Abstract
Background:
People who tend to impulsively choose smaller, sooner rewards over larger, later rewards are at increased risk for addiction and psychiatric disorders. A neurobiological measure of the tendency to overvalue immediate gratification could facilitate the study of individuals who are susceptible to these mental disorders. The objective of this research was to develop a cortical assay of impulsive choice for immediate rewards.
Methods:
A cortex-based assay of impulsive choice was developed using 1,105 healthy adults from the Human Connectome Project, and then cross-validated in two independent samples of adults with elevated rates of psychiatric disorders.
Results:
Study 1: Cortical-delay discounting (C-DD) was developed using a multivariate additive model of gray matter thickness across both hemispheres. Higher C-DD corresponded to thinner cortex and greater impulsive choice for immediate reward. It also predicted cannabis use beyond established risk factors for drug use, including familial substance use, childhood conduct problems, personality traits, and cognitive functioning. Study 2: C-DD replicated the association with delay discounting performance from Study 1. Structural equation modeling showed C-DD covaried with symptoms of externalizing, but not internalizing disorders. Study 3: C-DD positively predicted future delay discounting behavior (6-34 months later).
Conclusions:
Across three studies, a cortical assay of impulsive choice evidenced consistent associations with drug use and delay discounting task performance. It was also uniquely associated with psychiatric disorders that share impulsivity as a core feature. Together, findings support the utility of C-DD as a neurobiological assay of impulsive decision-making and a possible biomarker of externalizing disorders.
Keywords: cortical thickness, delay discounting, externalizing disorders, substance use, reward valuation
It is generally accepted that larger rewards are more desirable than smaller ones, and rewards that are immediately available are preferable to those that are delayed in time. However, everyday decisions are rarely so clean-cut and often require individuals to choose between pursuing rewards that are highly valued, but whose benefit is not immediately evident (e.g., avoiding illness during a pandemic), versus those that are immediately available but less valuable in the long run (e.g., drinking at a bar with friends). Across species and reward types, delay discounting paradigms have proven to be robust measures of the tendency to impulsively choose immediate rewards, a decision-making style with strong predictive validity for explaining addictive behaviors and psychiatric disorders (Amlung et al., 2019; Amlung et al., 2017; Bickel et al., 2019; Yoon et al., 2007). Discounting paradigms are used to estimate the rate at which an individual devalues rewards as a function of time (i.e., delay-discounting rate or k value) (Odum, 2011a). Individuals with addiction show particularly steep discounting rates (Amlung et al., 2017), as do those with externalizing spectrum disorders, characterized by chronic drug and alcohol use, impulsivity, and antisocial behavior (Bobova, Finn, Rickert, & Lucas, 2009; Finn, Gunn, & Gerst, 2015).
Efforts to identify biomarkers of delay discounting have focused on cortical regions that regulate impulsive urges and evaluate future outcomes, and limbic/paralimbic structures that value reinforcers (McClure, Laibson, Loewenstein, & Cohen, 2004; Noda et al., 2020). In terms of structural abnormalities, steeper discounting has been associated with decreased cortical thickness and/or gray-matter volume in several regions of the prefrontal cortex (Barry, Koeppel, & Ho, 2020; Bernhardt et al., 2014; Bjork, Momenan, & Hommer, 2009), as well as the cingulate (Bernhardt et al., 2014; Cho et al., 2013) and putamen (Cho et al., 2013; Dombrovski et al., 2012). The largest published study of adults to date (N=1,038) found that delay discounting increased as gray matter volume decreased in 20 discrete regions across the cortex, and total cortical (but not total subcortical) gray matter volume was inversely related to delay discounting (Owens et al., 2017). Based on these findings, it is clear the tendency to discount future rewards is not limited to a small subset of cortical regions, but rather evidences widespread associations across the cortex. The broad spectrum of regions that have been associated with delay discounting suggests a cortical assay of impulsive choice that incorporates many regions is needed to represent the cognitive neural underpinnings of this complex decision-making process.
To test the utility of such a measure, we created a cortical delay discounting (C-DD) assay using a multivariate additive model of gray matter thickness across 148 brain regions. Although subcortical regions likely play a role in impulsive choice, we focused on cortical thickness based on the findings of Owens and colleagues (2017), which is the largest structural study of delay discounting to date. We did not consider functional activation or connectivity in creation of C-DD, because we were interested in developing a neurobiological metric of impulsive choice with relatively stable trait-like properties that could be easily implemented by researchers using widely available neuroimaging scans. As cortical thickness tends to have greater temporal stability and reliability than functional neuroimaging measures (e.g., Han et al., 2006; Noble, Spann, Tokoglu, Shen, Constable, & Scheinost, 2017), and T1-weighted anatomical scans are collected in all MRI research studies and routinely collected clinically, we focused exclusively on cortical thickness as our neurobiological metric. We hypothesized that this cortical assay would reliably relate to known correlates of impulsive choice, specifically drug use, delay discounting rate, and externalizing disorder symptoms. To avoid the confounds that arise in highly impulsive samples (e.g., the effects of long-term substance use on cortical thickness), we used a large healthy sample to develop the cortical assay and then cross-validated it in two independent samples with elevated rates of psychiatric disorders.
Methods
Participants
Study 1:
All 1,105 healthy adults [506 men (45.8%)] aged 22-37 (M/SD = 28.8/3.7) with cortical thickness and delay discounting data from the Human Connectome Project (Van Essen et al., 2012) were included in analyses. Inclusion criteria were: ages 22-35 and ability to give valid informed consent. Exclusion criteria were: significant history of psychiatric disorder or substance abuse, serious neurological or medical conditions (e.g., cardiovascular disease, history of seizures, multiple sclerosis), genetic disorders, head injuries, premature birth, history of chemotherapy or radiation treatment, thyroid hormone treatment, current treatment for diabetes, use of daily migraine medication, and contraindications to MRI (metal in body, pregnancy, claustrophobia). The sample was predominantly White (74.8%) [Black/African-American (15.1%), Asian/Native Hawaiian/Pacific Islander (5.7%) and Other Race (2.7%)], with 8.6% identifying as Latino/a. Informed consent was acquired by the HCP and approved by the Washington University Institutional Review Board.
