, Heaton RK, Clifford D, Collier AC, Gelman B, McArthur J, Morgello S, et al. CD4 nadir is a predictor of HIV neurocognitive impairment in the era of combination antiretroviral therapy. AIDS. 2011;25(14):1747–1751. doi: 10.1097/QAD.0b013e32834a40cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walker KA, Brown GG. HIV-associated executive dysfunction in the era of modern antiretroviral therapy: a systematic review and meta-analysis. J Clin Exp Neuropsychol. 2018;40(4):357–376. doi: 10.1080/13803395.2017.1349879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yusuf AJ, Hassan A, Mamman AI, Muktar HM, Suleiman AM, Baiyewu O. Prevalence of HIV-Associated Neurocognitive Disorder (HAND) among Patients Attending a Tertiary Health Facility in Northern Nigeria. J Int Assoc Provid AIDS Care. 2017;16(1):48–55. doi: 10.1177/2325957414553839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wright EJ, Grund B, Cysique LA, Robertson KR, Brew BJ, Collins G, Shlay JC, Winston A, Read TR, Price RW, et al. Factors associated with neurocognitive test performance at baseline: a substudy of the INSIGHT Strategic Timing of AntiRetroviral Treatment (START) trial. HIV Med. 2015;16(Suppl 1):97–108. doi: 10.1111/hiv.12238. [DOI] [PubMed] [Google Scholar]
- 21.McCutchan JA, Marquie-Beck JA, Fitzsimons CA, Letendre SL, Ellis RJ, Heaton RK, Wolfson T, Rosario D, Alexander TJ, Marra C, et al. Role of obesity, metabolic variables, and diabetes in HIV-associated neurocognitive disorder. Neurology. 2012;78(7):485–492. doi: 10.1212/WNL.0b013e3182478d64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCombe JA, Vivithanaporn P, Gill MJ, Power C. Predictors of symptomatic HIV-associated neurocognitive disorders in universal health care. HIV Med. 2013;14(2):99–107. doi: 10.1111/j.1468-1293.2012.01043.x. [DOI] [PubMed] [Google Scholar]
- 23.Fabbiani M, Ciccarelli N, Castelli V, Soria A, Borghetti A, Colella E, Moschese D, Valsecchi M, Emiliozzi A, Gori A, et al. Hepatitis C virus-related factors associated WITH cognitive performance in HIV-HCV-coinfected patients. J Neurovirol. 2019;25(6):866–873. doi: 10.1007/s13365-019-00780-9. [DOI] [PubMed] [Google Scholar]
- 24.Winston A, Spudich S. Cognitive disorders in people living with HIV. Lancet HIV. 2020;7(7):e504–e513. doi: 10.1016/S2352-3018(20)30107-7. [DOI] [PubMed] [Google Scholar]
- 25.Pezzin LE, Fleishman JA. Is outpatient care associated with lower use of inpatient and emergency care? An analysis of persons with HIV disease. Acad Emerg Med. 2003;10(11):1228–1238. doi: 10.1197/S1069-6563(03)00493-7. [DOI] [PubMed] [Google Scholar]
- 26.Nau DPJS, VA: Pharmacy Quality Alliance: Proportion of days covered (PDC) as a preferred method of measuring medication adherence. 2012, 6:25.
- 27.Chieh Yu Liu, Yunh Tai Hung, Yi Li Chuang, Yi Ju Chen, Wen Shun Weng, Jih Shin Liu, Kung Yee Liang: Incorporating Development Stratification of Taiwan Townships into Sampling Design of Large Scale Health Interview Survey. 2006, 4(1):1-22.
- 28.Kattan MW. Nomograms are superior to staging and risk grouping systems for identifying high-risk patients: preoperative application in prostate cancer. Curr Opin Urol. 2003;13(2):111–116. doi: 10.1097/00042307-200303000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Tsai YT, Chen YC, Hsieh CY, Ko WC, Ko NY. Incidence of neurological disorders among HIV-infected individuals with universal health care in Taiwan from 2000 to 2010. J Acquir Immune Defic Syndr. 2017;75(5):509–516. doi: 10.1097/QAI.0000000000001448. [DOI] [PubMed] [Google Scholar]
- 30.Wright MJ, Woo E, Foley J, Ettenhofer ML, Cottingham ME, Gooding AL, Jang J, Kim MS, Castellon SA, Miller EN, et al. Antiretroviral adherence and the nature of HIV-associated verbal memory impairment. J Neuropsychiatry Clin Neurosci. 2011;23(3):324–331. doi: 10.1176/jnp.23.3.jnp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Obermeit LC, Morgan EE, Casaletto KB, Grant I, Woods SP. Group HIVNRP: antiretroviral non-adherence is associated with a retrieval profile of deficits in verbal episodic memory. Clin Neuropsychol. 2015;29(2):197–213. doi: 10.1080/13854046.2015.1018950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lovden M, Fratiglioni L, Glymour MM, Lindenberger U, Tucker-Drob EM. Education and cognitive functioning across the life span. Psychol Sci Public Interest. 2020;21(1):6–41. doi: 10.1177/1529100620920576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kariuki W, Manuel JI, Kariuki N, Tuchman E, O'Neal J, Lalanne GA. HIV and smoking: associated risks and prevention strategies. HIV AIDS (Auckl) 2016;8:17–36. doi: 10.2147/HIV.S56952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ma Q, Vaida F, Wong J, Sanders CA, Kao YT, Croteau D, Clifford DB, Collier AC, Gelman BB, Marra CM, et al. Long-term efavirenz use is associated with worse neurocognitive functioning in HIV-infected patients. J Neurovirol. 2016;22(2):170–178. doi: 10.1007/s13365-015-0382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mollan KR, Smurzynski M, Eron JJ, Daar ES, Campbell TB, Sax PE, Gulick RM, Na L, O'Keefe L, Robertson KR, et al. Association between efavirenz as initial therapy for HIV-1 infection and increased risk for suicidal ideation or attempted or completed suicide: an analysis of trial data. Ann Intern Med. 2014;161(1):1–10. doi: 10.7326/M14-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.The relationship between education, income, economic freedom and happiness. https://www.shs-conferences.org/articles/shsconf/pdf/2020/03/shsconf_ichtml_2020_03004.pdf.
- 37.Carlson R, McChesney CJTE: Income sustainability through educational attainment. 2015, 4(1).
- 38.Uwishema O, Ayoub G, Badri R, Onyeaka H, Berjaoui C, Karabulut E, Anis H, Sammour C, Mohammed Yagoub FEA, Chalhoub E. Neurological disorders in HIV: Hope despite challenges. Immun Inflamm Dis. 2022;10(3):e591. doi: 10.1002/iid3.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kranick SM, Nath A. Neurologic complications of HIV-1 infection and its treatment in the era of antiretroviral therapy. Continuum (Minneap Minn) 2012;18(6 Infectious Disease):1319–1337. doi: 10.1212/01.CON.0000423849.24900.ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weber E, Morgan EE, Iudicello JE, Blackstone K, Grant I, Ellis RJ, Letendre SL, Little S, Morris S, Smith DM, et al. Substance use is a risk factor for neurocognitive deficits and neuropsychiatric distress in acute and early HIV infection. J Neurovirol. 2013;19(1):65–74. doi: 10.1007/s13365-012-0141-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Simpson DM, Haidich AB, Schifitto G, Yiannoutsos CT, Geraci AP, McArthur JC, Katzenstein DA. team As: Severity of HIV-associated neuropathy is associated with plasma HIV-1 RNA levels. AIDS. 2002;16(3):407–412. doi: 10.1097/00002030-200202150-00012. [DOI] [PubMed] [Google Scholar]
- 42.Hinkin CH, Castellon SA, Durvasula RS, Hardy DJ, Lam MN, Mason KI, Thrasher D, Goetz MB, Stefaniak M. Medication adherence among HIV+ adults: effects of cognitive dysfunction and regimen complexity. Neurology. 2002;59(12):1944–1950. doi: 10.1212/01.WNL.0000038347.48137.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weikum D. Neurocognitive Impairment Impacts Hiv Medication Adherence. 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Table 1. ICD-9 and ICD 10 codes used for neurological disorders and covariates.
Data Availability Statement
The de-linked datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. The data are not publicly available because the use of the National Health Insurance Research Database is limited to research purposes only.