Study 2.
A community sample of 152 adults [77 men (50.7%)] aged 18–50 (M/SD = 31.3/8.3) were recruited using flyers and online advertisements for a study on risky behavior. Inclusion criteria were: ages 18-50 and English fluency. Exclusion criteria were: current psychosis, serious medical or neurological condition (e.g., epilepsy), or other contraindications to MRI. Three individuals with unreliable task or interview data were excluded from analyses. Six individuals were excluded due to unusable neuroimaging data due to movement (final N = 152). The sample was diverse (52.0% White, 34.4% Black, 8.6% Asian, 4.7% Other race, 15.1% Latino/a) and socioeconomically disadvantaged (median household income was $35,000, 51.3% participants reported prior justice-system involvement). Informed consent was obtained before participation. University of Delaware’s Institutional Review Board approved all protocols and procedures (Protocol #’s: 1073423-17, 1361164-1).
Study 3.
A sample of 73 adults [34 men (46.6%)] aged 19–50 (M/SD = 30.5/8.0) were recruited from a larger sample that completed an MRI study between 179-1042 days (M/SD = 579.7/241.5) prior to a follow-up delay discounting assessment. A subset of these participants also participated in Study 2 (n=34). Inclusion criteria were: ages 18-50 and English fluency. Exclusion criteria were: current psychosis, serious medical or neurological condition (e.g., epilepsy), or other contraindications to MRI. The sample was diverse (57.5% White, 24.7% Black, 13.7% Asian, 4.1% Other race, 20.5% Latino/a) and socioeconomically disadvantaged (median household income was $38,000, 41.1% participants reported prior justice-system involvement). Informed consent was obtained before participation. University of Delaware’s Institutional Review Board approved all protocols and procedures (Protocol #’s: 1073423-17, 1361164-1).
Measures
MRI Acquisition.
Study 1.
Structural data were acquired on a modified Siemens 3T Skyra System using a 32-channel coil. Two T1-weighted MPRAGE scans were acquired (resolution = 0.7mm3; TR = 2400ms; TE = 2.14ms; TI = 1000ms; flip angle = 8°), and the images were averaged together to increase signal to noise. Two T2-weighted images were acquired using a variable flip angle turbo-spin echo sequence (resolution = 0.7mm3; TR=3200 ms; TE=565 ms) and averaged.
Study 2-3.
Data were collected using a Siemens 3T Magnetom Prisma scanner with a 64-channel head coil. A T1-weighted multi-echo MPRAGE anatomical scan (resolution = 1mm3, TR = 2530ms, TEs = 1.69,3.55,5.41,7.27ms) was collected, which has the advantage of less distortion and higher contrast than standard MPRAGE sequences, resulting in more reliable cortical models (van der Kouwe et al., 2008). A T2-weighted variable flip-angle turbo spin-echo scan (resolution = 1mm3, TR = 3200ms, TE = 564ms) was also collected.
Cortical Thickness.
Thickness of the cortical mantle was estimated using FreeSurfer’s (v6) standard morphometric pipeline (Glasser et al., 2013). T1 and T2 images were visually inspected and at least two trained raters examined the data for errors, including the inclusion of dura or skull after brain extraction or errors in the pial or white matter surfaces. Cortical thickness was calculated for each parcellation derived from the FreeSurfer Destrieux Atlas which parcellates the cortex into 74 neuroanatomically-distinct structures for each hemisphere (Destrieux, Fischl, Dale, & Halgren, 2010; van der Kouwe, Benner, Salat, & Fischl, 2008).
Delay Discounting.
Participants chose between hypothetical monetary rewards, where one reward is smaller but available sooner and the other reward is larger but delayed (Odum, 2011a). Indifference points at each temporal delay were used to calculate k-values using Mazur’s hyperbolic equation (Mazur, 1987) as an estimate of the delay discounting rate (Odum, 2011a). Since discount rates are not normally distributed, the estimated k-values were natural-log-transformed. Larger values of ln k indicated a greater degree of discounting future rewards. The tasks used varied across the studies and details are provided in Supplemental Materials.
Cannabis Use.
In Study 1, lifetime cannabis use was assessed with the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA; Bucholz et al., 1994) and measured on a 5-point scale (never = 0; 1-5x = 1; 6-10 = 2; 11-100 = 3; 101-999 = 4; >1000 = 5; M/SD = 1.4/1.7). Recent cannabis use was assessed with a positive THC urine drug screen (Alere iScreen 6-panel urine drug test dip card; DOA-164-551), which occurred in 11.2% of the sample.
Psychiatric Disorders.
In Study 2, psychiatric symptoms were assessed with the Structured Clinical Interview for DSM-5 (SCID-5; First, Williams, Karg, & Spitzer, 2015) administered by a Clinical Psychologist or advanced doctoral student. Reliability among raters was high (ICC= 0.95–0.98). Symptom totals reflect summed threshold and subthreshold symptoms for the most severe lifetime episode (where applicable): Alcohol Use Disorder (M/SD = 2.5/3.4 symptoms), Substance Use Disorders (M/SD = 4.0/4.4 symptoms; based on the drug selected as “most problematic” from cannabis, stimulants, opioids, sedatives, hallucinogens), Antisocial Personality Disorder (M/SD = 3.4/4.1 symptoms), Major Depressive Disorder (M/SD = 3.6/3.8 symptoms), Panic Disorder (M/SD = 0.8/1.3 symptoms), Social Anxiety Disorder (M/SD = 0.8/2.1 symptoms), and Generalized Anxiety Disorder (M/SD = 0.6/1.2 symptoms).
Control Variables.
To examine the incremental validity of the cortical assay above existing predictors of drug use, we included demographic characteristics, parental history of substance use problems (parent had drug/alcohol problems: present = 1, absent = 0), childhood conduct problems (SSAGA number of behavioral problems before age 15 scaled from none = 0 to 3+ = 3), and normal personality traits (NEO-Five Factor Inventory; Costa & McCrae, 1989) in analyses. Based on prior research (Petker et al., 2019), we included measures of processing speed (Pattern Comparison Processing Speed Test age-adjusted score; Weintraub et al., 2013), episodic memory (Picture Sequence Memory Test age-adjusted score; Weintraub et al., 2013), and fluid intelligence (correct responses on an abbreviated version of Raven’s Progressive Matrices; Bilker et al., 2012) in analyses as covariates in Study 1, which was the only sample with this range of variables available.
As a test of discriminant validity, we examined C-DD in relation to performance on a measure of executive function (Flanker Inhibitory Control and Attention Test age-adjusted score) and sustained attention (Short Penn Continuous Performance Test sensitivity score), which were not expected to correlate with C-DD based on prior research (for details, see Yeh, Myerson, & Green, 2021).
Data Analysis
Cortical Delay Discounting.
In Study 1, cortical delay discounting (C-DD) was calculated by regressing average gray matter thickness in each cortical parcellation on ln(k) values, age, and sex, and extracting the standardized beta coefficient for each regression analysis. We then computed total C-DD by weighting each z-scored cortical thickness parcellation by its corresponding standardized beta coefficient and summing the resulting values (see Supplemental Materials for the calculation). These same beta coefficients were used to create C-DD scores in Studies 2 and 3.
We examined relations between C-DD and criterion variables (e.g., drug use) using logistic or linear regression analyses. R-square values and odds ratios were calculated to provide measures of effect size. Rates of psychiatric disorders were sufficiently high in Study 2 to examine C-DD in relation to the internalizing and externalizing spectra of psychopathology, which we modeled using confirmatory factor analysis. Internalizing was modeled using lifetime symptoms of major depressive, panic, social anxiety, and generalized anxiety disorders (Kendler, Prescott, Myers, & Neale, 2003), whereas externalizing was modeled using lifetime symptoms of substance use, alcohol use, and antisocial personality disorders (Krueger, Markon, Patrick, Benning, & Kramer, 2007).
Results
Study 1
Cortical Delay Discounting.
Average thickness in each cortical parcellation was regressed on delay discounting k-values, age, and sex, resulting in 148 standardized beta coefficients that were used to weight each cortical parcellation that contributed to the C-DD assay. The beta coefficients were predominantly negative (78%), indicating higher C-DD values corresponded to thinner cortex.
Delay Discounting.
C-DD correlated positively with k-values (β = 0.11, SE = 0.05, p<.001, R2 = .01), consistent with the interpretation that higher values on the cortical assay correspond to greater impulsive choice. Given that C-DD is an additive measure of thickness, we examined whether it predicted k-values above and beyond total thickness across the cortex and found that it did (β = 1.07, SE = 0.21, p<.001, ΔR2 = .07).
Cannabis Use.
We tested whether C-DD explained variance in drug use, which is a known correlate of impulsive choice for immediate reward. We focused our analysis on cannabis use, because it was the illicit drug category most commonly endorsed in the sample (54.8% reported lifetime marijuana use). Results of these analyses are presented in Tables 1 and 2. C-DD was a significant predictor of both objective and self-report measures of cannabis use in models accounting for the influence of demographic characteristics, familial risk for substance use, childhood conduct problems, personality traits, and cognitive functioning previously linked to cannabis use. Specifically, C-DD was associated with increased odds of a positive THC urine screen (Table 1) and greater lifetime cannabis use (Table 2).
Table 1.
Cortical Delay Discounting Predicts Increased Odds of Recent Cannabis Use
| THC+ Urine Screen | |||||||
|---|---|---|---|---|---|---|---|
| Step 1 | B | SE | Wald χ2 | OR | P-value | Cox & Snell R- Square |
Chi- Square Test |
| Age | −0.23 | 0.11 | 4.45 | 0.80 | 0.035 | 0.11 | 123.58* |
| Biological Sex | 0.40 | 0.12 | 11.36 | 1.50 | 0.001 | ||
| Parent with Drug or Alcohol Problems | 0.28 | 0.09 | 9.81 | 1.32 | 0.002 | ||
| Childhood Conduct Problems | 0.11 | 0.10 | 1.25 | 1.16 | 0.264 | ||
| Agreeableness | −0.27 | 0.11 | 5.58 | 0.77 | 0.018 | ||
| Conscientiousness | 0.16 | 0.12 | 1.78 | 1.18 | 0.183 | ||
| Extraversion | −0.04 | 0.12 | 0.12 | 0.96 | 0.724 | ||
| Neuroticism | 0.08 | 0.12 | 0.44 | 1.08 | 0.505 | ||
| Openness | 0.54 | 0.11 | 22.94 | 1.72 | <0.001 | ||
| Picture Sequence Memory | −0.33 | 0.11 | 8.61 | 0.72 | 0.003 | ||
| Raven’s Progressive Matrices | −0.41 | 0.11 | 13.40 | 0.67 | <0.001 | ||
| Pattern Completion Processing Speed | −0.25 | 0.11 | 5.56 | 0.78 | 0.018 | ||
| Step 2 | |||||||
| Cortical Delay Discounting | 0.42 | 0.11 | 16.31 | 1.53 | <0.001 | 0.12 | 16.63* |
Note. N = 1105. Sex: woman = 0; man = 1. Parent with Drug or Alcohol Problems: 0 = No; 1 = Yes. Child Conduct Problems = number of problems reported on the SSAGA. Personality Traits measured by the NEO Personality Inventory. Predictors were converted to z-scores to aid interpretation of odds ratios. *p <.001
Table 2.
Cortical Delay Discounting Positively Predicts Lifetime Cannabis Use
| Lifetime Frequency Cannabis Use | |||||||
|---|---|---|---|---|---|---|---|
| Step 1 | B | SE | Beta | t | P-value | R-Square | F Change |
| Age | 0.04 | 0.05 | 0.03 | 0.86 | 0.389 | 0.13 | 12.91* |
| Biological Sex | 0.23 | 0.06 | 0.13 | 4.12 | < 0.001 | ||
| Parent with Drug or Alcohol Problems | 0.14 | 0.05 | 0.09 | 2.94 | 0.003 | ||
| Childhood Conduct Problems | 0.22 | 0.05 | 0.13 | 4.39 | < 0.001 | ||
| Agreeableness | −0.13 | 0.06 | −0.08 | −2.29 | 0.022 | ||
| Conscientiousness | −0.06 | 0.06 | −0.04 | −1.18 | 0.239 | ||
| Extraversion | 0.06 | 0.05 | 0.03 | 1.07 | 0.283 | ||
| Neuroticism | −0.02 | 0.06 | −0.01 | −0.26 | 0.795 | ||
| Openness | 0.35 | 0.05 | 0.21 | 6.87 | < 0.001 | ||
| Picture Sequence Memory | −0.03 | 0.05 | −0.02 | −0.57 | 0.572 | ||
| Raven’s Progressive Matrices | −0.12 | 0.05 | −0.07 | −2.19 | 0.029 | ||
| Pattern Completion Processing Speed | −0.02 | 0.05 | −0.01 | −0.45 | 0.656 | ||
| Step 2 | |||||||
| Cortical Delay Discounting | 0.24 | 0.05 | 0.14 | 4.87 | <0.001 | 0.02 | 23.69* |
Note. N = 1105. Sex: woman = 0; man = 1. Parent with Drug or Alcohol Problems: 0 = No; 1 = Yes. Child Conduct Problems = number of problems reported on the SSAGA. Personality Traits measured by the NEO Personality Inventory. *p <.001.
Discriminant Validity.
We examined whether C-DD was associated with performance on neuropsychological tasks that were not expected to correlate with the delay discounting construct based on prior research, specifically the Flanker Inhibitory Control and Attention (FICA) Test, a measure of executive function, and the Short Penn Continuous Performance (SPCP) Test, a measure of sustained attention (Yeh, Myerson, & Green, 2021). As expected, C-DD was not associated with FICA performance (β = −.039, p =.20), or SPCP performance (β = −.016, p =.58), indicating it is not a measure of cognitive functioning broadly defined.
Study 2
The goal of Study 2 was to examine the replicability of the findings in Study 1 in an independent sample of adults with addiction and psychiatric pathology. We also evaluated the translational significance of the cortical delay discounting score by examining its association with psychiatric disorders. More than half (57.9%) of the sample met criteria for at least one externalizing disorder (Alcohol Use = 35.5%, Substance Use = 48.7%, Antisocial Personality = 7.9%), and 50.0% met criteria for at least one internalizing disorder (Major Depressive = 34.9%; Generalized Anxiety = 13.8%; Panic = 3.9%; Social Anxiety = 9.9%).
Delay Discounting.
C-DD (created using the betas computed in Study 1) was positively associated with k-values (β = 0.29, SE = 0.25, p=.009, R2 = .08). As displayed in Figure 1, this finding replicated the association between C-DD and delay discounting observed in Study 1. Follow-up analyses revealed that C-DD was moderately related to k-values in individuals with a lifetime history of an externalizing disorder (r = .34, p = .017) and unrelated to delay discounting in individuals without an externalizing diagnosis (r = −.08, p = .653).
Figure 1. Correlation between cortical delay discounting and impulsive choice in an independent sample.
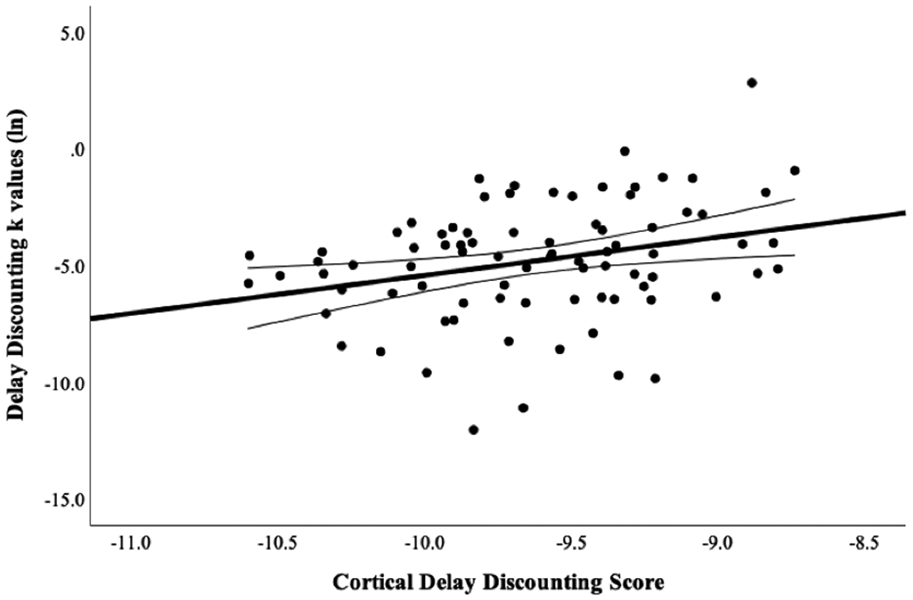
Note. N = 152. Figure depicts relation of the cortical thickness derived measure of delay discounting from Study 1 as a function of delay discounting k-values in Study 2.
Psychiatric Disorders.
We used structural equation modeling to examine whether C-DD predicted symptoms of externalizing and internalizing disorders. Given these disorders are moderately intercorrelated, we examined their relations with C-DD simultaneously to test the hypothesis that the cortical assay would be related to externalizing, but not internalizing, disorders. As depicted in Figure 2, C-DD predicted greater symptoms of externalizing disorders (β = 0.43, SE = 0.07, p< 0.001), but was unrelated to symptoms of internalizing disorders (β = 0.05, SE = 0.12, p = 0.70). The association between C-DD and the latent externalizing variable remained significant with age and sex added to the model (β = 0.21, SE = 0.09, p = .015).
Figure 2. Structural equation model of cortical delay discounting and psychiatric symptoms in adults.
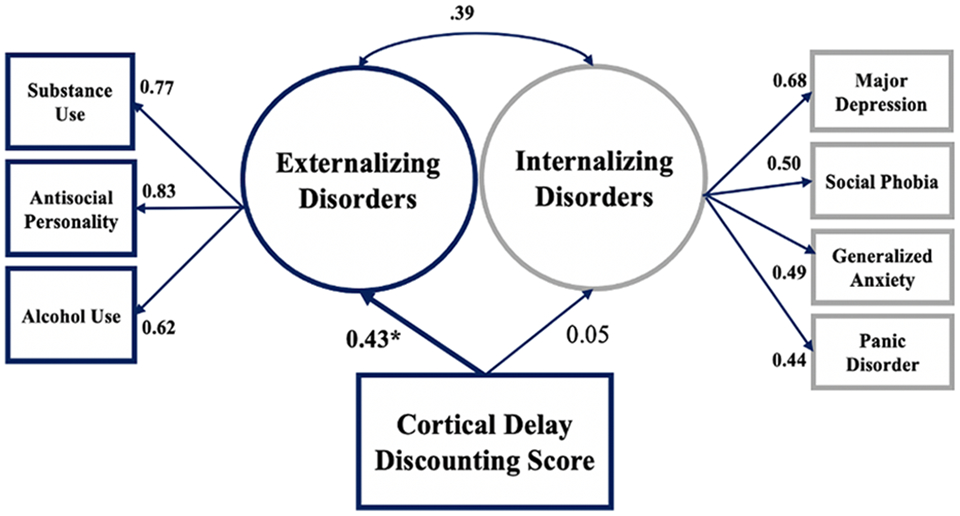
Note. N = 152. RMSEA = .06, SRMR = .06, CFI = .94. Substance Use Disorder symptoms are based on the drug selected as “most problematic” from cannabis, stimulants, opioids, sedatives, hallucinogens. Significant standardized parameter estimates are depicted in bold (p < .001). * p <.001.
Finally, we examined the incremental validity of C-DD when considered in a model with k-values - the traditional measure of delay discounting. Specifically, we added k-values to the structural equation model as predictors of the latent externalizing and internalizing variables. As expected, C-DD positively predicted latent externalizing symptoms (β = 0.36, SE = 0.07, p <.001) with k-values in the model (β = 0.27, SE = 0.12, p =.032), indicating it explains unique variance in this spectrum of psychopathology that is not captured by k-values. In contrast, C-DD (β = −0.01, SE = 0.11, p =.91) and k-values (β = .23, SE = 0.15, p =.12) were unrelated to internalizing symptoms.
Study 3
The goal of Study 3 was to evaluate the predictive validity of the C-DD by examining its association with future delay discounting behavior. The C-DD score was created using the betas computed in Study 1. A linear regression showed that C-DD at baseline positively predicted delay discounting k-values at the follow-up assessment (β = 0.32, SE = 0.11, p=.005, R2 = .10), replicating the association between C-DD and delay discounting behavior using a longitudinal design. Because the Study 2 and 3 samples overlapped, we reran this analysis using only new cases (i.e., participants not included in Study 2) and found the C-DD association with k-values held (β = 0.41, SE = 0.15, p =.01, R2 = .17).
Discussion
Results from three studies provide promising initial support for the development and validation of a whole-cortex assay of impulsive choice. In Study 1, higher cortical delay discounting (C-DD) was associated with greater impulsive choice for immediate rewards and cannabis use - an established correlate of delay discounting (Strickland, Lee, Vandrey, & Johnson, 2020) - above and beyond multiple risk factors for drug use. Cross-validation of the cortical assay in an independent sample with elevated rates of psychiatric disorders replicated the association between C-DD and impulsive choice (k-values). Moreover, C-DD covaried with symptoms of psychiatric disorders that share a susceptibility to addiction and impulsivity (Iacono, Malone, & McGue, 2008; Patrick et al., 2013) above and beyond delay discounting task performance, and prospectively predicted future delay discounting behavior at a magnitude similar to its cross-sectional associations. These findings demonstrate the utility of C-DD for indexing impulsive choice and susceptibility to externalizing disorders, suggesting it measures the underlying pathology that contributes to these syndromes. Together, results from these studies provide initial evidence that C-DD can be used as a neurobiological assay of impulsive choice for immediate rewards and as a possible biomarker of externalizing disorder symptoms.
Development of C-DD in a sample of healthy adults minimized confounds associated with extreme impulsivity, such as the effects of long-term substance abuse and stress exposure on cortical thinning. Nonetheless, part of the promise of developing a cortical assay is its potential utility for measuring neurobiological susceptibility to pathology, which depends in part on how well the measure performs in at-risk samples and can discriminate between clinical phenomena. To begin to evaluate its clinical correlates, we examined C-DD in an independent sample with pronounced psychiatric pathology. Importantly, we computed C-DD based on the betas derived from Study 1, thus avoiding any overfitting issues, and allowing for an independent test of the utility of this measure. As depicted in Figure 1, the association between C-DD and delay discounting replicated in this unseen sample, cross-validating the association observed in Study 1. The reproducibility of this finding is notable given the substantive differences between the samples in terms of psychosocial characteristics, psychiatric diagnoses, and age range. Indeed, the association of C-DD with a widely validated behavioral measure of impulsive choice across two independent samples bolsters confidence in the reliability and construct validity of the assay.
Using structural equation modeling, we also demonstrated that C-DD was positively associated with externalizing disorder symptoms (substance use, alcohol use, antisocial personality), but unrelated to internalizing disorder symptoms (major depression, panic, generalized anxiety, social phobia). These findings not only replicate previous research showing a robust link between psychiatric disorders, delay discounting, and trait impulsivity (Amlung et al., 2019; Odum, 2011b), but extend it by pointing to cortical thickness as an intermediate mechanism instantiating these relationships. Further, the differential associations observed with externalizing and internalizing disorders is evidence of the discriminant validity of the C-DD assay, suggesting it indexes susceptibility for psychiatric disorders characterized by trait impulsivity, rather than mental illness more broadly. Although prior research has shown internalizing disorders are associated with greater discounting of delayed rewards compared to healthy controls (Amlung et al., 2019), our findings suggest C-DD evidences a more robust association with externalizing than internalizing disorders when covariance among these pathologies is considered. Not all psychopathology phenotypes were examined in this study, however, and future research exploring the association of this cortical biomarker with specific types of mental illness and related outcomes that have been linked to impulsivity, like suicide-related behaviors (Serafini et al., 2017), will be important for fully ascertaining the clinical relevance of the C-DD.
Finally, we conducted an initial test of the utility of the C-DD for predicting future delay discounting behavior in a third study and again replicated the positive association between C-DD and k-values. The stability of this association over time is noteworthy given the duration of the follow-up period, which ranged from approximately 6-34 months. Although preliminary, these findings suggest C-DD may provide a novel means of tracking risk for delay discounting over time and/or identifying individuals at elevated risk for these behaviors early in development. Such questions are outside the scope of the current investigation but could easily be addressed by existing longitudinal datasets with cortical thickness measures.
As with any novel measure, replication is required before strong conclusions about its utility can be drawn, and limitations of the study need to be considered. First, the small effect size for the delay discounting analyses suggest C-DD is capturing an aspect of impulsive choice for reward, but it is not the only factor that contributes to or explains discounting behavior. We theorize that C-DD specifically indexes a propensity to discounting future rewards that is conferred specifically by variation in cortical thickness, representing one dimension of a multifactorial process that results in impulsive choice. Thus, although C-DD is a viable biomarker of impulsive choice, it is not sufficient for assaying delay discounting behavior. Second, analyses were conducted in samples that varied in terms of the degree of impulsivity, from a healthy sample (Study 1) to a community sample with elevated psychiatric symptoms (Studies 2-3). We expect C-DD would explain greater variance in delay discounting behavior in samples that are elevated on impulsive phenotypes, such as clinical samples of individuals with addictive or antisocial disorders. Consistent with this hypothesis, follow-up analyses revealed that C-DD was moderately related to k-values in individuals with a lifetime history of an externalizing disorder (r = .34) and unrelated in those without (r = −.08). Therefore, brain-behavior relationships for C-DD are likely stronger in samples with functional impairments associated with discounting decision-making. However, further investigation of C-DD relationships with impulsive phenotypes in diverse clinical samples is required to confirm this interpretation. Third, the use of a single assessment point to derive C-DD prevents consideration of how the cortical instantiation of impulsive choice may vary over time. Along the same line, the utility of this metric was not examined across developmental periods and, thus, the findings may not be generalizable to children, adolescents, or older adults. Longitudinal investigations of the relations between cortical thickness and delay discounting are needed to answer these questions. Fourth, the cross-sectional nature of the data on associations between C-DD and psychiatric symptoms and the relatively small clinical sample precludes strong conclusions from being drawn about the potential utility of C-DD in a clinical setting, including as a diagnostic tool. Research using a prospective design with larger clinical samples than was possible here is needed before its usefulness in a clinical context can be determined. Finally, the validation samples used were modest, necessitating further replication in larger samples.
There are several noteworthy strengths of this study that enhance confidence in the findings. First, the measure was created by combining effect sizes across 148 brain regions, which increases the reliability of the C-DD assay by reducing the likelihood that it is unduly influenced by the effects of outliers. Further, derivation of the score in a sample of over one-thousand healthy adults and testing the reproducibility of our findings in unseen samples enhances confidence in the representativeness and reliability of the metric. We also used publicly available data to create C-DD, ensuring interested researchers can recreate and validate our findings. Finally, C-DD showed expected associations with criterion variables of impulsive choice across a range of methodologies, including diagnostic interviews, surveys, and drug screens, confirming that the observed associations were not due to shared method variance.
Ultimately, validation of C-DD as a biomarker of impulsive choice could reduce reliance on behavioral phenotyping by fostering a more neuroscience-based assessment of impulsive decision-making than is currently available. Such an assay may prove useful for many fields of study given the significance of impulsive choice as a mechanism across disease processes (Bickel et al., 2019). However, the phenotypic complexity of the externalizing spectrum of psychopathology makes it unlikely that a single biomarker, like C-DD, will be sufficient for predicting or explaining this constellation of symptoms. Given the substantial literature documenting the role of subcortical involvement in impulsive choice for reward (e.g., Loganathan et al., 2021; Noda et al., 2020), future research examining the interplay of C-DD with the structure and function of subcortical regions will be important for furthering its construct validity. Moreover, because the developmental and validation studies presented here were conducted with continuous outcome variables (e.g., k-values, psychopathology symptom counts), C-DD was not optimized to predict categorical variables, like diagnostic status. Nonetheless, C-DD may provide novel information about risk for these outcomes that are not captured by other well-established risk factors for externalizing psychopathology. Research examining the value of adding C-DD to established etiological models of externalizing disorders as well as studies investigating how it interacts with extant risk processes, such as aberrant reward processing, trauma exposure, genetic risk, emotional dysregulation, and executive dysfunction (Baskin-Sommers, Curtin & Newman, 2015; Krueger & South, 2009), would be valuable for evaluating the practical utility of C-DD as an assessment tool. Thus, it is premature to conceptualize C-DD as a diagnostic tool based on these initial studies, but it may prove to be a useful predictor of psychiatric outcomes when combined with other risk factors.
In conclusion, the consistency of the findings across studies underscores the potential value of C-DD as an assay of impulsive decision-making and neurobiological susceptibility to externalizing disorders. One advantage of C-DD is that it summarizes cortical thickness associations with impulsive choice across many brain regions in a single score, akin to movement toward the use of polygenic risk scores to index an individual's genetic liability to a trait or disease (Sadeh et al., 2019; Sugrue & Desikan, 2019). Further validation of C-DD will be necessary to continue to investigate how well it measures susceptibility to impulsive choice and externalizing disorders prospectively. For example, although stability and change in C-DD overtime and across development requires further research, the relative stability of cortical thickness in comparison to functional neuroimaging measures means C-DD is likely a marker of trait-like vulnerability for impulsive choice. Thus, research examining how it interacts with more dynamic risk processes will be important for evaluating its predictive validity and utility for identifying individuals at risk of developing or worsening impulsive behaviors and externalizing behaviors.
Supplementary Material
Acknowledgments
Data collection and sharing for this project was provided by the MGH-USC Human Connectome Project (HCP; Principal Investigators: Bruce Rosen, M.D., Ph.D., Arthur W. Toga, Ph.D., Van J. Weeden, MD). HCP funding was provided by the National Institute of Dental and Craniofacial Research (NIDCR), the National Institute of Mental Health (NIMH), and the National Institute of Neurological Disorders and Stroke (NINDS). HCP data are disseminated by the Laboratory of Neuro Imaging at the University of Southern California. This research was also supported by grants from the National Institute of General Medical Sciences [2P20GM103653-06-6527] and National Institute of Mental Health [1R01MH116228] (awarded to Naomi Sadeh, Ph.D.), and National Institute of Mental Health NRSA [1F31MH120936] (awarded to Nadia Bounoua), the National Science Foundation (GRF to Ana Sheehan), and the University of Delaware General University Research fund (awarded to Naomi Sadeh, Ph.D.)
Footnotes
Financial Disclosures
The authors have nothing to declare.
References
- Amlung M, Marsden E, Holshausen K, Morris V, Patel H, Vedelago L, … & McCabe RE (2019). Delay discounting as a transdiagnostic process in psychiatric disorders: a meta-analysis. JAMA Psychiatry, 76(11), 1176–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung M, Vedelago L, Acker J, Balodis I, & MacKillop J (2017). Steep delay discounting and addictive behavior: A meta-analysis of continuous associations. Addiction, 112(1), 51–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow P, Reeves A, McKee M, Galea G, & Stuckler D (2016). Unhealthy diets, obesity and time discounting: a systematic literature review and network analysis. Obesity Reviews, 17(9), 810–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry AB, Koeppel JA, & Ho BC (2020). Impulsive decision making, brain cortical thickness and familial schizophrenia risk. Schizophrenia Research, 220, 54–60. [DOI] [PubMed] [Google Scholar]
- Baskin-Sommers AR, Curtin JJ, & Newman JP (2015). Altering the cognitive-affective dysfunctions of psychopathic and externalizing offender subtypes with cognitive remediation. Clinical Psychological Science, 3(1), 45–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernhardt BC, Smallwood J, Tusche A, Ruby FJ, Engen HG, Steinbeis N, & Singer T (2014). Medial prefrontal and anterior cingulate cortical thickness predicts shared individual differences in self-generated thought and temporal discounting. Neuroimage, 90, 290–297. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Athamneh LN, Basso JC, Mellis AM, DeHart WB, Craft WH, & Pope D (2019). Excessive discounting of delayed reinforcers as a trans-disease process: Update on the state of the science. Current Opinion in Psychology, 30, 59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilker WB, Hansen JA, Brensinger CM, Richard J, Gur RE, & Gur RC (2012). Development of abbreviated nine-item forms of the Raven’s standard progressive matrices test. Assessment, 19(3), 354–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjork JM, Momenan R, & Hommer DW (2009). Delay discounting correlates with proportional lateral frontal cortex volumes. Biological Psychiatry, 65(8), 710–713. [DOI] [PubMed] [Google Scholar]
- Bobova L, Finn P, Rickert M, & Lucas J (2009). Disinhibitory Psychopathology and Delay Discounting in Alcohol Dependence: Personality and Cognitive Correlates. Experimental and Clinical Psychopharmacology, 17(1), 51–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI Jr, … & Schuckit MA (1994). A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. Journal of Studies on Alcohol, 55(2), 149–158. [DOI] [PubMed] [Google Scholar]
- Cho SS, Pellecchia G, Aminian K, Ray N, Segura B, Obeso I, & Strafella AP (2013). Morphometric correlation of impulsivity in medial prefrontal cortex. Brain Topography, 26(3), 479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1989). NEO five-factor inventory (NEO-FFI). Odessa, FL: Psychological Assessment Resources, 3. [Google Scholar]
- Destrieux C, Fischl B, Dale A, & Halgren E (2010). Automatic parcellation of human cortical gyri and sulci using standard anatomical nomenclature. Neuroimage, 53(1), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Siegle GJ, Szanto K, Clark L, Phil D, Reynolds CF 3rd, & Aizenstein H (2012). The temptation of suicide: striatal gray matter, discounting of delayed rewards, and suicide attempts in late-life depression. Psychological Medicine, 42(6), 1203–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn PR, Gunn RL, & Gerst KR (2015). The effects of a working memory load on delay discounting in those with externalizing psychopathology. Clinical Psychological Science, 3(2), 202–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, & Spitzer RL (2015). Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV). Arlington, VA: American Psychiatric Association, 1–94. [Google Scholar]
- Glasser MF, Sotiropoulos SN, Wilson JA, Coalson TS, Fischl B, Andersson JL, … & Wu-Minn HCP Consortium. (2013). The minimal preprocessing pipelines for the Human Connectome Project. Neuroimage, 80, 105–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han X, Jovicich J, Salat D, van der Kouwe A, Quinn B, Czanner S, … & Fischl B (2006). Reliability of MRI-derived measurements of human cerebral cortical thickness: the effects of field strength, scanner upgrade and manufacturer. Neuroimage, 32(1), 180–194. [DOI] [PubMed] [Google Scholar]
- Holt DD, Green L, & Myerson J (2012). Estimating the subjective value of future rewards: Comparison of adjusting-amount and adjusting-delay procedures. Behavioural Processes, 90(3), 302–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono WG, Malone SM, & McGue M (2008). Behavioral disinhibition and the development of early-onset addiction: common and specific influences. Annual Review of Clinical Psychology, 4, 325–348. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, & Neale MC (2003). The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry, 60(9), 929–937. [DOI] [PubMed] [Google Scholar]
- Koffarnus MN, & Bickel WK (2014). A 5-trial adjusting delay discounting task: Accurate discount rates in less than one minute. Experimental and Clinical Psychopharmacology, 22(3), 222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon K, Patrick C, Benning S, & Kramer M (2007). Linking Antisocial Behavior, Substance Use, and Personality: An Integrative Quantitative Model of the Adult Externalizing Spectrum. Journal of Abnormal Psychology, 116(4), 645–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, & South SC (2009). Externalizing disorders: Cluster 5 of the proposed meta-structure for DSM-V and ICD-11: Paper 6 of 7 of the thematic section:’A proposal for a meta-structure for DSM-V and ICD-11’. Psychological Medicine, 39(12), 2061–2070. [DOI] [PubMed] [Google Scholar]
- Noble S, Spann MN, Tokoglu F, Shen X, Constable RT, & Scheinost D (2017). Influences on the test–retest reliability of functional connectivity MRI and its relationship with behavioral utility. Cerebral Cortex, 27(11), 5415–5429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazur JE (1987). An adjusting procedure for studying delayed reinforcement. Commons, ML.; Mazur, JE.; Nevin, JA, 55–73. [Google Scholar]
- McClure SM, Laibson DI, Loewenstein G, & Cohen JD (2004). Separate neural systems value immediate and delayed monetary rewards. Science, 306(5695), 503–507. [DOI] [PubMed] [Google Scholar]
- Odum AL (2011a). Delay discounting: I'm a k, you're a k. Journal of the Experimental Analysis of Behavior, 96(3), 427–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odum AL (2011b). Delay discounting: trait variable?. Behavioural processes, 87(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens MM, Gray JC, Amlung MT, Oshri A, Sweet LH, & MacKillop J (2017). Neuroanatomical foundations of delayed reward discounting decision making. NeuroImage, 161, 261–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ, Venables NC, Yancey JR, Hicks BM, Nelson LD, & Kramer M (2013). A construct-network approach to bridging diagnostic and physiological domains: Application to assessment of externalizing psychopathology. Journal of Abnormal Psychology, 122(3), 902–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petker T, Owens MM, Amlung MT, Oshri A, Sweet LH, & MacKillop J (2019). Cannabis Involvement and Neuropsychological Performance: Findings From the Human Connectome Project. Journal of Psychiatry & Neuroscience, 44(6), 414–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh N, Spielberg JM, Logue MW, Hayes JP, Wolf EJ, McGlinchey RE, … & Miller MW (2019). Linking genes, circuits, and behavior: network connectivity as a novel endophenotype of externalizing. Psychological Medicine, 49(11), 1905–1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salat DH, Buckner RL, Snyder AZ, Greve DN, Desikan RS, Busa E, … & Fischl B (2004). Thinning of the cerebral cortex in aging. Cerebral Cortex, 14(7), 721–730. [DOI] [PubMed] [Google Scholar]
- Serafini G, Canepa G, Adavastro G, Nebbia J, Belvederi Murri M, Erbuto D, Pocai B, Fiorillo A, Pompili M, Flouri E, & Amore M (2017). The relationship between childhood maltreatment and non-suicidal self-injury: A systematic review. Frontiers in Psychiatry, 8, 149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugrue LP, & Desikan RS (2019). What are polygenic scores and why are they important?. JAMA, 321(18), 1820–1821. [DOI] [PubMed] [Google Scholar]
- Strickland JC, Lee DC, Vandrey R, & Johnson MW (2020). A systematic review and meta-analysis of delay discounting and cannabis use. Experimental and Clinical Psychopharmacology. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Kouwe AJ, Benner T, Salat DH, & Fischl B (2008). Brain morphometry with multiecho MPRAGE. Neuroimage, 40(2), 559–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Essen DC, Smith SM, Barch DM, Behrens TE, Yacoub E, Ugurbil K, & WU-Minn HCP Consortium. (2013). The WU-Minn human connectome project: An overview. NeuroImage, 80, 62–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Essen DC, Ugurbil K, Auerbach E, Barch D, Behrens TE, Bucholz R, … & WU-Minn HCP Consortium. (2012). The Human Connectome Project: a data acquisition perspective. Neuroimage, 62(4), 2222–2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weintraub S, Dikmen SS, Heaton RK, Tulsky DS, Zelazo PD, Bauer PJ, … & Gershon RC (2013). Cognition assessment using the NIH Toolbox. Neurology, 80(11 Supplement 3), S54–S64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh YH, Myerson J, & Green L (2021). Delay discounting, cognitive ability, and personality: What matters?. Psychonomic Bulletin & Review, 28(2), 686–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon JH, De La Garza R, Newton TF, Suchting R, Weaver MT, Brown GS, … & Haliwa I (2017). A comparison of Mazur’sk and area under the curve for describing steep discounters. The Psychological Record, 67(3), 355–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, Thomas CS, & Badger GJ (2007). Delay Discounting Predicts Postpartum Relapse to Cigarette Smoking Among Pregnant Women. Experimental and Clinical Psychopharmacology, 15(2), 176–186. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


